 Open Access
Open Access
ARTICLE
Linking 24-h Movement Behavior Guidelines to Cognitive Difficulties, Internalizing and Externalizing Problems in Preterm Youth
1 Body-Brain-Mind Laboratory, School of Psychology, Shenzhen University, Shenzhen, 518060, China
2 Department of Kinesiology and Health, Rutgers University, New Brunswick, NJ 08901, USA
3 Metropolitan University Center of Maringá, Maringá-PR, 87020, Brazil
4 School of Health and Rehabilitation Sciences, AECC University College, Bournemouth, BH5 2DF, UK
5 Research Group Degenerative and Chronic Diseases, Movement, Faculty of Health Sciences Brandenburg, University of Potsdam, Potsdam, 14476, Germany
* Corresponding Author: Yanping Gao. Email:
(This article belongs to the Special Issue: Healthy Lifestyle Behaviours and Mental Health in Children and Adolescents)
International Journal of Mental Health Promotion 2024, 26(8), 651-662. https://doi.org/10.32604/ijmhp.2024.055351
Received 24 June 2024; Accepted 09 August 2024; Issue published 30 August 2024
Abstract
Background: Given the heightened risk of developmental challenges associated with preterm birth, it is crucial to explore interventions that may ameliorate potential adverse outcomes. This study aimed to examine whether meeting the 24-h movement behavior (24-HMB) guidelines, which include recommendations on physical activity (PA), screen time (ST), and sleep (SL), is related to indicators of cognitive difficulties, internalizing problems (e.g., depression and anxiety), and externalizing problems (e.g., difficulties in making friends and arguing) in a sample of preterm youth (children and adolescents born preterm). Method: In this cross-sectional study, data from 3410 preterm youth (aged 6 to 17 years) were included for data analyses. Multivariable logistic regression was used to investigate associations between meeting the 24-HMB guidelines and the above-mentioned health outcomes, while controlling for sociodemographic and health-related factors. Results: The prevalence of meeting 24-HMB guidelines varied across independent and integrated components of the 24-HMB guidelines. Meeting the ST guideline alone (p < 0.05) and integrated guidelines (i.e., ST + SL and ST + SL + PA) were associated with fewer cognitive difficulties and reduced internalizing and externalizing problems (p < 0.05). Specifically, meeting the SL guideline alone and integrated guidelines (i.e., SL + ST) were associated with lower odds of depression and anxiety (p < 0.01). Additionally, meeting independent, and integrated (PA and/or ST) guidelines were associated with less pronounced difficulties in making friends and arguing (p < 0.05). Meeting 24-HMB guidelines in an isolated and integrated manner are linked to better cognitive performance and fewer internalizing and externalizing problems in preterm youth. Conclusion: Results suggest that advocating for the implementation of the 24-HMB guidelines may reduce cognitive challenges and behavioral issues, which is of high relevance for improving public health. Future longitudinal studies in preterm youth should investigate how modifying specific 24-HMB behaviors, especially ST, influence cognitive difficulties, internalizing and externalizing problems in this vulnerable population.Keywords
Recent estimates suggest that in 2020, 9.9% of all worldwide live births (approximately 13.4 million in absolute numbers) were preterm (referring to any successful live birth occurring before 37 weeks of pregnancy), and global deaths in preterm infants have reached 1 million [1]. For the 2016 US birth cohort, the discounted present value of the excess cost associated with preterm birth was estimated at $25.2 billion, with a lifetime incremental cost per preterm child of $64,815 compared to a full-term child [2]. In light of the growing prevalence of preterm births and their consequences on public health and economic resources, it is important to investigate cost-efficient strategies for enhancing the quality of life and health among preterm individuals, especially at early stages of life including childhood and adolescence (hereafter referred to as youth).
Notably, preterm infants are at a higher risk of immediate health complications at birth [3,4] as well as health issues throughout their lives including life stages such as middle childhood and adolescence [5–7]. Several studies provide evidence that preterm youth are at higher risk for negative health consequences including but not limited to cognitive difficulties [8,9], depression [10,11], anxiety [11,12], and behavioral issues [13,14] compared to full-term-born children. Specifically, preterm youth also exhibit a greater susceptibility to externalizing problems, such as excessive arguing and difficulties in making friends [15–17]. Addressing these negative behaviors and other health risks associated with preterm youth is costly, and burdensome for family members, and requires the availability of qualified professionals [2], which in turn may limit the accessibility of such intervention approaches for those in need.
Notably, findings of previous research suggest that higher levels of physical activity (PA) [18,19], sufficient sleep duration [20], and reduced screen time (ST) [21] can improve the quality of life and physical health of youth born preterm. Therefore, it is reasonable to assume that promoting lifestyle changes such as engaging in PA, getting sufficient sleep, and minimizing ST is a promising intervention strategy to reduce health issues associated with preterm birth. These lifestyle changes can be implemented at minimal cost and are thus accessible to everyone. However, few studies have examined the influence of these lifestyle factors from a holistic perspective, such as the 24-h movement behavior (24-HMB) framework, among preterm youth. The holistic framework referred to as the 24-h Movement Behaviors guidelines considers the interdependence of the lifestyle factors PA, sedentary behavior (SB), and sleep (SL), and recommends a minimum of 60 min of moderate-to-vigorous PA per day, no more than 2 h of ST, and sleep durations of 9–11 h for healthy development [22–24]. Several studies indicate that meeting these 24-HMB guidelines is associated with better physical, cognitive, emotional, and social development, as well as overall well-being, in neurotypical youth and those with neurodevelopmental disorders [25,26].
Despite these promising findings, it remains unclear whether such positive associations between meeting 24-HMB guidelines and reduced risk of cognitive difficulties, internalizing problems, and externalizing problems are generalizable to preterm youth. To this end, we aimed to explore associations between meeting 24-HMB guidelines and indicators of the health-related domains among preterm youth. Specifically, we hypothesized that meeting one or more components within 24-HMB guidelines is associated with lower odds of (i) cognitive difficulties; (ii) internalizing problems; and (iii) externalizing problems.
This cross-sectional study used data from the U.S. National Survey of Children’s Health (NSCH), conducted between June 2022 and January 2023. A total of 54,103 parents or legal guardians responded to the NSCH survey in 2022. Further details on the survey’s data collection are accessible at (https://www.childhealthdata.org, accessed 20 July 2024). This study followed established protocols similar to those in earlier research [25,26], except for the criteria for selecting the specific population in our study. This research focused on youth aged between 6–17 years who were born prematurely, defined as being born at least 3 weeks before their expected due date. After excluding all non-preterm children, children under 6 years, and invalid data across various variables (e.g., excluding participants with missing data values for depression), we finally retained a valid dataset of 3410 participants. Detailed descriptions of the assessments used in this study are provided below. The study was approved by the Ethics Committee of the Shenzhen University (IRB number: PN-2022-00075). No participants received financial incentives, and all participants signed the informed consent in this study.
Demographic and medical information
This study included factors like sociodemographic variables (e.g., gender, family income, ethnicity, primary caregiver’s education) [27–29], overweight status [30], and adverse childhood experiences [31] that were known to significantly influence youth health. Additionally, parental emotional support, household child count, mental health care, and the severity of preterm birth are also known to influence health-related parameters in youth [32–36]. Therefore, these variables were included as covariates in our statistical analysis. Specifically, youth were identified as overweight based on caregiver reports of a medical professional’s diagnosis. Adverse childhood experiences were operationalized as challenging events encountered during early childhood, including financial hardships that affect basic needs, parental divorce or separation, the death of a parent or guardian, and similar distressing life circumstances. Parental emotional support was measured by caregivers’ access to emotional help for parenting within the last year. Mental health care utilization indicated whether the child received professional mental health treatment or counseling during the same period.
The 24-HMB guidelines include 3 key components: PA, ST, and SL. These guidelines were operationalized numerically and categorically. Specifically, the number of guidelines met can fall within a range of 0 to 3, while the 3 component(s) can be categorized individually (i.e., PA, ST, or SL) or in combinations of meeting the 24-HMB guidelines (i.e., PA + ST, PA + SL, ST + SL, or PA + ST + SL).
To determine whether preterm youth met the PA guideline, a single-item question was asked to the caregiver(s) of the participating children: “During the past week, on how many days did your child exercise, play a sport, or participate in physical activity for at least 60 min?” Respondents were provided with four response options (1 = 0 days, 2 = 1–3 days, 3 = 4–6 days, and 4 = daily). Those whose parents chose option 4 (daily) were deemed to have met the PA guidelines.
Second, ST was measured using a single-item question: “On most weekdays, about how much time does your child usually spend in front of a TV, computer, cell phone, or other electronic device watching programs, playing games, accessing the internet, or using social media, not including schoolwork?” Parents had five options to choose from: 1) under 1 h/day, 2) 1 h/day, 3) 2 h/day, 4) 3 h/day, and 5) 4 h/day or more. Children whose parents selected options 1 to 3 were considered compliant with the ST guidelines.
Third, SL was evaluated with a single-item question: “During the past week, how many hours of sleep did your child get on most weeknights?” The answers were rated on a 7-point scale (1 = less than 6 hours, 2 = 6 h, 3 = 7 h, 4 = 8 h, 5 = 9 h, 6 = 10 h, 7 = 11 h or more). Based on the child’s age, different responses indicated compliance with the SL guideline: for children aged 5 to 13, 9 h or more (options 5 to 7 h) were deemed appropriate, while for adolescents aged 14 to 17 years, 8 to 10 h (options 4 to 6) were considered adequate.
Cognitive difficulties were assessed using the following parent-reported single-item question: “Does this child have serious difficulty concentrating, remembering, or making decisions because of a physical, mental, or emotional condition? [25]” Responses were binary: 0 (no) or 1 (yes).
Internalizing issues were identified based on responses to two distinct questions posed to the primary caregiver(s): (a) “Does your child have anxiety problems?” and (b) “Does your child have depression?” An affirmative response to either question resulted in the child’s inclusion in the study.
Externalizing problems were evaluated through two distinct questions provided by the primary caregiver(s): (a) “Compared to other children their age, how much difficulty does this child have making or keeping friends?” Responses were scored on a 3-point scale: 1 (no difficulty), 2 (some difficulty), and 3 (a lot of difficulty). (b) “How often does this child argue too much?” Responses were scored on a 4-point scale: 1 (always), 2 (often), 3 (sometimes), and 4 (never).
In this study, the statistical analysis was conducted using the Stata software (StataCorp. 2023. Stata Statistical Software: Release 18. College Station, TX: StataCorp LLC.). A composite variable named STRATACROSS was generated by merging the state residency code (FIPSST), the youth-marked household identifier (STRATUM), and the unique household ID to facilitate the use of sampling weights in the analysis. Subpopulations were identified as premature-born youth if they were born alive before 37 weeks of pregnancy. Descriptive statistics were computed for all variables. Continuous data were summarized with average values and standard deviations, while categorical data were presented through counts and percentages, adjusted for weights. Odds ratios (OR) and their 95% confidence intervals (95% CI) were calculated using multivariable logistic regression to determine the association between compliance with 24-HMB guidelines and various outcomes, including cognitive difficulties and both internalizing (e.g., depression, anxiety) and externalizing issues (e.g., socializing challenges, excessive arguing). The adherence to 24-HMB guidelines was examined both in terms of the total number of guidelines met (as a continuous variable) and meeting each guideline individually (as categorical variables) within the statistical models. Factors considered in the analysis were age, gender, ethnicity, household economic status, family size, the education level of the primary caregivers, whether the child was overweight, exposure to adverse experiences in childhood, access to emotional support, and mental health service utilization. The threshold for statistical significance was set at p < 0.05 for all statistical tests.
The study encompassed responses from 3410 preterm-born young people, ranging from 6 to 17 years old. Participant characteristics were male (54.46%), white (76.42%), and received emotional support (79.44%). The average age was 11.86 years. Nearly 69% of the households surveyed had incomes exceedingly twice the federal poverty threshold, while over half of the caregivers (58.04%) possessed a college degree or higher education. Mental health services were utilized by 19.74%, with 21.73% of the participants showing high anxiety and 10.12% signs of depression.
Results showed that 20.50% (699 individuals) of the preterm youth failed to meet any component within 24-HMB guidelines. Over 42% (1449 participants) of the study sample met one of the three 24-HMB guidelines: 28.45% (N = 970) for SL, 10.47% (N = 357) for ST, and 3.58% (N = 122) for PA. Furthermore, 29.7% of the participants (N = 1013) met two of the three 24-HMB guidelines. The most commonly met combinations were ST + SL (N = 724, 21.23%), followed by PA + SL (N = 198, 5.81%), and PA + ST (N = 91, 2.67%). Additionally, only 7.30% (249 preterm youth) met all 24-HMB guidelines. More detailed information can be found in Table 1. To visualize our results, we used a Venn diagram (see Fig. 1) that shows the specific numbers and actual proportional sizes of preterm youth meeting the specific guidelines of the 24-HMB framework. In Fig. 2, we provide a graphical summary of our findings.
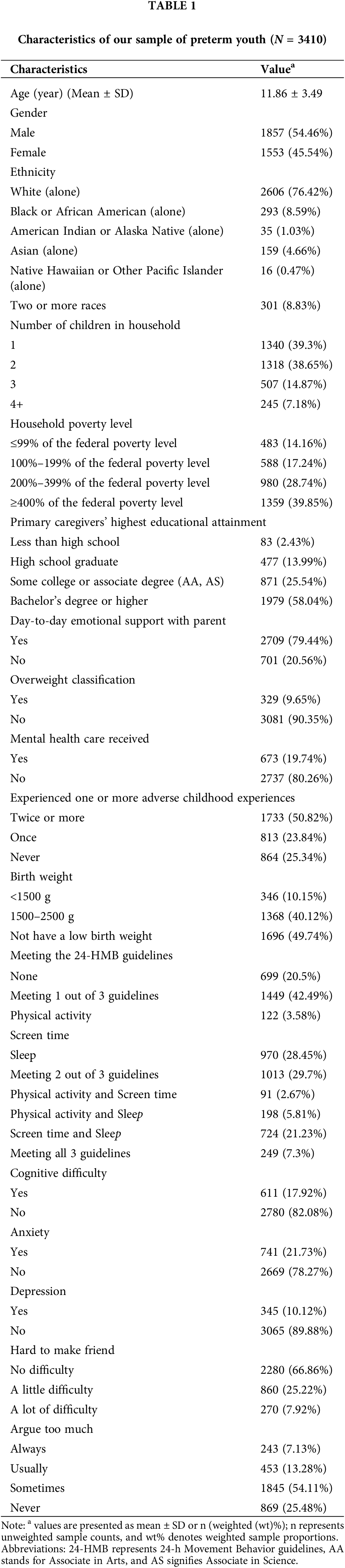
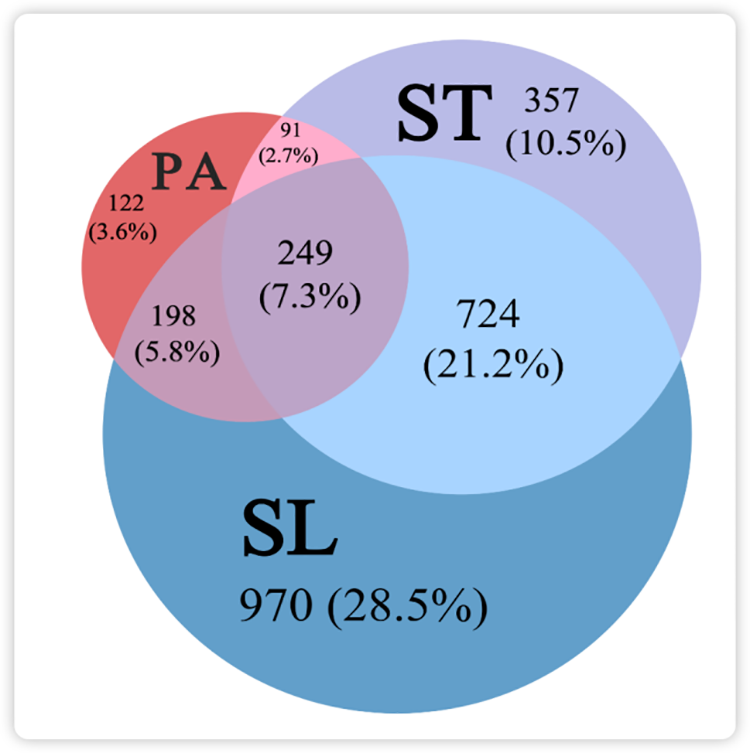
Figure 1: Venn diagram illustrating the proportions of participants meeting specific guidelines of the 24-HMB recommendations (PA: physical activity, ST: screen time, SL: sleep). Values are shown as n (wt%), where n indicates unweighted sample counts and wt% represents weighted sample proportions. Note: 699 participants (20.5%) did not meet any of the 24-HMB guidelines.
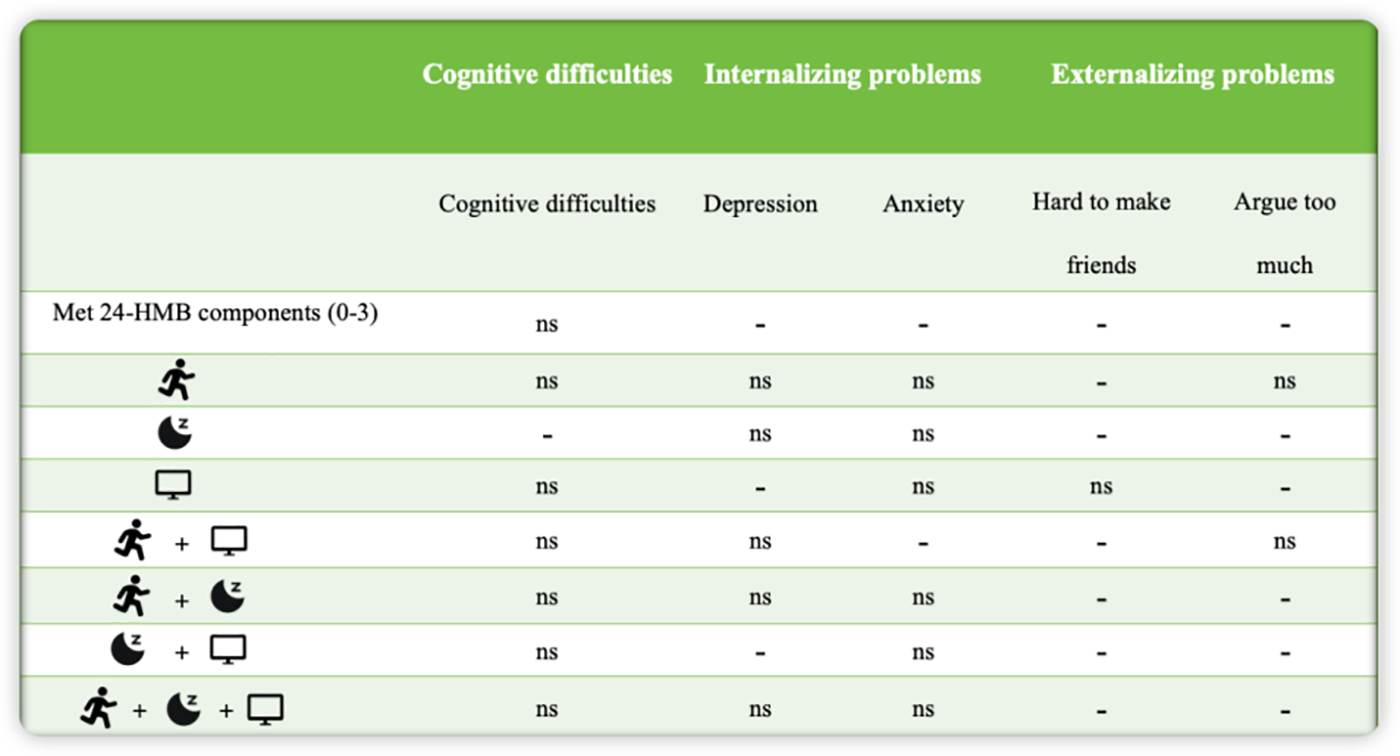
Figure 2: Associations between meeting to 24-HMB guidelines and cognitive difficulties, internalizing, and externalizing problems among preterm youth. “ns” denotes no significant association, while “-” indicates a negative correlation.
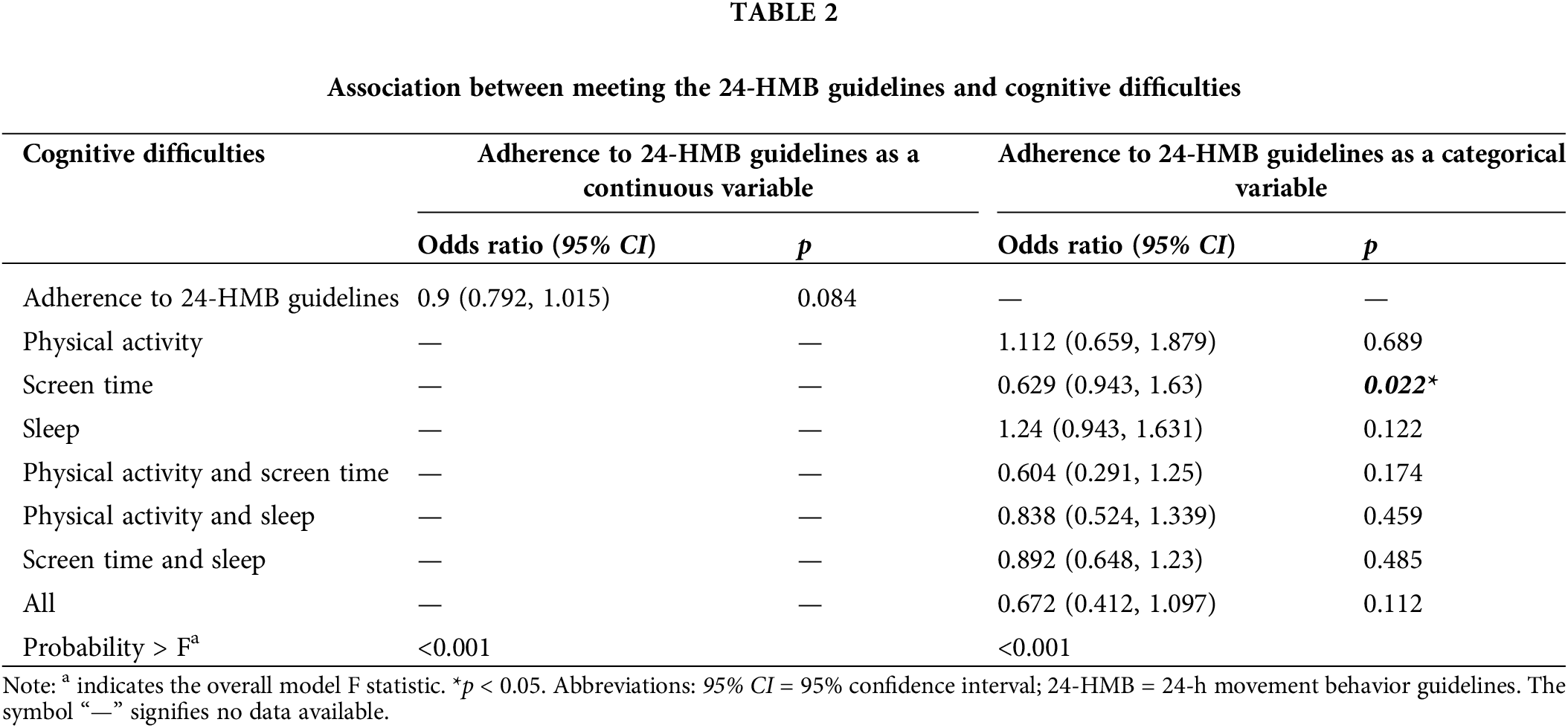
Association between meeting the 24-HMB guidelines and cognitive difficulties
Table 2 illustrates the relationship between meeting the 24-HMB guidelines and cognitive difficulties. When treated as a continuous variable, no significant association was found between adherence to the 24-HMB guidelines and cognitive difficulties (OR = 0.9, 95% CI = 0.797–1.015, p = 0.086). However, compared to not meeting any of the 24-HMB guidelines, meeting the ST guideline was associated with a lower likelihood of cognitive difficulties (OR = 0.639, 95% CI = 0.429–0.952, p = 0.028).
Association between meeting the 24-HMB guidelines and internalizing problems
Table 3 displays the association between meeting the 24-HMB guidelines and depression. When treated as a continuous variable, a higher number of 24-HMB guidelines met was associated with a lower risk of depression (OR = 0.703, 95% CI = 0.582–0.849, p < 0.001). In the categorical analysis, meeting the SL guideline (OR = 0.609, 95% CI = 0.423–0.876, p = 0.008) or meeting both the ST and SL guidelines (OR = 0.354, 95% CI = 0.220–0.569, p < 0.001) was associated with lower odds of depression. The overall model was statistically significant (p < 0.001).
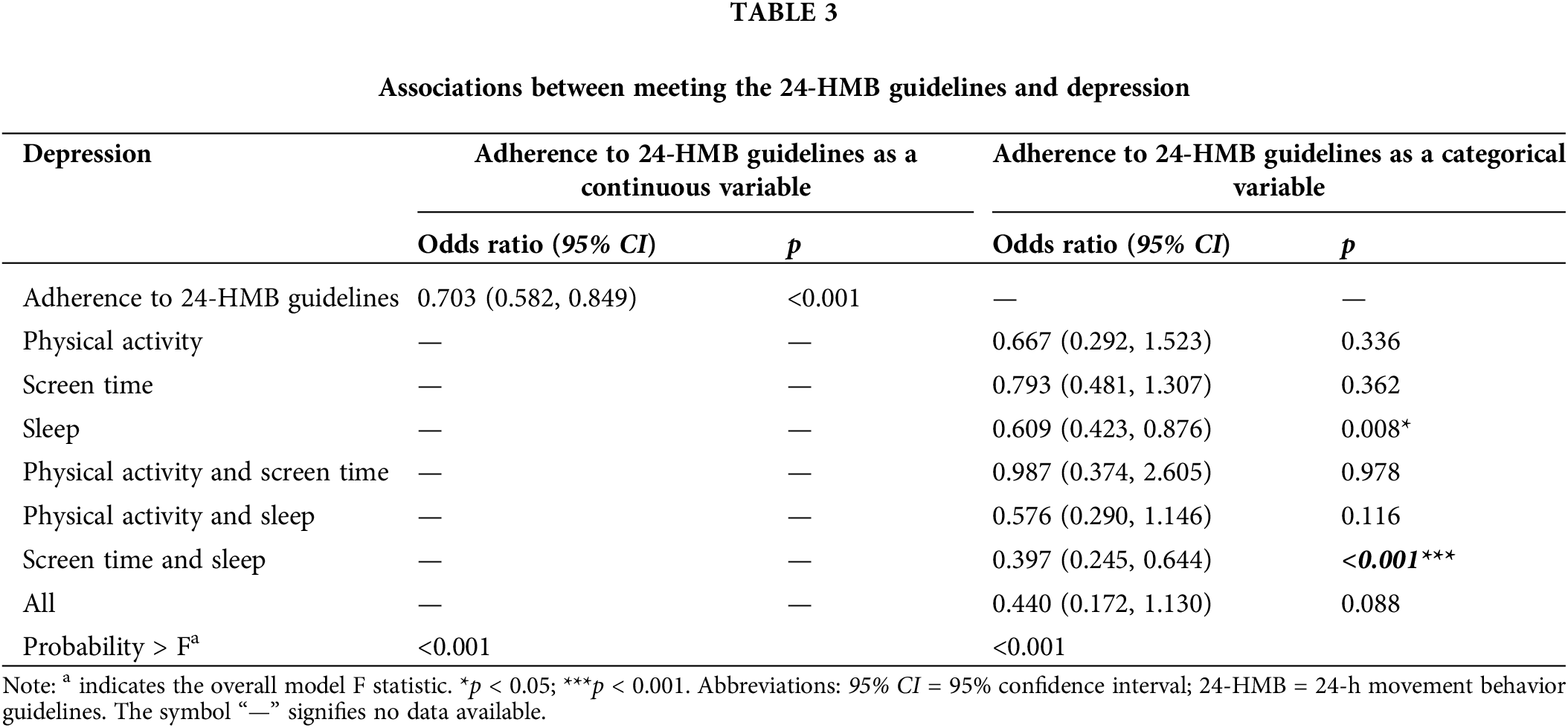
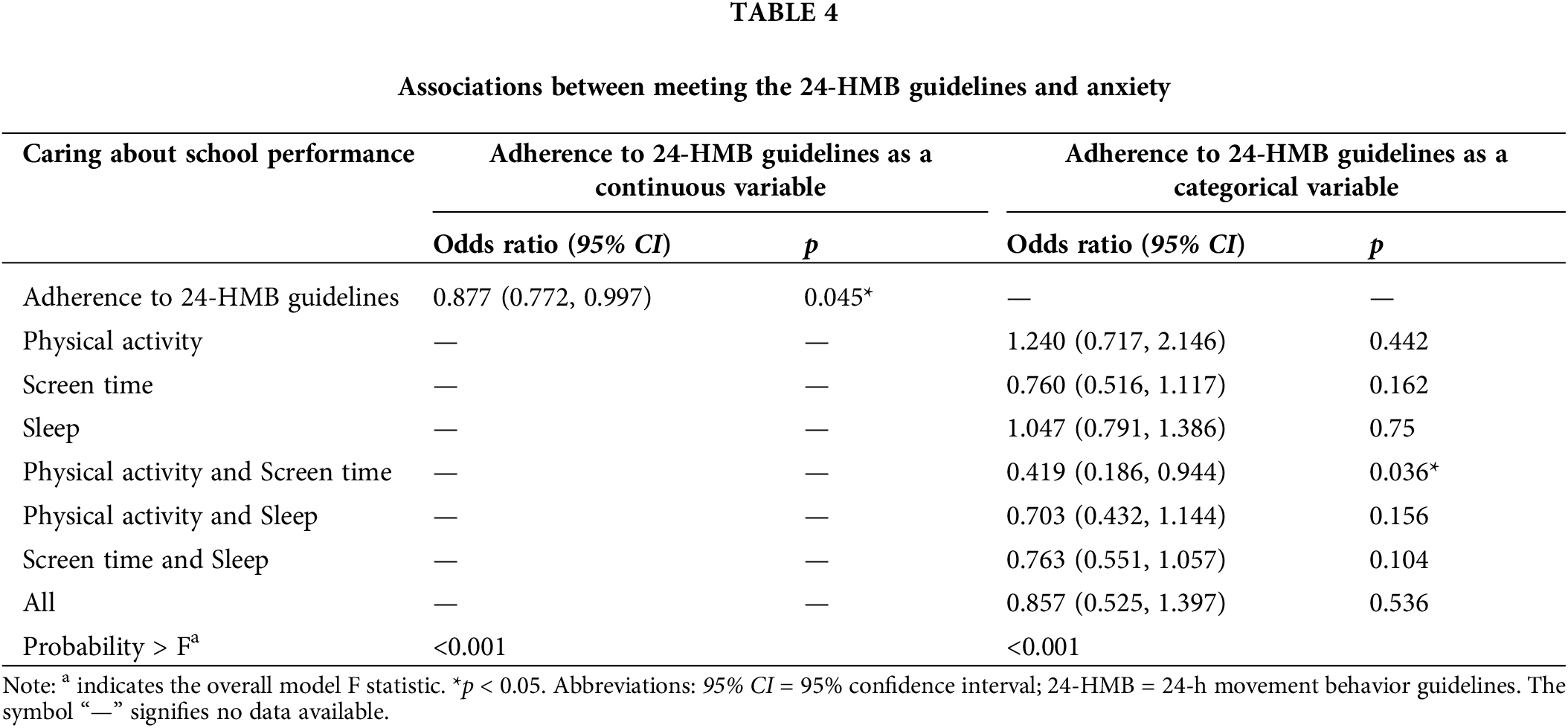
Table 4 summarizes the associations between meeting the 24-HMB guidelines and anxiety. When analyzed as a continuous variable, meeting a higher number of 24-HMB guidelines was associated with a decreased risk of anxiety (OR = 0.877, 95% CI = 0.772–0.997, p = 0.045). In the categorical analysis, only the combination of meeting the PA and ST guidelines was significantly associated with reduced anxiety (OR = 0.419, 95% CI = 0.186–0.944, p = 0.036). The overall model was significant (p < 0.001).
Association between the 24-HMB guidelines and externalizing problems
Table 5 illustrates the associations between meeting the 24-HMB guidelines and difficulties in making friends. When treated as a continuous variable, meeting more of the 24-HMB guidelines was associated with lower odds of difficulties in making friends (OR = 0.470, 95% CI = 0.324–0.681, p < 0.001). In categorical analysis, meeting either the PA guideline alone (OR = 0.471, 95% CI = 0.296–0.751, p = 0.002) or the ST guideline alone (OR = 0.615, 95% CI = 0.462–0.820, p < 0.001) was associated with lower odds of difficulties in making friends. Combinations of meeting specific 24-HMB guidelines, such as PA + ST (OR = 0.350, 95% CI = 0.194–0.632, p < 0.001), PA + SL (OR = 0.563, 95% CI = 0.387–0.819, p = 0.003), and ST + SL guidelines (OR = 0.709, 95% CI = 0.560–0.899, p = 0.005), also showed associations with lower difficulties in making friends. Notably, preterm youth meeting all three 24-HMB guidelines exhibited the lowest levels of difficulties in making friends (OR = 0.470, 95% CI = 0.324–0.681, p < 0.001). The overall model demonstrated statistical significance (p < 0.001).
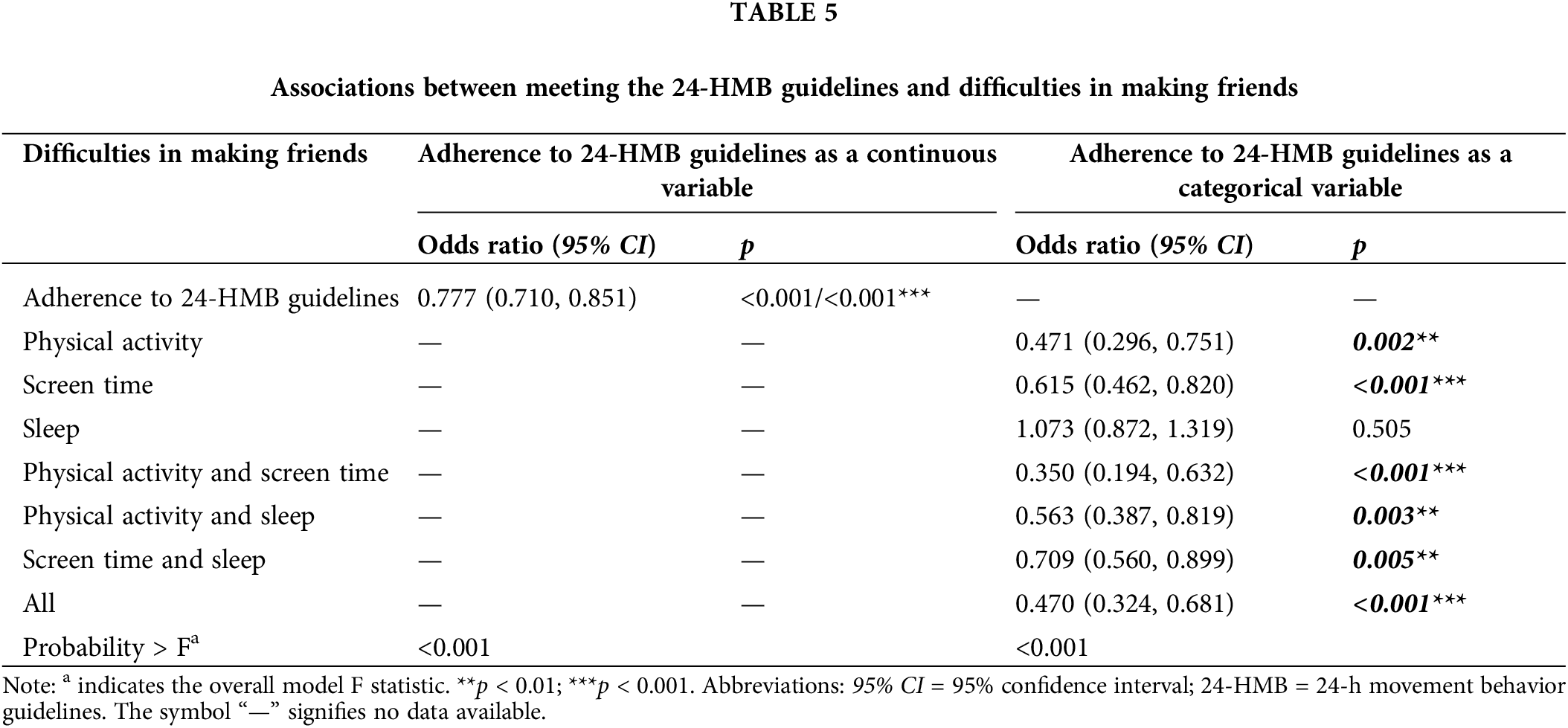
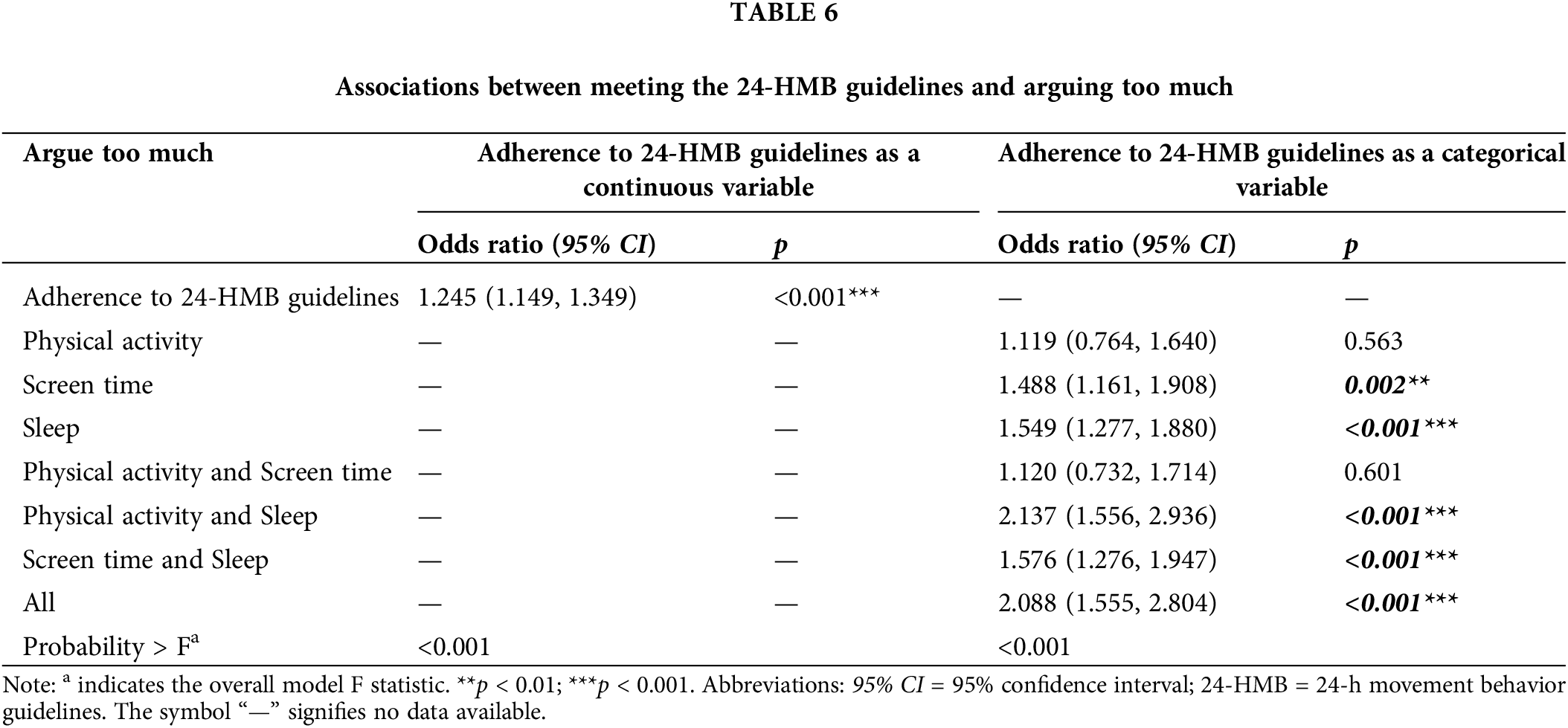
Table 6 displays the associations between meeting the 24-HMB guidelines and the frequency of arguing too much. When treated as a continuous variable, meeting a higher number of 24-HMB guidelines was not associated with the likelihood of arguing too much (OR = 1.119, 95% CI = 0.764–1.640, p = 0.563). In categorical analysis, meeting the ST guideline alone (OR = 1.488, 95% CI = 1.161–1.908, p = 0.002) and SL guideline alone (OR = 1.549, 95% CI = 1.277–1.880, p < 0.001) were associated with lower odds of arguing too much. Preterm youth who met specific combinations of the 24-HMB guidelines, such as PA + SL (OR = 2.137, 95% CI = 1.556–2.936, p < 0.001) and ST + SL (OR = 1.576, 95% CI = 1.276–1.947, p < 0.001), also showed lower odds of arguing too much. Meeting all three 24-HMB guidelines (OR = 2.088, 95% CI = 1.555–2.804, p < 0.001) was associated with the lowest odds of arguing too much.
This cross-sectional study investigated whether meeting the 24-HMB guidelines relates to cognitive difficulties, internalizing problems, and externalizing problems in a nationally representative sample of U.S. youth aged 6 to 17 years born preterm. We observed significant associations between meeting specific guidelines within the 24-HMB framework and our three main outcomes (see Fig. 1 for details). Given that our study results are consistent with the evidence in the existing literature, which generally suggests that meeting the 24-HMB guidelines conveys health benefits, our findings underscore the importance of advocating for the promotion of healthy lifestyle behaviors. (i.e., appropriate PA and SL, limited ST) among preterm youth, their caregivers, and relevant stakeholders (e.g., teachers).
The urgent need to promote healthy lifestyle behaviors among youth born preterm is supported by our finding that approximately 42.49% of preterm youth met at least one of the 24-HMB guidelines, while around 29.7% met two guidelines, and a smaller proportion, 7.3%, met all three 24-HMB guidelines. These findings align with the observation of previous research conducted on youth with neurodevelopmental conditions like autism spectrum disorder [26], attention-deficit/hyperactivity disorder [25], and epilepsy [37].
Based on the growing evidence linking adherence to the 24-HMB guidelines to health benefits [37], our findings underscore the importance of advocating for and promoting healthy lifestyle behaviors among preterm youth across different environments.
Association between meeting the 24-HMB guidelines and cognitive difficulties
In our study, we did not find an overall statistically significant association between meeting the 24-HMB guidelines and parent-reported cognitive difficulties, which was somewhat unexpected. This observation is perhaps attributable to two factors: first, our sample consisted of preterm youth aged 6 years or older, whereas previous research indicates that by 36 months (i.e., 3 years), the cognitive development of preterm youth aligns with that of full-term peers [38]. Second, the assessment of cognitive difficulties relied exclusively on parent reports, potentially reducing our ability to identify statistically significant associations compared to more sensitive methods like standardized neuropsychological evaluations.
Our results suggest that preterm youth who met the ST guideline alone exhibited fewer parent-reported cognitive difficulties. This result is consistent with previous research indicating a negative association between ST and cognitive development [39]. From a neurobiological perspective, such an observation is perhaps related to findings from neuroimaging studies showing that prolonged ST is linked to reduced connectivity in neural networks associated with attention and cognitive control [40]. Moreover, excessive ST was often accompanied by prolonged sitting, a sedentary behavior that negatively affects physical health and can pose a serious threat to brain health, especially cognitively passive sedentary behaviors (e.g., watching TV) [41].
Although several studies provide evidence for a positive association between PA and cognitive function [42–47], the present study focused on cognitive difficulties, which are less prevalent among adolescents [48] and were assessed with a parent-reported instrument. Thus, our study is not fully comparable to the previous literature in which cognitive performance was mainly operationalized via computerized cognitive tests. However, replacing ST with PA remains a practical and cost-effective means for fostering the health of preterm youth through lifestyle changes. Numerous studies have demonstrated that regular engagement in structured, repetitive, and planned forms of PA, particularly moderate-intensity exercise, along with decreased ST, can have beneficial effects on brain development [43,49]. Specifically, these behaviors are linked to enhanced structural and functional integrity of key brain regions including the prefrontal cortex, hippocampus, and cerebellum, which are crucial for advanced cognitive functions such as executive function [50,51]. Our findings indicate that meeting the ST component of 24-HMB guidelines is linked to fewer cognitive difficulties among preterm youth. This suggests that maintaining a healthy lifestyle could potentially mitigate cognitive challenges in this population, although further interventional studies are needed to empirically support this hypothesis.
Association between meeting the 24-HMB guidelines and internalizing problems
In our current study, meeting individual or combined components of 24-HMB guidelines showed specific associations with indicators of internalizing problems. Specifically, meeting the SL guideline alone, as well as the combination of SL and ST guidelines, were associated with a lower likelihood of reporting depression. A recent seminal meta-analysis [52] indicated that disturbed sleep (including sleep disturbances or insomnia) is linked to a higher prevalence of depression among a larger sample of youth (N = 28,895). Thus, intervention strategies to prevent depression should be implemented as early as possible in childhood by promoting healthy lifestyle behaviors such as adequate sleep. In this context, sleep could perhaps be improved by intervention approaches such as PA promotion or mindfulness training, although the evidence in this direction is currently somewhat sparse and inconclusive [53]. Moreover, preterm youth who met both the SL and ST guidelines had lower odds of experiencing depressive symptoms compared to those who did not meet any of the 24-HMB guidelines. A recent study showed that engaging in bedtime screen activities such as streaming movies, talking or texting on the phone, and using social media, was associated with disrupted sleep patterns (as reflected by trouble falling/staying asleep) in healthy adolescents aged between 10 and 14 (N = 10,280) [54], which in turn may result in greater levels of depression severity [55]. Furthermore, meeting both PA and ST guidelines is associated with a lower likelihood of experiencing anxiety. Such a finding is partially supported by observations of a 4-year longitudinal study indicating that a 60-min increase in average time spent for the use of social media (e.g., television viewing and computer use) in a given year was correlated with a 0.21 unit increase in the severity of anxiety symptoms within that same year [56]. These findings suggest that ST should be limited, especially before bedtime, to improve sleep hygiene and foster overall health.
In this context, a considerable number of studies provided evidence for the importance of physical exercise in alleviating negative emotions including depression and anxiety [57–59]. A recent review emphasized that physical exercise can positively influence several neurobiological processes, such as brain plasticity, neurogenesis, and neuroprotection, facilitated by neurotrophic factors such as brain-derived neurotrophic factor (BDNF) [60]. Moreover, physical exercise decreases neural responses to stress in brain regions that regulate sympathetic activity, thereby supporting the interaction between the heart and brain known as ‘heart-brain crosstalk’ [60]. These exercise-induced changes in specific neurobiological processes may converge on a behavioral level in lower levels of anxiety and depression. Collectively, physical exercise can reduce both central and peripheral sympathetic activity, selectively influencing neurochemicals like norepinephrine. This modulation potentially mitigates the mental health effects associated with oxidative stress and immune suppression [61]. Additionally, meeting a higher number of guidelines provided in the 24-HMB recommendations is associated with a lower likelihood of experiencing internalizing problems, such as depression and anxiety [62].
Associations between meeting the 24-HMB guidelines and externalizing problems
The results of our study indicate that meeting individual and combined components of the 24-HMB guidelines is associated with a reduced likelihood of externalizing problems. Specifically, meeting the PA and ST guidelines independently, as well as combinations such as PA + ST, PA + SL, and PA + ST + SL, are linked to reduced difficulties in making friends among our sample of preterm youth. The aforementioned findings partially align with results from previous studies involving youth with neurodevelopmental disorders, such as ASD [26] and ADHD [25]. Consistent with existing literature, our findings reinforce the idea that PA and physical fitness play crucial roles in the social development of youth [63,64]. Moreover, increasing evidence suggests that reducing leisure ST can enhance youth’s social skills by allowing more time for interpersonal connections, potentially facilitating the development of friendships [65,66]. Our study demonstrated that meeting any combination of the three 24-HMB guidelines is linked to improved friendship scores. Therefore, promoting adherence to the 24-HMB guidelines among preterm youth, their caregivers, and stakeholders appears beneficial when aiming to mitigate externalizing problems in preterm youth.
Our findings indicate that meeting individual (such as SL or ST) or combined 24-HMB guidelines (such as PA + SL, SL + ST, and PA + SL + ST) is associated with a reduced frequency of arguments. This suggests that maintaining adequate sleep duration and limiting ST are important factors that may influence argument frequency. A growing amount of evidence suggests that sufficient sleep quality and duration can enhance emotion regulation [67], potentially leading to fewer school-related issues and arguments. Moreover, the findings of a meta-analysis indicated that increased ST was associated with higher levels of externalizing behavior problems like aggression and inattention [68]. This association may be attributable to potential exposure to inappropriate content, including aggression and violent behavior [68]. However, our findings did not establish a link between meeting the PA guideline and issues related to arguments. This observation is perhaps related to the competitive nature of certain types of PAs that youth commonly participate in (e.g., football, basketball, rugby, boxing), which may increase the likelihood of argumentative behavior [69]. Based on this observation and considering that associations with either SL or ST became statistically significant in our cohort of preterm youth, prioritizing interventions that address ST and SL appears a promising option for future trials aimed at reducing externalizing problems. Furthermore, our findings indicate that meeting a higher number of 24-HMB guidelines is associated with a lower likelihood of experiencing externalizing problems. This underscores the notion that various lifestyle behaviors may work synergistically to enhance specific health outcomes.
While our study has offered valuable insights into the associations between meeting individual and combined components of the 24-HMB guidelines and cognitive difficulties, as well as internalizing and externalizing problems in preterm youth, several limitations must be acknowledged. First, the cross-sectional design limits our ability to establish causality. Second, the reliance on caregiver proxy reports in the NSCH survey to assess behaviors introduces potential biases arising from subjective reporting, such as parents’ tendencies to overestimate or underestimate their child’s level of PA.
Given these limitations, it is imperative to utilize more objective and comprehensive assessment tools, such as accelerometer-based measurements of PA, to validate the findings of our study and further enhance our understanding of how meeting the 24-HMB guidelines impacts health outcomes in youth born preterm. Such evidence is crucial for developing effective interventions and policies aimed at promoting the overall health of this population. Additionally, future studies should consider a detailed analysis of different types of ST, distinguishing between cognitively passive activities (e.g., watching TV) and cognitively active activities (e.g., playing video games), as these may have distinct associations with mental health outcomes [41]. Given these considerations, it is prudent to interpret our results cautiously.
Based on the cross-sectional study design, which limits the applicability of our conclusions, future research should gather and analyze longitudinal data (e.g., from public data repositories such as the Biobank and Millennium Cohort Study), to study the directionality of changes in PA, ST, and SL, and its association with health-related outcomes (e.g., cognitive difficulties, internalizing and externalizing problems) among preterm youth. Moreover, future studies should investigate the unique impacts of interventions promoting the adherence to the 24-HMB in preterm youth, particularly in comparison to those born at term, to better understand the specific needs and health effects of lifestyle behaviors in this vulnerable population.
The findings of our study suggest that a significant number of preterm youths did not meet the 24-h Movement Behavior (24-HMB) guidelines. However, we observed that meeting these 24-HMB guidelines, comprising recommendations on physical activity, sleep, and screen time, was associated with better mental health outcomes, particularly for internalizing and externalizing problems in youth born preterm. To improve mental well-being among preterm youth, interventions should prioritize promoting healthy lifestyle behaviors, including higher levels of physical activity and reduced screen time, among youth born preterm and relevant stakeholders (e.g., teachers). Given that the prevalence of meeting the physical activity guideline was notably lower than other components of the 24-HMB guidelines, future physical activity interventions should be tailored to the specific needs of preterm youth. This includes developing target-group-specific physical activity manuals and providing psychological support, considering barriers and promoters of physical activity in this vulnerable population.
Acknowledgement: The authors wish to acknowledge the support received from various funding bodies, including the Shenzhen Educational Research Funding, the Shenzhen Science and Technology Innovation Commission, and the Social Science Foundation from China’s Ministry of Education.
Funding Statement: This study was supported by the Shenzhen Educational Research Funding (Grant No. zdzb2014), the Shenzhen Science and Technology Innovation Commission (Grant No. 202307313000096), the Social Science Foundation from China’s Ministry of Education (Grant No. 23YJA880093), a Post-Doctoral Fellowship (Grant No. 2022M711174), the National Center for Mental Health (Grant No. Z014), and a Research Excellence Scholarship of Shenzhen University (Grant No. ZYZD2305).
Author Contributions: Zhihui Cheng conceptualized the study, analyzed the data, and wrote the first draft of the manuscript. All other authors revised and edited the manuscript drafts. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The datasets generated and/or analyzed during the current study are available in the U.S. Census Bureau repository at https://www.childhealthdata.org/browse (accessed on 20 July).
Ethics Approval: The study was approved by the Ethics Committee of the Shenzhen University (IRB number: PN-2022-00075). No participants received financial incentives, and all participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Vogel JP, Chawanpaiboon S, Moller A-B, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstetr Gynaecol. 2018;52:3–12; [Google Scholar]
2. Waitzman NJ, Jalali A, Grosse SD. Preterm birth lifetime costs in the United States in 2016: an update. Semin Perinatol. 2021;45(3):151390. [Google Scholar] [PubMed]
3. Butler AS, Behrman RE. Preterm birth: causes, consequences, and prevention. Amsterdam, Netherlands: National Academies Press; 2007. [Google Scholar]
4. Anderson J, Do LAH, Wurzel D, Licciardi PV. Understanding the increased susceptibility to asthma development in preterm infants. Allergy. 2023;78(4):928–39. [Google Scholar] [PubMed]
5. Crump C, Groves A, Sundquist J, Sundquist K. Association of preterm birth with long-term risk of heart failure into adulthood. JAMA Pediatr. 2021;175(7):689–97. [Google Scholar] [PubMed]
6. Crump C, Sundquist J, Sundquist K. Preterm or early term birth and long-term risk of asthma into midadulthood: a national cohort and cosibling study. Thorax. 2023;78(7):653–60. [Google Scholar] [PubMed]
7. Barrett PM, McCarthy FP, Evans M, Kublickas M, Perry IJ, Stenvinkel P, et al. Risk of long-term renal disease in women with a history of preterm delivery: a population-based cohort study. BMC Med. 2020;18(1):66. [Google Scholar] [PubMed]
8. Dean B, Ginnell L, Boardman JP, Fletcher-Watson S. Social cognition following preterm birth: a systematic review. Neurosci Biobehav Rev. 2021;124:151–67. [Google Scholar] [PubMed]
9. Breeman LD, Jaekel J, Baumann N, Bartmann P, Wolke D. Preterm cognitive function into adulthood. Pediatrics. 2015;136(3):415–23. [Google Scholar] [PubMed]
10. Upadhyaya S, Sourander A, Luntamo T, Matinolli HM, Chudal R, Hinkka-Yli-Salomäki S, et al. Preterm birth is associated with depression from childhood to early adulthood. J Am Acad Child Adolesc Psychiat. 2021;60(9):1127–36. [Google Scholar]
11. Singh GK, Kenney MK, Ghandour R, Kogan MD, Lu MC. Mental health outcomes in US children and adolescents born prematurely or with low birthweight. Depress Res Treat. 2013;2013. [Google Scholar]
12. Fitzallen GC, Sagar YK, Taylor HG, Bora S. Anxiety and depressive disorders in children born preterm: a meta-analysis. J Dev Behav Pediatr. 2021;42(2):154–62. [Google Scholar] [PubMed]
13. Arpi E, Ferrari F. Preterm birth and behaviour problems in infants and preschool-age children: a review of the recent literature. Dev Med Child Neurol. 2013;55(9):788–96. [Google Scholar] [PubMed]
14. Spittle AJ, Treyvaud K, Doyle LW, Roberts G, Lee KJ, Inder TE, et al. Early emergence of behavior and social-emotional problems in very preterm infants. J Am Acad Child Adolesc Psychiat. 2009;48(9):909–18. [Google Scholar]
15. Reyes LM, Jaekel J, Heuser KM, Wolke D. Developmental cascades of social inhibition and friendships in preterm and full-term children. Infant Child Dev. 2019;28:16. doi:10.1002/icd.2165. [Google Scholar] [CrossRef]
16. Reyes LM, Jaekel J, Bartmann P, Wolke D. Peer relationship trajectories in very preterm and term individuals from childhood to early adulthood. J Dev Behav Pediatr. 2021;42(8):621–30. [Google Scholar] [PubMed]
17. Ritchie K, Bora S, Woodward LJ. Peer relationship outcomes of school-age children born very preterm. J Pediatr. 2018;201:238–44. doi:10.1016/j.jpeds.2018.05.034. [Google Scholar] [PubMed] [CrossRef]
18. Schulzke SM, Kaempfen S, Trachsel D, Patole SK. Physical activity programs for promoting bone mineralization and growth in preterm infants. Cochrane Database Syst Rev. 1996;2014(4):550. doi:10.1002/14651858.CD005387.pub2. [Google Scholar] [PubMed] [CrossRef]
19. Valizadeh L, Sanaeefar M, Hosseini MB, Jafarabadi MA, Shamili A. Effect of early physical activity programs on motor performance and neuromuscular development in infants born preterm: a randomized clinical trial. J Caring Sci. 2017;6(1):67. doi:10.15171/jcs.2017.008. [Google Scholar] [PubMed] [CrossRef]
20. Hibbs AM, Storfer-Isser A, Rosen C, Ievers-Landis CE, Taveras EM, Redline S. Advanced sleep phase in adolescents born preterm. Behav Sleep Med. 2014;12(5):412–24. doi:10.1080/15402002.2013.825838. [Google Scholar] [PubMed] [CrossRef]
21. Vohr BR, McGowan EC, Bann C, Das A, Higgins R, Hintz S, et al. Association of high screen-time use with school-age cognitive, executive function, and behavior outcomes in extremely preterm children. JAMA Pediatr. 2021;175(10):1025–34. doi:10.1001/jamapediatrics.2021.2041. [Google Scholar] [PubMed] [CrossRef]
22. Gunnell KE, Flament MF, Buchholz A, Henderson KA, Obeid N, Schubert N, et al. Examining the bidirectional relationship between physical activity, screen time, and symptoms of anxiety and depression over time during adolescence. Prev Med. 2016;88:147–52. [Google Scholar] [PubMed]
23. Oberle E, Ji XR, Kerai S, Guhn M, Schonert-Reichl KA, Gadermann AM. Screen time and extracurricular activities as risk and protective factors for mental health in adolescence: a population-level study. Prev Med. 2020;141:106291. [Google Scholar] [PubMed]
24. Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L, et al. Canadian 24-hour movement guidelines for the early years (0–4 yearsan integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17(Suppl 5):874. [Google Scholar] [PubMed]
25. Taylor A, Kong C, Zhang Z, Herold F, Ludyga S, Healy S, et al. Associations of meeting 24-h movement behavior guidelines with cognitive difficulty and social relationships in children and adolescents with attention deficit/hyperactive disorder. Child Adolesc Psychiat Ment Health. 2023;17(1):42. [Google Scholar]
26. Kong C, Chen A, Ludyga S, Herold F, Healy S, Zhao M, et al. Associations between meeting 24-hour movement guidelines and quality of life among children and adolescents with autism spectrum disorder. J Sport Health Sci. 2023;12(1):73–86. [Google Scholar] [PubMed]
27. Asztalos EV, Church PT, Riley P, Fajardo C, Shah PS, Network CN, et al. Association between primary caregiver education and cognitive and language development of preterm neonates. Am J Perinatol. 2017;34(4):364–71. [Google Scholar] [PubMed]
28. Karvonen KL, Baer RJ, Rogers EE, Steurer MA, Jelliffe-Pawlowski LL, Pantell MS. Brief report: acute care visits vary by race and ethnicity among publicly insured preterm infants. Pediatr Res. 2021;90(4):712–6. [Google Scholar] [PubMed]
29. Boone KM, Nelin MA, Chisolm DJ, Keim SA. Gaps and factors related to receipt of care within a medical home for toddlers born preterm. J Pediatr. 2019;207:161–8.e1. [Google Scholar] [PubMed]
30. Belfort MB, Gillman MW, Buka SL, Casey PH, McCormick MC. Preterm infant linear growth and adiposity gain: trade-offs for later weight status and intelligence quotient. J Pediatr. 2013;163(6):1564–9.e2. [Google Scholar] [PubMed]
31. Sulaiman S, Premji SS, Tavangar F, Yim IS, Lebold M. Total adverse childhood experiences and preterm birth: a systematic review. Maternal Child Health J. 2021;25:1581–94. [Google Scholar]
32. Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: a cohort study of an urban, minority sample in the U.S. Child Abuse Negl. 2013;37(11):917–25. [Google Scholar] [PubMed]
33. Yang B, Chen BB, Qu Y, Zhu Y. Impacts of parental burnout on chinese youth’s mental health: the role of parents’ autonomy support and emotion regulation. J Youth Adolesc. 2021;50(8):1679–92. [Google Scholar] [PubMed]
34. Boudreault-Bouchard AM, Dion J, Hains J, Vandermeerschen J, Laberge L, Perron M. Impact of parental emotional support and coercive control on adolescents’ self-esteem and psychological distress: results of a four-year longitudinal study. J Adolesc. 2013;36(4):695–704. [Google Scholar] [PubMed]
35. Boyle MH, Racine Y, Georgiades K, Snelling D, Hong S, Omariba W, et al. The influence of economic development level, household wealth and maternal education on child health in the developing world. Soc Sci Med. 2006;63(8):2242–54. [Google Scholar] [PubMed]
36. Burnett A, Davey CG, Wood SJ, Wilson-Ching M, Molloy C, Cheong JL, et al. Extremely preterm birth and adolescent mental health in a geographical cohort born in the 1990s. Psychol Med. 2014;44(7):1533–44. [Google Scholar] [PubMed]
37. Rollo S, Antsygina O, Tremblay MS. The whole day matters: understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9(6):493–510. doi:10.1016/j.jshs.2020.07.004. [Google Scholar] [PubMed] [CrossRef]
38. Ionio C, Riboni E, Confalonieri E, Dallatomasina C, Mascheroni E, Bonanomi A, et al. Paths of cognitive and language development in healthy preterm infants. Infant Behav Dev. 2016;44:199–207. doi:10.1016/j.infbeh.2016.07.004. [Google Scholar] [PubMed] [CrossRef]
39. Zhang Z, Adamo KB, Ogden N, Goldfield GS, Okely AD, Kuzik N, et al. Associations between screen time and cognitive development in preschoolers. Paediatr Child Health. 2021;27(2):105–10. doi:10.1093/pch/pxab067. [Google Scholar] [PubMed] [CrossRef]
40. Meri R, Hutton J, Farah R, DiFrancesco M, Gozman L, Horowitz-Kraus T. Higher access to screens is related to decreased functional connectivity between neural networks associated with basic attention skills and cognitive control in children. Child Neuropsychol. 2023;29(4):666–85. doi:10.1080/09297049.2022.2110577. [Google Scholar] [PubMed] [CrossRef]
41. Zou L, Herold F, Cheval B, Wheeler MJ, Pindus DM, Erickson KI, et al. Sedentary behavior and lifespan brain health. Trends Cogn Sci. 2024;28(4):369–82. doi:10.1016/j.tics.2024.02.003. [Google Scholar] [PubMed] [CrossRef]
42. Lu Y, Zhao M. Adherence to 24-h movement guidelines and cognitive difficulties in adolescents. Complement Ther Clin Pract. 2023;51:101744. [Google Scholar] [PubMed]
43. Erickson KI, Hillman C, Stillman CM, Ballard RM, Bloodgood B, Conroy DE, et al. Physical activity, cognition, and brain outcomes: a review of the 2018 physical activity guidelines. Med Sci Sports Exerc. 2019;51(6):1242–51. [Google Scholar] [PubMed]
44. Haverkamp BF, Wiersma R, Vertessen K, van Ewijk H, Oosterlaan J, Hartman E. Effects of physical activity interventions on cognitive outcomes and academic performance in adolescents and young adults: a meta-analysis. J Sports Sci. 2020;38(23):2637–60. [Google Scholar] [PubMed]
45. Hillman CH, McDonald KM, Logan NE. A review of the effects of physical activity on cognition and brain health across children and adolescence. Nestle Nutr Inst Workshop Ser. 2020;95:116–26. [Google Scholar] [PubMed]
46. Vasilopoulos F, Jeffrey H, Wu Y, Dumontheil I. Multi-level meta-analysis of physical activity interventions during childhood: effects of physical activity on cognition and academic achievement. Educ Psychol Rev. 2023;35(2):59. [Google Scholar]
47. Hou M, Herold F, Zhang Z, Ando S, Cheval B, Ludyga S, et al. Human dopaminergic system in the exercise-cognition link. Trends Mol Med. 2024;70. doi:10.1016/j.molmed.2024.04.011. [Google Scholar] [PubMed] [CrossRef]
48. Schulte-Körne G. Mental health problems in a school setting in children and adolescents. Dtsch Arztebl Int. 2016;113(11):183–90. [Google Scholar]
49. Black MM, Singhal A, Hillman CH. Building future health and well-being of thriving toddlers and young children. In: 95th Nestlé Nutrition Institute Workshop, Sep. 2020; Geneva, Switzerland, Karger Medical and Scientific Publishers. [Google Scholar]
50. Best JR. Effects of physical activity on children’s executive function: contributions of experimental research on aerobic exercise. Devel Rev. 2010;30(4):331–51. [Google Scholar]
51. Chaddock-Heyman L, Erickson KI, Voss MW, Knecht AM, Pontifex MB, Castelli DM, et al. The effects of physical activity on functional MRI activation associated with cognitive control in children: a randomized controlled intervention. Front Hum Neurosci. 2013;7:72. [Google Scholar] [PubMed]
52. Marino C, Andrade B, Campisi SC, Wong M, Zhao H, Jing X, et al. Association between disturbed sleep and depression in children and youths: a systematic review and meta-analysis of cohort studies. JAMA Netw Open. 2021;4(3):e212373. [Google Scholar] [PubMed]
53. Kline CE, Hillman CH, Bloodgood Sheppard B, Tennant B, Conroy DE, Macko RF, et al. Physical activity and sleep: an updated umbrella review of the 2018 physical activity guidelines advisory committee report. Sleep Med Rev. 2021;58:101489. [Google Scholar] [PubMed]
54. Nagata JM, Singh G, Yang JH, Smith N, Kiss O, Ganson KT, et al. Bedtime screen use behaviors and sleep outcomes: findings from the adolescent brain cognitive development (ABCD) study. Sleep Health. 2023;9(4):497–502. [Google Scholar] [PubMed]
55. Roberts RE, Duong HT. The prospective association between sleep deprivation and depression among adolescents. Sleep. 2014;37(2):239–44. [Google Scholar] [PubMed]
56. Boers E, Afzali MH, Conrod P. Temporal associations of screen time and anxiety symptoms among adolescents. Can J Psychiat. 2019;65(3):206–8. [Google Scholar]
57. Mead GE, Morley W, Campbell P, Greig CA, Mcmurdo MET, Lawlor DA. Exercise for depression. Cochrane Database Syst Rev. 2009;3:CD004366. [Google Scholar]
58. Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9(3):366–78. [Google Scholar] [PubMed]
59. Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res. 2016;77:42–51. [Google Scholar] [PubMed]
60. Herring MP, Meyer JD. Resistance exercise for anxiety and depression: efficacy and plausible mechanisms. Trends Mol Med. 2024;30(3):204–6. [Google Scholar] [PubMed]
61. Dishman RK, Berthoud HR, Booth FW, Cotman CW, Edgerton VR, Fleshner MR, et al. Neurobiology of exercise. Obesity. 2006;14(3):345–56. [Google Scholar] [PubMed]
62. Gao Y, Yu Q, Schuch FB, Herold F, Hossain MM, Ludyga S, et al. Meeting 24-h movement behavior guidelines is linked to academic engagement, psychological functioning, and cognitive difficulties in youth with internalizing problems. J Affect Disord. 2024;349:176–86. [Google Scholar] [PubMed]
63. Hou M, Herold F, Healy S, Haegele JA, Block ME, Ludyga S, et al. 24-Hour movement behaviors among visually impaired US children and adolescents. Ment Health Phys Act. 2023;25:100545. [Google Scholar]
64. Colombo-Dougovito AM, Lee J. Social skill outcomes following physical activity-based interventions for individuals on the autism spectrum: a scoping review spanning young childhood through young adulthood. Adapt Phys Activ Q. 2021;38(1):138–69. [Google Scholar] [PubMed]
65. Ma S, Li J, Chen EE. Does screen media hurt young children’s social development? Longitudinal associations between parental engagement, children’s screen time, and their social competence. Early Educ Dev. 2024;35(1):10–25. [Google Scholar]
66. Muppalla SK, Vuppalapati S, Reddy Pulliahgaru A, Sreenivasulu H. Effects of excessive screen time on child development: an updated review and strategies for management. Cureus. 2023;15(6):e40608. [Google Scholar] [PubMed]
67. Palmer CA, Alfano CA. Sleep and emotion regulation: an organizing, integrative review. Sleep Med Rev. 2017;31:6–16. [Google Scholar] [PubMed]
68. Eirich R, McArthur BA, Anhorn C, McGuinness C, Christakis DA, Madigan S. Association of screen time with internalizing and externalizing behavior problems in children 12 years or younger: a systematic review and meta-analysis. JAMA Psychiat. 2022;79(5):393–405. [Google Scholar]
69. Donahue EG, Rip B, Vallerand RJ. When winning is everything: on passion, identity, and aggression in sport. Psychol Sport Exercise. 2009;10(5):526–34. [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools