 Open Access
Open Access
ARTICLE
The Impact of Sleep Determination on Procrastination before Bedtime: The Role of Anxiety
1 School of Sociology and Ethnology, University of Chinese Academy of Social Sciences, Beijing, 102488, China
2 School of Mental Health, Wenzhou Medical University, Wenzhou, 325000, China
3 Institute of Psychosocial Services, Kangning Hospital of Wenzhou Medical University, Wenzhou, 325000, China
4 Postgraduate School, Harbin Sport University, Harbin, 150008, China
* Corresponding Author: Wanli Zang. Email:
International Journal of Mental Health Promotion 2024, 26(5), 377-387. https://doi.org/10.32604/ijmhp.2024.047808
Received 18 November 2023; Accepted 20 March 2024; Issue published 30 May 2024
Abstract
Objective: The importance of good sleep for energy recovery and overall physical and mental health cannot be overstated. However, the increasing competitiveness of society, diversifying lifestyles, and the rapid spread of the internet and electronic devices have significantly impacted people’s sleep patterns, particularly through bedtime procrastination. Therefore, this study aims to investigate the relationship and underlying mechanisms between sleep determination, anxiety, and bedtime procrastination among the Chinese population. Method: The study utilized data from a national survey—the China Residents’ Sleep Condition Survey (November 2021, with 6,037 participants). By constructing mediation and moderation models, it analyzed the relationship and mechanisms between sleep determination and bedtime procrastination, highlighting the dual role of anxiety: as a mediator between sleep determination and bedtime procrastination, and as a moderator of their relationship. Results: There was a negative correlation between sleep determination and bedtime procrastination; anxiety was related to an increase in bedtime procrastination behaviors; In the interplay between sleep determination and pre-bedtime procrastination, the regulatory effect of anxiety is found to be more pronounced than its intermediary role, with anxiety significantly diminishing the inverse relationship between sleep determination and procrastination before bedtime. Conclusion: Bedtime procrastination can lead to sleep issues, thus reducing sleep quality. Enhancing sleep determination or alleviating pre-sleep anxiety can help inhibit bedtime procrastination behaviors. Intervening and reducing bedtime procrastination is one of the effective measures to improve sleep quality.Keywords
Sleep, a fundamental human need and a key physiological factor in regulating homeostasis [1], plays a critical role in cognitive functioning and overall physical and mental health [2–4]. Adequate sleep duration is an essential indicator of sleep quality, which has been extensively studied [5,6]. Persistent poor sleep quality can lead to numerous physiological and psychological issues, such as impaired bodily functions [7], depression, anxiety, and reduced brain activity and functionality [8]. However, with increasing societal competition, diversification of lifestyles, and the rapid proliferation of the internet and electronic devices, bedtime procrastination has emerged as a prevalent phenomenon in the sleep process. Smartphone addiction, in particular, has been shown to have a significant positive correlation with bedtime procrastination [9,10]. The relationship between bedtime procrastination and sleep quality and health is intimately connected. Existing research has linked bedtime procrastination with poorer subjective and objective sleep metrics, higher daytime fatigue, poorer mental health, and shorter sleep duration [11,12]. Bedtime procrastination, a widespread issue of self-regulation failure, leads to insufficient sleep, thereby compromising sleep quality. Therefore, this study, conducted in November 2021 with a national sample, regards bedtime procrastination as a contributing factor to insufficient or poor sleep quality [13]. It aims to investigate its influencing factors and underlying mechanisms, with the goal of proposing targeted interventions to reduce bedtime procrastination behaviors and enhance sleep quality.
Bedtime procrastination, defined as the voluntary delay of an intended course of action despite expecting to be worse off for the delay, has been introduced into the field of health behavior by Kroese as a specific type of procrastination associated with insufficient sleep, thereby impacting physical health [14]. Kroese defines bedtime procrastination as ‘failing to go to bed at the intended time while no external circumstances prevent a person from doing so [13].’ This definition specifically refers to procrastination before going to bed, not after getting into bed. Subsequent measures used in studies inquire about the respondents’ intentions and specific behavioral routines but exclude related activities like using smartphones, gaming, or reading. Procrastination, including bedtime procrastination, involves a gap between intention and action and can indicate a failure in self-regulation due to poor behavioral self-control [14]. Bedtime procrastination is negatively correlated with self-regulation [9,13]. Numerous studies support this, with most researchers agreeing that bedtime procrastination is a result of poor self-control leading to self-regulatory failure [13–15]. They conceptualize self-control as a finite resource. In daily life, each act requiring self-control depletes this ability, and the depleted self-control resource continues to govern subsequent behaviors, making one more susceptible to impulses and temptations. This depleted state is termed ego depletion [16,17]. Since the decision to go to sleep typically occurs at the end of the day when self-control is weakest and psychological energy is low, this often leads to self-regulation failure and delayed sleep, making bedtime procrastination likely [18]. Kamphorst’s research supports this notion, showing that individuals who resist temptations throughout the day are more prone to bedtime procrastination. He explains this relationship through the ‘cumulative effect’ of resisting desires, leading to the ‘depletion of self-regulatory resources,’ meaning after resisting these temptations, individuals lack sufficient self-regulatory resources to resist entertainment temptations before bed [15]. Baumeister emphasizes self-regulation as a behavioral capacity, while Kamphorst views it as a resource [17]. Though their perspectives slightly differ, both ultimately agree that bedtime procrastination results from an inability to resist temptations (i.e., unintentional bedtime procrastination behaviors).
The influence of variables related to self-regulation on bedtime procrastination has been substantiated. Boredom, a variable associated with self-regulation failure, exacerbates procrastination and negatively impacts sleep quality [19–21]. Boredom triggers impulses to escape the feeling, leading to situations where tired individuals refuse to go to bed and instead seek engaging activities [22]. Furthermore, research has demonstrated a positive correlation between physical activity and self-regulation [23]. Thus, physical activity may connect to bedtime procrastination through self-regulation. Additionally, physical activity has been shown to enhance sleep quality [24,25]. In the context of the mechanisms linking self-regulation and bedtime procrastination, Kadzikowska-Wrzosek suggests that poor self-regulatory capabilities may lead to delays in the sleep-wake rhythm, consequently increasing the tendency towards bedtime procrastination [12].
Bedtime procrastination and anxiety
Bedtime procrastination is linked to emotional self-regulation. Sirois and colleagues have suggested that failures in self-regulation might relate to short-term emotional repair and emotion regulation [26]. When individuals prioritize short-term goals such as emotional repair over long-term objectives, they are more likely to postpone tasks. Unpleasant emotional states often shift focus towards managing one’s negative emotions. This form of emotion regulation, specifically short-term emotional repair, represents unsuccessful self-regulation and can perpetuate procrastinatory behaviors. In other words, negative emotions lead to procrastination [27,28]. Building on this, Sirois et al. proposed that self-compassion is associated with less bedtime procrastination, with low negative emotions being more critical than high positive emotions in this relationship. The impact of self-compassion on bedtime procrastination is partly mediated by cognitive reappraisal, an adaptive emotional regulation strategy [29]. Bedtime procrastination is also related to anxiety and depression. Empirical studies have shown that negative emotions significantly predict individual bedtime procrastination behaviors, with anxiety being a manifestation of negative emotions [30]. In essence, the more anxiety experienced, the more severe the bedtime procrastination. Chung et al. confirmed a positive correlation between bedtime procrastination and depressive symptoms [31]. Furthermore, Cui and colleagues collected survey data from 1,181 Chinese university students at two time points 12 months apart, covering problematic smartphone use, bedtime procrastination, sleep quality, and depressive symptoms. They employed a cross-lagged model to examine the longitudinal relationships among these variables. The study found that bedtime procrastination unidirectionally predicts subsequent depressive symptoms [32]. Given the close association between anxiety or stressors and the occurrence of depressive symptoms [33], it is posited that there is a correlative relationship between bedtime procrastination and anxiety.
Bedtime procrastination and sleep determination
In addressing the gap between intention and behavior in sleep behaviors, Kroese introduces the concept of ‘self-regulation failure’ and identifies three reasons for the divergence between intentions and actions: 1. Lack of required skills or resources; 2. A tendency towards immediate gratification over long-term benefits, leading to impulsive tendencies; 3. Compensatory health beliefs (e.g., ‘I plan to diet tomorrow, so I can overindulge today’), where the original intention is neither implemented nor abandoned but remains intact for other occasions [34]. However, our study posits a different perspective from most research on bedtime procrastination: the discrepancy between intention and action might simply be due to insufficient strength of intention. Therefore, a variable that can substitute for behavioral intention and possesses a stronger motivational force is needed to explain behavior realization. Sleep determination refers to the strong desire and resolve an individual develops in the pursuit of good sleep. It can replace behavioral intention to explain individual actions. Sleep determination places greater emphasis on the individual’s internal willingness and resolve, reflecting the importance and firmness they attribute to good sleep and can motivate individuals to take proactive actions to reduce bedtime procrastination and improve sleep habits. Compared to behavioral intention in traditional theory of planned behavior, sleep determination is more stable and enduring, less susceptible to external influences and others. Hence, sleep determination serves as a significant factor in explaining individual behavior. The intensity and stability of sleep determination help explain why some people maintain good sleep behaviors, while others fall into bedtime procrastination and poor sleep habits. This understanding is crucial for improving individual sleep behaviors.
The moderating role of anxiety
The Theory of Reasoned Action [35], proposed by American scholars Fishbein and Ajzen in 1977, posits that individual behavior is driven by behavioral intentions, which are in turn determined by two factors: the individual’s attitude towards the behavior and subjective norms regarding the behavior. It assumes that personal intention is the primary prerequisite for behavior; the stronger the intention to perform a behavior, the greater the likelihood of its execution. This theory presupposes a critical assumption: individuals are rational and, prior to engaging in a behavior, they consider the significance and consequences of their actions by integrating various pieces of information, and the behaviors they perform are within their control. However, in real life, people are often influenced by various factors such as material conditions and living environments. Therefore, the practical applicability of this theory is significantly reduced when faced with situations or external objective factors beyond personal control. Given this special premise of the Theory of Reasoned Action, and the fact that in the real world, people’s behaviors are often subject to many external influences [36], Ajzen introduced the Theory of Planned Behavior in 1985 [37]. This theory incorporated a new variable, ‘perceived behavioral control,’ referring to an individual’s perception of their control capabilities, such as information control and resource control. However, the Theory of Planned Behavior also has its limitations. While it considers the level of perceived behavioral control, building upon its predecessor, it fails to account for the emotional aspects of the individual. See Fig. 1. Based on this, we wished to explore whether there are differences in the effect of behavioral intention (sleep determination) on behavior (bedtime procrastination) across anxiety states.
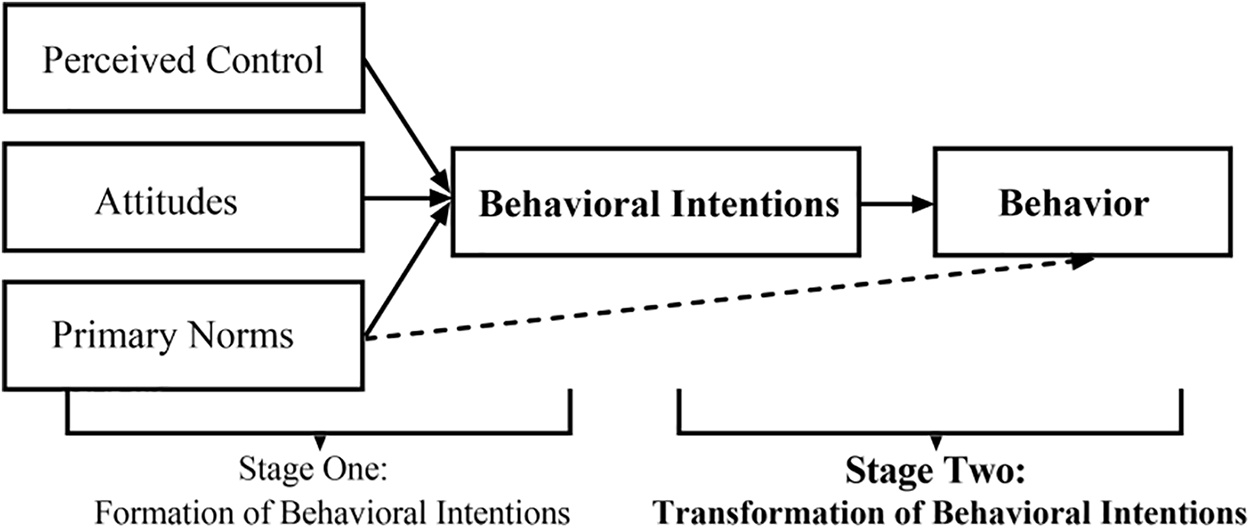
Figure 1: Conceptual diagram of the theory of reasoned action.
Therefore, this study divides the Theory of Planned Behavior into two stages: the formation of behavioral intention and the transformation of behavioral intention. It focuses on verifying whether the transformation stage of this theory is applicable in the domain of sleep behavior within the field of health behavior (see Fig. 2). Specifically, the study examines whether an individual’s sleep determination has any impact on bedtime procrastination behaviors. Additionally, considering the influence of individual emotional states on behavior, the study introduces anxiety—a common negative emotion in modern society—as a mediating factor between sleep determination and bedtime procrastination. On the one hand, we aim to explore the role of anxiety in the transformation process from intention to behavior; on the other hand, we seek to explain the gap between the strength of intention and behavior through different pathways. This approach aims to enrich the research on the influencing factors and mechanisms of bedtime procrastination.
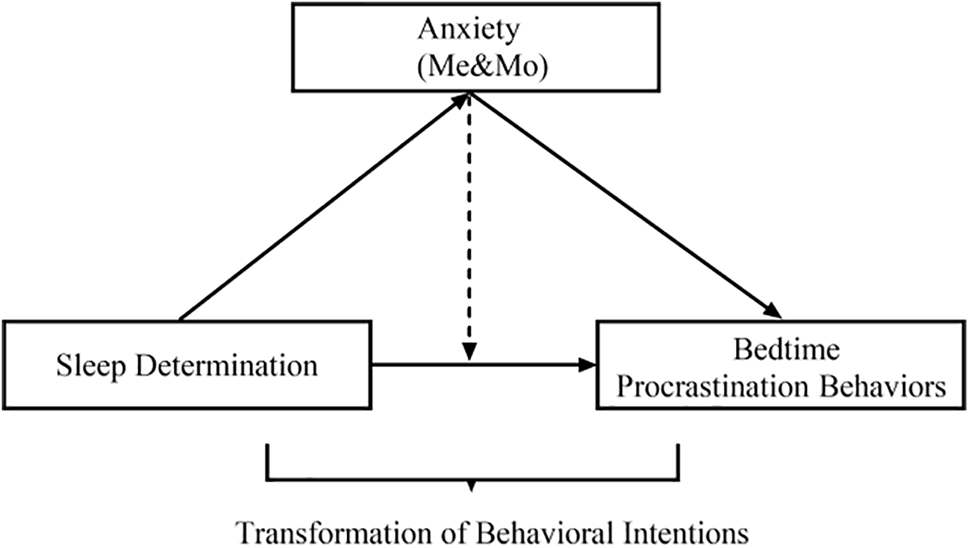
Figure 2: Structural framework of the current study.
In summary, this study approaches from a psychological perspective, focusing firstly on exploring the relationship between sleep determination and bedtime procrastination based on the Theory of Planned Behavior. Secondly, following the research logic of how emotions affect the intention-behavior process, we conduct a multi-faceted exploration of the mechanisms by which sleep determination influences bedtime procrastination. Based on the foregoing discussion, this study proposes three hypotheses:
Hypothesis 1: There is a negative correlation between sleep determination and bedtime procrastination.
Hypothesis 2: Anxiety mediates the relationship between sleep determination and bedtime procrastination.
Hypothesis 3: Anxiety negatively moderates the relationship between sleep determination and bedtime procrastination.
Sample design and participants
This study utilizes data from the China Residents’ Sleep Condition Survey conducted in November 2021 by the Institute of Sociology, Chinese Academy of Social Sciences. This research was sanctioned by the academic board of the Institute of Sociology at the Chinese Academy of Social Sciences. All participants signed the informed consent in this study. Using a probability proportionate to size (PPS) sampling method and based on the population and economic development levels of each province as detailed in the ‘China Statistical Yearbook (2021)’ (National Bureau of Statistics, 2021), sampling quotas for each province were determined. The survey sampled adults aged 18 to 71, with the final sample covering 27 provinces, autonomous regions, and municipalities, excluding Tibet, Ningxia, Qinghai, Hainan, and Hong Kong, Macao, and Taiwan. Before completing the online questionnaire, respondents were presented with a page of text explaining the survey’s purpose and significance, assuring confidentiality of their information, and requesting honest responses based on their actual situations. Trap questions and logic tests were incorporated to ensure data quality. After excluding invalid questionnaires, a total of 4,196 valid samples were obtained.
The dependent variable in this study is bedtime procrastination. The assessment of bedtime procrastination behavior is systematically performed utilizing the Bedtime Procrastination Scale (BPS) [13], a validated instrument developed by Kroese et al. [38]. This scale comprises nine items, such as “I go to bed later than I had intended,” “Even if I don’t have to get up early the next day, I will still go to bed early,” “If it’s time to turn off the lights and go to sleep, I do it right away,” “I often do other things when it’s time to sleep,” “Even if I am very sleepy, I can easily get distracted by other activities,” “I do not go to bed at a regular time,” “I have a regular bedtime,” “I want to go to bed on time, but I just can’t seem to do it,” and “If it’s time to sleep, I can easily stop what I’m doing.” Responses range from “almost never” to “always,” scored as 1, 2, 3, 4, and 5 respectively. Items 2, 3, 7, and 9 are scored in reverse. Given that previous research suggests the scale has a unifactorial structure, the average score of these nine items is often used as the overall scale score. The questionnaire’s Cronbach’s alpha coefficient is 0.853, indicating good internal consistency. The scale ranges from 1 to 5, with higher scores indicating more frequent bedtime procrastination behaviors. Bedtime procrastination is treated as a continuous variable in this paper.
The independent variable is sleeping determination. In this study, we measured the intensity of behavioral intentions related to sleep actions using three items: “I am willing to sacrifice sleep time for work or study,” “I am willing to sacrifice sleep time for leisure activities,” and “I am not willing to sacrifice sleep time for any reason.” These items are designed to reflect the participants’ perceived importance of sleep and their determination to safeguard their sleep time. A Likert 5-point scoring method is employed, where “1 = Strongly agree, 2 = Somewhat agree, 3 = Neutral, 4 = Somewhat disagree, 5 = Strongly disagree.” Scores for each item range from 1 to 5. The third item of the scale is reverse-scored, and behavioral intention is represented by the average score of three items, ranging from 1 to 5. Higher scores indicate stronger sleep determination, that is, a more intense intention to ensure adequate sleep. Sleep determination is also considered as a continuous variable in this study.
The mediating/moderating variable is anxiety. In this study, we employed the revised General Health Questionnaire (GHQ-20) by Li et al. [39], tailored to the psychological characteristics of the Chinese population. The questionnaire comprises 20 items divided into three dimensions: depression, anxiety, and self-affirmation. Each item is answered with a binary choice: “yes” or “no.” The total score is calculated by summing the item scores, resulting in a psychological health score ranging from 0 to 20. Additionally, the depression dimension contains six items, with scores ranging from 0 to 6; the anxiety dimension has five items, with scores from 0 to 5; and the self-affirmation dimension includes nine items, with scores from 0 to 9. Higher scores indicate higher levels of depression, anxiety, and self-affirmation. The questionnaire’s Cronbach’s alpha coefficient is 0.752, indicating good internal consistency. Research suggests that daily emotional states are remarkably stable over time, and half of the variability in daily emotions can be attributed to trait-level qualities [40], which supports the questionnaire and measurement approach we used for assessing anxiety. In our study, we only utilized the anxiety dimension and is treated as a continuous variable.
Descriptive statistical analysis was utilized to conduct an overall assessment of bedtime procrastination, sleep determination, and anxiety among participants. The relationship between these three primary variables was examined through correlational analysis. Multivariate linear regression and hierarchical regression were employed to analyze the effects of sleep determination and anxiety, both individually and collectively, on bedtime procrastination after controlling for demographic characteristics. The mediating effect of anxiety was tested using a Bootstrap sampling method with 1,000 iterations. Additionally, hierarchical regression analysis was used to examine the mediating effect of anxiety. In this study, the threshold for statistical significance was set at p < 0.1.
Demographic characteristics of the participants
The participants in this study had an average age of 29.17 ± 0.14 years, with 2,422 males (57.72%) and 1,774 females (42.28%). Educational levels (N = 4,196) were categorized as follows: junior high school or below (3.32%), high school (5.65%), vocational/technical school (7.84%), junior college (23.09%), undergraduate (50.45%), graduate or above (9.65%). Marital status (N = 4,170) was divided into single (52.09%), first marriage with a spouse (42.64%), remarried with a spouse (1.68%), divorced (1.41%), widowed (0.38%), and cohabiting (1.80%). Household registration (N = 4,141) was classified into local non-agricultural (42.84%), local agricultural (27.65%), non-local non-agricultural (12.22%), and non-local agricultural in urban areas (17.29%). Subjective social class (N = 4,196) was distributed as lower (1.36%), lower-middle (12.82%), middle (44.16%), upper-middle (30.41%), and upper (11.25%). Furthermore, participants’ personal monthly income, family income, employment, and work status were also detailedly differentiated. In subsequent data analyses, these demographic characteristics were controlled as covariates to eliminate the influence of extraneous variables on the research outcomes.
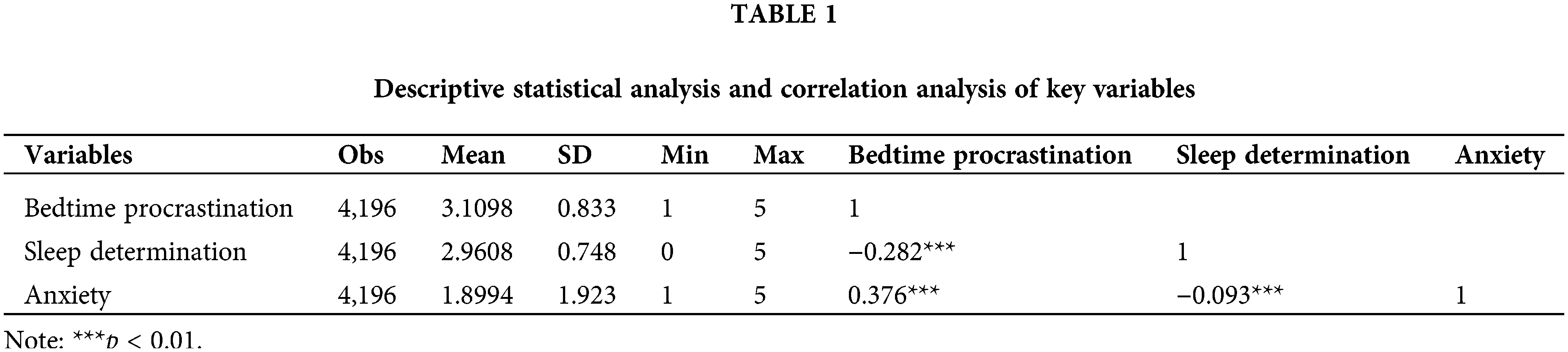
Descriptive statistics and correlation analysis
As indicated in Table 1, the average score for bedtime procrastination is slightly above the median, suggesting the presence of bedtime procrastination behaviors among the public, though not to a severe extent. The average score for sleep determination is slightly below the median. The average score for anxiety is below the median, indicating a generally low level of anxiety among the public. However, the large standard deviation in anxiety scores (SD = 1.92) suggests a polarization in the population, with some individuals experiencing little to no anxiety and others experiencing high levels of anxiety. Additionally, correlational analysis reveals that sleep determination is significantly negatively correlated with bedtime procrastination (r = −0.282), anxiety is significantly positively correlated with bedtime procrastination (r = 0.376), and there is a significant negative correlation between sleep determination and anxiety (r = −0.093).
Upon examination, the Variance Inflation Factor (VIF) for anxiety and sleep determination was found to be 1.01, well below the threshold of 10, indicating that there is no significant collinearity between sleep determination and anxiety. This result validates the feasibility of constructing subsequent models and testing hypotheses. Consequently, a multiple regression analysis was conducted on the variables.
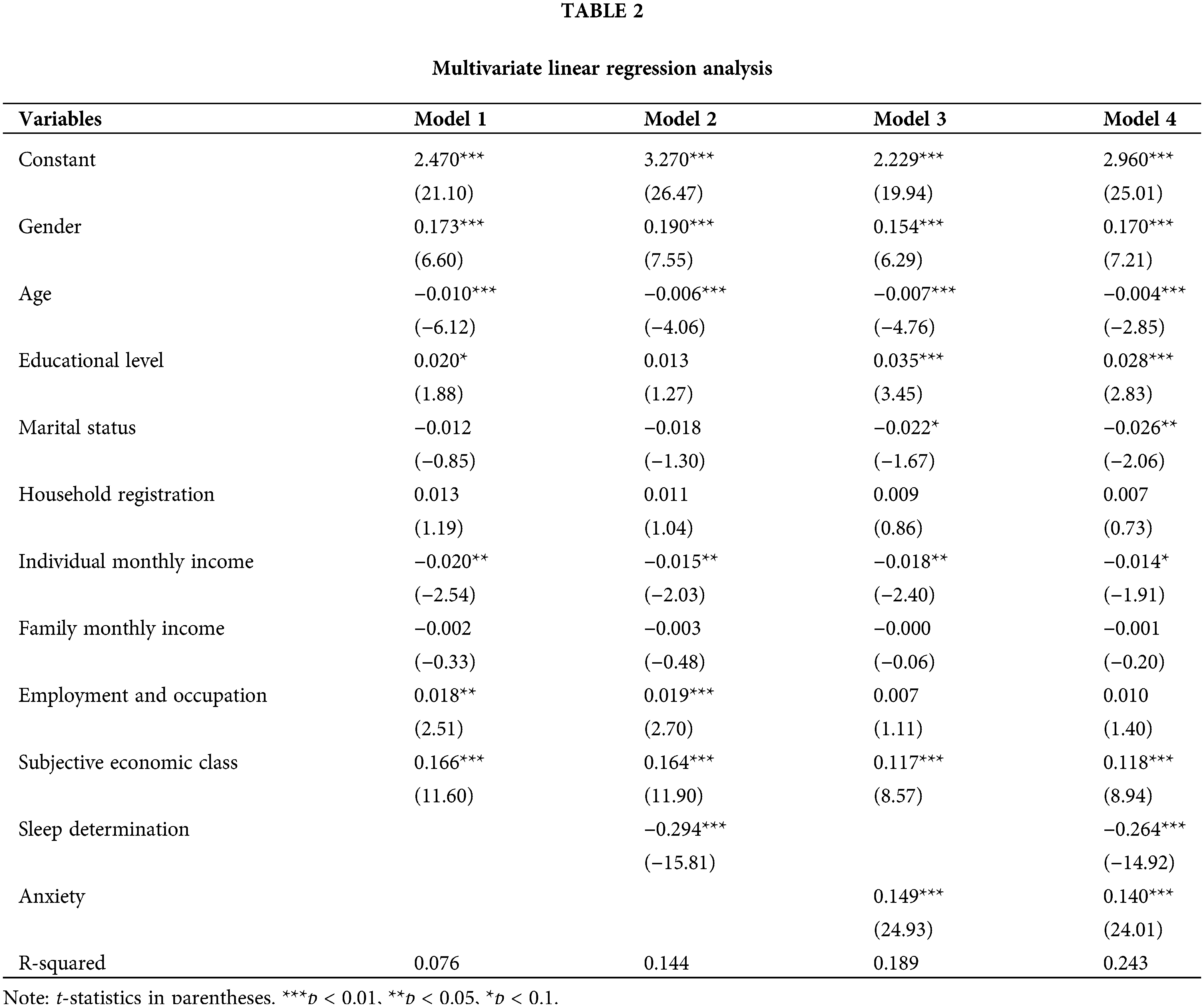
As shown in Table 2, Model 1, which incorporates control variables (gender, age, education level, marital status, household registration, individual and family monthly income, employment, work, and subjective economic class), accounts for 7.6% of the variance in bedtime procrastination. Model 2, which adds sleep determination to Model 1, explains 14.4% of the variance in bedtime procrastination, indicating that sleep determination independently explains 6.8% of this variance. Model 3 adds anxiety to Model 1 and accounts for 18.9% of the variance, with anxiety independently explaining 11.3% of the variance in bedtime procrastination. Model 4, which includes both sleep determination and anxiety, explains 24.3% of the variance in bedtime procrastination, indicating a combined explanatory power of 16.7% for these factors. This is less than the sum of their individual explanatory powers (18.1%), suggesting an interference effect between sleep determination and anxiety. It is hypothesized that anxiety might weaken the negative correlation between sleep determination and bedtime procrastination.
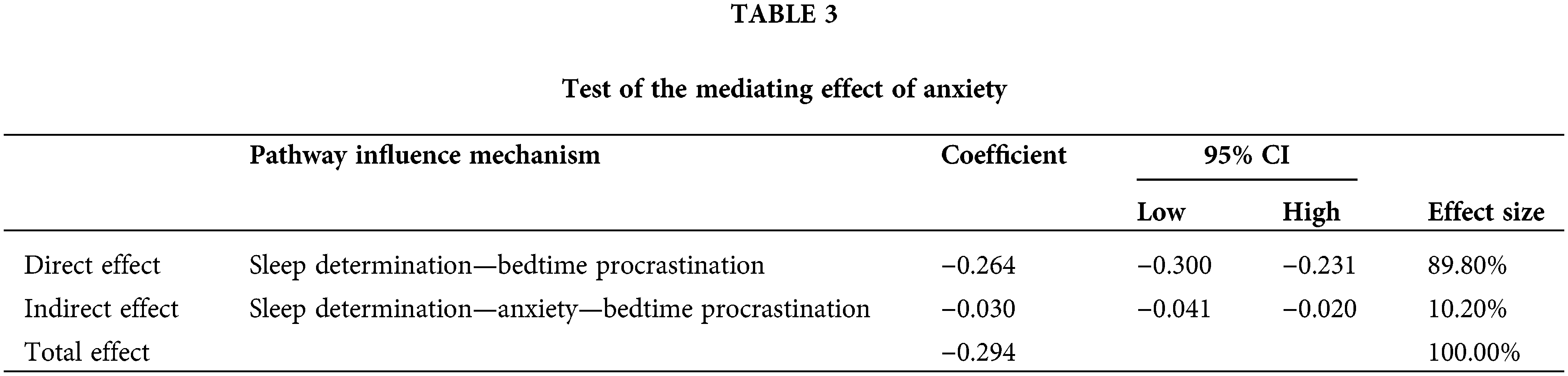
As shown in Table 3, the direct effect of sleep determination on bedtime procrastination (β = −0.264, 95% CI = [−0.300 to −0.231]) and the indirect effect (β = −0.030, 95% CI = [−0.041 to −0.020]) are both significant. The total effect (β = −0.294) indicates a mediating role of anxiety in the relationship between sleep determination and bedtime procrastination. The direct effect (−0.264) and the mediating effect (−0.030) respectively account for 89.80% and 10.20% of the total effect (−0.294), the indirect effect is significantly lower than the direct effect.
The modulating effect of anxiety
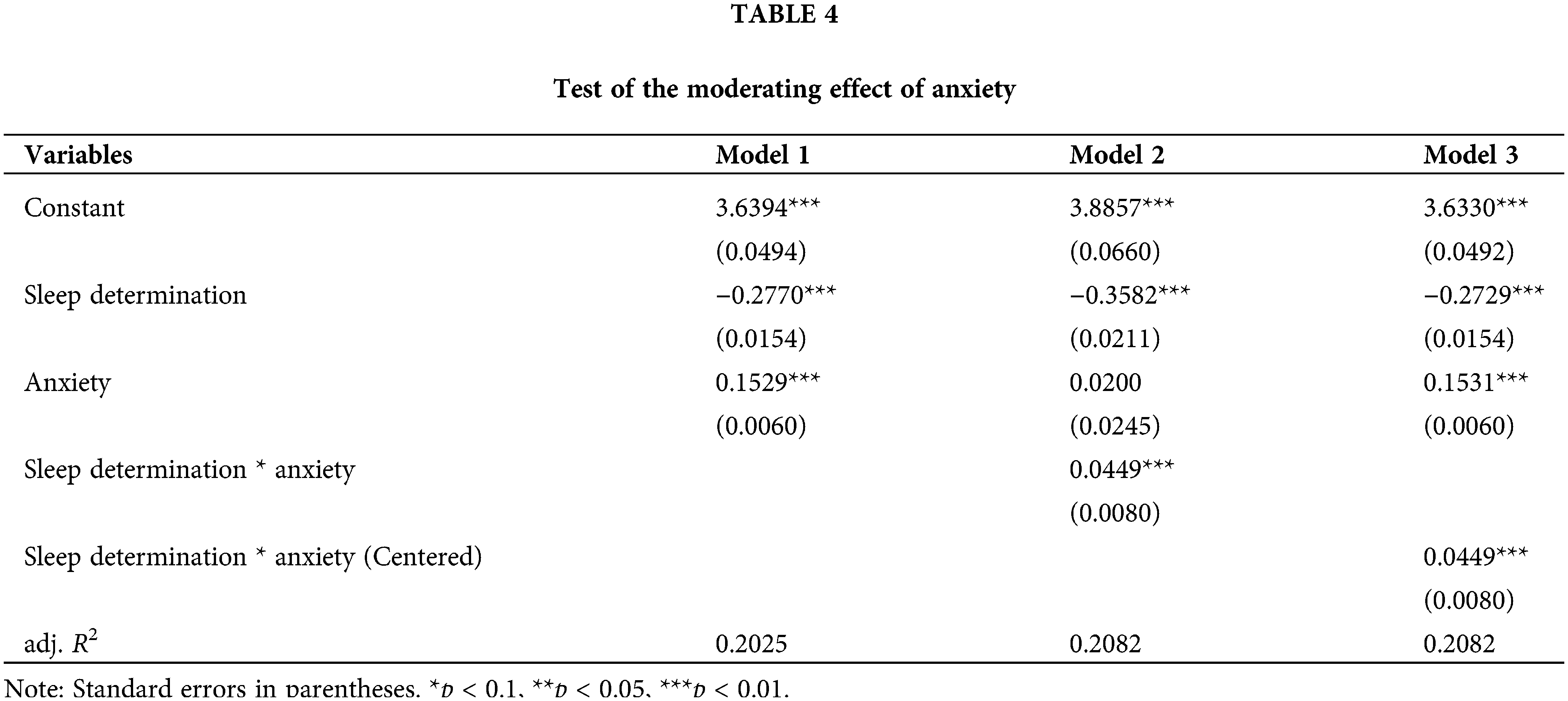
Table 4 shows that Model 2, built upon Model 1, adds the interaction term between sleep determination and anxiety. For ease of interpretation, Model 3 incorporates the centered variables of sleep determination and anxiety and their interaction term. The results of Models 2 and 3 are largely consistent. In Model 1, anxiety (B = 0.1529) significantly affects bedtime procrastination. However, in Model 2, the effect of anxiety on bedtime procrastination is no longer significant, while the interaction term has a significant effect. This indicates that anxiety has a moderating effect, and the latter part of the previously validated mediation pathway of anxiety (anxiety −> bedtime procrastination) is no longer valid at this point. Additionally, the correlation coefficient between sleep determination (B = −0.2729) and the interaction term of centered sleep determination and anxiety (B = 0.0449) is significantly opposite in sign. This indicates that anxiety significantly weakens the impact of sleep determination on bedtime procrastination. The statement “I am unwilling to sacrifice sleep for anything” can be seen as a strong behavioral intention against bedtime procrastination. The data show that in the absence of other disturbances, there is a negative correlation between sleep determination and bedtime procrastination, meaning the stronger the determination to ensure sleep, the less the bedtime procrastination behavior. However, this relationship is disrupted by anxiety, suggesting that the stronger an individual’s anxiety, the weaker the inhibitory effect of sleep determination on bedtime procrastination.
Firstly, the findings of this study validate the consistency observed in the field of health behavior concerning the enhancement of sleep determination and the reduction of bedtime procrastination. A negative correlation exists between sleep determination and bedtime procrastination. Sleep determination is a tangible manifestation of the behavioral intention to sleep, and the intensity of this intention can be measured by sleep determination. According to Maslow’s hierarchy of needs, the most basic level of physiological needs includes necessities like food, water, sleep, air, and shelter. If these needs are not met, individuals develop motivations to satisfy their current needs, driving their behavior—thus creating a need-motivation-behavior link. Similarly, sleep determination relates to the individual’s physiological need for sleep, influenced by factors like the biological clock, fatigue, and daily activities, fostering a stronger motivational force for behavior. The intensity of this motivation is a crucial determinant of behavioral outcomes [41]. Successful self-regulators do not rely solely on willpower to transform intentions into actions but utilize adaptive, effortless strategies (such as habits) [42] that are immune to variable mindsets or states. Possessing good sleep habits, including regular bedtimes and wake times, can reduce the risk of self-regulation failure. Habit formation can be supported through self-regulation, such as the realization of intentions. Loft and colleagues have found that implementing intention interventions can improve sleep behaviors, thereby enhancing sleep quality in workers [43]. Therefore, the study’s results are grounded in rational behavior theory and enhance the explanatory power and credibility of behavioral intention on bedtime procrastination by incorporating sleep determination as an operationalizable variable reflecting the strength of sleep-related behavioral intentions, thus offering new insights into the previously observed inconsistency between intention and behavior [14,44]. In addition, in the realm of sleep, behaviors related to sleep, along with perceptions and cognitions of these behaviors, play a significant role in regulating nocturnal sleep [45]. Numerous findings indicate that distorted beliefs and perceptions may be important psychological factors determining sleep quality, demonstrating that beliefs not only transform into related behaviors but also significantly influence actual physiological responses to emotions [46–48]. The perception of the importance of sleep is negatively correlated with bedtime procrastination, suggesting that individuals who devalue sleep are more likely to procrastinate before bedtime. This aligns with earlier findings on academic procrastination, where the perceived importance of performing well in a subject seldom correlates with high procrastination in that subject [49]. This suggests that changing personal views on the importance of sleep can also alter bedtime procrastination behaviors. Increasing clinical and experimental studies have also validated the effectiveness of cognitive approaches in treating insomnia and circadian rhythm disorders, such as correcting misconceptions, raising sleep hygiene awareness, and rectifying misconceptions about sleep deprivation [50,51]. In this study, although sleep determination is not entirely equivalent to sleep cognition, an individual’s cognition and beliefs about sleep influence their needs and decisions regarding sleep. This is manifested in the form that stronger cognition of sleep importance leads to stronger sleep determination, weaker anxiety, and reduced bedtime procrastination behaviors.
Secondly, this research finds a correlation between increased anxiety and increased bedtime procrastination, aligning with prior studies. Research by Guo et al. [52] and Türkarslan et al. [53] has demonstrated associations between bedtime procrastination and depression and anxiety, respectively. Sirois et al. [29] found that delaying sleep time is linked to individuals’ ability to regulate emotions, suggesting that lower negative emotions are conducive to reducing bedtime procrastination. Rubin [54] reported that individuals who procrastinate bedtime exhibit higher levels of depression and anxiety symptoms and poorer sleep quality. Geng et al. [55] also posited that anxiety and depressive symptoms can predict bedtime procrastination. Collectively, these findings indicate a vicious cycle between anxiety and bedtime procrastination, with anxiety leading to difficulty in falling asleep and bedtime procrastination further delaying sleep onset, increasing anxiety. This cycle can deteriorate sleep quality and negatively affect daily functioning and mental health. Therefore, maintaining a positive emotional state before sleep is crucial. Techniques such as relaxation, deep breathing, progressive muscle relaxation, meditation, and mindfulness can help alleviate anxiety. Additionally, learning to manage negative thoughts and worries, cognitive restructuring strategies can be employed to attempt and adjust other procrastination-reinforcing (irrational) cognitions into more positive evaluations. Cognitive restructuring can alter negative emotional and thinking patterns, aiding individuals in viewing problems from a positive and realistic perspective, thereby finding strategies to address anxiety issues [56,57].
Thirdly, In the association between sleep determination and pre-bedtime procrastination, the moderating effect of anxiety is found to be more significant than its mediating effect. While sleep determination can reduce pre-bedtime procrastination behaviors by decreasing individuals’ anxiety levels, the link between sleep determination and pre-bedtime procrastination is more susceptible to interference from individuals’ pre-existing levels of anxiety. Although this study confirms a partial mediating effect of anxiety within the relationship between sleep determination and pre-bedtime procrastination—that is, sleep determination can reduce pre-bedtime procrastination behaviors by lowering anxiety levels—this mechanism appears to be more evident in individuals with higher anxiety levels. In contrast, it holds less explanatory power for individuals with lower anxiety levels. Furthermore, given that individual anxiety levels are influenced by a myriad of factors, this uncertainty also diminishes the credibility of anxiety’s mediating effect in the relationship between sleep determination and pre-bedtime procrastination. However, as a moderating variable, anxiety weakens the negative correlation between sleep determination and bedtime procrastination. This means that when the strength of sleep determination is constant, individuals with higher levels of anxiety exhibit increased bedtime procrastination compared to those with lower levels of anxiety. Implementation intentions like Mental Contrasting with Implementation Intentions (MCII) can reduce bedtime procrastination caused by self-regulation failure [58], as they do not require significant cognitive resources [59,60]. However, this approach may not be effective in different contexts, such as in states of anxiety. However, these may not be effective in other situations, such as states of anxiety. The study’s results indicate that the negative explanatory power of sleep determination on bedtime procrastination is less than the positive explanatory power of anxiety on the same. In other words, although sleep determination can reduce bedtime procrastination, this effect is significantly weakened in states of high anxiety. Therefore, it is believed that sleep determination needs to be in a more positive emotional context to effectively reduce bedtime procrastination. This finding supplements Kroese’s interventions for bedtime procrastination based on failures in self-regulation. Consequently, this study offers practical suggestions to reduce bedtime procrastination. Firstly, recognizing the importance of sleep can subconsciously reduce the intention to procrastinate before going to bed, thus strengthening sleep determination. On workdays, as people’s school or work hours are typically fixed, this implies that waking times are also fixed. Choosing to sacrifice or reduce sleep for other activities often means delaying bedtime, thus reinforcing sleep determination can help reduce the spontaneity of procrastination behaviors. Additionally, regulating emotions before sleep is vital. Before deciding to go to bed, it is important to ease emotions and ensure the body is in a relaxed state of readiness for sleep, rather than rigidly enforcing a set sleep time. Such unrealistic beliefs could, in fact, trigger anxiety [61,62], further increasing bedtime procrastination.
Certainly, this study has its limitations. Firstly, although the sample size is substantial and covers a nationwide scope, individual-level random variations and personality differences may have been averaged out, meaning the results may not be universally applicable to all groups. Secondly, the study did not exclude individuals with insomnia disorders or other factors that might cause bedtime procrastination, such as internet addiction, which could introduce bias into the results. Future research could validate the findings across different groups and exclude other sleep-affecting confounders. Thirdly, the measures in this study are entirely based on participants’ self-reported subjective indicators rather than objective ones. Although self-reported questionnaires are highly correlated with objective measurements of sleep [63], to enhance the credibility of the findings, future research could employ multiple assessment methods, such as sleep diaries and wearable devices, to obtain more objective data and strengthen the validity of the conclusions. Fourthly, although both theoretical construction and empirical research have confirmed the validity of the hypotheses, the cross-sectional nature of the data used in the study does not allow for precise inference of causal relationships between variables. Future studies should consider using longitudinal tracking data or experimental data to verify the causal relationships between variables.
Strengthening sleep determination effectively reduces bedtime procrastination; anxiety intensifies bedtime procrastination; Within the relationship between sleep determination and pre-bedtime procrastination, the moderating effect of anxiety surpasses its mediating effect, in that anxiety attenuates the negative correlation between sleep determination and pre-bedtime procrastination. Consequently, we propose specific recommendations to reduce bedtime procrastination, including reinforcing the understanding of the importance of sleep, adopting positive emotional regulation strategies, and formulating moderate sleep plans. Our research underscores the significance of enhancing sleep determination and reducing anxiety in mitigating bedtime procrastination, aiding individuals in reevaluating bedtime procrastination from diverse perspectives and adopting proactive coping measures to improve sleep health.
Acknowledgement: We are grateful to the associate editors and reviewers for providing feedback suggestions that refined this article.
Funding Statement: None.
Author Contributions: NL: research idea and study design. JW and NL: data acquisition. NL: data analysis/interpretation. WZ: supervision or mentorship. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Availability of Data and Materials: At present, the data from the survey on the sleep conditions of Chinese residents is classified and restricted for internal use only. However, it is anticipated to be made available to the public in the near future. For a more comprehensive understanding of the survey on the sleep conditions of Chinese residents, one is advised to consult the “ANNUAL SLEEP REPORT OF CHINA 2022” [63].
Ethics Approval: This research was sanctioned by the academic board of the Institute of Sociology at the Chinese Academy of Social Sciences. All participants signed the informed consent in this study. In our methodology, we ensured that no personally identifiable information was either collected or used. Prior to initiating the survey, participants were thoroughly briefed about its objectives, including th e potential benefits and risks involved. They expressed their consent by clicking the ‘next’ button before commencing the questionnaire. It was explicitly communicated that participation was voluntary, with the option to withdraw at any point during the survey. For their participation, individuals were compensated with an amount of CNY 6 upon completion of the questionnaire.
Conflicts of Interest: The authors have declared that there are no conflicts of interest regarding the research, authorship, and publication of this article.
References
1. Buysse DJ. Sleep health: can we define it? does it matter? Sleep. 2014;37(1):9–17. doi:10.5665/sleep.3298 [Google Scholar] [PubMed] [CrossRef]
2. Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci & Med. 2010;71(5):1027–36. doi:10.1016/j.socscimed.2010.05.041 [Google Scholar] [PubMed] [CrossRef]
3. Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the national health interview survey. Sleep. 2010;33(8):1037–42. doi:10.1093/sleep/33.8.1037 [Google Scholar] [PubMed] [CrossRef]
4. Stickgold R, Hobson JA, Fosse R, Fosse M. Sleep, learning, and dreams: off-line memory reprocessing. Science. 2001;294(5544):1052–7. doi:10.1126/science.1063530 [Google Scholar] [PubMed] [CrossRef]
5. Bian XH, Hou XL, Zuo ZH, Quan H, Ju K, Wu W, et al. Depression and sleep quality among Chinese college students: the roles of rumination and self-compassion. Curr Psychol. 2022;41(7):4242–51. doi:10.1007/s12144-020-00946-3. [Google Scholar] [CrossRef]
6. Li YY, Bai W, Zhu B, Duan RX, Yu X, Xu W, et al. Prevalence and correlates of poor sleep quality among college students: a cross-sectional survey. Health Qual Life Outcomes. 2020;18(1):210. doi:10.1186/s12955-020-01465-2 [Google Scholar] [PubMed] [CrossRef]
7. Mishra AA, Friedman EM, Mihalec-Adkins BP, Evich CD, Christ SL, Marceau K. Childhood maltreatment exposure and physical functional limitations in late adulthood: examining subjective sleep quality in midlife as a mediator. Psychol & Health. 2020;35(5):573–92. doi:10.1080/08870446.2019.1657576 [Google Scholar] [PubMed] [CrossRef]
8. Liu QQ, Zhou ZK, Yang XJ, Kong FC, Sun XJ, Fan CY. Mindfulness and sleep quality in adolescents: analysis of rumination as a mediator and self-control as a moderator. Pers Individ Differ. 2018;122:171–6. doi:10.1016/j.paid.2017.10.031. [Google Scholar] [CrossRef]
9. Zhang MX, Wu AMS. Effects of smartphone addiction on sleep quality among Chinese university students: the mediating role of self-regulation and bedtime procrastination. Addict Behav. 2020;111:106552. doi:10.1016/j.addbeh.2020.106552 [Google Scholar] [PubMed] [CrossRef]
10. Cui G, Yin Y, Li S, Chen L, Liu X, Tang K, et al. Longitudinal relationships among problematic mobile phone use, bedtime procrastination, sleep quality and depressive symptoms in Chinese college students: a cross-lagged panel analysis. BMC Psychiatry. 2021;21(1):449. doi:10.1186/s12888-021-03451-4 [Google Scholar] [PubMed] [CrossRef]
11. Pu Z, Leong RLF, Chee MWL, Massar SAA. Bedtime procrastination and chronotype differentially predict adolescent sleep on school nights and non-school nights. Sleep Health. 2022;8(6):640–7. doi:10.1016/j.sleh.2022.09.007 [Google Scholar] [PubMed] [CrossRef]
12. Kadzikowska-Wrzosek R. Self-regulation and bedtime procrastination: the role of self-regulation skills and chronotype. Pers Individ Dif. 2018;128:10–5. doi:10.1016/j.paid.2018.02.015. [Google Scholar] [CrossRef]
13. Kroese FM, de Ridder DT, Evers C, Adriaanse MA. Bedtime procrastination: introducing a new area of procrastination. Front Psychol. 2014;5:611 [Google Scholar] [PubMed]
14. Steel P. The nature of procrastination: a meta-analytic and theoretical review of quintessential self-regulatory failure. Psychol Bull. 2007;133(1):65–94. doi:10.1037/0033-2909.133.1.65 [Google Scholar] [PubMed] [CrossRef]
15. Kamphorst BA, Nauts S, de Ridder DTD, Anderson JH. Too depleted to turn in: tthe relevance of end-of-the-day resource depletion for reducing bedtime procrastination. Front Psychol. 2018;9:252. doi:10.3389/fpsyg.2018.00252 [Google Scholar] [PubMed] [CrossRef]
16. Baumeister RF, Bratslavsky E, Muraven M, Tice DME. Ego depletion: is the active self a limited resource? J Pers Soc Psychol. 1998;74(5):1252–65. doi:10.1037/0022-3514.74.5.1252 [Google Scholar] [PubMed] [CrossRef]
17. Baumeister RF, Vohs KD. Self-regulation, ego depletion, and motivation. Soc Pers Psychol Compass. 2007;1(1):115–28. doi:10.1111/spco.2007.1.issue-1. [Google Scholar] [CrossRef]
18. Baumeister RF. Yielding to temptation: self-control failure, impulsive purchasing, and consumer behavior. J Consum Res. 2002;28(4):670–6. doi:10.1086/jcr.2002.28.issue-4. [Google Scholar] [CrossRef]
19. Ferrari JR. Procrastination and attention: factor analysis of attention deficit, boredomness, intelligence, self-esteem, and task delay frequencies. J Soc Behav & Pers. 2000;15(5):185–96. [Google Scholar]
20. Tanaka H, Shirakawa S. Sleep health, lifestyle and mental health in the Japanese elderly. J Psychosom Res. 2004;56(5):465–77. doi:10.1016/j.jpsychores.2004.03.002 [Google Scholar] [PubMed] [CrossRef]
21. Zhang L, Yuan QJ, Wu QL, Kwauk S, Liao SJ, Wang CL. Sleep quality and sleep disturbing factors of inpatients in a Chinese general hospital. J Clin Nurs. 2009;18(17):2521–9. doi:10.1111/jcn.2009.18.issue-17. [Google Scholar] [CrossRef]
22. Martin M, Sadlo G, Stew G. The phenomenon of boredom. Qual Res Psychol. 2006;3(3):193–211. doi:10.1191/1478088706qrp066oa. [Google Scholar] [CrossRef]
23. Andrade AM, Coutinho SR, Silva MN, Mata J, Vieira PN, Minderico CS, et al. The effect of physical activity on weight loss is mediated by eating self-regulation. Patient Educ Couns. 2010;79(3):320–6. doi:10.1016/j.pec.2010.01.006 [Google Scholar] [PubMed] [CrossRef]
24. Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, Otto MW. The effects of physical activity on sleep: a meta-analytic review. J Behav Med. 2015;38(3):427–49. doi:10.1007/s10865-015-9617-6 [Google Scholar] [PubMed] [CrossRef]
25. Wang F, Boros S. The effect of physical activity on sleep quality: a systematic review. Eur J Physiother. 2021;23(1):11–8. doi:10.1080/21679169.2019.1623314. [Google Scholar] [CrossRef]
26. Sirois F, Pychyl T. Procrastination and the priority of short-term mood regulation: consequences for future self. Soc Pers Psychol Compass. 2013;7(2):115–27. doi:10.1111/spco.2013.7.issue-2. [Google Scholar] [CrossRef]
27. Gort C, Marcusson-Clavertz D, Kuehner C. Procrastination, affective state, rumination, and sleep quality: investigating reciprocal effects with ambulatory assessment. J Ration-Emot & Cogn-Behav Ther. 2021;39(1):58–85. doi:10.1007/s10942-020-00353-4. [Google Scholar] [CrossRef]
28. Procee R, Kamphorst BA, van Wissen A, Meyer JJ, Hindriks K, de Weerdt M, et al. A formal model of procrastination. In: BNAIC 2013: Proceedings of the 25th Benelux Conference on Artificial Intelligence, 2013. p. 152–9. [Google Scholar]
29. Sirois FM, Nauts S, Molnar DS. Self-compassion and bedtime procrastination: an emotion regulation perspective. Mindfulness. 2019;10(3):434–45. doi:10.1007/s12671-018-0983-3. [Google Scholar] [CrossRef]
30. Feng Y, Meng D, Guo J, Zhao Y, Ma X, Zhu L, et al. Bedtime procrastination in the relationship between self-control and depressive symptoms in medical students: from the perspective of sex differences. Sleep Med. 2022;95:84–90. doi:10.1016/j.sleep.2022.04.022 [Google Scholar] [PubMed] [CrossRef]
31. Chung SJ, An H, Suh S. What do people do before going to bed? A study of bedtime procrastination using time use surveys. Sleep. 2020;43(4):zsz267. doi:10.1093/sleep/zsz267 [Google Scholar] [PubMed] [CrossRef]
32. Oppenheimer CW, Hankin BL, Young J. Effect of parenting and peer stressors on cognitive vulnerability and risk for depression among youth. J Abnorm Child Psychol. 2018;46(3):597–612. doi:10.1007/s10802-017-0315-4 [Google Scholar] [PubMed] [CrossRef]
33. Shi M, Wang X, Bian Y, Wang L. The mediating role of resilience in the relationship between stress and life satisfaction among Chinese medical students: a cross-sectional study. BMC Med Educ. 2015;15(1):16. doi:10.1186/s12909-015-0297-2 [Google Scholar] [PubMed] [CrossRef]
34. Kroese FM, de Ridder DT. Health behaviour procrastination: a novel reasoned route towards self-regulatory failure. Health Psychol Rev. 2016;10(3):313–25. doi:10.1080/17437199.2015.1116019 [Google Scholar] [PubMed] [CrossRef]
35. Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Philosophy and Rhetoric. 1977;10(2):130–2. [Google Scholar]
36. Sheppard BH, Hartwick J, Warshaw PR. The theory of reasoned action: a meta-analysis of past research with recommendations for modifications and future research. J Consum Res. 1988;15(3):325. doi:10.1086/jcr.1988.15.issue-3. [Google Scholar] [CrossRef]
37. Ajzen I. From intentions to actions: a theory of planned behavior. In: Action control: from cognition to behavior. Berlin, Heidelberg: Springer Berlin Heidelberg; 1985. p. 11–39. [Google Scholar]
38. Kroese FM, de Ridder DTD, Evers C, Adriaanse MA. Bedtime procrastination: introducing a new area of procrastination. Front Psychol. 2014;5:611 [Google Scholar] [PubMed]
39. Li H, Boey KW. Assessing psychological well-being of college students: psychometric properties of GHQ-20. J Psychol Dev Educ. 2002;18(1):75–9. [Google Scholar]
40. Hudson NW, Lucas RE, Donnellan MB. Day-to-day affect is surprisingly stable: a 2-year longitudinal study of well-being. Soc Psychol Pers Sci. 2017;8(1):45–54. doi:10.1177/1948550616662129 [Google Scholar] [PubMed] [CrossRef]
41. McClelland DC. How motives, skills, and values determine what people do. Am Psychol. 1985;40(7):812–25. doi:10.1037/0003-066X.40.7.812. [Google Scholar] [CrossRef]
42. Gillebaart M, de Ridder DTD. Effortless self-control: a novel perspective on response conflict strategies in trait self-control. Soc Pers Psychol Compass. 2015;9(2):88–99. doi:10.1111/spc3.v9.2. [Google Scholar] [CrossRef]
43. Loft MH, Cameron LD. Using mental imagery to deliver self-regulation techniques to improve sleep behaviors. Ann Behav Med. 2013;46(3):260–72. doi:10.1007/s12160-013-9503-9 [Google Scholar] [PubMed] [CrossRef]
44. Sheeran P, Webb TL. The intention-behavior gap. Soc Pers Psychol Compass. 2016;10(9):503–18. doi:10.1111/spc3.v10.9. [Google Scholar] [CrossRef]
45. Lundh LG, Broman JE. Insomnia as an interaction between sleep-interfering and sleep-interpreting processes. J Psychosom Res. 2000;49(5):299–310. doi:10.1016/S0022-3999(00)00150-1 [Google Scholar] [PubMed] [CrossRef]
46. Eidelman P, Talbot L, Ivers H, Belanger L, Morin CM, Harvey AG. Change in dysfunctional beliefs about sleep in Behavior Therapy, cognitive therapy, and cognitive-behavioral therapy for insomnia. Behav Therapy. 2016;47(1):102–15. doi:10.1016/j.beth.2015.10.002 [Google Scholar] [PubMed] [CrossRef]
47. Kuo MF, Nitsche MA. Effects of transcranial electrical stimulation on cognition. Clin EEG Neurosci. 2012;43(3):192–9. doi:10.1177/1550059412444975 [Google Scholar] [PubMed] [CrossRef]
48. Crönlein T, Wagner S, Langguth B, Geisler P, Eichhammer P, Wetter TC. Are dysfunctional attitudes and beliefs about sleep unique to primary insomnia? Sleep Med. 2014;15(12):1463–7. doi:10.1016/j.sleep.2014.06.018 [Google Scholar] [PubMed] [CrossRef]
49. Kljajic K, Gaudreau P. Does it matter if students procrastinate more in some courses than in others? A multilevel perspective on procrastination and academic achievement. Learn Instr. 2018;58:193–200. doi:10.1016/j.learninstruc.2018.06.005. [Google Scholar] [CrossRef]
50. Perrault AA, Pomares FB, Smith D, Cross NE, Gong K, Maltezos A, et al. Effects of cognitive behavioral therapy for insomnia on subjective and objective measures of sleep and cognition. Sleep Med. 2022;97:13–26. doi:10.1016/j.sleep.2022.05.010 [Google Scholar] [PubMed] [CrossRef]
51. Tan X, Van Egmond L, Partinen M, Lange T, Benedict C. A narrative review of interventions for improving sleep and reducing circadian disruption in medical inpatients. Sleep Med. 2019;59:42–50. doi:10.1016/j.sleep.2018.08.007 [Google Scholar] [PubMed] [CrossRef]
52. Guo J, Meng D, Ma X, Zhu L, Yang L, Mu L. The impact of bedtime procrastination on depression symptoms in Chinese medical students. Sleep Breath. 2020;24(3):1247–55. doi:10.1007/s11325-020-02079-0 [Google Scholar] [PubMed] [CrossRef]
53. Türkarslan KK, Okay D, Çevrim M, Bozo Ö. Life is short, stay awake: death anxiety and bedtime procrastination. J Gen Psychol. 2020;147(1):43–61. doi:10.1080/00221309.2019.1633994 [Google Scholar] [PubMed] [CrossRef]
54. Rubin R. Matters of the mind—bedtime procrastination, relaxation-induced anxiety, lonely tweeters. JAMA. 2020;323(1):15–6. doi:10.1001/jama.2019.20014 [Google Scholar] [PubMed] [CrossRef]
55. Geng Y, Gu J, Wang J, Zhang R. Smartphone addiction and depression, anxiety: the role of bedtime procrastination and self-control. J Affect Disord. 2021;293:415–21. doi:10.1016/j.jad.2021.06.062 [Google Scholar] [PubMed] [CrossRef]
56. Clark DA, Beck AT. Cognitive theory and therapy of anxiety and depression: convergence with neurobiological findings. Trends Cogn Sci. 2010;14(9):418–24. doi:10.1016/j.tics.2010.06.007 [Google Scholar] [PubMed] [CrossRef]
57. Rozental A, Carlbring P. Understanding and treating procrastination: a review of a common self-regulatory failure. Psychology. 2014;5(13):1488–1502. doi:10.4236/psych.2014.513160. [Google Scholar] [CrossRef]
58. Schmidt LI, Neubauer AB, Stoffel M, Ditzen B, Schirmaier J, Farrenkopf C, et al. Effects of mental contrasting on sleep and associations with stress: a randomized controlled trial. J Health Psychol. 2023;28(11):1057–71. doi:10.1177/13591053231159168 [Google Scholar] [PubMed] [CrossRef]
59. Webb TL, Sheeran P. How do implementation intentions promote goal attainment? A test of component processes. J Exp Soc Psychol. 2007;43(2):295–302. doi:10.1016/j.jesp.2006.02.001. [Google Scholar] [CrossRef]
60. Sheeran P, Trafimow D, Armitage CJ. Predicting behaviour from perceived behavioural control: tests of the accuracy assumption of the theory of planned behaviour. Br J Soc Psychol. 2003;42(3):393–410. doi:10.1348/014466603322438224 [Google Scholar] [PubMed] [CrossRef]
61. Ascher LM, Efran JS. Use of paradoxical intention in a behavioral program for sleep onset insomnia. J Consult Clin Psychol. 1978;46(3):547–50. doi:10.1037/0022-006X.46.3.547 [Google Scholar] [PubMed] [CrossRef]
62. Wang J, Zhang Y, Liu Y. Annual sleep report of China 2022. Beijing, China: Social Sciences Academic Press; 2023. [Google Scholar]
63. Díaz-Morales JF, Escribano C, Jankowski KS, Vollmer C, Randler C. Evening adolescents: the role of family relationships and pubertal development. J Adolesc. 2014;37(4):425–32. doi:10.1016/j.adolescence.2014.03.001 [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools