 Open Access
Open Access
ARTICLE
Exploring the Prevalence and Contributing Factors of Depression among Sickle Cell Anemia Patients in Saudi Arabia’s Jazan Region
1 Family and Community Medicine Department, Faculty of Medicine, Jazan University, Jazan, 45142, Saudi Arabia
2 Laboratory Department, King Fahd Central Hospital, Ministry of Health, Jazan, 45142, Saudi Arabia
3 Internal Medicine Department, Prince Mohammad bin Nasser Hospital, Ministry of Health, Jazan, 45142, Saudi Arabia
4 Hematology Department, King AbdulAziz Medical City for National Guard, Riyadh, 11426, Saudi Arabia
* Corresponding Author: Ahmad Y. Alqassim. Email:
International Journal of Mental Health Promotion 2024, 26(5), 351-359. https://doi.org/10.32604/ijmhp.2024.047219
Received 29 October 2023; Accepted 19 March 2024; Issue published 30 May 2024
Abstract
Sickle Cell Anemia (SCA) is a prevalent genetic condition in Saudi Arabia, particularly in the Jazan region. The study’s purpose was to assess the prevalence of de-pression among individuals with SCA in this area and to identify the factors associated with this condition. The study involved 391 adult participants, all patients in the hematology center of Prince Mohammed bin Nasser Hospital (PMNH). Data was collected through an anonymous interview questionnaire–the Arabic version of the Patient Health Questionnaire-9 (PHQ-9)–between March–May 2022. The questionnaire covered socio-demographic information and variables related to the participant’s SCA history, such as pain levels, frequency of pain, hospitalization duration, and frequency of blood transfusions. These variables underwent Chi-square and One-way ANOVA testing, followed by multivariate regression. The study found a 42% prevalence of depression among the SCA patients. Factors significantly linked with heightened depression levels included being widowed or divorced, experiencing frequent and severe pain, and longer duration of hospital stays. An educational level of at least a bachelor’s degree was also a significant factor. The study reveals a high prevalence of depression among SCA patients in the Jazan region. It underscores the need for policymakers to educate both physicians and patients about the importance of mental health in SCA management. The study also highlights the need for more research into the specific causes and effects of depressive symptoms in SCA patients to inform the creation of effective management plans.Keywords
Sickle cell disease (SCD) is an autosomal recessive ailment resulting from genetic mutations in the beta-globin chain that causes the formation of hemoglobin S [1]. Hemoglobin S is a mutated form of hemoglobin that causes red blood cells to become rigid, sticky, and misshapen. SCD affects multiple organ systems in those with the disease who are called patients with SCD, and the impact of this pleiotropic disease is increased morbidity and health expenditures along with decreased life expectancy and health related quality of life (HRQoL) [1,2]. The disease has many different effects and severity from patient to patient and an individual may experience a variety of effects over their lifetime [3]. The most frequent complication is vaso-occlusive crisis which leads to several other conditions and complications over time including cerebral infarction, cardiomyopathy, growth retardation, and hepatic-splenic sequestration, among others [3,4]. A vaso-occlusive crisis is a common complication of SCD that occurs when sickle-shaped red blood cells block small blood vessels. Treatment for vaso-occlusive crisis includes pain management with opioids such as morphine and hydration therapy [5]. The clinical course for patients with SCD including multiple hospitalizations (among the highest rates for any disease worldwide), frequent blood transfusion requirements, frequent emergency room visits and various unpredictable symptoms, creates daily difficulties leading to a reduction in quality of life for patients [6].
SCD is a relatively frequent genetic condition in Saudi Arabia, where the clinical phenotype is the Arab Indian haplotype, which differs from the Benin western haplotype SCD in its manifestations and complications [7]. With a consanguineous marriage rate of over 50%, SCD is prevalent in the country [8]. Several studies have explored the prevalence of depression among SCD patients in Saudi Arabia. One study reported a prevalence of 45.4%, with the highest rates found among single unemployed well-educated males [9]. In contrast, another study conducted in the southern region of Saudi Arabia found that socio-demographic factors were not significant predictors of depression in SCD patients, and the prevalence of depressive symptoms was 85.9% [10]. Two studies, one conducted in the U.S. and one in the Kingdom of Saudi Arabia, discovered that the prevalence of depression in females with SCD was higher than in males [6,11]. A study that was published in 2019 indicated that in the United States, individuals diagnosed with SCD had an average life expectancy of 42 years for men and 48 years for women [12]. The reported prevalence for sickle-cell trait ranges from 2% to 27%, and up to 2.6% will have SCD in some areas [7].
As two reviews revealed, there is an association between chronic medical conditions and depression, although SCD was not among the conditions included [13,14]. Until recently, the psycho-social impact of the disease was underestimated as most studies have focused on the pathophysiological and clinical morbidity of the disease [3,7]. A 1999 U.S. study of 440 adult person with SCD patients who showed depressive symptoms reported more frequent and severe vaso-occlusive crisis episodes [4]. Several national studies have found a significant and robust relationship between depression and SCD [15,16]. Two American studies reported 22%–36% depression rates among adults and 46% among children and adolescents with SCD with corresponding rates of suicidal ideation [15,17]. A study conducted in Brazil stated that the rate of depression among SCD patients was 27.6% and mean pain in depressed patients was higher compared to non-depressed [18]. A Jamaican study reported a depression rate of 21.6% that was strongly associated with sociodemographic variables such as education status and employment in this population [19]. Oudin Doglioni et al. criticized the prevalence of depression in people with SCD, underlining the methodological difficulties of such an assessment and suggesting ways of avoiding errors [20].
SCA patients experience substantial symptom burden and complications that can vary in severity, negatively impacting physical, emotional, and social well-being and compromising quality of life [21]. SCD confers significant health and economic implications, requiring substantial medical resources. Studies demonstrate SCD markedly increases healthcare costs, with hospitalizations representing a major cost driver [22]. Adolescents and young adults with SCD encounter numerous acute and chronic complications; their higher mortality underscores the importance of addressing health challenges in this age group [23]. Conducting research on SCA patients is critical for improving emotional well-being and managing disease burden. Given the robust association between SCD and depression reported in the literature, investigating this relationship further and devising strategies to enhance quality of life for individuals with SCD is imperative from a public health perspective.
SCD is an endemic disease in the Jazan region, ranking the second-highest rate of the disease prevalence in Saudi Arabia [24]. According to a study conducted in the Jazan region, this genetic abnormality affects up to 10% of the population in Jazan city, 8% in Abu Arish, 9% in Sabia, 6% in Baish, and 4% in Samtah [24]. We have encountered a major knowledge gap regarding the relationship between depression and SCD in the Jazan region. Such data will help in a management plan of SCD, hence providing a better health outcome. As there is a lack of studies that assess depression among SCD patients in Saudi Arabia, especially in the Jazan region, we aimed to determine the prevalence of depression and the associated factors that might influence their levels among patients with SCD in the Jazan region.
We conducted a cross-sectional design to determine depression levels in SCD patients in the Jazan region of the KSA. Data were collected from 391 adult SCD patients registered at Prince Mohammed bin Nasser Hospital (PMNH) during the period of March–May 2022. PMNH is a tertiary hospital in Jazan City, Saudi Arabia, and is considered a referral facility with specialized centers for all hematological disorders that receive most of the SCD cases in the Jazan region. We invited adult person with SCD who were enrolled in the hematology department at PMNH, who visited the Sickle Cell Clinic during the period from March to May 2022. Adult patients diagnosed with SCA receiving care at the hematology center of Prince Mohammed bin Nasser Hospital in Jazan City, Saudi Arabia were recruited for this study. Inclusion criteria were: (1) confirmed diagnosis of SCA, (2) age 18 years or older, (3) resident of the Jazan region of Saudi Arabia, and (4) ability to comprehend the survey questions and provide informed consent. Exclusion criteria were: (1) absence of a sickle cell disease diagnosis, (2) residence outside of the Jazan region, (3) inability to understand the survey content, and (4) age under 18 years. Patients were approached in the hematology clinic waiting area and invited to participate. After obtaining verbal informed consent, participants who agreed to enroll were escorted to a private room to complete the anonymous questionnaire.
All variables were elicited using a validated Arabic version of the Patient Health Questionnaire-9 (PHQ-9) [25]. The PHQ-9 has been widely used and validated in various patient populations, including those with chronic illnesses such as diabetes and heart disease, and has been shown to have good reliability and validity After taking the participants to a private waiting room, the data collectors helped and clarified the incomprehensible questions to the participants [26,27].
To obtain a statistically sufficient sample size, the Epi InfoTM7 (Centers for Disease Control and Prevention, Atlanta, Georgia, USA) was used. The minimal sample size calculated using this method was 384 to produce a margin of error of no more than 5% with a 95% confidence interval [28].
Depression symptom severity was assessed using PHQ-9, a validated 9-item tool that examines how often in the past 2 weeks patients have been bothered by anhedonia, depressed mood, sleep disturbances, fatigue, appetite changes, negative self-perception, concentration deficits, psychomotor retardation or agitation, and suicidal ideation. Each item is scored on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Total scores range from 0 to 27, with higher scores indicating more severe depression. For analysis, PHQ-9 scores were categorized as minimal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), or severe (20–27) depression. A cutoff of ≥10 was used to define the presence of clinically significant depressive symptoms. This threshold has been well validated against clinical interviews and functional impairment measures [29].
The socio-demographic variables of age, gender, marital status, educational level, and employment status were measured to determine the association of these factors with depression among SCA patients. Medical history factors assessed for an association with depressive symptoms included smoking status, pregnancy, previous surgery, and family history of SCA. The statistical significance of the association of the severity of SCA with depressive symptoms in participants was assessed using the following six variables: frequency of pain crises induced monthly hospital visits and follow-ups, frequency and severity of pain episodes, total number of blood transfusions, and the longest hospitalization.
All data was analyzed in a three-step process using the STATA, version 2016 (StataCorp LLC, Texas, USA). Statistical significance was established at a p-value of ≤0.05. In the first phase participant characteristics were described and secondly subjected to either One-way ANOVA or Chi-square tests. Finally, multivariate regression was applied to test for confounding variables with a confidence interval of 95%.
The Institutional Review Board of the Jazan Health Ethics Committee of the Ministry of Health, Saudi Arabia approved the ethics of this study. Approval Number 2203, on 11th January 2022. Those who agreed to participate were taken to a private room to read and understand the informed consent before filling out the questionnaire.
Table 1 reports the results of the Chi-square and One-way ANOVA tests for patient characteristics grouped by participants reporting or not reporting depression. The study found that depression rates were significantly higher among participants aged 30 years or under (46% vs. one third among those over 30; p = 0.024), divorced or widowed participants (OR 5.367, p = 0.038), those with health insurance (OR 2.538, p = 0.010), and those experiencing a higher number of pain episodes (OR 2.004, p = 0.032 for 5–8 episodes; OR 3.501, p ≤ 0.001 for more than 8 episodes). Furthermore, compared to participants with pain levels less than eight, those with pain levels more than eight reported depression 1.8 times as often (OR 1.823, p = 0.029). The occurrence of blood transfusion did not show a significant difference in reported depression.
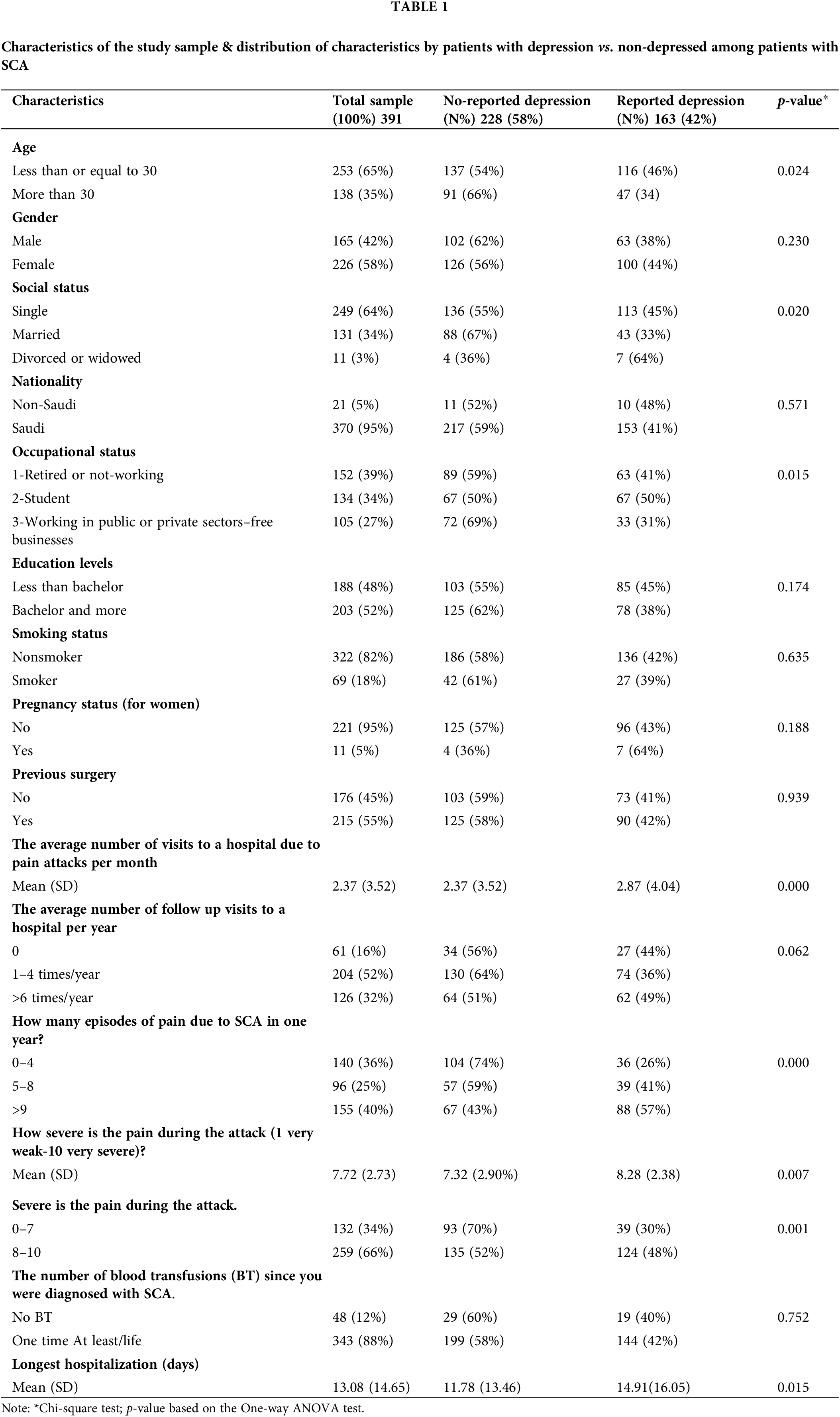
Table 2 reports the results of the multi-logistic regression for patient characteristics among SCD patients in the Jazan region. The study found that divorced or widowed participants (OR 5.367, p = 0.038), participants with health insurance (OR 2.538, p = 0.010), and those with a higher number of pain episodes (OR 2.004, p = 0.032 for 5–8 episodes; OR 3.501, p ≤ 0.001 for more than 8 episodes) had significantly higher odds of reporting depression. Moreover, compared to participants with an educational level below a bachelor’s degree, those with a bachelor’s degree had a slightly higher rate of reported depression (OR 1.006, p = 0.010). Additionally, the mean length of hospital stay was significantly associated with depression, with per one-day increase in the longest hospitalization history for a patient with SCD due to the episode, the log odds of depression will increase by 1.348 times (OR 1.348, p = 0.048).
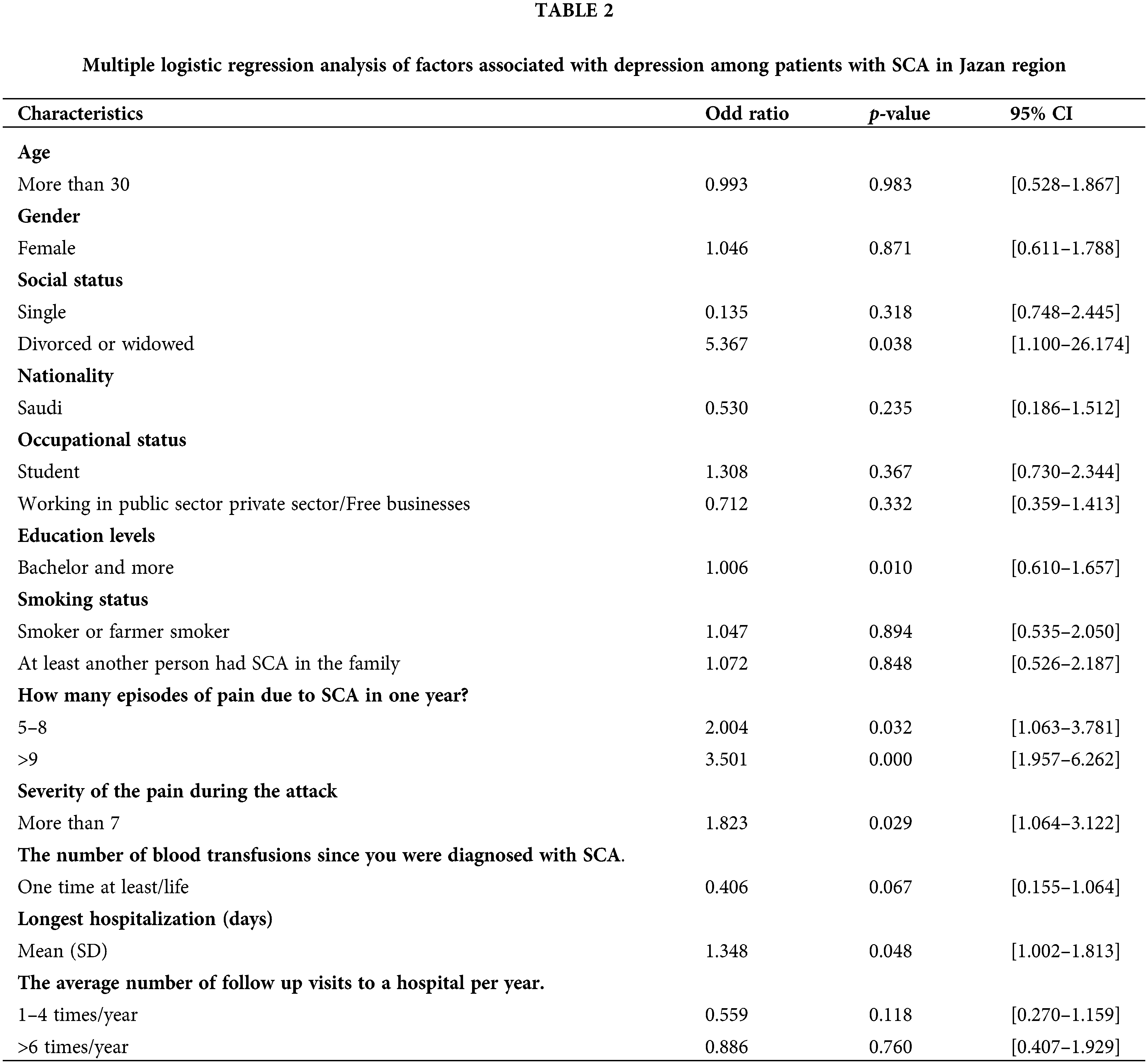
This study examined depression in SCD patients in Jazan, Saudi Arabia and its associated factors. Results showed that age, marital status, educational level, health insurance, frequency/severity of pain episodes, and length of hospital stay were significant factors. Notably, almost half of patients under 30 reported depression, and divorced/widowed patients had higher rates of depression. Health insurance was also associated with higher rates. The study highlights the need for early identification and management of depression, especially among younger, divorced/widowed, insured patients with frequent/severe pain. Our findings demonstrated a significant association between greater severity of SCAand increased likelihood of depression. Compared to the reference group, patients experiencing 5–8 annual SCA pain episodes had 2.004 times higher odds of depression (OR 2.004, 95% CI 1.063–3.781, p = 0.032). This elevated risk further increased to 3.501 times higher odds of depression (OR 3.501, 95% CI 1.957–6.262, p ≤ 0.001) among those with over eight annual SCA pain episodes. Patients reporting SCA pain severity above 7 on a 10-point scale also showed 1.823 times greater odds of depression compared to those with lower pain severity (OR 1.823, 95% CI 1.064–3.122, p = 0.029). Additionally, the length of the longest hospitalization significantly predicted depression risk, wherein each extra day of hospitalization was associated with a 1.348 times increase in the odds of depression (OR 1.348, 95% CI 1.002–1.813, p = 0.048). Overall, our analysis highlights a dose-response relationship between SCA disease severity indicators and depression risk in this population. Policymakers and healthcare providers can improve patient quality of life by addressing psychological/social aspects of the condition.
International studies have shown slightly higher rates of depression, such as a study in Columbia finding 46% [17]. One Saudi study conducted at King Abdelaziz university hospital in Jeddah, KSA showed high rate and reporting 45.4% [9]. Conversely, another one conducted at King Salman Armed Hospital in Tabuk found a lower prevalence of depression of 36% [11]. In addition, an African American study reported a lower prevalence of depression (28%) and a study in Jamaica has also shown a lower prevalence of depression (21.6%) [18,19]. In our study, we used the prevalence of depression reported in a previous Saudi study, which was 45.4% [9]. We chose this prevalence figure because it was the most recent study conducted in Saudi Arabia and had a relatively large sample size. While we did mention another study that reported a higher prevalence of depression (85.9%), this was conducted in a different region of Saudi Arabia and had a smaller sample size. Therefore, we did not use this figure in our calculation of the sample size [10].
Following are those factors that showed a statistically significant association with SCA. In the comparison of social status, divorced and widowed participants had a statistically significant 436% higher rate of reported depression compared to single or married participants as confirmed by regression which is counter to findings in one Saudi study that single patients suffered from higher rates of depression [9]. This may be due to the fact that married patients tend to receive greater support and assistance from their companions compared to divorced and widowed patients with SCA, who may lack social support. A previous study found that participants with at least a bachelor’s degree had a slightly higher incidence (0.6%) of reported depression compared to those with lower education levels [9]. Our findings contradict two other studies reporting higher depression rates among SCA patients with lower education [1,30,31]. This may be attributed to its limited sample size and low generalizability. Furthermore, the other study [30] was conducted in low socioeconomic African settings, making direct comparisons to our Saudi population difficult. Additionally, the categorization of education levels differed between their study [31] and ours. Given these methodological differences, our findings add a unique perspective by demonstrating in a large Saudi sample that higher education is associated with slightly elevated depression risk, unlike in some other populations. More research is needed to elucidate this relationship and identify factors mediating or moderating it. Overall, our study indicates education impacts depression prevalence in SCA, though not always in the expected direction, highlighting the need to consider socio-cultural factors.
Manifestations of pain including frequency of painful episodes and severity of pain correlated with increases in reported depression The result of the analysis of these variables in our study indicates that patients who suffered from more than nine episodes of pain due to SCA in one year had a 250% higher incidence of depression compared to those who had fewer pain episodes. Pain levels of more than seven had 82% higher rates of reported depression compared to participants with lower pain levels. Our findings that pain is related to reported depression is consistent with other authors. In like manner, compared to participants with fewer hospital days, those who had longer hospitalization had a 35% higher incidence of depression. This finding may be the first as, to our knowledge, no other authors have reported it. These findings are consistent with the majority of prior studies, as with more severe disease, frequent pain episodes, and longer hospitalization, patients are more prone to being depressed [4,6,19,31].
Our findings contradict one Brazilian study [18] that found no difference in healthcare utilization between depressed and non-depressed SCD patients, despite depressed patients having more severe disease. The discrepancy may be attributed to their focus on opioid analgesic use, a controlled medication, which could obscure differences. In alignment with meta-analyses [16], our data indicates depressed patients utilize more healthcare, irrespective of opioid use.
Furthermore, we found no link between depression and the total number of hospital visits, which is consistent with the findings of one study [18], while other studies show a higher risk of depression in individuals who frequently visit the hospital or clinic [1,16,31].
The current study did not show a significant association between depressive symptoms and sociodemographic factors like age and gender. However, regarding gender, our results showed the depression rate among females was higher than males (p > 0.05). These findings are consistent with many international studies that state that female patients with SCA have more depressive symptoms than male patients [1,30]. Similarly, one national study conducted in Tabuk agreed that female people patients have a higher depression rate [11]. This may be due to the hormonal effects, or the increased burden of care borne by females, especially if the patients with SCA had a child with SCA. On the other hand, there is one study conducted at King Abdulaziz University Hospital that opposes these results and states that the rate of depression in men is higher than in females [9]. When comparing depression rates across different age groups, these findings failed to show any statistical significance, agreeing with many other studies [11,31]. Many studies have revealed that patients with a positive SCA family history were more depressed than those without [9,11]. This could be because these individuals have at least one family member who has the same disease, which can have a spontaneous negative psychological effect on the patient. However, we found that this relation is not entirely significant.
Regarding occupational status, our research found no association between depression and occupational status in SCA patients, consistent with a previous study [31]. The similarity in findings may be attributed to conducting both studies in different cities within Saudi Arabia but with comparable populations. As mentioned previously, a comprehensive management plan for patients with SCA must include a mental health assessment and appropriate treatment to enhance their quality of life. Our findings provide valuable insights for policymakers, highlighting the need to address mental health alongside the medical aspects of SCA. This approach aligns with the healthcare reforms under Vision 2030’s New Model of Care, aiming for optimum healthcare quality. To fully integrate mental health care into the best practices for SCA management, the education of both physicians and patients is recommended to enhance awareness of the problem and its effects on the overall health of patients with SCA. Further studies are needed to determine cause and effect of the presence of depressive symptoms in patients with SCA so that the factors that are most important may be solved to give patients with SCA a better quality of life. Longitudinal studies documenting the mental health changes in SCA patients over time should be conducted to give physicians information about the stages to closely monitor with their patients.
This study provides decision-makers with the scope of psychological problems facing patients with SCA and the urgency of addressing their mental health needs since ap-proximately 42% of patients with SCA suffer from depression. We suggest that the first step is to provide a mental health evaluation to all patients with SCA at diagnosis as well as routine follow up as early detection and management of mental health symptoms will help mitigate the impacts on their disease. The second important step is that parents should be provided with educational interventional programs to deal with their children’s mental status. Finally, social awareness and support for SCA patients may improve their mental health status in living with this chronic disease.
This study has several limitations worth noting. The cross-sectional design precludes determining causal relationships between sickle cell disease severity indicators and depression. Additionally, we did not account for potential effects of the COVID-19 pandemic on measured depression prevalence [32]. Further research should investigate these temporal associations through longitudinal follow-up. The single-center nature of this study may limit generalizability of findings to the broader Saudi sickle cell disease population. As sickle cell disease is common nationwide, larger multi-center studies are needed. Although we identified multiple SCA factors associated with depression risk, our analysis could not elucidate underlying mechanisms or directionality. Future studies should incorporate mediation analyses to explicate pathways linking disease severity markers to depressive symptoms emergence. Finally, we did not examine relationships between depression and quality of life domains. Incorporating health-related quality of life measures would provide further insights into the patient experience and functional impacts of comorbid mood disorders.
The reported 42% prevalence of depression among SCA patients in the Jazan region is cause for concern. In addition, there are several statistically significant determinants associated with higher rates of depression, in descending order: Being divorced or widowed, the disease indicators of increasing pain episode frequency and severity, increased LOS due to severity and complication of diseases (longest hospitalization history), and finally, those with a bachelor’s degree or higher had a slightly higher rate of reported depression. This study supports the need for comprehensive management of SCA in closing symptoms of depression. Further study is needed to identify the causal factors for depression in patients with SCA to alleviate the concurrent suffering experienced by these patients.
Acknowledgement: We would like to extend our deepest gratitude to the Department of Family and Community Medicine at the Faculty of Medicine for their unwavering support throughout this study. Their guidance and mentorship have been invaluable. We also express our heartfelt appreciation to the staff of the Hematology Center at Prince Mohammed bin Nasser Hospital (PMNH) for their dedication and cooperation. Their commitment to patient care has been instrumental in the successful execution of this research. This work was made possible by the funding support from the Deanship of Scientific Research at Jazan University. Their financial endorsement played a pivotal role in the successful execution of our research. We are deeply thankful for their commitment to fostering a conducive environment for scientific inquiry and advancement.
Funding Statement: This research was funded by the Deanship of Scientific Research at Jazan University.
Author Contributions: Conceptualization, A.A. and N.A.; Data curation, A.A., A.Y.A., N.A., R.A., A.M.A., H.M., M.B., and A.M.; Formal analysis, A.A., N.A., R.A., F.A., S.M., I.O., G.A., and Y.A.; Funding acquisition, A.A.; Investigation, A.A., A.Y.A., M.M., N.A., and G.A.; Methodology, A.A., M.M., N.A., R.A., F.A., S.M., and G.A.; Project administration, A.A., N.A., A.M.A., H.M., M.B., and A.M.; Resources, A.A., N.A., I.O., G.A., Y.A., and M.B.; Software, A.A., N.A., R.A., F.A., S.M., I.O., G.A., and Y.A.; Supervision, A.A., A.Y.A., A.M.A., H.M., and A.M.; Validation, A.A., A.Y.A., M.M., N.A., S.M., I.O., and Y.A.; Visualization, A.A., A.M.A., H.M., M.B., and A.M.; Writing–original draft, A.A., A.Y.A., M.M., N.A., R.A., F.A., S.M., I.O., and G.A.; Writing–review & editing, A.A., A.Y.A., M.M., and N.A.
Availability of Data and Materials: The datasets generated and/or analyzed during the current study are not publicly available due to privacy and ethical restrictions. However, they are available from the corresponding author on reasonable request.
Ethics Approval: The Institutional Review Board of the Jazan Health Ethics Committee of the Ministry of Health, Saudi Arabia approved the ethics of this study. Approval Number 2203, on 11th January 2022. Those who agreed to participate were taken to a private room to read and understand the informed consent before filling out the questionnaire.
Conflicts of Interest: The authors declare no conflict of interest.
References
1. Hasan SP, Hashmi S, Alhassen M, Lawson W, Castro O. Depression in sickle cell disease. J Natl Med Assoc. 2003;95(7):533–7 [Google Scholar] [PubMed]
2. Aylor C, Parsonage M, McDaid D, Knapp M, Fossey M, Galea A. Long-term conditions and mental health: the cost of co-morbidities; 2012. [Google Scholar]
3. Ballas SK, Lieff S, Benjamin LJ, Dampier CD, Heeney MM, Hoppe C, et al. Definitions of the phenotypic manifestations of sickle cell disease. Am J Hematol. 2010;85(1):6–13. doi:10.1002/ajh.21550 [Google Scholar] [PubMed] [CrossRef]
4. Wison Schaeffer JJ, Gil KM, Burchinal M, Kramer KD, Nash KB, Orringer E, et al. Depression, disease severity, and sickle cell disease. J Behav Med. 1999;22(2):115–26. doi:10.1023/A:1018755831101 [Google Scholar] [PubMed] [CrossRef]
5. Alanazi N. Clinical guidelines for management of acute painful episodes of vaso-occlusive crisis in children with sickle cell disease. Adv Life Sci. 2021;8(3):221–7. [Google Scholar]
6. Adam SS, Flahiff CM, Kamble S, Telen MJ, Reed SD, De Castro LM. Depression, quality of life, and medical resource utilization in sickle cell disease. Blood Adv. 2017;1(23):1983–92. doi:10.1182/bloodadvances.2017006940 [Google Scholar] [PubMed] [CrossRef]
7. Jastaniah W. Epidemiology of sickle cell disease in Saudi Arabia. Ann Saudi Med. 2011;31(3):289–93. doi:10.4103/0256-4947.81540 [Google Scholar] [PubMed] [CrossRef]
8. Alhamdan NA, Almazrou YY, Alswaidi FM, Choudhry AJ. Premarital screening for thalassemia and sickle cell disease in Saudi Arabia. Genet Med. 2007;9(6):372–7. doi:10.1097/GIM.0b013e318065a9e8 [Google Scholar] [PubMed] [CrossRef]
9. Al-Marzouki AF, Alrefaie NI, Aljohani NA, Alandanusi RA, Alghamdi AA, Radhwi OO. The prevalence of depression and anxiety among sickle cell disease patients in king Abdulaziz University hospital. Cureus. 2021;13(9):e18374. doi:10.7759/cureus.18374 [Google Scholar] [PubMed] [CrossRef]
10. Alsubaie SS, Almathami MA, Abouelyazid A, Alqahtani MM. Prevalence of depression among adults with sickle cell disease in the southern region of Saudi Arabia. Pak J Med Sci. 2018;34(4):929–33. doi:10.12669/pjms.344.14760 [Google Scholar] [PubMed] [CrossRef]
11. Al Zahrani OS, Mukhtar O, Al Subaie M, Al Howiti WE. Systematic psychiatric assessment of patients with sickle cell disease. Saudi Med J. 2019;40(1):59–65. doi:10.15537/smj.2019.1.22919 [Google Scholar] [PubMed] [CrossRef]
12. Abu-Shaheen A, Dahan D, Henaa H, Nofal A, Abdelmoety DA, Riaz M, et al. Sickle cell disease in gulf cooperation council countries: a systematic review. Expert Rev Hematol. 2022;15(10):893–909. doi:10.1080/17474086.2022.2132225 [Google Scholar] [PubMed] [CrossRef]
13. Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis. 2005;2(1):A14 [Google Scholar] [PubMed]
14. DeJean D, Giacomini M, Vanstone M, Brundisini F. Patient experiences of depression and anxiety with chronic disease: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013;13(16):1–33. [Google Scholar]
15. Edwards CL, Green M, Wellington CC, Muhammad M, Wood M, Feliu M, et al. Suicidal ideation, and attempts in black patients with sickle cell disease. J Natl Med Assoc. 2009;101(11):1090–5. doi:10.1016/s0027-9684(15)31103-2. [Google Scholar] [CrossRef]
16. Jonassaint CR, Jones VL, Leong S, Frierson GM. A systematic review of the association between depression and health care utilization in children and adults with sickle cell disease. Br J Haematol. 2016;174(1):136–47. doi:10.1111/bjh.14023 [Google Scholar] [PubMed] [CrossRef]
17. Jerrell JM, Tripathi A, McIntyre RS. McIntyre, prevalence and treatment of depression in children and adolescents with sickle cell disease: a retrospective cohort study. Prim Care Companion CNS Disord. 2011;13(2):13–2. doi:10.4088/PCC.10m01063. [Google Scholar] [CrossRef]
18. Levenson JL, McClish DK, Dahman BA, Bovbjerg VE, de Citero AV, Penberthy LT, et al. Depression and anxiety in adults with sickle cell disease: the PiSCES project. Psychosom Med. 2008;70(2):192–6. doi:10.1097/PSY.0b013e31815ff5c5 [Google Scholar] [PubMed] [CrossRef]
19. Asnani MR, Fraser R, Lewis NA, Reid ME. Depression and loneliness in Jamaicans with sickle cell disease. BMC Psychiatry. 2010;10(1):40. doi:10.1186/1471-244X-10-40 [Google Scholar] [PubMed] [CrossRef]
20. Oudin Doglioni D, Chabasseur V, Barbot F, Galactéros F, Gay MC. Depression in adults with sickle cell disease: a systematic review of the methodological issues in assessing prevalence of depression. BMC Psychol. 2021;9(1):54. doi:10.1186/s40359-021-00543-4 [Google Scholar] [PubMed] [CrossRef]
21. Dos Santos JP, Gomes Neto M. Sociodemographic aspects and quality of life of patients with sickle cell anemia. Rev Bras Hematol Hemoter. 2013;35(4):242–5. doi:10.5581/1516-8484.20130093 [Google Scholar] [PubMed] [CrossRef]
22. Raphael JL, Dietrich CL, Whitmire D, Mahoney DH, Mueller BU, Giardino AP. Healthcare utilization and expenditures for low income children with sickle cell disease. Pediatr Blood Cancer. 2009;52(2):263–7. doi:10.1002/pbc.21781 [Google Scholar] [PubMed] [CrossRef]
23. Kanter J, Bhor M, Li X, Li FY, Paulose J. High healthcare utilization in adolescents with sickle cell disease prior to transition to adult care: a retrospective study. J Health Econ Outcomes Res. 2019;6(3):174–84. doi:10.36469/10512 [Google Scholar] [PubMed] [CrossRef]
24. Abushagah TM, Alsomaili M, Solan YO, Marran NM, Masmali AM. Prevalence of depression among sickle cell anemia patients in Jazan, Saudi Arabia. Int J Med Dev Countries. 2019;3(2):1–15. doi:10.24911/IJMDC.51-1546561408. [Google Scholar] [CrossRef]
25. AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, et al. An Arabic translation, reliability, and validation of patient health questionnaire in a saudi sample. Ann Gen Psychiatry. 2017;16(1):32. doi:10.1186/s12991-017-0155-1 [Google Scholar] [PubMed] [CrossRef]
26. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi:10.1046/j.1525-1497.2001.016009606.x [Google Scholar] [PubMed] [CrossRef]
27. Razykov I, Ziegelstein RC, Whooley MA, Thombs BD. The PHQ-9 versus the PHQ-8--is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the heart and soul study. J Psychosom Res. 2012;73(3):163–8. doi:10.1016/j.jpsychores.2012.06.001 [Google Scholar] [PubMed] [CrossRef]
28. Lazic SE. Four simple ways to increase power without increasing the sample size. Lab Anim. 2018;52(6):621–9. doi:10.1177/0023677218767478 [Google Scholar] [PubMed] [CrossRef]
29. Alhalafi AH. Prevalence of anxiety and depression during the coronavirus disease 2019 pandemic in Riyadh, Saudi Arabia: a web-based cross-sectional survey. J Pharm Res Int. 2020;32(27):65–73. doi:10.9734/jpri/2020/v32i2730857. [Google Scholar] [CrossRef]
30. Adzika VA, Glozah FN, Ayim-Aboagye D, Ahorlu CSK. Socio-demographic characteristics and psychosocial consequences of sickle cell disease: the case of patients in a public hospital in Ghana. J Health Popul Nutr. 2017;36(1):4. doi:10.1186/s41043-017-0081-5 [Google Scholar] [PubMed] [CrossRef]
31. Alhomoud MA, Gosadi IM, Wahbi HA. Depression among sickle cell anemia patients in the eastern province of Saudi Arabia. Saudi J Med Med Sci. 2018;6(1):8–12. doi:10.4103/sjmms.sjmms_123_16 [Google Scholar] [PubMed] [CrossRef]
32. Alharbi A. The prevalence of depression and related factors during the COVID-19 pandemic among the general population of the Jazan Region of Saudi Arabia. Cureus. 2022;6, 14(2):e21965. doi:10.7759/cureus.21965 [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools