 Open Access
Open Access
ARTICLE
Research on the Intervention Effect of Vibroacoustic Therapy in the Treatment of Patients with Depression
1 School of Education, Xuchang University, Xuchang, 461000, China
2 Department of Psychological Medicine, Henan Provincial People’s Hospital, Zhengzhou, 463599, China
3 Department of Clinical Psychology, Xuchang Jian’an Hospital, Xuchang, 461000, China
* Corresponding Author: Xiaodan Wang. Email:
International Journal of Mental Health Promotion 2024, 26(2), 149-160. https://doi.org/10.32604/ijmhp.2023.030755
Received 04 April 2023; Accepted 28 June 2023; Issue published 08 March 2024
Abstract
Research purpose: This study implemented somatosensory music therapy on patients with depressive disorders, and explored the effects of somatosensory music therapy on the degree of depression, positive and negative emotions, intuitive stress and autonomic nervous function of patients. Research method: We collected 66 patients diagnosed with depression from the Department of Psychological Medicine of Henan Provincial People’s Hospital, and divided them into a control group and an intervention group according to the random number table, with 33 people in each group. The control group received routine psychiatric treatment and nursing. On the basis of the control group, the intervention group received somatosensory music therapy 3 times a week, 30 min each time, for 4 consecutive weeks. The Hamilton Depression Scale, Positive and Negative Emotion Scale, Perceived Stress Scale, and Heart Rate Variability Index were collected and analyzed at baseline (T0), 2 weeks after treatment (T1) and 4 weeks after treatment (T2). Research results: After 4 weeks of treatment, the HAMD scores of the two groups decreased to varying degrees, and the difference between the groups was statistically significant (p < 0.05). After 4 weeks of treatment, the scores of positive emotions in both groups increased to varying degrees, and the scores of negative emotions increased to varying degrees. The scores decreased to varying degrees, and there were statistically significant differences between the positive and negative emotion groups (p < 0.05). After 4 weeks of treatment, the CPSS scores of the two groups decreased to varying degrees, and the difference between the two groups was statistically significant (p < 0.05). Analyzing the main effect of intervention factors alone, after 4 weeks of treatment, SDNN and RMSSD indexes all increased to varying degrees, and the degree of increase in the intervention group was greater than that in the control group, and the difference between the groups was statistically significant (p < 0.05). Research conclusion: assisting somatosensory music therapy for patients with depressive disorders can improve depressive symptoms, increase positive emotions, reduce negative emotions, and reduce perceived stress. These are beneficial to restore the balance of autonomic nervous system, and are effective for the treatment of depression.Keywords
Depressive disorder is one of the most common mental disorders. It is a general term for a group of diseases mainly characterized by low mood or mood, accompanied by varying degrees of cognitive and behavioral changes, and may also be accompanied by psychotic symptoms, such as hallucinations, delusions, etc. [1]. Depression is a disease manifestation of depressive disorder, which is characterized by high prevalence, high suicide rate, heavy disease burden, and high relapse rate. A report by the World Health Organization in 2017 pointed out that the global population of depression is estimated to reach 322 million people, accounting for 4.4% of the world’s population, of which the prevalence rate in China is 4.2% [2]. According to the World Health Organization’s Global Burden of Disease study, depressive disorders account for 10% of the disability caused by non-infectious diseases, and have become the second largest disease burden after cardiovascular diseases [3]. A study on the disease burden of depression in Beijing in 2010 showed that the time-point prevalence of depression in the resident population was 1.1%. Depression causes a large disease burden, especially in the middle-aged and elderly population [4]. Depressive disorder is a mental illness most closely related to suicide and self-harm, and is the main cause of disability [5]. Depressive disorders are easy to co-morbid with physical diseases, such as cardiovascular and cerebrovascular diseases and metabolic diseases, and it is also common for cancer patients to be accompanied by depressive disorders, which will increase the mortality rate of patients with depressive disorders.
The core symptoms of depressive disorders are depressed mood, loss of interest, and anhedonia, often accompanied by other cognitive, physical, and behavioral manifestations, such as inattention, unresponsiveness, sleep disturbance, decreased behavioral activity, and fatigue sense [6]. It is a common emotional disorder. Brain areas such as the amygdala play an important role in the process of emotional regulation, and these brain areas are called “emotional response areas” [7]. Studies have shown that the amygdala is over-activated in patients with depressive disorders when faced with negative emotional stimuli [8]. The mechanism may be that the negative cognitive processing bias reflects the enhanced bottom-up response to negative emotional stimuli, or that the negative cognitive processing bias reflects the insufficient top-down cognitive control [9]. The processing of negative emotions is closely related to the occurrence of depression, and improving the mood of patients with depression plays an important role in improving symptoms.
In clinical practice, drug therapy is the main treatment for depression, and antidepressant drugs are still the first-line treatment for depression. However, only one-third to one-half of patients with major depressive disorder achieve remission after completing an initial course of antidepressant medication. Even if the treatment is prescribed by the doctor, there is a 20% relapse rate, and the relapse rate is as high as 80% for those who do not adhere to the treatment, which makes it difficult for depressed patients to fully recover. In recent years, the field of psychiatry has become more comprehensive, and there are more and more treatment methods for mental disorders. In order to meet the health needs of patients, more and more clinicians are inclined to art therapy and other psychotherapy [10–12].
In receptive music therapy, Vibroacoustic therapy (VAT) has been gradually recognized by people. VAT, also known as vibro-acoustic therapy, is a low-frequency sound wave stimulation therapy. Through vibro-acoustic equipment, the low-frequency signal of 16–150 Hz in music is amplified and physically transduced, and acts on a part of the human body through skin receptors and nerve conduction. A music therapy technique [13]. The combination of music and somatosensory complements each other. Listening to beautiful music while experiencing the body can make the human body obtain high-quality inner joy and relaxation in a short period of time, and can effectively relieve depression, anxiety, insomnia, nervous disorders and other psychosomatic diseases. Studies have proved that VAT can treat depression, but most of them are applied in rehabilitation department or in combination with traditional Chinese medicine [14]. VAT alone as a treatment measure needs to be promoted in psychiatry.
Therefore, this study attempts to apply VAT to patients with depression in mental illness. To explore whether it can improve the mood of patients with depression, reduce their pressure perception, increase stress resistance, improve heart rate variability, obtain autonomic stability and balance, and provide a basis for clinical adjuvant treatment.
Perceived stress and the autonomic nervous system in depression
Depression arises from adaptive mechanisms in response to evolutionary pressures [15]. In exploring the pathogenesis of depression, many studies have found that patients with depressive disorders have dysfunction of the hypothalamic-pituitary-adrenal (HPA) axis. The more severe the depression, the more obvious the abnormality of the HPA axis [16]. One study found that abnormal cortisol levels in children with depressive disorders were associated with increased perceived stress in children and altered neurohormonal regulation due to activation of the HPA axis [17]. Repetitive stress, especially early in life, can lead to hyperresponsiveness of the HPA axis, which in turn increases the levels of cortisol and other glucocorticoids, which can also induce depressive symptoms [18]. Stress is a form of psychological stress, and living stressful experiences can increase the risk of depression. Most depressive episodes are preceded by stressful life events. The level of stress perception after negative life events varies among individuals, and different factors lead to different susceptibility to stress. Individuals have different perceptions of stress, that is, stress perception, and stress susceptibility increases the risk of depressive disorders [19,20]. Stress perception, also known as perceived stress (Perceived Stress, PS), refers to the individual’s psychological response to stimuli or threatening events in the environment after his own cognitive evaluation [21]. Studies have shown that stress perception is positively correlated with depression. The more obvious the perceived stress is, the stronger the depression may be. At the same time, depression also has a significant positive predictive effect on stress perception [22,23].
The autonomic nervous system (Autonomic Nervous System, ANS) is a part of the peripheral efferent nervous system, which can regulate the activities of visceral and vascular smooth muscles, myocardium and glands. It is composed of sympathetic and parasympathetic nerves, also known as the autonomic nervous system [24]. The two nerves antagonize each other and regulate together, and finally make the ANS reach a balanced state, and jointly maintain the stability of the body’s nerves. Autonomic nervous function is a physiological indicator that is often monitored in psychiatry, especially in patients with depression. Autonomic dysfunction is considered to be a potential psychopathological mechanism of depression. Several studies have shown that autonomic dysregulation in patients with depression is characterized by a decrease in overall heart rate variability (HRV), which is characterized by low and high frequencies [25]. HRV is a non-invasive method to assess the level of ANS activity and is a quantitative measure [26]. According to the neurovisceral integration model, reduced HRV is a consequence of reduced activation of the central autonomic network that controls visceral motility, neuroendocrine, and behavioral flexibility [27]. HRV was first used in cardiovascular disease (Cardiovascular disease, CVD). CVD patients with depressive symptoms have a strong sympathetic response to stress, which may promote the formation of atherosclerosis. CVD patients also have impairment of social function, which also increases the risk of depression, and depression and cardiovascular disease may cause and effect each other. Autonomic dysfunction may also be a common risk factor for both disorders [28,29]. Therefore, HRV index has attracted much attention in recent years as a referral biomarker for psychopathology.
The principle and application of VAT
VAT is an ancient technology, but in the past ten years, with the continuous development of rehabilitation and auxiliary therapy technology, it has begun to rise again. The use of single-stringed instruments and vibroacoustic devices has received widespread attention in the use of music therapy to guide relaxation and imagery techniques [30]. VAT uses frequencies within the human hearing range, with the lower frequency range being best experienced and may contribute to better relaxation and/or pain and symptom relief. Studies have shown that the use of 20 Hz somatosensory vibration stimulation is feasible for regulating the functional state of the brain [31]. Isacsson et al. explored the neuro-physiological response of somatosensory music to Rett syndrome, in which the somatosensory music used was a tone between 20 and 70 Hz [32]. It is the main feature of somatosensory music to use the vibration of sound to form tactile stimulation while listening to music. Somatosensory music technology cleverly combines the psychological process (music listening) with the physiological process (tactile sound vibration), which activates both the efferent neural activity that inhibits pain and the afferent neural activity that inhibits pain. These two pathways also integrate somatic and auditory nerve activity into synergistic mechanisms of the central nervous system [33].
The main experiential outcome of somatosensory music is to promote a state of relaxation or relaxation response. This relaxation response includes physical, emotional, and mental relaxation, and is characterized by decreased breathing, heart rate, blood pressure, and a slowed metabolism. After the body produces a relaxation response, the anxiety state caused by different reasons will be relieved. Applying somatosensory music to dying patients, as a method of palliative care, can relieve anxiety and fear of death [34]. Somatosensory music can also be used in the treatment of anxiety in psychiatric disorders. Anxiety disorder is a mood disorder characterized by persistent nervousness, worry, fear, or seizures of panic, with behavioral features such as autonomic symptoms and restlessness in movement [35]. Some somatosensory music therapy systems come with conditioning exercises, including breathing relaxation and muscle relaxation. Relaxation adjustment before the somatosensory music therapy will make it easier to integrate into the music environment, better stimulate the relaxation response and reduce anxiety. A healthy autonomic nervous system (ANS) is able to adjust the body’s inherent bodily functions to an optimal state to maintain the original and rebuild and adapt to a new homeostasis. The antagonism between the parasympathetic nervous system (PNS) and the sympathetic nervous system (SNS) is the key to ensure the adaptation of the organism at the physiological level [36]. When stress persists, it can cause autonomic dysfunction. Somatosensory music regulates stress response by adjusting autonomic nervous function. A study on the effect of somatosensory music on heart rate variability in Germany showed that music can promote relaxation and effectively relieve stress by changing autonomic nerves [37], and heart rate variability is an indicator of autonomic nerve function. Li et al. studied somatosensory music therapy combined with acupuncture in the treatment of post-stroke depression, and observed the changes in mood, cognition and daily living ability of the patients after 4 and 8 weeks. The results show that somatosensory music and acupuncture can relieve post-stroke depression, promote post-stroke neurological recovery, and improve quality of life [38]. Yue’s study found that acupuncture combined with somatosensory music can effectively improve the depression in patients with post-stroke depression (PSD), improve the quality of life of patients, and promote the rehabilitation of PSD patients [39].
The etiology of psychiatric disorders is complex and drug therapy alone is prolonged. Somatosensory music as an auxiliary treatment is very important for the early recovery of patients. At present, somatosensory music is mostly used in the treatment of patients with post-stroke depression, but it is rarely used for depressive episodes without comorbidities, especially adolescent depression, and further research is needed.
We selected 66 inpatients who were diagnosed with moderate depressive episodes from Henan Provincial People’s Hospital from January 2018 to October 2018. We randomly divided the patients into a control group of 33 cases and an intervention group of 33 cases using a random number table. The subjects received routine psychiatric treatment and nursing, and the drug treatment was SSRIs. Inclusion criteria: ① meet the ICD-10 diagnostic criteria for depressive episodes; ② age 18–65 years old, gender is not limited; ③ 24-item Hamilton Depression Rating Scale (24-HAMD) score greater than 20 points; ④ normal hearing, no aversion to music, a those who have not received music therapy within the year; ⑤ Patients who voluntarily signed the informed consent and cooperated. Exclusion criteria: ① Patients with mental retardation or heart disease; ② Combined with severe psychiatric symptoms or personality disorders; ③ Music-related, graduated from a music major, and music-intolerant; ④ There are auditory, visual, tactile and other perceptions People with disabilities; ⑤ Yoga teachers, athletes and pregnant women; ⑥ Those who have received MECT treatment in the past 6 months; ⑦ Patients who are participating in other studies. Dropout criteria: ① those who failed to complete the somatosensory music therapy for 3 times; ② those who did not participate in the somatosensory music therapy for 2 times.
This study was approved by the ethics committee of Xuchang City Jian’an Hospital University and informed consent was provided. (Approval number: 20180232-APP-S). The informed consent form is standardized, easy to understand by most people, and requires the signatures of the subjects themselves and the researcher. If the subjects have doubts, they should give correct answers. All subjects can be enrolled in the research group after carefully reading and signing the informed consent form to ensure the subjects’ right to voluntary participation and informed consent.
After the patients were admitted to the hospital, various examinations were completed, and after two doctors made a joint diagnosis, they were completely randomly assigned to the control group and the intervention group according to the inclusion and exclusion criteria. The control group received routine psychiatric treatment and nursing, and avoided activities related to somatosensory music. The intervention group was given somatosensory music therapy on the basis of routine psychiatric treatment and nursing. The detailed arrangement of somatosensory music therapy is shown in Table 1.
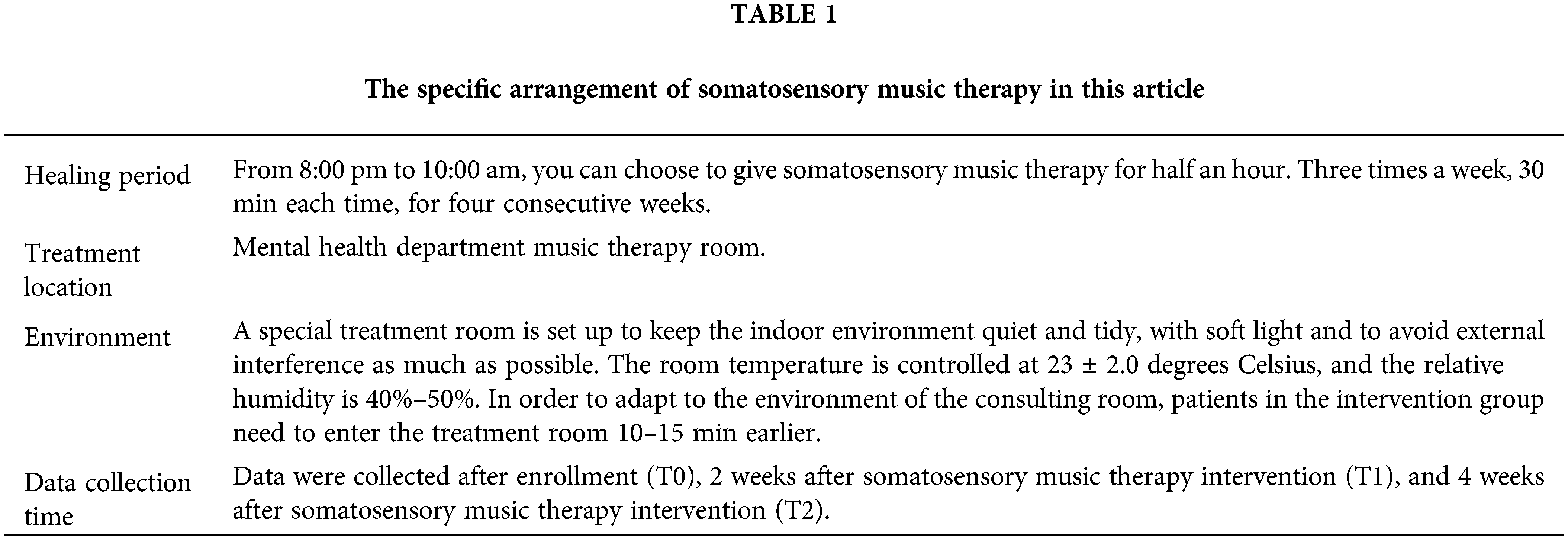
After the patients in the treatment group entered the treatment room, the therapist gave a demonstration of somatosensory music therapy to ensure that the patients successfully completed the treatment. The intervention process of somatosensory music therapy is as follows:
Step 1: We instruct the subjects to sit on the somato-sensory music therapy chair steadily, lean their head against the back of the chair as far as possible, press and hold the stretch button on the right side of the chair, and the chair will open slowly. The subjects choose the most suitable opening angle according to their individual needs.
Step 2: Subjects choose to wear headphones or play music according to their personal preference, clip the heart rate sensor to the right index finger, and observe the changes in physiological indicators during the treatment.
Step 3: After the subject adjusted his posture, he turned on the computer and entered the somatosensory sound wave feedback system interface. After the somatosensory sofa, sensors, and earphones show that the connection is successful, click on the somatosensory music mode, set the time, volume and vibration intensity, and inform the patient that the treatment has started.
Step 4: The treatment lasts for 30 min. After the intervention of somatosensory music, the therapist will slowly wake up the patient to make sure that the patient is awake and has no adverse reactions. The nurse will safely send the patient back to the ward and inform the next treatment time.
In the treatment of somatosensory music, there are still some precautions that need to be observed. First, one hour before the start of the intervention, patients are prohibited from consuming irritating beverages or foods such as tobacco, alcohol, tea, and coffee, so as not to affect the effect of the intervention. The second is that the volume of the power amplifier is controlled at about 40–60 decibels, and it is advisable for the patient to feel comfortable when playing on the earphone. The third is that the volume of the music is gradually increased, and the vibration volume and volume of the music are adjusted in time according to the patient’s response. Fourth, the therapist should be accompanied throughout the treatment to observe the treatment effect at any time and ensure the personal safety of the patient. Other people are prohibited from entering and leaving to avoid disturbing the patient.
The tools used in this study are the self-made situation questionnaire, the Hamilton Depression Scale, the Positive and Negative Affective Scale, the Perceived Stress Scale and heart rate variability analysis. The questionnaire included the patient’s age, sex, education level, marital status, occupation, number of hospital admissions, whether he liked music, and the frequency of listening to music.
HAMD was compiled by Hamilton in 1960 and is the most commonly used scale for clinical assessment of depression. There are 3 versions of the scale with 17 items, 21 items and 24 items. The 24-item version was used in this study, and two psychiatrists in our research group scored the patients. Most HAMD items use a 5-point scoring method ranging from 0 to 4 points, and the standards for each level are: 0 = none, 1 = mild, 2 = moderate, 3 = severe, 4 = extremely severe. A few items use a 3-level scoring method of 0–2 points, and the grading standards are: 0 = none; 1 = mild to moderate; 2 = severe. A total score of more than 35 is considered severe depression, a score of more than 20 is considered mild or moderate depression, and a score of less than 8 indicates no depressive symptoms. The reliability coefficient r of the scale evaluation is 0.88–0.99, and the empirical authenticity coefficient reflecting the severity of clinical symptoms is 0.92.
PANAS is an emotional self-assessment scale jointly compiled by Watson, Clark and Tellegen in 1988, which is used to assess the emotional feelings of individuals in the last 1 to 2 weeks. Positive emotions (PA) consists of 10 adjectives describing positive emotions. Negative emotions (NA) consists of 10 adjectives describing negative emotions. The scale uses a five-point scoring method: 1 = almost nothing, 2 = somewhat, 3 = moderately, 4 = somewhat, 5 = very much. The scores for each dimension range from 10 to 50 points, and the higher the score, the higher the corresponding emotion experienced by the individual. A high score on positive emotions indicates that the individual is energetic and able to concentrate on happy emotions, while a low score indicates that the individual is relatively indifferent. A high score of negative emotion indicates that the individual feels more confused and has painful emotions, while a low score indicates that the individual is calmer.
PSS was compiled by American psychologist Dr. Cohen in 1983. It is a self-evaluation scale that reflects the degree of stress through the tension of individual perception. It is a general stress measurement tool, including 2 dimensions of loss of control and tension, consisting of 14 items. The item rating ranges from 0 (never) to 4 (always), and the total score ranges from 0 to 56. The higher the score, the greater the individual’s perceived pressure. The optimal cut-off value of PSS is 25/26, that is, the scale score ≥26 points can be judged as having health-threatening stress, and ≤25 points can be judged as having no health-threatening stress, which is suitable for quantifying psychological stress in the general population and special populations evaluation and clinical research.
HRV analysis refers to reflecting the change of heart rate by measuring the variability of continuous RR interval change, which is one of the observation indicators of cardiac auto-nomic nervous activity. There are many evaluation methods for autonomic nervous function, and HRV analysis is a non-invasive, quantitative and sensitive index that is currently recognized in medicine. HRV analysis can detect coordination and antagonism between sympathetic and parasympathetic nerves, and can also be used to assess mental stress. HRV analysis methods include time domain analysis, frequency domain analysis, spectrum analysis, geometric analysis and nonlinear analysis, among which time domain analysis and frequency domain analysis are more commonly used. We use a 24-bit analog-to-digital converter to sample HRV data, and the sampling rate is set to 128 Hz. HRV was continuously recorded throughout the test, and these physiological signals were stored on a computer running the Microsoft operating system. A 5-min short-term HRV test was performed on the subjects at T0, T1, and T2 time points, respectively. Before each test, the subjects rested for 10 min in a quiet state. Afterwards, we asked the subject to breathe naturally and calmly, connected the pulse oxygen clip to the subject’s right index finger, and within 5 min without interference, recorded the HRV data through the analyzer and analyzed it to obtain a report.
We used SPSS 21.0 software for statistical analysis of data, and Graph Pad Prism 8.0 for statistical mapping. The measurement data conforming to the normal distribution is described by the mean ± standard deviation, the non-normal distribution data is described by the median (interquartile distance), and the measurement data between the two groups is compared by an independent sample t test, involving two factors of time Repeated measures analysis of variance was used in the experiment. The count data were described by percentage, and the statistical analysis was Chi-square test. Pearson correlation was used to conduct linear correlation analysis among influencing factors, and α = 0.05 was used as the test level.
Experimental Results and Analysis
A total of 61 patients with depressive disorders were enrolled in this study, 30 of whom entered the intervention group to receive somatosensory music therapy, and the other 31 patients entered the control group to receive routine treatment and nursing. In the intervention group, 2 patients were considered dropped out because they did not participate in somatosensory music therapy twice. 1 patient dropped out of treatment midway. In the control group, 2 patients were automatically discharged early and failed to be followed up as dropped out.
Analysis of the therapeutic effect of somatosensory music therapy on patients with depression
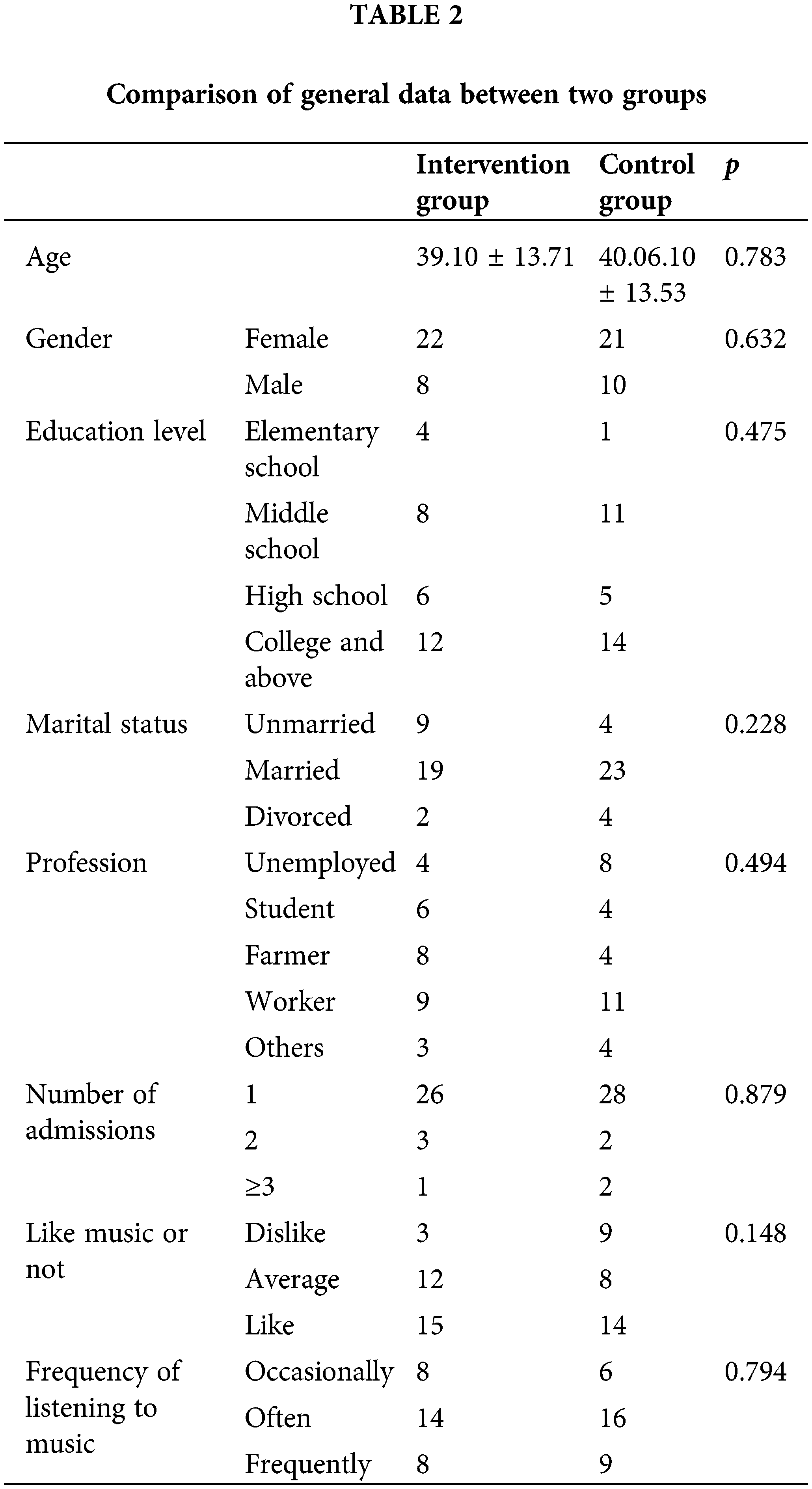
The demographic characteristics of the two groups were compared through the general situation questionnaire, and the results showed that there was no statistical significance between the two groups in terms of age, gender, education level, marital status, occupation, number of hospital admissions, whether they liked listening to music and the frequency of listening to music (p > 0.05), specifically as shown in Table 2.
The results of repeated measures analysis of variance showed that the HAMD scores of the two groups decreased to varying degrees after 4 weeks of treatment, and the difference between the two groups was statistically significant (p < 0.05). Analyzing the time factor alone, the HAMD score decreased to varying degrees with the prolongation of time, and the difference was statistically significant (p < 0.01). There was an interaction between time and intervention factors (p < 0.05). The specific results are shown in Table 3 and Fig. 1.
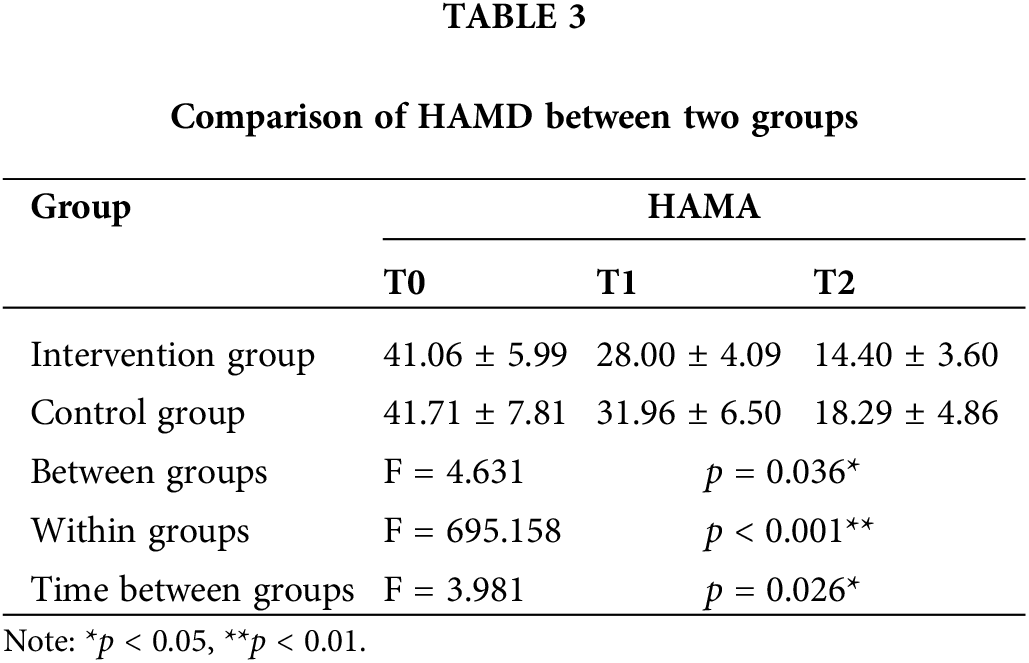
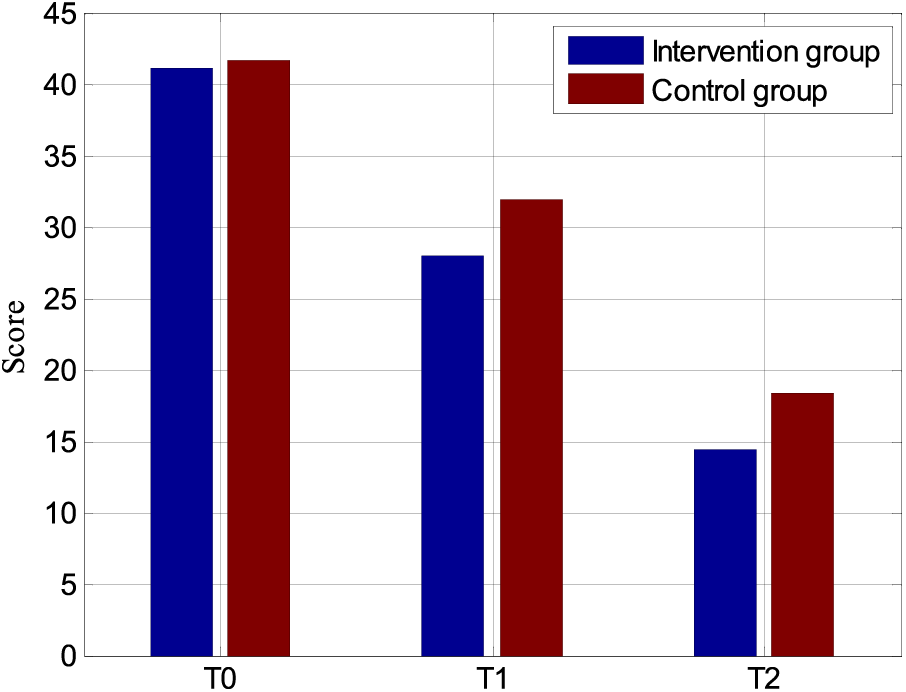
Figure 1: Comparison of HAMD between two groups in graphical results.
Table 4 and Fig. 2 compare the positive and negative emotions of the intervention group and the control group. Positive emotion: After 4 weeks of treatment, the positive emotion scores of the two groups increased to varying degrees, and the differences between the groups were statistically significant (p < 0.05). The effect of time in the two groups was analyzed separately, and the scores increased to varying degrees with the prolongation of time, and the difference within the group was statistically significant (p < 0.01). There was no interaction between time and intervention factors (p > 0.05). Negative emotion: After 4 weeks of treatment, the negative emotion scores of the two groups decreased to varying degrees, and the differences between the groups were statistically significant (p < 0.05). Analyzing the effect of time in the two groups separately, the scores decreased to varying degrees with the prolongation of time, and the difference within the group was statistically significant (p < 0.01). There was no interaction between time and intervention factors (p > 0.05).
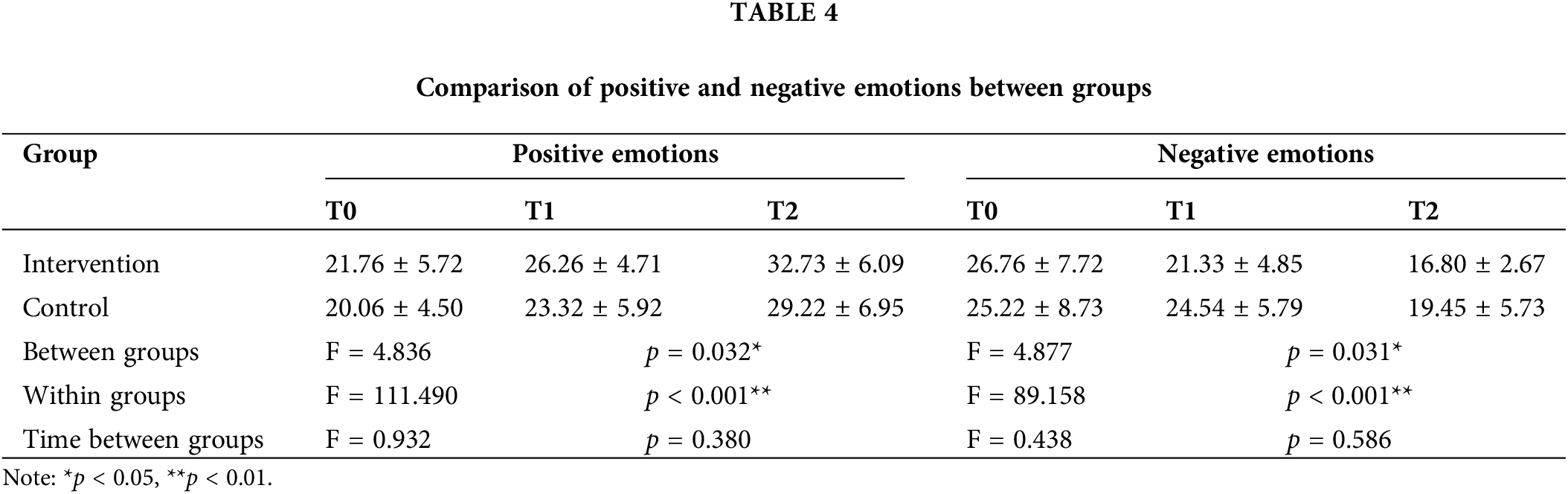
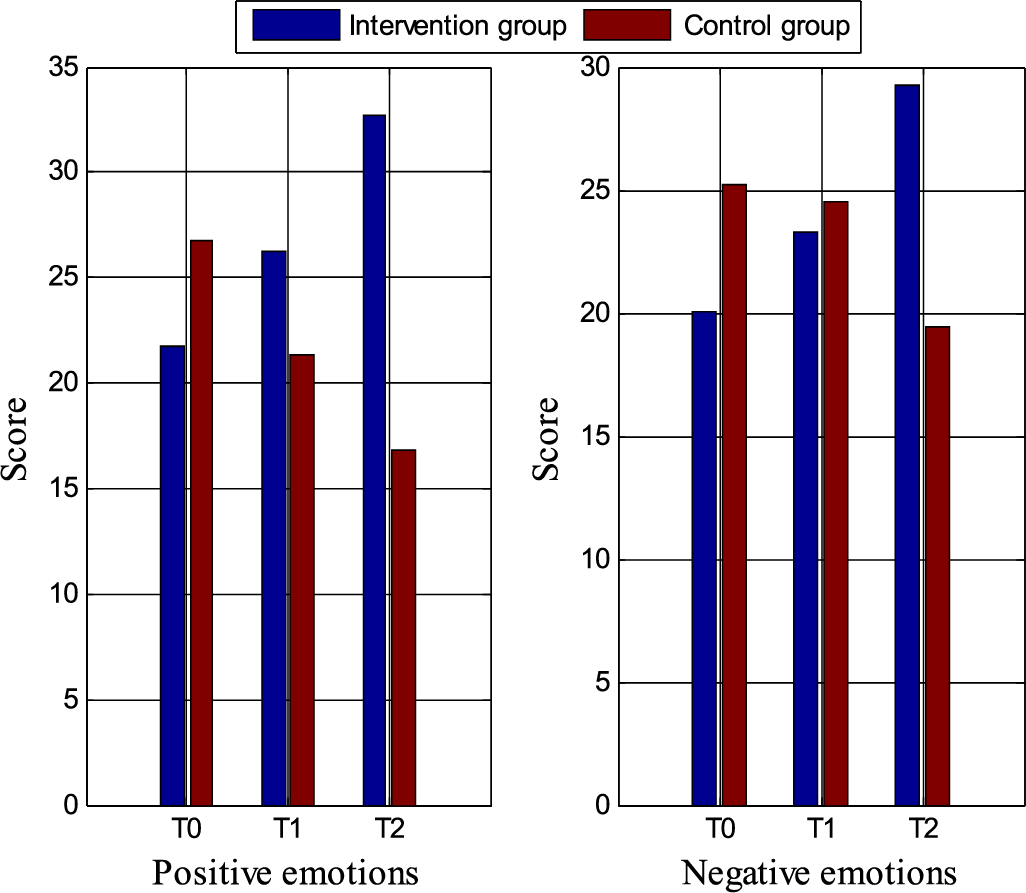
Figure 2: Comparison of positive and negative emotions between groups in graphical results.
Table 5 and Fig. 3 compare the scores of the Perceived Stress Scale between the intervention group and the control group. The results of repeated measures analysis of variance showed that the CPSS scores of the two groups decreased to varying degrees after 4 weeks of treatment, and the difference between the two groups was statistically significant (p < 0.05). When analyzing the effect of time alone, the CPSS score decreased to varying degrees with the prolongation of time, and the difference between groups was statistically significant (p < 0.01). There was an interaction between time and intervention factors (p < 0.01).
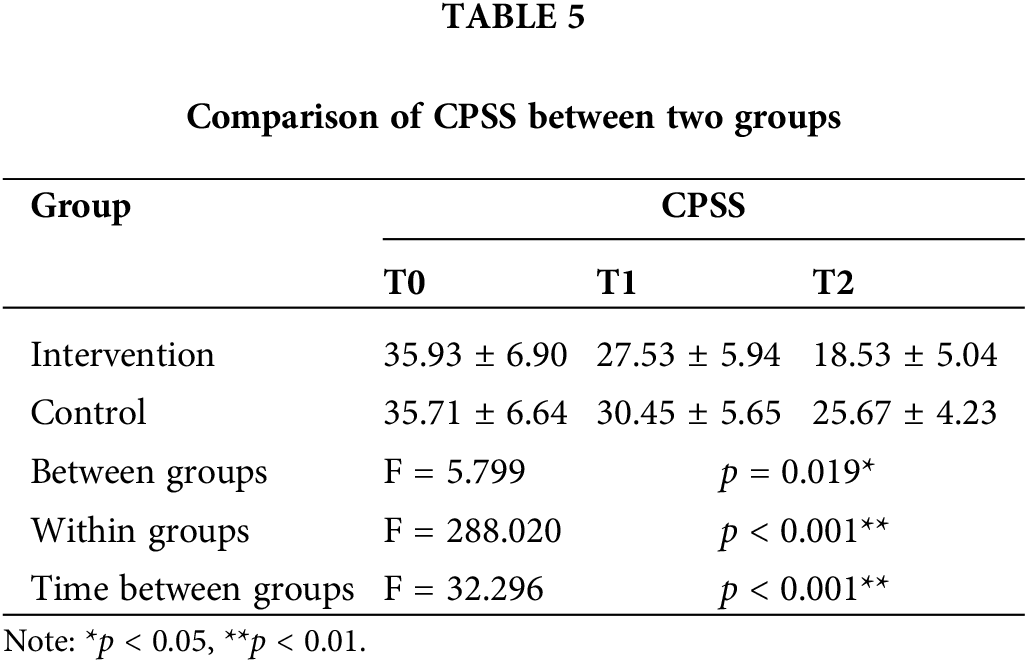
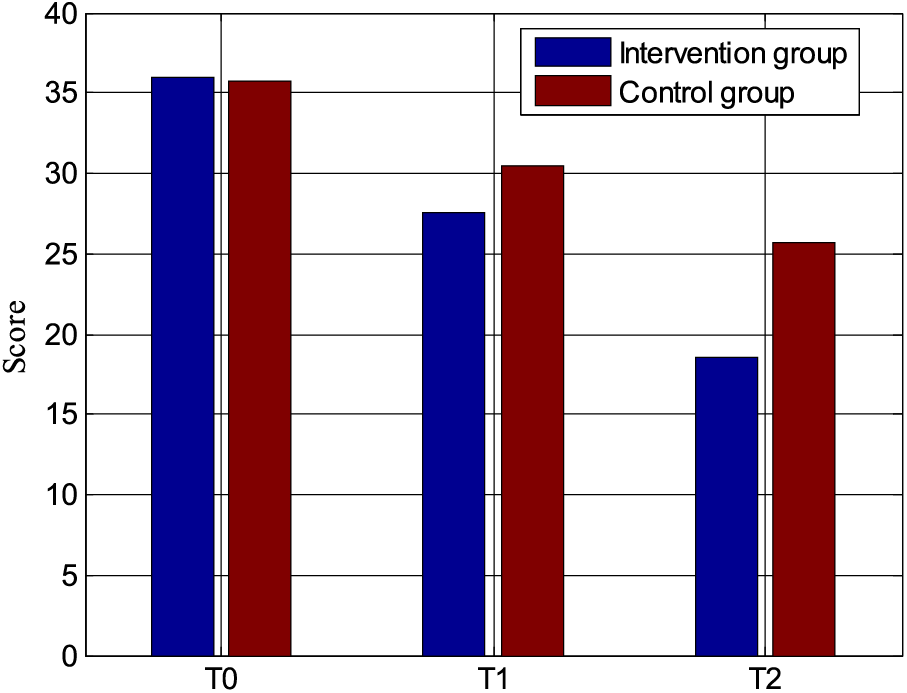
Figure 3: Comparison of CPSS between two groups in graphical results.
Table 6 and Fig. 4 are the comparison of HRV time-domain indicators between the intervention group and the control group. The main effect of the intervention factors was analyzed separately, and after 4 weeks of treatment, SDNN and RMSSD indicators all increased to varying degrees. The degree of increase in the intervention group was greater than that in the control group, and the difference between the groups was statistically significant (p < 0.05). When analyzing the main effect of time alone, SDNN and RMSSD indicators also tended to increase, and the difference within the group was statistically significant (p < 0.01). There was an interaction between time and intervention factors (p < 0.05).
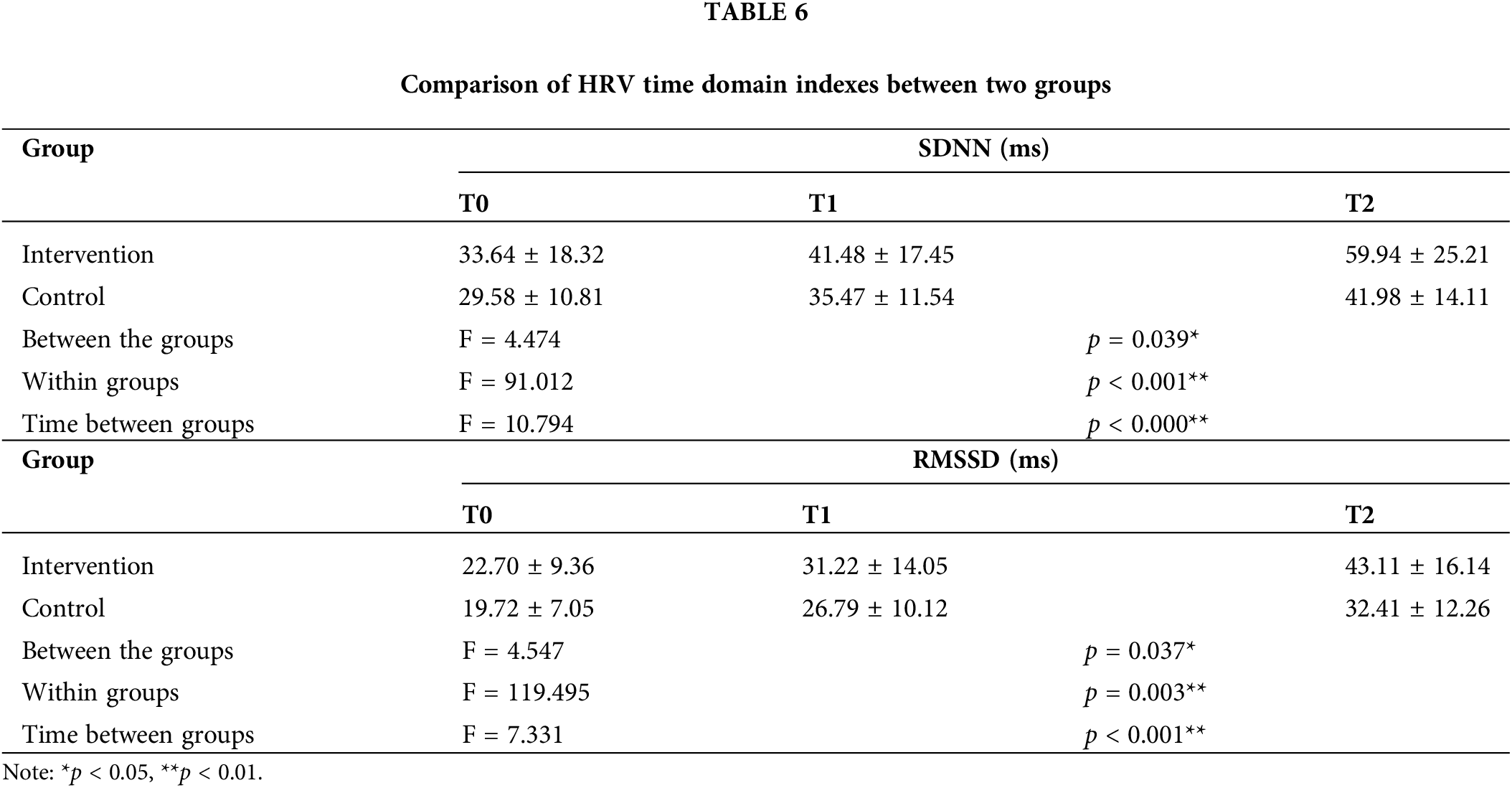
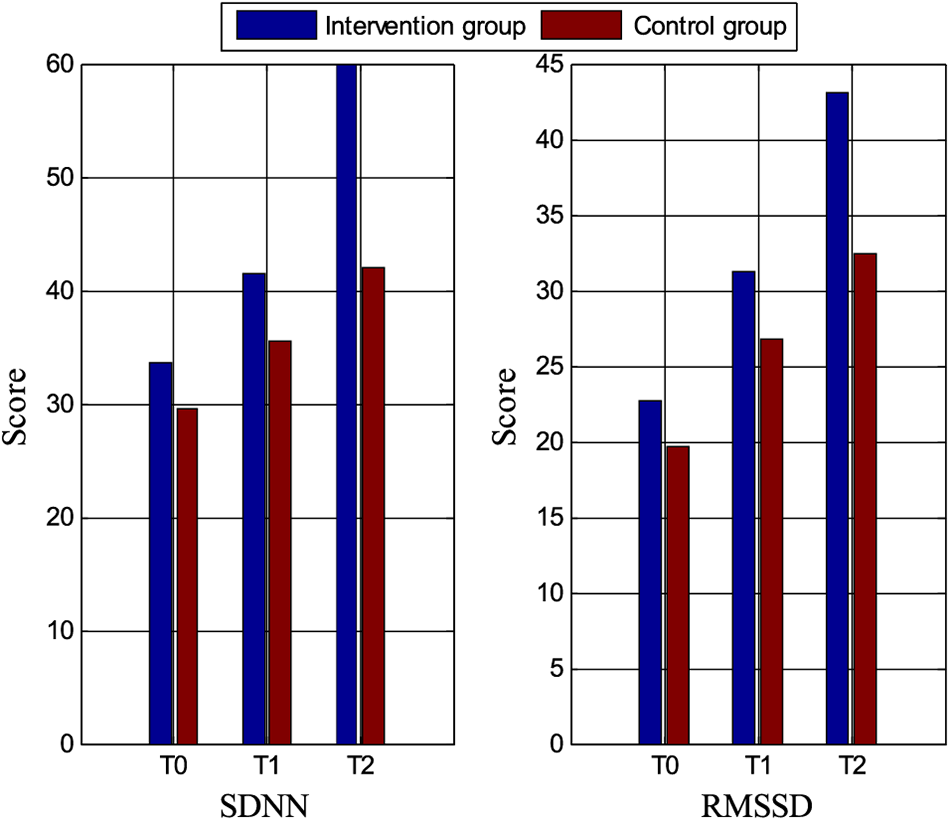
Figure 4: Comparison of HRV time domain indexes between two groups in graphical results.
Improvement of depression severity with somatosensory music therapy
Depression is a common disease in psychiatry, and it is self-evident to explore effective treatment methods in clinical practice for individuals and society. In this study, somatosensory music therapy was used to evaluate its effects on the degree of depression, positive and negative emotions, perceived stress, and HRV in patients with depressive disorders. This study proves the efficacy of somatosensory music-assisted therapy in the treatment of depressive disorders. This safe, effective, and non-drug treatment is worthy of promotion in mental illness.
After 4 weeks of somatosensory music intervention, the HAMD scores of both the intervention group and the control group were lower than before, and the depressive symptoms were alleviated to varying degrees, but the treatment effect of the intervention group was better than that of the control group. The intervention group basically reached the level of mild depression at the end of treatment. This shows that somatosensory music has a certain effect on relieving depressive symptoms and reducing the severity of the disease, and the therapeutic effect is more obvious as time goes on. Somatosensory music therapy is considered to be a non-invasive, non-drug and non-electrical form of low-frequency sound wave stimulation. When the stimulation acts on the human body, the vibration and pressure mechanoreceptors (Pacinian corpuscle, PC) around the internal organs and joints can sense the pressure and vibration stimulation [40]. One hypothesis is that the PC sends afferent impulses through the vagus nerve until the medulla, nucleus solitary tract, and visceral nerves within spinal fibers reach the spinal sensory ganglia [41]. The vagus nerve enters the brain through the nucleus solitary tract, connecting the amygdala, frontal cortex, and other brain regions. These brain regions are related to depression and play an important role in emotion regulation, which may be a mechanism for somatosensory music to relieve depressive symptoms. Previous studies have shown that adding music therapy to standard treatment and nursing can significantly reduce depressive symptoms and have a special impact on the overall state and function of patients [42]. The study by Janzen et al. [43] showed that music intervention alone and somatosensory music stimulation can reduce the degree of depression and associated symptoms in patients with depressive disorders. The above studies are consistent with the results of this study, which shows that adding music intervention to standard treatment and care is a promising adjunctive treatment for depression. Most previous studies believed that drugs play a dominant role in the treatment of antidepressants, and this study does not rule out the role of drugs. However, drug treatment still leaves certain symptoms, which cannot achieve a 100% recovery, resulting in recurrence or resurgence of the disease after discharge. Therefore, assisting simple and easy-to-accept non-drug treatment during hospitalization plays a vital role in the improvement of clinical symptoms and family rehabilitation after discharge.
With the continuous deepening of research on mental illness, patients have higher and higher expectations for treatment. Mere drug therapy cannot meet the psychological needs of patients. Effective and diverse treatments can enrich patients’ hospital life and reduce the incidence of cardiovascular and metabolic diseases. A new type of VA treatment device has been researched and developed and experienced by 26 volunteers. The results show that VAT treatment can promote relaxation response, relieve pain, reduce anxiety and depression, and can be used in various places to promote health and even treat diseases [44].
Effect of somatosensory music therapy on positive and negative emotions and perceived pressure in patients with depression
Attentional bias in patients with depressive disorders is an important issue in the study of disease cognition. Some researchers used standardized emotional pictures to test the emotion recognition of patients with depressive disorders, and found that patients with depressive disorders have negative emotion bias [45]. Most of them have difficulties in emotion recognition and cognitive bias, and have inhibitory dysfunction to negative information, pay more attention to and be more easily affected by negative emotions and information, but are not affected by positive emotions. In this study, after the intervention group received somatosensory music therapy, the negative emotions decreased and the positive emotions increased. The first may be the drug’s effect on emotion-regulating brain regions such as the amygdala. Secondly, when the patient receives somatosensory music therapy, the patient devotes himself to the physical experience and auditory experience. The wonderful and comfortable environment corrects the patient’s attentional bias, allowing patients to pay more attention to positive emotions and events, while the protective environment reduces the stimulation of negative emotions and events. In this way, the effect of positive emotions is strengthened, so the negative emotions of patients with depression are reduced, and the positive emotions are increased, and this effect becomes more obvious as time goes on. A study on the regulation of music on depression showed that the less music clips used to stimulate negative emotions, the more music clips used to stimulate positive emotions, the lower the score of the depression self-rating scale, and the less obvious the depression [46]. Music and somatosensory can affect emotions, and more mechanisms are worthy of our continuous and in-depth research in the future.
PS refers to people’s experience of some kind of super-personal ability, and PSS is the most widely used psychological tool to measure stress. The items are designed to understand how unpredictable, uncontrollable, and overloading stress can be, and are used to measure the degree of perceived stress in an individual’s life. One study found that people with low perceived stress had less increase in depressed mood in the face of negative life events, whereas people with high perceived stress had a greater increase in depressed mood in the face of negative life events [47]. Our study found that after 4 weeks of somatosensory music-assisted therapy, the perceived pressure of the control group and the intervention group decreased, and the difference between the two groups was statistically significant. At baseline, patients had higher HAMD scores, negative mood scores, and perceived stress scores. With the increase of treatment and the prolongation of time, the scores of all three decreased. This is consistent with the results of the previous study, and also reveals that there may be some correlation among the three. Many studies have shown that perceived stress plays a mediating role in the relationship between depression and anxiety symptoms and quality of life [48].
This study also evaluates the perceived stress, because the reduction of perceived stress may be a manifestation of the improvement of depressive symptoms, which can indirectly measure the curative effect of somatosensory music therapy on patients with depressive disorder. When patients receive somatosensory music therapy, one theory is that baro-receptors receive stimulation from low-frequency music, which promotes a relaxation response. Another theory is that continuous stress can cause autonomic dysfunction, and somatosensory music therapy can reduce stress by adjusting the balance of autonomic function. In the process of somatosensory music therapy, patients have better self-experience, and their compliance increases with time. Therefore, after the intervention, the pressure of patients is reduced, and the influence of psychological effects cannot be ruled out.
Effect of somatosensory music therapy on autonomic nervous function in patients with depressive disorder
The autonomic nervous system functions through the dynamic nature of the balance between the sympathetic and parasympathetic nerves. Among them, HRV is an effective non-invasive measurement method to assess the autonomic regulation of the heart, which mainly reflects the balance between sympathetic and parasympathetic input in cardiac pacing. A low HRV implies an increase in cardiac sympathetic modulation or a relative decrease in cardiac parasympathetic modulation. A large number of studies have shown that autonomic imbalance and possibly depression are related. In this study, HRV index was used to evaluate autonomic nervous function, SDNN reflected the effect of sympathetic nerve, and RMSSD mainly reflected the influence of parasympathetic nerve on heart rate.
After 4 weeks of intervention in this study, compared with the control group, the two indicators of SDNN and RMSSD increased in the intervention group, and the difference was statistically significant, and the increase in the two indicators was also similar. This is because SDNN is the standard deviation value, and RMSSD is the square root of the mean square deviation, and there is a correlation between the calculation methods of the two indicators. Several studies have also shown that HRV is reduced in depressed patients with and without cardiovascular disease compared with non-depressed patients [49,50]. The results of this study support the hypothesis that depression may be an altered autonomic regulation of the heart, a state of more sympathetic and less parasympathetic activation. Although our study cannot explain the underlying mechanism of HRV changes in depression, somatosensory music therapy can indirectly reduce the excitability of sympathetic nerves and increase the excitability of parasympathetic nerves to relieve depressive symptoms.
Controversy exists as to whether cardiac autonomic dysfunction is a feature of depression itself or a result of antidepressant drug treatment. The study by Licht et al. [51] supported the reduction of cardiac vagal tone by antidepressants (TCAs, SNRIs and SSRIs). In addition, their study also showed that stopping antidepressant medication can restore the autonomic regulation of the heart. This suggests that the adverse effects of the drug on cardiac autonomics are (at least partially) reversible. Some studies have also shown that fluoxetine in SSRIs does not affect HRV and heart rate [52]. Consistent conclusions have not been drawn regarding the effects of drugs on autonomic function. This study also failed to separate drugs and somatosensory music therapy for discussion. However, this adjuvant treatment has been shown to have an effect on autonomic balance and emotional stability. If the balance of the nerves can be adjusted through non-drug interventions, the side effects of drugs can be avoided, and it is also a new therapy worthy of research.
In this study, the data of 61 patients with depressive disorders were collected and analyzed, and 30 patients received somatosensory music therapy intervention. The results show that somatosensory music-assisted therapy can reduce the degree of depression, relieve depression, reduce stress perception, increase heart rate variability, and is beneficial to the balance of autonomic nerves. However, due to the small sample size of this study, the sample size will be increased in the future, and the correlation study of the mechanism and cause will be carried out independently without interference factors. This study only collected the data of 4 weeks of somatosensory music therapy intervention, and failed to extend the intervention time and follow-up at the end of the treatment. In the future, the intervention group will be followed up and the control group will be given the same somatosensory music therapy after the trial. Due to the existence of psychological effects and treatment tendencies, this study cannot rule out the influence of psychological effects and personal preferences. Because most mental illnesses are psychologically active and respond to placebo treatments. Therefore, follow-up research should conduct interviews with patients receiving somatosensory music to understand their psychological changes and personal feelings. This study cannot rule out the influence of drugs, because the presence of drugs is essential in order to meet the treatment needs of patients in clinic. However, drugs for mental illness cannot achieve 100% therapeutic effect, and there are certain drawbacks. The introduction of some non-drug-assisted treatment is beneficial to the recovery of the disease and the physical and mental health of the patients, but the homogeneity of the drugs should also be achieved during the research process to reduce unnecessary confounding factors.
The goal of this study is to bring the psychosomatic experience of somatosensory music to clinical patients, and to confirm its efficacy in depression, improve the singleness of drug treatment, and provide a new strategy for clinical treatment. The effect of somatosensory music on HRV should be further explored. Previous studies have shown that autonomic dysfunction is manifested by reduced HRV, which may be a mechanism by which depression increases the risk of cardiovascular disease [53]. At the same time, there are changes in HRV indicators in patients with depression. If this indicator is used to identify susceptible populations and regulate autonomic regulation through changes in living habits and non-pharmaceutical interventions, it will help reduce the incidence of depression and related adverse cardiovascular diseases in the future.
In recent years, the incidence of mental illness has shown an upward trend, and the spectrum of mental illness has undergone great changes. Anxiety disorders and mood disorders have significantly surpassed schizophrenia and other mental disorders, and depression is the most common mood disorder. Therefore, we should continuously improve the treatment strategies for diseases such as anxiety and depression to meet the needs of current disease changes. The somatosensory music therapy in this study has a certain therapeutic effect on the degree of depression, positive and negative emotions, perceived stress and HRV of patients with depressive disorder. The study in this paper is acceptable to all patients receiving somatosensory music therapy regardless of age, gender, and education level, and no adverse reactions related to somatosensory music therapy were observed during the intervention. All these prove that the therapy is safe and reliable, and has a wide range of applicable values. In the future, the long-term curative effect will be tracked and followed up, and more beneficial value of somatosensory music therapy will be discovered, and its application scope will be expanded, especially family rehabilitation treatment in the recovery period of mental illness.
Acknowledgement: The authors thank research participants for their participation in this study.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Xiaodan Wang; data collection: Zheng Xie; analysis and interpretation of results: Guiping Du; draft manuscript preparation: Xiaodan Wang, Zheng Xie, Guiping Du. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The experimental data used to support the findings of this study are available from the corresponding author upon request.
Ethics Approval: This study was approved by the ethics committee of Xuchang City Jian’an Hospital University and informed consent was provided. Approval number: 20180232-APP-S.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Sroufe L. Psychopathology as an outcome of development. Dev Psychopathol. 1997;9(2):251–68. doi:10.1017/S0954579497002046. [Google Scholar] [PubMed] [CrossRef]
2. Friedrich M. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517. doi:10.1001/jama.2017.3826. [Google Scholar] [PubMed] [CrossRef]
3. Vos T, Flaxman A, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2163–96. doi:10.1016/S0140-6736(12)61729-2. [Google Scholar] [PubMed] [CrossRef]
4. Su J, Wei Z, Gao Y, Wang J. Disease burden of depressive disorders in Beijing, 2010. Capital J Public Health. 2018;2018(1):34–6. [Google Scholar]
5. Vos T, Allen C, Arora M, Barber R, Bhutta Z, Brown A, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1545–602. doi:10.1016/S0140-6736(16)31678-6. [Google Scholar] [PubMed] [CrossRef]
6. Stringaris A. Editorial: what is depression? J Child Psychol Psychiatry. 2017;58(12):1287–9. doi:10.1111/jcpp.12844. [Google Scholar] [PubMed] [CrossRef]
7. Etkin A, gner T, Peraza D, Kandel E, Hirsch J. Resolving emotional conflict: a role for the rostral anterior cingulate cortex in modulating activity in the amygdala. Neuron. 2006;51(6):871–82. doi:10.1016/j.neuron.2006.07.029. [Google Scholar] [PubMed] [CrossRef]
8. Dannlowski U, Ohrmann P, Konrad C, Domschke K, Bauer J, Kugel H, et al. Reduced amygdala-prefrontal coupling in major depression: association with MAOA genotype and illness severity. Int J Neuropsychopharmacol. 2009;12(1):11–22. doi:10.1017/S1461145708008973. [Google Scholar] [PubMed] [CrossRef]
9. Wang Y, Yang S, Sun W, Shi Y, Duan H. Altered functional interaction hub between affective network and cognitive control network in patients with major depressive disorder. Behav Brain Res. 2016;298(829):301–9. doi:10.1016/j.bbr.2015.10.040. [Google Scholar] [PubMed] [CrossRef]
10. Bennabi D, Yrondi A, Charpeaud T, Genty J, Destouches S, Lancrenonet S, et al. Clinical guidelines for the management of depression with specific comorbid psychiatric conditions French recommendations from experts (the French Association for Biological Psychiatry and Neuropsychopharmacology and the fondation FondaMental). BMC Psychiatry. 2019;19(1):1–9. doi:10.1186/s12888-019-2025-7. [Google Scholar] [PubMed] [CrossRef]
11. Wang J, Wang H, Zhang D. Impact of group music therapy on the depression mood of college students. Health. 2011;3(3):151–5. [Google Scholar]
12. Chen C, Chen Y, Ho C, Lee Y. Effects of preferred music therapy on peer attachment, depression, and salivary cortisol among early adolescents in Taiwan. J Adv Nurs. 2019;75(9):1911–21. doi:10.1111/jan.13975. [Google Scholar] [PubMed] [CrossRef]
13. Ruute E, Ratnik M, Tamm E, Zilensk H. The experience of vibroacoustic therapy in the therapeutic intervention of adolescent girls. Nord J Music Ther. 2004;13(1):33–46. doi:10.1080/08098130409478096. [Google Scholar] [CrossRef]
14. Koike Y, Hoshitani M, Tavata Y, Seki K, Nishimura R, Kano Y. Effects of vibroacoustic therapy on elderly nursing home residents with depression. J Phys Ther Sci. 2012;24(3):291–4. doi:10.1589/jpts.24.291. [Google Scholar] [CrossRef]
15. Chen Z, Zhang H, Wang X, Lv X. Three theoretical perspectives on the origin of depression. Adv Psychol Sci. 2018;26(6):1041–53. doi:10.3724/SP.J.1042.2018.01041. [Google Scholar] [CrossRef]
16. Sorgdrager F, Doornbos B, Penninx B, Jonge P, Kema I. The association between the hypothalamic pituitary adrenal axis and tryptophan metabolism in persons with recurrent major depressive disorder and healthy controls. J Affect Disord. 2017;222:32–3. doi:10.1016/j.jad.2017.06.052. [Google Scholar] [PubMed] [CrossRef]
17. Davis S, Kaulfers A, Lochman J, Morrison S, Pryor E, Rice M. Depressive symptoms, perceived stress, and cortisol in school-age children with Type 1 diabetes: a pilot study. Biol Res Nurs. 2019;21(2):166–72. doi:10.1177/1099800418813713. [Google Scholar] [PubMed] [CrossRef]
18. Daches S, Vine V, George C, Kovacs M. Adversity and depression: the moderating role of stress reactivity among high and low risk youth. J Abnorm Child Psychol. 2019;47(8):1391–9. doi:10.1007/s10802-019-00527-4. [Google Scholar] [PubMed] [CrossRef]
19. Park C, Rosenblat J, Brietzke E, Pan Z, Lee Y, Cao B, et al. Stress, epigenetics and depression: a systematic review. Neurosci Biobehav Rev. 2019;102(9):139–52. doi:10.1016/j.neubiorev.2019.04.010. [Google Scholar] [PubMed] [CrossRef]
20. Levin G, Xu L. How could stress lead to major depressive disorder? IBRO Rep. 2018;4:38–43. doi:10.1016/j.ibror.2018.04.001. [Google Scholar] [PubMed] [CrossRef]
21. Vasunilashorn S, Glei D, Weinstein M, Goldman N. Perceived stress and mortality in a Taiwanese older adult population. Stress. 2013;16(6):600–6. doi:10.3109/10253890.2013.823943. [Google Scholar] [PubMed] [CrossRef]
22. Yavuzer Y, Albayrak G, Kilicarslan S. Relationships amongst aggression, self-theory, loneliness, and depression in emerging adults. Psychol Rep. 2019;122(4):1235–58. doi:10.1177/0033294118784866. [Google Scholar] [PubMed] [CrossRef]
23. Lamis D, Hirsch J, Pugh K, Topciu R, Nsamenang S, Goodman A, et al. Perceived cognitive deficits and depressive symptoms in patients with multiple sclerosis: perceived stress and sleep quality as mediators. Mult Scler Relat Disord. 2018;25(3):150–5. doi:10.1016/j.msard.2018.07.019. [Google Scholar] [PubMed] [CrossRef]
24. Gibbons C. Basics of autonomic nervous system function. Handb Clin Neurol. 2019;160:407–18. [Google Scholar] [PubMed]
25. Lin I, Fan S, Yen C, Yeh Y, Tang T, Huang M, et al. Heart rate variability biofeedback increased autonomic activation and improved symptoms of depression and insomnia among patients with major depression disorder. Clin Psychopharmacol Neurosci. 2019;17(2):222–32. doi:10.9758/cpn.2019.17.2.222. [Google Scholar] [PubMed] [CrossRef]
26. Bassett D. A literature review of heart rate variability in depressive and bipolar disorders. Aust N Z J Psychiatry. 2016;50(6):511–9. doi:10.1177/0004867415622689. [Google Scholar] [PubMed] [CrossRef]
27. Beauchaine T, Thayer J. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int J Psychophysiol. 2015;98(2):338–50. doi:10.1016/j.ijpsycho.2015.08.004. [Google Scholar] [PubMed] [CrossRef]
28. Ha J, Park S, Yoon D, Kim B. Short-term heart rate variability in older patients with newly diagnosed depression. Psychiatry Res. 2015;226(2–3):484–8. doi:10.1016/j.psychres.2015.02.005. [Google Scholar] [PubMed] [CrossRef]
29. Kemp A, Quintana D, Quinn C, Hopkinson P, Harris A. Major depressive disorder with melancholia displays robust alterations in resting state heart rate and its variability: implications for future morbidity and mortality. Front Psychol. 2014;5:1–9. doi:10.3389/fpsyg.2014.01387. [Google Scholar] [PubMed] [CrossRef]
30. Dietrich C, Teut M, Samwel K, Narayanasamy S, Rathapillil T, Thathews G. Treating palliative care patients with pain with the body tambura: a prospective case study at St. Joseph’s hospice for dying destitute in Dindigul South India. Indian J Palliat Care. 2015;21(2):236–41. doi:10.4103/0973-1075.156509. [Google Scholar] [PubMed] [CrossRef]
31. Ma N, Wang X, Tian M, Liu J, Qi H, Ming D. Research on the effects of 20 Hz frequency somatosensory vibration stimulation on electroencephalogram features. J Biomed Eng. 2016;33(6):1046–52. [Google Scholar]
32. Isacsson M, Lagerkvist B, Holck U, Gold C. Neurophysiological responses to music and vibroacoustic stimuli in Rett syndrome. Res Dev Disabil. 2014;35(6):1281–91. doi:10.1016/j.ridd.2014.03.002. [Google Scholar] [PubMed] [CrossRef]
33. Lim E, Lim R, Suhaimi A, Chan B, Wahab A. Treatment of chronic back pain using indirect vibroacoustic therapy: a pilot study. J Back Musculoskelet Rehabil. 2018;31(6):1041–7. doi:10.3233/BMR-171042. [Google Scholar] [PubMed] [CrossRef]
34. Warth M, Kessler J, Kotz S, Hillecke T, Bardenheuer H. Effects of vibroacoustic stimulation in music therapy for palliative care patients: a feasibility study. BMC Complement Altern Med. 2015;15(1):1–8. doi:10.1186/s12906-015-0933-8. [Google Scholar] [PubMed] [CrossRef]
35. Hajebi A, Motevalian S, Movaghar A, Sharifi V, Esmaeili M, Radgoodarzi R, et al. Major anxiety disorders in Iran: prevalence, sociodemographic correlates and service utilization. BMC Psychiatry. 2018;18(1):1–8. doi:10.1186/s12888-018-1828-2. [Google Scholar] [PubMed] [CrossRef]
36. Krkovic K, Clamor A, Lincoln T. Emotion regulation as a predictor of the endocrine, autonomic, affective, and symptomatic stress response and recovery. Psychoneuroendocrinology. 2018;94:112–20. doi:10.1016/j.psyneuen.2018.04.028. [Google Scholar] [PubMed] [CrossRef]
37. Gaebel C, Garrrido N, Koenig J, Hillecke T, Warth M. Effects of monochord music on heart rate variability and self-reports of relaxation in healthy adults. Complement. 2017;24(2):97–103. doi:10.1159/000455133. [Google Scholar] [PubMed] [CrossRef]
38. Li X, Wang J, Xu A, Huang J, Meng L, Huang R, et al. Clinical effects and safety of electroacupuncture for the treatment of post-stroke depression: a systematic review and meta-analysis of randomised controlled trials. Acupunct Med. 2018;36(5):284–93. doi:10.1136/acupmed-2016-011300. [Google Scholar] [PubMed] [CrossRef]
39. Yue H. Effect of acupuncture and moxibustion combined with somatosensory music therapy on the rehabilitation of patients with post-stroke depression. Jilin J Chinese Med. 2015;35(2):203–5. [Google Scholar]
40. Feito J, Suarez O, Piqueras J, Mesa Y, Sanchez A, Suazo I, et al. The development of human digital meissner’s and Pacinian corpuscles. ANN ANAT. 2018;219:8–24. doi:10.1016/j.aanat.2018.05.001. [Google Scholar] [PubMed] [CrossRef]
41. Biswas A, Manivannan M, Srinivasan M. Vibrotactile sensitivity threshold: nonlinear stochastic mechanotransduction model of the Pacinian corpuscle. IEEE Trans Haptics. 2014;8(1):102–13. doi:10.1109/TOH.2014.2369422. [Google Scholar] [PubMed] [CrossRef]
42. Leubner D, Hinterberger T. Reviewing the effectiveness of music interventions in treating depression. Front. 2017;8:1–21. doi:10.3389/fpsyg.2017.01109. [Google Scholar] [PubMed] [CrossRef]
43. Janzen T, Shirawai M, Rogzinger S, Kennedy S, Bartel L. A pilot study investigating the effect of music-based intervention on depression and anhedonia. Front. 2019;10:1–13. doi:10.3389/fpsyg.2019.01038. [Google Scholar] [PubMed] [CrossRef]
44. Sigurdardottir G, Nielsen P, Ronager J, Wang A. A pilot study on high amplitude low frequency-music impulse stimulation as an add-on treatment for depression. Brain Behav. 2019;9(10):1–6. doi:10.1002/brb3.1399. [Google Scholar] [PubMed] [CrossRef]
45. Zhang L, Yu F, Hu Q, Qiao Y, Xuan R, Ji G, et al. Effects of SSRI antidepressants on attentional bias toward emotional scenes in first-episode depressive patients: evidence from an eye-tracking study. Psychiatry Investig. 2020;17(9):871–9. doi:10.30773/pi.2019.0345. [Google Scholar] [PubMed] [CrossRef]
46. Patil A, Lin C, Lee S, Huang H, Wu S, Madathil D, et al. Review of EEG-based neurofeedback as a therapeutic intervention to treat depression. Psychiatry Res. 2023;329:111591. doi:10.1016/j.pscychresns.2023.111591. [Google Scholar] [PubMed] [CrossRef]
47. Kuiper N, Olinger L, Lyons L. Global perceived stress level as a moderator of the relationship between negative life events and depression. J Hum Stress. 1986;12(4):149–53. doi:10.1080/0097840X.1986.9936781. [Google Scholar] [PubMed] [CrossRef]
48. Pereira-Morales A, Adan A, Forero DA. Perceived stress as a mediator of the relationship between neuroticism and depression and anxiety symptoms. Curr Psychol. 2019;38(1):66–74. [Google Scholar]
49. Lesnewich L, Conway F, Buckman J, Brush C, Ehmann P, Eddie D, et al. Associations of depression severity with heart rate and heart rate variability in young adults across normative and clinical populations. Int J Psychophysiol. 2019;142:57–65. doi:10.1016/j.ijpsycho.2019.06.005. [Google Scholar] [PubMed] [CrossRef]
50. Jangpangi D, Mondal S, Bandhu R, Kataria D, Gandhi A. Alteration of heart rate variability in patients of depression. JCDR. 2016;10(12):CM04–6. doi:10.7860/JCDR/2016/22882.9063. [Google Scholar] [PubMed] [CrossRef]
51. Licht C, Geus E, Dyck R, Penninx B. Longitudinal evidence for unfavorable effects of antidepressants on heart rate variability. Biol Psychiatry. 2010;68(9):861–8. doi:10.1016/j.biopsych.2010.06.032. [Google Scholar] [PubMed] [CrossRef]
52. Kemp AH, Fraguas R, Brunoni AR, Bittencourt MS, Nunes MA, Dantas EM, et al. Differential associations of specific selective serotonin reuptake inhibitors with resting-state heart rate and heart rate variability: implications for health and well-being. Psychosom Med. 2016;78(7):810–8. doi:10.1097/PSY.0000000000000336. [Google Scholar] [PubMed] [CrossRef]
53. Carney RM, Blumenthal JA, Stein PK, Watkins L, Gatellier D, Berkman LF, et al. Depression, heart rate variability, and acute myocardial infarction. Circulation. 2001;104(17):2024–8. doi:10.1161/hc4201.097834. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools