 Open Access
Open Access
ARTICLE
Optimism, Social Support, and Caregiving Burden among the Long-Term Caregivers: The Mediating Effect of Psychological Resilience
1 Department of Gerontology and Health Care Management, Chang Gung University of Science and Technology, Taoyuan, 33303, Taiwan
2 Department of Psychology and Counseling, National Taipei University of Education, Taipei, 106, Taiwan
* Corresponding Author: Chia-Hui Hou. Email:
International Journal of Mental Health Promotion 2024, 26(9), 697-708. https://doi.org/10.32604/ijmhp.2024.051751
Received 14 March 2024; Accepted 09 August 2024; Issue published 20 September 2024
Abstract
Background: As the elderly population grows, the demand for long-term care services is increasing. Despite significant investments in care quality and workforce training, long-term care workers often face challenges such as work fatigue, heavy workloads, and inadequate support. These issues can impact job satisfaction, mental health, and care quality, leading to staff turnover. This study examines how optimism, social support, and psychological resilience relate to caregiving burden, aiming to understand their effects on caregivers’ well-being and performance to enhance the quality of long-term care services. Methods: The participants were 542 long-term care workers. Descriptive statistics, t-tests, one-way ANOVA, and hierarchical regression were used for data analysis. Results: (1) Optimism and social support were significantly and positively correlated with psychological resilience and significantly and negatively associated with caregiving burden. (2) Regarding differences in optimism, social support, psychological resilience, and caregiving burden among long-term care workers, females scored significantly higher than males in “social support;” married workers scored significantly higher than unmarried workers in “optimism,” “social support,” and “psychological resilience”; workers aged 45–65 scored significantly higher than those aged 25–45 in “optimism”; workers aged 25–45 scored significantly higher than those aged 45–65 in “caregiving burden”; social workers scored significantly higher than nursing staff in “optimism.” (3) Psychological resilience partially mediated the relationship between social support and caregiving burden concerning explanatory and predictive power. Conclusions: These findings suggest that optimism, social support, and psychological resilience are essential factors in reducing the caregiving burden among long-term care workers. The study highlights the importance of promoting psychological resilience and providing social support to alleviate the burden of caregiving.Keywords
Population aging and low birth rates are global trends. Taking Taiwan as an example, according to the data in 2023, the proportion of older adults in the total population has reached 15%, and it is expected to reach 20% with 4.68 million individuals in 2025. The proportion of older adults is estimated to exceed 30% by 2039 and reach 43.6% by 2070 [1]. Therefore, issues related to older adult care and social support have become necessary, and the demand for long-term care resources and professional labor is increasing.
Taiwan has implemented the “Ten-Year Long-Term Care Plan” since 2007, aiming to combine private resources to establish a complete long-term care system to meet long-term care needs, improve care quality, and reduce the burden on the public. Additionally, there are clear regulations for the qualifications and training methods of long-term care personnel, including pre-service and in-service training, and planning of different education and training models and counseling mechanisms to obtain certificates to improve the quality of care service personnel in Taiwan. However, there is a considerable workforce shortage and turnover rates under various long-term care plans [2].
Studies have found that factors related to the turnover intention of long-term care service personnel in related institutions include work fatigue, workload, supervisor support, health factors, and job satisfaction [3]. This is a significant challenge and source of pressure for employees, especially when facing the expectations and demands of family and work members. Over time, these pressures may lead to negative results, making it difficult for individuals to meet their needs, resulting in physical, psychological, and social problems, role stress, work fatigue, and care burden, thereby reducing care quality and causing the risk of turnover [4].
Therefore, it is essential to understand the optimism, social support, psychological resilience, and care burden of long-term care personnel and their relationships. Further, planning positive talent training, improving positive psychology such as optimism, social support, and psychological resilience, and reducing care burden can effectively construct a resilient care service. This is believed to be helpful for the future long-term care service industry.
Caregiver burden refers to the stress experienced by caregivers due to their caregiving responsibilities and is a crucial factor influencing their quality of life. Caregivers often prioritize the needs of others over their own, neglecting their own need for love and support. Long-term caregiving can restrict their time and social interactions, leading to feelings of isolation and psychological strain, which in turn can result in low mood and a sense of helplessness [5,6]. Common psychological challenges among caregivers include anxiety and depression [7]. Particularly in long-term care settings, the heavy workload, sense of responsibility, and relationship dynamics between caregivers and care recipients can make caregiving overwhelming, contributing to fatigue and stress [8]. Caregiver burden becomes especially pronounced when care recipients have high levels of dependency and behavioral issues. The level of social support available also impacts caregiver burden, with insufficient support exacerbating the burden [9]. Hoenig et al. [7] proposed the concept of burden, which can be subjective and objective. Subjective burden mainly involves caregivers’ feelings when performing care-giving duties, whereas objective burden is events or activities related to negative caregiving experiences [7]. The three characteristics of caregiver burden include: (1) it is self-perceived, (2) it is a combination of multiple pressures, and (3) it changes over time. Caregiver health perception relates to caregiver burden, psychological health, and social support [10]. The consequences of caregiver burden include reduced caregiving, decreased quality of life, and the deterioration of physical and mental health [11]. When caregivers are stressed, lack social support networks, and rely on them, they are more likely to experience caregiver overload [12]. Therefore, paying more attention to the burdens borne by long-term care workers during caregiving is necessary.
The resilience theory refers to how individuals are affected and adapt to challenging situations such as adversity, change, loss, and risk. This theory has been extensively researched in various fields, including psychiatry, human development, and change management [13]. Resilience primarily comes from within individuals and requires resources to support self-care and balance work and life [14,15]. Resilience moderates mediate and prevents adverse effects [16]. It emphasizes the importance of individual traits in situations of adversity and crisis, and research has shown that individuals with high adaptability in high-risk environments tend to possess resilient traits, enabling them to demonstrate better adaptability in crises [17]. Psychological resilience sometimes referred to as “mental fortitude” [18]. According to the American Psychological Association (APA) definition, resilience is the process and outcome of successfully adapting to complex or challenging life experiences. It has mental, emotional, and behavioral flexibility and can adjust to internal and external demands per APA. Resilience has been portrayed as a positive trait that enhances prospects for survival (in the case of organizations) and recovery (in the case of individuals) [19]. Organizations and individuals with high resilience capacity are adaptable and change-oriented [20]. Resilience is often discussed as a desirable feature in and of itself, helping prevent psychological states such as burnout in physicians [21]. Resilience can be considered a factor or relatively stable trait in both the presence and absence of adversity [22,23].
Caring for older adults is a challenging task. Some professionals may find themselves in complex situations for which they may not be prepared. The repercussions of these problematic experiences depend on personal factors. Resilience serves as a buffer against difficulties and experiences [24]. Resilience can help lighten that load, help us better respond to these challenges, and help us bounce back quicker; it influences how you present yourself to the world, your relationships, and how you interact with others and life. Internal and external factors work together [25–27].
In this study, caregiving burden is viewed from the perspective of subjective caregiving burden. It refers to the stress or discomfort experienced by caregivers in the physical, psychological, emotional, economic, and social aspects due to providing care for care recipients. These feelings belong to subjective emotions and perceptions. If these emotions or perceptions are not alleviated or addressed, they may lead to physical and mental discomfort. This viewpoint emphasizes the caregivers’ emotions and subjective experiences. Furthermore, as the study focuses on a broad range of long-term care personnel, their experience of caregiving burden is not entirely negative; it also includes many positive feelings of resilience and achievement. Therefore, the study interprets the concept of caregiving burden based on the foundation of subjective caregiving burden.
Optimism and social support are essential factors for psychological resilience. Optimism refers to maintaining a positive, hopeful, and optimistic attitude towards life. Optimistic individuals tend to believe in their abilities to overcome future challenges and have confidence. This mindset helps individuals maintain a positive outlook when facing adversity, find solutions to problems, and learn and grow from them. Social support refers to emotional, tangible, and informational support received from others. This includes support from family, friends, communities, and organizations. Social support provides emotional support and encouragement, practical assistance, resources, and information and advice. This support helps individuals alleviate stress, enhances their ability to cope with difficulties, and increases psychological resilience. Optimism and social support are interconnected and mutually rein forced. Optimistic individuals are more likely to seek social support, actively and social support enhances their optimistic outlook [28]. The combined effects of these two factors can improve an individual’s ability to cope with stress and adversity and promote the development of psychological resilience. Support is needed to enable informal caregivers to continue their roles as long as possible without compromising their physical or mental health [29]. Effective and adaptive coping strategies may play a protective role in reducing caregiver distress [30]. Perceived social support mediates the association between resilience and burden among caregivers of older adults in Singapore. It is crucial for healthcare professionals, particularly those who interact with and deliver services to assist caregivers, to promote and identify supportive family and friend networks that may help address caregiver burden [31]. Caregivers’ resilience and social support were protective factors against caregiver burden [29]. Optimism or resilience as control-related intrapsychic variables may promote more successful adaptation to the demands involved in providing care, and social support (external re-sources) may also play a protective role in caregivers’ burden [29]. Social support and intergenerational contact are essential for health outcomes in older adults, aging, and ageism [32]. Caregivers may seek social support from family or friends or elicit information from professionals, which can also be a form of social support [33].
Mediation effects of psychological resilience on social support, caregiving burden, and optimism
Individual characteristics influence the number of resources perceived as available, thereby amplifying the effects of others’ resource-depleting or resource-replenishing behaviors [34,35]. For long-term caregivers, the resource balance perspective helps to provide a more integrated understanding and explanation of phenomena such as work stress and occupational burnout, forming a meso-level theoretical model of workplace health.
Psychological resilience has been found to mediate the relationships between social support, caregiving burden, and optimism in caregivers. A study by [33] investigated these mediation effects in a sample of family caregivers of individuals with dementia. The results showed that higher levels of perceived social support were associated with greater psychological resilience in caregivers. In turn, caregivers with higher psychological resilience reported lower levels of caregiving burden and higher levels of optimism.
Psychological resilience therefore appears to be a key mechanism through which social support influences caregiver well-being. Caregivers who feel adequately supported by their social network are more likely to maintain a sense of resilience in the face of caregiving challenges. This resilience then helps buffer against the negative impacts of caregiving stress and burden, while also promoting a more optimistic outlook. These findings highlight the importance of bolstering psychological resilience in caregivers through interventions that enhance social support. Programs that provide caregivers with emotional support, respite care, and other resources may help foster greater resilience and, in turn, reduce burden and increase optimism. Strategies that directly target resilience, such as cognitive-behavioral stress management and mindfulness training, may also be beneficial for caregiver well-being [36–38].
In sum, psychological resilience plays a vital role in the complex interplay between social support, caregiving burden, and optimism. Strengthening caregiver resilience should be a key focus of efforts to support this important population.
The main purpose of this study is to investigate the impact of optimism and social support on caregiver burden among long-term care workers, and to analyze the mediating effect of psychological resilience. This research aims to provide insights for the development and management of long-term care personnel and institutions.
The research process and participants primarily involved purposive sampling. We invited personnel from long-term care institutions in the northern region of Taiwan (Taipei City, New Taipei City, Keelung City, Taoyuan City, Hsinchu County, and Miaoli County) to participate in this study. The investigation period of this study is from 31 July 2023 to 15 September 2023. After obtaining written informed consent approved by the Institutional Review Board of the Chang Gung Medical Foundation (IRB number: 202300837B0), the participants were informed of the study’s purpose, methods and procedures, risks and remedial measures, confidentiality, and participants’ rights. After confirming that they understood and agreed to participate, they completed an online questionnaire. A total of 542 individuals participated in the survey. There were 439 (81%) female and 103 (19%) males. In terms of age, the highest proportion was 336 individuals (62%) between the ages of 46 and 65, followed by 146 individuals (26.9%) between the ages of 25 and 45, 32 individuals (5.9%) under the age of 25, and 28 individuals (5.2%) over 65. Regarding marital status, 217 (40%) were unmarried, and 325 (60%) were married. Regarding the nature of long-term care work, there were 330 caregivers (60.9%), 66 home care supervisors (12.2%), 42 social workers (7.7%), 21 institutional managers (3.9%), and 10 administrative staff members (1.8%).
(1) What is the current status of optimism, social support, psychological resilience, and caregiving burden?
(2) To what extent do demographic variables (e.g., age, gender, marital status, long-term caregivers by task) correlate with levels of optimism, social support, psychological resilience, and caregiving burden among long-term care workers?
(3) What are the associations between optimism and social support, psychological resilience, and caregiving burden?
(4) Do psychological resilience mediate the relationship between optimism, social support and caregiving burden?
This study used four scales to measure the variables of interest: the Chinese version of the Revised Life Orientation Test (CLOT-R), the Multidimensional Scale of Perceived Social Support (MSPSS), the Cannor-Davidson Resilience Scale (CD-RISC), and the Caregiver Burden Inventory (CBI). The scales are described as follows.
Chinese version of the revised life orientation test
The Chinese version of the Revised Life Orientation Test was used to measure the dimensions of “optimism.” This scale was translated and revised by [39]. It is a dual-factor measurement tool comprising six items, and respondents rate their agreement on a five-point Likert scale, ranging from “strongly disagree (1 point)” to “strongly agree (5 points).” A higher average score indicated a higher level of optimism. The internal con-sistency of the CLOT-R, assessed using Cronbach’s α coefficient, was found to be 0.66 after item analysis and item deletion. The results of the Bartlett sphericity test showed no significant correlations among the variables (χ2 = 637.19, df = 15, p < 0.001). The Kaiser–Meyer–Olkin (KMO) value was 0.676, indicating that the CLOT-R is suitable for factor analysis. We determined that the two factors should be retained based on the screen plot by applying an eigenvalue more significant than one criterion. These two factors accounted for 63.21% of the variance. Therefore, the CLOT-R demonstrated acceptable reliability (Cronbach’s α = 0.66) and validity (explained variance of 63.21%). The results showed that the model could be considered satisfactory (χ2 = 38.190, df = 8, GFI = 0.97, CFI = 0.95, RMSEA = 0.084).
Multidimensional scale of perceived social support
The Multidimensional Scale of Perceived Social Support used in this study was developed by Zimet et al. [40] to measure social support. It comprises 12 items and is a du-al-factor measurement tool. Respondents rate their agreement on a five-point Likert scale, ranging from “strongly disagree (1 point)” to “strongly agree (5 points).” A higher average score indicates a higher level of perceived social support. The internal consistency of the MSPSS, assessed using Cronbach’s α coefficient, was found to be 0.96 after item analysis and item deletion. The results of the Bartlett sphericity test showed no significant correlations among the variables (χ2 = 6213.013, df = 66, p < 0.001). The KMO value was 0.942, indicating that the MSPSS was suitable for factor analyses. By applying an eigenvalue more significant than one criterion, we determined that the two factors should be retained based on the screen plot. These two factors account for 77.25% of the variance. Therefore, the MSPSS demonstrated high reliability (Cronbach’s α = 0.96) and validity (explained variance of 77.25%). These research tools were carefully selected and validated to measure the constructs under investigation accurately. The results showed that the model could be considered satisfactory (χ2 = 635.789, df = 53, GFI = 0.83, CFI = 0.91, RMSEA = 0.085).
Cannor-Davidson resilience scale
The Chinese version of the Cannor-Davidson Resilience Scale used in this study was translated by Yu et al. [41] and introduced in Taiwan by Wang et al. [42] after revisions by several Taiwanese scholars. This scale comprises five factors: F1 Personal competence, high standards, and tenacity; F2 Trusting instincts, tolerance of negative affect, and resilience; F3 Positive acceptance of change and secure relationships; F4 Control; F5 Spiritual influences. It contains 25 items, and respondents rate their agreement on a five-point Likert scale, ranging from “strongly disagree (1 point)” to “strongly agree (5 points).” A higher average score indicated a higher level of resilience. The internal consistency of the CD-RISC, assessed using Cronbach’s α coefficient, was found to be 0.97 after item analysis and item deletion. The results of the Bartlett sphericity test showed no significant correlations among the variables (χ2 = 11195.785, df = 300, p < 0.001). The KMO value was 0.968, indicating that the CD-RISC was suitable for factor analyses. We determined that one factor should be retained based on the scree plot by applying an eigen-value more significant than one criterion. This factor accounted for 58.14% of the variance. Therefore, the CD-RISC demonstrated high reliability (Cronbach’s α = 0.97) and validity (explained variance of 58.14%).
The Caregiver Burden Inventory used in this study was based on the scale used by Chien [43]. This scale adopts the widely accepted measurement tool for burden developed by Zarit et al. [44] and Novak et al. [45]. The CBI is a dual-factor measurement tool consisting of 9 items, and respondents rate their agreement on a five-point Likert scale, ranging from “strongly disagree (1 point)” to “strongly agree (5 points).” A higher average score indicates a higher level of caregiver burden. The internal consistency of the CBI, assessed using Cronbach’s α coefficient, was found to be 0.88 after item analysis and item deletion. The results of the Bartlett sphericity test showed no significant correlations among the variables (χ2 = 2926.465, df = 36, p < 0.001). The KMO value was 0.873, indicating that the CBI was suitable for factor analysis. We determined that the two factors should be retained based on the scree plot by applying an eigenvalue more significant than one criterion. These two factors accounted for 71.18% of the variance. Therefore, the CBI demonstrated good reliability (Cronbach’s α = 0.88) and validity (explained variance of 71.18%). These research tools were carefully selected, translated, and validated to ensure accurate measurement of the constructs under investigation in this study. The results showed that the model could be considered satisfactory (χ2= 136.672, df = 26, GFI = 0.95, CFI = 0.96, RMSEA = 0.089).
This study proposes a research framework, as shown in Fig. 1, which explores the relationships among the background variables of long-term care workers, optimism and social support, psychological resilience, and caregiver burden mentioned in the literature review.
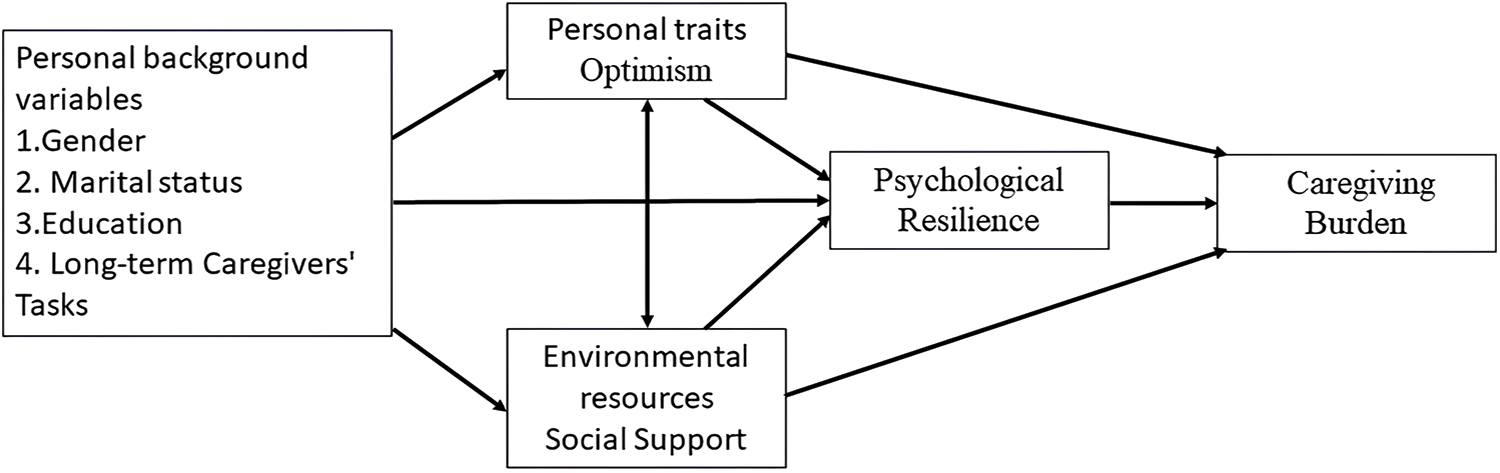
Figure 1: Research framework.
The data collected in this study were analyzed using SPSS for Windows version 22 after removing consistent responses. The following statistical analyses were performed: (1) Descriptive statistics were used to understand the characteristics of the sample and summarize the mean and standard deviation of each observed variable. (2) Pearson’s correlation coefficient was used to calculate the correlation coefficients between optimism, social support, psychological resilience, and caregiver burden. (3) Independent sample t-tests and one-way ANOVA were used to examine differences in optimism, social support, psychological resilience, and caregiver burden among long-term care workers with different background variables. (4) Bootstrapping with 5000 resamples and a 95% confidence interval was used to test the indirect effects of psychological resilience on life orientation and caregiver burden and the mediating effects of psychological resilience on social support and caregiver burden. Hierarchical regression was used to explore the mediating effects of psychological resilience. The results of these analyses will provide insights into the relationships among the variables studied in this research. Further, they will contribute to a better understanding of the factors that influence psychological resilience and the caregiver burden of long-term care workers. A threshold p-value of 0.05 was used to determine statistical significance.
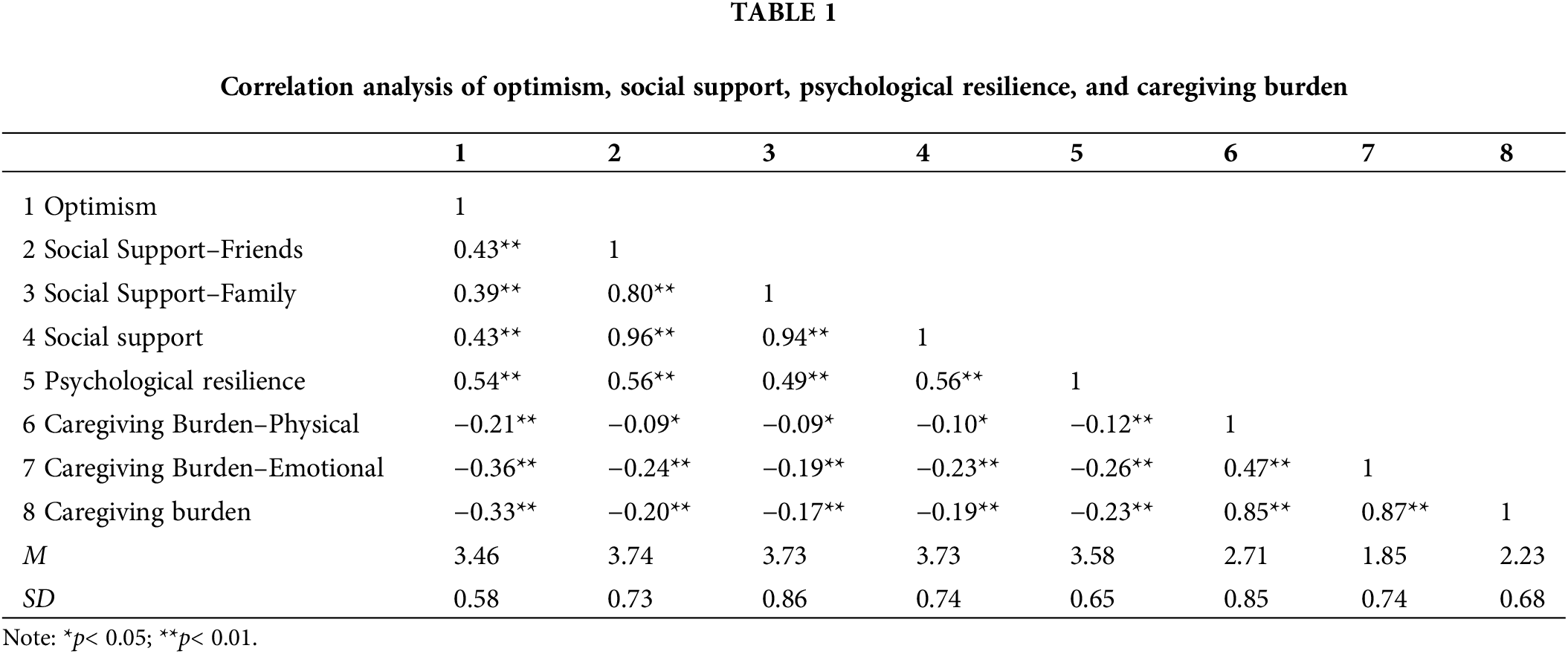
Correlations between optimism, social support, resilience and caregiving burden
Table 1 shows the scores and correlation coefficients for optimism, social support, psychological resilience, and caregiver burden among long-term care workers. Among these four variables, optimism, social support (r = 0.43, p < 0.01), and psychological resilience (r = 0.54, p < 0.01) showed significant positive correlations, whereas caregiver burden (r = −0.33, p < 0.01) showed a significant negative correlation. Social support and psychological resilience (r = 0.56, p < 0.01) showed a significant positive correlation, whereas caregiver burden (r = −0.19, p < 0.05) showed a significant negative correlation. Psychological resilience and caregiver burden (r = −0.23, p < 0.01) showed a significant negative correlation. This indicates that optimism, social support, and psychological resilience have positive effects on each other and negative effects on caregiver burden.
Differences in optimism, social support, psychological resilience, and caregiving burden
This study analyzed differences in Optimism, Social Support, Psychological Resilience, and Caregiving Burden among long-term caregivers based on different background variables. These results can be explained as follows.
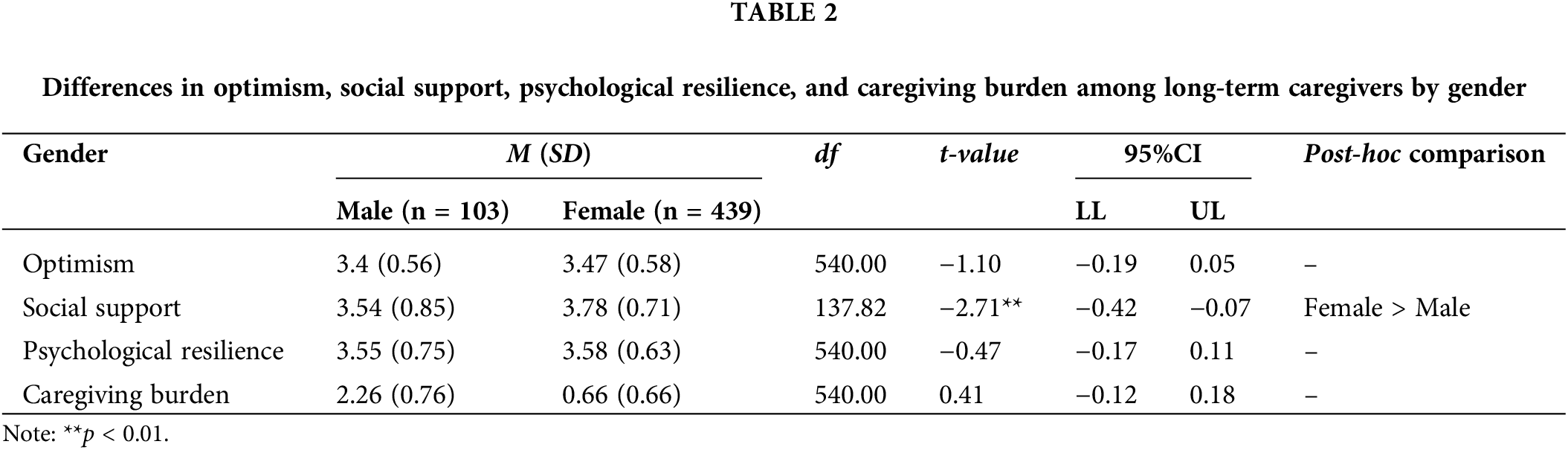
The means, standard deviations, and significance test results for Optimism, Social Support, Psychological Resilience, and Caregiving Burden among participants of different gender are presented in Table 2. Female (M = 3.78, SD = 0.71) showed significantly higher levels of “Social Support” compared to male (M = 3.54, SD = 0.85; t = −2.71, p < 0.001).
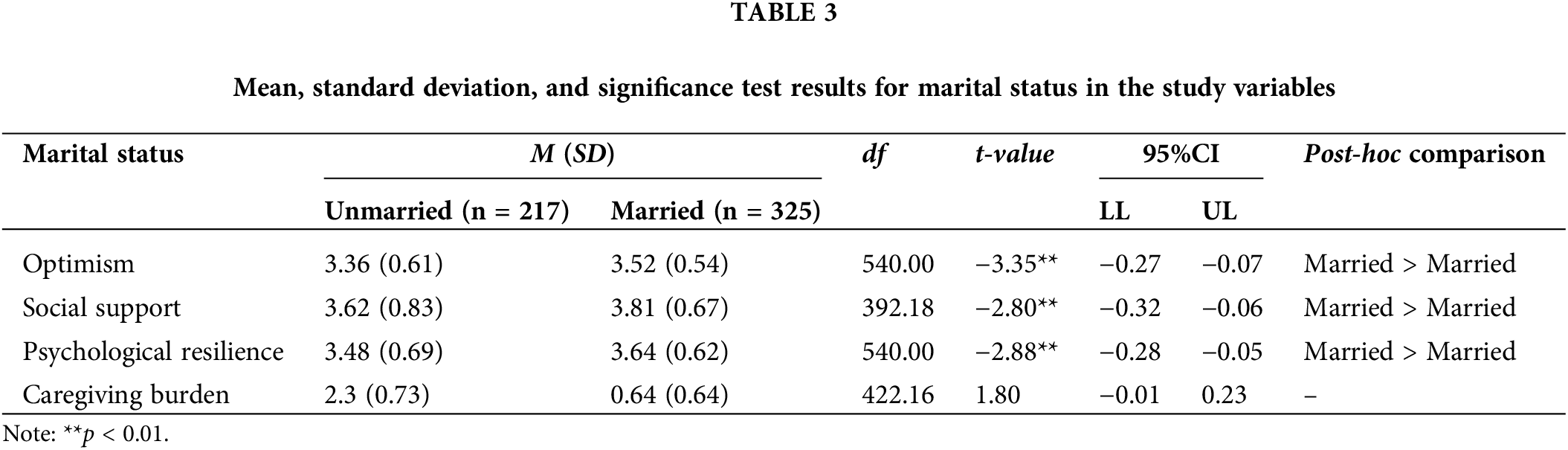
The means, standard deviations, and significance test results for Optimism, Social Support, Psychological Resilience, and Caregiving Burden among participants of different marital statuses are presented in Table 3. Married individuals (M = 3.52, SD = 0.54; M = 3.81, SD = 0.67; M = 3.64, SD = 0.62) showed significantly higher levels of “Optimism” (t = −3.35, p < 0.01), “Social Support” (t = −2.80, p < 0.01), and “Psychological Resilience” (t = −2.88, p < 0.01) compared to unmarried individuals (M = 3.36, SD = 0.61; M = 3.62, SD = 0.83; M = 3.48, SD = 0.69).
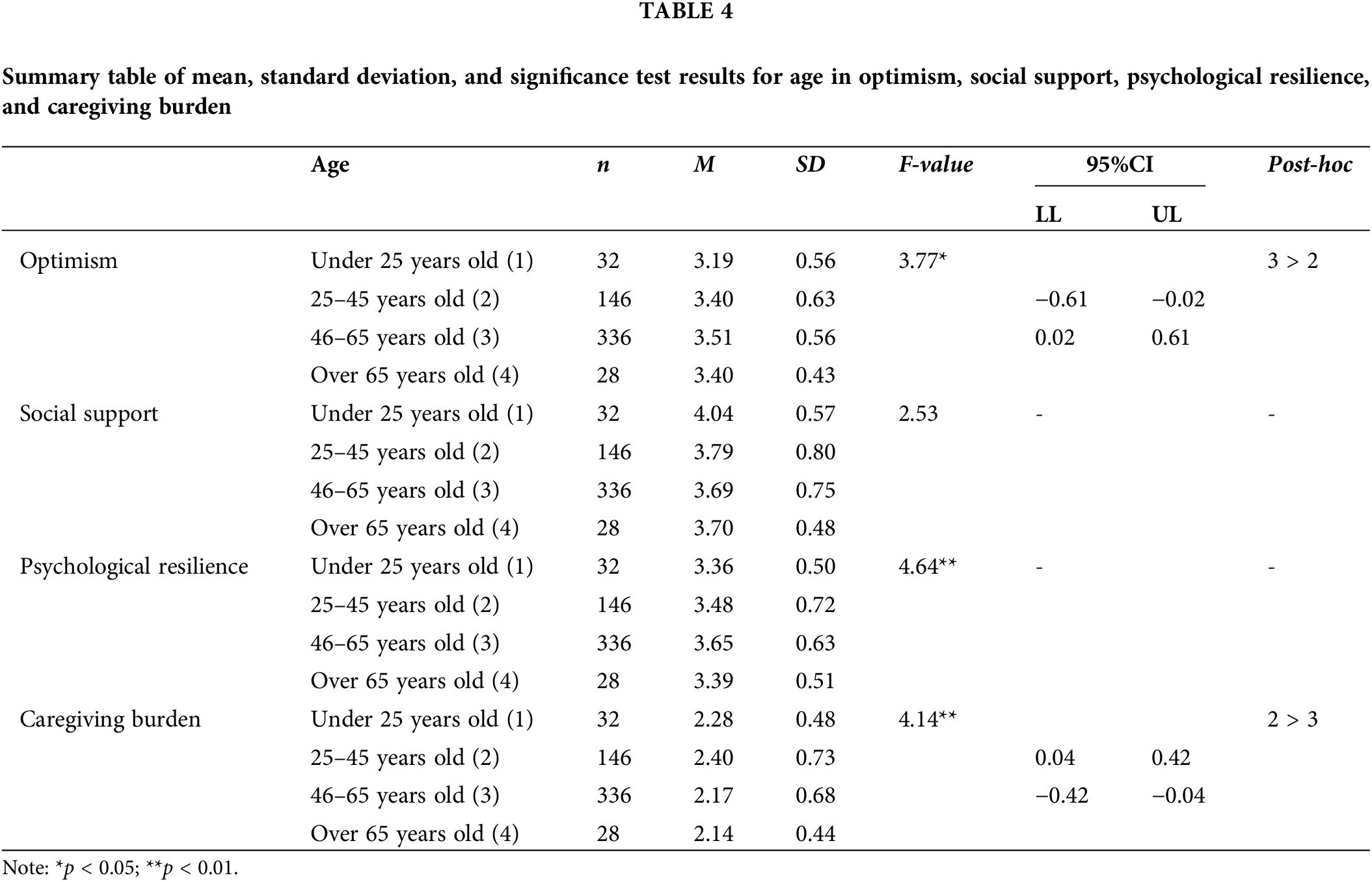
The means, standard deviations, and significance test results for optimism, social support, psychological resilience, and caregiver burden among participants of different age groups are presented in Table 4. Significant differences were found in “Optimism” (F = 3.77, p < 0.01), “Psychological Resilience” (F = 4.64, p < 0.01), and “Caregiving Burden” (F = 4.14, p < 0.01). Further post-hoc comparisons using Scheffé’s method revealed that there was no significant difference in “Psychological Resilience.” In contrast, in “Optimism,” the mean score of the 45–65 age group was significantly higher than that of the 25–45 age group. In “Caregiving Burden,” the mean score of the 25–45 age group was significantly higher than that of the 45–65 age group.
Differences in long-term caregivers’ tasks
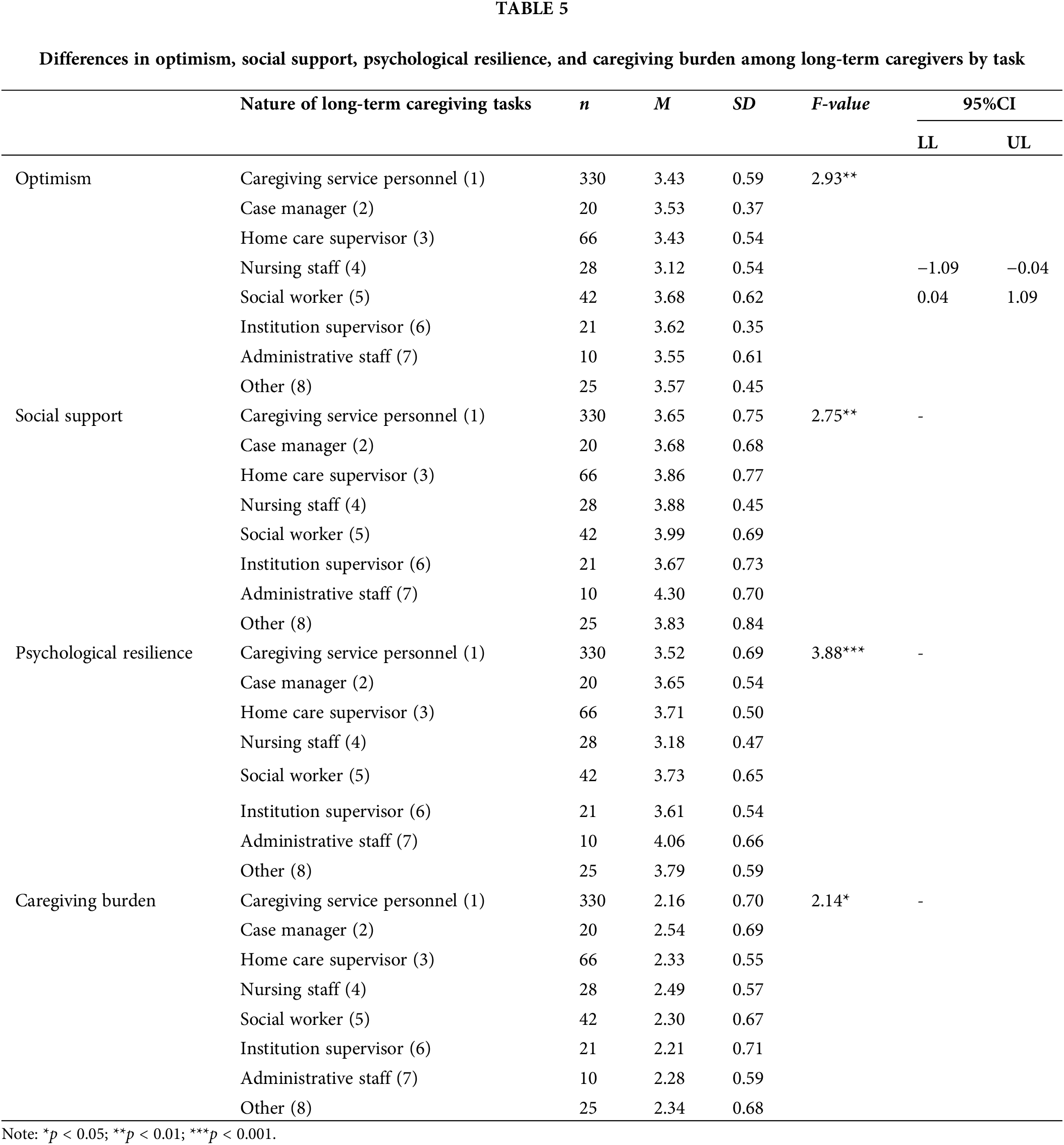
The means, standard deviations, and significance test results for Optimism, Social Support, Psychological Resilience, and Caregiving Burden among participants with different long-term caregiving tasks are presented in Table 5. Significant differences were found in “Optimism” (F = 2.93, p < 0.01), “Social Support” (F = 2.75, p < 0.01), “Psychological Resilience” (F = 3.88, p < 0.001), and “Caregiving Burden” (F = 2.14, p < 0.01). Further post-hoc comparisons using Scheffé’s method revealed that there was no significant difference in “Social Support,” “Psychological Resilience,” and “Caregiving Burden.” However, in “Optimism,” the mean score of social workers was significantly higher than that of nursing staff.
Mediation effects of psychological resilience on optimism, caregiving burden, and social support
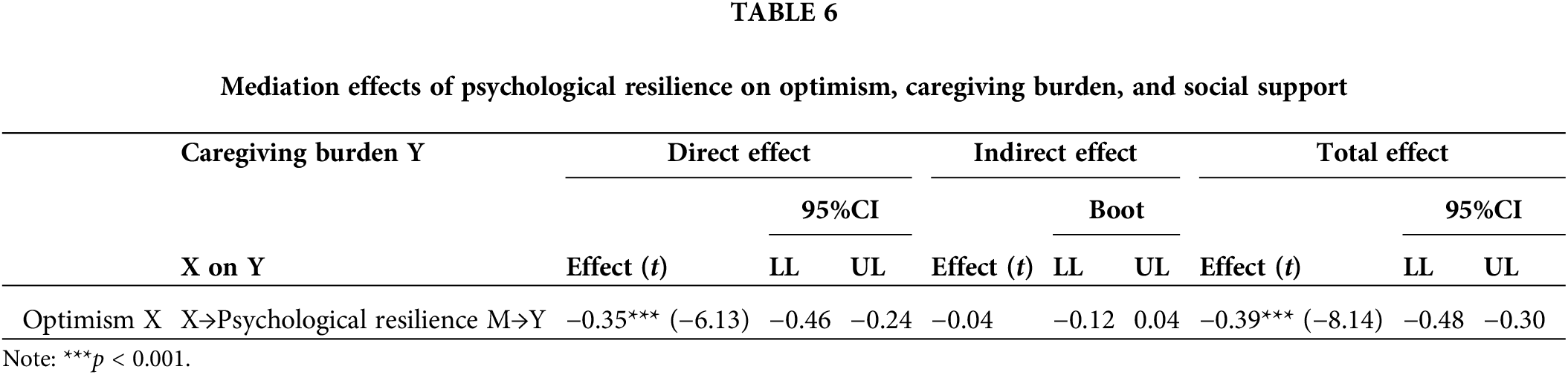
The significance of the mediation effects was tested using bootstrapping, a resampling technique proposed by Efron [46]. Statistical analysis was conducted using a sample obtained from 5000 repeated resampling processes. Mediation regression model 4 from the process software developed by Hayes [47]. Following the analysis guidelines proposed by Cheung et al. [48] and Lau et al. [49] to assess mediation effects. As shown in Table 6, the results of the process model 4 analysis for the path from optimism (X) to psychological resilience (M) to caregiving burden (Y) revealed an indirect effect of −0.04, with a 95% confidence interval, including zero, indicating no significant mediation effect of Psychological Resilience on the relationship between Optimism and Caregiving Burden. Optimism had a significant negative predictive effect on caregiver burden (effect = −0.35, p < 0.001).
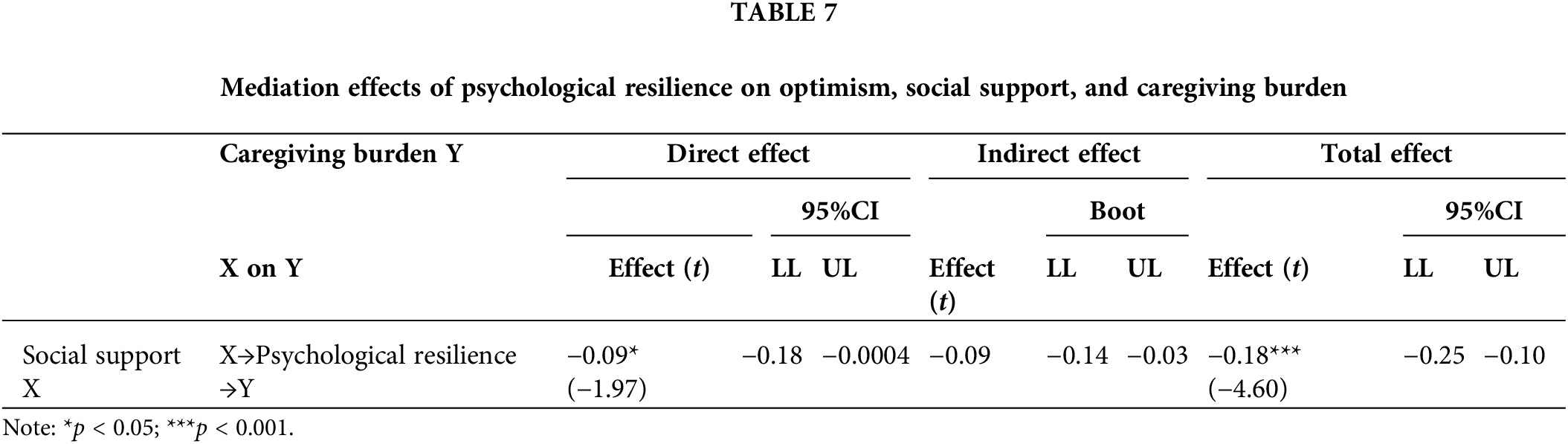
As shown in Table 7, the results of the process model 4 analysis for the path from social support (X) to psychological resilience (M) to caregiving burden (Y) revealed an indirect effect of −0.09, with the 95% confidence interval not including zero, indicating a significant mediation effect of Psychological Resilience on the relationship between social support and caregiving burden. Further observation showed that the direct effect was −0.09, with the 95% confidence interval not including zero, indicating a significant partial mediation effect. Therefore, based on the criteria above for assessing mediating effects, it can be inferred that Psychological Resilience has a significant partial mediating effect on the explanatory predictive relationship between Social Support and Caregiving Burden.
Consistent with extant literature, the results indicate that psychological resilience partially mediates the relationship between social support and caregiving burden. This finding is congruent with studies by [50,51], which identified resilience and social support as protective factors against caregiver burden. The partial mediation observed in our study suggests that while psychological resilience is crucial, social support also exerts a direct influence in alleviating caregiving burden. This underscores the necessity of enhancing both caregivers’ internal resilience and external support systems.
Contrary to some previous studies, our research did not find a significant mediating effect of psychological resilience on the relationship between optimism and caregiving burden. This diverges from findings that propose optimism influences positive adaptation through various mediators, including resilience [52]. Nevertheless, optimism demonstrated a significant direct negative effect on caregiving burden, aligning with prior research suggesting that optimistic individuals are better equipped to manage stressors [53]. This direct effect underscores the potential benefits of fostering optimism among caregivers to mitigate their burden.
This study regarding demographic differences in optimism, social support, psychological resilience, and caregiving burden offer nuanced insights into the experiences of different caregiver subgroups. For example, the higher levels of social support reported by female caregivers compared to their male counterparts align with previous research indicating gender differences in perceived social support [32]. The observed age-related differences, with middle-aged caregivers (45–65 years old) reporting higher optimism and lower burden than younger caregivers (25–45 years old), suggest that life experience and the development of coping skills over time may play a role [54].
The significant differences identified across various long-term care roles (e.g., social workers reporting higher optimism than nursing staff) highlight the importance of considering job-specific factors in understanding caregiver well-being. These findings suggest that interventions and support systems may need to be tailored to address the unique challenges and needs of different caregiver roles within the long-term care system.
Theoretically, our results support the conceptualization of resilience as a dynamic process rather than a fixed trait, as proposed by [55]. The partial mediation effect of resilience between social support and caregiving burden suggests that resilience can be influenced by external factors and, in turn, affect outcomes. This aligns with contemporary resilience frameworks that emphasize the interplay between internal and external resources in promoting positive adaptation [17].
The study’s findings have important practical implications for supporting long-term care workers. The significant role of psychological resilience in mediating the relationship between social support and caregiving burden suggests that interventions aimed at enhancing resilience could be particularly effective. This aligns with recommendations by [56] for resilience-focused interventions to improve coping strategies and reduce symptomatology among caregivers.
Moreover, the direct effects of optimism and social support on reducing caregiving burden highlight the potential benefits of multifaceted interventions that address both individual psychological factors and environmental support systems. This comprehensive approach is consistent with recent calls in the literature for holistic strategies to support caregiver well-being [14,27].
This study contributes to our understanding of the factors influencing caregiving burden among long-term care workers in Taiwan. By highlighting the role of psychological resilience as a mediator and identifying key differences across demographic and professional subgroups, these findings can inform the development of targeted interventions and support systems to enhance caregiver well-being and ultimately improve the quality of long-term care services.
Recommendations for enhancing the psychological resilience of long-term care personnel
The present study results indicate that optimism has a significant direct negative effect on caregiver burden. This aligns with previous research suggesting that optimistic individuals tend to maintain a positive outlook when facing adversity, which can help in managing the stresses associated with caregiving [28]. However, contrary to our expectations, we did not find a significant mediating effect of psychological resilience on the relationship between optimism and caregiver burden. This is somewhat surprising, given that previous studies have suggested that resilience often acts as a buffer against difficulties and challenging experiences [24]. This discrepancy might be explained by the unique context of long-term care work. Unlike family caregivers, who were the focus of many previous studies [34], professional caregivers may have different motivations and coping mechanisms. Their optimism might directly influence their perception of caregiving challenges without necessarily enhancing their psychological resilience. This finding underscores the need for more research specifically focused on professional caregivers in long-term care settings. On the other hand, our analysis revealed a significant partial mediating effect of psychological resilience on the relationship between social support and caregiver burden. This finding is consistent with previous research highlighting the importance of social support in enhancing resilience and reducing caregiver burden [31,32].
The partial mediation suggests that while social support directly reduces caregiver burden, it also works indirectly by enhancing psychological resilience. This result supports the resource balance perspective discussed in the literature [53,54], which posits that individual characteristics (in this case, resilience) influence the perception of available resources (social support), thereby affecting outcomes (caregiver burden). It also aligns with the findings of Halbesleben et al. [34], who found similar mediation effects in family caregivers of individuals with dementia. The significant role of social support in our model emphasizes the importance of interpersonal resources in the caregiving context. As noted by Jafari et al. [33], social support and intergenerational contact are crucial for health outcomes in older adults and those caring for them. Our findings suggest that fostering strong support networks for long-term care workers could be an effective strategy for reducing caregiver burden, both directly and by enhancing psychological resilience. It’s worth noting that while our study focused on subjective caregiver burden, as defined in the literature review, future research might benefit from examining both subjective and objective burden [7]. This could provide a more comprehensive understanding of the caregiving experience in long-term care settings. Moreover, this study findings highlight the potential value of interventions aimed at enhancing both social support and psychological resilience among long-term care workers. As suggested by previous research [35–37], strategies such as cognitive-behavioral stress management and mindfulness training could be beneficial.
Additionally, programs that provide caregivers with emotional support, respite care, and other resources may help foster greater resilience and, in turn, reduce burden. In conclusion, this study contributes to the growing body of literature on caregiver burden by examining these relationships specifically in the context of long-term care work. While our findings largely support previous research on the importance of social support and resilience, they also highlight the unique aspects of professional caregiving that may differ from family caregiving contexts. Future research should continue to explore these nuances to develop targeted interventions for reducing caregiver burden and improving well-being among long-term care workers.
This study found that individual traits and environmental factors differed regarding psychological resilience and caregiving burden. Psychological resilience can serve as a mediator in increasing positive adaptation and reducing negative impacts, an essential factor in helping long-term care personnel achieve reasonable psychological adjustment. Psychological resilience is a dynamic and adaptive process through which direct and indirect strengthening strategies can be established: (1) Direct strategy: When long-term care personnel are under stress, they will have better psychological resilience to help them rebound from adversity if they have positive personality traits (e.g., optimism, hope, and resilience,) or good coping abilities (e.g., problem-focused coping, positive reappraisal, and seeking social support). (2) Indirect strategy: When long-term care personnel do not have positive personality traits or good stress-coping abilities and do not have good psychological resilience for self-adjustment, they can use psychological enhancement to guide themselves to find and create meaning for psychological adjustment, redefine themselves, reassess beliefs, and experience more personal growth [56]. Research has indicated that psychological resilience can be enhanced through stress awareness, cognitive assessment, coping strategies, and seeking social support, which can reduce stress and emotional symptoms [55]. Psychological resilience is no longer seen as a stable trait but a dynamic adaptive process that training can enhance [52]. Increasing support and resources for caregivers, including respite care, psychological counseling, and support groups, is crucial for reducing caregiving stress and improving support systems. These measures are essential for enhancing the quality of life for both caregivers and patients [57]. As personality traits and environmental factors are complex to change, it is imperative to intervene in psychological resilience to improve caregiver stress’s psychological and social impacts on long-term care personnel. This study aimed to apply these results to clinical practice. In the future, psychological enhancement education and training can be used to intervene and strengthen the psychological resilience of long-term care personnel in their psychological care, reduce negative impacts, and help them learn to face the challenges of caregiving work positively. Valuing the cultivation of workers’ psychological resilience and providing appropriate social support and encouragement can help reduce the caregiving burden on long-term care personnel and improve work efficiency.
Recommendations for future research directions
This study has three research limitations: 1. It adopts a cross-sectional design and cannot infer causal relationships. When long-term care personnel experience more positive personal growth and face major stressful events in the future, whether there will be better psychological resilience to cope with stressful events, and whether positive personal growth is also one of the factors that promote psychological resilience, is yet to be determined. 2. The research subjects of this study are long-term care personnel under the Taiwanese system, which is highly heterogeneous. Whether the research results can be generalized to long-term care personnel in other countries requires further comparison and discussion. 3. There are still many potential factors that have not been considered in this study, such as different long-term care service experiences. Whether they will affect the adjustment results of psychological resilience still needs further testing in the future. Future research could explore these relationships in diverse cultural settings and investigate other potential mediators or moderators in the relationship between personal resources (like optimism and social support) and care burden.
Acknowledgement: None.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: Chia-Hui Hou: conception of the idea of investigation, direction, and execution of the investigation and wrote the main manuscript text. Po-Lin Chen: analysis of results, discussion and writing of the manuscript. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The datasets generated and analyzed in the current study are available from the corresponding author upon reasonable request.
Ethics Approval: All methods were carried out in accordance with relevant guidelines and regulations. The study was approved by the Chang Gung Medical Foundation Institutional Review Board (IRB No. 202300837B0). Informed consent was obtained from all subjects and/or their legal guardian(s).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. National Development Council. Report on the population estimation (2022–2070) of the Republic of China; 2022. Available from: https://www.ndc.gov.tw/nc_14813_36128. [Accessed 2023]. [Google Scholar]
2. Zhang J, Lai X. A preliminary exploration of our country’s medical and long-term care system in response to aging; 2022. Legislative Yuan Research Report. Available from: https://www.ly.gov.tw/Pages/List.aspx?nodeid=45615. [Accessed 2023]. [Google Scholar]
3. Chen M. A study on the factors of turnover intention among caregivers in long-term care institutions (Master’s Thesis). Department of Healthcare Administration, Asia University: Taichung, Taiwan; 2012. [Google Scholar]
4. Wang M, Lin J, Huang C. The impact of elderly music activities on caregiver burden from the perspective of adult day care staff. Meiho J. 2014;33:305–30. [Google Scholar]
5. Chen Y-H. Alleviating the shortage of long-term care personnel! Initiating the establish-ment of the “Care Industry Human Resources Alliance”; 2022. Innovative Care. Available from: https://www.ankecare.com/article/2047-2022-07-19-01-57-53. [Accessed 2023]. [Google Scholar]
6. Chu CY, Lee SC, Wang TC, Hsieh JY, Lee CY, Lin HL. A qualitative study of burden among female caregivers. Taipei City Med J. 2010;7:144–53. doi:10.6200/TCMJ.2010.7.2.05. [Google Scholar] [CrossRef]
7. Hoenig J, Hamilton MW. The schizophrenic patient in the community and his effect on the household. Int J Soc Psychiatr. 1966;12:165–76. doi:10.1177/002076406601200301. [Google Scholar] [PubMed] [CrossRef]
8. Martinez ALM, Diaz MB, Soler JAC. Workload experimentation during care, main characteristics to take in consideration for your intervention: negative dimensions, effects and measuring instruments. Cult Cuidados. 2020;24:253–70. doi:10.14198/cuid.2020.58.22. [Google Scholar] [CrossRef]
9. Chiu C-J, Hsu S-P, Wu C-M. Review of domestic research literature on caregiver burden, stress, and coping. J Med Health Sci. 2002;4:273–90. [Google Scholar]
10. Hernández-Padilla JM, Ruiz-Fernández MD, Granero-Molina J, Ortíz-Amo R, López Rodríguez MML, Fernández-Sola C. Perceived health, caregiver overload and per-ceived social support in family caregivers of patients with Alzheimer’s: gender differences. Health Soc Care Commun. 2021;29:1001–9. [Google Scholar]
11. Liu Z, Heffernan C, Tan J. Caregiver burden: a concept analysis. Int J Nurs Sci. 2020;7:438–45. doi:10.1016/j.ijnss.2020.07.012. [Google Scholar] [PubMed] [CrossRef]
12. Kobayasi DY, Rodrigues RAP, Fhon JRS, Silva LM, De Souza AC, Chayamiti EMPC. Overload, social support network and emotional stress on the caregiver of elderly. Av Enferm. 2019;37:140–8. doi:10.15446/av.enferm.v37n2.73044. [Google Scholar] [CrossRef]
13. Guo YF, Cross W, Plummer V, Lam L, Luo YH, Zhang JP. Exploring resilience in Chinese nurses: a cross-sectional study. J Nurs Manage. 2017;25:223–30. doi:10.1111/jonm.12457. [Google Scholar] [PubMed] [CrossRef]
14. Connelly DM, Garnett A, Snobelen N, Guitar N, Flores-Sandoval C, Sinha S, et al. Re-silience amongst Ontario registered practical nurses in long-term care homes during COVID-19: a grounded theory study. J Adv Nurs. 2022;78:4221–35. doi:10.1111/jan.15453. [Google Scholar] [PubMed] [CrossRef]
15. McDonald G, Jackson D, Wilkes L, Vickers MH. Personal resilience in nurses and mid-wives: effects of a work-based educational intervention. Contemp Nurse. 2013;45:134–43. [Google Scholar] [PubMed]
16. Donnellan WJ, Bennett KM, Soulsby LK. What are the factors that facilitate or hinder resilience in older spousal dementia carers? A qualitative study. Aging Ment Health. 2015;19:932–9. doi:10.1080/13607863.2014.977771. [Google Scholar] [PubMed] [CrossRef]
17. Walsh F. Applying a family resilience framework in training, practice, and research: mastering the art of the possible. Fam Process. 2016;55:616–32. doi:10.1111/famp.12260. [Google Scholar] [PubMed] [CrossRef]
18. Hurley K. What is resilience? Your guide to facing life’s challenges, adversities, and crises; 2022. Available from: https://www.everydayhealth.com/wellness/resilience/. [Accessed 2023]. [Google Scholar]
19. Robertson HD, Elliott AM, Burton C, Iversen L, Murchie P, Porteous T, et al. Resilience of primary healthcare professionals: a systematic review. Br J Gen Pract. 2016;66:e423–33. [Google Scholar] [PubMed]
20. Duchek S. Organizational resilience: a capability-based conceptualization. Bus Res. 2020;13:215–46. [Google Scholar]
21. Nituica CB, Bota OA, Blebea J. Specialty differences in resident resilience and burn-out—a national survey. Am J Surg. 2021;222:319–28. [Google Scholar] [PubMed]
22. Troy AS, Willroth EC, Shallcross AJ, Giuliani NR, Gross JJ, Mauss IB. Psychological resilience: an affect-regulation framework. Annu Rev Psychol. 2023;74:547–76. [Google Scholar] [PubMed]
23. Meese KA, Colón-López A, Singh JA, Burkholder GA, Rogers DA. Healthcare is a team sport: stress, resilience, and correlates of well-being among health system employees in a crisis. J Healthc Manage. 2021;66:304. [Google Scholar]
24. Pérez-Rojo G, López J, Noriega C, Velasco C. Resilience among direct care staff in nursing homes: validation of the CD-RISC2. Clin Gerontol. 2023;46:608–18. doi:10.1080/07317115.2022.2111013. [Google Scholar] [PubMed] [CrossRef]
25. Sood A. Everyday health assessment: get your resilience score; 2022. Available from: https://www.everydayhealth.com/wellness/resilience/get-your-resilience-score/. [Accessed 2023]. [Google Scholar]
26. Berkland BE, Werneburg BL, Jenkins SM, Friend JL, Clark MM, Rosedahl JK, et al. A worksite wellness intervention: improving happiness, life satisfaction, and gratitude in health care workers. Mayo Clin Proc Innov Qual Outcomes. 2017;1:203–10. doi:10.1016/j.mayocpiqo.2017.09.002. [Google Scholar] [PubMed] [CrossRef]
27. Bhagra A, Medina-Inojosa JR, Vinnakota S, Arciniegas MC, Garcia M, Sood A, et al. Stress management and resilience intervention in a women’s heart clinic: a pilot study. J Womens Health. 2019;28:1705–10. doi:10.1089/jwh.2018.7216. [Google Scholar] [PubMed] [CrossRef]
28. Segerstrom SC. Optimism and resources: effects on each other and on health over 10 years. J Res Pers. 2007;41(4):772–86. [Google Scholar]
29. Ruisoto P, Contador I, Fernández-Calvo B, Serra L, Jenaro C, Flores N, et al. Mediating effect of social support on the relationship between resilience and burden in caregivers of people with dementia. Arch Gerontol Geriatr. 2020 Jan–Feb;86:103952. doi:10.1016/j.archger.2019.103952. [Google Scholar] [PubMed] [CrossRef]
30. Iavarone A, Ziello AR, Pastore F, Fasanaro AM, Poderico C. Caregiver burden and coping strategies in caregivers of patients with Alzheimer’s disease. Neuropsychiatr Dis Treat. 2014;10:1407–13. [Google Scholar] [PubMed]
31. Ong HL, Vaingankar JA, Abdin E, Sambasivam R, Fauziana R, Tan ME, et al. Resilience and burden in caregivers of older adults: moderating and mediating effects of per-ceived social support. BMC Psychiatr. 2018;18:27. doi:10.1186/s12888-018-1616-z. [Google Scholar] [PubMed] [CrossRef]
32. Yaghoobzadeh A, Sharif Nia H, Pahlevan Sharif S, Hosseinigolafshani SZ, Mohammadi F, Oveisi S, et al. Role of sex, socioeconomic status, and emotional support in predicting aging perception among older adults. Int J Aging Hum Dev. 2018;87:77–89. [Google Scholar] [PubMed]
33. Jafari A, Hesampoor F. The comparison of coping strategies and psychological hardiness between parents of children with cancer of positive and negative responding to treatment. J Ilam Univ Med Sci. 2017;24:189–202. [Google Scholar]
34. Halbesleben JR, Neveu JP, Paustian-Underdahl SC, Westman M. Getting to the COR understanding the role of resources in conservation of resources theory. J Manage. 2014;40(5):1334–64. [Google Scholar]
35. Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: advancing conservation of resources theory. Appl Psychol. 2001;50(3):337–421. [Google Scholar]
36. Brissette I, Scheier MF, Carver CS. The role of optimism in social network development, coping, and psychological adjustment during a life transition. J Pers Soc Psychol. 2002;82(1):102. doi:10.1037/0022-3514.82.1.102. [Google Scholar] [PubMed] [CrossRef]
37. Applebaum AJ, Stein EM, Lord-Bessen J, Pessin H, Rosenfeld B, Breitbart W. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psychooncology. 2014;23(3):299–306. doi:10.1002/pon.3418. [Google Scholar] [PubMed] [CrossRef]
38. Hu T, Xiao J, Peng J, Kuang X, He B. Relationship between resilience, social support as well as anxiety/depression of lung cancer patients: an cross-sectional observation study. J Cancer Res Ther. 2018;14(1):72. doi:10.4103/jcrt.JCRT_849_17. [Google Scholar] [PubMed] [CrossRef]
39. Lai JCL. Psychological impact of economic restructuring in Hong Kong. In: 5th Biennial Conference of the Asian Association of Social Psychology, 2009; Manila, Philippines. doi: 10.1016/j.paid.2009.03.007. [Google Scholar] [CrossRef]
40. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52:30–41. [Google Scholar]
41. Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Pers. 2007;35:19–30. doi:10.2224/sbp.2007.35.1.19. [Google Scholar] [CrossRef]
42. Wang S-H, Wang Z-R, Hsu S-T, Wang M-H. Validity and reliability analysis of the Chinese version of the Connor-Davidson Resilience Scale. Rehabil Couns. 2017;8:47–71. [Google Scholar]
43. Chien PH. Caregiver burden, stress, and coping strategies among caregivers of in-dividuals with dementia: a case study in Taiwan (Master’s thesis). Graduate Institute of Social Work, National Taiwan University: Taiwan; 2017. [Google Scholar]
44. Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1985;25:297–302. [Google Scholar]
45. Novak M, Guest C. Application of a multidimensional Caregiver Burden Inventory. Gerontologist. 1989;29:798–803. doi:10.1093/geront/29.6.798. [Google Scholar] [PubMed] [CrossRef]
46. Efron B. Bootstrap methods: another look at the jackknife. Ann Statist. 1979;7:1–26. doi:10.1214/aos/1176344552. [Google Scholar] [CrossRef]
47. Hayes AF. PROCESS: a versatile computational tool for observed variable mediation, moderation, and conditional process modeling. In: White paper; 2012. [Google Scholar]
48. Cheung GW, Lau RS. Testing mediation and suppression effects of latent variables: bootstrapping with structural equation models. Organ Res Methods. 2008;11:296–325. doi:10.1177/1094428107300343. [Google Scholar] [CrossRef]
49. Lau RS, Cheung GW. Estimating and comparing specific mediation effects in complex latent variable models. Organ Res Methods. 2012;15:3–16. doi:10.1177/1094428110391673. [Google Scholar] [CrossRef]
50. Gallagher MW, Long LJ, Richardson A, D’Souza JM. Resilience and coping in cancer survivors: the unique effects of optimism and mastery. Cognit Ther Res. 2019;43(1):32–44. doi:10.1007/s10608-018-9975-9. [Google Scholar] [PubMed] [CrossRef]
51. Chou Y-C. The impact of optimism and social support on the psychosocial adjustment of breast cancer survivors: the mediating role of psychological resilience (Master’s thesis). National Taiwan University:Taiwan; 2022. [Google Scholar]
52. Carver CS, Scheier MF, Segerstrom SC. Optimism. Clin Psychol Rev. 2010 Nov;30(7):879–89. doi:10.1016/j.cpr.2010.01.006. [Google Scholar] [PubMed] [CrossRef]
53. Conversano C, Rotondo A, Lensi E, Della Vista O, Arpone F, Reda MA. Optimism and its impact on mental and physical well-being. Clin Pract Epidemol Ment Health. 2010;6:25–9. doi:10.2174/1745017901006010025. [Google Scholar] [PubMed] [CrossRef]
54. Kim HH, Kim SY, Kim JM, Kim SW, Shin IS, Shim HJ, et al. Influence of caregiver personality on the burden of family caregivers of terminally ill cancer patients. Palliat Support Care. 2016;14(1):5–12. doi:10.1017/S1478951515000073. [Google Scholar] [PubMed] [CrossRef]
55. Chmitorz A, Kunzler A, Helmreich I, Tüscher O, Kalisch R, Kubiak T, et al. Intervention studies to foster resilience-A systematic review and proposal for a re-silience framework in future intervention studies. Clin Psychol Rev. 2018;59:78–100. doi:10.1016/j.cpr.2017.11.002. [Google Scholar] [PubMed] [CrossRef]
56. Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health. 2008;56:445–53. doi:10.3200/JACH.56.44.445-454. [Google Scholar] [PubMed] [CrossRef]
57. Hoenig J, Hamilton MW. The caregiving burden in Alzheimer’s disease and related disorders. Gerontologist. 1996;36(6):771–7. [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools