 Open Access
Open Access
ARTICLE
Citizens’ Mental Health Issues and Psychological Trauma Experience due to a Crowd-Crush Disaster in Korea
1 Red Cross College of Nursing, Chung-Ang University, Seoul, 06974, South Korea
2 Graduate School of Nursing and Professions, Chung-Ang University, Seoul, 06974, South Korea
3 Nursing Department, Graduate School of Chung-Ang University, Seoul, 06974, South Korea
* Corresponding Author: Yun-Jung Choi. Email:
International Journal of Mental Health Promotion 2024, 26(6), 439-447. https://doi.org/10.32604/ijmhp.2024.050458
Received 07 February 2024; Accepted 30 April 2024; Issue published 28 June 2024
Abstract
This study evaluated the state of anxiety, depression, post-traumatic stress disorder, general mental health, and mental well-being among citizens after a crowd-crush disaster in Korea. Individuals who experienced the crowd crush had significantly higher anxiety, depression, and post-traumatic stress disorder (PTSD) scores than those who did not (p < 0.001). Additionally, people who avoided the disaster area had significantly higher depression and PTSD scores than those who did not avoid the area (p < 0.001). Those who directly witnessed the Seoul Halloween crowd crush had a significant difference in PTSD levels in either group than those who experienced it indirectly (p = 0.005). There was a significant difference in PTSD scores in cases of direct damage or death of an acquaintance (p < 0.001). The Seoul Halloween crowd crush caused psychological damage through indiscriminate exposure to the public, and symptoms of PTSD appeared over a long period. It is crucial to provide essential resources for ongoing treatment and case management.Keywords
On October 29, 2022, a crowd crush occurred near the Hamilton Hotel in Itaewon, Seoul, Korea due to the numerous people participating in the Halloween festival. As a result of this accident, 196 people were injured and 159 people died [1].
At the time of the October 29 disaster at Itaewon, media related to the incident were spread mainly through SNSs, exposing people to scenes from the crowd crush without any filtering, thereby resulting in an indirect experience of the tragic incident [2]. The form and scale of such disasters are unpredictable, and the direct or indirect victims of disasters may experience post-traumatic stress or trauma reactions [3]. Trauma has differential effects on people and manifests in very different patterns, with symptoms ranging from mild to severe and brief to long-term. Therefore, the consequences of traumatic experiences must be examined from the beginning of life, and an approach that considers developmental tasks is necessary [4].
Recent studies have shown growing interest in delayed-onset post-traumatic stress disorder (PTSD), which is caused by delayed PTSD symptoms. The results show that a quarter of PTSD cases tend to be delayed and that PTSD symptoms may appear completely six months after a psychological traumatic event occurs [5]. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the definition of PTSD has been extended to the following: When one has experienced real death or death threats, serious conditions, and illnesses; when one has directly experienced sexual violence; when one knows that it has happened to a close family member or friend; or when one is repeatedly or extremely exposed to hateful details about a trauma case [6].
In addition to the severity of an event that causes psychological symptoms in individuals who have experienced a disaster, an individual’s subjective perception is interconnected with its influence on psychological distress [7]. Thus, PTSD not only has a high comorbidity with several mental disorders, including depression, panic, and anxiety, but also contributes to adaptive difficulties, including high levels of depression and anxiety [8]. However, longitudinal studies on individuals who have experienced disasters are limited, and studies confirming the psychological trauma status of survivors are even more limited. This study aimed to clarify the changes in the mental health status of people who have experienced trauma, as we investigate the mental health of those who directly or indirectly experienced the October 29 disaster and determine its impact nine months after the disaster.
This study used a cross-sectional design to determine the impact on the mental health of Korean citizens as of August 01, 2023, nine months after experiencing the traumatic event of the Seoul Halloween crowd crush on October 29, 2022.
The study participants comprised 301 adults living in Korea aged 19–69 years, who voluntarily agreed to participate.
General characteristics are defined as characteristics seen in trauma, including gender, age, occupation, residence area, family type, and experience of harm due to the Seoul Halloween crowd crush. Variables about alcohol were included, such as frequency of problematic drinking, changes in drinking frequency, and alcohol consumption. Traumatic experiences can lead to changes in alcohol consumption, most often associated with increased drinking behavior [9,10]. Avoiding area of the disaster and the reasons were also included. Avoidance is a symptom of post-traumatic stress disorder and refers to the tendency to run away from sensations, feelings, or thoughts that a person does not want to face [11].
The Generalized Anxiety Disorder Assessment-7 (GAD-7) is a self-report tool developed by Spitzer et al. [12] to screen for generalized anxiety disorders and evaluate the severity of symptoms [13]. It consists of seven questions on a four-point Likert scale from 0 to 3 to rate the anxiety experienced in the past two weeks. With a maximum score of 21 points, the threshold points for mild, moderate, and severe anxiety are 5, 10, and 15 points, respectively. Additional clinical treatment is recommended if the score is 10 or more [13]. The reliability of the tool was assessed in previous studies with Cronbach’s α ranging from 0.91 to 0.92 [12,14].
The Patient Health Questionnaire-9 (PHQ-9) was developed by Spitzer et al. [15] to aid in the diagnosis of mental disorders commonly encountered in primary clinical settings. It comprises nine questions that determine how much one has experienced specific problems in the past two weeks. Responses are evaluated on a four-point scale as follows: “not at all,” “for a few days,” “more than a week,” and “almost every day.” Total scores range from 0 to 27, and a score of 0–4 represents normality; 5–9, mild depression; 10–19, moderate depression; and 20–27, severe depression. The reliability of the tool was assessed in previous studies with Cronbach’s α ranging from 0.80 to 0.84 [16,17].
The Korean version of the Mental Health Continuum Short Form (K-MHC-SF) is a self-report mental well-being scale, which was adapted and validated by Lim et al. [18] from Keyes et al. [19]. It consists of 14 questions on a six-point Likert scale. There are three subscales, consisting of emotional, psychological, and social well-being, and they are evaluated as Flourishing, Moderately Mentally Healthy, and Languishing [18]. The reliability of the tool was assessed in previous studies as Cronbach’s α ranging from 0.91 to 0.93 [18,20].
Shin [21] adapted and validated the Korean version of the General Health Questionnaire-20 (GHQ-20). This self-report tool was developed by identifying and typifying factors related to mental health problems in the current health status of general patients [21]. This scale consists of 20 questions rated on a four-point Likert scale, with scores ranging from 0 to 80 [21]. The threshold is 13 points or higher, and it is classified as “abnormal” or “normal”. The reliability of the tool was assessed in previous studies as Cronbach’s α ranging from 0.82 to 0.94 [22,23].
The Korean Version of the Impact of Event Scale-Revised (IES-R-K) was adapted and validated by Eun et al. [24], based on the Event Impact Scale, a trauma-related scale developed by Horowitz et al. [25]. The frequency of symptoms over the past week is assessed using 22 questions, with responses evaluated on a five-point scale. Total scores range from 0 to 88, with scores of 24 or less denoting normal status and 25 or more denoting PTSD [24,26]. The reliability of the tool was assessed in previous studies with Cronbach’s α ranging from 0.83 to 0.93 [24,27].
In order to eliminate the influence of other traumatic events, the researcher added the question, “Are you aware that this survey is about the Seoul Halloween crowd crush?”. In addition, no specific geographic restrictions were set for this study. The Seoul Halloween crowd crush was a catastrophic tragedy that affected a particular region, which could have led to bias if the survey was limited to the Seoul metropolitan area.
An online survey was conducted from July 28 to August 01, 2023 on those who were willing to participate in the study. The survey took approximately 15 min.
This study was approved by the Chung-Ang University Ethics Committee (IRB No. 1041078-20221129-HR-019). The questionnaire provided informed consent, and all participants signed the informed consent in this study. The researchers explained the study to the participants and conducted the survey only among those who consented to participate. They explained that the data would be used only for research purposes and that anonymity and confidentiality would be maintained. Moreover, the participants were informed that they could withdraw their participation at any time if they wished without any disadvantages. Participants were given a small reward for their participation.
The data were analyzed using SPSS 25.0. The probability of statistical significance was set at p < 0.05. The general characteristics of the participants were analyzed using frequency analysis and Cronbach’s α. Differences in the distribution of severity of mental health variables according to participants’ experiences of the Seoul Halloween crowd crush were confirmed using chi-square tests. Differences in mental health variables according to general characteristics were investigated using independent t-test and one-way analysis of variance. Scheffe’s test was performed for post-hoc analysis.
Table 1 presents the summary statistics of the general characteristics of the 301 participants. While 33.2% were men, 66.8% were women, with 45.8% being in the age group of 19–29 years; 34.6%, in the age group of 30–39 years; 15.6%, in the age group of 40–49 years; 2.7%, in the age group of 50–59 years; and 1.3%, in the age group of 60 years and above. Among the participants, 74.1% were employed, 4.3% were unemployed, and 21.6% were students. Moreover, 69.8% lived in Seoul and metropolitan cities, whereas 30.2%. lived in other regions. Regarding the family type, 33.2% lived alone, 11.6% lived with a spouse or partner, 4.7% lived with dependents, 22.9% lived with a spouse and children, and 28.6% lived with parents or siblings.
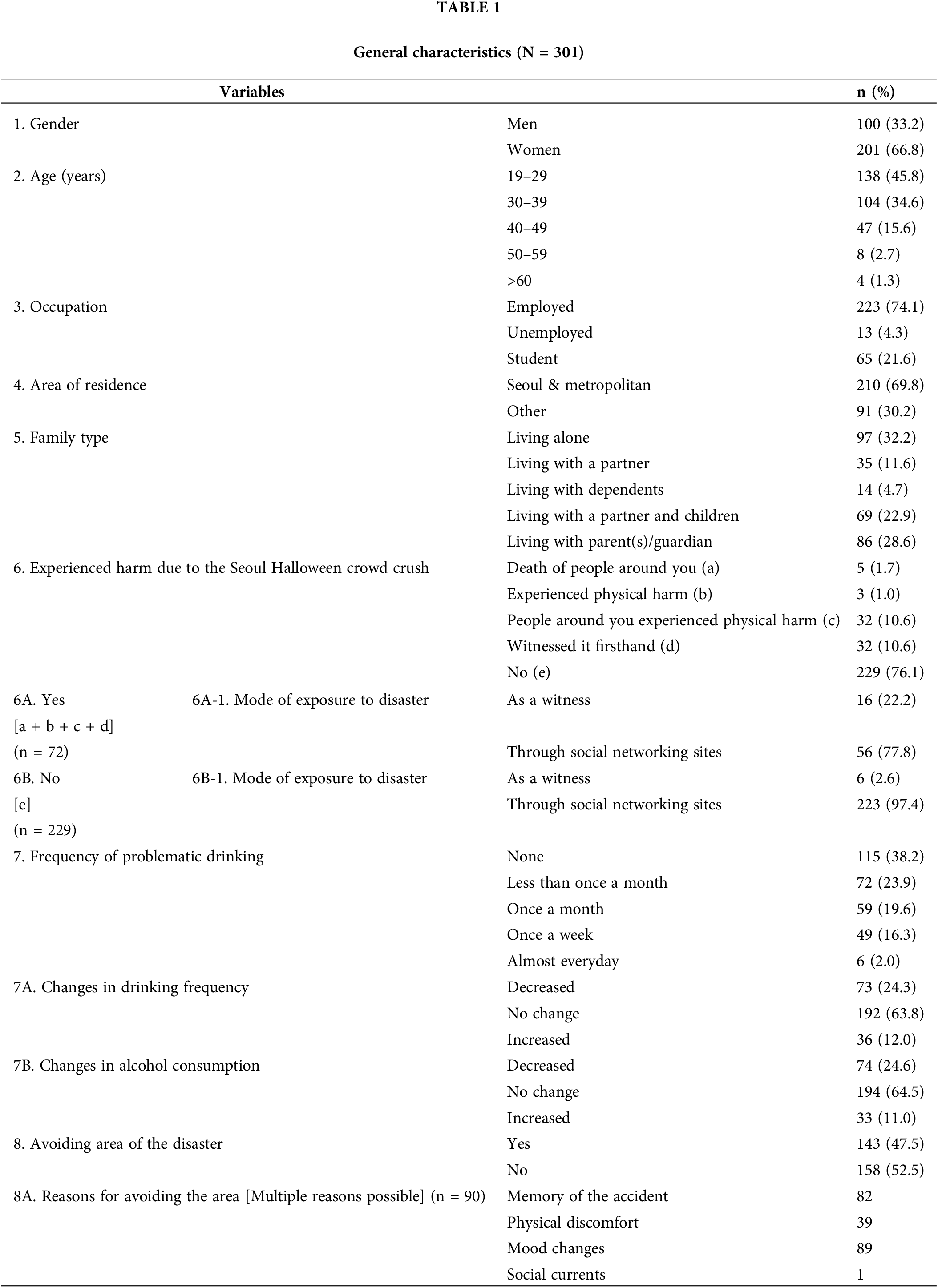
Table 2 reports the comparison of the mental health indicators based on whether the participants experienced harm due to the Seoul Halloween crowd crush. Among the related scales, anxiety (p < 0.001), depression (p < 0.001) and PTSD (p < 0.001) showed significant differences. Among those who experienced harm due to the Seoul Halloween crowd crush, 72.3% were found to have depression; among those who did not experience harm, 26.6% were found to have depression. Regarding PTSD, 72.2% of those who experienced harm due to the disaster were classified as high-risk, while 21.8% of those who did not experience harm were classified as high-risk.
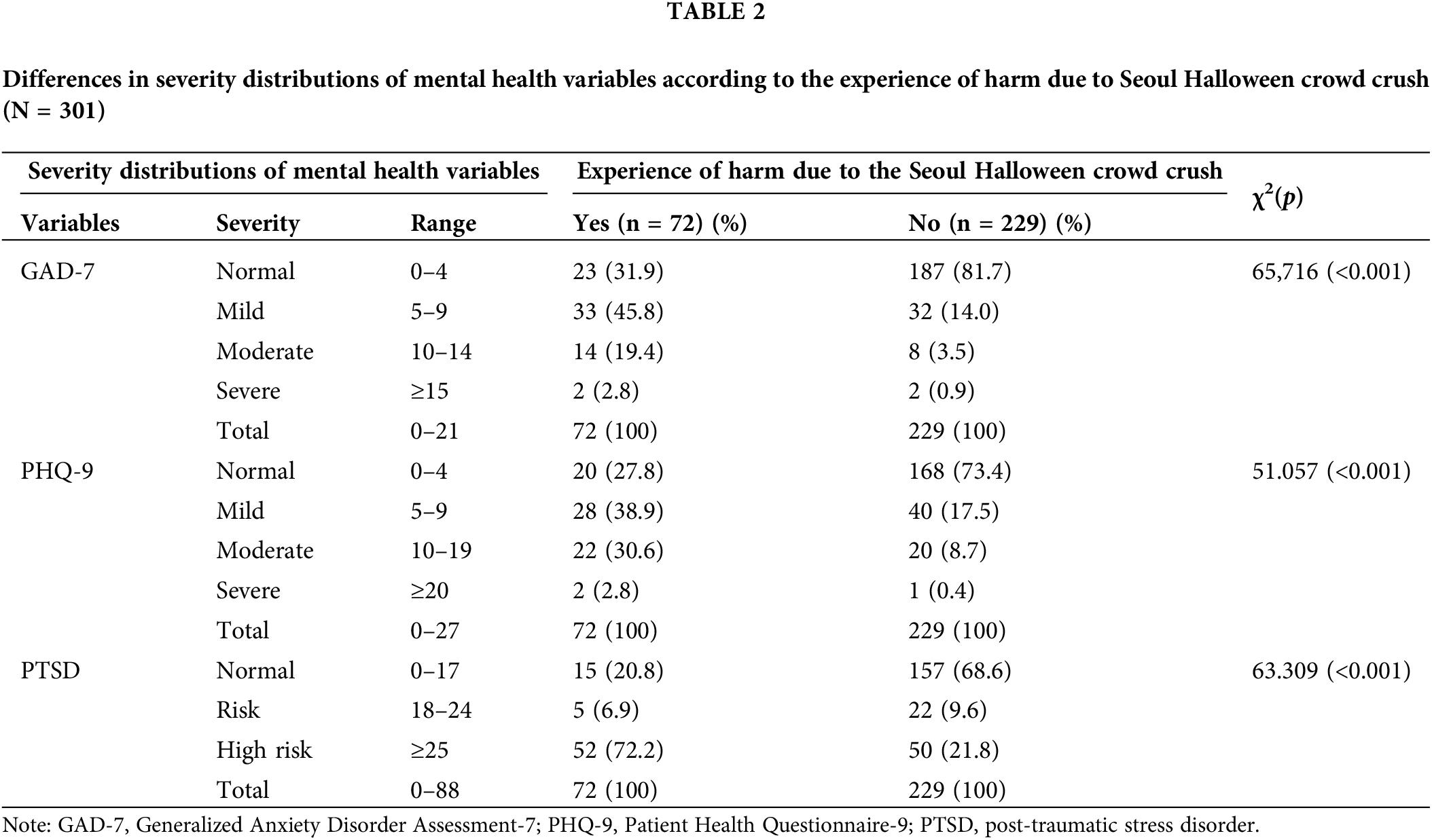
Table 3 compares the mental health indicators based on participants’ experience of avoiding the Itaewon area. Among the scales related to avoidance, those that showed significant differences were anxiety (p < 0.001), depression (p < 0.001) and PTSD (p < 0.001). Among the participants who avoided the disaster area, 56.0% were found to have depression, while 20.9% of those who reported not avoiding the area were found to have depression. Moreover, 57.3% of the participants who avoided the disaster area were classified as high-risk on the PTSD index, while 8.2% of those who reported not avoiding the area were classified as high-risk.
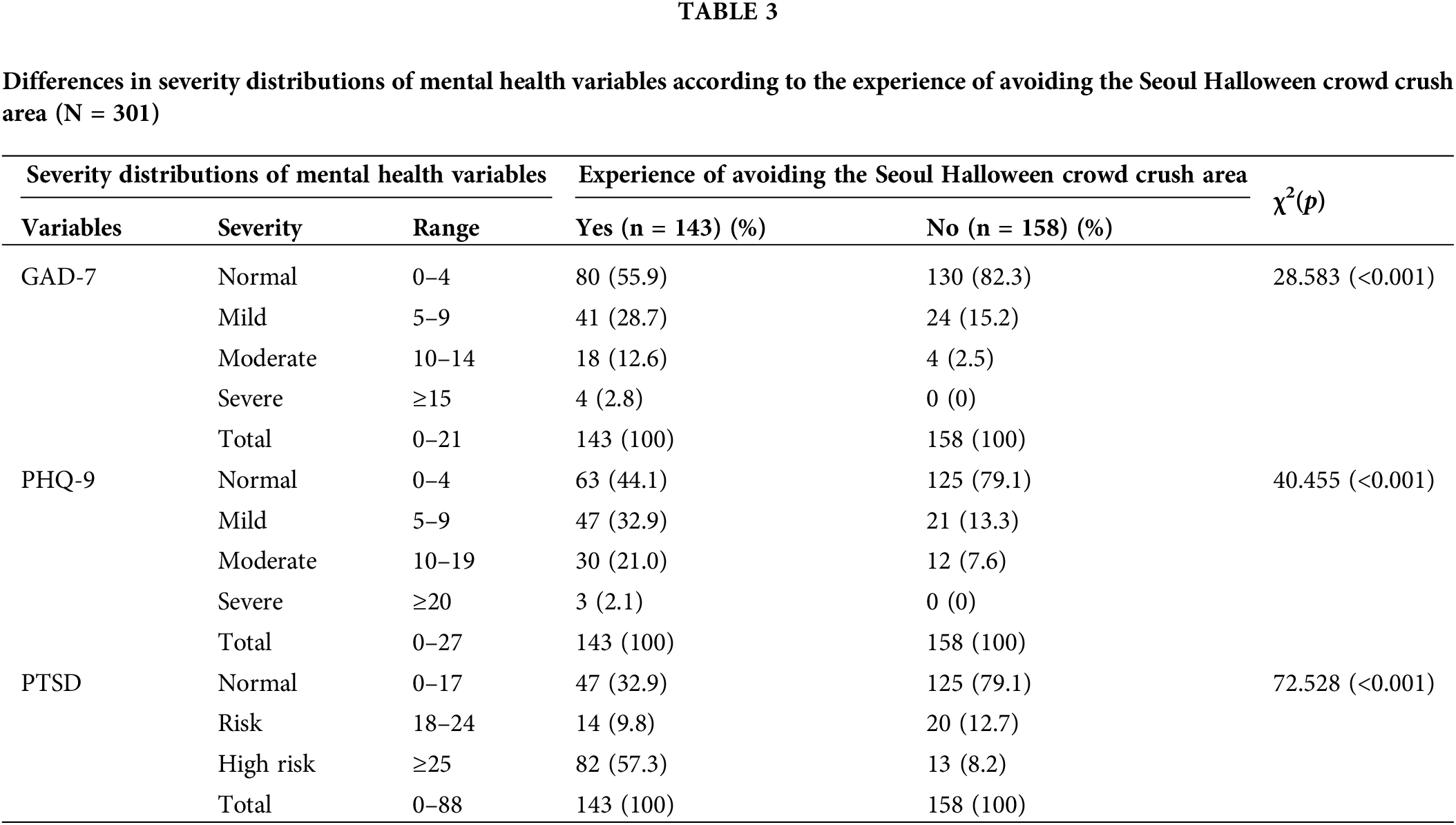
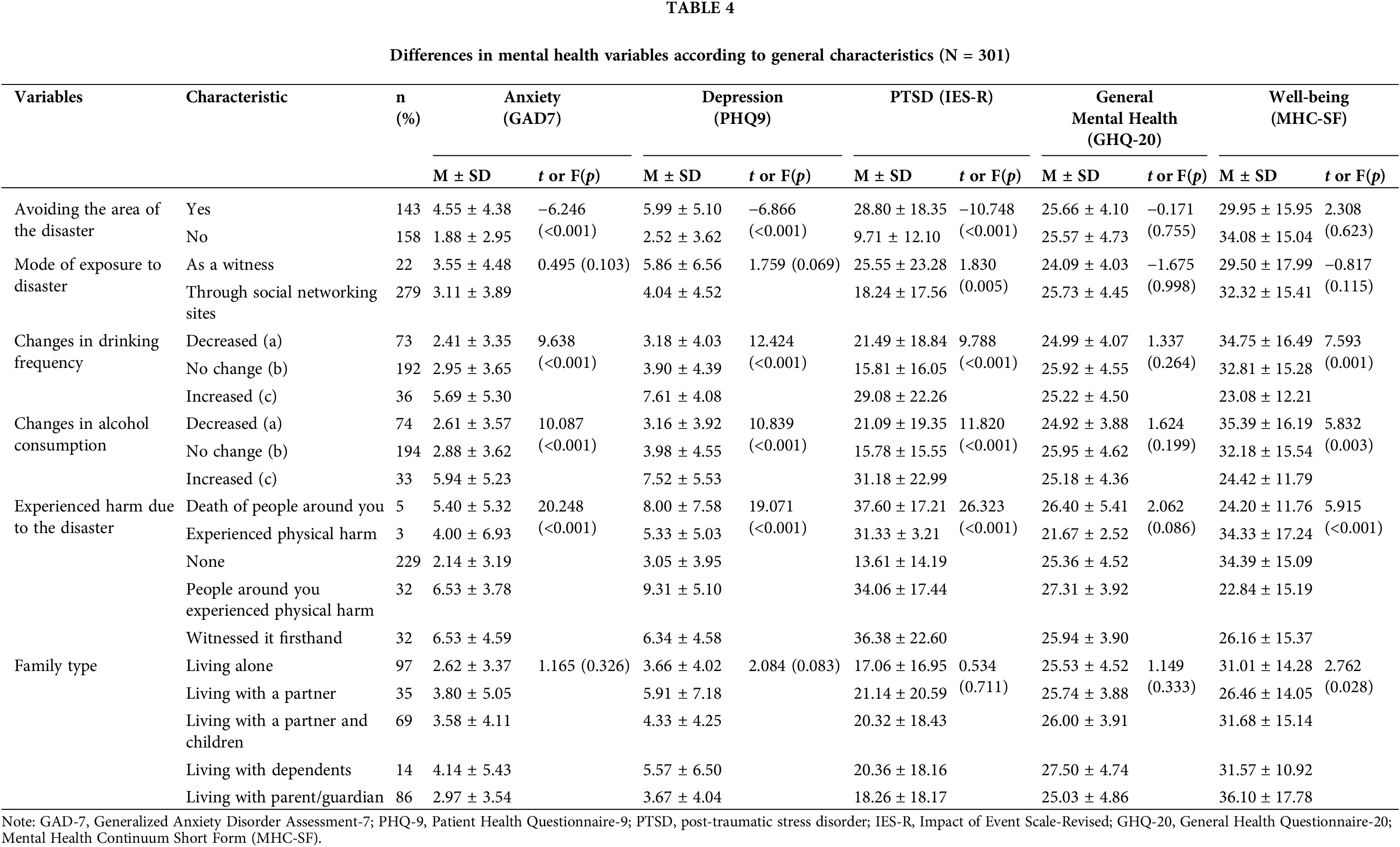
Table 4 compares the mental health variables based on participants’ general characteristics. Significant differences were observed in anxiety (p < 0.001), depression (p < 0.001), and PTSD (p < 0.001) with respect to avoiding the affected area. With regard to the mode of exposure to the disaster (witness/SNS), there was a significant difference in PTSD (p = 0.005). There was a significant difference in anxiety (p =< 0.001), depression (p < 0.001), PTSD (p < 0.001), and well-being (p = 0.001) with regard to the changes in drinking frequency; and in anxiety (p < 0.001), depression (p < 0.001), PTSD (p < 0.001) and well-being (p = 0.003), with regard to the changes in drinking consumption. Regarding their experience of harm, there were significant differences between the groups in anxiety (p < 0.001), depression (p < 0.001), PTSD (p < 0.001) and well-being (p < 0.001). With regard to family type, there was a significant difference between the groups on the well-being scale (p = 0.028).
This study assessed the degree of anxiety, depression, PTSD, general mental health, and mental well-being of participants who experienced the Itaewon crowd crush disaster on October 29, 2022. The variables of interest included changes in drinking frequency and alcohol consumption quantity, family type, experience of harm due to the disaster, mode of exposure to the disaster, and avoidance of the disaster area. We now discuss the findings based on our analyses.
First, in this study, anxiety, depression and PTSD among people who experienced harm due to the disaster were more severe than among those who did not experience harm, and there was a significant difference between the groups. This supports previous findings that show that patients with PTSD have a 65% chance of being diagnosed with major depressive disorder [28]. In particular, social support is an important factor in improving the mental health of people who have experienced a disaster; however, when an individual’s acquaintance or family member dies or experiences harm, their support system may be impaired, and subsequently, their post-traumatic stress is found to be serious. This means that those who have experienced a disaster also experience the loss of meaningful relationships because of the injury or death of a close neighbor or a family member [29]. The loss of social relationships among those who experience such disasters is a risk factor for their mental health and return to daily life [30]. Among these changes, parts that can be recovered may be easily recovered, but those that cannot be recovered may have a lasting impact on the daily lives of disaster survivors [31]. Ultimately, because humans live in complex interactions with the various layers of the surrounding environment, even if a disaster has a direct impact in terms of human casualties and economic and psychological damage to one’s life, its aftereffects can occur as a result of one’s entire life being intertwined [4,32]. According to a study conducted on 3,010 people who had experienced a disaster, the extent of recovery from disaster damage was related to whether or not there was physical injury [4]. Thus, people who have experienced disasters directly or indirectly may have their social networks impaired, their resilience may be reduced, and consequently, they may experience mental health difficulties. To improve the resilience of those who have experienced disaster, a system needs to be developed to strengthen their social network.
Second, 82 people (57.3%) responded with “memory of the accident” and 39 (27.3%) responded with “physical discomfort,” when referring to the reasons for avoiding the area after the disaster. This indicates various physical, psychological, and cognitive reactions such as nightmares, insomnia, anxiety about recurrence, helplessness, and re-experience or recollection of trauma experiences that disaster survivors generally undergo [33–35]. Among the various symptoms of PTSD, survivors may experience flashbacks, in which painful and terrible memories of the trauma are revived, making them believe that they are back again in the time and space of the trauma [36]. Flashbacks are a major symptom experienced by those who have experienced disasters [37]. According to a study on the Gangwon forest fire, 33.3% of those who experienced the disaster experienced vivid flashbacks, and 76.2% responded that they experienced somatization symptoms [38]. This figure was much higher in the group that experienced the disaster than in the group that did not [38]. People who experience flashbacks feel embarrassed that they have no control over their condition [37]. Somatization symptoms are one of the most common symptoms among those who have experienced disasters. Traumatic stress activates the sympathetic nervous system and triggers a stress response in the neuroendocrine system, leading to physical symptoms that are more frequent in individuals with depression and PTSD [39]. The mental health problems of individuals complaining of these symptoms can persist for a long time. For example, in case of the Ash Wednesday bushfires in Australia, a study found that the criteria for PTSD and depression were met even 12 and 20 months after the disaster [33]. Similar to the findings of previous studies, we found that depression and PTSD in those who have experienced disasters may cause various symptoms that may not be resolved in a short period of time. To support people with ongoing mental health crises, it is crucial to establish a system to provide mental health services along with continuous case management.
Third, those who experienced the Seoul Halloween crowd crush showed changes in drinking frequency and consumption, depending on anxiety, depression, PTSD, and mental well-being. PTSD is closely related to addiction and is one of the factors underlying a wide range of addiction issues, including not only alcohol addiction but also behavioral addictions such as to drugs [40]. In previous studies, alcohol use was reported to be very high in groups with PTSD symptoms; more than one in three people with disaster experiences used alcohol as a means of self-treatment to reduce psychological pain and PTSD symptoms, and the more severe the symptoms, the more severe the alcohol use disorder [40,41]. The general interpretation is that alcohol is used as a means of self-healing to overcome the pain caused by the initial trauma and that problematic drinking behavior continues subsequently owing to the individual’s dependence on or addiction to alcohol [42]. According to a study comparing PTSD and problematic drinking patterns of Korean individuals divided into disaster experience and control groups (197 people each), disasters not only caused an increase in simple drinking but also increased the tendency of PTSD and alcohol use disorder afterwards by about four times [43]. According to Reifels et al. [29], those who have experienced disasters are likely to experience problems due to alcohol use disorders; moreover, problematic drinking was found to increase the prevalence of mental disorders over the lifetime of those who have experienced disasters. This indicates that people who have experienced disasters choose alcohol as a means to achieve psychological stability, which has been known to lead to secondary problems. To prevent this, measures for preventing drinking must be included in disaster management systems.
This study has several limitations. First, it was difficult to accurately determine the mental health of the high-risk groups because the evaluation was conducted using a self-report questionnaire in which those who experienced trauma were asked to determine their own mental health. Second, longitudinal data on the mental health assessment of the participants could not be collected; therefore, it was not possible to determine how their mental health changed over time. Third, the disaster experience in this study may not be representative of other types of disaster experience, and our analysis included both participants with direct and indirect experiences, making it difficult to obtain results by type of experience. As the study progressed, we identified the need for research on survivors of varied types of disasters at different points in time.
The main finding of this study was that there were differences in depression, post-traumatic stress, general mental health, and mental well-being among those who experienced direct and indirect harm due to the Seoul Halloween crowd crush disaster and those who did not. Those who had experienced the disaster were also indiscriminately exposed to it through social media. And there were differences in the PTSD scores depending on the exposure type. Consequently, people avoided the affected area owing to reliving the experience and physical discomfort; the frequency and amount of drinking were also affected. There was a significant difference in the levels of mental health problems among those who had experienced the disaster.
As this study investigates the state of mental health nine months after the Seoul Halloween crowd crush, our findings are meaningful as not just a simple survey but also because they provide essential data to improve the mental health of those who experienced the disaster. Therefore, instead of providing one-time support, a government-wide system is needed for the continuous treatment of psychological trauma and the restoration of social networks of those who experienced harm due to the disaster. Therefore, this study provides the basic data required to improve the mental health of those who experienced the Seoul Halloween crowd crush.
Acknowledgement: The authors would like to thank Hee-Won Song and Na-Rae Lee for their support in the survey process and statistical advice.
Funding Statement: This research was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korean government (NRF-2023R1A2C2003043), and the Chung-Ang University Research Scholarship Grants in 2023.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Choi; data collection: Choi; analysis and interpretation of results: Choi and Kwak; draft manuscript preparation: Kwak; manuscript revision: Choi and Namgung. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research supporting data is not available.
Ethics Approval: This study was approved by the Chung-Ang University Ethics Committee (IRB No. 1041078-20221129-HR-019). The questionnaire provided informed consent, and all participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Korean Neuropsychiatric Association. Activate the government-wide disaster response headquarters and respond with all the government’s power to resolve the accident and take prompt action; 2022a. Available from: https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=373425. [Accessed 2023]. [Google Scholar]
2. Korean Neuropsychiatric Association. What parents (caregivers) can do for children who have seen shocking photos or videos related to the Seoul Halloween crowd crush in the media. Available from: https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=373425. [Accessed 2023]. [Google Scholar]
3. Wang SJ. Safety in mass gathering: basic survey for crowd crush. J Korean Soc Disaster Secur. 2023;16(1):49–60. [Google Scholar]
4. Lim HS, Nam DY, Lee KY. The moderating effect of local community resilience on the level of recovery of disaster victims. Korean Soc Welf Surv. 2022;75:5–30. [Google Scholar]
5. Glaesmer H, Sierau S, Bottche M. Die Konsequenzen traumatischer Erfahrungen. Trauma Gewalt. 2020;4:266–76. [Google Scholar]
6. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington DC: American Psychiatric Pub Inc.; 2013. doi:10.1176/appi.books.9780890425596. [Google Scholar] [CrossRef]
7. Kim JY, Kim SH, Heo S, Donghun L. Trauma types and psychological symptoms in Korean adults. Rehabil Psychol. 2023;30(2):219–45. [Google Scholar]
8. Geng F, Zhou Y, Liang Y, Zheng X, Li Y, Chen X, et al. Posttraumatic stress disorder and psychiatric comorbidity among adolescent earthquake survivors: a longitudinal cohort study. J Abnorm Child Psychol. 2018;46:1–11. [Google Scholar]
9. Fetzner MG, McMillan KA, Sareen J, Asmundson GJ. What is the association between traumatic life events and alcohol abuse/dependence in people with and without PTSD? Findings from a nationally representative sample. Depress Anxiety. 2011;28(8):632–8. doi:10.1002/da.20852. [Google Scholar] [PubMed] [CrossRef]
10. Guliyev C, Kalkan Ö., Tekin K, Tuna ZO, Ögel K. Comparison of individuals with and without the risk of post-traumatic stress disorder in terms of substance use features and psychological problems according to their substance preferences. Alpha Psychol. 2021;22(3):153–8. [Google Scholar]
11. Brereton A, McGlinchey E. Self-harm, emotion regulation, and experiential avoidance: a systematic review. Arch Suicide Res. 2020;24(sup1):1–24. doi:10.1080/13811118.2018.1563575. [Google Scholar] [PubMed] [CrossRef]
12. Kroenke KRL, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi:10.1001/archinte.166.10.1092. [Google Scholar] [PubMed] [CrossRef]
13. Mun M, Shin J, Yoo Y, Ahn C, Lee H. Mental health of asymptomatic or mildly symptomatic COVID-19 patients in the Seoul metropolitan city community treatment center: cross sectional analysis of depression, anxiety, trauma experience, and suicidal tendency. Anxiety Mood. 2022;18(2):101–8. [Google Scholar]
14. Seo JG, Park SP. Validation of the generalized anxiety disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain. 2015;16:97. doi:10.1186/s10194-015-0583-8. [Google Scholar] [PubMed] [CrossRef]
15. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–44. doi:10.1001/jama.282.18.1737. [Google Scholar] [PubMed] [CrossRef]
16. Park GY. Reliability, validity, and clinical utility of the Korean version of Patient Health Questionnaire-9 (PHQ-9). Glob Health Sci Pract. 2017;7(2):71–8. [Google Scholar]
17. Park SJ, Choi HR, Choi JH, Kim KW, Hong JP. Reliability and validity of the Korean version of the depression screening tool (Patient Health Questionnaire-9, PHQ-9). Korean J Anxiety Med. 2010;6(2):119–24. [Google Scholar]
18. Lim YJ, Ko YG, Shin HC, Cho YR. Validation study of the Korean version of the Mental Well-being Scale (MHC-SF). J Korean Psychol Assoc: Gen. 2012;31(2):369–86. [Google Scholar]
19. Keyes CLM, Wissing M, Potgieter JP, Temane M, Kruger A, van Rooy S. Evaluation of the mental health continuum-short form (MHC-SF) in setswana-speaking South Africans. Clin Psychol Psychother. 2008;15(3):181–92. doi:10.1002/cpp.572. [Google Scholar] [PubMed] [CrossRef]
20. Lim YJ. Psychometric characteristics of the Korean mental health continuum-short form in an adolescent sample. J Psychoeduc Assess. 2014;32(4):356–64. doi:10.1177/0734282913511431. [Google Scholar] [CrossRef]
21. Shin SI. Study on the development of the Korean version of the General Mental Health Scale (KGHQ) I—Focusing on KGHQ-20 and KGHQ-30. Korean Soc Welf. 2001;46:210–35. [Google Scholar]
22. Bratås O, Grønning K, Forbord T. Psychometric properties of the hospital anxiety and depression scale and the general health questionnaire-20 in COPD inpatients. Scand J Caring Sci. 2014;28(2):413–20. doi:10.1111/scs.12054. [Google Scholar] [PubMed] [CrossRef]
23. Nunnally J, Bernstein I. Psychometric theory. New York: McGraw-Hill; 1994. [Google Scholar]
24. Eun HJ, Kwon TW, Lee S, Kim TH, Choi MR, Jo SJ. A study on the reliability and validity of the revised (Korean version) of the event impact scale. Neuropsychiatry. 2005;44(3):303–10. [Google Scholar]
25. Horowitz M, Wilner N, Alvarez W. Impact of event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–18. doi:10.1097/00006842-197905000-00004. [Google Scholar] [PubMed] [CrossRef]
26. Kim HS, Park GR, Lee HJ. Influencing factors on incident shock for firefighters. Korean J Crisis Manag. 2013;9(5):1–16. [Google Scholar]
27. Jeong BS, Lee SW, Lee JS, Yoo JH, Kim GU, Jo SY, et al. The psychometric properties of the Korean version of the verbal abuse questionnaire in university students. Psychiatry Investig. 2015;12(2):190–6. doi:10.4306/pi.2015.12.2.190. [Google Scholar] [PubMed] [CrossRef]
28. Gallagher MW, Brown TA. Bayesian analysis of current and lifetime comorbidity rates of mood and anxiety disorders in individuals with posttraumatic stress disorder. J Psychopathol Behav Assess. 2015;37(1):60–6. doi:10.1007/s10862-014-9436-z. [Google Scholar] [PubMed] [CrossRef]
29. Reifels L, Mills K, Dückers MLA, O’Donnell ML. Psychiatric epidemiology and disaster exposure in Australia. Epidemiol Psychiatr Sci. 2019;28(3):310–20. doi:10.1017/S2045796017000531. [Google Scholar] [PubMed] [CrossRef]
30. Kim JS, Lee SY. Protective and risk factors that influence PTSS and comorbidity of natural disaster victims. Korean J Health Psychol. 2022;27(1):1–26. [Google Scholar]
31. Lim HS, Sim K. The effects of life changes on post-traumatic stress disorder after disasters. Stress. 2018;26(4):319–26. doi:10.17547/kjsr.2018.26.4.319. [Google Scholar] [CrossRef]
32. Bronfenbrenner U. Ecology of the family as a context for human development: research perspectives. Dev Psychol. 1986;22(6):723–42. doi:10.1037/0012-1649.22.6.723. [Google Scholar] [CrossRef]
33. Bryant RA, Gibbs L, Gallagher HC, Pattison P, Lusher D, MacDougall C, et al. Longitudinal study of changing psychological outcomes following the Victorian black Saturday bushfires. Aust N Z J Psychiatry. 2018;52(6):542–51. doi:10.1177/0004867417714337. [Google Scholar] [PubMed] [CrossRef]
34. Psarros C, Theleritis C, Economou M, Tzavara C, Kioulos KT, Mantonakis L, et al. Insomnia and PTSD one month after wildfires: evidence for an independent role of the ‘fear of imminent death’. Int J Psychiatry Clin Pract. 2017;21(2):137–41. doi:10.1080/13651501.2016.1276192. [Google Scholar] [PubMed] [CrossRef]
35. Papanikolaou V, Adamis D, Mellon RC, Prodromitis G. Psychological distress following wildfires disaster in a rural part of Greece: a case-control population-based study. Int J Emerg Ment Health. 2011;13(1):11–26. [Google Scholar] [PubMed]
36. Bourne C, Mackay CE, Holmes EA. The neural basis of flashback formation: the impact of viewing trauma. Psychol Med. 2013;43(7):1521–32. doi:10.1017/S0033291712002358. [Google Scholar] [PubMed] [CrossRef]
37. Jeon YS. Christian counseling understanding of flashbacks of psychological trauma and application of cognitive behavioral therapy strategies. Theol Pract. 2021;74:331–57. [Google Scholar]
38. Hong JS, Hyun SY, Lee JH, Sim M. Mental health effects of the Gangwon wildfires. BMC Public Health. 2022;22(1):1183. doi:10.1186/s12889-022-13560-8. [Google Scholar] [PubMed] [CrossRef]
39. Ursano RJ, Fullerton CS, Weisaeth L, Raphael BJ. Individual and community responses to disasters. In: Ursano RJ, Fullerton CS, Weisaeth L, Raphael BJ, editors. Textbook of disaster psychiatry. Cambridge, UK: Cambridge University Press; 2017. p. 1–24. [Google Scholar]
40. Levin Y, Bar-Or RL, Forer R, Vaserman M, Kor A, Lev-Ran S. The association between type of trauma, level of exposure and addiction. Addict Behav. 2021;118:106889. doi:10.1016/j.addbeh.2021.106889. [Google Scholar] [PubMed] [CrossRef]
41. Fulerton CS, Mckibben JB, Reissman DB, Scharf T, Kowalski-Trakofler KM, Shultz JM, et al. Posttraumatic stress disorder, depression, and alcohol and tobacco use in public health workers after the 2004 Florida hurricanes. Disaster Med Public Health Prep. 2013;7(1):89–95. doi:10.1017/dmp.2013.6. [Google Scholar] [PubMed] [CrossRef]
42. Lee S, Kim E, So M. Status and intervention of alcohol use disorder after disaster. Addict Psychiat. 2015;19(1):23–8. [Google Scholar]
43. Shim GO. Relationship between increased alcohol consumption, PTSD, and depression in disaster victims: risk and protective factors. J Korean Psychol Assoc: Addict. 2019;4(1):19–30. [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools