 Open Access
Open Access
ARTICLE
Validity and Reliability of a Mental Health Recovery Checklist for Young Adults
1 Research Department, The Dorm, New York, 10023, USA
2 Department of Educational Psychology, Ball State University, Muncie, 47306, USA
* Corresponding Author: Brianna Cerrito. Email:
International Journal of Mental Health Promotion 2024, 26(4), 317-323. https://doi.org/10.32604/ijmhp.2024.047876
Received 20 November 2023; Accepted 01 March 2024; Issue published 04 May 2024
Abstract
The purpose of the present study is to evaluate the internal consistency and construct validity of a self-report checklist measuring clinical mental health recovery across six key domains: family and relationships, occupation and school, physical health, mental health, spirituality, and social support systems. The Mental Health Recovery Checklist (MHRC) was developed at The Dorm, an intensive outpatient mental health treatment program for young adults in New York, NY, and Washington DC that services individuals between the ages of 18 and 35 years old. The present study is cross-sectional, as data were pulled from clients’ records who were discharged between January 2018 and May 2023. Pearson Correlations and Cronbach’s alpha were used to determine scale reliability. To establish validity, an Exploratory Factor Analysis (EFA) was conducted to assess a single-factor model using Principal Axis Factoring. Cronbach’s alpha was high (α = 0.88), indicating good reliability. In the EFA, all items loaded strongly on a single factor. The unidimensional structure revealed in the EFA highlights the interconnected nature of various life domains as they pertain to mental health recovery in young adults. Future research is warranted to explore whether there are additional dimensions of mental health recovery that have not been assessed in the present scale.Keywords
Research cites that there is variation and ambiguity in defining the construct of mental health recovery [1]. While some agreement exists in the field on guiding principles for recovery (i.e., individualized, or person-centered experience; feelings of empowerment, purpose, and hope), there is little experimental research uncovering the specific domains that encompass mental health recovery. The World Health Organization defines mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community” [2]. This definition is also consistent with that of the word “flourishing” [3]. Furthermore, Deegan [4] has defined the concept of mental health recovery as acceptance in the face of overcoming mental illness. Given these conceptual definitions, it is understood that to attain a state of mental well-being, certain domains in one’s life (i.e., community, work) must be in harmony [2–4].
Research strongly points to quality of relationships, job status, physical health, mental well-being, and spiritual practice as indicators of clinical mental health recovery [5–9]. For example, it is clearly indicated in the literature that having a steady occupation or academic pursuit and experiencing supportive relationships can foster feelings of belongingness, importance, and capability [5,7,8]. Physical health, too, not only improves mood but can prevent health issues that are shown to have negative impact on mental well-being (i.e., type II diabetes, cardiovascular disease, cancer) [6,9,10]. There is some conflicting literature on the relationship between spirituality and mental health. Tuck et al. [3] discussed mental health recovery, coining spirituality as a “pathway to resilience” and suggests that factors such as forgiveness, flourishing, and resilience, are related conceptual expressions of spirituality that can facilitate mental health recovery [3]. On the other hand, research focusing on the construct of mental health points to the damage that can be caused by negative spiritual or religious coping (i.e., suicidal ideation, substance use, anxiety) [11].
While many tools are available to measure distinct facets of mental health recovery, there is a gap in the published literature on valid and reliable measurement devices for assessing mental health recovery as a unified construct. The goal of the present study is to evaluate internal consistency and construct validity of a scale developed by The Dorm, an intensive outpatient mental health treatment program for young adults in New York, NY and Washington DC. The Mental Health Recovery Checklist (MHRC) assesses six domains related to mental health recovery (family and relationships, occupation and school, physical health, mental health, spirituality, and social support systems).
Checklists for measuring clinical recovery
One theoretical research paper posits a bi-directional relationship between 8 dimensions of overall young adult development similar to that of the MHRC (i.e., physical health, psychological and emotional well-being, life skills, ethical behavior, healthy family and social relationships, educational attainment, constructive educational and occupational engagement, civic engagement) [12]. While many scales exist to measure mental health recovery, as outlined in Sklar et al. [13], it is noted that many of the existing instruments are multi-factor scales, whereas the present study is seeking to evaluate a single factor covered in 6 items [13].
A 2014 psychometric evaluation of the Dutch version of the Mental Health Recovery Measure (MHRM) found the following to be subfactors of mental health recovery (i.e., overcoming stuckness, self-empowerment, learning and self-redefinition, basic functioning, overall well-being, new potentials, advocacy/enrichment, and spirituality) [14]. However, these domains do not take into account community and social factors. Whereas, The Recovery Process Inventory (RPI) identifies six factors related to recovery, such as anguish, connected to others, confidence and purpose, others’ care and help, good living situation, and hopeful/cares for self, which fail to account for important factors like occupation and academic goals [15].
While there is some evidence suggesting an underlying theoretical framework surrounding mental health recovery, despite extensive literature review, there is a lack of brief validated checklists to measure mental health recovery as a unidimensional construct [12]. The present study aims to assess the validity and reliability of a short checklist measuring six all-encompassing factors related to mental health recovery.
Research shows that higher levels of reciprocal family support is associated with a willingness to seek help or assistance, which in turn contributes to greater likelihood of mental health recovery [16]. Further, reciprocity of family support networks correlates positively with self-confidence, self-esteem, and optimism about recovery [16]. While close social relationships have the potential to be both supportive and harmful to mental health, research indicates that, collectively, all social contact is more beneficial than no social contact at all [17]. In family systems with higher levels of warmth, positive regard, and mutuality, relationships with family members provided moral support, practical support, and intrinsic motivation for recovery [18]. Furthermore, the benefits of strong friendships include social connectedness, feelings of support, companionship, and promotion of a healthier sense of self [19].
Employment research clearly outlines the benefit of occupational engagement in the mental health recovery process (i.e., structure and routine, purpose, connectedness, meaningfulness, sense of identity) [20]. Research in clinically acute populations indicates that work provides personal meaning through its impact on pride, self-esteem, and financial benefit, as well as overall mental health recovery [21]. Work is also perceived as an intrinsic motivator because the sense of achievement and personal empowerment that comes with employment contributes to restoration of mental well-being [22]. Research also demonstrates a strong correlation between higher academic achievement and positive mental health [23].
Physical health is important for mental well-being and the recovery process. Research strongly indicates a link between chronic conditions (e.g., cardiovascular disease, diabetes, obesity) and mental illness (e.g., depression, bipolar disorder, and schizophrenia) [24–27]. Additionally, many studies demonstrate that higher levels of physical activity are associated with reduction in symptoms of depression as well as improvements in quality of life among those with mental health disorders [28,29]. Taken together, physical health is an important aspect of the recovery process.
Positive mental health can be defined as not only the absence of symptoms but incorporates the presence of positive emotional states, acceptance, resilience, and overall quality of life [30]. Research clearly demonstrates that mental health and well-being are associated with a decrease in the intensity of mental illness symptoms in various populations [31–34]. Additionally, research shows that as individuals recover from mental health issues, they are better able to set long-term and broader goals in various areas of life (i.e., employment, physical health), as well as experience increased productivity and higher levels of performance in the workplace compared to individuals with active symptoms [35,36].
When defining spirituality in the literature, there is controversy over the complex and multidimensional nature of this concept, and how it is defined (as separate from religion) [37]. Many studies combine the two concepts of religion and spirituality. Spirituality and religion were found to be significantly related to altruism and can potentially act as a source of hope and connection in individuals with mental illness [38]. Additionally, a 2009 review on spirituality, religion, and mental health found that a large portion of the identified studies indicate lower rates of suicide, substance use, and depression in those who identified as religious; however, a flat side to religious beliefs is that religious-related delusions were found to be common in people with psychotic disorders [39]. Other research indicates that utilizing negative religious coping, or manifesting extrinsic religious and spiritual orientation is associated with lower overall well-being [11]. Spirituality is of particular interest in the validation of the MHRC due to the controversial nature of the literature.
Research indicates that social support (i.e., friends, family members, and a larger sense of community) plays a significant role in improving mental health and protecting against onset of mental illness (i.e., anxiety and depression) [40,41]. Important factors of social support include level of engagement within the community and reported satisfaction with members of the social support system, such that higher engagement in community activities and higher self-reported satisfaction with social networks is associated with stronger mental health recovery [42,43]. Research also strongly suggests a bi-directional relationship between social support and recovery, such that those performing altruistic acts of service are more likely to experience greater well-being and mental health, as these types of activities help individuals to feel valued and respected by those they are helping [44,45].
The study was approved by the Institutional Review Board at Ball State University (IRB number: 2000946-1). Data was collected via retrospective chart review; thus, the IRB waived the requirement for signed informed consent.
The study was cross-sectional, as data were pulled from clients’ records who were discharged between January 2018 and May 2023. A total of 574 client charts were selected. However, clients were removed from the study if 1) the client’s age was below 18 or more than 35, upon admission, and 2) if any item on the MHRC scale was left blank. In cases where more than one choice was selected for a particular item on the scale, the average score was taken, and the client’s data was included in the study. A total of 351 client charts fit the indicated criteria and were included in analysis.
The Dorm is an intensive outpatient mental health treatment program for young adults that services individuals between the ages of 18 and 35 years old. Over 80% of clients at The Dorm are multi-diagnostic, indicating that they have more than one co-occurring mental health disorder, including anxiety, depression, psychotic disorders, substance use disorders, personality disorders, and eating disorders. Licensed clinical social workers serve as therapists and clinical coaches who meet with clients individually and facilitate group sessions, which make up a majority of the programming at The Dorm, which is community oriented. Empirically supported behavioral psychosocial methodologies are utilized to serve a variance of mental health illnesses and co-occurring disorders. Average length of stay at The Dorm is one year.
The scale being assessed for reliability and validity is The Dorm’s MHRC. This tool measures mental health recovery across six domains: family/relationships, occupation/school, physical health, mental health, spirituality, social support systems. Each item is rated on a 5-point Likert scale (1 = poor, 5 = excellent) (Table 1).
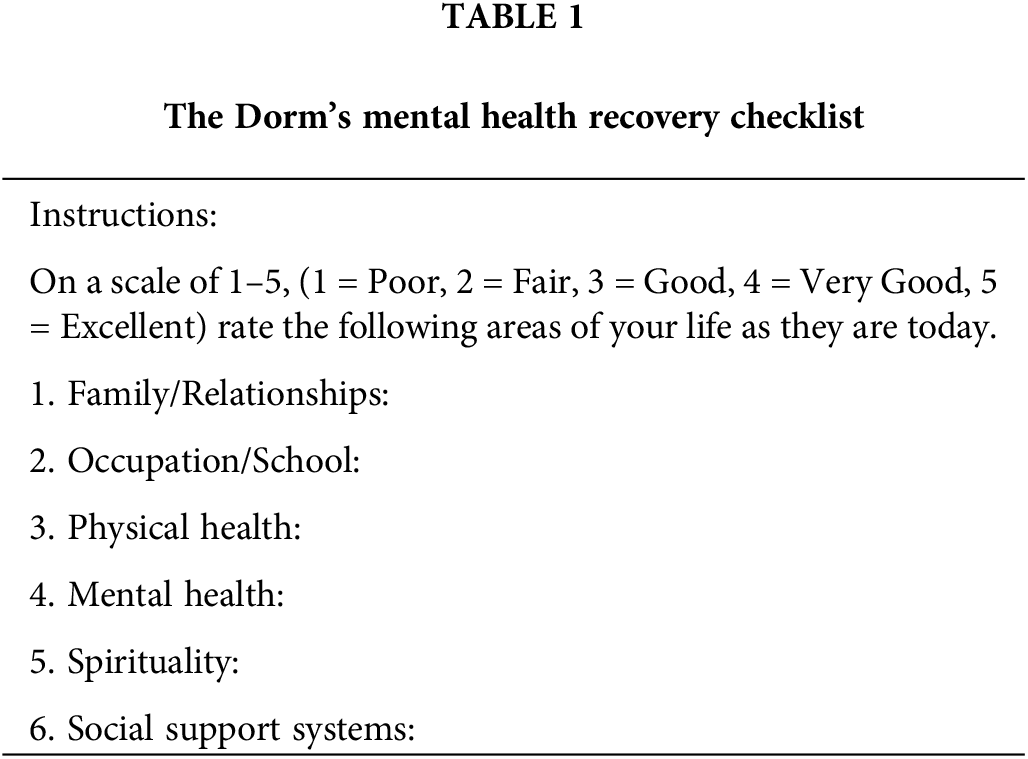
The MHRC is a self-report checklist where clients indicate, at discharge, a rating for each domain. There are a total of 6 items, one item per recovery domain. In responding to the survey, clients are instructed to “rate the following areas of your life as they are today.”
Data were analyzed using SPSS for Mac, version 29.0.1.0. Pearson Correlations and Cronbach’s alpha were used to determine scale reliability. To establish validity, an Exploratory Factor Analysis (EFA) was conducted to assess a single-factor model using Principal Axis Factoring. Prior, KMO and Bartlett’s Test of Sphericity were conducted to ensure the factorial solution was appropriate. Additionally, a two-factor model was assessed via Principal Axis Factoring and Varimax Rotation with Kaiser Normalization. Due to the exploratory nature of this analysis, not knowing how these factors would load, we tested a number of factor structures. Descriptive statistics have been reported below.
Mean age of participants was 22.03 (SD = 3.37). Of 351 participants, 144 individuals identified as cisgender female, 127 identified as cisgender male, 26 identified as transgender non-binary (TGNB), 4 were undecided/exploring, and a total of 50 individuals did not disclose their gender.
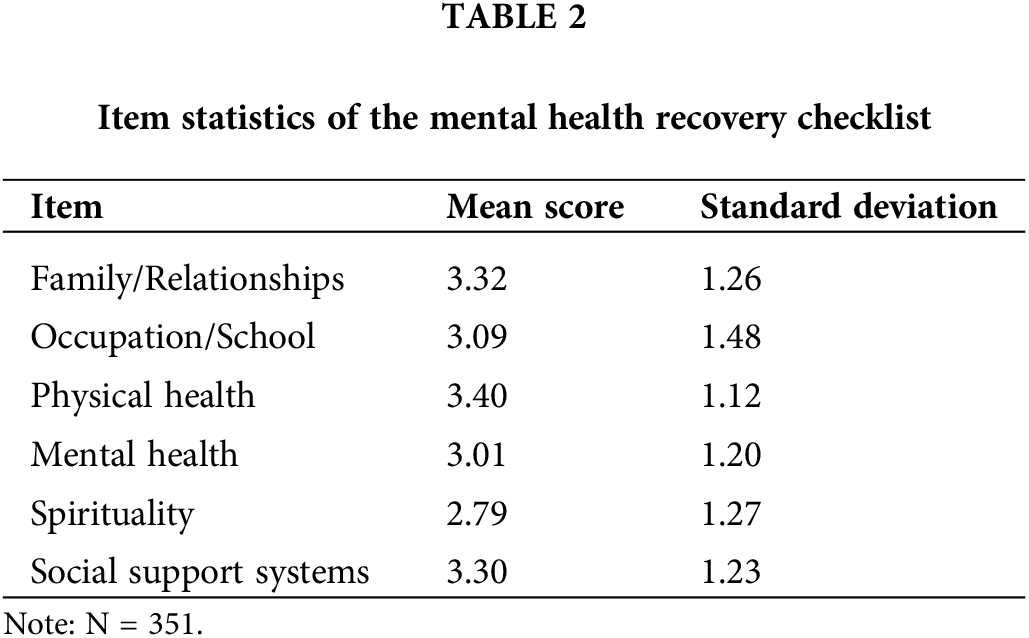
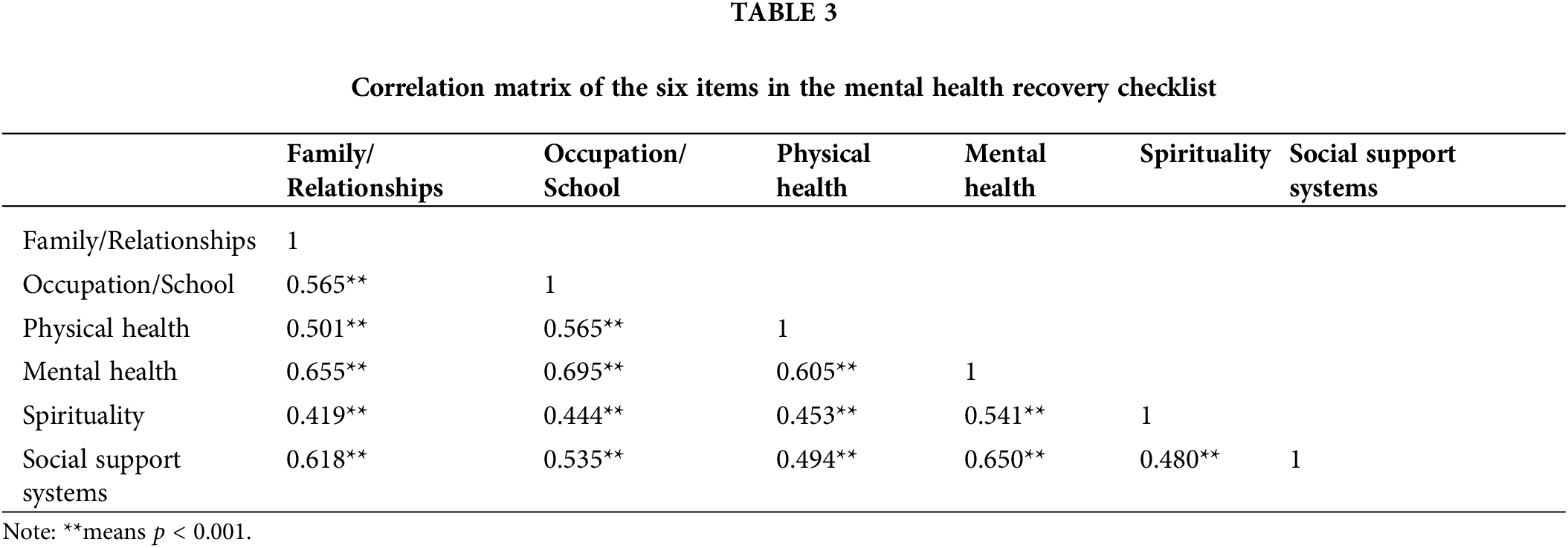
Item means were above 3.0 (M = 3.01–3.40) except for spirituality (M = 2.79) (Table 2). The correlation matrix of item pairs indicated statistical significance across all pairs (p < 0.01) (Table 3). The Family/Relationships, Occupation/School, and Social Support Systems domains were strongly correlated with each other (coefficient range: 0.54 to 0.62). Spirituality was moderately correlated with the other variables (coefficient range: 0.42 to 0.54). Mental Health, in particular, was most strongly correlated with each of the domains on the checklist (coefficient range: 0.61–0.70), with the exception of spirituality (coefficient: 0.54). Cronbach’s alpha was high (α = 0.88).
Kaiser-Meyer-Olkin measure of sampling adequacy was 0.892, above the recommended value of at least 0.50 [46]. Bartlett’s test of sphericity was significant (χ2 = (15) = 1007.800, p < 0.001). To determine the number of factors to extract, a scree plot of the eigenvalues was examined using the ‘elbow criterion,’ where the tapering off of the plot clearly indicated a unidimensional structure [47].
The exploratory factor analysis revealed that a unidimensional factor accounts for 56% of the variance in the data. The factor matrix (Table 4) shows that all items loaded strongly on the single factor, with a loading range from 0.61 to 0.88. The results of the exploratory factor analysis for a two-factor model resulted in cross-loadings across every domain, further supporting the evidence of a single-factor structure.
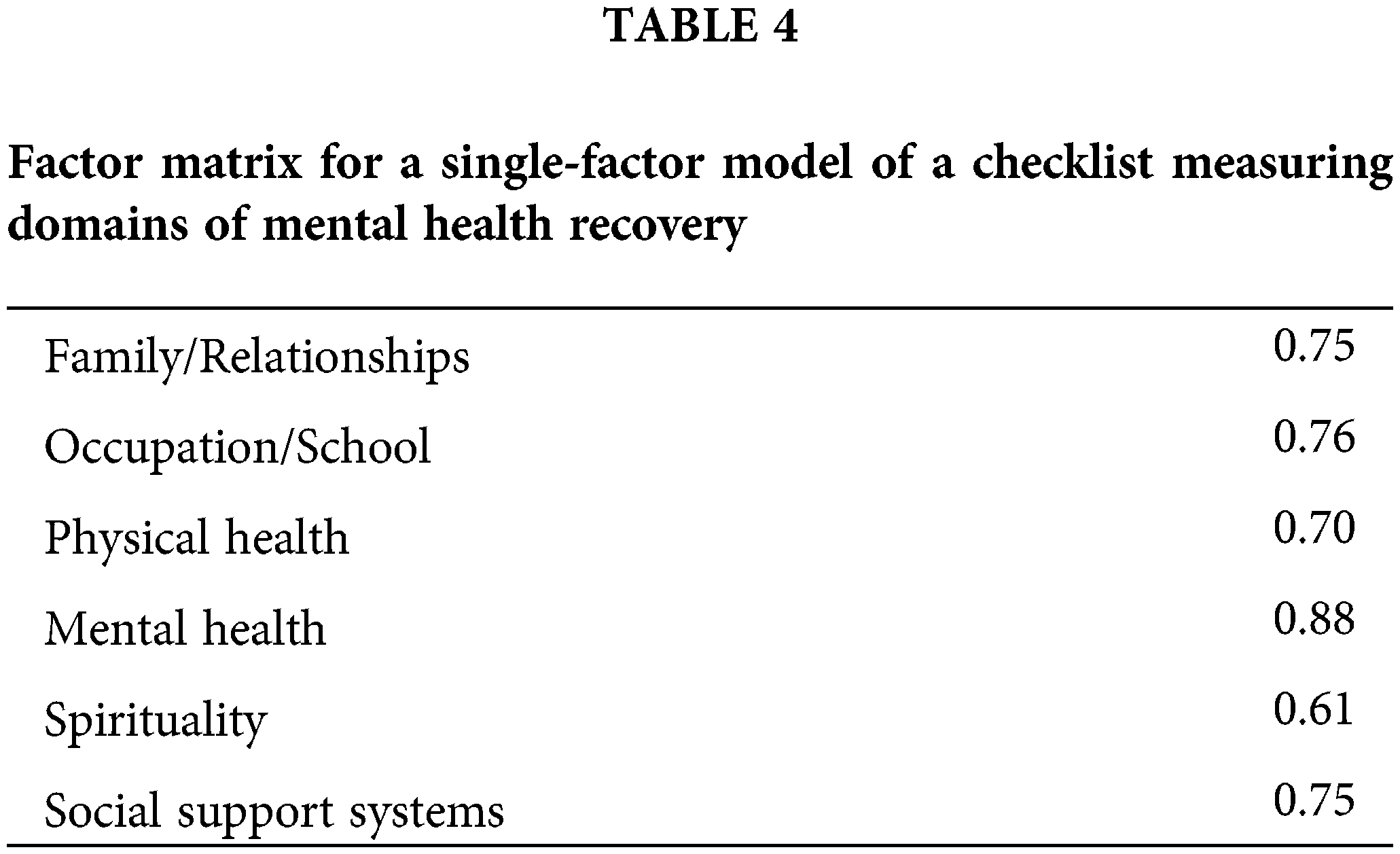
Results indicate that MHRC has good reliability and validity in assessing mental health recovery. A unidimensional structure accounts for a substantial proportion (56%) of the variance in the data. This unidimensional structure suggests that the variables within the MHRC checklist share a common underlying construct, pointing towards a unified concept of various life domains. The strong factor loadings observed across all items (ranging from 0.61 to 0.88) on the single factor further bolster the evidence for the unidimensional structure.
The findings of this study hold important implications for both research and practical application. The unidimensional structure revealed by the factor analysis highlights the interconnectedness of various life domains as they pertain to mental health recovery, emphasizing the complex interplay between different facets of young adults’ lives. This interconnectedness may offer support for a holistic approach when addressing well-being and mental health, recognizing that improvements in one domain can potentially have positive spillover effects on others.
Each item on the MHRC scale has been identified as clinically relevant for clients of The Dorm and empirically supported by the literature as important areas for whole-person mental health recovery [5–9]. The spirituality item, in particular, offers unique perspectives that contribute to the holistic understanding of well-being and mental health. Our findings demonstrate that the spirituality item exhibited moderate correlations with the other variables, particularly within the mental health and social support domains. However, while not as strongly correlated as other variables, spirituality does contribute to the unidimensional structure revealed by the factor analysis conducted and is clearly correlated with other dimensions of clinical recovery for young adults. Spirituality does not stand out as a dominant factor in this study, but interacts with mental health and social support dimensions, which have the potential to influence individuals’ overall clinical recovery [11]. Developmental theorists suggest that young adulthood includes a period of psychosocial conflict that can result in existential crisis (i.e., issues concerning morals, values, purpose). The spirituality item’s moderate correlation with the other variables on the scale may suggest that spirituality is context-dependent, such that higher levels of spirituality could be more strongly associated with these domains compared to those with lower levels of spirituality [48]. Future research should explore these subgroups further, which could lead to targeted interventions to acknowledge and leverage spirituality as a potential moderator in the relationship between different life domains.
Future research is warranted to explore whether there are additional dimensions of mental health recovery that have not been assessed in the present scale. For example, research shows that mental health recovery involves the development of a sense of meaning and purpose in life [49].
Furthermore, generalizability is limited, as the present sample only includes young adults who sought private intensive outpatient mental health treatment in New York City and Washington DC. Other studies should consider diversity of population across several demographics (i.e., socioeconomic status). For example, economic factors can significantly impact access to resources, opportunities, and the ability to engage in certain occupations or maintain physical and mental health.
Additionally, the authors did not have access to repeated measures data, which is important for future research to consider. Repeated measures in future studies would enable a longitudinal assessment of individual mental health recovery over time, allowing for tracking dynamic patterns of progress and fluctuations, offering a more nuanced understanding of the trajectory of mental health recovery during treatment, and not only post-discharge.
Acknowledgement: We would like to thank the editors and reviewers of this journal for their time and feedback in finalizing this paper.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Cerrito, B., Bolin, J.; data collection: Cerrito, B.; analysis and interpretation of results: Cerrito, B., Bolin, J.; draft manuscript preparation: Xiao, J., Cerrito, B., Fialk, A., DiTomasso, A. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data was collected from a mental health treatment program for young adults. Due to the confidential nature of this information, raw data cannot be accessed.
Ethics Approval: The study was approved by the Institutional Review Board at Ball State University (IRB number: 2000946-1). Data was collected via retrospective chart review; thus, the IRB waived the requirement for signed informed consent.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Ellison ML, Belanger LK, Niles BL, Evans LC, Bauer MS. Explication and definition of mental health recovery: a systematic review. Adm Policy Ment Health Ment Health Serv Res. 2016;45(1):91–102. doi:10.1007/s10488-016-0767-9. [Google Scholar] [PubMed] [CrossRef]
2. World Health Organization. Promoting mental health: concepts, emerging evidence, practice. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
3. Tuck I, Forgiveness L. Forgiveness, flourishing, and resilience: the influences of expressions of spirituality on mental health recovery. Issues Ment Health Nurs. 2014;35(4):277–82. doi:10.3109/01612840.2014.885623. [Google Scholar] [PubMed] [CrossRef]
4. Deegan PE. Recovery: the lived experience of rehabilitation. Psychosoc Rehabil J. 1988;11(4):11–9. doi:10.1037/h0099565. [Google Scholar] [CrossRef]
5. Andersen MF, Svendsen PA, Nielsen K, Brinkmann S, Rugulies R, Madsen IEH. Influence at work is a key factor for mental health-but what do contemporary employees in knowledge and relational work mean by “influence at work”? Int J Qual Stud Health Well-Being. 2022;17(1). doi:10.1080/17482631.2022.2054513. [Google Scholar] [PubMed] [CrossRef]
6. Carney R, Imran S, Law H, Firth J, Parker S. Physical health interventions on adolescent mental health in client units: a systematic review and call to action. Early Interv Psychiatry. 2020;15:439–48. doi:10.1111/eip.12981. [Google Scholar] [PubMed] [CrossRef]
7. Gao S, Assink M, Cipriani A, Lin K. Associations between rejection sensitivity and mental health outcomes: a meta-analytic review. Clin Psychol Rev. 2017;57:59–74. doi:10.1016/j.cpr.2017.08.007. [Google Scholar] [PubMed] [CrossRef]
8. Hogue A, Becker SJ, Wenzel K, Henderson CE, Bobek M, Levy S, et al. Family involvement in treatment and recovery for substance use disorders among transition-age youth: research bedrocks and opportunities. J Subst Abuse Treat. 2021;129:108402. doi:10.1016/j.jsat.2021.108402. [Google Scholar] [PubMed] [CrossRef]
9. Ungar M, Theron L. Resilience and mental health: how multisystemic processes contribute to positive outcomes. Lancet. 2020;7(5):441–8. doi:10.1016/S2215-0366(19)30434-1. [Google Scholar] [PubMed] [CrossRef]
10. Mahindru A, Patil P, Agrawal V. Role of physical activity on mental health and well-being: a review. Cureus. 2023;15(1):e33475. doi:10.7759/cureus.33475. [Google Scholar] [PubMed] [CrossRef]
11. Weber SR, Pargament KI. The role of religion and spirituality in mental health. Curr Opin Psychiatry. 2014;27(5):358–63. doi:10.1097/yco.0000000000000080. [Google Scholar] [PubMed] [CrossRef]
12. Scales PC, Benson PL, Oesterle S, Hill KG, Hawkins JD, Pashak TJ. The dimensions of successful young adult development: a conceptual and measurement framework. Appl Dev Sci. 2016;20:150–74. doi:10.1080/10888691.2015.1082429. [Google Scholar] [PubMed] [CrossRef]
13. Sklar M, Groessl EJ, O’Connell M, Davidson L, Aarons GA. Instruments for measuring mental health recovery: a systematic review. Clin Psychol Rev. 2013;33(8):1082–95. doi:10.1016/j.cpr.2013.08.002. [Google Scholar] [PubMed] [CrossRef]
14. van Nieuwenhuizen C, Wilrycx G, Moradi M, Brouwers E. Psychometric evaluation of the dutch version of the mental health recovery measure (MHRM). Int J Soc Psychiatry. 2014;60(2):162–8. doi:10.1177/0020764012472302. [Google Scholar] [PubMed] [CrossRef]
15. Jerrell JM, Cousins VC, Roberts KM. Psychometrics of the recovery process inventory. J Behav Health Serv Res. 2006;33:464–73. doi:10.1007/s11414-006-9031-5. [Google Scholar] [PubMed] [CrossRef]
16. Pernice-Duca F. Family network support and mental health recovery. J Marital Fam Ther. 2010;36:13–27. doi:10.1111/j.1752-0606.2009.00182.x. [Google Scholar] [PubMed] [CrossRef]
17. Green G, Hayes C, Dickinson D, Whittaker A, Gilheany B. The role and impact of social relationships upon well-being reported by mental health service users: a qualitative study. J Ment Health. 2009;11(5):565–79. doi:10.1080/09638230020023912. [Google Scholar] [CrossRef]
18. Aldersey HM, Whitley R. Family influence in recovery from severe mental illness. Commun Ment Health J. 2015;51:467–76. doi:10.1007/s10597-014-9783-y. [Google Scholar] [PubMed] [CrossRef]
19. Cleary M, Lees D, Sayers J. Friendship and mental health. Issues Ment Health Nurs. 2018;39(3):279–81. doi:10.1080/01612840.2018.1431444. [Google Scholar] [PubMed] [CrossRef]
20. Doroud N, Fossey E, Fortune T. Recovery as an occupational journey: a scoping review exploring the links between occupational engagement and recovery for people with enduring mental health issues. Aust Occup Ther J. 2015;62(6):378–92. doi:10.1111/1440-1630.12238. [Google Scholar] [PubMed] [CrossRef]
21. Dunn EC, Wewiorski NJ, Rogers ES. The meaning and importance of employment to people in recovery from serious mental illness: results of a qualitative study. Psychiatr Rehabil J. 2008;32(1):59–62. doi:10.2975/32.1.2008.59.62. [Google Scholar] [PubMed] [CrossRef]
22. Mee J, Sumsion T. Mental health clients confirm the motivating power of occupation. Br J Occup Ther. 2001;64(3):121–8. doi:10.1177/030802260106400303. [Google Scholar] [CrossRef]
23. O’Connor M, Cloney D, Kvalsvig A, Goldfeld S. Positive mental health and academic achievement in elementary school: new evidence from a matching analysis. Educ Res. 2019;48(4):205–16. doi:10.3102/0013189X19848724. [Google Scholar] [PubMed] [CrossRef]
24. Allison DB, Newcomer JW, Dunn AL, Blumenthal JA, Fabricatore AN, Daumit GL, et al. Obesity among those with mental disorders: a national institute of mental health meeting report. Am J Prev Med. 2009;36(4):341–50. doi:10.1016/j.amepre.2008.11.020. [Google Scholar] [PubMed] [CrossRef]
25. Brown LC, Majumdar SR, Newman SC, Johnson JA. History of depression increases risk of type 2 diabetes in younger adults. Diabetes Care. 2005;28(5):1063–7. doi:10.2337/diacare.28.5.1063. [Google Scholar] [PubMed] [CrossRef]
26. Cassidy F, Ahearn E, Caroll J. Elevated frequency of diabetes mellitus in hospitalized manic-depressive patients. Am J Psychiatry. 1999;156(9):1417–20. doi:10.1176/ajp.156.9.1417. [Google Scholar] [PubMed] [CrossRef]
27. de Hert M, Dekker J, Wood D, Kahl K, Holt R, Möller H. Cardiovascular disease and diabetes in people with severe mental illness: position statement from the European Psychiatric Association (EPAsupported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiat. 2009;24(6):412–24. doi:10.1016/j.eurpsy.2009.01.005. [Google Scholar] [PubMed] [CrossRef]
28. Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: meta-analysis and systematic review. Scand J Med Sci Sports. 2013;24(2):259–72. doi:10.1111/sms.12050. [Google Scholar] [PubMed] [CrossRef]
29. Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiat. 2014;75(9):964–74. doi:10.4088/JCP.13r08765. [Google Scholar] [PubMed] [CrossRef]
30. Chang S, Sambasivam R, Seow E, Subramaniam M, Assudani HA, Tan GCY, et al. Positive mental health in psychotherapy: a qualitative study from psychotherapists’ perspectives. BMC Psychol. 2022;10:58. doi:10.1186/s40359-022-00816-6. [Google Scholar] [PubMed] [CrossRef]
31. Browne J, Penn DL, Meyer-Kalos PS, Mueser KT, Estroff SE, Brunette MF, et al. Psychological well-being and mental health recovery in the NIMH RAISE early treatment program. Schizophr Res. 2017;185:167–72. doi:10.1016/j.schres.2016.11.032. [Google Scholar] [PubMed] [CrossRef]
32. Grant F, Guille C, Sen S. Well-being and the risk of depression under stress. PLoS One. 2013;8(7):e67395. doi:10.1371/journal.pone.0067395. [Google Scholar] [PubMed] [CrossRef]
33. Iasiello M, van Agteren J, Keyes CLM, Cochrane EM. Positive mental health as a predictor of recovery from mental illness. J Affect Disord. 2019;251:227–30. doi:10.1016/j.jad.2019.03.065. [Google Scholar] [PubMed] [CrossRef]
34. Keyes CLM, Dhingra SS, Simoes EJ. Change in level of positive mental health as a predictor of future risk of mental illness. Am J Public Health. 2010;12:2366–71. doi:10.2105/AJPH.2010.192245. [Google Scholar] [PubMed] [CrossRef]
35. Clarke S, Oades LG, Crowe TP. Recovery in mental health: a movement towards well-being and meaning in contrast to an avoidance of symptoms. Psychiatr Rehabil J. 2012;35(4):297–304. doi:10.2975/35.4.2012.297.304. [Google Scholar] [PubMed] [CrossRef]
36. Goetzel RZ, Ozminkowski RJ, Sederer LI, Mark TL. The business case for quality mental health services: why employers should care about the mental health and well-being of their employees. J Occup Environ Med. 2002;44(4):320–330. doi:10.1097/00043764-200204000-00012. [Google Scholar] [PubMed] [CrossRef]
37. McClintock C, Anderson M, Svob C, Wickramaratne P, Neugebauer R, Miller L, et al. Multidimensional understanding of religiosity/spirituality: relationship to major depression and familial risk. Psychol Med. 2019;49(14):2379–88. doi:10.1017/S0033291718003276. [Google Scholar] [PubMed] [CrossRef]
38. Neugebauer R, Wickramaratne P, Svob C, McClintock CH, Gameroff MJ, Miller L, et al. Contribution of religion/spirituality and major depressive disorder to altruism. J Affect Disord. 2020;262:16–22. doi:10.1016/j.jad.2019.10.031. [Google Scholar] [PubMed] [CrossRef]
39. Koenig HG. Research on religion, spirituality, and mental health: a review. Can J Psychiatry. 2009;54(5):283–91. doi:10.1177/070674370905400502. [Google Scholar] [PubMed] [CrossRef]
40. Greenblatt M, Becerra RM, Serafetinides EA. Social networks and mental health: an overview. Am J Psychiat. 1982;139(8):977–84. doi:10.1176/ajp.139.8.977. [Google Scholar] [PubMed] [CrossRef]
41. Matud MP, Díaz A, Bethencourt JM, Ibáñez I. Stress and psychological distress in emerging adulthood: a gender analysis. J Clin Med. 2020;9:2859. doi:10.3390/jcm9092859. [Google Scholar] [PubMed] [CrossRef]
42. Corrigan PW, Phelan SM. Social support and recovery in people with serious mental illnesses. Commun Ment Health J. 2004;40:513–23. doi:10.1007/s10597-004-6125-5. [Google Scholar] [PubMed] [CrossRef]
43. Hendryx M, Green CA, Perrin NA. Social support, activities, and recovery from serious mental illness: sTARS study findings. J Behav Health Serv Res. 2008;36:320–9. doi:10.1007/s11414-008-9151-1. [Google Scholar] [PubMed] [CrossRef]
44. Gates TG, Dentato MP. Volunteerism, mental health, and well-being in the lesbian, gay and bisexual community. Soc Work Ment Health. 2020;18(6):670–83. doi:10.1080/15332985.2020.1837333. [Google Scholar] [CrossRef]
45. Pérez-Corrales J, Pérez-de-Heredia-Torres M, Martínez-Piedrola R, Sánchez-Camarero C, Parás-Bravo P, Palacios-Ceña D. Being normal’ and self-identity: the experience of volunteering in individuals with severe mental disorders—A qualitative study. BMJ Open. 2019;9:e025363. doi:10.1136/bmjopen-2018-025363. [Google Scholar] [PubMed] [CrossRef]
46. Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39(1):31–6. [Google Scholar]
47. Auerswald M, Moshagen M. How to determine the number of factors to retain in exploratory factor analysis: a comparison of extraction methods under realistic conditions. Psychol Methods. 2019;24(4):468–91. doi:10.1037/met0000200. [Google Scholar] [PubMed] [CrossRef]
48. Brown DR, Carney JS, Parrish MS, Klem JL. Assessing spirituality: the relationship between spirituality and mental health. J Spiritual Ment Health. 2013;15(2):107–22. doi:10.1080/19349637.2013.776442. [Google Scholar] [CrossRef]
49. Cruwys T, Stewart B, Buckley L, Gumley J, Scholz B. The recovery model in chronic mental health: a community-based investigation of social identity processes. Psychiatry Res. 2020;291:113241. doi:10.1016/j.psychres.2020.113241. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools