 Open Access
Open Access
ARTICLE
The Association between Fear of COVID-19, Obsession with COVID-19, and Post Traumatic Stress Disorder in Korean Emergency Rescue Firefighters: A Cross-Sectional Study
1 Red Cross College of Nursing, Chung-Ang University, Seoul, South Korea
2 Department of Nursing, Chung-Ang University, Seoul, South Korea
* Corresponding Author: Heewon Song. Email:
International Journal of Mental Health Promotion 2024, 26(6), 475-480. https://doi.org/10.32604/ijmhp.2024.050824
Received 19 February 2024; Accepted 23 May 2024; Issue published 28 June 2024
Abstract
During the rapid spread of COVID-19, first responders are at risk of being exposed to COVID-19 due to their role in providing first aid and responding to an unspecified number of people. This uncertainty can have adverse mental health effects, such as increased anxiety and fear. This study aimed to investigate the degree of association between fear of COVID-19, obsession with COVID-19, and post-traumatic stress disorder (PTSD) in emergency rescue firefighters. The participants were 150 emergency rescue firefighters working in Region S, Korea. They filled out self-report questionnaires: The data obtained through the Fear of COVID-19 Scale, Obsession with COVID-19 Scale, and Impact of Event Scale-Revised Korean version were subjected to nonparametric statistical analysis using SPSS WIN 25.0. The study found a significant correlation between emergency rescue firefighters’ fear of COVID-19, obsession with COVID-19, and PTSD. Fear and obsession with COVID-19 were higher among first responder firefighters who were directly involved in COVID-19-related tasks. Furthermore, a one-point increase in obsession was associated with a 2.837-point increase in PTSD. Based on the results, we found that there is a need for effective control of obsessions and fears among first responder firefighters during COVID-19, and we suggest that there is a need for mental health care for first responder firefighters during the pandemic through the development and support of programs to prevent and mitigate obsessions.Keywords
First reported in Wuhan, China in December 2019, COVID-19 quickly spread around the world, leading to a global pandemic. High infection and mortality rates made people fearful of contact with others [1,2]. The heightened fear and anxiety extended to high-level fears, such as stigma, discrimination, and hatred of the infected. This had a significant impact on people’s behavior and psychological well-being [3]. COVID-19 has led to an increase in obsessive behaviors such as handwashing, laundering, and avoidance of contact due to fear of infection, which in turn results in a deterioration in quality of life [4].
Emergency rescue firefighters are at high risk of exposure to COVID-19 due to their role as first responders, requiring them to perform emergency treatment and response for unknown numbers of individuals. Such uncertain circumstances heighten anxiety and contribute to increased obsessions and fears.
Anxiety, obsessions, and fears are positively correlated and influence the severity of post-traumatic stress disorder (PTSD) [5]. Previous studies have found a prevalence of PTSD of 73.4%, depression of 50.7%, and anxiety of 44.7% among healthcare workers who had contact with confirmed or suspected COVID-19 patients, confirming that COVID-19-related work has a significant negative impact on mental health.
Since 2020, research has been conducted on the mental health of healthcare professionals and its association with COVID-19 [6–8]. However, to our knowledge, there is limited research assessing the mental health of first responders during the COVID-19 pandemic, particularly on obsessions and fears, which are symptoms of mental health due to the strain and constant exposure to a specific infectious disease, rather than general mental health such as anxiety and depression. In the case of infectious diseases, there is a need to assess mental health about obsessive symptoms such as protective clothing and infection control, so this study aimed to examine the association between fear of COVID-19, obsession with COVID-19, and post-traumatic stress disorder in first responders. By identifying PTSD, obsessions, and fears among firefighters who are first responders in infectious disease settings such as COVID-19 in their communities, this study will help identify their mental health issues and provide appropriate coping strategies to promote mental health.
This study had a cross-sectional design to investigate the association between fear of COVID-19, obsession with COVID-19, and PTSD in emergency rescue firefighters.
This study was conducted with firefighters from five fire departments out of the twenty-five fire departments in Seoul, Korea by convenient sampling. The sample size was determined from 119 calculated using G*Power 3.1.9.7 to 150 considering dropout. For this study, the researcher obtained the consent of the fire chiefs and posted a recruitment notice on the intranet bulletin board of their respective organization. Participants were firefighters who were employed in their respective workplaces. The researcher conducted the study with participants who sent mobile messages and phone calls to the researcher, indicating their willingness to participate in the study.
Data for this study was collected from July 01–15, 2021, when ‘Maintain distancing’ (prohibiting gatherings of more than five people as part of South Korea’s COVID control policy) was in effect due to the spread of the delta variant virus. The researcher explained the purpose of the study to the institution and obtained approval for the study. The researcher then approached participants who voluntarily expressed their willingness to participate in the study. The researcher collected data by personally visiting the institution and approaching participants individually, explaining the study’s purpose, methods, and anonymity. Written informed consent was obtained by explaining verbally and in writing that they could stop participating at any time during the study and would not be penalized. The final participants who understood the study questionnaire and expressed their willingness to participate were asked to complete a self-report questionnaire, which the researcher promptly returned.
We used the Fear of COVID-19 Scale (FCV-19S), developed by Ahorsu et al. [9], to measure participants’ fear of COVID-19. We translated the scale into Korean with the permission of the original author as per protocol. This consists of 7 items; higher scores indicate greater fearfulness. Each item is scored on a 5-point Likert scale. Representative questions for this measure include ‘I am most worried about COVID-19’ and ‘Thinking about COVID-19 makes me uncomfortable’. The scale’s reliability, as measured by Cronbach’s alpha, is 0.82. In this study, it was 0.83.
Participants filled out the Obsession with COVID-19 Scale (OCS), developed for adults by Lee [10]. This consists of 4 items rated on a 5-point Likert scale, ranging from 0 (not at all) to 4 (almost every day in the past two weeks). A total OCS score ≥7 indicates the possibility of the existence of a non-functioning accident related to COVID-19. This indicates that the participant’s problematic symptoms should be further evaluated or treated. Representative questions include, ‘I keep thinking that I might have COVID-19’ and ‘I keep thinking that people I see might have COVID-19’. The reliability of this scale, as measured by Cronbach’s alpha, is 0.83; in this study, it was 0.82.
Post traumatic stress disorder
To measure the level of PTSD symptoms, we used the Impact of Event Scale-Revised Korean version (IES-R-K) [11]. This is a Korean version of Impact of Event Scale-Revised (IES-R), developed by Weiss et al. [12]. The scale consists of 22 items on a 5-point Likert scale, with total scores ranging from 0 to 88. The higher the total score, the more severe the post-traumatic stress, where 0–17 is considered normal, 18–24 is considered risk, and 25 and above is considered high risk. The representative question is, ‘When I think about the event, I feel the emotions I felt at the time come back.’ The Cronbach’s alpha of the IES-R-K was 0.83, and the coefficient of this study was 0.91.
Data were analyzed using SPSS WIN 25.0 for Windows. Due to the non-normality of the study dataset, data analysis was performed using non-normality statistics. The participants’ levels of PTSD symptoms, obsession with COVID-19, and fear of COVID-19 were analyzed using descriptive statistics. Differences between variables were analyzed using the Mann-Whitney U test and the statistical significance was set to p ≤ 0.05. The correlation between variables was analyzed using the Spearman rank correlation test. Finally, Bayesian estimator regression analysis was used to identify the factors affecting levels of PTSD symptoms.
The study was approved by Ethics Committee at the University of Chung-Ang (IRB number: 1041078-202011-HR-318-01). All participants signed the informed consent in this study. We explained the purpose, method, anonymity of participation, voluntary participation in the study, and the possibility of discontinuing the study at any time during the study with no penalty to all participants.
Participant characteristics are shown in Table 1. Participants included 136 males (90.7%) and 14 females (9.3%). The most common age distribution was 50–59 years old. Being married was most common (70.7%), followed by unmarried (27.3%). Thirty-three (22%) and 117 (78%) participants practiced and did not engage in religious activities, respectively. Sixty-four (42.7%) respondents performed work that was directly related to COVID-19 (such as transportation and rescue of infected individuals).
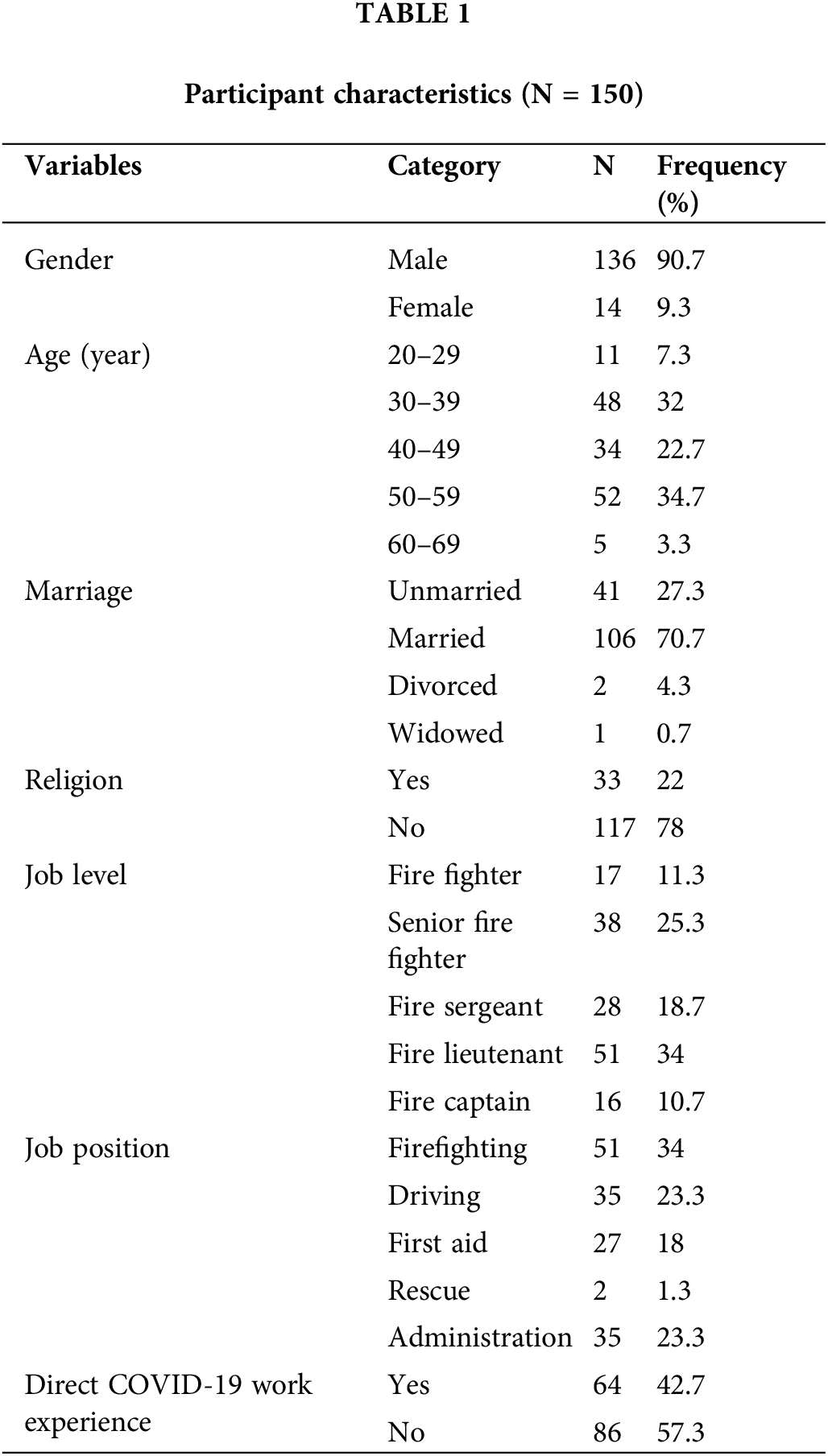
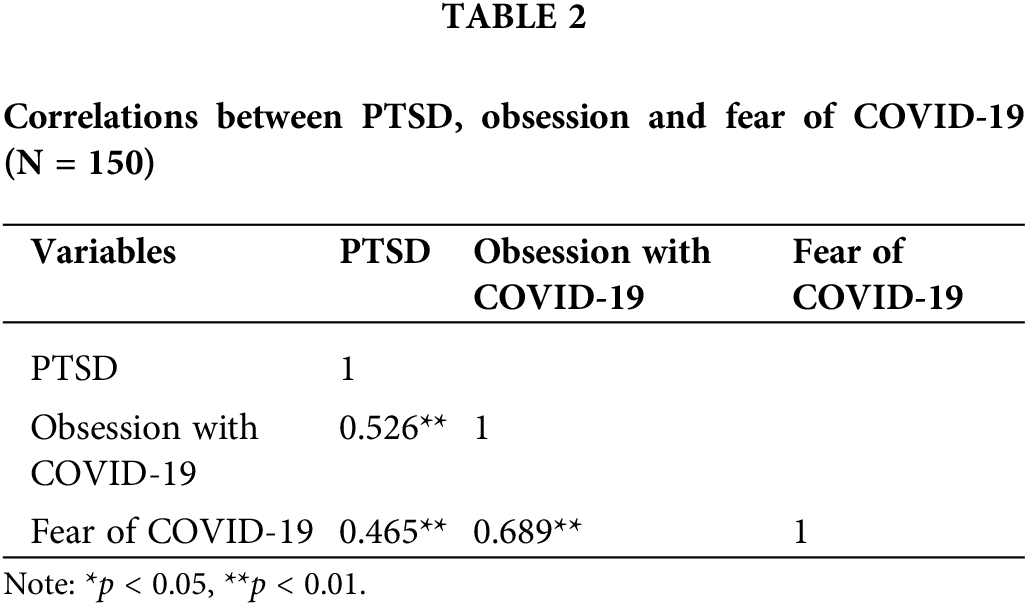
Table 2 shows the results correlation between participants’ PTSD symptoms, fear of COVID-19, and obsession with COVID-19. PTSD scores were significantly positively correlated with COVD-19 obsession (r = 0.526, p < 0.01) and COVID-19 fear (r = 0.465, p < 0.01). These data showed that higher PTSD scores were associated with higher fear of and obsession with COVID-19. In addition, obsession and fear were also significantly correlated (r = 0.689, p < 0.01).
Next, we performed a Mann-Whitney U test to compare scores between participants who had or had not experienced work related to COVID-19 (Table 3). There was a significantly higher fear of and obsession with COVID-19 in emergency rescue firefighters who had direct COVID-19 work experiences when compared with those who did not. On the other hand, it was confirmed to have no significant effect on PTSD (p = 0.067).
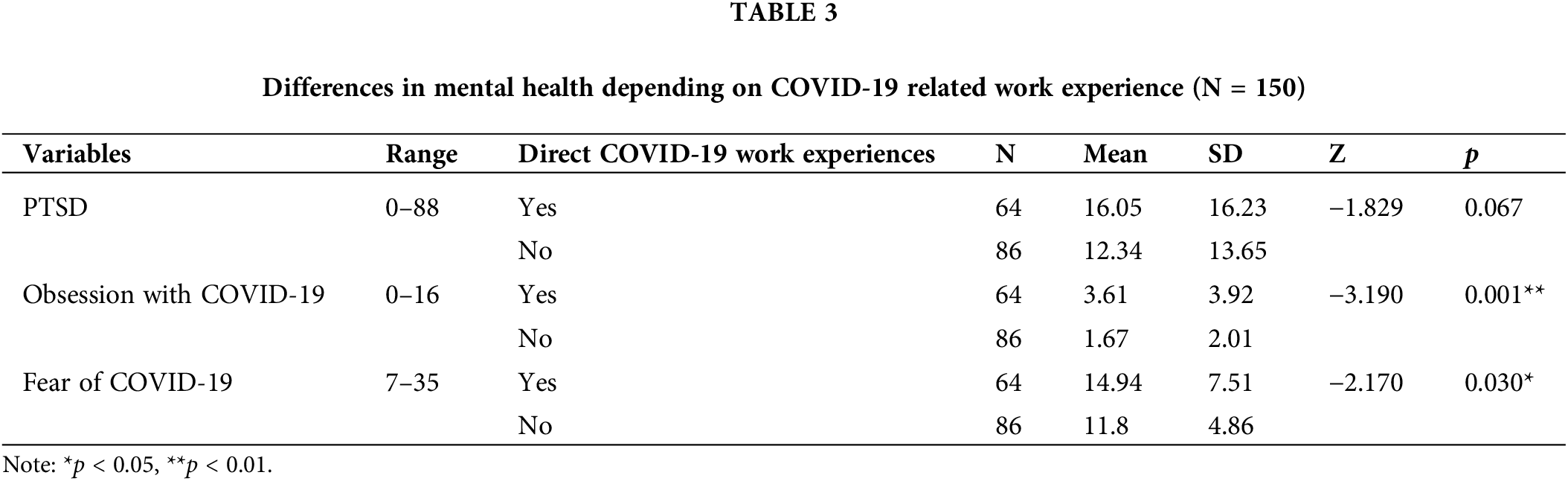
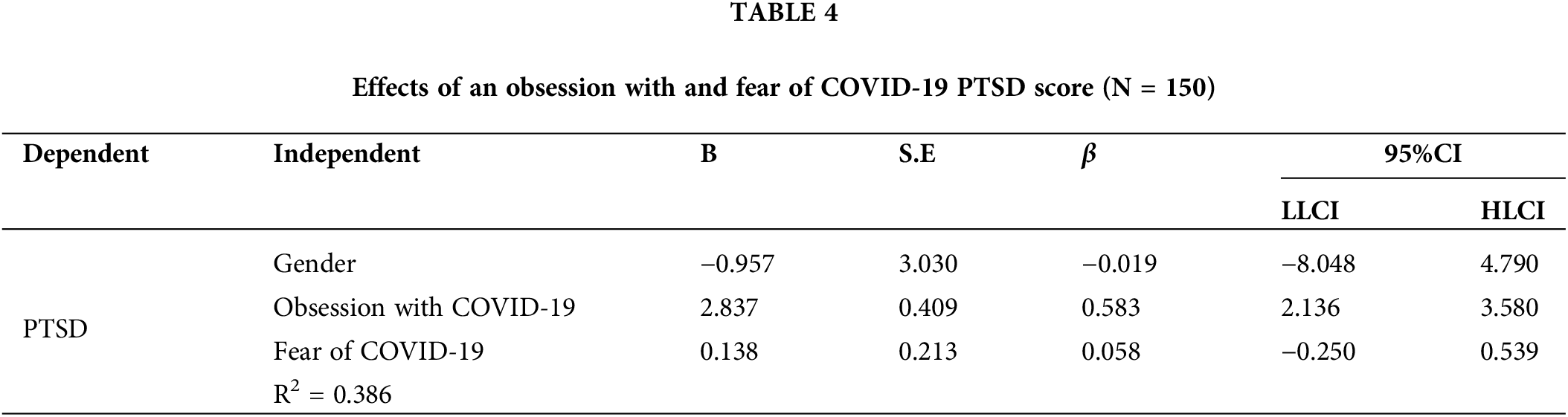
Table 4 shows the results of the regression analysis of the effects of fear of COVID-19 and obsession with COVID-19 on levels of PTSD. The data in this study is non-normality, to test our regression model, we used a Bayesian estimator rather than a maximum likelihood (ML) estimator. For non-normality data, Bayesian analysis is easier to estimate because it does not rely on normality assumptions and allows for more straightforward and exact inferences [13]. Based on Table 4, fear of COVID-19 did not have a significant effect on PTSD score (B = 0.138, 95%CI = [−0.250, 0.539]). By contrast, obsession with COVID-19 had a significant effect on the PTSD score (B = 2.837, 95%CI = [2.136, 3.580]); when the obsession with COVID-19 score increased by 1 point, the PTSD score increased by 2.837.
The purpose of this study was to identify the association between the degree of PTSD, fear of COVID-19, and obsession with COVID-19 in emergency rescue firefighters. The results of this study provide basic data to support the promotion of positive mental health in these individuals.
In this study, PTSD, obsession with COVID-19 and fear of COVID-19 were positively correlated; higher PTSD scores were associated with higher obsession with COVID-19 and fear of COVID-19 scores. These results are consistent with previous studies on the negative psychosocial impact of COVID-19 [14]. Additionally, they support previous studies that have shown high correlations in occupations working at the forefront of infectious diseases [14–16]. Emergency rescue firefighters interact with a large number of people without information on their health status. Further, they participate in various quarantine activities and support the ambulance service by providing additional patient transport options. These activities within their role can help to explain the research results in this study.
Participants in this study whose work was directly related to COVID-19 were more likely to have preoccupation and fear of COVID-19, which is consistent with findings from a study of nurses who cared for patients infected with COVID-19, who reported feeling very fearful during the pandemic [17]. In addition, social isolation and quarantine during a pandemic can lead to psychiatric symptoms such as depression, anxiety, obsessions, and PTSD [18]. Our findings are also supported by prior research that suggests that fear of contamination and obsession are more pronounced in people who are vulnerable to indiscriminate exposure to infectious diseases, such as the participants in this study [19]. Therefore, special management of the mental health of personnel who worked closely with COVID-19 is necessary.
As a result of a regression analysis of whether the fear and obsession with COVID-19 affected firefighters’ PTSD, it was found that only the obsession with COVID-19 affected PTSD. This is consistent with previous research showing that obsession in unpredictable situations, such as a pandemic, increases anxiety causing PTSD [20]. The obsession questionnaire used in this study included items such as “I could not stop thinking about the coronavirus” and “I kept thinking that I might be infected,” which may have contributed to the avoidance and emotional paralysis of PTSD. In addition, since group meetings were prohibited by law in Korea during the study period, it is believed that firefighters, the first community responders to COVID-19, had a strong compulsion to avoid infection while performing their duties. In this study, the results showed that fear of COVID-19 did not affect PTSD, which is contradictory to previous research [21,22]. However, this can be explained by linking it to previous findings that firefighters have a certain tolerance for emergencies and, in the case of COVID-19, a low disgust sensitivity, which means that firefighters have a lower fear of COVID-19 and can cope with it more easily [23]. In addition, because firefighters have experience in numerous trauma scenes, we cannot rule out the possibility that COVID-19 may have been less impactful than the traumatic events they are frequently exposed to.
This study is meaningful in examining the levels and association between obsession with COVID-19, fear of COVID-19, and PTSD in emergency rescue firefighters responding to the COVID-19 pandemic. Special attention should be paid to the mental health of emergency rescue firefighters because they are more likely to be exposed to traumatic events at work. Preventive measures should be taken to protect them from the negative consequences of these experiences. Furthermore, systematic interventions are required by developing a strategy and special program to promote positive mental health in emergency rescue firefighters. Policies should be established reflecting these conditions.
The limitation of this study is that it is difficult to generalize the results to all emergency rescue firefighters because it was conducted in one area using a cross-sectional approach. Therefore, future studies should be conducted with more participants across different regions. Follow-up studies should seek to understand the comprehensive mental health status of emergency rescue firefighters and study any mental health intervention strategies based on these characteristics.
This study confirmed that fear of COVID-19, obsession with COVID-19, and PTSD in emergency rescue firefighter were significantly correlated with each other. In particular, the fear of and obsession with COVID-19 was significantly higher in emergency rescue firefighters working direct on COVID-19-related activities than in those who had no direct work experience with COVID-19. We also looked at the variables that affect PTSD and found that fear of COVID-19 had no effect. At the same time, for obsessions, a 1-point increase in obsessions was associated with a 2.837 increase in PTSD.
This study suggests that it is essential to understand the mental health levels of firefighters’ direct work involvement in an epidemic situation such as COVID-19 and to understand the mental health status of obsessions. In addition, it is necessary to provide program and policy support to effectively control firefighters’ obsessions and fears of infectious diseases in preparation for possible future epidemic situations and to establish a broad support system by linking them with PTSD.
Acknowledgement: None to declare.
Funding Statement: This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No. NRF-2020R1A2B5B0100208).
Author Contributions: Study conception and design: C. and S. data collection: S. analysis and interpretation of results: C. and S. draft manuscript preparation: S. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Ethics Approval: The study was approved by Ethics Committee at the University of Chung-Ang (IRB number: 1041078-202011-HR-318-01). All participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Lin CY. Social reaction toward the 2019 novel coronavirus (COVID-19). Soc Health Behav. 2020;3(1):1–2. doi:10.4103/SHB.SHB_11_20. [Google Scholar] [CrossRef]
2. World Health Organization. Coronavirus disease (COVID-19) pandemic. WHO; 2020. Available from: https://www.who.int/emergencies/diseases/ novel-coronavirus-2019. [Accessed 2024]. [Google Scholar]
3. Liu S, Yang L, Zhang C, Xiang Y, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–8. doi:10.1016/S2215-0366(20)30077-8. [Google Scholar] [PubMed] [CrossRef]
4. Homayuni A, Hosseini Z, Shahabi N, Ezati R, Moayedi F. Quality of life and its related psychological problems during coronavirus pandemic. PLoS One. 2022;17(10):e0276841. doi:10.1371/journal.pone.0276841. [Google Scholar] [PubMed] [CrossRef]
5. Mirela A, Kathryn M, Kerri A, Saarah K. Obsessive-compulsive tendencies in a sample of veterans with posttraumatic stress disorder. J Cogn Psychother. 2019;33(1):33–45. doi:10.1891/0889-8391.33.1.33. [Google Scholar] [PubMed] [CrossRef]
6. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiat Res. 2020;288:112954. doi:10.1016/j.psychres.2020.112954. [Google Scholar] [PubMed] [CrossRef]
7. Nemati M, Ebrahimi B, Nemati F. Assessment of Iranian nurses’ knowledge and anxiety toward COVID-19 during the current outbreak in Iran. Arch Clin Infect Dis. 2020;15. doi:10.5812/archcid.102848. [Google Scholar] [CrossRef]
8. Yun SR. Correlations between nurses’ knowledge of COVID-19 and infection control compliance, resilience, and psychosocial well-being (Master Thesis). Chung-Ang University: Seoul, South Korea; 2020. [Google Scholar]
9. Ahorsu D, Lin C, Imani V, Saffari M, Griffiths M, Pakpour A. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020;20(3):1537–45. doi:10.1007/s11469-020-00270-8. [Google Scholar] [PubMed] [CrossRef]
10. Lee SH. Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Studies. 2020;44(7):393–401. doi:10.1080/07481187.2020.1748481. [Google Scholar] [PubMed] [CrossRef]
11. Eun HJ, Kwon TH, Lee SM, Kim TH, Choi MR, Cho SJ. A study on reliability and validity of the Korean version of impact of event scale-revised. J Korean Neuropsychiat Assoc. 2005;44(3):303–10. [Google Scholar]
12. Weiss DS, Marmar CR. The impact of event scale-revised. In: Wilson JP, Keane TM, editor. Assessing psychological trauma an PTSD. New York, NY: Guilford Press; 1997. p. 399–411. [Google Scholar]
13. Muthén B. Bayesian analysis in Mplus: a brief introduction. 2010. Available from: http://www.statmodel.com/download/IntroBayesVersion%203.pdf. [Accessed 2024]. [Google Scholar]
14. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr: Clin Res Rev. 2020;14(5):779–8. doi:10.1016/j.dsx.2020.05.035. [Google Scholar] [PubMed] [CrossRef]
15. Su TP, Lien TC, Yang CY, Su YL, Wang JH, Tsai SL. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. 2007;41(1–2):119–30. doi:10.1016/j.jpsychires.2005.12.006. [Google Scholar] [PubMed] [CrossRef]
16. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54(5):302–11. doi:10.1177/070674370905400504. [Google Scholar] [PubMed] [CrossRef]
17. Labrague LJ, de Los Santos JAA. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J Nurs Manag. 2021;29(3):395–403. doi:10.1111/jonm.13168. [Google Scholar] [PubMed] [CrossRef]
18. Erdoğan A, Hocaoğlu C. Psychiatric aspect of infectious diseases and pandemic: a review. Klinik Psikiyatri Dergisi. 2020;23(1):72–80. doi:10.5505/kpd.2020.90277. [Google Scholar] [CrossRef]
19. Moradi Motlagh M, Nainian M, Fata L, Fesharaki M, Ghaedi G. Investigation of the moderating role of perceived vulnerability to infectious diseases regarding the relationship between disgust and fear of contamination. Avicenna J Clin Med. 2019;26(1):34–43. doi:10.29252/ajcm.26.1.34. [Google Scholar] [CrossRef]
20. Gokhale MV, Chakole S. A review of effects of pandemic on the patients of obsessive-compulsive disorder. Cureus. 2022;14(10):e30628. doi:10.7759/cureus.30628. [Google Scholar] [PubMed] [CrossRef]
21. Edith F, Tanja M, Schäfer K, Roxanne M. COVID-19-related distress is associated with analogue PTSD symptoms after exposure to an analogue stressor. Eur J Psychotraumatol. 2022;13(2):1–11. doi:10.1080/20008066.2022.2127185. [Google Scholar] [PubMed] [CrossRef]
22. Chung M, Wang Y, Wu X, Wang N, Liu F, Ye Z, et al. Comparison between emerging adults and adults in terms of contamination fear, post-COVID-19 PTSD and psychiatric comorbidity. Curr Psychol. 2022;43(15):14075–86. doi:10.1007/s12144-022-03719-2. [Google Scholar] [PubMed] [CrossRef]
23. Coelho M, Suttiwan P, Arato N, Zsido N. On the nature of fear and anxiety triggered by COVID-19. Front Psychol. 2020;11:581314. doi:10.3389/fpsyg.2020.581314. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools