 Open Access
Open Access
ARTICLE
An Experimental Study on the Effectiveness of Individualized Online Intervention for Mental Health Literacy of Community Residents
1 School of Economics, Wuhan Textile University, Wuhan, 430200, China
2 School of Psychology, Central China Normal University, Wuhan, 430079, China
3 School of Management, Wuhan University of Technology, Wuhan, 430070, China
4 School of Public Administration, Zhongnan University of Economics and Law, Wuhan, 430200, China
* Corresponding Author: Mian Xia. Email:
International Journal of Mental Health Promotion 2024, 26(8), 663-670. https://doi.org/10.32604/ijmhp.2024.049161
Received 29 December 2023; Accepted 06 May 2024; Issue published 30 August 2024
Abstract
Background: Understanding how to improve mental health literacy is conducive to maintaining and promoting individuals’ mental health and well-being. However, to date, interventions for mental health literacy primarily depend on traditional education and contact interventions, which have limitations with regard to pertinence and individualization. Artificial intelligence (AI) and big data technology have influenced mental health services to be more intellectual and digital, and they also provide greater technical convenience for individualized interventions for promoting mental health literacy. However, there is relatively little research on the effectiveness of individualized online intervention for mental health literacy in the literature. This study aims to fill this void. To verify whether individualized online intervention can improve the level of mental health literacy. Methods: We conducted a pretest–post-test control experiment. The participants were recruited from a large community located in central China. A total of 152 participants completed the research. We use mixed linear model estimation and paired t-tests to analyze the data. Results: Individualized online intervention can effectively improve the mental health literacy level of participants. Specifically, we found that compared with the control group, the mental health literacy in the experimental group was significantly improved after receiving individualized online intervention. Likewise, the mental health literacy of the control group has also improved after receiving individualized online intervention. In addition, we compared the mental health literacy level of the experimental group at Time 3 to those at Time 2 and found that the mental health literacy level at Time 3 had not decreased one month later. This shows that individualized online intervention was not only momentarily effective, but also had long-term efficacy. Conclusion: This study illustrates that the individualized online intervention has both great momentary and long-term effectiveness in improving community residents’ mental health literacy.Keywords
Mental health literacy refers to “the knowledge and beliefs about mental disorders that aid in their recognition, management, or prevention” [1]. It can help individuals learn about and recognize mental disorders and understand aspects of the help-seeking process regarding how and where to seek help [2–4] and then take action for better self or other mental health [5–7].
Having a high level of mental health literacy is critically important because it is closely related to significant mental health outcomes [8]. Empirical studies have consistently suggested that individuals’ mental well-being, help-seeking attitudes, life satisfaction, and self-efficacy in coping with psychological problems can be enhanced with better mental health literacy [9–12]. Given its positivity, how to improve the level of mental health literacy has been widely discussed by psychologists [8,13–15].
Generally, four types of interventions can improve mental health literacy: (a) whole-of-community campaigns [16–18], (b) educational interventions [19,20], (c) mental health first aid training [21], and (d) informational websites [22,23]. However, the demand for mental health literacy varies across individuals [3], requiring individualized approaches to enable mental health literacy. Meanwhile, the traditional mental health intervention methods have limitations in accuracy, timeliness, and effectiveness [24–26]. To a certain extent, the existing methods for improving mental health literacy are not fully able to meet individuals’ personalized needs. However, the extant research has not adequately addressed this gap. Specifically, the effectiveness of individualized online intervention for mental health literacy has not been explored in the literature. Developing individualized online intervention to address individual needs for improving mental health literacy and boosting individual mental health is thus essential.
In recent years, with the rapid development of artificial intelligence (AI) and big data technology, AI technology has become widely used in the fields of psychological problem diagnosis and counseling. Mental health services have become more intelligent and convenient [27–30], which brings more opportunities for realizing the individualization of mental health literacy interventions. The application of online interventions is also continuously evolving in the field of mental health [31–33]. Valente described the concept of “network (online) interventions” as using social network data in the process of interventions to accelerate behavior change [34]. Individualized online intervention is widely defined as the utilization of online networks to promote mental health based on the client’s individualized needs and preferences. Different from standardized network-based interventions, individualized online interventions are designed to meet individuals’ personalized needs, which makes individualized online interventions are attractive to different groups [35]. However, more studies are needed to assess whether individualized online interventions are actually effective in promoting the mental health literacy of individuals. The purpose of this study is to test whether individualized online intervention can help improve the mental health literacy. We predict that there is a positive relationship between individualized online intervention and mental health literacy. With community residents as participants, we investigated and explored whether an individualized online intervention was helpful in improving mental health literacy by adopting a continuous pretest-posttest experimental research design. This study fills the gap in the research on the relationship between individualized online intervention and mental health literacy and hopefully provides government and mental health institutions with practical guidance about how to use individualized online interventions to improve mental health literacy. Also, this study urges individuals to use individualized online intervention to improve their mental health literacy in order to boost life satisfaction and well-being.
Participants for this study were recruited from a large community located in central China. With the assistance of the community committee director, community residents were invited to participate in our survey by completing questionnaires. The questionnaires set out the aims of the study and assured potential participants that their responses would be confidential. Community residents interested in participating could leave their contact details. The study was approved by the Institutional Ethics Committee at Zhongnan University of Economics and Law (IRB number: 2022012). All participants signed the informed consent in this study.
Initially, 192 participants completed the pretest questionnaire. Following the principle of randomization, the participants were divided randomly into two groups: the experimental group and the control group. During the intervention process, 40 participants withdrew from the experiment. A total of 152 participants completed all the phases, including 75 participants in the experimental group and 77 participants in the control group. The average age of the participants was 30.9 years (SD = 12.8). Among them, 55.3% were male (n = 84) and 44.7% were female (n = 68); 15.1% (n = 23) were aged between 8 and 22 years old, 48.7% (n = 74) were between 23 and 29 years old, 21.7% (n = 33) were between 30 and 45 years old, and 14.5% (n = 22) were between 46 and 92 years old; 43.4% of participants (n = 66) had a college or university degree, 38.8% (n = 59) had a master’s degree, and 17.8% (n = 27) completed high school or less.
To enhance the reliability and validity of our experimental results, the participants were randomly divided into experimental and control groups. To examine the efficiency and differences before and after the intervention, we used a continuous pretest-posttest experimental design, which gives the advantage of comparing differences between the pretest and posttest to verify the effectiveness of an experimental treatment; to some extent, it can control the influence of “difference selection” and the loss of participants [36]. The design of this study appears in Fig. 1.
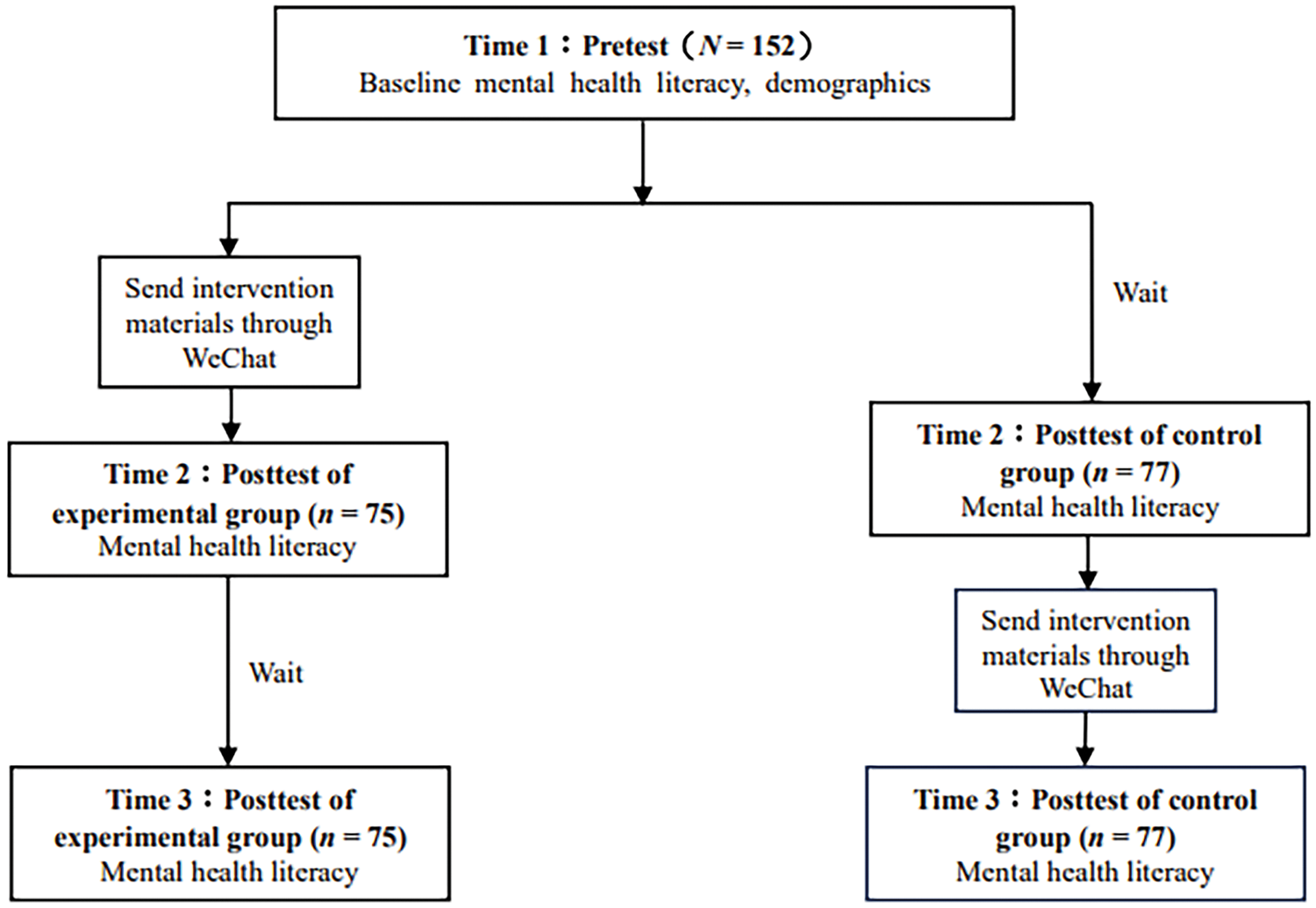
Figure 1: Experimental design
Specifically, the experimental steps were as follows. First, all the participants filled in a pretest questionnaire at Time 1, reporting the baseline level of mental health literacy and demographics (i.e., age, gender, education). Next, all the participants were randomly divided into the experimental group and the control group. The former received an experimental treatment, whereas the latter did not. When the experimental group participants finished learning all the intervention materials, the control group participants were concurrently asked to complete the posttest mental health literacy questionnaire at Time 2. Then, the differences between the two groups were compared, and if they were significant, we could infer that our individualized online intervention was effective in improving the participants’ mental health literacy.
Finally, to assess whether the intervention’s impact was momentary or relatively stable after the intervention, experimental group participants completed the survey again 1 month later (Time 3). If there was no difference or a decrease in the level of mental health literacy at Time 3 compared to Time 2, it indicated that the intervention’s effect was stable. Meanwhile, we conducted an experimental treatment for the control group by sending the intervention materials (which were the same as those in the experimental group) to the participants through WeChat. After the control group finished learning the intervention materials, we asked them to fill out the posttest questionnaire, assessing their mental health literacy at Time 3. If the level of mental health literacy in the control group also improved after the intervention, it further proved that the individualized online intervention was effective in boosting mental health literacy.
We conducted qualitative research to create our individualized intervention materials. This was done in two stages. First, we conducted a qualitative study where we content-analyzed open-ended responses from 15 community residents, comprising 5 males and 10 females. We asked them to provide open-ended responses to a question about their demands for mental health services. The participants collectively listed 43 unique demands. Three psychologists with doctoral degrees in clinical and counselling psychology content-analyzed these 43 responses independently by identifying common themes. Through discussion to reach a consensus, 15 themes emerged that fit our definition of the requested individualized online intervention. Then, we included these 15 themes in the survey for the 311 community residents in the same community to further refine the validity of the themes.
Second, we sought to reduce the number of themes by identifying the most important mental health demands of the community residents. Reducing our themes to represent the most important mental health demands ensured that the themes were both relevant to community residents and would provide variability in responses. The survey listed the 15 potential themes and asked the community residents to indicate how important each theme was, where 0 = not important at all, 1 = has minimal importance, 2 = has some importance, 3 = has moderate importance, and 4 = has great importance. Using the 311 respondents’ data, we examined the importance and relevance that community residents reported. Of the 15 themes, two were dropped because they were not important (i.e., participants reported a score of 0 on our 5-point scale) by more than 90% of the sample. Additional four were excluded due to having minimal importance for more than 80% of the sample. Finally, we reached a consensus on nine intervention themes from our analysis. The themes included knowledge about emotional adjustment and stress coping; family relationships and family atmosphere construction; mental health and mental abnormalities; identification and intervention of psychological crises; senior citizens’ mental health and emotions; adolescent psychology and parent-child communication; how to cope with pressure as parents; how to take care of family members with mental disorders; and how to cope with mental illness stigma. Based on the nine themes, we designed 19 pieces of content and corresponding interventions, including lectures, cartoons, and articles. The themes, specific contents, and corresponding intervention forms appear in Table 1.
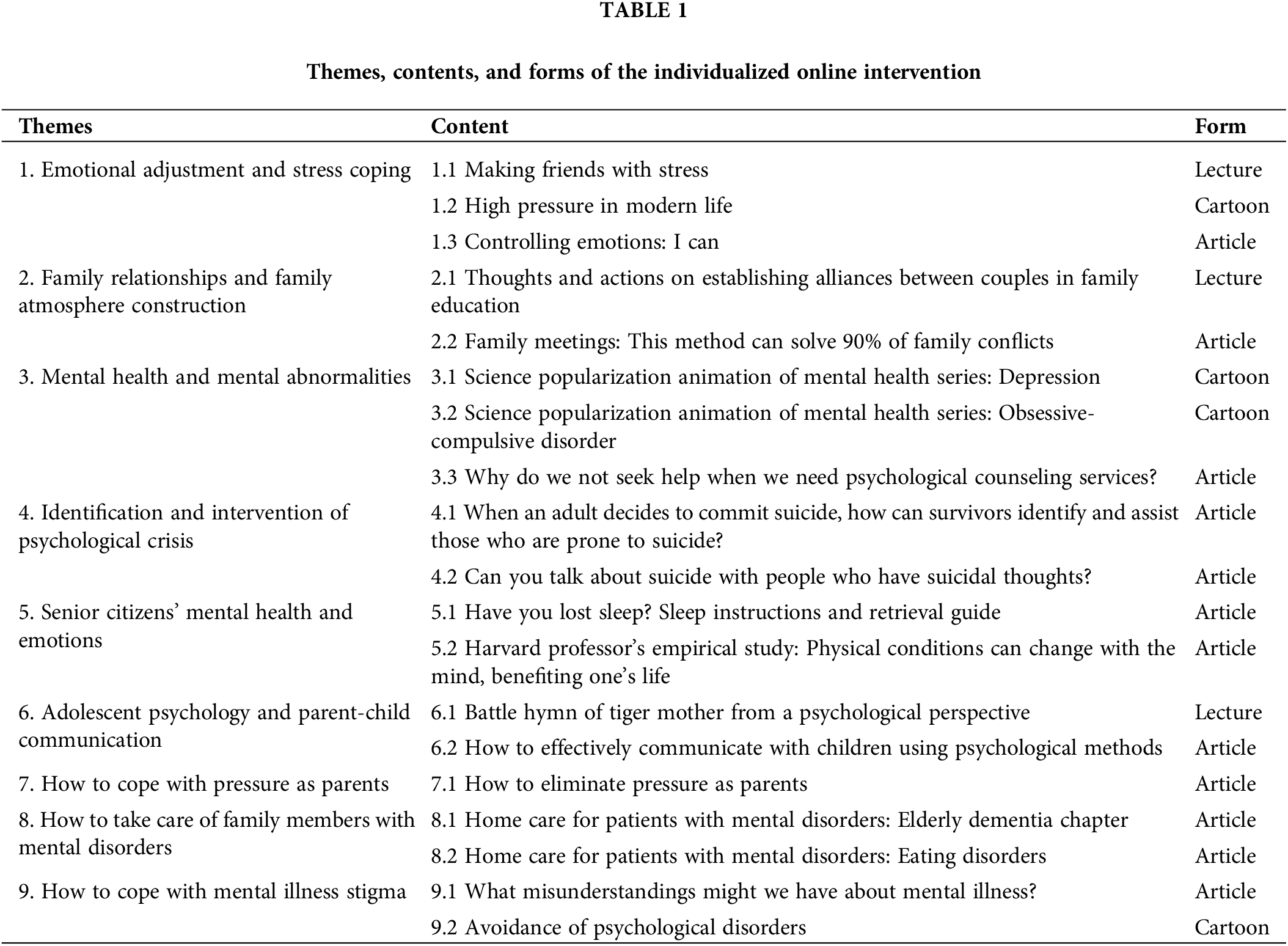
During the pretest, we provided nine themes that relate to the improvement of mental health literacy. The participants could freely choose one or more intervention themes. We then started the intervention stage, during which we sent the materials related to the intervention themes that the participants chose to each participant. After they completed learning the intervention themes, we invited the participants to complete a “challenge game” that aimed to test how well they learned and mastered the intervention materials. The contents of the challenge game all came from the invention materials. If someone failed the test, they were invited to learn the intervention material once again until they successfully passed the test.
We used the Mental Health Literacy Scale developed by Wu to assess participants’ level of mental health literacy [37]. The scale included two dimensions: knowledge and beliefs about maintaining psychological health and preventing mental disorders, and attitudes and habits of maintaining psychological health. Sample items: “Mental illness has nothing to do with genetics” (knowledge and beliefs about maintaining psychological health) and “I think my mental health is the most important thing.” With the knowledge and beliefs about maintaining psychological health subscale, participants were asked to respond true or false. “True” was coded as 1, “false” was coded as 0. With the attitudes and habits of maintaining psychological health subscale, participants were asked to respond on a Likert scale ranging from (1 = strongly disagree to 5 = strongly agree). High scores indicated a high level of mental health literacy. In the current study, the Cronbach’s alphas for the first subscale were estimated to be 0.64, 0.77, and 0.68 at Time 1, Time 2, and Time 3, respectively. The Cronbach’s alphas for the attitudes and habits of maintaining psychological health subscale were estimated to be 0.77, 0.69, and 0.74 at Time 1, Time 2, and Time 3, respectively.
In this study, SPSS 26.0 was used for data analysis and processing. The primary statistical analysis methods involved reliability analysis on the Mental Health Literacy Scale, Mann-Whitney U analysis on differences between the experimental and control groups in demographic variables, independent sample t-test on testing the effectiveness of the intervention, and paired sample t-test on testing the stability and robustness of the intervention. The highest level of significance for this study was p < 0.001.
First, to test whether there were differences in demographic variables between the experimental and control groups, we used independent sample t-testing and Mann-Whitney U tests to analyze the participants’ demographics. The age of the experimental group was significantly higher than that of the control group, with t(150) = 2.181, p = 0.03, d = 0.35, M age of experimental group = 33.17, SD age of experimental group = 14.72; M age of control group = 28.7, SD age of control group = 10.21. The Mann-Whitney U test showed that the two groups had different educational backgrounds, z = 3.232, p = 0.001. Following the guidelines of Bernerth et al. [38], we controlled for the subjects’ age and education in a follow-up statistical analysis.
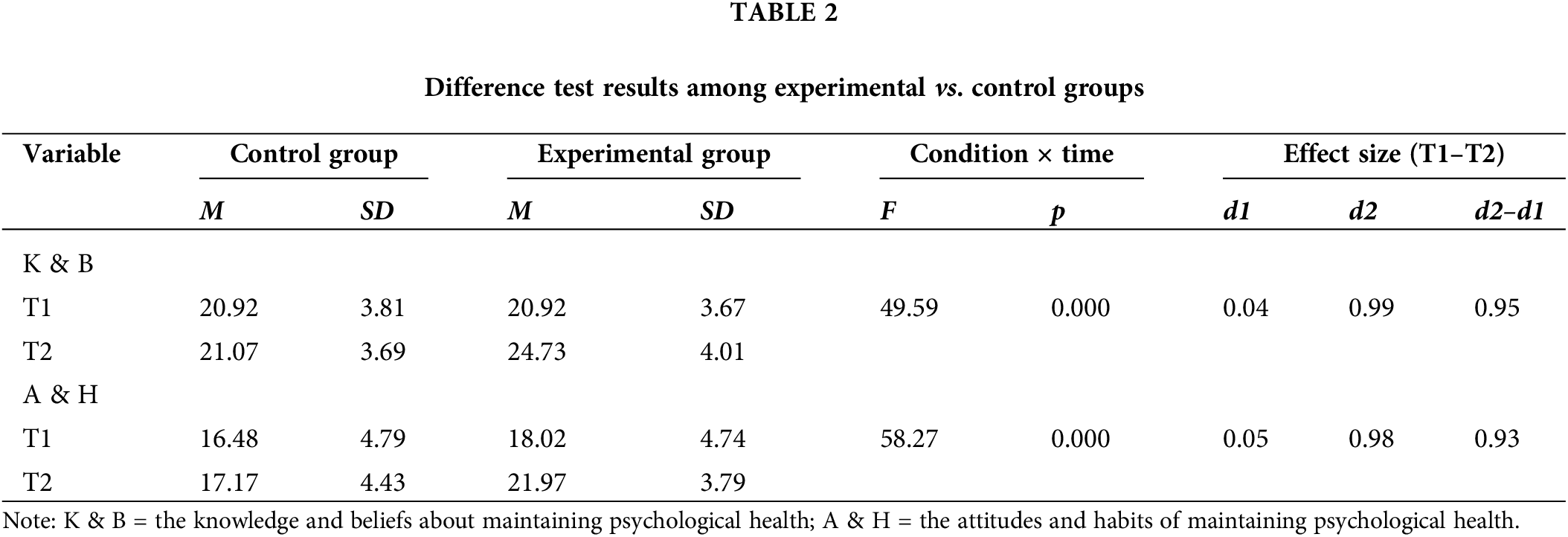
Then, to test whether there was a difference in baseline mental health literacy between the experimental and control groups, we conducted an independent sample t-test. We found no difference in the knowledge and beliefs about maintaining psychological health, M control group = 20.92, SD control group = 3.81; M experimental group = 20.92, SD experimental group = 3.67; t(150) = 1.45, p = 0.15: or in the attitudes and habits of maintaining psychological health between the two groups, M control group = 16.48, SD control group = 4.79; M experimental group = 18.02, SD experimental group = 4.74; t(150) = 0.34, p = 0.74.
Testing the effectiveness of the intervention
During Time 1 and Time 2, the experimental group received the individualized online intervention, while the control group did not receive the experimental treatment. To test whether there was any difference in mental health literacy between the experimental group and the control group from Time 1 to Time 2, we used a mixed linear model of maximum likelihood estimation. We used two dimensions of mental health literacy as dependent variables, time (Time 1, Time 2) and grouping (experimental group, control group) as factors, and age and education as covariables to conduct the analysis. As shown in Table 2, the interaction term between the knowledge and beliefs about maintaining psychological health and time was significant, F (1, 152) = 49.59, p < 0.001. A simple slope test showed that compared with the control group, the knowledge and beliefs about maintaining psychological health in the experimental group were significantly improved after the intervention, F (1, 152) = 105.90, p < 0.001, d = 0.95; the interaction term between attitudes and habits of maintaining psychological health and time was significant, F (1, 152) = 58.27, p < 0.001. A simple slope test showed that, compared with the control group, the attitudes and habits of maintaining psychological health in the experimental group were significantly improved after the intervention, F (1, 152) = 172.30, p < 0.001, d = 0.93.
Testing the stability of the intervention
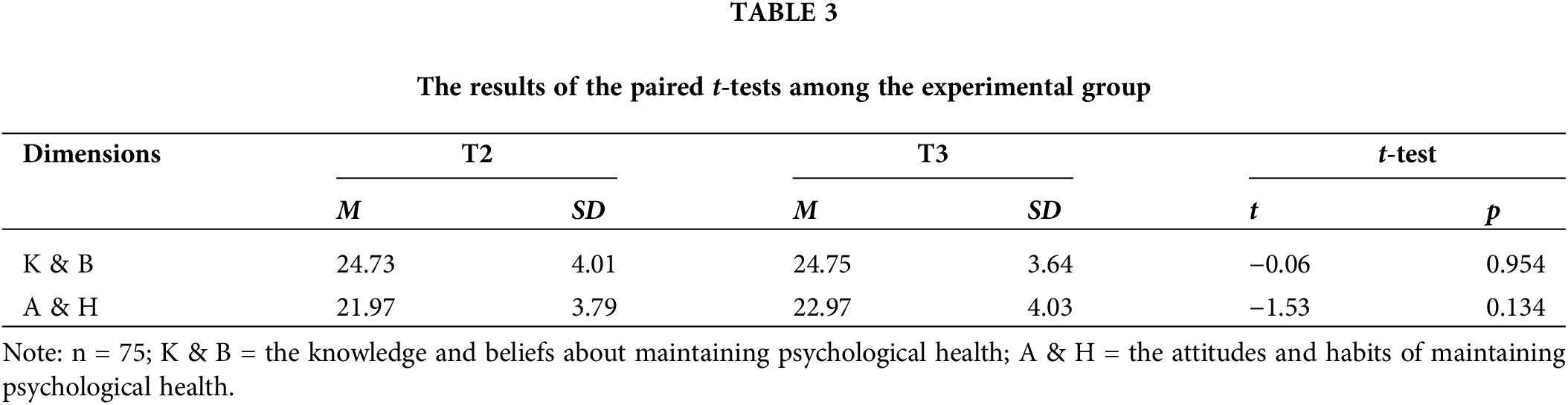
To test whether the effectiveness of the individualized online intervention had long-term stability, we contacted participants in the experimental group who reported their mental health literacy at Time 3 once again (1 month later). The results of our paired sample t-test appear in Table 3: The score of the knowledge and beliefs about maintaining psychological health at Time 3 was not significantly different from that at Time 2, t(74) = −0.06, p = 0.954, and the score of habits of the maintaining psychological health at Time 3 was also not significantly higher than that at Time 2, t(74) = −1.53, p = 0.134, d = 0.17. Thus, the effectiveness of our individualized online intervention in promoting individuals’ mental health literacy was relatively stable, not momentary.
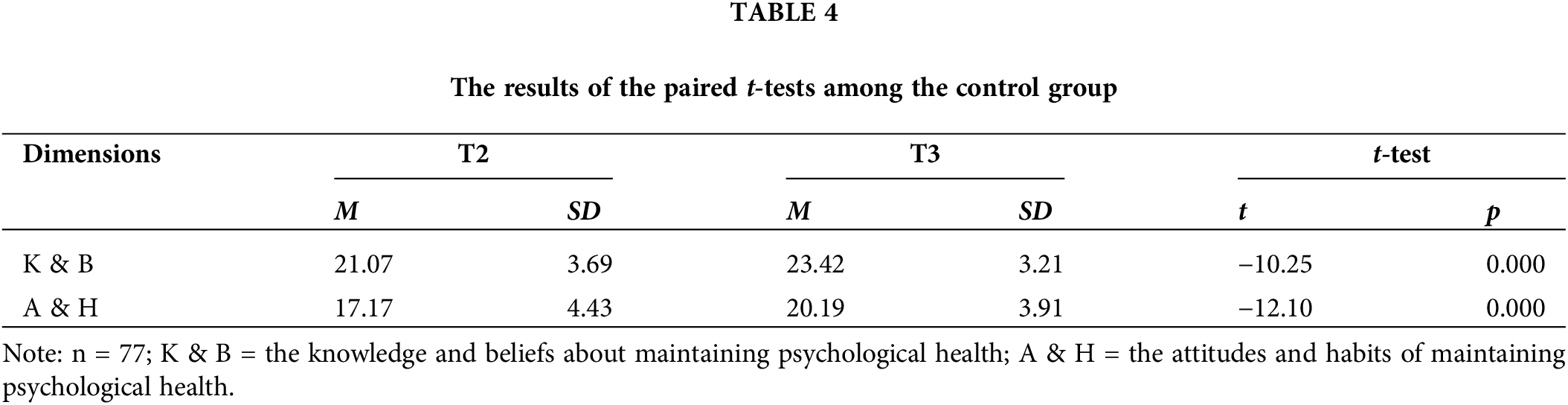
Testing the robustness of the intervention
To further test the effectiveness of the individualized online intervention, we invited the control group to experience the individualized online intervention at Time 3. The results of our paired sample t-test appear in Table 4: Scores on the knowledge and beliefs about maintaining psychological health and attitudes and habits of maintaining psychological health at Time 3 were significantly higher than those at Time 2, t(76) = −10.25, p < 0.001, d = 0.68; t(76) = −12.10, p < 0.001, d = 0.72. These results further reflect the effectiveness of our individualized online intervention in promoting individuals’ mental health literacy.
The purpose of this study was to evaluate the efficacy of individualized online intervention in improving individuals’ mental health literacy. The results from our pretest and posttest research design showed that our individualized online intervention significantly improved the participants’ levels of mental health literacy, including improved knowledge and beliefs about maintaining psychological health and improved attitudes and habits about maintaining psychological health. Specifically, we found that, compared with the control group, the two dimensions of mental health literacy in the experimental group were significantly improved after they experienced the individualized online intervention. Meanwhile, compared to that at Time 2, the mental health literacy of the control group at Time 3 also improved after receiving the individualized online intervention. Furthermore, we compared the levels of metal health literacy of the experimental group at Time 3 to those at Time 2, and found that the level of metal health literacy at Time 3 had not decreased 1 month later. Thus, the individualized online intervention was not only momentarily effective; it also had long-term efficacy.
Our research shows that the individualized online intervention can significantly improve the mental health literacy of community residents. Insights for researchers and practitioners include the following: First, this study confirmed the positive relationship between individualized online intervention and mental health literacy, filled the gap in research on the effectiveness of individualized online intervention for mental health literacy, and contributes to the field of mental health. Second, this study deepens the understanding of the themes of mental health literacy interventions. Based on interviews with 15 community residents and a survey of 311 community residents, we found that the demands for mental health literacy varied across individuals, as found in Farrer [39]. However, these demands were categorized into nine themes in the Chinese context. The results provide practitioners with a theoretical framework to rapidly and efficiently identify their clients’ demands for mental health services. Third, this study might provide government and mental health service institutions with insights into interventions for mental health literacy. In the past, methods to improve mental health literacy primarily relied on whole-of-community campaigns [16–18], educational interventions [19,20], mental health first aid training [21], and informational websites [22,23]. However, these intervention methods struggle to meet the personalized needs for improving individuals’ mental health literacy and are often constrained by resource limitations [13,40]. With the progress and development of AI technology, mental health services have increasingly become digital. In this study, we proved that the individualized online intervention can overcome time, space, and resource constraints to provide a targeted intervention based on individualized needs. More “intelligent” interventions and personalized interventions involving artificial intelligence can be developed in future research. Fourth, given the efficacy of our individualized online intervention, individuals and counselors who aim to improve their or their clients’ mental health literacy can reap benefits from using the individualized online intervention. With the rapid development of big data technology and AI, the effective resources for improving mental health are continuously expanding for individuals and counselors. For example, with the help of the individualized online intervention, individuals and counselors can conveniently obtain relevant knowledge about mental illness and how to correctly deal with or even prevent it.
Nevertheless, despite having several limitations, our research also suggests avenues for further investigation. First, as we created our individualized online intervention, we also lost some subjects from the senior age group. This was because most of the senior subjects had little experience with new media and did not know how to use them. Hence, our sample fell short of representing all groups of people, which limits the generalizability of our findings. Future studies might sample only senior residents to test the efficacy of the individualized online intervention. Second, we only assessed gender, education, and age demographics for our study; thus, we might have missed measuring some otherwise relevant variables. For instance, Hollingshead and Redlich found that socioeconomic status could influence mental health literacy [41]. We wanted to measure this in our survey, but some of our subjects were sensitive about revealing their personal income because they believed it was private information. As a result, we did not collect complete information regarding subjects’ socioeconomic status, and thus we were unable to determine how it related to their mental health literacy. Future scholars might consider surveying subjects’ socioeconomic status and including it in their research model along with gender, education, and age. Thirdly, we spent a relatively long time in collecting our pretest data because of the difficulty associated with data collection. This limited our time to implement the intervention. A future study might strictly control the duration of the data collection period during the pretest phase. Fourth, this study overall examined the effectiveness of individualized online intervention for mental health literacy, which provides evidence for supporting the efficacy of individualized online intervention based on a higher-level notion. However, it is interesting to further explore the effectiveness of different personalized learning modules for mental health literacy. For example, is a single learning module sufficient for improving mental health literacy? or is it necessary to learn a specific number of modules for such improvement?
With a continuous pretest-posttest experimental design, this study illustrates that the individualized online intervention has both great momentary and long-term effectiveness in improving community residents’ mental health literacy.
Acknowledgement: The authors thank research participants for their participation in this study.
Funding Statement: This research was funded by the National Social Science Fund Project—Research on the Construction Strategy of Community Home-Based Elderly Care Service Ecological Chain from the Perspective of Stakeholders (Grant Number, 22BSH137).
Author Contributions: The authors confirm contribution to the paper as follows: Conceptualization, Zongjun Ke, Mian Xia, and Weibo Yang; Data curation, Mian Xia, and Bingjie Hou; Formal analysis, Zongjun Ke, and Weibo Yang; Methodology, Zongjun Ke, and Mian Xia; Writing—original draft, Zongjun Ke, and Mia Xia; Writing—review & editing, Mian Xia, Weibo Yang, and Hanhui Deng. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data presented in this study are available upon request from the corresponding author.
Ethics Approval: The study was approved by the Institutional Ethics Committee at Zhongnan University of Economics and Law (IRB number: 2022012). All participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy: a survey of the public’s ability to recognize mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166(4):182–6. doi:10.5694/j.1326-5377.1997.tb140071.x. [Google Scholar] [CrossRef]
2. Rüsch N, Evans-Lacko SE, Henderson C, Flach C, Thornicroft G. Knowledge and attitudes as predictors of intentions to seek help for, and disclose, a mental illness. Psychiatr Serv. 2011;62:675–8. [Google Scholar]
3. Hee CK. Mental health literacy as a mediator on the relationship between depression and actual mental health help-seeking behaviors among university students in South Korea. Mental Health & Social Work. 2020;48(2):5–32. doi:10.24301/MHSW.2020.06.48.2.5. [Google Scholar] [CrossRef]
4. Angermeyer MC, Dietrich H. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113(3):163–79. doi:10.1111/j.1600-0447.2005.00699.x. [Google Scholar] [PubMed] [CrossRef]
5. Furnham A, Swami V. Mental health literacy: a review of what it is and why it matters. Int Persp Psychol. 2018;7(4):240–57. doi:10.1037/ipp0000094. [Google Scholar] [CrossRef]
6. Jorm A. Why do we need the concept of “Mental Health Literacy”. Health Commun. 2015;30(12):1166–8. doi:10.1080/10410236.2015.1037423. [Google Scholar] [PubMed] [CrossRef]
7. Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67(3):231–43. doi:10.1037/a0025957. [Google Scholar] [PubMed] [CrossRef]
8. Kutcher S, Wei Y, Coniglio C. Mental health literacy: past, present and future. Can J Psychiatry. 2016;61(3):1540158. doi:10.1177/0706743715616609. [Google Scholar] [PubMed] [CrossRef]
9. Zhang Z, Chen S, Wang X, Liu J, Zhang Y, Mei Y, et al. The relationship between mental health literacy and subjective well-being of young and middle-aged residents: perceived the mediating role of social support and its urban-rural differences. Int J Ment Health Promot. 2023;25(4):471–83. doi:10.32604/ijmhp.2022.024918. [Google Scholar] [CrossRef]
10. Kodama S, Shido K, Ikeda N. Development of mental health literacy scale for depression affecting the help-seeking process in health professional students. Int J Ment Health Promot. 2021;23(3):331–52. doi:10.32604/IJMHP.2021.016337. [Google Scholar] [CrossRef]
11. Zhou C, Yue XD, Zhang X, Shangguan F, Zhang XY. Self-efficacy and mental health problems during COVID-19 pandemic: a multiple mediation model based on the health belief model. Pers Individ Dif. 2021;179(2):110893. doi:10.1016/j.paid.2021.110893. [Google Scholar] [PubMed] [CrossRef]
12. Jafari A, Nejatian M, Momeniyan V, Barsalani FR, Tehrani H, et al. Mental health literacy and quality of life in Iran: a cross-sectional study. BMC Psychiat. 2021;21(1):499. doi:10.1186/s12888-021-03507-5. [Google Scholar] [PubMed] [CrossRef]
13. Jeong YW, Kim JH, Park HK. Study on the relationship between mental health literacy and psychological symptoms of university students: mediating effect of grit. Int J Ment Health Promot. 2023;25(7):813–21. doi:10.32604/ijmhp.2023.027383. [Google Scholar] [CrossRef]
14. Ethan M, Patricia F. The impact of the campus climate and mental health literacy on students’ well-being. J Ment Health Train, Educ Pract. 2021;16(3):245–56. doi:10.1108/JMHTEP-12-2020-0088. [Google Scholar] [CrossRef]
15. Tan CH, Koo AC, Rahmat H, Siew WF, Cheang AWO, Sharji EA. Workplace wellness, mental health literacy, and usage intention of e-mental health amongst digital workers during the COVID-19 pandemic. Int J Ment Health Promot. 2023;25(1):99–126. doi:10.32604/ijmhp.2022.025004. [Google Scholar] [CrossRef]
16. Dumesnil H, Verger P. Public awareness campaigns about depression and suicide: a review. Psychiatr Serv. 2009;60(9):1203–13. doi:10.1176/ps.2009.60.9.1203. [Google Scholar] [PubMed] [CrossRef]
17. Dietrich S, Mergl R, Freudenberg P, Althaus D, Hegerl U. Impact of a campaign on the public’s attitudes towards depression. Health Educ Res. 2010;25(1):135–50. doi:10.1093/her/cyp050. [Google Scholar] [PubMed] [CrossRef]
18. Joa I, Johannessen JO, Auestad B, Friis S, McGlashan T, Melle I, et al. The key to reducing duration of untreated first psychosis: information campaigns. Schizophr Bull. 2008;34(3):466–72. doi:10.1093/schbul/sbm095. [Google Scholar] [PubMed] [CrossRef]
19. Esters IG, Cooker PG, Ittenbach RF. Effects of a unit of instruction in mental health on rural adolescents’ conceptions of mental illness and attitudes about seeking help. Adolescence. 1998;33(130):469–76. [Google Scholar] [PubMed]
20. Pinto-Foltz MD, Logsdon MC, Myers JA. Feasibility, acceptability, and initial efficacy of a knowledge-contact program to reduce mental illness stigma and improve mental health literacy in adolescents. Soc Sci Med. 2011;72(12):2011–9. doi:10.1016/j.socscimed.2011.04.006. [Google Scholar] [PubMed] [CrossRef]
21. Kitchener BA, Jorm AF. Mental health first aid: an international programme for early intervention. Early Interv Psychiatry. 2008;2(1):55–61. doi:10.1111/j.1751-7893.2007.00056.x. [Google Scholar] [PubMed] [CrossRef]
22. Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. BMJ: Brit Med J. 2004;328(7434):265–9. doi:10.1136/bmj.37945.566632.EE. [Google Scholar] [PubMed] [CrossRef]
23. Mackinnon A, Griffiths KM, Christensen H. Comparative randomised trial of online cognitive-behavioral therapy and an information website for depression: 12-month outcomes. Brit J Psychiatry. 2008;192(2):130–4. doi:10.1192/bjp.bp.106.032078. [Google Scholar] [PubMed] [CrossRef]
24. D’Alfonso S. AI in mental health. Curr Opin Psychol. 2020;36:112–7. doi:10.1016/j.copsyc.2020.04.005. [Google Scholar] [PubMed] [CrossRef]
25. Graham S, Depp C, Lee EE, Nebeker C, Tu X, Kim HC, et al. Artificial intelligence for mental health and mental illnesses: an overview. Curr Psychiatry Rep. 2019;21(11):1–18. doi:10.1007/s11920-019-1094-0. [Google Scholar] [PubMed] [CrossRef]
26. Ren P, Wang Y, Liu D, Li T, Luo F. Intelligent application of mental health assessment and intervention. J Beijing Normal Univ: Soc Sci Ed. 2022;(4):150–60 (In Chinese). [Google Scholar]
27. Lee EE, Torous J, De Choudhury M, Depp CA, Graham SA, Kim HC, et al. Artificial intelligence for mental health care: clinical applications, barriers, facilitators, and artificial wisdom. Biol Psychiatry: Cogn Neurosci Neuroimaging. 2021;6(9):856–64. doi:10.1016/j.bpsc.2021.02.001. [Google Scholar] [PubMed] [CrossRef]
28. Fulmer R, Joerin A, Gentile B, Lakerink L, Rauws M. Using psychological artificial intelligence (Tess) to relieve symptoms of depression and anxiety: randomized controlled trial. JMIR Ment Health. 2018;5(4):e64. doi:10.2196/mental.9782. [Google Scholar] [PubMed] [CrossRef]
29. Zhou S, Zhao J, Zhang L. Application of artificial intelligence on psychological interventions and diagnosis: an overview. Front Psychiat. 2022;13:811665. doi:10.3389/fpsyt.2022.811665. [Google Scholar] [PubMed] [CrossRef]
30. Wang Y, Shi J. Internet use and mental health among older adults in China: beneficial for those who lack of intergenerational emotional support or suffering from chronic diseases? Int J Ment Health Promot. 2024;26(1):69–80. doi:10.32604/ijmhp.2023.044641. [Google Scholar] [CrossRef]
31. Reupert A, Bartholomew C, Cuff R, Foster K, Matar J, Maybery DJ, et al. An online intervention to promote mental health and well-being for young adults whose parents have mental illness and/or substance use problems: theoretical basis and intervention description. Front Psychiat. 2019;10:59. doi:10.3389/fpsyt.2019.00059. [Google Scholar] [PubMed] [CrossRef]
32. Fu Z, Burger H, Arjadi R, Bockting CL. Effectiveness of digital psychological interventions for mental health problems in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Psychiat. 2020;7(10):851–64. doi:10.1016/S2215-0366(20)30256-X. [Google Scholar] [PubMed] [CrossRef]
33. Feijt M, De Kort Y, Bongers I, Bierbooms J, Westerink J, IJsselsteijn W. Mental health care goes online: practitioners’ experiences of providing mental health care during the COVID-19 pandemic. Cyberpsychol, Behavior, Soc Netw. 2020;23(12):860–4. doi:10.1089/cyber.2020.0370. [Google Scholar] [PubMed] [CrossRef]
34. Valente TW. Network interventions. Science. 2012;337(6090):49–53. doi:10.1126/science.1217330. [Google Scholar] [PubMed] [CrossRef]
35. Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust. 2007;187(S7):S26–30. doi:10.5694/j.1326-5377.2007.tb01332.x. [Google Scholar] [PubMed] [CrossRef]
36. Dugard P, Todman J. Analysis of pre-test-post-test control group designs in educational research. Educ Psychol. 1995;15(2):181–98. doi:10.1080/0144341950150207. [Google Scholar] [CrossRef]
37. Wu J, Zhu X, Li YQ, Liu GD, Zhang LK, Zhang Y, et al. Compilation of national mental health literacy questionnaire. In: The 21st Chinese psychological society abstract collection. Beijing, China; 2020. [Google Scholar]
38. Bernerth JB, Aguinis H. A critical review and best-practice recommendations for control variable usage. Pers Psychol. 2016;69(1):229–83. doi:10.1111/peps.12103. [Google Scholar] [CrossRef]
39. Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: evidence from a national US survey conducted in march 2020. J Gerontol: Series B. 2021;76(2):e24–9. doi:10.1093/geronb/gbaa074. [Google Scholar] [PubMed] [CrossRef]
40. Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiat. 2017;16(3):287–98. doi:10.1002/wps.20472. [Google Scholar] [PubMed] [CrossRef]
41. Hollingshead AB, Redlich FC. Social class and mental illness: a community study. Am J Public Health. 2007;97(10):1756–7. doi:10.2105/ajph.97.10.1756. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools