 Open Access
Open Access
REVIEW
The Effectiveness of Psychotherapy on Posttraumatic Stress Disorder in Soldier: A Systematic Review
School of Physical Education, Central China Normal University, Wuhan, 430079, China
* Corresponding Author: Bin Wang. Email:
International Journal of Mental Health Promotion 2024, 26(7), 499-516. https://doi.org/10.32604/ijmhp.2024.052309
Received 29 March 2024; Accepted 16 May 2024; Issue published 30 July 2024
Abstract
The objective of this systematic review is to examine the effectiveness of psychotherapy in treating Post-Traumatic Stress Disorder (PTSD) in military personnel. PubMed, Web of Science, The Cochrane Library, EBSCO and CNKI databases were searched from 1 January, 2000 to November 2022 for Randomized Controlled Trials (RCTs) on psychotherapeutic interventions for military PTSD. The physical Therapy Evidence Database (PEDro) scale was used to evaluate the quality of the literature. Two researchers conducted literature screening, data extraction, and risk bias assessment in accordance with inclusion and exclusion criteria. Ultimately, 49 RCTs were included, involving a total of 5073 veterans, retired and active military from four countries. The average score on the PEDro scale was 7.60. The primary psychotherapeutic modalities for military PTSD intervention include Cognitive-Behavioral Therapy, Exposure Therapy, Mindfulness interventions, psychotherapy based on new technological tools, and other emerging psychotherapeutic tools. The review highlights that Cognitive Processing Therapy (CPT) and Prolonged Exposure Therapy (PET) stand out as the primary psychotherapeutic modalities for treating PTSD in military personnel. In cases where CPT and PET yield limited benefits, Mindfulness interventions emerge as effective alternatives. Moreover, considering the diverse needs and high dropout rates in the military, population, the review suggests using web-based, computer, and virtual reality technology tools as supplements to first-line treatments (CPT/PET) to enhance overall intervention effectiveness. For the advancement of future psychotherapeutic initiatives, there is a pronounced emphasis on prioritizing proven first-line interventions, CPT and PET while also recognizing the potential of mindfulness-based interventions as credible alternatives. In tandem with this, the active integration of technological tools is advocated to amplify the therapeutic impact of conventional psychological treatment modalities.Keywords
Supplementary Material
Supplementary Material FilePost-Traumatic Stress Disorder (PTSD) is a debilitating psychological condition that arises after a single or a series of traumatic events, such as war, terrorism, abuse, or rape. Approximately 6.8% of individuals affected by PTSD are prone to lifelong psychopathy [1]. The prevalence of PTSD is notably high in special groups like police, nurse personnel, firefighters and soldier, with the veterans exhibiting the highest prevalence rate at 23% [2]. About 13% veterans experienced PTSD after Iraq or Afghanistan wars, 10% after Gulf War, and 11% after the Vietnam War, with symptoms persisting up to 40 years post-war [3–5]. In 2012, over 500,000 veterans in the US sought treatment for PTSD, but the outcomes were not promising despite the considerable cost of treatment [6]. Risk factors for PTSD in the military population include exposure to war zones, injuries, younger age at deployment, lower education, more childhood trauma, and reduced social support both during and after deployment [7]. Military-related PTSD often coexists with mental and physical health issues, notably depression, anxiety, and substance abuse [8], posing a gradual and potentially lifelong challenge if left untreated [9]. Currently, regional conflicts and localized wars are frequent, posing serious challenges to the mental health of military personnel. Especially post-war, the issue of post-traumatic stress disorder (PTSD) among military personnel is becoming increasingly prominent and has become a public health issue that cannot be ignored [10].
Psychological interventions have been widely recommended for treating PTSD, with growing number of randomized clinical trials (RCTs) report positive outcomes in the treatment of PTSD among military populations. Compared to pharmacological treatment, psychotherapy circumvents the potential side effects of medication, such as dependency and withdrawal symptoms [11], which is essential for military personnel who need to maintain physical and mental alertness. Moreover, it facilitates cognitive and emotional processing of trauma, bolsters coping skills among military individuals [12], and aids in more effective management of PTSD symptoms. Furthermore, psychotherapy contributes to the preservation of military operational capabilities [13], enhances treatment acceptance [14], and ameliorates social and familial functioning [15]—areas often overlooked by pharmacological interventions. Concurrently, the US Department of Defense and the Department of Veterans Affairs have shifted the focus of PTSD treatment for veterans towards evidence-based approaches [16], In both clinical guidelines and actual treatment by these departments, psychotherapy consistently emerges as the primary recommended approach over medication for treating PTSD [16]. Cognitive therapy (CT) [17], exposure therapy [18], and mindfulness meditation [19] have been demonstrated to effectively assist military personnel in managing post-traumatic emotional distress, reducing symptoms such as anxiety, depression, and avoidant behavior. However, existing research on psychological treatments for PTSD in military populations often struggles to draw robust conclusions due to a weak evidentiary foundation, highlighting the need for a systematic review and integrated discussion of these therapeutic approaches [20]. Moreover, with the emergence of novel treatment modalities, it becomes increasingly important to compare traditional and innovative methods, evaluating their efficacy and suitability in the treatment of military-related PTSD [21]. Current psychological treatment research for civilian PTSD faces numerous challenges, including methodological constraints, therapist-related factors [22], and the absence of standardized treatment protocols [23]. These issues may manifest more complexly within the specialized group of military personnel.
It is necessary to conduct a systematic review on the effectiveness of psychological treatment interventions for PTSD in military personnel. This review will assess the efficacy and acceptability of various psychological treatments for military PTSD, providing clinical practice with robust evidence to better guide the intervention and treatment of PTSD in military populations.
The review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [24]. A hybrid approach involving both subject and free word searches was employed in this study. Source databases such as PubMed, Web of Science, The Cochrane Library, EBSCO, and CNKI were extensively utilized. The search spanned from 1 January, 2000 to 31 December, 2022 to capture a comprehensive range of literature. Furthermore, to expand our pool of pertinent literature, reference tracing of review articles was conducted. The detailed search strategy is delineated in Box 1:
BOX 1
Web of science search strategy
#1: military* OR soldier* OR serviceman* OR veteran*
#2: (post-trauma* OR post trauma*) OR PTSD AND (stress OR disorder)
#3: (psychotherapy* OR therapy* OR exposure* OR CBT OR psychodynamic* OR psychoeducation* OR eye movement desensitization and reprocessing OR eye movement desensitization and reprocessing OR EMDR OR narrative exposure OR NET OR trauma-focused* OR trauma-focused OR prolonged exposure OR cognitive processing OR cognitive therapy OR CT OR non-trauma-focused* OR non-trauma focused OR present-centered* OR present-centered OR mindfulness OR relaxation* OR supportive counselling OR supportive counseling OR counselling OR counseling OR brief eclectic therapy OR BET OR)
#4: randomized controlled trial* OR RCT*
#5: #1 AND #2 AND #3 AND #4
Inclusion and exclusion criteria
Inclusion criteria: 1) Study subjects: military group with PTSD (ex-military, veterans, or active military). 2) Intervention measures: Experimental groups treated with psychotherapy intervention, and control groups treated with no intervention, waitlist, psychoeducational or treatment as usual (TAU). 3) Study topic: Studies on Psychological Treatment Approaches for PTSD Intervention in Military Personnel. 4) Research design: randomized controlled trials (RCTs).
Exclusion criteria: 1) Studies with drug intervention or non-psychological intervention in both the experimental and control groups. 2) Studies with a primary outcome that is not a PTSD indicator or an outcome after a PTSD-free intervention. 3) Studies where the outcome indicator is not a professional PTSD evaluation scale (CAPS/PCL/PSS-I). 4) Studies with experimental designs that are not RCTs. 5) Exclusion of repeated published studies, general reviews, or unpublished papers (including conference abstracts, doctoral papers, etc.). 6) Category review, systematic review or Meta-analysis. 7) Literature published before the year 2000.
Literature screening and data extraction
The included studies underwent categorization, and data extraction was independently conducted by two researchers following the proposed scheme. If there is a disagreement, it should be discussed and negotiated with another researcher. He extracted data encompassed details such as the first author, country, year of publication, sample size/loss of follow-up, subject information (gender, age, veteran/in-service status, etc.), intervention/control specifics (period of intervention, duration of follow-up), outcome indicators, and more. The retrieved literature underwent an initial sequential screening based on title and abstract. Subsequently, literature not aligning with the study criteria was excluded by reading the full text in accordance with the predefined inclusion and exclusion criteria. The systematic review was conducted according to PRISMA guidelines (Supplementary Checklist). The process and results of the literature screening are shown in Fig. 1.
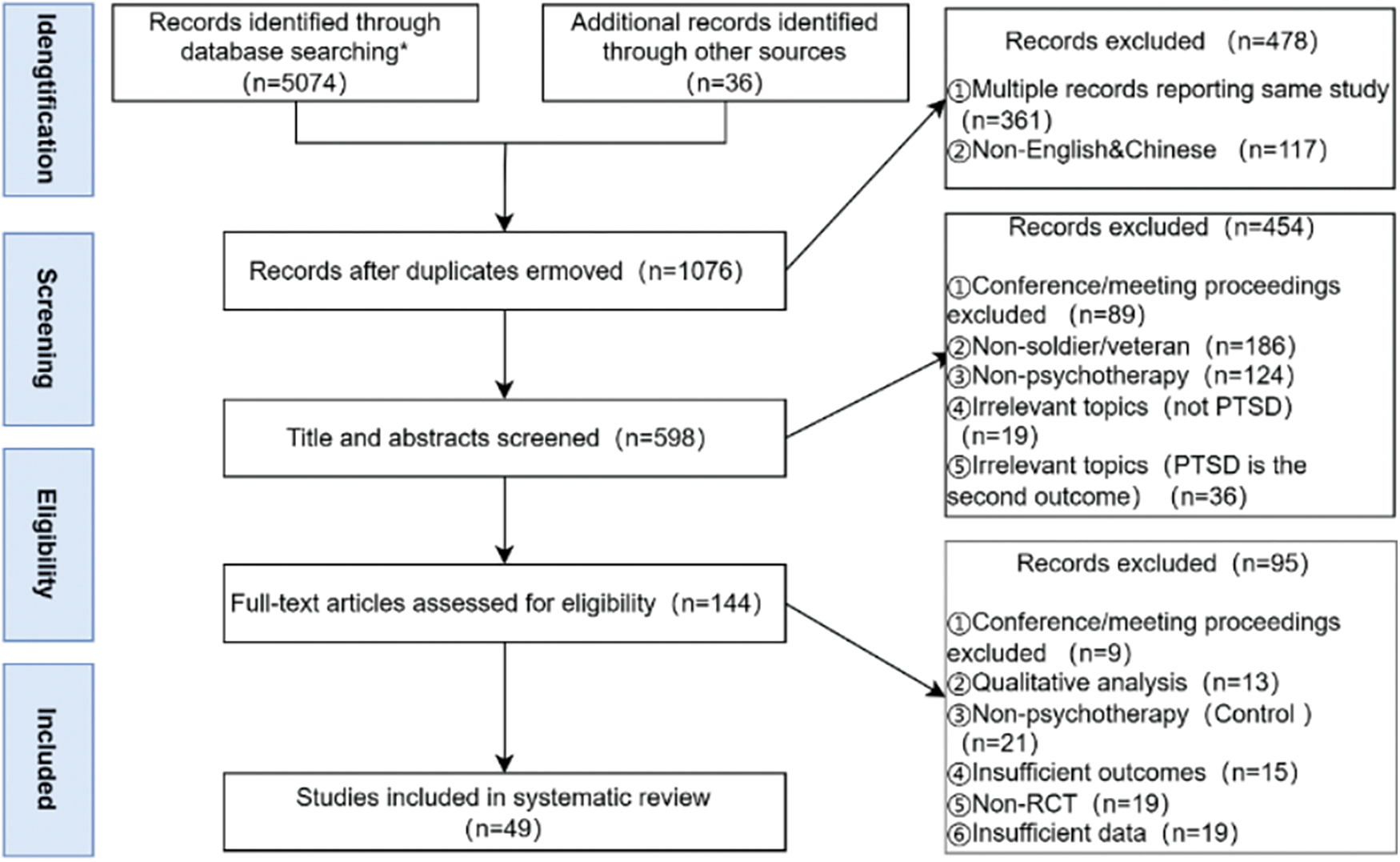
Figure 1: Flow diagram of the literature search. *Results of specific searches of literature in each database were PubMed (n = 1282), EBSCO (n = 927), The Cochrane Library (n = 659), Web of Science (n = 1668), CNKI (n = 538); RCT: randomized controlled trial.
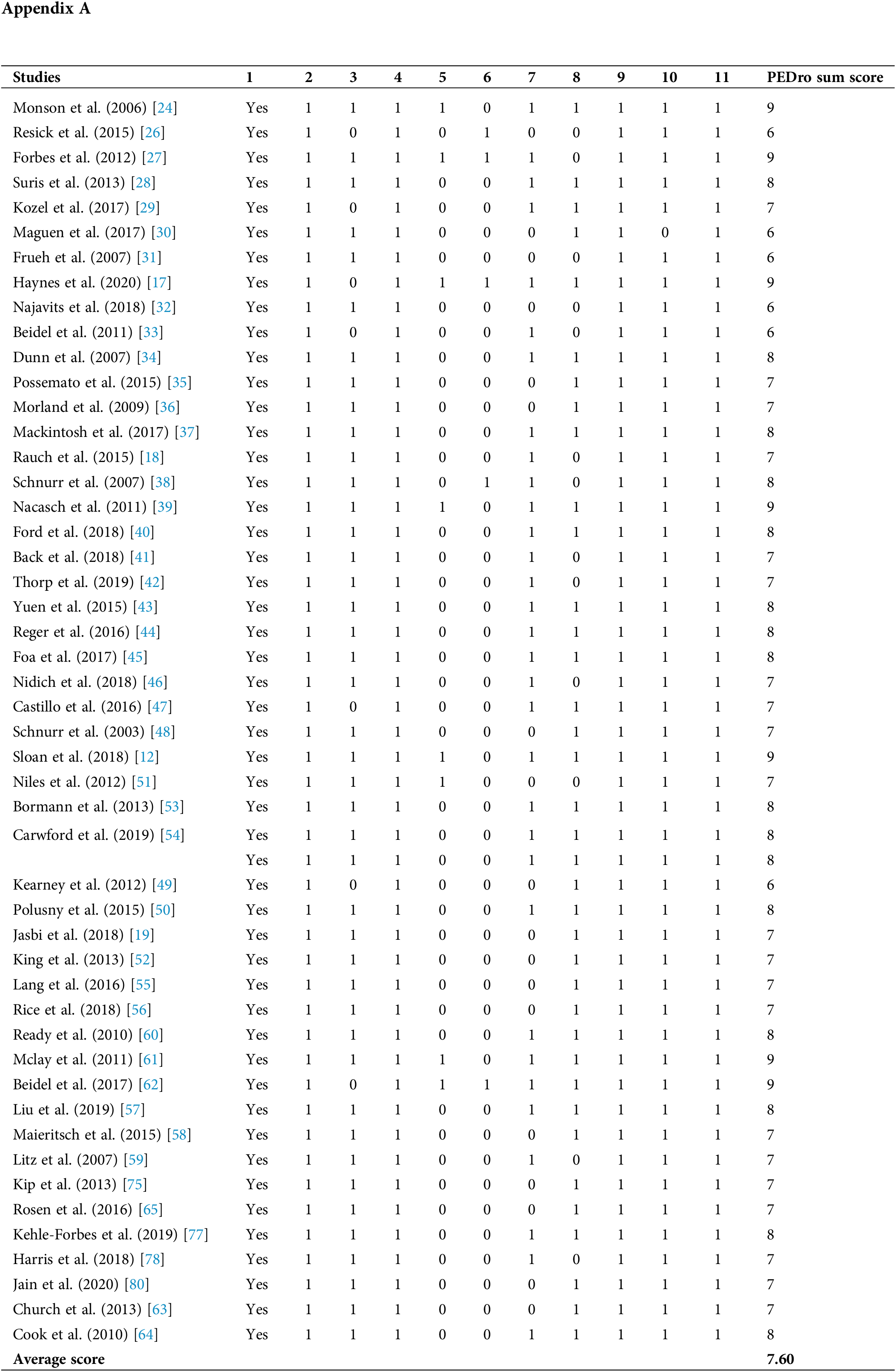
Quality assessment of included literature
The Physiotherapy Evidence Database (PEDro) served as the tool for methodological quality assessment, featuring 11 items where items 2–11 were scored, with a maximum score of 10 points. Classification criteria were set at ≥6 for high quality, 4–5 for average quality, and <4 for low quality. Two researchers independently conducted the literature quality evaluation, and any discrepancies were resolved through discussion and negotiation with a third researcher. Quality assessment was performed for the 49 papers included in the systematic review, revealing an average literature quality score of 7.60. This score suggests that the overall quality of the included literature was generally high, as outlined in Table 1.
Characteristics of the included literature
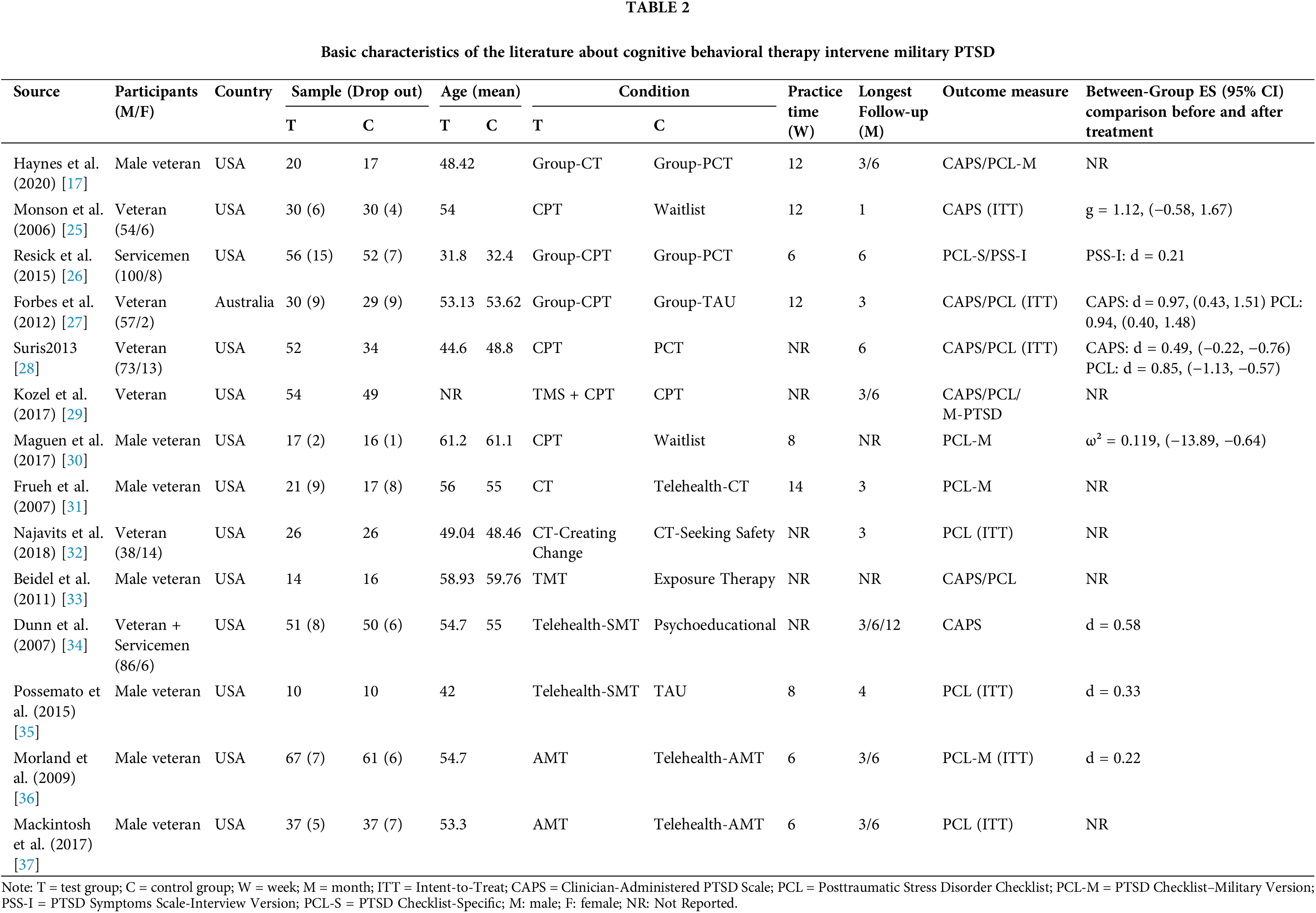
The systematic review incorporated 49 randomized controlled trials focusing on psychotherapeutic interventions for PTSD in military groups. The majority of these trials were conducted in the United States, with a few originating from other countries, including Australia, Iran, and Lebanon. The study involved 5073 participants comprising veterans, retired, and active-duty military individuals, with a mean age range spanning from 30.93–66.51. The trials encompassed diverse research fields, including rehabilitation psychology, military psychology, cognitive psychology, and others (Tables 2–6).
Psychological intervention program
In this studies, the primary psychological intervention programs comprised Cognitive Behavioral Therapy (CBT), Exposure Therapy (ET), and Mindfulness intervention. Additionally, there is a notable presence of treatments that leverage the internet, computer technology, and virtual reality, complemented by a range of innovative psychological therapies that are emerging in the field.
Cognitive Behavioral Therapy (Table 2) includes Cognitive Processing Therapy (CPT) [25–30], such as Group-CPT [26,27] and CPT combined with Transcranial Magnetic Stimulation (TMS) intervention [29]. Furthermore, there are also the Cognitive Therapy [17,31,32], Trauma Management Therapy (TMT) [33], Self-management Therapy (SMT) [34,35], and Angry Management Therapy (AMT) [36,37].
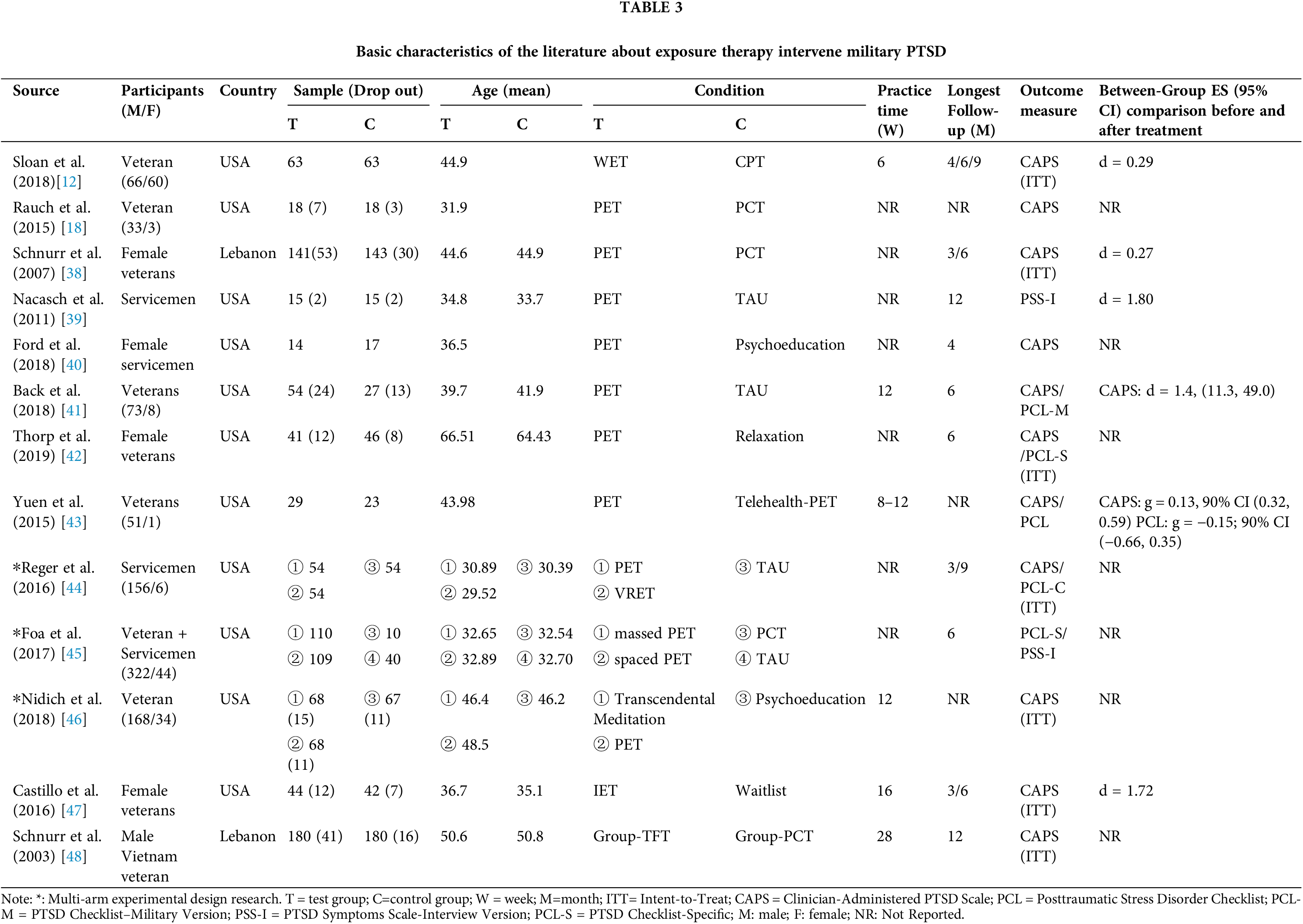
Exposure Therapies (Table 3) involve Prolonged Exposure Therapy (PET) [18,38–46], Written Exposure Therapy (WET) [12], Imagery Exposure Therapy (IET) [47], and Trauma-Focused group Therapy (TEGT) [48]. Notably, two studies were 3-arm RCTs [44,46], that not only compare the effectiveness of exposure therapy with that of the control group but also further explore its comparative effectiveness with mindfulness and virtual reality exposure interventions. Another 4-arm RCT [45] explored the contrasting effects between massively prolonged and spaced prolonged exposures.
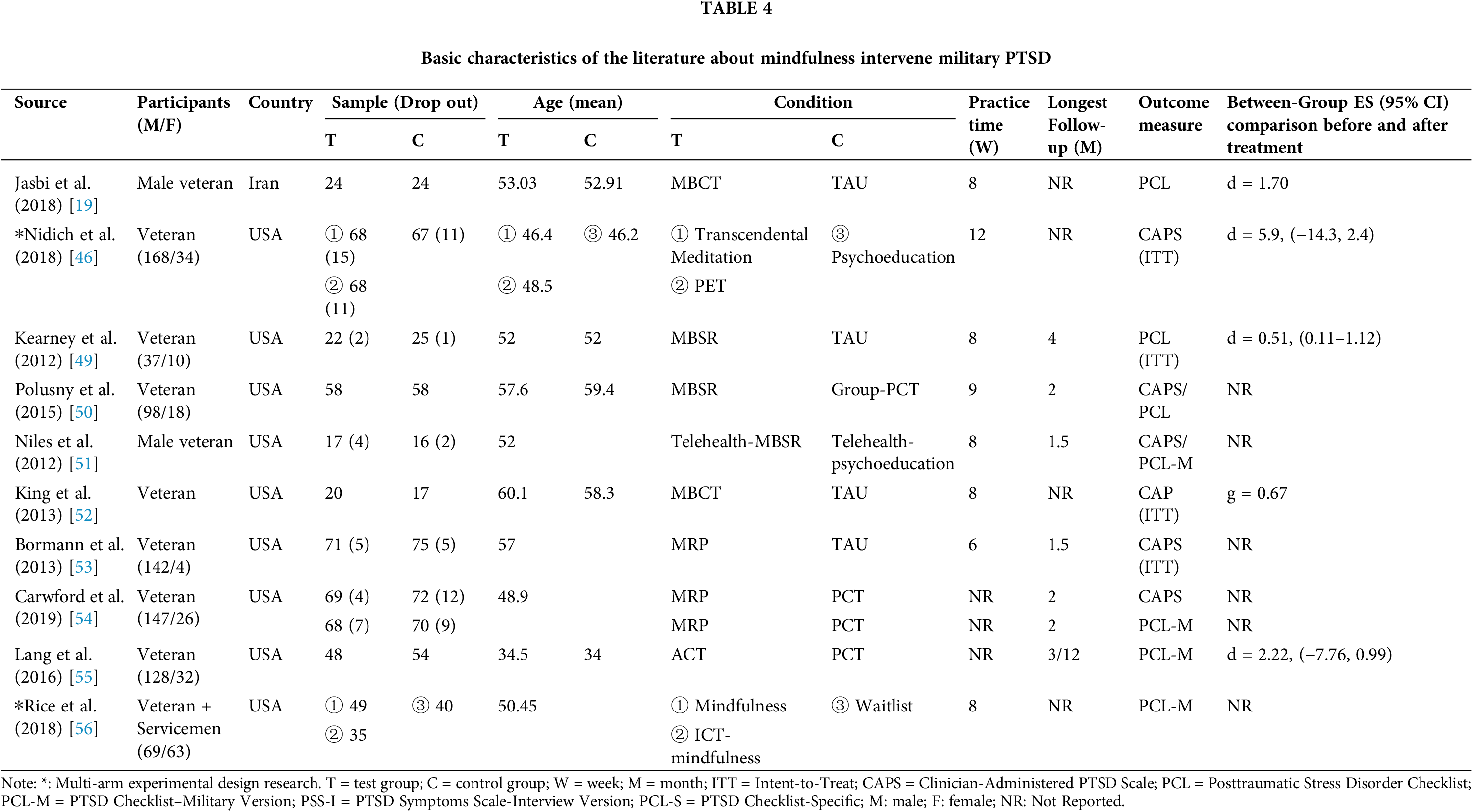
Mindfulness intervention (Table 4) includes Mindfulness-Based Stress Reduction (MBSR) and Telehealth MBSR [49–51] Mindfulness-Based Cognitive Therapy (MBCT) [19,52], Transcendental meditation (TM) [46], Mantram Repetition Program (MRP) [53,54], and Acceptance and commitment therapy (ACT) [55]. Two of these 3-arm RCTs [46,56] compared Mindfulness intervention with web-based Mindfulness and PET, respectively.
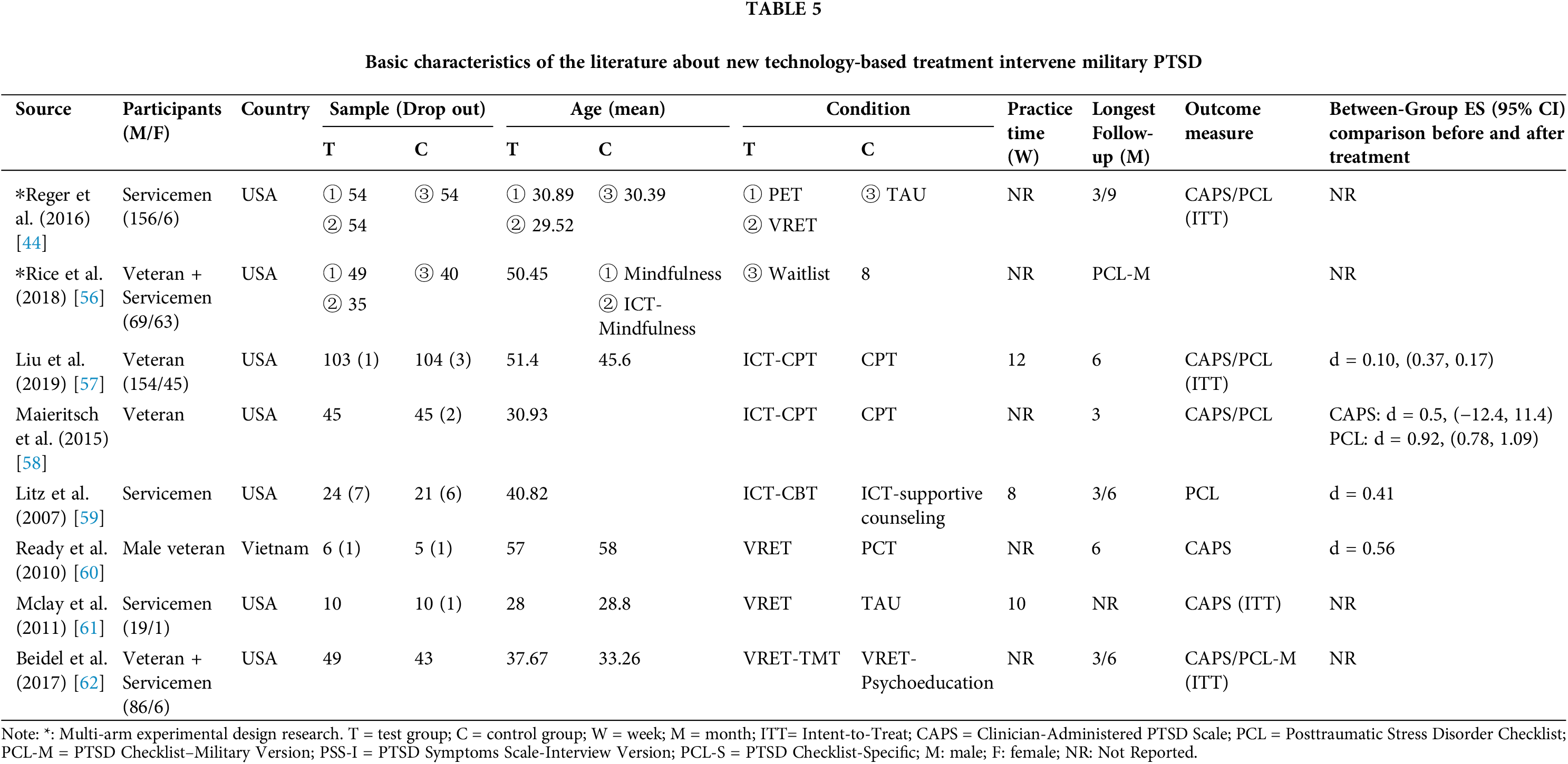
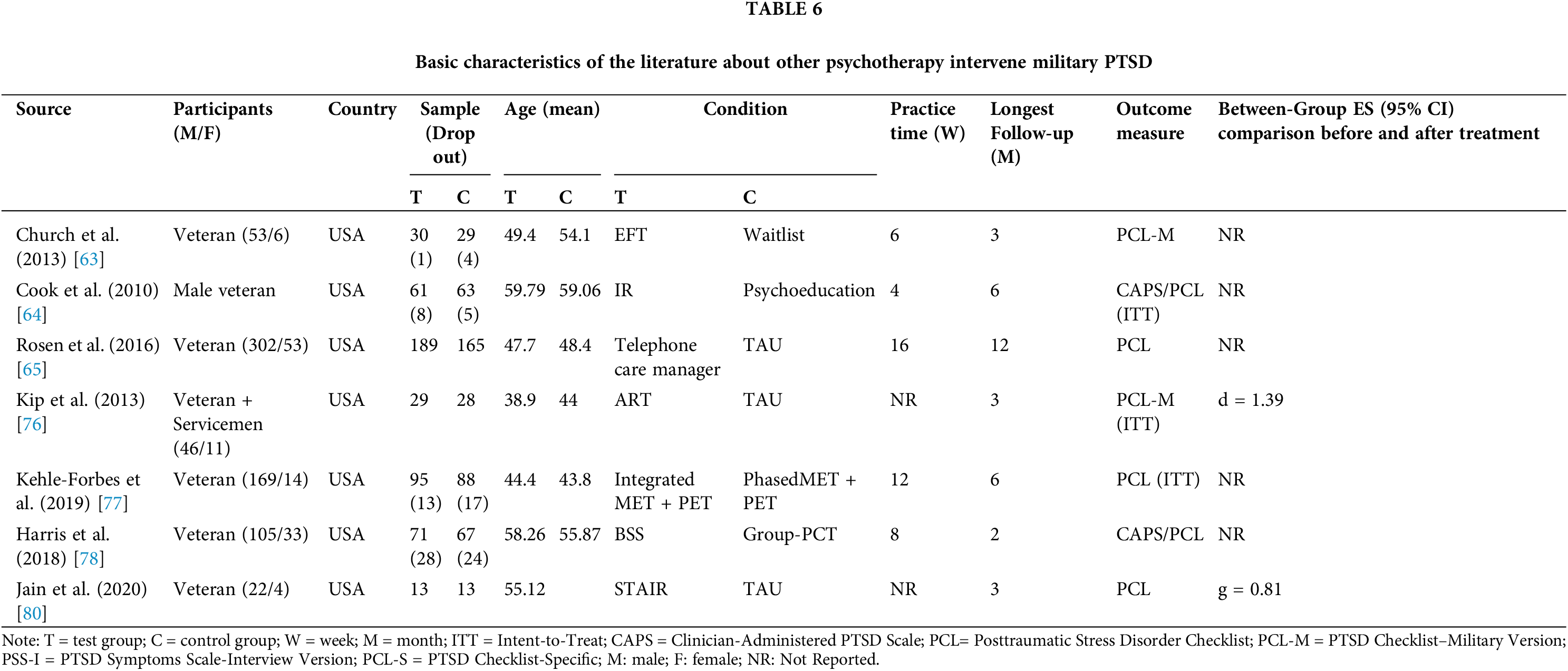
New technology-based treatments (Table 5) encompass Internet and Computer-based Treatment (ICT) modalities [56–59] and Virtual-Reality Exposure therapy (VRET) utilizing real-time computer graphics and head-mounted visual displays for intervention [44,60–62]. And the other psychotherapy (Table 6) included Emotional Freedom Techniques (EFT) [63], which combines Eastern meridian acupressure and Western psychology’s energy therapy, Imagery Rescripting (IR) [64], Telephone Care Management (TCM) [65], among others.
The control groups in the literature included Waitlist, Treatment as Usual, Present Centered Therapy (PCT), Relaxation, Psychoeducational, Supportive Counseling, and other comparative studies between different psychotherapies.
This paper includes six studies on Cognitive Processing Therapy interventions for PTSD in military personnel [25–30], encompassing 416 veterans and active-duty military personnel. CPT focuses on the interconnectedness of thoughts, feelings, behavior, and physical sensations, highlighting the significance and impact of traumatic experiences on individuals. Actively reviewing and processing traumatic events to address hindering mindsets is a crucial aspect of treatment. Widely used in the United States Departments of Defense and Veterans Affairs [66], CPT has proven beneficial in treating PTSD in military personnel when compared to control groups (waitlist/TAU/PCT) [25–28,30]. However, high dropout rates and a proportion of patients not benefiting significantly have prompted scholars to analyze CPT further.
Two studies [26,27] explored the efficacy of group-CPT interventions, revealing significant reductions in PTSD symptoms that persisted a year later. However, concerns arose as half of the patients still experienced distress. While group therapy may be beneficial, individual therapy was provided for those not showing improvement in group settings. Another study [29] examined the effectiveness of a comprehensive intervention (TMS + CPT) and found a more significant effect than CPT alone, with efficacy lasting up to six months post-treatment. This suggests a potential new psychological approach, though further clinical evidence is needed for validation.
Three studies focusing on the application of Cognitive Therapy interventions to address Post-Traumatic Stress Disorder (PTSD) within the military personnel population [17,31,32]. CT helps patients identify and change negative thoughts and beliefs, thus altering emotions and behaviors. A comparison of telehealth-CT [31] revealed no significant differences in clinical outcomes or dropout rates after three months. Another study [17] compared group-CT and group-PCT, showing no significant difference in treatment effectiveness, but a higher attendance rate in the group-CT, suggesting that group treatment may improve veteran participation in PTSD interventions. One study [32] evaluated the effectiveness of two CT interventions in veterans (Creating Change and Seeking Safety) and found no significant difference in their effectiveness on PTSD.
Beidel et al. conducted a comparative analysis of Trauma Management Therapy and Exposure Therapy (ET) [33], revealing that while ET proves effective in addressing the core symptoms of PTSD, TMT has shown a more pronounced enhancement in social participation and interpersonal functioning. TMT, a multicomponent behavioral treatment, involves individualized imaginal and in vivo exposure therapy followed by group social skills training.
The paper includes two randomized controlled trials [34,35] that utilize an app (PTSD Coach) for self-management interventions for PTSD. Self-Management Therapy is facilitated by a mobile application called PTSD Coach, which empowers patients to engage in self-directed management. This application is specifically designed to aid individuals suffering from Post-Traumatic Stress Disorder (PTSD) in enhancing their self-awareness and equipping them with the tools for more effective self-management [67]. Both studies indicate that there is no difference in symptoms and functioning among military personnel with PTSD after undergoing Self-management Therapy interventions with the assistance of the mobile PTSD Coach app. Despite the promising intervention outcomes of SMT in other populations [68], this review did not yield significant results regarding the efficacy of SMT interventions for military personnel suffering from Post-Traumatic Stress Disorder (PTSD).
Two randomized controlled trials investigated interventions with male veterans using Anger Management Treatment (AMT) vs. tele-AMT [36,37], highlighting the effectiveness and feasibility of remotely delivered cognitive-behavioral group therapy for PTSD-related anger issues. Tele-therapy demonstrated increased accessibility, reduced therapist workload, decreased treatment costs, and shortened practice time.
The study incorporates ten randomized controlled trials focusing on Prolonged Exposure Therapy interventions for PTSD in veterans [18,38–46]. PET, a trauma-focused cognitive-behavioral therapy developed by Foa et al. [69], is standardized for PTSD and draws on exposure therapies for anxiety disorders.
In comparisons with control groups (PCT\TAU\Relaxation\Psychoeducation) [18,38–42], PET significantly reduced PTSD symptoms in veterans. The intervention targets included regular veterans [18,42], female veterans [38], active-duty military personnel [39,40], and veterans with PTSD who also suffer from substance use disorders [41]. It is also pointed out that the effectiveness of PET intervention for PTSD patients among active military personnel has been sustained up to the follow-up at four months [40]. However, for PTSD intervention among veterans, the effects of PET disappeared at the six-month follow-up [42], and the long-term benefits of the treatment still require further verification. Moreover, compared to the control group, the dropout rate among patients undergoing PET intervention for military PTSD was higher [18,38,40,41]. In comparison with tele-PET [43], which is comparable to PET in terms of intervention effectiveness and process satisfaction, tele-PET effectively intervenes in veterans with PTSD. In a 4-arm RCT with active-duty military patients, mass PET (10 sessions/2 weeks) demonstrated greater reduction in PTSD symptoms compared to controls (PCT) and was comparable to the intervention effect of spaced PET (10 sessions/8 weeks). Interestingly, there was no significant difference between spaced PET and controls (PCT) [45]. There were also two three-arm studies [44,46], one of which compared PET with Virtual Reality Exposure Therapy (VRET) [44]. The results were contrary to the study hypothesis, with no significant differences between the PET and VRET groups in terms of statistical significance, and VRET was not found to be superior to PET. At the 3-month and 6-month follow-up assessments, the PET group showed greater improvement in the reduction of PTSD symptoms compared to the VRET group. Another study compared PET with Transcendental Meditation [46], and in terms of reducing the severity of PTSD symptoms, TM was proven to be equally effective as PET. TM was significantly non-inferior to PET in the change in Clinician-Administered PTSD Scale (CAPS) scores from baseline to the 3-month follow-up test.
In 2018, Sloan et al. [12] conducted a comparative efficacy study of Written Exposure Therapy and Cognitive Processing Therapy for treating PTSD among veterans. Their findings indicated that WET was equally effective in mitigating PTSD’s symptomatology as CPT, even with a condensed treatment schedule. Furthermore, Imagery Exposure Therapy, which involves the systematic and repetitive exposure to traumatic imagery within a secure environment, demonstrated statistical significance in treating PTSD specifically in female veterans, as reported in another study [47]. However, a distinct investigation examining the efficacy of group trauma-focused exposure therapy for PTSD within a group of male Vietnam veterans [48] did not reveal substantial therapeutic advantages for this demographic.
Efficacy of mindfulness intervention
This study encompasses 10 papers on Mindfulness interventions for PTSD in military personnel [19,46,49–56], comprising a total sample of 617 military personnel. Mindfulness is often defined as the non-judgmental focusing of attention on the current experience, encouraging practitioners to experience the present moment with non-judgmental openness and acceptance.
Three randomized controlled trials focused on Mindfulness-Based Stress Reduction (MBSR) interventions for PTSD in veterans [49–51]. MBSR is a stress management model based on positive thinking, delivered through an 8-week series of classes [70]. In comparison to the control group (TAU) [49], service members showed improved mindfulness skills, but more evaluation is needed on its effects on PTSD. In another comparison with Group-PCT [50], MBSR demonstrated greater reductions in veterans with severe PTSD symptoms. A study by Niles et al. [51] conducted an 8-week telehealth-MBSR vs. tele-psychoeducation intervention, revealing clinically significant improvements in PTSD scores. However, these improvements were not maintained at the 6-week follow-up, suggesting that brief Mindfulness interventions may not have sufficient intensity to sustain effects on PTSD symptoms. Further investigation into the long-term therapeutic benefits of Mindfulness interventions is warranted.
Two papers on Mindfulness-Based Cognitive Therapy for PTSD in veterans [19,52] were included in the study. MBCT, a group-based program based on Mindfulness therapy, combines Mindfulness Meditation Technique with Cognitive Behavioral Therapy in an 8-week group treatment modality, it has become one of the most valued psychological treatment methods in recent years due to its portability and effectiveness [71]. Compared to the control group (TAU), the MBCT group significantly reduced veterans’ PTSD symptoms and alleviated symptoms of depression, anxiety, and stress, making it a promising psychotherapy for PTSD in military personnel. Further examination of the validity of the randomized controlled experimental design and identification of factors affecting acceptability and validity is needed.
This article also discusses the research on Mantram Repetition Program for PTSD in veterans [53,54]. MRP is a portable meditation-based intervention that teaches three tools for training attention and regulating emotion [72]. In comparison to the control group (TAU/PCT), the MRP group was more effective for chronic PTSD in military personnel. MRP does not focus on trauma, and veterans can seek this form of treatment. However, further empirical research is needed to validate its effectiveness.
In 2016, Lang et al. [55] explored the effectiveness of Acceptance and Commitment Therapy for PTSD in military personnel. ACT, considered a major psychotherapeutic theory alongside cognitive-behavioral therapy, requires further investigation to understand why it does not perform as well as expected in veteran samples [73].
An RCT on Transcendental Meditation noted that TM is no less effective than Prolonged Exposure Therapy as an intervention for PTSD in military personnel [46]. TM is a non-invasive, simple, and relaxing treatment involving sitting for 20 min twice a day with eyes closed, allowing ordinary thought processes to become calmer [74]. While TM may be an option for PTSD patients unwilling or unable to expose trauma, its therapeutic benefits need further validation.
Additionally, a 3-arm RCT study [56] noted that Internet-based Mindfulness interventions had a reduction in PTSD symptoms for military personnel compared to a waitlist control group, while face-to-face Mindfulness training had a greater benefit for military personnel with PTSD relative to online training.
Efficacy of new technology-based treatment
This study incorporates eight investigations into the effects of new technology-based treatment modalities on military PTSD interventions, comprising 4 studies on Internet and Computer-based treatment and 4 studies utilizing real-time computer graphics and a head-mounted visual display device for virtual reality exposure therapy. Virtual Reality Exposure Therapy proves to be more effective in activating or altering the structure of patients’ fear, facilitating repeated exposure to specific fearful stimuli for PTSD intervention. However, VRET environments need careful pre-designing, are highly individualized, and have limited applicability.
One study [60] separately intervened with VRET and PCT in veterans with PTSD, revealing a moderate effect size for VRET during a 6-month follow-up period. McLay et al. [61] demonstrated a 70% effective improvement with VRET compared to the control group (TAU) after a 10-week VRET intervention in PTSD patients. In a 3-arm RCT [44], both VRET and PET were more effective than the control group in intervening in PTSD in military personnel. However, at follow-up, the PET group showed greater effectiveness than the VRET group in active-duty military personnel. The research results of Beidel et al. [62] also support the use of VRET as an effective treatment for combat-related PTSD. Although limited by factors like small sample sizes, lack of blinding, and single therapists, the results support VRET as a safe and effective treatment for combat-related PTSD.
Two studies [57,58] demonstrated the significant effectiveness of ICT-based Cognitive Processing Therapy in intervening in veterans’ PTSD symptoms. Litz et al. [59] indicated that ICT-based Cognitive Behavioral Therapy was more effective than the control group (supportive counseling) in intervening in PTSD symptoms and overall depression levels in active-duty military personnel, with sustained symptom improvement at the 6-month follow-up. In another 3-arm RCT [56], both ICT-based Mindfulness intervention and face-to-face Mindfulness intervention showed high clinical significance, with face-to-face Mindfulness intervention demonstrating better outcomes compared to the control group. Preliminary data suggest that psychotherapy utilizing ICT is equally effective as traditional psychotherapy and can provide more convenient treatment, especially for PTSD patients in the veteran population facing high levels of pathogenic stigma, distant geographic locations, and challenging economic circumstances.
Efficacy of other psychotherapy
PTSD in the military population, especially during war, is a complex and challenging disorder to treat. Experts and scholars are exploring more psychotherapeutic treatments for the military PTSD population (Table 6). Examples include Emotional Freedom Techniques, based on the traditional Chinese medical system [63], is a brief form of exposure therapy that includes both physical and cognitive components. It involves tapping on acupuncture points with the fingers in a way that encourages individuals to remember or verbalize somatic symptoms or negative memories. This process aids in releasing life stress and physical problems from the body’s energy system, facilitating a return to a state of physical and mental well-being. Another therapeutic approach is Imagery Rehearsal (IR) [64], which controls the reconstruction of situations by controlling imagery. In the first phase, the entire process of exposure and restructuring is recorded using a tape recorder as homework for the patient to repeatedly listen to. In the second phase, imagery exercises are focused on altering the pathogenic patterns. Furthermore, telephone care management [65] represents an intervention method that employs a telephonic therapy approach to provide remote support and guidance.
Accelerated Resolution Therapy (ART) is an innovative psychological treatment approach that assists patients in processing and reshaping their psychological trauma by re-describing painful events and utilizing metaphors as key elements in the therapeutic process. During ART sessions, therapists guide patients to identify and re-experience the negative memories and images that lead to Post-Traumatic Stress Disorder. Subsequently, positive imagery and metaphors are employed to help patients reconstruct these memories in a healthier and more constructive manner [75]. As early as 2013, Kip et al. [76] explored its effectiveness in intervening PTSD within military populations, but since then, there have been few further inquiries. And in 2019, Kehle-Forbes et al. [77] explored the efficacy of integrated Motivational Enhancement Therapy (MET) and PET interventions. These therapies use a series of question-and-answer exchanges and reflective techniques to assist patients in identifying and modifying their negative behaviors and perceptions. The goal of these interventions is to enhance patients’ motivation and autonomy, thereby promoting behavioral change. Additionally, Harris et al. [78] explored the impact of Building Spiritual Strength (BSS) on PTSD in veterans in 2018. BSS is an 8-week group therapy approach that integrates spiritual elements into the treatment process, aimed at alleviating symptoms of PTSD. It facilitates a resolution of spiritual distress and helps individuals develop a new, more adaptive, and holistic understanding of their traumatic experiences. This method views spiritual health as an essential component of overall well-being, and through group support and spiritual practices, it can enhance an individual’s inner strength and resilience [79]. Lastly, Jain et al. [80] explored the Skills Training in Affective and Interpersonal Regulation (STAIR) intervention in 2020. STAIR is a comprehensive approach that combines 8–12 sessions of trauma-focused work, which are based on skill-building exercises tailored to enhance emotional and interpersonal regulation. This method contributes to the ongoing efforts to develop effective treatment strategies that address the complex needs of individuals dealing with PTSD.
Psychotherapeutic approaches for treating Post-Traumatic Stress Disorder in military personnel are continuously evolving and being refined through ongoing research efforts. However, due to the limited number of studies and small sample sizes, there is still a significant need for further exploration and investigation in this field.
Psychotherapy for PTSD, notably PET, CPT, and EMDR, is well-established and regarded as leading evidence-based treatments according to major clinical guidelines [81]. However, EMDR has been less utilized in treating military personnel with PTSD after 2000 and is not covered in this article. Some suggest that EMDR’s effectiveness may be linked to therapist feedback during traumatic memory re-exposure or repair, rather than the specific eye movement component. In brief, research on EMDR’s efficacy generally focuses on the general population [82]. PET and CPT are recommended by the U.S. Department of Veterans Affairs as the primary psychological treatments for Post-Traumatic Stress Disorder (PTSD) in military populations, with a significant amount of clinical research supporting their use. However, concerns remain regarding dropout rates and residual symptoms. Among the 13 CPT and PET articles in this study, a notable number reported higher attrition rates in the experimental group [25,26,30,38,41,42], with ongoing symptoms during follow-up, this aligns with findings in related studies [66,83]. To compensate for the shortcomings of First-line psychotherapy, it is necessary to improve past intervention methods or to find alternative approaches.
Mindfulness intervention emerges as a thriving and effective treatment for PTSD, with numerous recent studies demonstrating its favorable effects on both veterans and the general population [52,84,85]. This study reviewed and included 10 studies that explored the effects of Mindfulness interventions on PTSD in military personnel, all of which consistently demonstrated the positive role of Mindfulness interventions in treating military PTSD. This finding aligns with the results of a meta-analysis [86], which also concluded that Mindfulness interventions serve as an effective alternative therapy for treating PTSD in the military. However, these studies did not reach a consensus on the specific details regarding the duration of the intervention and the extent of its effects [50,51,73]. The research by Hopwood et al. indicates that longer mindfulness practice may enhance skills acquisition, leading to greater reductions in PTSD symptoms [87]. Some studies have pointed out that individuals can only participate in intervention treatments and achieve good therapeutic effects under the supervision of professionals or after being fully trained and guided by professionals [88]. These all prompt us to consider Mindfulness intervention programs, their implementation processes, and the execution of these processes. It is important to conduct an in-depth exploration of the intervention duration to ensure the effectiveness and sustainability of Mindfulness interventions while not increasing the time commitment burden on individuals with PTSD. Simultaneously, it is indicated that group therapy represents a significant modality for mitigating and improving symptoms of PTSD in military personnel [17,26,27]. Utilization of group therapy models becomes particularly pertinent in contexts where the availability of therapists is constrained. Not only does this approach alleviate the shortage of individual therapists, but it also facilitates access to professional guidance for patients. Furthermore, there are differing perspectives within current research regarding the effectiveness of Mindfulness interventions, with some studies indicating that individuals in the control group experienced better symptom improvement than those in the Mindfulness intervention experimental group [89]. This suggests that different trauma populations may be more responsive to varying forms of exercises. Moreover, PTSD within military populations is more complex and requires intervention methods and processes that are specifically tailored to the individual’s traumatic experiences, personality traits, and living conditions.
Advancements in science and technology have introduced new horizons for psychotherapeutic techniques. Firstly, the high dropout rate in frontline treatments is particularly common among veterans, mainly attributed to factors such as the stigma associated with illness, the remote location of medical institutions, and the high cost of treatment [90]. The use of modern communication technology in remote video therapy platforms can effectively alleviate these issues. Secondly, the personal preferences of patients have a significant impact on the effectiveness of the treatment. If patients can choose their preferred method of treatment, not only may they achieve better therapeutic outcomes, but the completion rate of the treatment is also likely to increase [91]. Virtual Reality Exposure Therapy, as a highly personalized treatment plan, is particularly suitable for military patients with PTSD who have a higher demand for personalized treatment.
Although a multitude of psychological therapies have proven to be somewhat effective in the treatment of Post-Traumatic Stress Disorder, against the backdrop of current international tensions and frequent regional conflicts, the issue of PTSD among military personnel has become more pronounced. For this special group, particularly post-war veterans, the treatment of PTSD still faces many challenges. Firstly, many veterans, influenced by various factors, drop out during the treatment process and become uncontactable during follow-up visits, failing to complete the entire treatment regimen. This results in an inability to verify the therapeutic outcomes, which may point to deficiencies in the acceptability and compliance of existing therapies. Additionally, it could be related to a lack of professional expertise among medical personnel. Secondly, for patients with PTSD who also have co-occurring issues such as substance abuse, depression, and anxiety, the efficacy of universal psychological treatment plans is limited. It is necessary to further consider the applicability and specificity of treatment approaches for this particular group of patients. Thirdly, the current therapeutic approaches encounter a significant decline in efficacy during the post-intervention follow-up period, indicating that the assessment of long-term and delayed effects of psychological treatments has not been adequately emphasized. This oversight has led to a deficiency in understanding and managing the recurrence of PTSD and issues related to treatment resistance. Consequently, there is an urgent need for an in-depth analysis of existing treatment strategies and the exploration of novel therapeutic methods to meet the long-term treatment needs of patients.
Future research should place a greater emphasis on the prevention and treatment of PTSD caused by warfare, prioritizing first-line interventions, especially Cognitive Processing Therapy and Prolonged Exposure Therapy (PET). These evidence-based approaches have demonstrated substantial efficacy in addressing military-related PTSD. Additionally, Mindfulness interventions stand out as valuable alternative therapies, providing a complementary and diverse treatment option. Simultaneously, embracing advancements in technology is crucial for enhancing the therapeutic benefits of traditional psychotherapeutic tools. Integrating new technological tools, such as web-based platforms, computer applications, and virtual reality technologies, offers innovative avenues for improving intervention outcomes. By leveraging these tools, the field can adapt and evolve to meet the unique challenges and complexities of PTSD treatment in military populations. The synergy of established psychotherapeutic methods and cutting-edge technology holds great promise in furthering the effectiveness of interventions and ultimately improving the well-being of military personnel dealing with PTSD.
CPT and PET exhibit significant efficacy as evidence-based psychotherapeutic treatments for military PTSD. Mindfulness interventions serve as effective alternatives, especially when conventional interventions show limited benefits. Given individual differences and high dropout rates, web- and computer-based tele-interventions and personalized interventions using virtual reality may enhance the overall effectiveness of first-line psychotherapeutic interventions for military PTSD patients. Further high-quality studies are crucial for validating the clinical and individual benefits of emerging psychotherapeutic treatments in military populations with PTSD.
Acknowledgement: We thank BW (Physical Education and Sports, Central China Normal University) and YH (Tianjin University of Sports) for stimulating discussion.
Funding Statement: This research was funded by a research Grant CCNU22JC004 from Department of Science and Technology, Central China Normal University. And the Fundamental Research Funds for the Central Universities (CCNU23CS035).
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design, Wencen Lan, Bin Wang; data collection, analysis and interpretation of results: Wencen Lan, Gai Li, Jianming Liu; draft manuscript preparation: Wencen Lan. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The original contributions presented in the study are included in the Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://doi.org/10.32604/ijmhp.2024.052309.
References
1. Thakur A, Choudhary D, Kumar B, Chaudhary A. A review on post-traumatic stress disorder (PTSDsymptoms, therapies and recent case studies. Curr Mol Pharmacol. 2022;15(3):502–16. doi:10.2174/1874467214666210525160944. [Google Scholar] [PubMed] [CrossRef]
2. Björkman F, Ekblom Ö. Physical exercise as treatment for PTSD: a systematic review and meta-analysis. Mil Med. 2022;187(9–10):e1103–13. doi:10.1093/milmed/usab497. [Google Scholar] [PubMed] [CrossRef]
3. Inoue C, Shawler E, Jordan CH, Moore MJ, Jackson CA. Veteran and military mental health issues. In: StatPearls. Treasure Island (FLStatPearls Publishing; 2023 Aug 17. [Google Scholar]
4. Peterson AL. General perspective on the U.S. military conflicts in Iraq and Afghanistan after 20 years. Mil Med. 2022;187(9–10):248–51. doi:10.1093/milmed/usab496. [Google Scholar] [PubMed] [CrossRef]
5. Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, et al. Course of posttraumatic stress disorder 40 years after the vietnam war: findings from the National Vietnam veterans longitudinal study. JAMA Psychiatry. 2015;72(9):875–81. doi:10.1001/jamapsychiatry.2015.0803. [Google Scholar] [PubMed] [CrossRef]
6. Groessl EJ, Hafey C, McCarthy A, Hernandez RM, Prado-Nava M, Casteel D, et al. Yoga plus mantram repetition to reduce chronic pain in veterans with post-traumatic stress disorder: a feasibility trial. Glob Adv Integr Med Health. 2023;12:27536130231220623. doi:10.1177/27536130231220623. [Google Scholar] [PubMed] [CrossRef]
7. Obuobi-Donkor G, Oluwasina F, Nkire N, Agyapong VIO. A scoping review on the prevalence and determinants of post-traumatic stress disorder among military personnel and firefighters: iimplications for public policy and practice. Int J Environ Res Public Health. 2022;19(3):1565. doi:10.3390/ijerph19031565. [Google Scholar] [PubMed] [CrossRef]
8. Shahmiri Barzoki H, Ebrahimi M, Khoshdel A, Noorbala AA, Rahnejat AM, Avarzamani L, et al. Studying the prevalence of PTSD in veterans, combatants and freed soldiers of Iran-Iraq war: a systematic and meta-analysis review. Psychol Health Med. 2023;28(3):812–8. doi:10.1080/13548506.2021.1981408. [Google Scholar] [PubMed] [CrossRef]
9. LeardMann CA, Matsuno RK, Boyko EJ, Powell TM, Reger MA, Hoge CW, et al. Association of combat experiences with suicide attempts among active-duty US service members. JAMA Netw Open. 2021;4(2):e2036065. doi:10.1001/jamanetworkopen.2020.36065. [Google Scholar] [PubMed] [CrossRef]
10. Moore BA, Pujol L, Waltman S, Shearer DS. Management of post-traumatic stress disorder in Veterans and military service members: a review of pharmacologic and psychotherapeutic interventions since 2016. Curr Psychiatry Rep. 2021;23(2):9. doi:10.1007/s11920-020-01220-w. [Google Scholar] [PubMed] [CrossRef]
11. Leichsenring F, Steinert C, Rabung S, Ioannidis JPA. The efficacy of psychotherapies and pharmacotherapies for mental disorders in adults: an umbrella review and meta-analytic evaluation of recent meta-analyses. World Psychiatry. 2022;21(1):133–45. doi:10.1002/wps.20941. [Google Scholar] [PubMed] [CrossRef]
12. Sloan DM, Marx BP, Lee DJ, Resick PA. A Brief exposure-based treatment vs cognitive processing therapy for posttraumatic stress disorder: a randomized noninferiority clinical trial. JAMA Psychiat. 2018;75(3):233–9. doi:10.1001/jamapsychiatry.2017.4249. [Google Scholar] [PubMed] [CrossRef]
13. Fikretoglu D, Sharp ML, Adler AB, Bélanger S, Benassi H, Bennett C, et al. Pathways to mental health care in active military populations across the Five-Eyes nations: an integrated perspective. Clin Psychol Rev. 2022;91(2):102100. doi:10.1016/j.cpr.2021.102100. [Google Scholar] [PubMed] [CrossRef]
14. Heyman RE, Slep AMS, Parsons AM, Ellerbeck EL, McMillan KK. Systematic review of the military career impact of mental health evaluation and treatment. Mil Med. 2022;187(5–6):e598–618. doi:10.1093/milmed/usab283. [Google Scholar] [PubMed] [CrossRef]
15. Shepherd-Banigan M, Shapiro A, Sheahan KL, Ackland PE, Meis LA, Thompson-Hollands J, et al. Mental health therapy for veterans with PTSD as a family affair: a qualitative inquiry into how family support and social norms influence veteran engagement in care. Psychol Serv. 2023;20(4):839–48. doi:10.1037/ser0000742. [Google Scholar] [PubMed] [CrossRef]
16. Karlin BE, Ruzek JI, Chard KM, Eftekhari A, Monson CM, Hembree EA, et al. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. J Trauma Stress. 2010;23(6):663–73. doi:10.1002/jts.20588. [Google Scholar] [PubMed] [CrossRef]
17. Haynes PL, Burger SB, Kelly M, Emert S, Perkins S, Shea MT. Cognitive behavioral social rhythm group therapy versus present centered group therapy for veterans with posttraumatic stress disorder and major depressive disorder: a randomized controlled pilot trial. J Affect Disord. 2020;277:800–9. doi:10.1016/j.jad.2020.09.009. [Google Scholar] [PubMed] [CrossRef]
18. Rauch SA, King AP, Abelson J, Tuerk PW, Smith E, Rothbaum BO, et al. Biological and symptom changes in posttraumatic stress disorder treatment: a randomized clinical trial. Depress Anxiety. 2015;32(3):204–12. doi:10.1002/da.22331. [Google Scholar] [PubMed] [CrossRef]
19. Jasbi M, Sadeghi Bahmani D, Karami G, Omidbeygi M, Peyravi M, Panahi A, et al. Influence of adjuvant mindfulness-based cognitive therapy (MBCT) on symptoms of post-traumatic stress disorder (PTSD) in veterans-results from a randomized control study. Cogn Behav Ther. 2018;47(5):431–46. doi:10.1080/16506073.2018.1445773. [Google Scholar] [PubMed] [CrossRef]
20. Maercker A, Cloitre M, Bachem R, Schlumpf YR, Khoury N, Hitchcock C, et al. Complex post-traumatic stress disorder. Lancet. 2022;400(10345):60–72. doi:10.1016/S0140-6736(22)00821-2. [Google Scholar] [PubMed] [CrossRef]
21. Weber M, Schumacher S, Hannig W, Barth J, Lotzin A, Schäfer I, et al. Long-term outcomes of psychological treatment for posttraumatic stress disorder: a systematic review and meta-analysis. Psychol Med. 2021;51(9):1420–30. doi:10.1017/S003329172100163X. [Google Scholar] [PubMed] [CrossRef]
22. Bryant RA. Post-traumatic stress disorder: a state-of-the-art review of evidence and challenges. World Psychiat. 2019;18(3):259–69. doi:10.1002/wps.20656. [Google Scholar] [PubMed] [CrossRef]
23. Mavranezouli I, Megnin-Viggars O, Daly C, Dias S, Welton NJ, Stockton S, et al. Psychological treatments for post-traumatic stress disorder in adults: a network meta-analysis. Psychol Med. 2020;50(4):542–55. doi:10.1017/S0033291720000070. [Google Scholar] [PubMed] [CrossRef]
24. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA, 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29;372:n71. doi:10.1136/bmj.n71. [Google Scholar] [PubMed] [CrossRef]
25. Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol. 2006;74(5):898–907. doi:10.1037/0022-006X.74.5.898. [Google Scholar] [PubMed] [CrossRef]
26. Resick PA, Wachen JS, Mintz J, Young-McCaughan S, Roache JD, Borah AM, et al. A randomized clinical trial of group cognitive processing therapy compared with group present-centered therapy for PTSD among active duty military personnel. J Consult Clin Psychol. 2015;83(6):1058–68. doi:10.1037/ccp0000016. [Google Scholar] [PubMed] [CrossRef]
27. Forbes D, Lloyd D, Nixon RD, Elliott P, Varker T, Perry D, et al. A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. J Anxiety Disord. 2012;26(3):442–52. doi:10.1016/j.janxdis.2012.01.006. [Google Scholar] [PubMed] [CrossRef]
28. Surís A, Link-Malcolm J, Chard K, Ahn C, North C. A randomized clinical trial of cognitive processing therapy for veterans with PTSD related to military sexual trauma. J Trauma Stress. 2013;26(1):28–37. doi:10.1002/jts.21765. [Google Scholar] [PubMed] [CrossRef]
29. Kozel FA, Motes MA, Didehbani N, DeLaRosa B, Bass C, Schraufnagel CD, et al. Repetitive TMS to augment cognitive processing therapy in combat veterans of recent conflicts with PTSD: a randomized clinical trial. J Affect Disord. 2018;229:506–14. doi:10.1016/j.jad.2017.12.046. [Google Scholar] [PubMed] [CrossRef]
30. Maguen S, Burkman K, Madden E, Dinh J, Bosch J, Keyser J, et al. Impact of killing in war: a randomized, controlled pilot trial. J Clin Psychol. 2017;73(9):997–1012. doi:10.1002/jclp.22471. [Google Scholar] [PubMed] [CrossRef]
31. Frueh BC, Monnier J, Yim E, Grubaugh AL, Hamner MB, Knapp RG. A randomized trial of telepsychiatry for post-traumatic stress disorder. J Telemed Telecare. 2007;13(3):142–7. doi:10.1258/135763307780677604. [Google Scholar] [PubMed] [CrossRef]
32. Najavits LM, Krinsley K, Waring ME, Gallagher MW, Skidmore C. A randomized controlled trial for veterans with ptsd and substance use disorder: creating change versus seeking safety. Subst Use Misuse. 2018;53(11):1788–800. doi:10.1080/10826084.2018.1432653. [Google Scholar] [PubMed] [CrossRef]
33. Beidel DC, Frueh BC, Uhde TW, Wong N, Mentrikoski JM. Multicomponent behavioral treatment for chronic combat-related posttraumatic stress disorder: a randomized controlled trial. J Anxiety Disord. 2011;25(2):224–31. doi:10.1016/j.janxdis.2010.09.006. [Google Scholar] [PubMed] [CrossRef]
34. Dunn NJ, Rehm LP, Schillaci J, Souchek J, Mehta P, Ashton CM, et al. A randomized trial of self-management and psychoeducational group therapies for comorbid chronic posttraumatic stress disorder and depressive disorder. J Trauma Stress. 2007;20(3):221–37. doi:10.1002/jts.20214. [Google Scholar] [PubMed] [CrossRef]
35. Possemato K, Kuhn E, Johnson E, Hoffman JE, Owen JE, Kanuri N, et al. Using PTSD Coach in primary care with and without clinician support: a pilot randomized controlled trial. Gen Hosp Psychiatry. 2016;38:94–8. doi:10.1016/j.genhosppsych.2015.09.005. [Google Scholar] [PubMed] [CrossRef]
36. Morland LA, Greene CJ, Rosen CS, Foy D, Reilly P, Shore J, et al. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. J Clin Psychiat. 2010;71(7):855–63. doi:10.4088/JCP.09m05604blu. [Google Scholar] [PubMed] [CrossRef]
37. Mackintosh MA, Niehaus J, Taft CT, Marx BP, Grubbs K, Morland LA. Using a mobile application in the treatment of dysregulated anger among veterans. Mil Med. 2017;182(11):e1941–9. doi:10.7205/MILMED-D-17-00063. [Google Scholar] [PubMed] [CrossRef]
38. Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized controlled trial. JAMA. 2007;297(8):820–30. doi:10.1001/jama.297.8.820. [Google Scholar] [PubMed] [CrossRef]
39. Nacasch N, Foa EB, Huppert JD, Tzur D, Fostick L, Dinstein Y, et al. Prolonged exposure therapy for combat- and terror-related posttraumatic stress disorder: a randomized control comparison with treatment as usual. J Clin Psychiatry. 2011;72(9):1174–80. doi:10.4088/JCP.09m05682blu. [Google Scholar] [PubMed] [CrossRef]
40. Ford JD, Grasso DJ, Greene CA, Slivinsky M, DeViva JC. Randomized clinical trial pilot study of prolonged exposure versus present centred affect regulation therapy for PTSD and anger problems with male military combat veterans. Clin Psychol Psychother. 2018;25(5):641–9. doi:10.1002/cpp.2194. [Google Scholar] [PubMed] [CrossRef]
41. Back SE, Killeen T, Badour CL, Flanagan JC, Allan NP, Ana ES, et al. Concurrent treatment of substance use disorders and PTSD using prolonged exposure: a randomized clinical trial in military veterans. Addict Behav. 2019;90(7):369–77. doi:10.1016/j.addbeh.2018.11.032. [Google Scholar] [PubMed] [CrossRef]
42. Thorp SR, Glassman LH, Wells SY, Walter KH, Gebhardt H, Twamley E, et al. A randomized controlled trial of prolonged exposure therapy versus relaxation training for older veterans with military-related PTSD. J Anxiety Disord. 2019;64(2):45–54. doi:10.1016/j.janxdis.2019.02.003. [Google Scholar] [PubMed] [CrossRef]
43. Yuen EK, Gros DF, Price M, Zeigler S, Tuerk PW, Foa EB, et al. Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results. J Clin Psychol. 2015;71(6):500–12. doi:10.1002/jclp.22168. [Google Scholar] [PubMed] [CrossRef]
44. Reger GM, Koenen-Woods P, Zetocha K, Smolenski DJ, Holloway KM, Rothbaum BO, et al. Randomized controlled trial of prolonged exposure using imaginal exposure vs. virtual reality exposure in active duty soldiers with deployment-related posttraumatic stress disorder (PTSD). J Consult Clin Psychol. 2016;84(11):946–59. doi:10.1037/ccp0000134. [Google Scholar] [PubMed] [CrossRef]
45. Foa EB, McLean CP, Zang Y, Rosenfield D, Yadin E, Yarvis JS, et al. Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: a randomized clinical trial. JAMA. 2018;319(4):354–64. doi:10.1001/jama.2017.21242. [Google Scholar] [PubMed] [CrossRef]
46. Nidich S, Mills PJ, Rainforth M, Heppner P, Schneider RH, Rosenthal NE, et al. Non-trauma-focused meditation versus exposure therapy in veterans with post-traumatic stress disorder: a randomised controlled trial. Lancet Psychiatry. 2018;5(12):975–86. doi:10.1016/s2215-0366(18)30384-5. [Google Scholar] [PubMed] [CrossRef]
47. Castillo DT, Chee CL, Nason E, Keller J, C’De Baca J, Qualls C, et al. Group-delivered cognitive/exposure therapy for PTSD in women veterans: a randomized controlled trial. Psychol Trauma. 2016;8(3):404–12. doi:10.1037/tra0000111. [Google Scholar] [PubMed] [CrossRef]
48. Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, et al. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: results from a department of veterans affairs cooperative study. Arch Gen Psychiat. 2003;60(5):481–9. doi:10.1001/archpsyc.60.5.481. [Google Scholar] [PubMed] [CrossRef]
49. Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. J Clin Psychol. 2013;69(1):14–27. doi:10.1002/jclp.21911. [Google Scholar] [PubMed] [CrossRef]
50. Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA. 2015;314(5):456–65. doi:10.1001/jama.2015.8361. [Google Scholar] [PubMed] [CrossRef]
51. Niles BL, Silberbogen AK, Wolf EJ, Klunk-Gillis J, Ryngala DJ, Paysnick A. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychol Trauma-Theory Res Pract Policy. 2012;4(5):538–47. [Google Scholar]
52. King AP, Erickson TM, Giardino ND, Favorite T, Rauch SA, Robinson E, et al. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depress Anxiety. 2013;30(7):638–45. doi:10.1002/da.22104. [Google Scholar] [PubMed] [CrossRef]
53. Bormann JE, Thorp SR, Wetherell JL, Golshan S, Lang AJ. Meditation-based mantram intervention for veterans with posttraumatic stress disorder: a randomized trial. Psychol Trauma-Theory Res Pract Policy. 2013;5(3):259–67. [Google Scholar]
54. Crawford JN, Talkovsky AM, Bormann JE, Lang AJ. Targeting hyperarousal: mantram repetition program for PTSD in US veterans. Eur J Psychotraumatol. 2019;10(1):1665768. doi:10.1080/20008198.2019.1665768. [Google Scholar] [PubMed] [CrossRef]
55. Lang AJ, Schnurr PP, Jain S, He F, Walser RD, Bolton E, et al. Randomized controlled trial of acceptance and commitment therapy for distress and impairment in OEF/OIF/OND veterans. Psychol Trauma. 2017;9(Suppl 1):74–84. doi:10.1037/tra0000127. [Google Scholar] [PubMed] [CrossRef]
56. Rice VJ, Liu B, Schroeder PJ. Impact of in-person and virtual world mindfulness training on symptoms of post-traumatic stress disorder and attention deficit and hyperactivity disorder. Mil Med. 2018;183(suppl_1):413–20. doi:10.1093/milmed/usx227. [Google Scholar] [PubMed] [CrossRef]
57. Liu L, Thorp SR, Moreno L, Wells SY, Glassman LH, Busch AC, et al. Videoconferencing psychotherapy for veterans with PTSD: results from a randomized controlled non-inferiority trial. J Telemed Telecare. 2020;26(9):507–19. doi:10.1177/1357633x19853947. [Google Scholar] [PubMed] [CrossRef]
58. Maieritsch KP, Smith TL, Hessinger JD, Ahearn EP, Eickhoff JC, Zhao Q. Randomized controlled equivalence trial comparing videoconference and in person delivery of cognitive processing therapy for PTSD. J Telemed Telecare. 2016;22(4):238–43. doi:10.1177/1357633x15596109. [Google Scholar] [PubMed] [CrossRef]
59. Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. Am J Psychiatry. 2007;164(11):1676–83. doi:10.1176/appi.ajp.2007.06122057. [Google Scholar] [PubMed] [CrossRef]
60. Ready DJ, Gerardi RJ, Backscheider AG, Mascaro N, Rothbaum BO. Comparing virtual reality exposure therapy to present-centered therapy with 11 U.S. Vietnam veterans with PTSD. Cyberpsychol Behav Soc Netw. 2010;13(1):49–54. doi:10.1089/cyber.2009.0239. [Google Scholar] [PubMed] [CrossRef]
61. McLay RN, Wood DP, Webb-Murphy JA, Spira JL, Wiederhold MD, Pyne JM, et al. A randomized, controlled trial of virtual reality-graded exposure therapy for post-traumatic stress disorder in active duty service members with combat-related post-traumatic stress disorder. Cyberpsychol Behav Soc Netw. 2011;14(4):223–9. doi:10.1089/cyber.2011.0003. [Google Scholar] [PubMed] [CrossRef]
62. Beidel DC, Frueh BC, Neer SM, Bowers CA, Trachik B, Uhde TW, et al. Trauma management therapy with virtual-reality augmented exposure therapy for combat-related PTSD: a randomized controlled trial. J Anxiety Disord. 2019;61(1):64–74. doi:10.1016/j.janxdis.2017.08.005. [Google Scholar] [PubMed] [CrossRef]
63. Church D, Hawk C, Brooks AJ, Toukolehto O, Wren M, Dinter I, et al. Psychological trauma symptom improvement in veterans using emotional freedom techniques: a randomized controlled trial. J Nerv Ment Dis. 2013;201(2):153–60. doi:10.1097/NMD.0b013e31827f6351. [Google Scholar] [PubMed] [CrossRef]
64. Cook JM, Harb GC, Gehrman PR, Cary MS, Gamble GM, Forbes D, et al. Imagery rehearsal for posttraumatic nightmares: a randomized controlled trial. J Traumatic Stress. 2010;23(5):553–63. doi:10.1002/jts.20569. [Google Scholar] [PubMed] [CrossRef]
65. Rosen CS, Azevedo KJ, Tiet QQ, Greene CJ, Wood AE, Calhoun P, et al. An RCT of effects of telephone care management on treatment adherence and clinical outcomes among veterans with PTSD. Psychiatr Serv. 2017;68(2):151–8. doi:10.1176/appi.ps.201600069. [Google Scholar] [PubMed] [CrossRef]
66. Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489–500. doi:10.1001/jama.2015.8370. [Google Scholar] [PubMed] [CrossRef]
67. Kuhn E, Greene C, Hoffman J, Nguyen T, Wald L, Schmidt J, et al. Preliminary evaluation of PTSD coach, a smartphone app for post-traumatic stress symptoms. Mil Med. 2014;179(1):12–8. doi:10.7205/milmed-d-13-00271. [Google Scholar] [PubMed] [CrossRef]
68. Hensler I, Sveen J, Cernvall M, Arnberg FK. Efficacy, Benefits, and harms of a self-management app in a swedish trauma-exposed community sample (PTSD Coachrandomized controlled trial. J Med Internet Res. 2022;24(3):e31419. doi:10.2196/31419. [Google Scholar] [PubMed] [CrossRef]
69. Rauch SA, Eftekhari A, Ruzek JI. Review of exposure therapy: a gold standard for PTSD treatment. J Rehabil Res Dev. 2012;49(5):679–87. doi:10.1682/jrrd.2011.08.0152. [Google Scholar] [PubMed] [CrossRef]
70. Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–42. doi:10.1177/1073191107313003. [Google Scholar] [PubMed] [CrossRef]
71. Williams JM, Kuyken W. Mindfulness-based cognitive therapy: a promising new approach to preventing depressive relapse. Br J Psychiatry. 2012;200(5):359–60. doi:10.1192/bjp.bp.111.104745. [Google Scholar] [PubMed] [CrossRef]
72. Wadlinger HA, Isaacowitz DM. Fixing our focus: training attention to regulate emotion. Pers Soc Psychol Rev. 2011;15(1):75–102. doi:10.1177/1088868310365565. [Google Scholar] [PubMed] [CrossRef]
73. Ducasse D, Fond G. La thérapie d’acceptation et d’engagement. L'Encéphale. 2015;41(1):1–9. doi:10.1016/j.encep.2013.04.017. [Google Scholar] [CrossRef]
74. Travis F, Shear J. Focused attention, open monitoring and automatic self-transcending: categories to organize meditations from Vedic, Buddhist and Chinese traditions. Conscious Cogn. 2010;19(4):1110–8. doi:10.1016/j.concog.2010.01.007. [Google Scholar] [PubMed] [CrossRef]
75. Waits W, Marumoto M, Weaver J. Accelerated resolution therapy (ARTa review and research to date. Curr Psychiatry Rep. 2017;19(3):18. doi:10.1007/s11920-017-0765-y. [Google Scholar] [PubMed] [CrossRef]
76. Kip KE, Rosenzweig L, Hernandez DF, Shuman A, Sullivan KL, Long CJ, et al. Randomized controlled trial of accelerated resolution therapy (ART) for symptoms of combat-related post-traumatic stress disorder (PTSD). Mil Med. 2013;178(12):1298–309. doi:10.7205/milmed-d-13-00298. [Google Scholar] [PubMed] [CrossRef]
77. Kehle-Forbes SM, Chen S, Polusny MA, Lynch KG, Koffel E, Ingram E, et al. A randomized controlled trial evaluating integrated versus phased application of evidence-based psychotherapies for military veterans with comorbid PTSD and substance use disorders. Drug Alcohol Depend. 2019;205(5):107647. doi:10.1016/j.drugalcdep.2019.107647. [Google Scholar] [PubMed] [CrossRef]
78. Harris JI, Usset T, Voecks C, Thuras P, Currier J, Erbes C. Spiritually integrated care for PTSD: a randomized controlled trial of building spiritual strength. Psychiatry Res. 2018;267(1):420–8. doi:10.1016/j.psychres.2018.06.045. [Google Scholar] [PubMed] [CrossRef]
79. Harris JI, Erbes CR, Engdahl BE, Thuras P, Murray-Swank N, Grace D, et al. The effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma. J Clin Psychol. 2011;67(4):425–38. doi:10.1002/jclp.20777. [Google Scholar] [PubMed] [CrossRef]
80. Jain S, Ortigo K, Gimeno J, Baldor DA, Weiss BJ, Cloitre M. A randomized controlled trial of brief skills training in affective and interpersonal regulation (STAIR) for veterans in primary care. J Trauma Stress. 2020;33(4):401–9. doi:10.1002/jts.22523. [Google Scholar] [PubMed] [CrossRef]
81. Forbes D, Creamer M, Bisson JI, Cohen JA, Crow BE, Foa EB, et al. A guide to guidelines for the treatment of PTSD and related conditions. J Trauma Stress. 2010;23(5):537–52. doi:10.1002/jts.20565. [Google Scholar] [PubMed] [CrossRef]
82. Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clin Psychol Rev. 2010;30(6):635–41. doi:10.1016/j.cpr.2010.04.007. [Google Scholar] [PubMed] [CrossRef]
83. Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, Simon NM. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. J Trauma Stress. 2015;28(5):401–9. doi:10.1002/jts.22038. [Google Scholar] [PubMed] [CrossRef]
84. Jansen JE, Morris EMJ. Acceptance and commitment therapy for posttraumatic stress disorder in early psychosis: a case series. Cogn Behav Pract. 2017;24(2):187–99. doi:10.1016/j.cbpra.2016.04.003. [Google Scholar] [CrossRef]
85. Pigeon W, Allen C, Possemato K, Bergen-Cico D, Treatman S. Feasibility and acceptability of a brief mindfulness program for veterans in primary care with posttraumatic stress disorder. Mindfulness. 2015;6(5):986–95. doi:10.1007/s12671-014-0340-0. [Google Scholar] [CrossRef]
86. Sun LN, Gu JW, Huang LJ, Shang ZL, Zhou YG, Wu LL, et al. Military-related posttraumatic stress disorder and mindfulness meditation: a systematic review and meta-analysis. Chin J Traumatol. 2021;24(4):221–30. doi:10.1016/j.cjtee.2021.05.003. [Google Scholar] [PubMed] [CrossRef]
87. Hopwood TL, Schutte NS. A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clin Psychol Rev. 2017;57(2):12–20. doi:10.1016/j.cpr.2017.08.002. [Google Scholar] [PubMed] [CrossRef]
88. Lustyk MK, Chawla N, Nolan RS, Marlatt GA. Mindfulness meditation research: issues of participant screening, safety procedures, and researcher training. Adv Mind Body Med. 2009;24(1):20–30. [Google Scholar] [PubMed]
89. Heffner KL, Crean HF, Kemp JE. Meditation programs for veterans with posttraumatic stress disorder: aggregate findings from a multi-site evaluation. Psychol Trauma. 2016;8(3):365–74. doi:10.1037/tra0000106. [Google Scholar] [PubMed] [CrossRef]
90. Steenkamp MM, Litz BT, Marmar CR. First-line psychotherapies for military-related PTSD. JAMA. 2020;323(7):656–7. doi:10.1001/jama.2019.20825. [Google Scholar] [PubMed] [CrossRef]
91. Zoellner LA, Roy-Byrne PP, Mavissakalian M, Feeny NC. Doubly randomized preference trial of prolonged exposure versus sertraline for treatment of PTSD. Am J Psychiatry. 2019;176(4):287–96. doi:10.1176/appi.ajp.2018.17090995. [Google Scholar] [PubMed] [CrossRef]
Appendix A
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF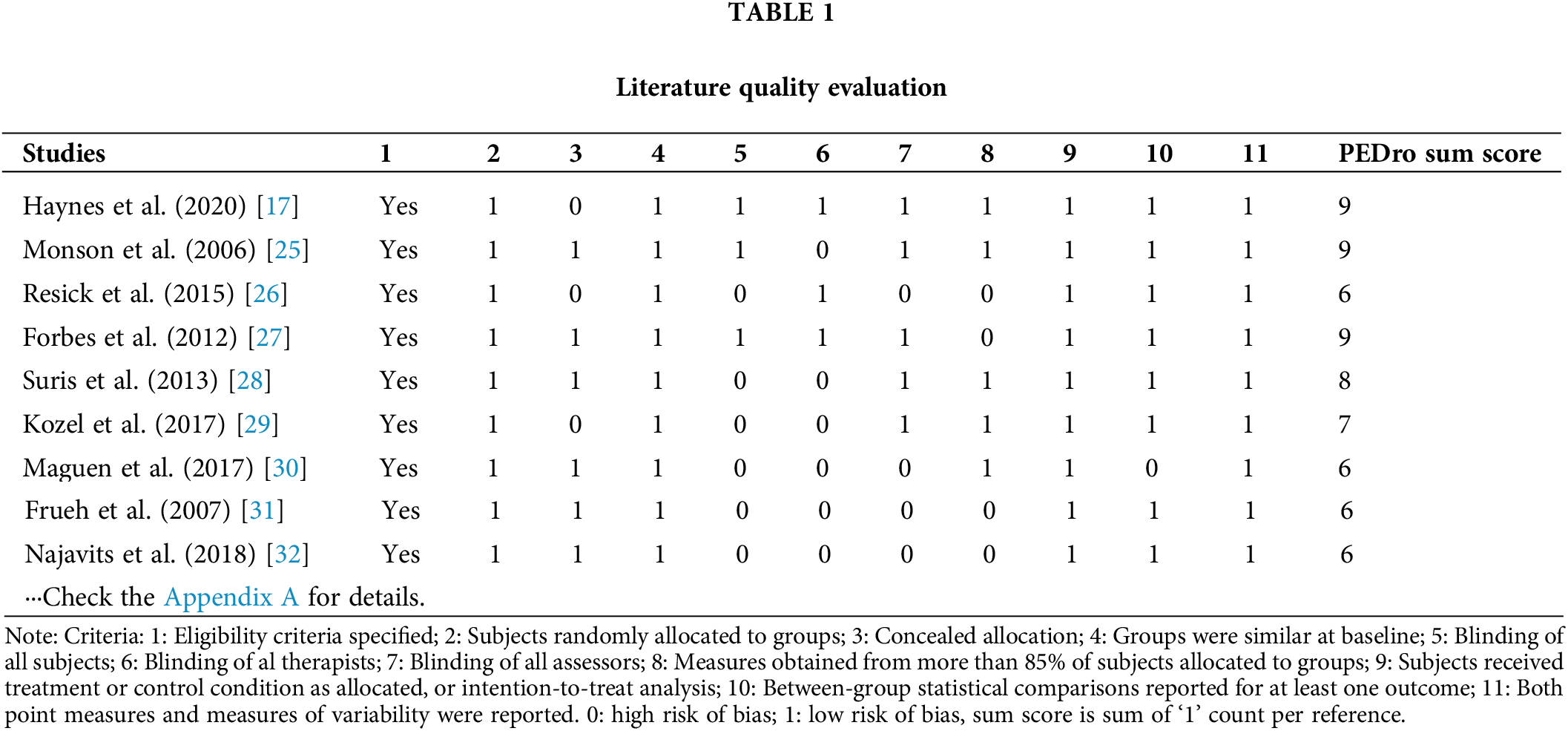
 Downloads
Downloads
 Citation Tools
Citation Tools