 Open Access
Open Access
ARTICLE
Tendency to Avoid Physical Activity and Sport: Associations with Weight Stigma, and Psychological Distress in a Two-Wave Longitudinal Study
1 Health Research Center, Life Style Institute, Baqiyatallah University of Medical Sciences, Tehran, 1435916471, Iran
2 Health Education Department, Faculty of Health, Baqiyatallah University of Medical Sciences, Tehran, 1435916471, Iran
3 Department of Early Childhood and Family Education, National Taipei University of Education, Taipei, 106, Taiwan
4 School of Physical Therapy, Graduate Institute of Rehabilitation Science, College of Medicine, Chang Gung University, Taoyuan, 333, Taiwan
5 Institute of Allied Health Sciences, College of Medicine, National Cheng Kung University, Tainan, 701, Taiwan
6 Division of Family Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, and School of Medicine, Tzu Chi University, Hualien, Taiwan
7 Data Science Degree Program, National Taiwan University and Academia Sinica, Taipei, Taiwan
8 Department of Family Medicine and Community Medicine, E-Da Hospital, I-Shou University, Kaohsiung, 824, Taiwan
9 College of Medicine, I-Shou University, Kaohsiung, 840, Taiwan
10 Department of Medical Research, E-Da Hospital, I-Shou University, Kaohsiung, 840, Taiwan
11 Sunway Business School, Sunway University, Selangor, 47500, Malaysia
12 International Gaming Research Unit, Psychology Department, Nottingham Trent University, Nottingham, NG1 4BU, UK
13 Department of Public Health, College of Medicine, National Cheng Kung University, Tainan, 701, Taiwan
14 Biostatistics Consulting Center, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan
15 Department of Occupational Therapy, College of Medicine, National Cheng Kung University, Tainan, 701, Taiwan
* Corresponding Authors: Chi Hsien Huang. Email: ,
; Chung-Ying Lin. Email:
# Saffari Mohsen and Yi-Ching Lin shared equal contribution to the paper
International Journal of Mental Health Promotion 2024, 26(8), 633-641. https://doi.org/10.32604/ijmhp.2024.053432
Received 30 April 2024; Accepted 09 July 2024; Issue published 30 August 2024
Abstract
Background: Physical inactivity is a major public health problem worldwide that results in physical and mental health problems. One major issue for physical inactivity is weight stigma (WS), especially perceived WS, which could lead to a tendency to avoid physical activity (PA). To better understand the association between perceived WS and PA, knowledge of the likely mediators in this association such as weight bias internalization (WBI) and psychological distress were investigated in the present study. Methods: Using a two-wave longitudinal study and convenient sampling, 388 Taiwanese participants (55% females; mean age = 29.7 years [SD ± 6.3]) completed two surveys six months apart. Body mass index (BMI), Perceived Weight Stigma Scale (PWSS), Weight Bias Internalization Scale (WBIS), Depression, Anxiety, Stress Scale (DASS-21), and Tendency to Avoid Physical Activity and Sport Scale (TAPAS) were assessed. Results: A mediation model controlling for age, gender, and BMI with 5000 bootstrapping resamples was performed. Perceived WS exerted significant direct effects on WBI (β = 0.25; p < 0.001), psychological distress (β = 0.15; p = 0.003), and tendency to avoid PA (β = 0.10; p = 0.027); WBI exerted a significant direct effect on tendency to avoid PA (β = 0.47; p < 0.001). Standardized indirect effects of WBI and psychological distress on the association between perceived WS and tendency to avoid PA were 0.12 and 0.01, respectively. Conclusion: Given the direct association of perceived WS on the tendency to avoid PA and the mediating role of WBI in this association, interventions addressing perceived WS and WBI may contribute to promoting PA. Therefore, health interventionists (both when planning and executing PA programs) need to consider weight stigmawhen encouraging physical activity.Keywords
Physical inactivity is an important health-threatening issue among young people. This may result in individuals developing obesity (the most common metabolic disorder) [1]. Moreover, over 13% of adults are diagnosed as obese [2], with a growing prevalence globally, including in East Asian countries [3]. For example, a recent population health survey reported nearly 33% of 15–84-year-old individuals in Hong Kong were obese [4]. The prevalence of obesity in Taiwan increased from 11.5% in 1996 to 23% in 2016 [5]. Although obesity (body mass index [BMI] at 30 kg/m2 or above for Westerners; 25 kg/m2 or above for Asians) and being overweight (BMI between 25 and 29.99 kg/m2 for Westerners; 23 and 24.99 kg/m2 for Asians) [6] are defined differently, their impacts on health are similar and hereafter, the present study uses the two terms interchangeably. Moreover, it should also be noted that the use of terms like ‘overweight’ and ‘obese’ (as defined by BMI measures) may also contribute to weight stigma (WS). Therefore, neutral word such as ‘higher weight’ may be preferable daily. However, the present study uses the terms ‘overweight’ and ‘obese’ because they are commonly used in the literature.
Individuals who have concerns about weight (especially those who are overweight) are at a higher risk for psychological distress than the general population [7]. Those who are overweight report elevated levels of psychological distress, body dissatisfaction [8], impaired self-esteem, and exposure to bullying [9,10]. Moreover, several longitudinal studies have emphasized that weight stigma rather than weight itself may cause psychological distress [11–13].
WS is defined as a kind of social devaluation among those who have weight concerns, even for those who are not overweight [14]. WS can be classified into different forms. In the present study, two specific types of WS were examined: perceived WS (how individuals perceive other people’s negative thoughts, feelings, and behaviors toward him/her) and weight bias internalization (WBI; how individuals accept the perceived weight stigma toward themselves) [15]. In most cultures and communities, body shapes beyond regular norms are exposed to judgment and frequent teasing in different situations, including education, job, and healthcare settings [16].
In general, WS may be considered as a risk factor for chronic stress, increased psychological distress, and lower engagement in healthy lifestyle, such as physical activity (PA) engagement and having a healthy diet [13,17]. Thoughts of victimization may also lead to suicidal behaviors/thoughts among this population due to being overweight [15]. Moreover, increasing evidence indicates that psychological distress may contribute to the development and continuity of being overweight [18]. For example, individuals having WS may use unhealthy coping strategies such as overeating and tend to engage in sedentary behaviors, which exacerbate weight gain [19].
The severity of perceived WS can include behaviors such as job discrimination [14]. Moreover, individuals who are overweight can experience isolation, rejection, feeling unattractive, feeling less competent, and feeling less intelligent due to stigmatization by strangers, friends, and even members of their own family [11,13]. There is also a significant association between increased risk of stress and stigmatization [19]. Moreover, psychological stress may concurrently be considered as one of the causes and outcomes of WS [8,20].
Frequently experiencing WS may be coupled with the perception of individual negative stereotypes and beliefs of being socially devalued, which may lead to internalizing weight bias [21]. Individuals may engage in a self-devaluation process and experience chronic stress due to being stigmatized for their weight irrespective of excess or not. This may lead to the development of WBI. Unfortunately, there is less information regarding WBI than WS is caused by social discrimination [22]. Nevertheless, studies have shown that WBI exists among individuals with all types of weight status and is associated with psychological distress and eating disorders [23].
However, some scholars have argued that WBI does not exist among individuals without weight problems but as other forms of disturbance (e.g., body image concerns) [24]. Nevertheless, the contribution of WBI (or body image disturbance; hereafter, WBI is used to indicate body image disturbance/concerns) to lowering engagement in health-promoting activities by negatively affecting self-efficacy has also been demonstrated [25]. Indeed, feelings such as not wanting to exercise and laziness are negative weight-related stereotypes may decrease self-efficacy and cause unwillingness to engage in a healthy lifestyle [23,26]. Therefore, a likely factor for this population’s the high prevalence of physical inactivity may be related to WBI.
Adolescents who sought treatment for obesity with less WS have shown a stronger desire to engage in PA than those with frequent WS exposure [27]. Similarly, youth who report more frequent WBI have lower levels of PA [28]. However, other studies have not reported significant associations between WS and PA [29,30]. They proposed other pathways that may mediate the associations between WS and PA. For example, PA and engagement in sports to get fit may provide a protective effect against social discrimination and WS, suggesting an interaction in this association [31]. Similarly, the positive effects of PA to decrease depressive symptoms and stress manifestations have been reported [32]. Therefore, further research is needed to assess the extent to which WS may influence PA and other factors that may affect this relationship is needed.
The present study investigated how perceived WS affects the tendency to engage in PA and whether WBI and psychological health mediate this relationship. Accordingly, the following two hypotheses (Hs) were proposed: (i) there would be a significant association between perceived WS and a tendency to avoid PA (H1), and (ii) WBI and psychological distress may play mediating roles between direct associations of perceived WS with a tendency to avoid PA (H2). Since most studies suggest a direction from stigmatization towards the tendency not to engage in PA, the likely causal direction between them was also investigated. Moreover, examining the associations over time provides a better picture of the relationships between these variables (perceived WS, WBI, psychological distress, and tendency to avoid PA) than cross-sectional designs. Therefore, the present study comprised longitudinal data collection over two waves (six months apart) to examine changes in the study’s variables over time.
The data, procedures, ethical code, and statistical software used are appropriately cited in the text. The corresponding author can requestthe data used for analyses in the present study. The present study was not preregistered in its design, hypotheses, or analyses. Using a Monte Carlo simulation calculator (https://schoemanna.shinyapps.io/mc_power_med/, accessed on 25 April, 2024) with moderate effect sizes of the studied variables (i.e., r = 0.3 for every two studied variables) [33,34], the required sample size to have significant parallel mediation effects with power at 0.9 is between 250 and 300.
Participants and recruitment procedure
The present study convenience sampling to recruit participants for a two-wave longitudinal design. For the first data collection (T1), 592 participants completed an online survey between August and September 2022. More specifically, the present authors posted a link to the online survey on social media platforms (e.g., Facebook and LINE) that are commonly used in Taiwan. If an individual (irrespective of weight status) was interested in participation, they could log onto the online survey via the link to complete the questions hosted on the SurveyMonkey platform.
Participants’ informed consent was obtained using the following method. The first page of the online survey clearly described the study’s purpose and the participants’ rights (e.g., the participant could withdraw anytime without any consequences). The participants could begin answering the survey after they had clicked the ‘agree’ icon on the first page. The online survey ended immediately if the participant clicked the ‘disagree’ icon. At the end of the online survey, the participants were requested to leave their contact email or cellphone number if they were interested in participating in the second wave of the study (i.e., Time 2). All the participants who provided their contact information were invited six months later to participate in the second wave of data collection. The first page of the T2 survey restated the study’s purpose and the participants’ rights. Again, only when the participant clicked the ‘agree’ icon could the participant complete the survey at T2. Moreover, only data from participants who completed both surveys were used for the formal analyses in the present study.
When a follow-up rate is between 60% and 80% (i.e., attrition rate <40%), the nonsignificant or trivial differences of demographics lost-to-follow-up suggests no severe biases [35,36], procedures for T1 and T2 surveys adhered to the (i) Declaration of Helsinki and (ii) ethical principles for medical, psychological, and sociological research involving human participants. The National Cheng Kung University Human Research Ethics Committee approved the study protocol (Approval No. NCKU HREC-E-110-486-2) before the authors distributed the online survey. Participants signed the informed consent form for the present study.
Demographics. The participants reported answers to the following demographic variables: age (in years), gender (male, female, or other), height (in cm), and weight (in kg). The height and weight information were then used to calculate the body mass index (BMI) with the unit of kg/m2 (i.e., weight in kilograms divided by the squared height in meters). Moreover, according to the WHO definition (among Asians), a BMI between 23 and 24.99 kg/m2 indicates being overweight, and a BMI of 25 kg/m2 or above indicates obesity [6].
Perceived Weight Stigma Scale (PWSS). The PWSS contains 10 items assessing how an individual perceives or experiences weight stigma (WS) [37]. All the PWSS items (e.g., “People act as if you are inferior”) with a suffix stem of “Because of your weight” were rated using a dichotomized scale (yes vs. no), and a higher PWSS score (possible score range: 0–10) indicates higher levels of perceived WS. The PWSS has been reported to have good psychometric properties [38–40], including the Chinese version [41]. In the present study, the Cronbach’s α of the PWSS was 0.86 (T1) and 0.84 (T2); McDonald’s ω was 0.86 (T1) and 0.84 (T2).
Weight Bias Internalization Scale (WBIS). The original WBIS contains 11 items assessing how an individual internalizes WS, especially for individuals who are overweight [42]. A modified WBIS was later developed for individuals with all types of weight categories [43]. All the WBIS items (e.g., “I am less attractive than most other people because of my weight”) are rated using a five-point Likert scale (1 to 5), and a higher WBIS score (possible score range: 11–55) indicates higher levels of weight-related self-stigma. The WBIS has been reported to have good psychometric properties [37,39,40,44], including the Chinese version [45]. In the present study, the Cronbach’s α of the WBIS was 0.90 (T1) and 0.90 (T2); McDonald’s ω was 0.91 (T1) and 0.90 (T2).
Depression, Anxiety, Stress Scale (DASS-21). The DASS-21 contains 21 items assessing psychological distress, including depression, anxiety, and stress [46]. All the DASS-21 items (e.g., “I found it hard to wind down”) are rated using a four-point Likert scale (0 to 3), and a higher DASS-21 score (possible score range: 0–63) indicates higher levels of psychological distress. The DASS-21 has been reported to have good psychometric properties [46], including the Chinese version [47]. In the present study, the Cronbach’s α of the DASS-21 was 0.93 (T1) and 0.95 (T2); McDonald’s ω was 0.94 (T1) and 0.95 (T2).
Tendency to Avoid Physical Activity and Sport Scale (TAPAS). The TAPAS contains 10 items assessing how an individual tends to avoid PA or sport [48] because of considerations regarding weight, appearance, or physical fitness. All the TAPAS items (e.g., “I find myself avoiding participating in sport because of my weight”) are rated using a five-point scale (1 to 5), and a higher TAPAS score (possible score range: 10–50) indicates higher levels of tendency to avoid PA and sport. The TAPAS has been reported to have good psychometric properties in the literature [48], including the Chinese version [49]. In the present study, the Cronbach’s α of the TAPAS was 0.94 (T1) and 0.94 (T2); McDonald’s ω was 0.94 (T1) and 0.94 (T2).
The participants’ demographics and scores on the measures were analyzed using descriptive statistics (e.g., means with standard deviations (SDs) and frequencies with percentages). Moreover, skewness and kurtosis values were used to examine if the continuous variables were normally distributed. When both skewness and kurtosis values are smaller than 3, normal distribution is supported. Pearson correlations were then used to examine the associations between the studied variables of PWSS, WBIS, DASS-21, and TAPAS scores at T1 and T2. A mediation model was then constructed to examine the mediating effects of WBIS and DASS-21 change scores in the association of PWSS with TAPAS change scores. In the mediation model, age, gender, and body mass index (BMI) were controlled for. The change scores of WBIS, DASS-21, PWSS, and TAPAS were calculated using their T2 scores minus T1 scores.
Moreover, a parallel mediation model was chosen to examine the mediating effect (i.e., Model 4 in the Hayes’ Process Macro) [50] and 5000 bootstrapping resamples were used to examine the mediating effects. The mediating effects are significant when the 95% confidence interval (CI) of the bootstrapping resample findings does not include 0 [51]. All the statistical analyses were conducted using the IBM SPSS 20.0 (IBM Corp., Armonk, NY, USA).
Among the 592 participants, 388 completed the Time 2 (T2) survey between February and April 2023 (34.4% attrition rate). There were no significant differences between the participants who completed two waves of surveys (n = 388) and those who only completed the T1 survey (n = 204) in terms of their gender (only completed T1: 45.1% male, 54.4% female, and 0.5% other; completed T1 and T2: 45.1% male, 54.6% female, and 0.3% other; p = 1.00) and body mass index (only completed T1: 23.89 [SD ± 4.75]; completed T1 and T2: 23.93 [SD ± 4.22]; p = 0.92). However, those who only completed the T1 survey were significantly younger than those who completed T1 and T2 surveys (28.12 years [SD ± 6.37] vs. 29.65 years [SD ± 6.27]; p = 0.01). Because the attrition rate was lower than 40% with nonsignificant to trivial differences between the retained and lost samples in the present study, the findings were not likely to have any severe biases.
The analyzed data included 388 participants who completed both T1 and T2 surveys. Over half of the 388 participants were female (n = 212; 54.6%), and one participant identified gender as other (0.3%), with the remaining participants being male (n = 175; 45.1%). Detailed information on the participants’ characteristics is presented in Table 1. In particular, over half of the participants did not have perceived weight stigma because 57.5% of the participants scored 0 for the PWSS at T1 and 59.3% at T2. Moreover, all the continuous variable scores were normally distributed (i.e., both skewness and kurtosis values <3).
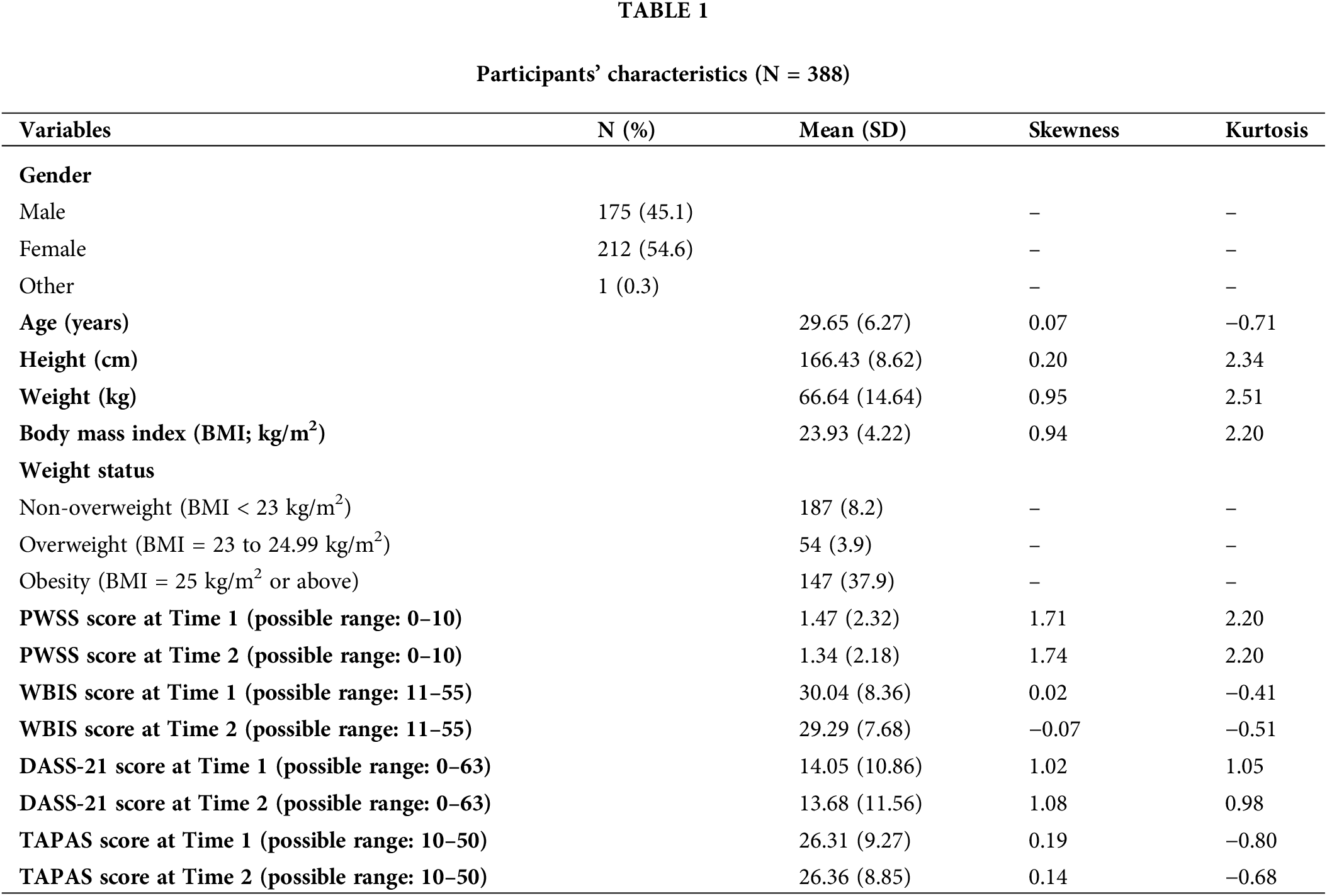
Table 2 presents the Pearson correlation coefficients between PWSS, WBIS, DASS-21, and TAPAS scores across T1 and T2. All the correlations were significant with the magnitude of r-values ranging between 0.24 and 0.69 (all p-values < 0.001). The mediation model results are presented in Table 3 and Fig. 1. More specifically, (i) PWSS score had significant direct effects on both WBIS (standardized coefficient [β] = 0.25; p < 0.001) and DASS-21 (β = 0.15; p = 0.003); and (ii) WBIS (β = 0.47; p < 0.001) but not DASS-21 (β = 0.08; p = 0.077) had significantly direct effects on TAPAS. In addition, the standardized indirect effect of (i) WBIS in the association of PWSS with TAPAS was 0.12 (bootstrapping SE = 0.04; 95% bootstrapping CI = 0.04, 0.20); and (ii) DASS-21 in the association of PWSS with TAPAS was 0.01 (bootstrapping SE = 0.01; 95% bootstrapping CI = −0.001, 0.03). The standardized total effect of PWSS on TAPAS (i.e., direct effect and indirect effects via WBIS and DASS-21) was 0.13 (bootstrapping SE = 0.04; 95% bootstrapping CI = 0.05, 0.21).
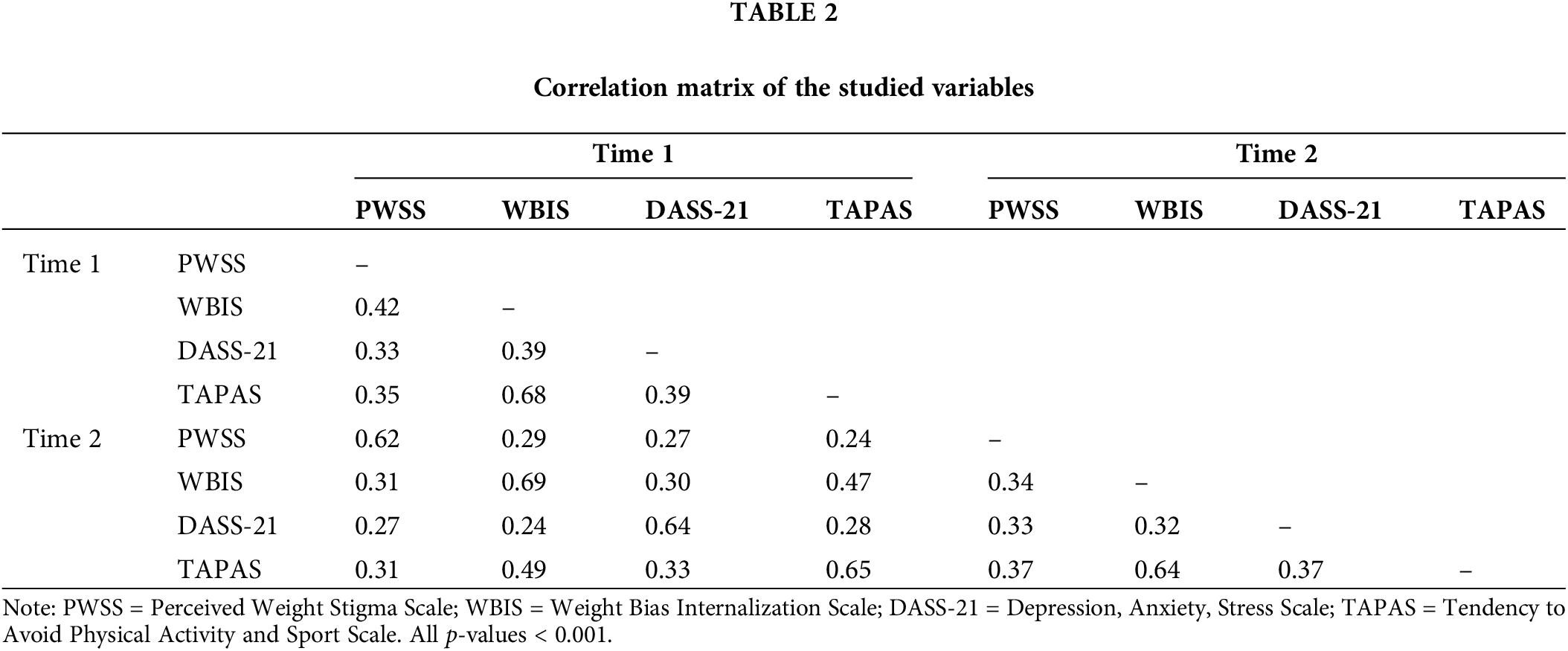
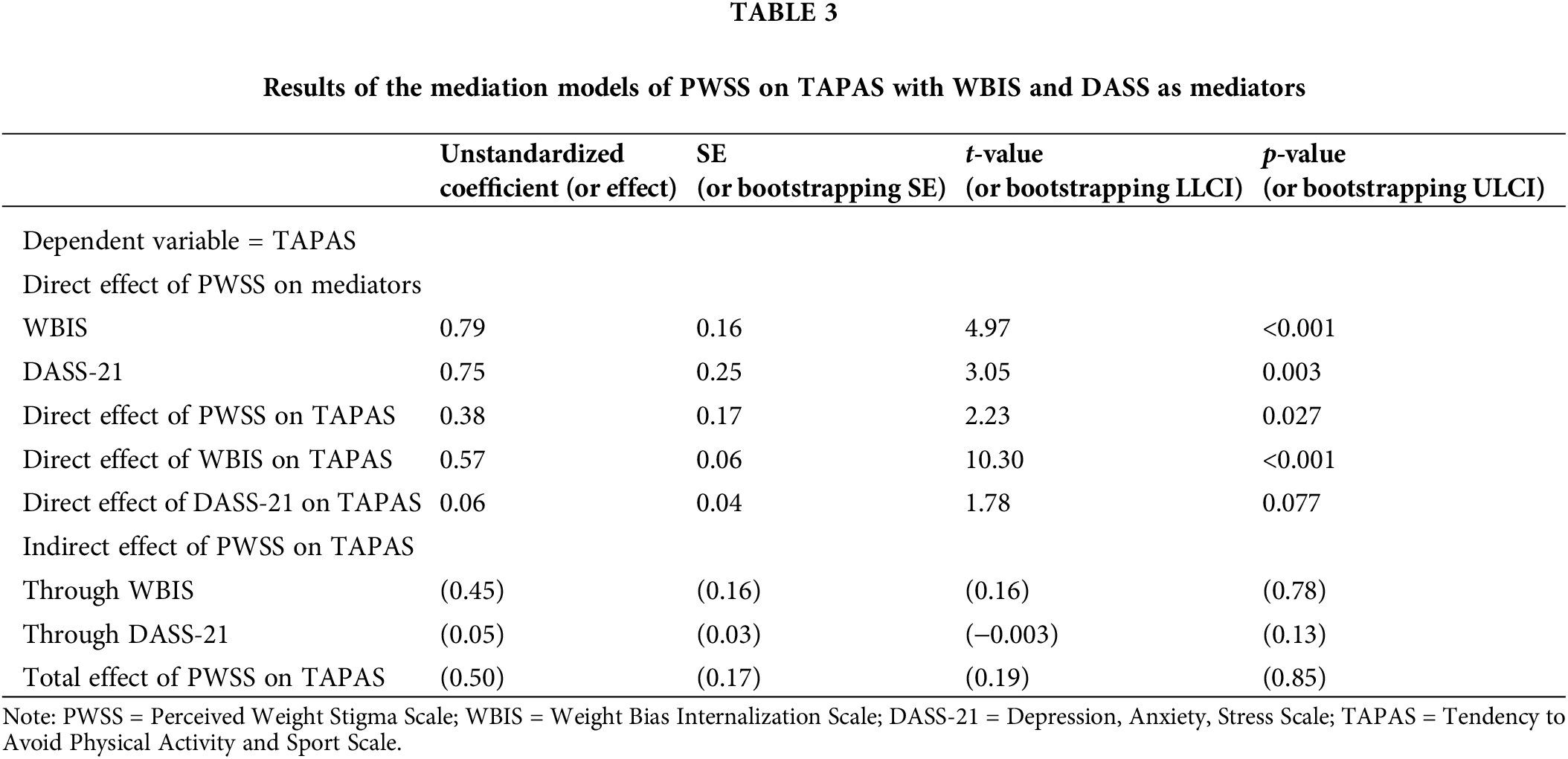
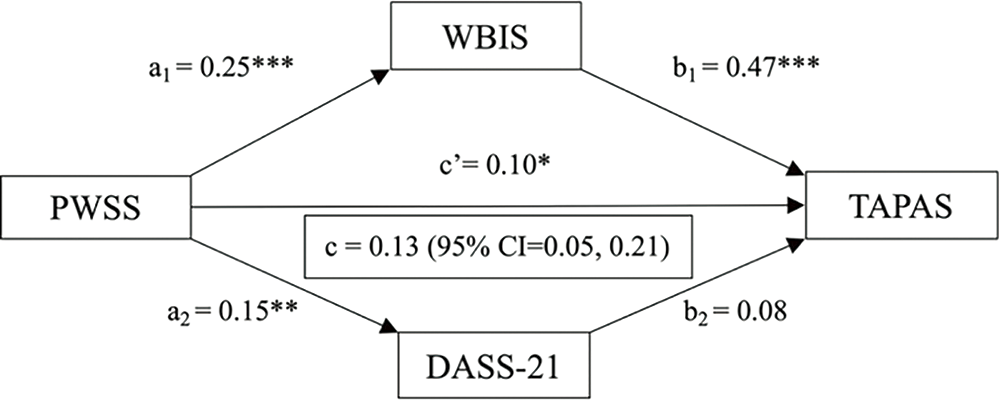
Figure 1: Results of the mediation model for Perceived Weight Stigma Scale (PWSS), Weight Bias Internalization Scale (WBIS), Depression Anxiety Stress Scale (DASS-21), and Tendency to Avoid Physical Activity and Sport Scale (TAPAS).
Note: *p < 0.05, **p < 0.01, ***p < 0.001; 95% CI = 95% bootstrapping confidence interval; a1 = standardized coefficient from PWSS to WBIS; b1 = standardized coefficient from WBIS to TAPAS; a2 = standardized coefficient from PWSS to DASS-21; b2 = standardized coefficient from DASS-21 to TAPAS; c’ = standardized coefficient from PWSS to TAPAS (i.e., standardized direct effect); c = standardized total effect.
The present study was designed to investigate the associations between weight bias (WS) (including perceived WS and weight bias internalization [WBI]) and the tendency to avoid physical activity (PA) among a convenience sample of the Taiwanese population. Moreover, the indirect associations between these two variables were assessed by including WBI and psychological distress as the mediators. The study findings indicated that while there was a significant association between the main variables of the study (i.e., perceived WS and tendency to avoid PA), there were significantly notable associations between the PWSS and both psychological distress and internalization of weight bias. The mediating role of WBI in the relationship between the main variables was also significant. However, the indirect association between perceived WS and the tendency to avoid PA via psychological distress was not confirmed.
Several studies have assessed the relationships between WS and PA particularly among youth. In a cross-sectional survey, Ajibewa et al. [17] examined the relationship between prior WS experiences and PA intention among college students. The average body mass index (BMI) score was similar to that of the present sample (23.9 ± 4 kg/m2). They found that prior experiences with WS were significantly associated with PA avoidance, while the association between WS and intention to do PA was non-significant [17]. Bevan et al. [48] in a similar study among college students that the development of the Tendency to Avoid Physical Activity and Sport Scale (TAPAS) (the scale used in the present study), recommended that due to the strong association between the WS and PA, any attempts to increase PA participation must firstly address WS concerns particularly among individuals who are overweight or have obesity [48]. A systematic review conducted in 2021 found 38 studies that investigated the associations between WS and PA. It was concluded that both perceived WS and WBI had significant associations with PA behaviors [16]. Moreover, direct and indirect effects of WS on PA were recognized which concur with the present study’s findings. However, one specific matter that differentiates the present study’s findings from previous results is the utilization of a new scale to assess the tendency to avoid PA. Apart from the study by Bevan et al., all the previous studies’ assessments were carried out by assessing PA behaviors through observation or self-report [16], whereas the present study did not assess the actual PA behaviors but rather the tendency to avoid such behaviors. It is believed that because the tendency to engage in or not to engage in a specific behavior may be a prerequisite of that behavior happening, it may provide more accurate information on the likelihood of its occurrence in the future.
To the best of the authors’ knowledge, the present study is the first to investigate the indirect pathways between perceived self-stigma and the tendency to avoid PA. Previous studies have confirmed the association between WS, and the mediators used in the present study (WBI and psychological distress). For example, Romano et al. suggested that due to the strong association between perceived WS and WBI and since WBI may be an underlying factor for general WS, interventions focusing on WBI are recommended for individuals who are overweight or have obesity [21]. Shank et al., in assessing the relationships between WS, WBI, and physical health among military personnel who were mostly at-risk of obesity, found that while WS and WBI were positively associated, only WS predicted a medical condition among these individuals and the WBI was not a significant predictor [52]. This finding confirms that although these variables are very similar, each one assesses different things, and they may be considered as underlying contributors for explaining their associations with other biopsychological variables.
In a study relatively similar to the present one, O’Brien et al. [20] assessed the relationship between WS and eating disorders by examining WBI and psychological distress as the mediators. They recruited 632 college students to complete an online survey and reported a direct association between WS and eating disorders. In addition, indirect associations between these two variables via WBI and psychological distress confirmed their mediating roles [20]. Although the measure used by O’Brien et al. to investigate WS differed from that of the present study, the same measures were used to assess WBI and psychological distress in both studies, suggesting consistency of measurement except for the dependent variable (eating disorders vs. TAPAS). Because diet and PA have determinative roles in weight-related problems, especially among those who are overweight or have obesity (and both are inter-correlated), similar results for both studies would be expected.
However, in the present study, the indirect association between WS and the dependent variable (i.e., PA) via psychological distress was non-significant (unlike the study by O’Brien et al. [20]). In addition to the similarities between these studies, there are also considerable differences between them that may explain relatively different outcomes. First and most important, there were different dependent variables. While there are associations between eating disorders such as polyphagia and the tendency to avoid PA [53], these are related to otherbehavioral patterns and are not necessarily inter-correlated. Second, the present study had a longitudinal design in an attempt to establish causation between variables since it covers the changes over time. In contrast, O’Brien et al.’s study [20] had a cross-sectional design. Third, the cultural differences between the two samples may also be a possible source of difference in outcomes.
Despite the strengths of the present study, such as the longitudinal design with adequate sample size and robust statistical methods to assess the likely associations (mediation analysis), several limitations should be noted when interpreting the results. First, a convenience sample was used with no specific inclusion or exclusion criteria, and all interested individuals could participate. Therefore, the generalizability of the findings specifically for defined categories of the individuals in terms of BMI or other relevant criteria was limited. Second, although the individuals who participated in the study in the second wave of data collection were not so different from the first wave in terms of demographic characteristics, there was an attrition rate of approximately 35% that may have negatively impacted the external validity of the findings. Third, all measures used were subjective and susceptible to reporting biases such as social desirability or recall bias. More objective measures, such as assessing the behaviors through observation or an individual’s actual height and weight, would likely provide more trustworthy data. Moreover, the variables used in the present study were primarily psychological and no objective measures were used to assess PA.
Along with the direct association between perceived WS and the tendency to avoid PA, these variables may also be correlated through bilateral mechanisms, including the WBI. Perceived WS should be considered as a likely source both for WBI as well as avoiding PA. Therefore, any program planning to address physical inactivity across weight status from healthy weight to obesity should include WS reduction strategies to be successful. For example, program planners may suggest environments that are supportive for PA among people with overweight/obesity without any triggers that may arouse weight stigma. Also, when exercising, grouping people with the same anthropometric measures may reduce the chance of weight stigmatization. Moreover, due to the underlying effect of WBI in the association between the PWSS and TAPAS, addressing interventions to reduce WBI would be helpful to improve PA intention, particularly among those who are at higher risk for weight gain and obesity. Therefore, further assessment of other likely effective psychological mediators such as self-esteem and self-concept in such associations are warranted.
Acknowledgement: We thank all the individuals who participated in the study.
Funding Statement: This research was funded by the Ministry of Science and Technology, Taiwan (MOST 110-2410-H-006-115; MOST 111-2410-H-006-100; NSTC 112-2410-H-006-089-SS2), E-Da Hospital (EDAHS112032, EDAHS113021 and EDAHS113036), and the Higher Education Sprout Project, Ministry of Education to the Headquarters of University Advancement at National Cheng Kung University (NCKU).
Author Contributions: Conceptualization, Saffari Mohsen, Yi-Ching Lin, Po-Ching Huang, Yu-Ting Huang, Ru-Yi Huang, Chi Hsien Huang, Jung-Sheng Chen, Wai Chuen Poon, Mark D. Griffiths, Chung-Ying Lin; methodology, Yi-Ching Lin, Po-Ching Huang, Yu-Ting Huang, Chi Hsien Huang, Chung-Ying Lin; software, Chung-Ying Lin; validation, Saffari Mohsen, Yi-Ching Lin, Po-Ching Huang, Yu-Ting Huang, Ru-Yi Huang, Chi Hsien Huang, Jung-Sheng Chen, Mark D. Griffiths, Chung-Ying Lin; formal analysis, Chung-Ying Lin; investigation, Yi-Ching Lin, Ru Yi Huang, Chi Hsien Huang, Chung-Ying Lin; resources, Yi-Ching Lin, Ru-Yi Huang, Chi Hsien Huang, Chung-Ying Lin; data curation, Yi-ChingLin, Po-Ching Huang, Ru-Yi Huang, Chung-Ying Lin; writing—original draft preparation, Saffari Mohsen, Chung-Ying Lin; writing—review and editing, Saffari Mohsen, Yi-Ching Lin, Po-Ching Huang, Yu-Ting Huang, Ru-Yi Huang, Chi Hsien Huang, Jung-Sheng Chen, Wai Chuen Poon, Mark D. Griffiths, Chung-Ying Lin; visualization, Chung-Ying Lin; supervision, Chung-Ying Lin; project administration, Chung-Ying Lin; funding acquisition, Ru-Yi Huang, Chi Hsien Huang, Chung-Ying Lin. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data used and/or analyzed during the present study are available from the corresponding author upon reasonable request.
Ethics Approval: The procedures for both T1 and T2 surveys adhered to the (i) Declaration of Helsinki, and (ii) ethical principles for medical, psychological, and sociological research involving human participants. The National Cheng Kung University Human Research Ethics Committee approved the study protocol (Approval No. NCKU HREC-E-110-486-2). All participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Wong MCS, Huang J, Wang J, Chan PSF, Lok V, Chen X, et al. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol. 2020;35(7):673–83. doi:10.1007/s10654-020-00650-3. [Google Scholar] [PubMed] [CrossRef]
2. World Health Organization. Obesity and overweight. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [Accessed 2023]. [Google Scholar]
3. Mu L, Liu J, Zhou G, Wu C, Chen B, Lu Y, et al. Obesity prevalence and risks among Chinese adults: findings from the China PEACE Million Persons Project, 2014–2018. Circ Cardiovasc Qual Outcomes. 2021;14(6):e007292. doi:10.1161/circoutcomes.120.007292. [Google Scholar] [PubMed] [CrossRef]
4. Non-Communicable Disease Branch-Centre for Health Protection. Report of population health survey. Available from: https://www.chp.gov.hk/files/pdf/dh_phs_2020-22_part_1_report_eng_rectified.pdf. [Accessed 2023]. [Google Scholar]
5. Hsieh TH, Lee JJ, Yu EWR, Hu HY, Lin SI, Ho CY. Association between obesity and education level among the elderly in Taipei, Taiwan between 2013 and 2015: a cross-sectional study. Sci Rep. 2020;10(1):20285. doi:10.1038/s41598-020-77306-5. [Google Scholar] [PubMed] [CrossRef]
6. Tan K, WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63. doi:10.1016/S0140-6736(03)15268-3. [Google Scholar] [PubMed] [CrossRef]
7. Kinlen D, Cody D, O’Shea D. Complications of obesity. QJM. 2018;111(7):437–43. doi:10.1093/qjmed/hcx152. [Google Scholar] [PubMed] [CrossRef]
8. Fulton S, Décarie-Spain L, Fioramonti X, Guiard B, Nakajima S. The menace of obesity to depression and anxiety prevalence. Trends Endocrinol Metab. 2022;33(1):18–35. doi:10.1016/j.tem.2021.10.005. [Google Scholar] [PubMed] [CrossRef]
9. Sánchez-Rojas AA, García-Galicia A, Vázquez-Cruz E, Montiel-Jarquín ÁJ, Aréchiga-Santamaría A. Self-image, self-esteem and depression in children and adolescents with and without obesity. Gaceta Medica de Mexico. 2022;158(3):118–23. doi:10.24875/gmm.m22000653. [Google Scholar] [PubMed] [CrossRef]
10. Rupp K, McCoy SM. Bullying perpetration and victimization among adolescents with overweight and obesity in a nationally representative sample. Childhood Obes. 2019;15(5):323–30. doi:10.1089/chi.2018.0233. [Google Scholar] [PubMed] [CrossRef]
11. Wu YK, Berry DC. Impact of weight stigma on physiological and psychological health outcomes for overweight and obese adults: a systematic review. J Adv Nurs. 2018;74(5):1030–42. doi:10.1111/jan.13511. [Google Scholar] [PubMed] [CrossRef]
12. Prunty A, Clark MK, Hahn A, Edmonds S, O’Shea A. Enacted weight stigma and weight self-stigma prevalence among 3821 adults. Obes Res Clin Pract. 2020;14(5):421–7. doi:10.1016/j.orcp.2020.09.003. [Google Scholar] [PubMed] [CrossRef]
13. Warnick JL, Darling KE, West CE, Jones L, Jelalian E. Weight stigma and mental health in youth: a systematic review and meta-analysis. J Pediatr Psychol. 2022;47(3):237–55. doi:10.1093/jpepsy/jsab110. [Google Scholar] [PubMed] [CrossRef]
14. Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–28. doi:10.2105/ajph.2009.159491. [Google Scholar] [PubMed] [CrossRef]
15. Brochu PM. Weight stigma as a risk factor for suicidality. Int J Obes. 2020;44(10):1979–80. doi:10.1038/s41366-020-0632-5. [Google Scholar] [PubMed] [CrossRef]
16. Pearl RL, Wadden TA, Jakicic JM. Is weight stigma associated with physical activity? A systematic review. Obesity. 2021;29(12):1994–2012. doi:10.1002/oby.23274. [Google Scholar] [PubMed] [CrossRef]
17. Ajibewa TA, Sonneville KR, Miller AL, Toledo-Corral CM, Robinson LE, Hasson RE. Weight stigma and physical activity avoidance among college-aged students. J Am Coll Health. 2022;2022:1–5. doi:10.1080/07448481.2022.2123708. [Google Scholar] [PubMed] [CrossRef]
18. Chu DT, Minh Nguyet NT, Nga VT, Thai Lien NV, Vo DD, Lien N, et al. An update on obesity: mental consequences and psychological interventions. Diabetes Metab Syndr. 2019;13(1):155–60. doi:10.1016/j.dsx.2018.07.015. [Google Scholar] [PubMed] [CrossRef]
19. Ajibewa TA, Adams TA, Gill AK, Mazin LE, Gerras JE, Hasson RE. Stress coping strategies and stress reactivity in adolescents with overweight/obesity. Stress Health. 2021;37(2):243–54. doi:10.1002/smi.2987. [Google Scholar] [PubMed] [CrossRef]
20. O’Brien KS, Latner JD, Puhl RM, Vartanian LR, Giles C, Griva K, et al. The relationship between weight stigma and eating behavior is explained by weight bias internalization and psychological distress. Appetite. 2016;102:70–6. doi:10.1016/j.appet.2016.02.032. [Google Scholar] [PubMed] [CrossRef]
21. Romano KA, Heron KE, Henson JM. Examining associations among weight stigma, weight bias internalization, body dissatisfaction, and eating disorder symptoms: does weight status matter? Body Image. 2021;37:38–49. doi:10.1016/j.bodyim.2021.01.006. [Google Scholar] [PubMed] [CrossRef]
22. Hübner C, Schmidt R, Selle J, Köhler H, Müller A, de Zwaan M, et al. Comparing self-report measures of internalized weight stigma: the weight self-stigma questionnaire versus the weight bias internalization scale. PLoS One. 2016;11(10):e0165566. doi:10.1371/journal.pone.0165566. [Google Scholar] [PubMed] [CrossRef]
23. Romano KA, Heron KE, Sandoval CM, MacIntyre RI, Howard LM, Scott M, et al. Weight bias internalization and psychosocial, physical, and behavioral health: a meta-analysis of cross-sectional and prospective associations. Behav Ther. 2023;54(3):539–56. doi:10.1016/j.beth.2022.12.003. [Google Scholar] [PubMed] [CrossRef]
24. Meadows A, Higgs S. A bifactor analysis of the Weight Bias Internalization Scale: what are we really measuring? Body Image. 2020;33:137–51. doi:10.1016/j.bodyim.2020.02.013. [Google Scholar] [PubMed] [CrossRef]
25. Levy M, Kakinami L, Alberga AS. The relationship between weight bias internalization and healthy and unhealthy weight control behaviours. Eat Weight Disord. 2022;27(5):1621–32. doi:10.1007/s40519-021-01291-5. [Google Scholar] [PubMed] [CrossRef]
26. Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018;19(8):1141–63. doi:10.1111/obr.12701. [Google Scholar] [PubMed] [CrossRef]
27. Ievers-Landis CE, Dykstra C, Uli N, O’Riordan MA. Weight-related teasing of adolescents who are primarily obese: roles of sociocultural attitudes towards appearance and physical activity self-efficacy. Int J Environ Res Public Health. 2019;16(9). doi:10.3390/ijerph16091540. [Google Scholar] [PubMed] [CrossRef]
28. Maïano C, Lepage G, Aimé A, Bayard C, Dansereau-Trahan É., Granger L, et al. Perceived weight-related victimization and physical activity outcomes among adolescents with overweight and obesity: indirect role of perceived physical abilities and fear of enacted stigma. Psychol Sport Exerc. 2018;34:70–8. doi:10.1016/j.psychsport.2017.08.007. [Google Scholar] [CrossRef]
29. Gayes LA, Steele RG. Comparison of two measures of weight criticism in youth: associations with physical activity engagement and attitudes, weight status, and health-related quality of life. J Pediatr Psychol. 2015;40(2):228–37. doi:10.1093/jpepsy/jsu080. [Google Scholar] [PubMed] [CrossRef]
30. Watanabe PI, Fontana FE, Silva MPD, Mazzardo O, Bacil EDA, Campos WD. Association between weight-teasing and physical activity in adolescents. Rev Paul Pediatr. 2017;35:309–15. doi:10.1590/1984-0462/;2017;35;3;00005. [Google Scholar] [PubMed] [CrossRef]
31. Martins Neto C, Confortin SC, Lima ABS, Mouzinho LSN, Oliveira B. Association between perceived discrimination and physical activity among adolescents. Cien Saude Colet. 2022;27(10):4003–13. doi:10.1590/1413-812320222710.05992022. [Google Scholar] [PubMed] [CrossRef]
32. Pearce M, Garcia L, Abbas A, Strain T, Schuch FB, Golubic R, et al. Association between physical activity and risk of depression: a systematic review and meta-analysis. JAMA Psychiat. 2022;79(6):550–9. doi:10.1001/jamapsychiatry.2022.0609. [Google Scholar] [PubMed] [CrossRef]
33. Saffari M, Wu HC, Chen JK, Bevan N, Chen JS, Chen HP, et al. Psychometric properties of the Tendency to Avoid Physical Activity and Sport Scale among Hong Kong university students. Meas Phys Educ Exerc Sci. 2024;1–11. doi:10.1080/1091367X.2024.2302607. [Google Scholar] [CrossRef]
34. Yi J, Chen IH, Chen HP, Lin IC, Chen JS, Huang PC, et al. Tendency to avoid physical activity mediates the association between perceived weight stigma and physical activity levels among university students. Ment Health Phys Act. 2024;26:100584. doi:10.1016/j.mhpa.2024.100584. [Google Scholar] [CrossRef]
35. Huang PC, Chen JS, Potenza MN, Griffiths MD, Pakpour AH, Chen JK, et al. Temporal associations between physical activity and three types of problematic use of the internet: a six-month longitudinal study. J Behav Addict. 2022;11(4):1055–67. doi:10.1556/2006.2022.00084. [Google Scholar] [PubMed] [CrossRef]
36. Kristman V, Manno M, Cote P. Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol. 2004;19(8):751–60. doi:10.1023/b:ejep.0000036568.02655.f8. [Google Scholar] [PubMed] [CrossRef]
37. Nadhiroh SR, Nurmala I, Pramukti I, Tivany ST, Tyas LW, Zari AP, et al. Weight stigma in Indonesian young adults: validating the Indonesian versions of the Weight Self-Stigma Questionnaire and Perceived Weight Stigma Scale. Asian J Soc Health Behav. 2022;5(4):169. doi:10.4103/shb.shb_189_22. [Google Scholar] [CrossRef]
38. Cheng MY, Wang SM, Lam YY, Luk HT, Man YC, Lin CY. The relationships between weight bias, perceived weight stigma, eating behavior, and psychological distress among undergraduate students in Hong Kong. J Nerv Ment Dis. 2018;206(9):705–10. doi:10.1097/NMD.0000000000000869. [Google Scholar] [PubMed] [CrossRef]
39. Andrés A, Fornieles-Deu A, Sepúlveda AR, Beltrán-Garrayo L, Montcada-Ribera A, Bach-Faig A, et al. Spanish validation of the modified weight bias internalization scale (WBIS-M) for adolescents. Eat Weight Disord. 2022;27(8):3245–56. doi:10.1007/s40519-022-01453-z. [Google Scholar] [PubMed] [CrossRef]
40. Lee MS, Dedrick RF. Weight Bias Internalization Scale: psychometric properties using alternative weight status classification approaches. Body Image. 2016;17:25–9. doi:10.1016/j.bodyim.2016.01.008. [Google Scholar] [PubMed] [CrossRef]
41. Ruckwongpatr K, Saffari M, Fung XCC, O’Brien KS, Chang YL, Lin YC, et al. The mediation effect of perceived weight stigma in association between weight status and eating disturbances among university students: is there any gender difference? J Eat Disord. 2022;10(1):28. doi:10.1186/s40337-022-00552-7. [Google Scholar] [PubMed] [CrossRef]
42. Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity. 2008;16:S80–6. doi:10.1038/oby.2008.448. [Google Scholar] [PubMed] [CrossRef]
43. Pearl RL, Puhl RM. Measuring internalized weight attitudes across body weight categories: validation of the modified weight bias internalization scale. Body Image. 2014;11(1):89–92. doi:10.1016/j.bodyim.2013.09.005. [Google Scholar] [PubMed] [CrossRef]
44. Macho S, Andrés A, Saldaña C. Validation of the modified Weight Bias Internalization Scale in a Spanish adult population. Clin Obes. 2021;11(4):e12454. doi:10.1111/cob.12454. [Google Scholar] [PubMed] [CrossRef]
45. Pakpour AH, Tsai MC, Lin YC, Strong C, Latner JD, Fung XCC, et al. Psychometric properties and measurement invariance of the Weight Self-Stigma Questionnaire and Weight Bias Internalization Scale in children and adolescents. Int J Clin Health Psychol. 2019;19(2):150–9. doi:10.1016/j.ijchp.2019.03.001. [Google Scholar] [PubMed] [CrossRef]
46. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43. doi:10.1016/0005-7967(94)00075-u. [Google Scholar] [PubMed] [CrossRef]
47. Zanon C, Brenner RE, Baptista MN, Vogel DL, Rubin M, Al-Darmaki FR, et al. Examining the dimensionality, reliability, and invariance of the Depression, Anxiety, and Stress Scale-21 (DASS-21) across eight countries. Assessment. 2021;28(6):1531–44. doi:10.1177/1073191119887449. [Google Scholar] [PubMed] [CrossRef]
48. Bevan N, O’Brien KS, Latner JD, Lin CY, Vandenberg B, Jeanes R, et al. Weight stigma and avoidance of physical activity and sport: development of a scale and establishment of correlates. Int J Environ Res Public Health. 2022;19(23):16370. doi:10.3390/ijerph192316370. [Google Scholar] [PubMed] [CrossRef]
49. Saffari M, Chen IH, Huang PC, O’Brien KS, Hsieh YP, Chen JK, et al. Measurement invariance and psychometric evaluation of the Tendency to Avoid Physical Activity and Sport Scale (TAPAS) among mainland Chinese university students. Psychol Res Behav Manag. 2023;2023(16):3821–36. doi:10.2147/PRBM.S425804. [Google Scholar] [PubMed] [CrossRef]
50. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Publications; 2017. [Google Scholar]
51. Levy JA, Landerman LR, Davis LL. Advances in mediation analysis can facilitate nursing research. Nurs Res. 2011;60(5):333–9. doi:10.1097/NNR.0b013e318227efca. [Google Scholar] [PubMed] [CrossRef]
52. Shank LM, Schvey NA, Ekundayo K, Schreiber-Gregory D, Bates D, Maurer D, et al. The relationship between weight stigma, weight bias internalization, and physical health in military personnel with or at high-risk of overweight/obesity. Body Image. 2019;28:25–33. doi:10.1016/j.bodyim.2018.11.003. [Google Scholar] [PubMed] [CrossRef]
53. Rizk M, Mattar L, Kern L, Berthoz S, Duclos J, Viltart O, et al. Physical activity in eating disorders: a systematic review. Nutrients. 2020;12(1). doi:10.3390/nu12010183. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools