 Open Access
Open Access
ARTICLE
Sleep Quality and Emotional Adaptation among Freshmen in Elite Chinese Universities during Prolonged COVID-19 Lockdown: The Mediating Role of Anxiety Symptoms
School of Education, Tianjin University, Tianjin, 300350, China
* Corresponding Author: Xinqiao Liu. Email:
(This article belongs to the Special Issue: Coping with Life Stress During/After the COVID-19 Pandemic and Its Impact on Mental Health)
International Journal of Mental Health Promotion 2024, 26(2), 105-116. https://doi.org/10.32604/ijmhp.2023.042359
Received 27 May 2023; Accepted 24 November 2023; Issue published 08 March 2024
Abstract
Under the effects of COVID-19 and a number of ongoing lockdown tactics, anxiety symptoms and poor sleep quality have become common mental health issues among college freshmen and are intimately related to their emotional adaptation. To explore this connection, this study gathered data from a sample of 256 freshmen enrolled in an elite university in China in September 2022. The association between sleep quality, anxiety symptoms, and emotional adaptation was clarified using correlation analysis. Additionally, the mediating function of anxiety symptoms between sleep quality and emotional adaptation was investigated using a structural equation model. The results reveal that: (1) Chinese elite university freshmen who were subjected to prolonged lockdown had poor sleep quality and mild anxiety symptoms; (2) a significant positive correlation between poor sleep quality and anxiety symptoms was identified; (3) anxiety symptoms were found to have a significant negative impact on emotional adaptation; (4) poor sleep quality had a negative impact on emotional adaptation through anxiety symptoms. This research makes a valuable contribution by offering insights into the intricate relationship between sleep quality and emotional adaptation among freshmen in elite Chinese universities during prolonged lockdown conditions, and it is beneficial for schools and educators to further improve school schedules and psychological health initiatives.Keywords
The global COVID-19 epidemic and its sequence of societal lockdown measures have had profoundly devastating effects on people’s daily lives and mental health [1–4]. It is imperative to acknowledge that even during the latter phases of the COVID-19 pandemic, strict control measures continue to be implemented by many universities in China. Under prolonged lockdown conditions, various issues, such as the complexity of online learning, peer infections, and restricted freedom, have further harmed the mental health of university students [5]. This is particularly concerning for college freshmen who are already facing the difficulties of transitioning from high school to university and undergoing significant identity transformations. And how well-adjusted they are during this time can affect their academic performance, physical and mental health, self-efficacy and social interactions [6,7]. Among them, anxiety symptoms are becoming increasingly common among college freshmen. Notably, there was a significant rise in anxiety among American college students between 2007 and 2018 [8]. This issue is not limited to one region, as around the world, nearly one-third of first-year college students experience at least one diagnosable mental health disorder, with generalized anxiety disorder being the most widespread [9]. High expectations and standards at elite colleges put pressure on students externally [10], which results in anxiety, depression, and other mental health issues [11]. Therefore, it is crucial to carry out a comprehensive examination of the relationship between sleep, anxiety issues, and the adaptation of elite university freshmen to college life during ongoing lockdown conditions.
Previous research has shown that emotions are multidimensional and consist of experiential, behavioral, and physiological components [12]. Emotion can affect an individual’s learning, career adaptability and memory abilities [13,14]. The ability to regulate emotions serves as a foundation for addressing a wide range of psychological health issues and psychological outcomes among young individuals [15]. It is essential to empirically examine key factors related to personal emotions in college freshmen. Many studies have focused on investigating the relationship between sleep and academic performance, cognitive achievement emotions, and mental health among adolescents and college students [16–20] Among them, sleep quality appears to be closely associated with emotions [21]. Numerous studies have substantiated the fact that a considerable portion of college students suffer from substandard sleep quality. A study conducted across multiple schools in the United States reported that 62% of students met the criteria for poor sleep quality [22]. Another survey conducted among American college students revealed that 64% of students experienced sleep problems [23]. In Norway, a study revealed that a significant proportion of university students, approximately 30.5% experienced insomnia [24]. Sleep issues among college students have become more prominent during the pandemic. A survey of students from Wuhan, China, conducted after the COVID-19 outbreak found that 32.73% of students experienced insomnia [25]. Another large-scale survey conducted during the post-COVID-19 pandemic period in China revealed that 16.9% of college students suffered from sleep problems [26]. Therefore, clarifying the correlation between sleep quality and emotional adaptation will help improve the mental health of first-year students and provide references for targeted psychological interventions. In this study, emotional adaptation refers to the degree of psychological or physical distress symptoms experienced by students.
Furthermore, analyzing the influence mechanism of sleep on emotional adaptation is significant since it may determine how sleep affects psychological or physical distress symptoms during the college adaptation phase. College students’ anxiety is linked to their sleep and emotional adaptation [27–29], and it may operate as a mediating element to explain how they are related. Anxiety levels increase during the transition to college for first-year freshmen [30,31]. Sleep disorders among college freshmen are frequently linked to anxiety issues during this transition [31]. According to the data obtained from the Beijing College Students Panel Survey, it was found that students enrolled in college experienced a moderate level of anxiety throughout the initial three years of their academic journey [32], and anxiety issues among Chinese college students gradually decreased throughout their four years of study. This suggests that freshmen generally experience the highest levels of anxiety [33].
With the emergence of the pandemic, anxiety symptoms among college students have worsened. According to a comprehensive study conducted in the United States, specifically at Texas A&M University, concerning the mental well-being of a substantial sample size of 2,031 students, it was found that a notable percentage (38.38%) experienced varying levels of anxiety ranging from moderate to severe amidst the ongoing pandemic period [34]. Furthermore, a meta-analysis examining anxiety symptom prevalence among college students globally discovered a prevalence rate of 39.0% [35]. Nevertheless, research on the potential mediating effects of anxiety symptoms on the relationship between sleep quality and emotional adaptation is limited. This shortage is particularly evident in regard to empirical analysis specifically focused on Chinese college freshmen. This study aims to empirically explore the relationship and mechanisms between sleep quality and emotional adaptation among elite Chinese university freshmen under continuous lockdown conditions. The findings will help clarify the complex relationship between sleep quality, anxiety symptoms, and emotional adaptation, providing insights for universities to improve students’ sleep quality and enhance their mental health, thus facilitating a smooth college transition for freshmen.
Relationship between sleep quality and emotional adaptation
Currently, there have been limited studies that have explored the connection between sleep quality and positive emotions, and most of the studies conducted thus far have primarily focused on the interplay between sleep quality and negative emotions. However, the role of sleep in promoting positive emotions is worth investigating. Ensuring an adequate amount of sleep can facilitate positive emotions, and improving sleep quality can reduce emotional disorders [36]. Sleep deprivation inhibits positive responses to pleasant events [37]. People who suffer from sleep deprivation usually report much lower levels of positive emotions than those who do not [38]. Adolescents who go to bed earlier, sleep for longer periods of time, and spend more time in bed had significantly fewer cases of insomnia and depression symptoms [39].
Sleep deprivation can impair emotional regulation abilities, leading to a worsening of emotional states [40,41]. It results in an increase in negative emotions [42] and a decrease in positive emotions [43,44]. A study involving 3,374 adults discovered a significant correlation between sleep duration and emotional instability, with shorter sleep duration associated with greater emotional instability [45]. Several experimental studies have demonstrated a noteworthy surge in negative emotions including but not limited to anxiety, depression, anger, and tension, subsequent to different levels of sleep deprivation [40,43,46]. A study investigating Chinese engineering students during the epidemic showed that sleep disorders can affect students’ emotional control and regulation functions, thereby increasing the risk of depression [47]. Sleep deprivation has a worse impact on emotional regulation in adolescents than in adults [48]. A study conducted on 907 adolescents aged 13–16 in Cleveland showed that subjective sleepiness can lead to general negative emotions and a decrease in emotional regulation abilities, resulting in depressive and anxious emotions and physical symptoms [49].
Furthermore, the interaction between sleep and emotions primarily occurs within emotional brain networks [21]. The prefrontal cortex (PFC), a crucial area responsible for regulating emotions, may be compromised by sleep deprivation and decreased sleep quality, leading to reduced control over negative emotions [50]. Sleep deprivation impairs memory encoding in the brain, selectively altering memory processes. Individuals who undergo sleep deprivation tend to remember negative memories while paying little attention to or neglecting positive memories [21,41].
In conclusion, the role of sleep in protecting against positive emotions, resisting negative emotions, and ensuring emotional adaptation in freshmen is worth investigating.
Relationship between sleep quality and anxiety symptoms
Research has demonstrated that anxiety is linked to various functional impairments, particularly sleep-related issues [51]. At least three sleep-related issues are present in the majority of young people with anxiety disorders [52]. Compared with those without anxiety symptoms, children and adolescents who experience anxiety often exhibit more pronounced and noticeable sleep problems [53]. Jennifer et al. investigated sleep patterns and problems in children with anxiety disorders and nonclinical children. They discovered that, in comparison to their peers who did not have anxiety symptoms, children with clinically significant anxiety disorders typically had later bedtimes and much less sleep during the week [51]. A comprehensive investigation conducted with college students revealed a noteworthy association between self-reported difficulties with sleep and symptoms of anxiety [28]. In an investigation aimed at comparing adolescents diagnosed with Generalized Anxiety Disorder (GAD) with a control group of healthy individuals, it was revealed that those suffering from GAD frequently encounter sleep-related issues. These issues include experiencing longer periods of time to fall asleep (known as sleep latency) and extended sleep duration. Furthermore, it was identified that a decrease in nighttime sleep duration is directly correlated with heightened levels of anxiety in the morning [54].
Insomnia and sleep deprivation are common symptoms, consequences, or complications of anxiety disorders, including GAD, PTSD, panic disorder, and obsessive-compulsive disorder [55]. The occurrence of insomnia in people diagnosed with anxiety disorders varies significantly, with rates typically ranging from 70% to 90% [56]. Sleep, being fundamentally an inhibitory behavior, is disrupted in individuals with anxiety disorders who experience increased fear and vigilance, heightened cognitive activity, and elevated levels of worry before bedtime. These uncontrollable presleep worries prevent people from initiating sleep, which makes it harder for them to fall asleep [50,57]. Sleep problems often precede the onset of anxiety symptoms, and sleep deprivation can affect anxiety [55,58,59]. Experimental studies have shown that both chronic and acute sleep deprivation can lead to increased anxiety levels the following day in adults and children [60]. Numerous experimental studies have used sleep deprivation as a controlled variable to examine how sleep loss affects anxiety. One study found that adults who experienced 24 h of sleep deprivation exhibited higher levels of anxiety than those who had normal sleep [61]. Another study involving 12 healthy male participants aged between 18 and 26 revealed that 36 h of extended wakefulness led to an increase in self-reported anxiety levels [62].
Additionally, college freshmen with evening chronotype (night owl) habits tend to have higher levels of anxiety [27]. A study involving 1,406 adolescents demonstrated that individuals who experience elevated levels of anxiety are significantly more inclined to possess an evening chronotype, possibly due to a mismatch between the sleep-wake schedule of evening chronotype adolescents and the traditional school timetable. To meet school requirements, they must wake up early to study. Moreover, individuals who have evening chronotype habits frequently encounter noticeable disparities in the amount of sleep they get between school days and non-school days. This often leads to the accumulation of a significant sleep debt specifically on school days [63]. Comparative analysis of sleep status between 742 individuals with evening chronotype and 1,005 individuals with morning chronotype revealed that evening chronotype individuals frequently nap during school days and report daytime sleepiness [64] and were particularly prone to experiencing symptoms of depression and anxiety with daytime sleepiness [65].
Relationship between anxiety symptoms and emotional adaptation
Few studies have discussed the connection between sleep and emotional adaptation as well as its underlying mechanisms, despite previous literature supporting the correlation between sleep and emotions. It has been proposed that anxiety symptoms may act as a mediator in elucidating this relationship. Anxiety disorders signify an inability to choose adaptive responses or inhibit maladaptive reactions in specific situations [66]. According to the emotion dysregulation model, Generalized Anxiety Disorder (GAD) is distinguished by notable deficiencies in emotional experiences and adjustment. Specifically, individuals with GAD experience four aspects of emotional dysfunction. First, when comparing individuals with Generalized Anxiety Disorder (GAD) to those without this condition, it becomes evident that individuals with GAD tend to experience and react to emotions in a more heightened and intense manner. Second, people with GAD struggle to identify and articulate their emotional experiences, indicating insufficient understanding of emotions. Third, individuals with GAD tend to exhibit worse negative cognitive reactions to emotions, making it challenging to attend to and allow the natural unfolding of emotional experiences. Fourth, individuals who suffer from Generalized Anxiety Disorder (GAD) often actively engage in strategies to cope with or reduce the impact of their negative emotions when they arise [67–69]. Previous studies have supported the notion of emotional dysregulation in individuals with GAD [68,70]. Avoidance theory, another hypothesis of GAD, contends that anxiety is a persistent cognitive activity that enables people to process emotions at an abstract and conceptual level. Worry is a coping mechanism used by people with GAD to try to avoid negative intentions and physiological arousal associated with negative emotions [71,72]. Worry is reinforced and grows chronic because it prevents the emotional experience of unfavorable opposing conditions, in contrast to the suppression of negative emotions. According to this hypothesis, the sudden change from a normal condition to intensely negative moods is much more unpleasant than the constant feeling of stress and anxiety [73].
Previous studies have provided evidence suggesting that the relationship between anxiety symptoms and the severity of insomnia symptoms is influenced by emotional adjustment [74]. Moreover, research also supports the notion that emotional dysregulation acts as a mediator in the connection between generalized anxiety disorder and sleep issues [75]. However, there is a paucity of literature simultaneously investigating emotions, anxiety symptoms, and sleep quality. To the best of our knowledge, no research has been conducted to examine the role of anxiety symptoms in mediating the relationship between sleep quality and emotional adaptation. Therefore, this study holds great significance as it contributes to elucidating the complex mechanisms underlying sleep quality, anxiety symptoms, and emotional adaptation. Furthermore, it provides valuable insights for universities to improve students’ sleep quality and enhance their psychological well-being.
Given the substantial occurrence of anxiety symptoms among college students and adolescents, anxiety symptoms may play a crucial mediating role between sleep quality and emotional adaptation. Insufficient research has been conducted to explore the correlation between different sleep problems and emotional adaptation in college freshmen, particularly regarding the limited understanding of the mediating role of anxiety symptoms in the relationship between sleep quality and emotional adaptation. Furthermore, there is a lack of in-depth empirical research specifically focused on elite university freshmen in China. What are the characteristics of sleep quality among elite university freshmen during the ongoing lockdown? How do anxiety symptoms mediate the relationship between sleep quality and emotional adaptation? This study empirically examines the relationship between sleep quality and emotional adaptation among elite university freshmen in China during the ongoing lockdown. Additionally, the study explores the potential role of anxiety symptoms as a mediator in this relationship.
Drawing upon pertinent literature and established theories, we have meticulously constructed a comprehensive theoretical research framework, visually illustrated in Fig. 1. After conducting an extensive review of the literature, carefully considering our predetermined research objectives, and aligning them with the theoretical framework, we propose the subsequent research hypotheses.
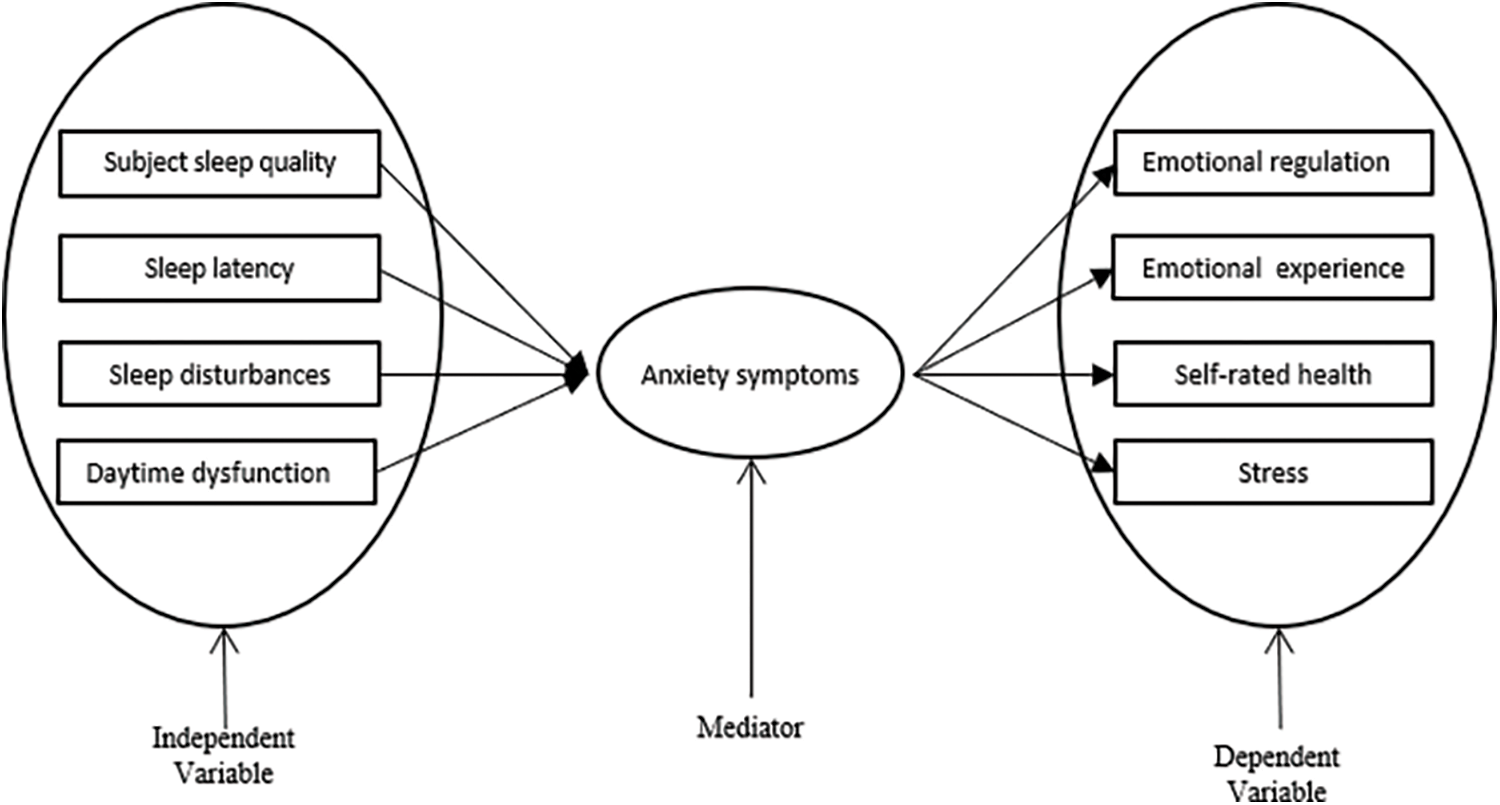
Figure 1: Theoretical framework.
Hypothesis 1: College freshmen generally experience poor sleep quality and anxiety issues.
Hypothesis 2.1: Poor sleep quality among college freshmen is significantly positively correlated with anxiety symptoms.
Hypothesis 2.2: Poor sleep quality among college freshmen is significantly negatively correlated with emotional adaptation.
Hypothesis 3: Poor sleep quality negatively influences college freshmen’s emotional adaptation when using anxiety symptoms as mediators.
We constructed a theoretical research framework (refer to Fig. 1) after considering the research hypotheses, pertinent literature, and theoretical foundations.
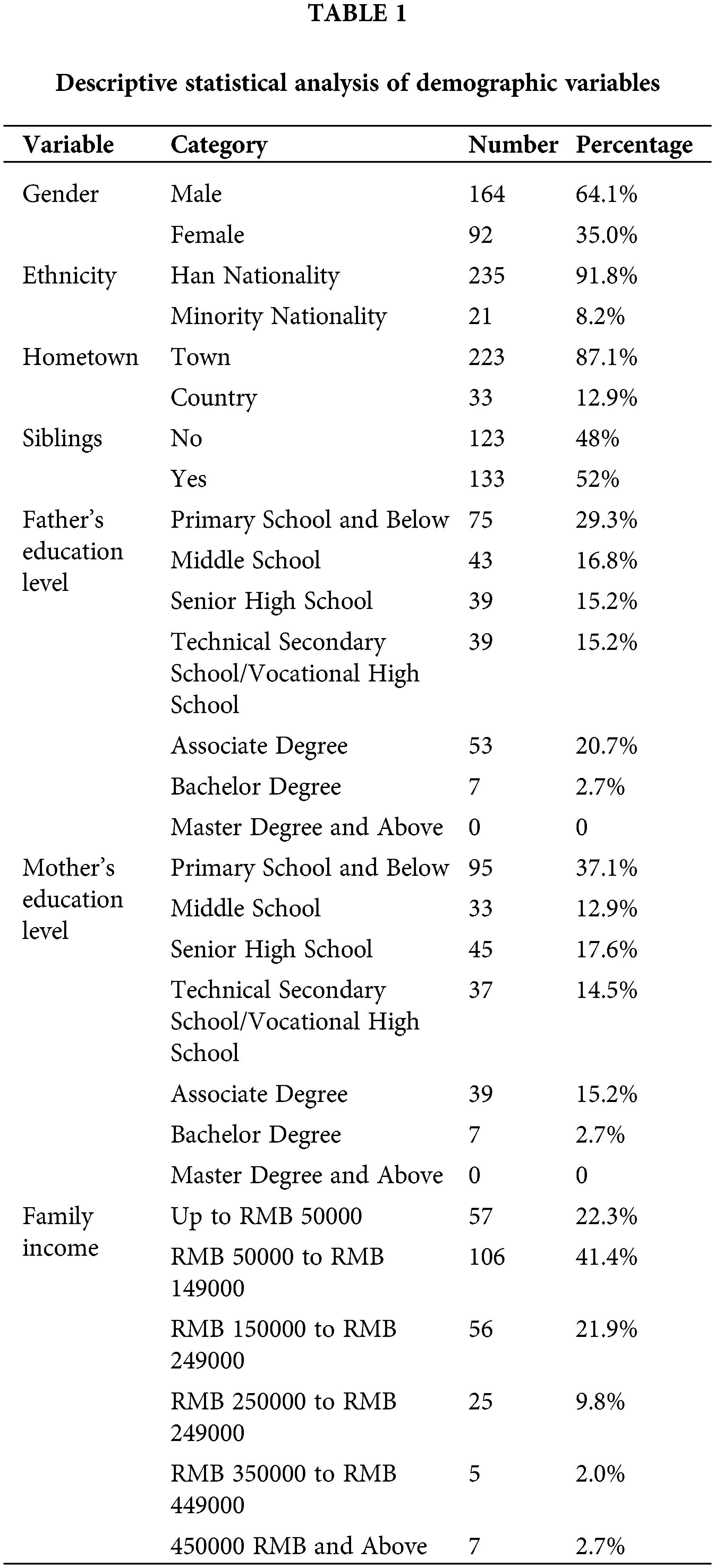
This study was conducted at T University, a prominent elite university in Northern China with 19,033 undergraduate students and 19,739 master’s and doctoral students. The sample we conducted was the university’s first-year university students who enrolled in September 2022, for a total of 4,741 students in the class of 2022. To obtain a representative sample of freshmen at this elite Chinese university, a simple random sampling method was employed. Data collection took place one month after the students’ enrollment. Data collection was conducted one month after the freshmen’s enrollment. Under the prolonged lockdown, to prevent factors such as policy adjustments and changes in students’ mentality from affecting the accuracy of the data, we carried out short-term data collection on the basis of ensuring sample representativeness. The questionnaire was comprehensive, including basic personal information of the university freshmen. The survey gathered relevant data on the sleep quality, anxiety symptoms, and emotional adaptation of Chinese elite university freshmen during prolonged lockdown. A total of 264 questionnaires were gathered, and after careful evaluation, 256 of them were deemed valid. This gives us an impressive questionnaire validity rate of 97.71%. According to the authoritative book by Grace, for structural equation models, there are specific requirements for sample size [76]. The sample size of the data we collected is 256, which fully meets the sample size requirement of the model. Table 1 displays the descriptive statistical analysis of the participants’ demographic data.
The sleep quality of first-year university students was assessed by employing the Pittsburgh Sleep Quality Index (PSQI), an extensively researched questionnaire designed by Buysse et al. The PSQI consists of four dimensions: subjective sleep quality, sleep latency, sleep disturbances, and daytime dysfunction. It is the most commonly used method to measure sleep quality and sleep disturbances over a month in clinical and research settings. In this study, a modified version of the PSQI with 12 items was utilized. Each item needed participants to rate their sleep experience on a four-point scale, ranging from 0 to 3. The scores were then aggregated to obtain a total score, with higher scores indicating poorer sleep quality. According to the scoring criteria of the PSQI, individuals who obtain a cumulative score surpassing 5 are categorized as “poor sleepers.” Those with a total score lower than 5 are classified as “good sleepers” [77]. Since only the four dimensions of the PSQI were used in this study, the cutoff values for good and poor sleepers for each of the 12 items were determined based on the original cutoff values and the proportion to the total score. A total score higher than 3 was regarded as “poor sleep quality”, while a total score lower than 3 was indicative of “good sleep quality.” The total score of the PSQI is frequently utilized in research on college students and has been significantly correlated with the Insomnia Severity Index (ISI) in this population [22]. The Cronbach’s alpha coefficient for the PSQI in this study was 0.843, thereby demonstrating the measurement’s acceptable reliability.
An assessment was conducted to evaluate the indications of anxiety among first-year college students using the Generalized Anxiety Disorder-7 (GAD-7) scale. The GAD-7 is a concise self-report survey that was created by Spitzer et al. The questionnaire is designed to align with the diagnostic criteria for anxiety disorders in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). The GAD-7 is widely recognized internationally and has been proven to be a reliable and valid measure for assessing anxiety symptoms in Chinese adolescents aged 10–17 and university students. Previous studies have shown that the GAD-7 has strong psychometric properties [78,79]. The Generalized Anxiety Disorder 7-item scale (GAD-7) comprises seven assessment items, each assigned a rating on a 4-point scale (ranging from 1 to 4). A higher score on the scale suggests the presence of more pronounced symptoms of anxiety. The total score on the GAD-7 ranges from 7 to 28, with scores of 10, 15, and 20 representing mild, moderate, and severe anxiety symptoms, respectively. In this study, the Cronbach’s alpha coefficient for the GAD-7 was 0.907, indicating excellent reliability of the anxiety symptom measurement.
Emotional adaptation was measured using the dimension of emotional adaptation from the Student Adaptation to College Questionnaire (SACQ), specifically the revised version developed by Baker and Siryk. The SACQ is a diagnostic tool designed for college students to assess maladaptation [80]. The emotional adaptation dimension of the SACQ consists of 15 items that primarily measure emotional indicators such as depression, anxiety, and emotional control, as well as physiological indicators such as fatigue, appetite, and physical health. Each item is assessed using a 5-point scale that covers a range from “1 = strongly disagree” to “5 = strongly agree.” Some items in the questionnaire are reverse-scored, and higher total scores on the scale indicate better adaptation. Within this study, a Cronbach’s alpha coefficient of 0.860 was obtained for the SACQ, which indicates a commendable level of reliability in measuring emotional adaptation.
First, descriptive statistics were analyzed and presented using SPSS 18.0 for the sleep quality variables (including subjective sleep quality, sleep latency, sleep disturbances, and daytime dysfunction), anxiety symptoms, and emotional adaptation variables in Chinese elite university freshmen. Subsequently, bivariate correlation analyses were conducted to examine the relationships between sleep quality, anxiety symptoms, and emotional adaptation variables. To further investigate the association between sleep quality and emotional adaptation, a mediation model was empirically examined using Mplus 7.4. We conducted an assessment to specifically investigate the mediating effect of anxiety symptoms on the relationship under consideration.
Descriptive statistics and correlation analysis
Table 2 presents descriptive statistics for the variables of sleep quality, anxiety symptoms, and emotional adaptation, including the mean, standard deviation, minimum value, maximum value, skewness, and kurtosis. The data reveal that the average score for emotional adaptation is 52.38, indicating a normal level of emotional adaptation among university freshmen. Additionally, the average score for anxiety symptoms is 10.85, suggesting the presence of mild anxiety issues among university freshmen. The average sleep quality score among Chinese university freshmen during prolonged lockdown was 3.63, indicating a prevalent problem of poor sleep quality.
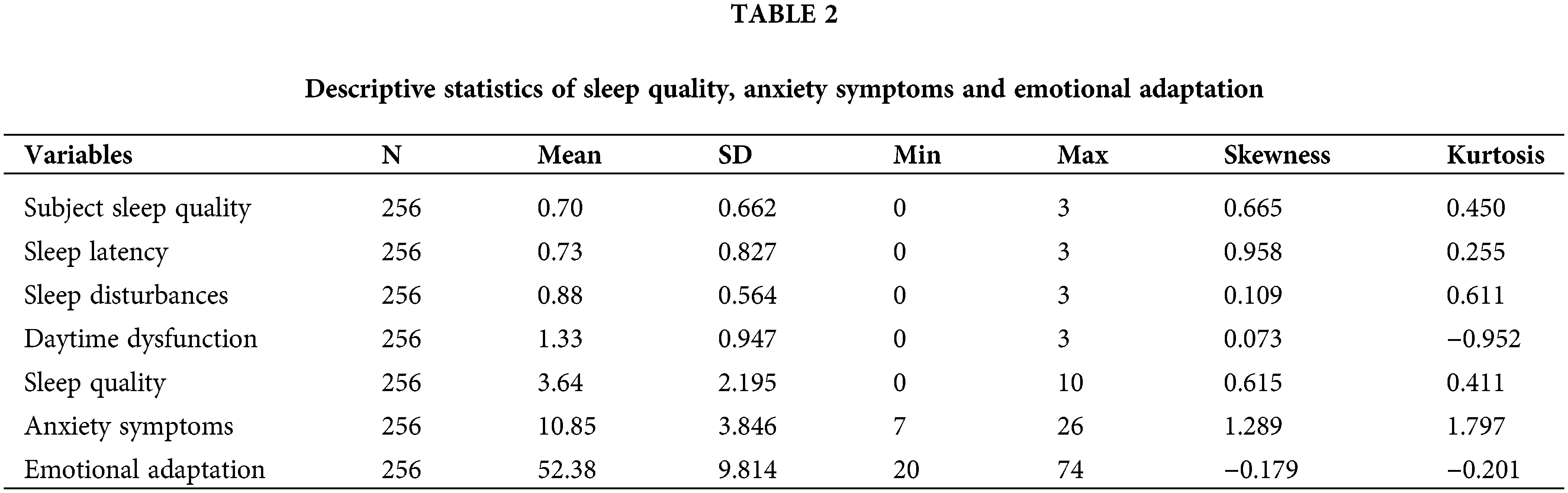
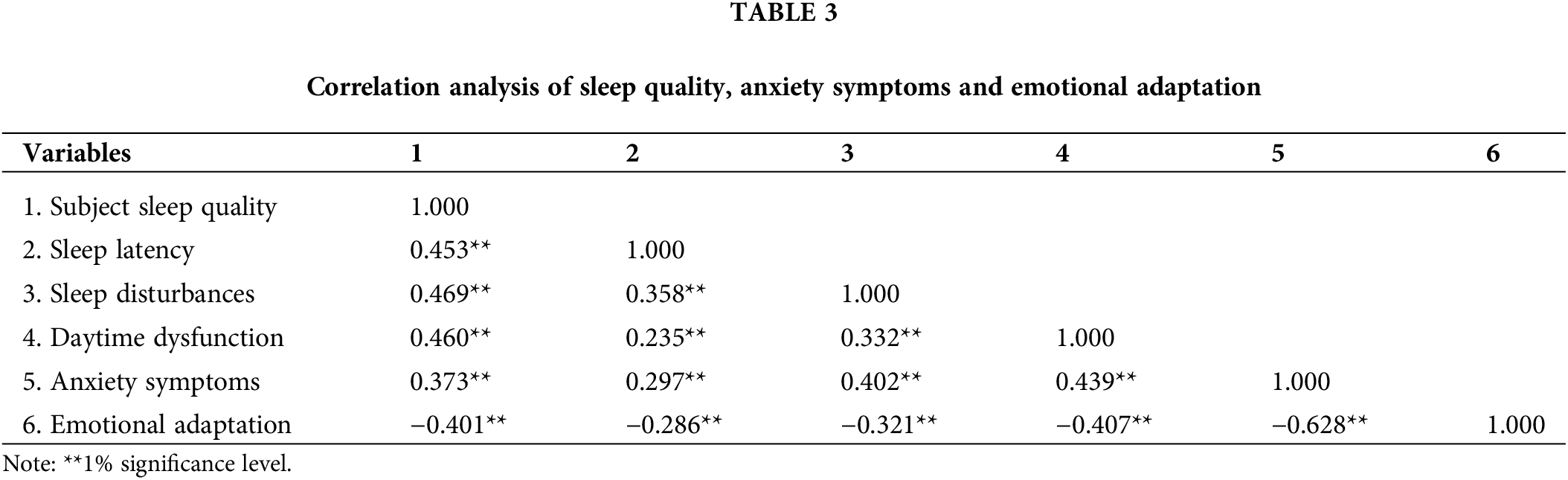
Table 3 presents the correlation coefficients between sleep quality, anxiety symptoms, and emotional adaptation. The results indicate a significant negative correlation between anxiety symptoms and emotional adaptation among Chinese elite university freshmen (p < 0.01) as well as between the scores of subjective sleep quality, sleep latency, sleep disturbances, daytime dysfunction, and emotional adaptation (p < 0.01). There was also a significant positive correlation between the scores of subjective sleep quality, sleep latency, sleep disturbances, daytime dysfunction, and anxiety symptoms (p < 0.01).
In our research, we implemented a mediation model alongside the bootstrap method to investigate the potential mediating influence of anxiety symptoms. We specifically focused on examining how anxiety symptoms contribute to the connection between sleep quality and emotional adaptation. The goodness-of-fit indices of our model indicate a favorable fit (RMSEA = 0.074, CFI = 0.931, SRMR = 0.049). The outcomes of the model are presented in Table 4.
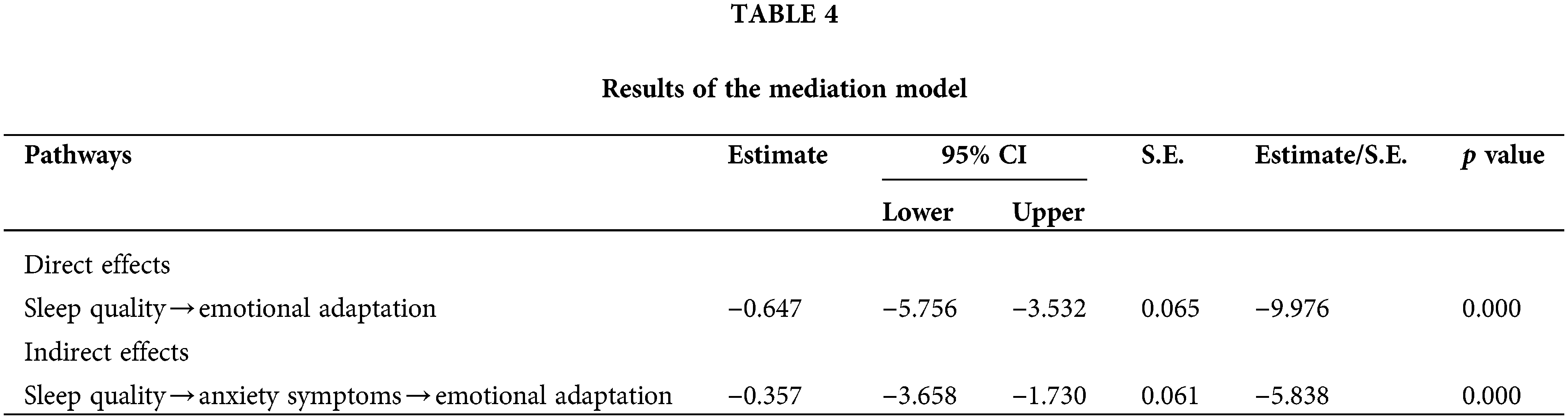
Notably, our findings reveal a significant direct effect of sleep quality on emotional adaptation, with a coefficient of −0.647 (p < 0.001) and a 95% confidence interval of [−5.756, −3.532]. This suggests that sleep quality has a direct impact on emotional adaptation. The indirect effect of anxiety symptoms between sleep quality and emotional adaptation was −0.357 (p < 0.001), with a confidence interval of [−3.658, −1.730], indicating a significant indirect effect.
The above results including Table 4 and Fig. 2 indicate that anxiety symptoms mediate the relationship between sleep quality and emotional adaptation among elite Chinese university freshmen. Specifically, when anxiety symptoms are mediators, poor sleep quality has a negative impact on emotional adaptation.
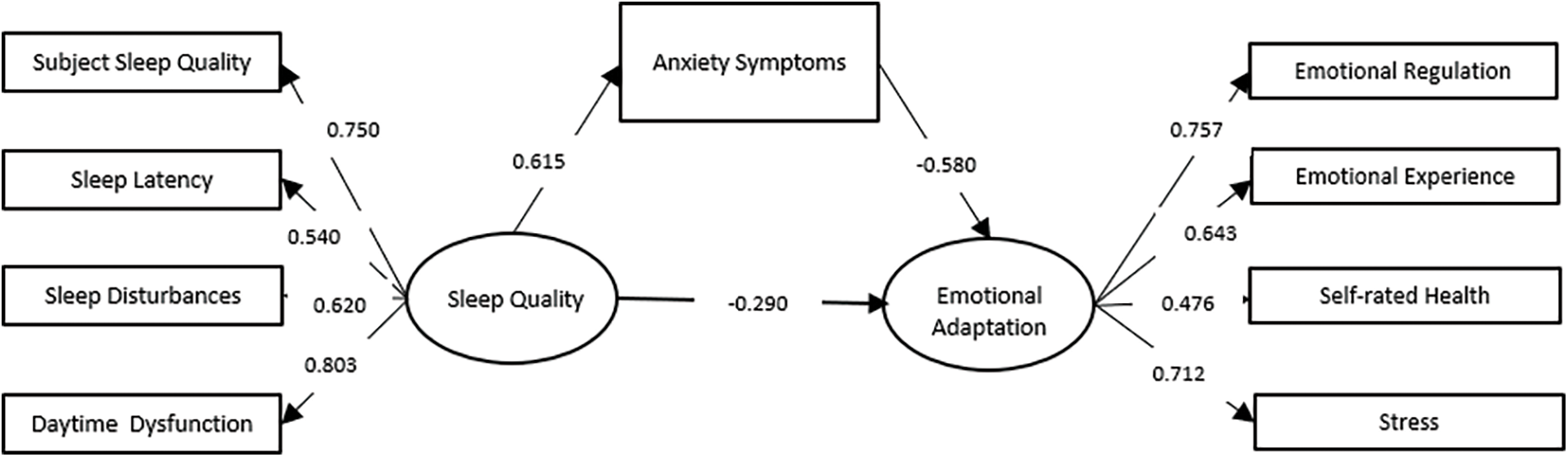
Figure 2: Mediation model of sleep quality, anxiety symptoms and emotional adaptation.
This study presents a comprehensive analysis of the relationship between sleep quality and emotional adaptation among freshmen in an elite Chinese university during the prolonged lockdown. The aim is to provide a deeper understanding of the ways in which sleep quality can affect emotional well-being, specifically focusing on the mediating effect of anxiety symptoms. The findings contribute valuable evidence to the field and aid in better understanding the interplay between these factors in the Chinese context.
Descriptive statistical analysis results revealed that the overall sleep quality of freshmen was poor during the prolonged lockdown. This aligns with previous research showing that college students commonly experience sleep problems, which may persist or even worsen [31], and freshmen are more likely to experience sleep disturbances than sophomores [81]. Particularly in the context of the COVID-19 pandemic, sleep problems among Chinese university students have become more prominent [25,26]. It is noted that sleep problems, especially daytime dysfunction, are particularly prominent among freshmen, which is probably related to the changes in teenagers’ circadian rhythms after puberty when they start to stay up late [82]. Research from multiple countries also shows that bedtime gets later as adolescents grow older [83]. In addition, external factors such as excessive use of electronic devices and academic stress contribute to college students staying up late. Students must get up early to study to satisfy the tough academic requirements of the university curriculum, which includes early morning classes. College students who have prolonged sleep debt owing to staying up late tend to experience daytime dysfunction, such as increased daytime tiredness [84]. Additionally, the occurrence of mild anxiety among first-year college students is consistent with previous research, which deserves significant attention. The prevalence of anxiety symptoms among children and adolescents during the COVID-19 lockdown was 11.5%, and anxiety symptoms increased with the duration of the lockdown [85]. During the COVID-19 pandemic, it was found that approximately one-fifth of university students in China experienced symptoms related to anxiety [86]. These findings highlight the fact that anxiety symptoms are prevalent among Chinese teenagers and demand the attention of educational authorities, teachers, and parents. To enhance the mental well-being of first-year students, it is recommended that education administration and schools implement measures such as leveraging artificial intelligence-based technologies in psychiatric research and practice. These technologies offer advantages including high accessibility, anonymity, and accurate identification, which can promote students’ mental well-being. Two specific AI-assisted screening methods, chatbots, and large-scale social media data analysis, can be utilized by schools to support students [87,88]. In addition, studies have shown that physical activity time has a significant negative correlation with depression symptoms [89]. Therefore, education administration and schools should create favorable conditions for physical activity, encourage extended physical activity time for adolescents, and closely monitor their emotional adaptation.
Correlation analysis revealed significant negative associations between subjective sleep quality, sleep latency, sleep disturbances, daytime dysfunction, and emotional adaptation. Since the Pittsburgh Sleep Quality Index indicates worse sleep conditions with higher scores, the results of the correlation analysis suggest that poorer sleep conditions are associated with poorer emotional adaptation among college freshmen. Research conducted in various countries has demonstrated that sleep disturbances can affect the functioning of brain areas responsible for regulating emotions. This can exacerbate negative emotions and decrease positive emotions [40,41,50]. Numerous experimental studies from other countries have shown that after experiencing acute sleep deprivation, negative emotions significantly increase [40,43,46]. This study supports previous research, indicating that, as in other countries, poor sleep quality among Chinese university freshmen impairs positive emotional adaptation. Moreover, the research revealed a significant negative relationship between anxiety symptoms and the process of emotional adaptation. This aligns with previous research, i.e., generalized anxiety disorder patients exhibit significant deficiencies in emotion regulation and have greater negative emotional reactions [67–69]. Freshmen in a transitional identity are prone to anxiety due to factors including, missing parents and close relatives, attempting to establish intimate relationships in a new setting, and worrying about university courses and future opportunities. Prolonged anxiety impairs their ability to regulate emotions [70], which results in poor emotional adaptation among freshmen. Therefore, further research should explore the relationship between anxiety symptoms and emotional adaptation among college freshmen.
In addition, this study confirmed the mediating role of anxiety symptoms between sleep quality and emotional adaptation among college freshmen. Prior studies have attempted to explore the connection between sleep quality and anxiety symptoms [28,51,90], anxiety symptoms and emotions [67,68,74], and the relationship between sleep quality and emotions [36,40,48]. However, there is scarce literature that investigates the relationship among all three factors. The study findings revealed that anxiety symptoms play a negative mediating role in the connection between sleep quality and emotional adaptation. This finding emphasizes the complexity of the relationship between sleep quality and emotional adaptation among college freshmen and provides evidence to some extent for nonclinical psychological health issues.
First, we obtained correlations between sleep quality, emotional adjustment, and anxiety symptoms based on cross-sectional data using only freshmen from an elite Chinese university, and caution is needed in generalizing our findings. Nevertheless, it is imperative to exercise utmost caution in various circumstances when generalizing our results to broader populations. We recommend that future studies to collect longitudinal data to enable a deeper analysis of the relationships between these variables should such information become available.
Second, due to the study design, the study cannot compare stress and anxiety levels before and after the pandemic. Regarding internal validity, our methods were limited by the constraints of their usage.
Furthermore, the data collected for sleep quality, emotional adaptation, and anxiety symptoms all relied on self-report questionnaires, which may introduce some degree of measurement bias.
Finally, further investigation is necessary to develop a more comprehensive understanding through theoretical research which sleep quality affects emotional adaptation through anxiety symptoms among college students. This would provide a clearer understanding of the relationship between these variables.
Implications of Educational Practice and Conclusions
Implications of educational practice
This paper demonstrates innovation and high academic value primarily in two aspects. First, research on the mental health, sleep, and adaptation of university students during prolonged lockdown periods is scarce. Given the difficulty of artificially creating an environment that forcibly locks down a large number of students, we took advantage of the policies implemented by the Chinese government during the COVID-19 period, which provided an opportunity to explore this research area and paved the way for future studies related to prolonged lockdown. Second, the transition in identity and adaptation to university life among incoming college freshmen is a topic of significant concern for university administrators. However, there is relatively limited research on the impact of sleep on freshmen’s adaptation. Therefore, it is necessary to investigate the effects of creating a conducive sleep environment and improving sleep quality on the development of incoming students.
This study also holds significant implications and practical significance for educational practices. First, the study’s findings indicate that the better the sleep quality is, the higher the level of emotional adaptation throughout the transition period of entering college. The impact of sleep quality on emotional adaptation should not be overlooked. Moving forward, further research could consider conducting randomized intervention experiments to explore the most scientifically and reasonably structured daily schedules that schools should adopt. This is an urgent matter that educational management departments, schools, and parents should understand.
Second, the results of our mediation model reveal a positive relationship between poor sleep quality and anxiety symptoms, as well as a negative relationship between anxiety symptoms and emotional adaptation. The occurrence of anxiety symptoms among college students may be a key mediator connecting sleep quality and emotional adaptation. This study compensates for the lack of attention to the process through which sleep quality affects emotional adaptation.
Third, to alleviate the poor emotional adaptation of college freshmen during their initial campus experience, educational management departments, schools, and parents must collaborate to prioritize the mental health of college freshmen and help students cultivate good sleep habits. At the same time, universities should proactively identify students at risk of poor emotional adaptation at the earliest possible stage and immediately implement measures to improve the sleep and emotional states of college freshmen, assisting them in smoothly navigating the adaptation period of their college stage.
First, during the prolonged lockdown, freshmen in elite Chinese universities commonly experience poor sleep quality and mild anxiety issues.
Second, there is a significant positive correlation between sleep quality (subjective sleep quality, sleep latency, sleep disturbances, and daytime dysfunction) and anxiety symptoms among university freshmen.
Third, there is a significant negative correlation between sleep quality (subjective sleep quality, sleep latency, sleep disturbances, and daytime dysfunction) and emotional adaptation among university freshmen.
Finally, poor sleep quality has a negative impact on the emotional adaptation of university freshmen when using anxiety symptoms as mediators.
Acknowledgement: We would like to thank the participants who filled out the questionnaire.
Funding Statement: This research was funded by the Tianjin Philosophy and Social Science Planning Project “Research on Value-Added Evaluation of Career Adaptability for Engineering Students Oriented towards Outstanding Engineers”, Grant Number TJJXQN22-001.
Author Contributions: X. L. designed the study; L. Z., X. Z. and X. L. wrote the manuscript and all authors contributed equally to this work and should be regarded as co-first authors. All authors have read and agreed to the published version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval: Informed consent was obtained from all subjects involved in the study. The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Tianjin University.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–12. [Google Scholar]
2. Alzueta E, Perrin P, Baker FC, Caffarra S, Ramos-Usuga D, Yuksel D, et al. How the COVID-19 pandemic has changed our lives: a study of psychological correlates across 59 countries. J Clin Psychol. 2021;77(3):556–70. [Google Scholar] [PubMed]
3. Javed B, Sarwer A, Soto EB, Mashwani ZUR. The coronavirus (COVID-19) pandemic’s impact on mental health. Int J Health Plann Manage. 2020;35(5):993–6. [Google Scholar] [PubMed]
4. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–20. [Google Scholar] [PubMed]
5. Ren ZY, Xin YD, Ge JP, Zhao Z, Liu DX, Ho RCM, et al. Psychological impact of COVID-19 on college students after school reopening: a cross-sectional study based on machine learning. Front Psychol. 2021;12:641806. [Google Scholar] [PubMed]
6. Valentine JC, Hirschy AS, Bremer CD, Novillo W, Castellano M, Banister A. Systematic reviews of research: postsecondary transitions. In: Identifying effective models and practices. Louisville, KY: National Research Center for Career and Technical Education; 2009. [Google Scholar]
7. Liu XQ, Ji XY, Zhang YF. Trajectories of college students’ general self-efficacy, the related predictors, and depression: a piecewise growth mixture modeling approach. Heliyon. 2023;9(5):e15750. [Google Scholar] [PubMed]
8. Duffy ME, Twenge JM, Joiner TE. Trends in mood and anxiety symptoms and suicide-related outcomes among US undergraduates, 2007–2018: evidence from two national surveys. J Adolesc Health. 2019;65(5):590–8. [Google Scholar] [PubMed]
9. Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–38. [Google Scholar] [PubMed]
10. Scholl A, Sassenberg K, Pfattheicher S. Pressured to be excellent? Social identification prevents negative affect from high university excellence norms. J Exp Soc Psychol. 2019;84:103796. [Google Scholar]
11. Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. 2015;173:90–6. [Google Scholar] [PubMed]
12. Lang PJ. The varieties of emotional experience: a meditation on James-Lange theory. Psychol Rev. 1994;101(2):211–21. [Google Scholar] [PubMed]
13. Tyng CM, Amin HU, Saad MNM, Malik AS. The influences of emotion on learning and memory. Front Psychol. 2017;8:1454. [Google Scholar] [PubMed]
14. Liu X, Ji X, Zhang Y, Gao W. Professional identity and career adaptability among chinese engineering students: the mediating role of learning engagement. Behav Sci. 2023;13(6):480. [Google Scholar] [PubMed]
15. Mansell W, Harvey A, Watkins ER, Shafran R. Cognitive behavioral processes across psychological disorders: a review of the utility and validity of the transdiagnostic approach. Int J Cogn Ther. 2008;1(3):181–91. [Google Scholar]
16. Chen WL, Chen JH. Consequences of inadequate sleep during the college years: sleep deprivation, grade point average, and college graduation. Prev Med. 2019;124(3):23–8. [Google Scholar] [PubMed]
17. Palmer CA, Oosterhoff B, Bower JL, Kaplow JB, Alfano CA. Associations among adolescent sleep problems, emotion regulation, and affective disorders: findings from a nationally representative sample. J Psychiatr Res. 2018;96(15):1–8. [Google Scholar] [PubMed]
18. Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;60(1):101556. [Google Scholar] [PubMed]
19. Cao XJ, Liu XQ. Time use and cognitive achievement among adolescents in China: depression symptoms as mediators. J Intell. 2023;11(5):88. [Google Scholar] [PubMed]
20. Cao XJ. Sleep time and depression symptoms as predictors of cognitive development among adolescents: a cross-lagged study from China. Psychol Rep. 2023. doi:10.1177/00332941231175833. [Google Scholar] [PubMed] [CrossRef]
21. Kahn M, Sheppes G, Sadeh A. Sleep and emotions: bidirectional links and underlying mechanisms. Int J Psychophysiol. 2013;89(2):218–28. [Google Scholar] [PubMed]
22. Becker SP, Jarrett MA, Luebbe AM, Garner AA, Burns GL, Kofler MJ. Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health. 2018;4(2):174–81. [Google Scholar] [PubMed]
23. Becker SP, Dvorsky MR, Holdaway AS, Luebbe AM. Sleep problems and suicidal behaviors in college students. J Psychiatr Res. 2018;99:122–8. [Google Scholar] [PubMed]
24. Vedaa Ø, Erevik EK, Hysing M, Hayley AC, Sivertsen B. Insomnia, sleep duration and academic performance: a national survey of Norwegian college and university students. Sleep Med: X. 2019;1:100005. [Google Scholar] [PubMed]
25. Duan H, Gong M, Zhang Q, Huang X, Wan B. Research on sleep status, body mass index, anxiety and depression of college students during the post-pandemic era in Wuhan, China. J Affect Disord. 2022;301(3):189–92. [Google Scholar] [PubMed]
26. Zhang YF, Wang DF, Zhao JB, Chen XY, Chen HL, Ma ZJ, et al. Insomnia and other sleep-related problems during the remission period of the COVID-19 pandemic: a large-scale survey among college students in China. Psychiatry Res. 2021;304(4):114153. [Google Scholar] [PubMed]
27. Lin YH, Gau SSF. Association between morningness-eveningness and the severity of compulsive internet use: the moderating role of gender and parenting style. Sleep Med. 2013;14(12):1398–404. [Google Scholar] [PubMed]
28. Orsal O, Orsal O, Alparslan GB, Unsal A. Evaluation of the relation between quality of sleep and anxiety among university students. HealthMED. 2012;6(7):2244–55. [Google Scholar]
29. Rea EM, Santiago CD, Nicholson L, Egbert AH, Bohnert AM. Sleep, affect, and emotion reactivity in first-year college students: a daily diary study. Int J Behav Med. 2023;30(5):753–68. [Google Scholar] [PubMed]
30. Kroshus E, Hawrilenko M, Browning A. Stress, self-compassion, and well-being during the transition to college. Soc Sci Med. 2021;269(3):113514. [Google Scholar] [PubMed]
31. Doane LD, Gress-Smith JL, Breitenstein RS. Multi-method assessments of sleep over the transition to college and the associations with depression and anxiety symptoms. J Youth Adolesc. 2015;44(2):389–404. [Google Scholar] [PubMed]
32. Gao WJ, Ping SQ, Liu XQ. Gender differences in depression, anxiety, and stress among college students: a longitudinal study from China. J Affect Disord. 2020;263(2):292–300. [Google Scholar] [PubMed]
33. Liu XQ, Cao XJ, Gao WJ. Does low self-esteem predict anxiety among Chinese college students? Psychol Res Behav Manag. 2022;15:1481–7. [Google Scholar] [PubMed]
34. Wang XM, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22(9):e22817. [Google Scholar] [PubMed]
35. Li WZ, Zhao ZY, Chen DJ, Peng Y, Lu ZX. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta-analysis. J Child Psychol Psyc. 2022;63(11):1222–30. [Google Scholar]
36. Shen L, van Schie J, Ditchburn G, Brook L, Bei B. Positive and negative emotions: differential associations with sleep duration and quality in adolescents. J Youth Adolesc. 2018;47(12):2584–95. [Google Scholar] [PubMed]
37. Zohar D, Tzischinsky O, Epstein R, Lavie P. The effects of sleep loss on medical residents’ emotional reactions to work events: a cognitive-energy model. Sleep. 2005;28(1):47–54. [Google Scholar] [PubMed]
38. Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10(6):831–41. [Google Scholar] [PubMed]
39. Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension and sleep hygiene advice on sleep and depressive symptoms in adolescents: a randomized controlled trial. J Child Psychol Psychiatry. 2014;55(3):273–83. [Google Scholar] [PubMed]
40. Kahn-Greene ET, Killgore DB, Kamimori GH, Balkin TJ, Killgore WDS. The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Med. 2007;8(3):215–21. [Google Scholar] [PubMed]
41. Walker MP, van der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychol Bull. 2009;135(5):731–48. [Google Scholar] [PubMed]
42. Drake CL, Roehrs TA, Burduvali E, Bonahoom A, Rosekind M, Roth T. Effects of rapid versus slow accumulation of eight hours of sleep loss. Psychophysiol. 2001;38(6):979–87. [Google Scholar]
43. Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psychiatry. 2014;55(2):180–90. [Google Scholar] [PubMed]
44. Reddy R, Palmer CA, Jackson C, Farris SG, Alfano CA. Impact of sleep restriction versus idealized sleep on emotional experience, reactivity and regulation in healthy adolescents. J Sleep Res. 2017;26(4):516–25. [Google Scholar] [PubMed]
45. Bowen R, Balbuena L, Baetz M, Schwartz L. Maintaining sleep and physical activity alleviate mood instability. Prev Med. 2013;57(5):461–5. [Google Scholar] [PubMed]
46. Conklin AI, Yao CA, Richardson CG. Chronic sleep deprivation and gender-specific risk of depression in adolescents: a prospective population-based study. BMC Public Health. 2018;18(1):724. [Google Scholar] [PubMed]
47. Liu XQ, Guo YX, Zhang WJ, Gao WJ. Influencing factors, prediction and prevention of depression in college students: a literature review. World J Psychiatr. 2022;12(7):860–73. [Google Scholar] [PubMed]
48. Beebe DW, Fallone G, Godiwala N, Flanigan M, Martin D, Schaffner L, et al. Feasibility and behavioral effects of an at-home multi-night sleep restriction protocol for adolescents. J Child Psychol Psychiatry. 2008;49(9):915–23. [Google Scholar] [PubMed]
49. Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Ancoli-Israel S, et al. Relationships among sleepiness, sleep time, and psychological functioning in adolescents. J Pediatr Psychol. 2009;34(10):1175–83. [Google Scholar] [PubMed]
50. Dahl RE, Lewin DS. Pathways to adolescent health: sleep regulation and behavior. J Adolesc Health. 2002;31(6):175–84. [Google Scholar] [PubMed]
51. Hudson JL, Gradisar M, Gamble A, Schniering CA, Rebelo I. The sleep patterns and problems of clinically anxious children. Behav Res Ther. 2009;47(4):339–44. [Google Scholar] [PubMed]
52. Alfano CA, Ginsburg GS, Kingery JN. Sleep-related problems among children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(2):224–32. [Google Scholar] [PubMed]
53. Forbes EE, Bertocci MA, Gregory AM, Ryan ND, Axelson DA, Birmaher B, et al. Objective sleep in pediatric anxiety disorders and major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2008;47(2):148–55. [Google Scholar] [PubMed]
54. Mullin BC, Pyle L, Haraden D, Riederer J, Brim N, Kaplan D, et al. A preliminary multimethod comparison of sleep among adolescents with and without generalized anxiety disorder. J Clin Child Adolesc Psychol. 2017;46(2):198–210. [Google Scholar] [PubMed]
55. Pires GN, Bezerra AG, Tufik S, Andersen ML. Effects of acute sleep deprivation on state anxiety levels: a systematic review and meta-analysis. Sleep Med. 2016;23:109–18. [Google Scholar]
56. Maher MJ, Rego SA, Asnis GM. Sleep disturbances in patients with post-traumatic stress disorder-epidemiology, impact and approaches to management. CNS Drugs. 2006;20(7):567–90. [Google Scholar] [PubMed]
57. Bélanger L, Morin CM, Gendron L, Blais FC. Pre-sleep cognitive activity and thought control strategies in insomnia. J Cog Psychother. 2005;19(1):19–28. [Google Scholar]
58. Gregory AM, Caspi A, Eley TC, Moffitt TE, O’Connor TG, Poulton R. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J Abnorm Child Psychol. 2005;33(2):157–63. [Google Scholar] [PubMed]
59. Liu XQ, Guo YX, Xu Y. Risk factors and digital interventions for anxiety disorders in college students: stakeholder perspectives. World J Clin Cases. 2023;11(7):1442–57. [Google Scholar] [PubMed]
60. Alfano CA, Pina AA, Zerr AA, Villalta IK. Pre-sleep arousal and sleep problems of anxiety-disordered youth. Child Psychiatry Hum Dev. 2010;41(2):156–67. [Google Scholar] [PubMed]
61. Babson KA, Trainor CD, Feldner MT, Blumenthal H. A test of the effects of acute sleep deprivation on general and specific self-reported anxiety and depressive symptoms: an experimental extension. J Behav Ther Exp Psychiatry. 2010;41(3):297–303. [Google Scholar] [PubMed]
62. Sagaspe P, Sanchez-Ortuno M, Charles A, Taillard J, Valtat C, Bioulac B, et al. Effects of sleep deprivation on color-word, emotional, and specific Stroop interference and on self-reported anxiety. Brain Cogn. 2006;60(1):76–87. [Google Scholar] [PubMed]
63. Diaz-Morales JF. Anxiety during adolescence: considering morningness-eveningness as a risk factor. Sleep Biol Rhythms. 2016;14(2):141–7. [Google Scholar]
64. Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11(3):191–9. [Google Scholar] [PubMed]
65. Ong JC, Huang JS, Kuo TF, Manber R. Characteristics of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med. 2007;3(3):289–94. [Google Scholar] [PubMed]
66. Thayer JF, Friedman BH, Borkovec TD, Johnsen BH, Molina S. Phasic heart period reactions to cued threat and nonthreat stimuli in generalized anxiety disorder. Psychophysiology. 2000;37(3):361–8. [Google Scholar] [PubMed]
67. Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behav Res Ther. 2005;43(10):1281–310. [Google Scholar] [PubMed]
68. Mennin DS, Holaway RM, Fresco DM, Moore MT, Heimberg RG. Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behav Ther. 2007;38(3):284–302. [Google Scholar] [PubMed]
69. Mennin DS, McLaughlin KA, Flanagan TJ. Emotion regulation deficits in generalized anxiety disorder, social anxiety disorder, and their co-occurrence. J Anxiety Disord. 2009;23(7):866–71. [Google Scholar] [PubMed]
70. Pawluk EJ, Koerner N, Kuo JR, Antony MM. An experience sampling investigatiosn of emotion and worry in people with generalized anxiety disorder. J Anxiety Disord. 2021;84(5):102478. [Google Scholar] [PubMed]
71. Borkovec TD. The nature, functions, and origins of worry. Oxford, England: John Wiley & Sons; 1994. [Google Scholar]
72. Borkovec TD, Alcaine OM, Behar E. Avoidance theory of worry and generalized anxiety disorder. In: Heimberg CLTRG, Mennin DS, editors. Generalized anxiety disorder: advances in research and practice. New York: Guilford Press; 2004. p. 77–108. [Google Scholar]
73. Newman MG, Llera SJ. A novel theory of experiential avoidance in generalized anxiety disorder: a review and synthesis of research supporting a contrast avoidance model of worry. Clin Psychol Rev. 2011;31(3):371–82. [Google Scholar] [PubMed]
74. Kirwan M, Pickett SM, Jarrett NL. Emotion regulation as a moderator between anxiety symptoms and insomnia symptom severity. Psychiatry Res. 2017;254(4):40–7. [Google Scholar] [PubMed]
75. Tsypes A, Aldao A, Mennin DS. Emotion dysregulation and sleep difficulties in generalized anxiety disorder. J Anxiety Disord. 2013;27(2):197–203. [Google Scholar] [PubMed]
76. Grace JB. Structural equation modeling and natural systems. New York: Cambridge University Press; 2006. p. 283. [Google Scholar]
77. Buysse DJ, Reynolds CFIII, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [Google Scholar] [PubMed]
78. Sun JA, Liang KX, Chi XL, Chen ST. Psychometric properties of the generalized anxiety disorder scale-7 item (GAD-7) in a large sample of Chinese adolescents. Healthcare. 2021;9(12):1709–12. [Google Scholar] [PubMed]
79. Zhang C, Wang TT, Zeng P, Zhao MH, Zhang GF, Zhai S, et al. Reliability, validity, and measurement invariance of the general anxiety disorder scale among Chinese medical university students. Front Psychiatry. 2021;12:648755. [Google Scholar] [PubMed]
80. Baker RW, Siryk B. Student adaptation to college questionnaire. In: Program of the Seventy-Fourth Annual Meeting1989Los Angeles, USA. [Google Scholar]
81. Suen LKP, Hon LKE, Tam WWS. Association between sleep behavior and sleep-related factors among university students in Hong Kong. Chronobiol Int. 2008;25(5):760–75. [Google Scholar] [PubMed]
82. Taylor DJ, Jenni OG, Acebo C, Carskadon MA. Sleep tendency during extended wakefulness: insights into adolescent sleep regulation and behavior. J Sleep Res. 2005;14(3):239–44. [Google Scholar] [PubMed]
83. Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8(6):602–12. [Google Scholar] [PubMed]
84. Bakotic M, Radosevic-Vidacek B, Koscec Bjelajac A. Morningness-eveningness and daytime functioning in university students: the mediating role of sleep characteristics. J Sleep Res. 2017;26(2):210–8. [Google Scholar] [PubMed]
85. Wang DF, Zhao JB, Zhai SY, Huang SQ, Yang Z, Pan Y, et al. Longitudinal trajectories of insomnia symptoms among college students during the COVID-19 lockdown in China. J Psychosom Res. 2022;157(21):110795. [Google Scholar] [PubMed]
86. Fu W, Yan S, Zong Q, Anderson-Luxford D, Song X, Lv Z, et al. Mental health of college students during the COVID-19 epidemic in China. J Affect Disord. 2021;280:7–10. [Google Scholar] [PubMed]
87. Cao XJ, Liu XQ. Artificial intelligence-assisted psychosis risk screening in adolescents: practices and challenges. World J. Psychiatr. 2022;12(10):1287–97. [Google Scholar] [PubMed]
88. Liu XQ, Guo YX, Zhang XR, Zhang LX, Zhang YF. Digital interventions empowering mental health reconstruction among students after the COVID-19 pandemic. World J Psychiatry. 2023;13(6):397–401. [Google Scholar] [PubMed]
89. Cao X, Zhang Q, Liu X. Cross-lagged relationship between physical activity time, openness and depression symptoms among adolescents: evidence from China. Int J Ment Health Promot. 2023;25(9):1009–18. [Google Scholar]
90. Chase RM, Pincus DB. Sleep-related problems in children and adolescents with anxiety disorders. Behav Sleep Med. 2011;9(4):224–36. [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools