 Open Access
Open Access
ARTICLE
Psychological Distress in the Association between Medical Education Changes and Clinical Learning Worry among Students Receiving Clinical Education during the COVID-19 Pandemic in Taiwan
1 Department of Nursing, College of Medicine, National Cheng Kung University, Tainan, 701401, Taiwan
2 Department of Public Health, College of Medicine, National Cheng Kung University, Tainan, 701401, Taiwan
3 Department of Internal Medicine, Section Nursing Science, Erasmus University Medical Center (Erasmus MC), Rotterdam, 3015 GD, The Netherlands
4 Division of Family Medicine, Taipei Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, New Taipei, 231405, Taiwan
5 School of Medicine, Tzu Chi University, Hualien, 231036, Taiwan
6 Data Science Degree Program, National Taiwan University and Academia Sinica, Taipei, 106319, Taiwan
7 Department of Occupational Therapy, College of Medicine, National Cheng Kung University, Tainan, 701401, Taiwan
8 Department of Medical Research, E-Da Hospital, I-Shou University, Kaohsiung, 824005, Taiwan
9 Department of Family Medicine and Community Medicine, E-Da Hospital, I-Shou University, Kaohsiung, 824005, Taiwan
10 School of Medicine, College of Medicine, I-Shou University, Kaohsiung, 824005, Taiwan
11 International Gaming Research Unit, Psychology Department, Nottingham Trent University, Nottingham, NG11 8NS, UK
12 Institute of Allied Health Sciences, College of Medicine, National Cheng Kung University, Tainan, 701401, Taiwan
13 Biostatistics Consulting Center, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 701401, Taiwan
* Corresponding Authors: Ming-Ta Hsieh. Email: ; Chung-Ying Lin. Email:
# These authors contributed equally to be the co-first authors
International Journal of Mental Health Promotion 2024, 26(12), 987-996. https://doi.org/10.32604/ijmhp.2024.057708
Received 26 August 2024; Accepted 15 November 2024; Issue published 31 December 2024
Abstract
Background: The COVID-19 pandemic profoundly impacted medical education and caused psychological distress and worry about clinical learning for those who received clinical medical education during this period. Although the acute phase of COVID-19 has now ended, understanding its impact is essential for strengthening medical system preparedness. Therefore, the present study examined the association between changes in medical education and worry about clinical learning, considering the mediating role of psychological distress among participants who received clinical training. Methods: A cross-sectional online survey was conducted with 542 post-graduate year (PGY) doctors and allied health students from the 2020 and 2021 cohorts in Taiwan. The survey assessed changes in clinical training modes, direct patient care, learning stress, psychological distress, and worry about clinical learning. Results: Among the participants, 76.0% experienced changes in clinical training mode, and 84.3% had direct patient care experience. Direct patient care/contact was significantly correlated with lower levels of worry about clinical learning. Learning stress was positively correlated with increased psychological distress and worry about clinical learning. Psychological distress partially mediated the relationship between learning stress and worry about clinical learning. Conclusion: The findings highlight the importance of direct contact with patients because it was associated with lower levels of worry about clinical learning. Moreover, increased learning stress was associated with psychological distress and worry about clinical learning. Therefore, effective support systems are essential to mitigate these impacts and enhance clinical training during national health crises. The findings provide valuable insights for improving medical education and support systems in future health emergencies. However, the present study used a cross-sectional study design. Therefore, the mediation findings should be interpreted with caution (i.e., no causal relationships can be determined based on cross-sectional data).Keywords
The COVID-19 pandemic profoundly affected health systems worldwide [1–3], primarily due to the overwhelming number of deaths and the subsequent strain on healthcare resources. As hospitals were overwhelmed by patients and lack of resources while working with limited knowledge of the new virus, the strain on medical education became evident. The pandemic exacerbated mental health issues across different populations, including frontline healthcare workers (HCWs; e.g., doctors and allied health professionals), who had to cope with inadequate protective equipment, fear of transmitting the virus to their families, and financial concerns [4,5].
For post-graduate year (PGY) doctors and allied health students, the situation was further compounded by decisions to suspend clinical duties to reduce infection risks. This led to a sudden transition to online learning, with virtual cases and simulated clinical environments becoming the main way to maintain educational continuity. Medical schools in northern Taiwan also took measures such as accelerating student graduations to address the urgent need for healthcare workers, reflecting the broader disruptions to medical training and the ongoing challenges within national health systems [6–8]. Although the World Health Organization [9] has now declared an end to the pandemic, lessons learned from the COVID-19 pandemic in medical training changes need to be documented so that authorities can be prepared for possible health epidemics in the future [10].
The COVID-19 pandemic drastically altered medical education, leading to heightened mental health challenges for medical students in the UK, USA, and Canada [11,12]. Even before the pandemic in Taiwan, symptoms of anxiety and depression were notably higher among PGY doctors and allied health students compared to the general population [13]. The abrupt reorganization of academic services exacerbated these issues, posing significant student challenges. Whether being on the frontline or being restricted from patient interactions, these students faced adverse psychological impacts. Clinical trainees such as PGY doctors and allied health students in countries such as America and Greece were particularly concerned about nosocomial infections, the risk of transmitting the virus to family members, and the frustrations of disrupted internships [14,15]. During the pandemic, HCWs involved in direct COVID-19 patient care were at higher risk for depression and anxiety, with inexperienced trainees feeling particularly stressed and uncomfortable [16,17]. These factors collectively underscore the urgent need for effective support systems to mitigate the psychological distress impacts on medical and allied health students during such unprecedented events.
Moreover, clinical rotations during the pandemic presented significant challenges for PGY doctors and allied health students, including providing patient care, integrating into the workplace, and confronting self-doubt [18]. Stress and anxiety during these rotations can impair clinical performance, reduce empathy, and negatively affect decision-making and patient relationships [19–21]. Prior studies conducted in the USA indicated that such stress is linked to decreased clinical practice and poor clinical outcomes [22,23]. Anxiety related to clinical practice can also diminish self-efficacy and negatively impact learning and performance in clinical skills [24–26].
As aforementioned, the pandemic led to major changes in medical education, most noticeably, the shift from in-person to online clinical training. Despite the benefits of online learning for medical students, it lacks hands-on training which is essential for developing clinical skills and reducing worry about clinical learning. The absence of in-person teaching and direct patient interactions can also impair students’ clinical competence and increase worry about clinical learning [27]. Some countries, such as Spain, allowed students to graduate early and work on the frontline during the pandemic [28]. However, despite their willingness, students may not have the confidence to engage in in-person medical care [29,30], which may be related to their lack of specific training [31]. Moreover, studies of previous infectious diseases have shown that knowledge and prior training can improve their attitudes and clinical learning [32,33].
In Taiwan (where the present study was carried out), the Ministry of Education initially implemented guidelines for medical and allied health student internships in response to infectious disease outbreaks in early 2020. Despite effective early control of COVID-19, a significant outbreak in May 2021 led to heightened alert levels and further adaptations in clinical training [34]. The shift to virtual and alternative learning methods prompted by the pandemic increased students’ concerns about clinical learning and medical skill acquisition. Social control measures, such as public health restrictions (e.g., social distancing), further compounded this by limiting in-person training and altering clinical experiences, introducing the challenge of maintaining educational quality while ensuring safety. There is a research gap in understanding how these changes in medical education and varying levels of social control influence the worry about clinical learning and consequent psychological distress among PGY doctors and allied health students. In addition, although numerous studies have examined the immediate impact of the COVID-19 pandemic on various aspects of medical students’ lives [11–15], there is a lack of research investigating the long-term effects on students’ psychological well-being and clinical confidence. Furthermore, the interplay between educational changes, distress, and worry in the context of a global health crisis remains unexplored. To better understand these relationships, the present study drew on Stress and Coping Theory [35], which provides a framework for exploring how changes in medical education (due to the effect of COVID-19) serve as external stressors, leading to emotional distress and influencing students’ cognitive appraisals, such as worry about clinical learning. Addressing these gaps is crucial because it will provide insights into the effectiveness of epidemic/pandemic-related educational adaptations and inform strategies for future health crises. Therefore, the present study aimed to (i) identify the association between changes in medical education and worry about clinical learning among PGY doctors and allied health students in Taiwan during the COVID-19 pandemic, (ii) evaluate the impact of social control, and (iii) assess the role of psychological distress as a mediating variable between learning stress and worry about clinical learning.
The study used a cross-sectional online survey (hosted on the SurveyMonkey platform) to collect data from Taiwanese PGY doctors and allied health students who received clinical practice at medical institutions between 2020 and 2021. The online surveys were completed anonymously, without requiring a name and account login when participants completed them. The corresponding authors of the present study sought assistance from their colleagues in charge of clinical training to distribute the survey link to potential target participants. The first page of the survey clearly stated the study information, including the eligibility to participate. The inclusion criteria were (i) being aged 18 years or older; (ii) receiving clinical training between 2020 and 2021; and (iii) being a student at Taiwan colleges or universities. The exclusion criteria were (i) being unwilling to provide e-consent for participation and (ii) self-reporting any mental health problems prior to the pandemic. Moreover, the present sample was not impacted by the student graduations acceleration because all the participants were in Southern Taiwan.
The sample included participants (PGY doctors and allied health students) from the 2020 and 2021 cohorts in Taiwan. The 2020 cohort experienced minimal COVID-19 disruption, while the 2021 cohort faced community spread and mixed virtual and physical clinical teaching in Taiwan. From the initial pool of 1037 participants who completed the survey, 542 met the inclusion criteria and were subsequently included in the study (Fig. 1). The survey procedures strictly adhered to ethical principles involving human participants and the Declaration of Helsinki. The National Cheng Kung University Human Research Ethics Committee approved the study protocol (Approval No. NCKU HREC-E-111-325-2) before the authors distributed the online survey. All participants provided their informed consent to take part in the study.
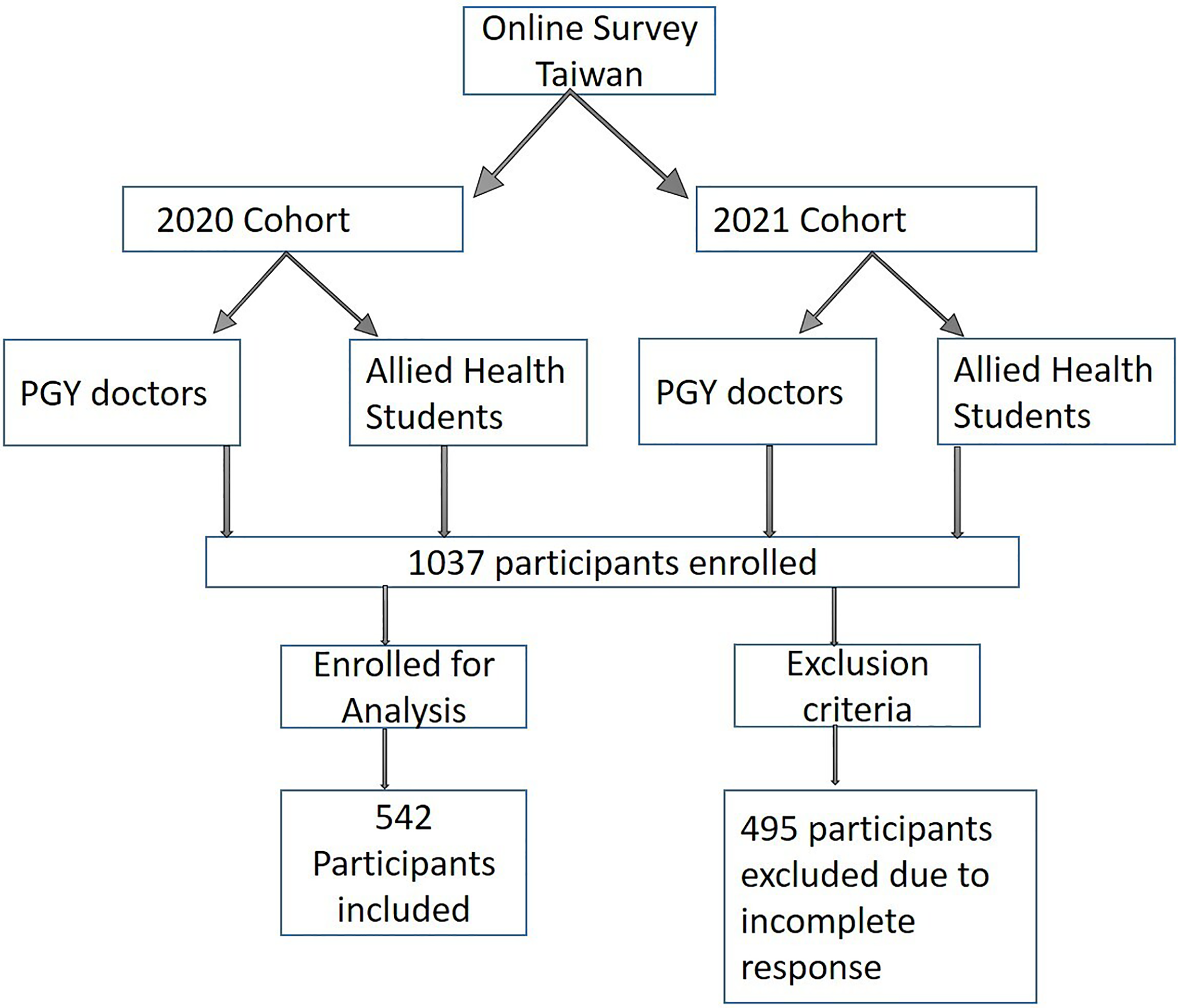
Figure 1: Flowchart illustrating participant numbers following inclusion and exclusion criteria.
A structured online survey was developed for the present study, comprising four sections: (I) demographic characteristics, (II) effects of the COVID-19 pandemic on medical students, (III) 21-item Depression, Anxiety and Stress Scale (DASS-21) Chinese version, and (IV) worry about clinical learning, which the study participants were asked to complete.
The demographic characteristics of the study participants were assessed, including gender, age, year of entering the clinical phase, and the presence of self-reported chronic physical illnesses (e.g., hypertension and diabetes) or psychological illnesses (e.g., depression and anxiety).
Effects of the COVID-19 pandemic on medical students
This section of the survey was based on a previously published study [36] and further modified to evaluate the impact of the COVID-19 pandemic on medical students’ experiences. It was divided into three sections: clinical training mode changed (one dichotomized item), direct patient contact during clinical practice (one dichotomized item), and changes in learning stress (two seven-point Likert items). These three indicators—clinical training mode changes, direct patient contact, and learning stress—collectively represent the ‘effect of COVID-19’ on medical education, as used in the present study’s models.
To assess changes in the learning mode, participants were asked if their clinical training was shortened, canceled, or converted to other forms (e.g., online) due to the COVID-19 pandemic (responded ‘yes’ or ‘no’). To evaluate direct patient contact, participants were asked if they had any direct patient care during PGY/clinical practice (responded ‘yes’ or ‘no’). To assess changes in learning stress, participants reported their learning stress levels focusing on emotional exhaustion, burnout, cynicism, and fatigue due to learning at two-time points (i.e., before the pandemic and during the pandemic) on a 7-point scale (1 = not at all, 4 = somewhat, 7 = extremely). The changes in learning stress were then computed by deducting the learning stress score during the pandemic from the learning stress before the pandemic.
Chinese version of the 21-item Depression, Anxiety, and Stress scale (DASS-21)
The Depression, Anxiety, and Stress Scale (DASS-21) is a 21-item self-report scale derived from the original 42-item version by Lovibond and Lovibond, designed to assess depression, anxiety, and stress [37]. Each subscale contains 7 items, assessing symptoms such as dysphoria, autonomic arousal, and chronic nonspecific arousal, respectively. Items are scored on a 4-point Likert scale, with higher scores indicating greater levels of distress. The present study used the Chinese version of the DASS-21, validated by Chen et al. [38], which reported good psychometric properties with an overall internal reliability of 0.93 and subscale reliabilities exceeding 0.80. Cao et al. [39,40], also reported good psychometric properties, with ωt and ωh values exceeding 0.80 across subscales. The full 21-item scale had good internal consistency in the present study (α = 0.950).
A self-developed 5-item scale was used to evaluate worry about clinical learning of PGY doctors and allied health students. The scale assessed concerns about clinical learning, including insufficient training, failing professional exams, inadequate future professional skills, the transition to online learning, and the lack of direct patient interaction. The scale ranged from 1 (not at all worried) to 5 (very worried). The total score was calculated by summing the responses, with higher scores indicating lower worry about clinical learning. The 5-item scale had good internal consistency in the present study (α = 0.869).
For content validity, the relevant literature was reviewed to identify potential items for assessing worry about clinical learning. Following this, an expert in public health screened and selected appropriate items, resulting in five items being retained. These were then evaluated by an expert panel (two physicians, two public health experts, two nursing experts, and one psychometrician).
In the present study, SPSS 17.0 was used to analyze the data, utilizing both descriptive and inferential statistics. Descriptive analysis focused on the distribution of demographic and other variables, describing categorical data by frequencies and percentages and continuous data by means and standard deviations. Inferential statistics included independent sample t-tests to explore differences in worry about clinical learning by gender (males vs. females), entry year (2020 vs. 2021), chronic physical illnesses (no vs. yes), and chronic psychological illnesses (no vs. yes). Additionally, mediation analysis using Hayes’ Process Macro (model 4) with 5000 bootstrapping samples examined the direct and indirect effects of changes in medical education on the worry about clinical learning, mediated by psychological distress, considering statistical significance at p < 0.05. Fig. 2 illustrates the three mediation models, where path c is referred to as the total effect, calculated as: cn = cn’ (direct effect) + an * bn (indirect effect). Moreover, multiple hierarchical regression was used to evaluate the influence of demographic and medical education changes on worry about clinical learning.
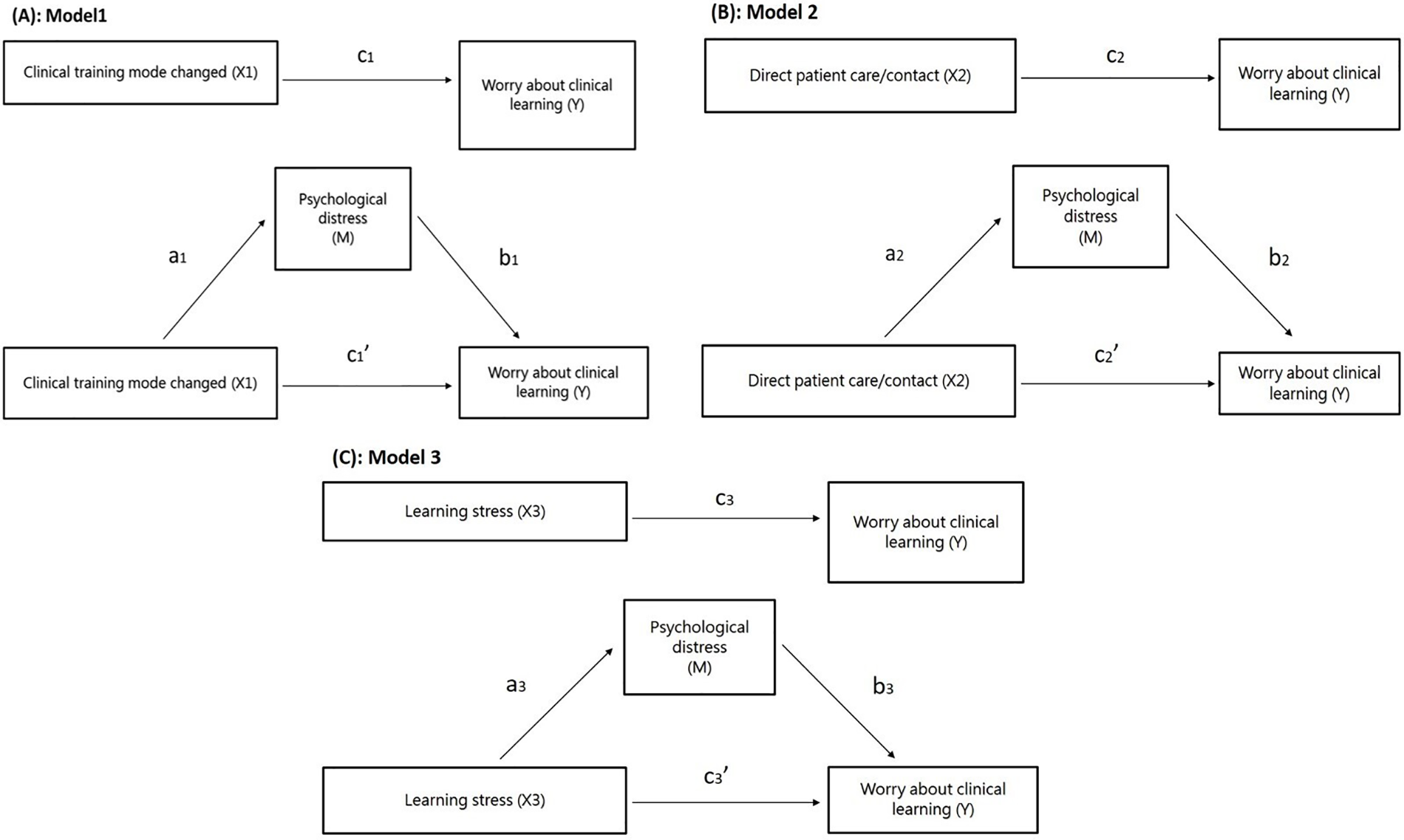
Figure 2: The present study’s conceptual framework for Model 1(A), Model 2(B), and Model 3(C).
Out of 542 participants, 343 (63.3%) belonged to the 2021 cohort. There were 348 female participants (64.2%); 32 self-reporting chronic physical conditions (5.9%) and 36 self-reporting chronic psychological conditions (6.6%) (Table 1). A total of 412 participants experienced a change in clinical training mode (76.0%), and 457 had direct patient care or contact experience (84.3%). The mean age of the participants was 24.47 years (SD = 3.59). The mean score on the DASS-21 was 9.47 (SD = 10.57), while the mean scores for learning stress and worry about clinical learning were 0.67 (SD = 1.21) and 14.25 (SD = 4.75), respectively.
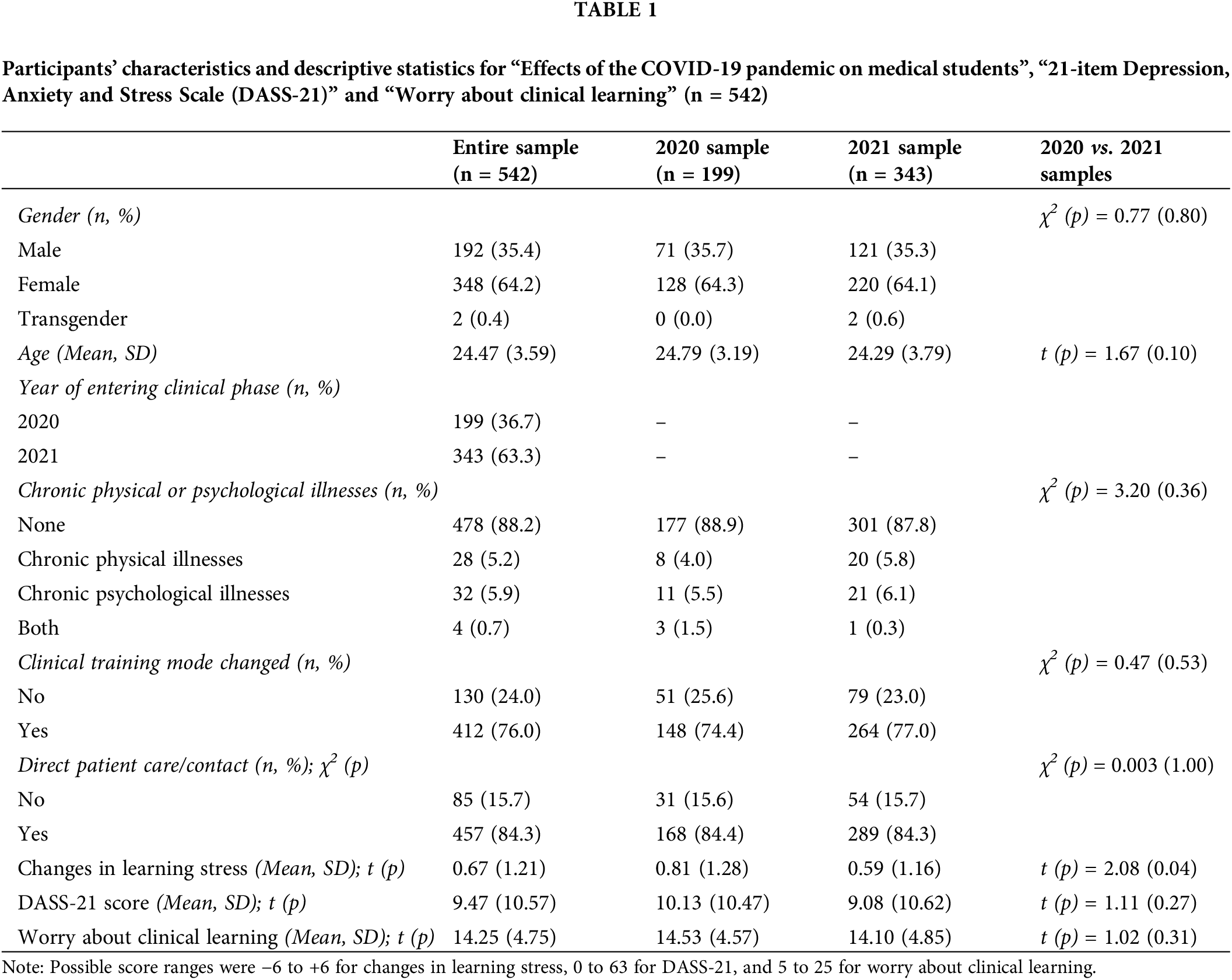
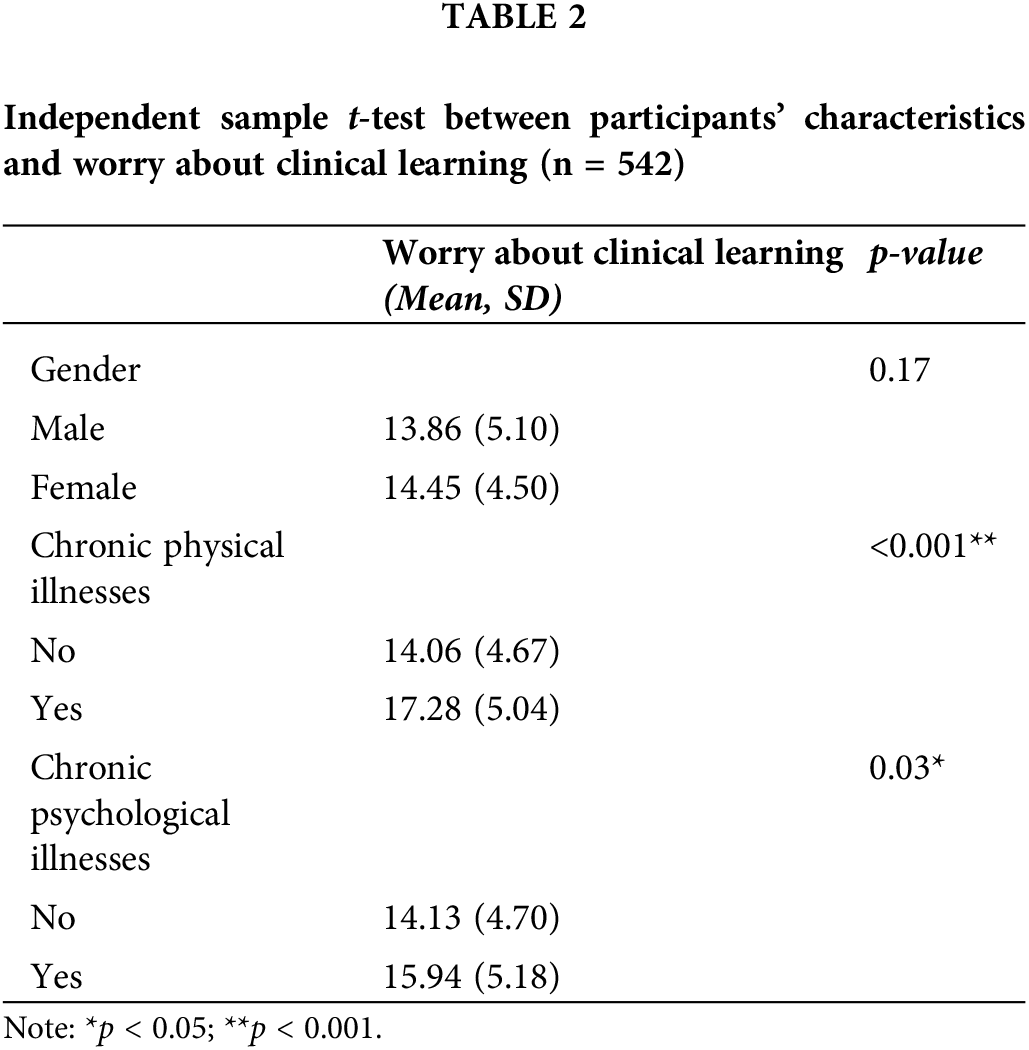
Table 2 shows that individuals with self-reported physical chronic illnesses had significantly higher worry about clinical learning than those without such conditions (p < 0.001); those who self-reported chronic psychological illnesses also had significantly higher worry about clinical learning than those without such conditions (p = 0.03). Moreover, there was no significant difference in worry about clinical learning based on gender or year of entering the clinical phase. The correlation analysis showed that age was not significantly correlated with worry about clinical learning.
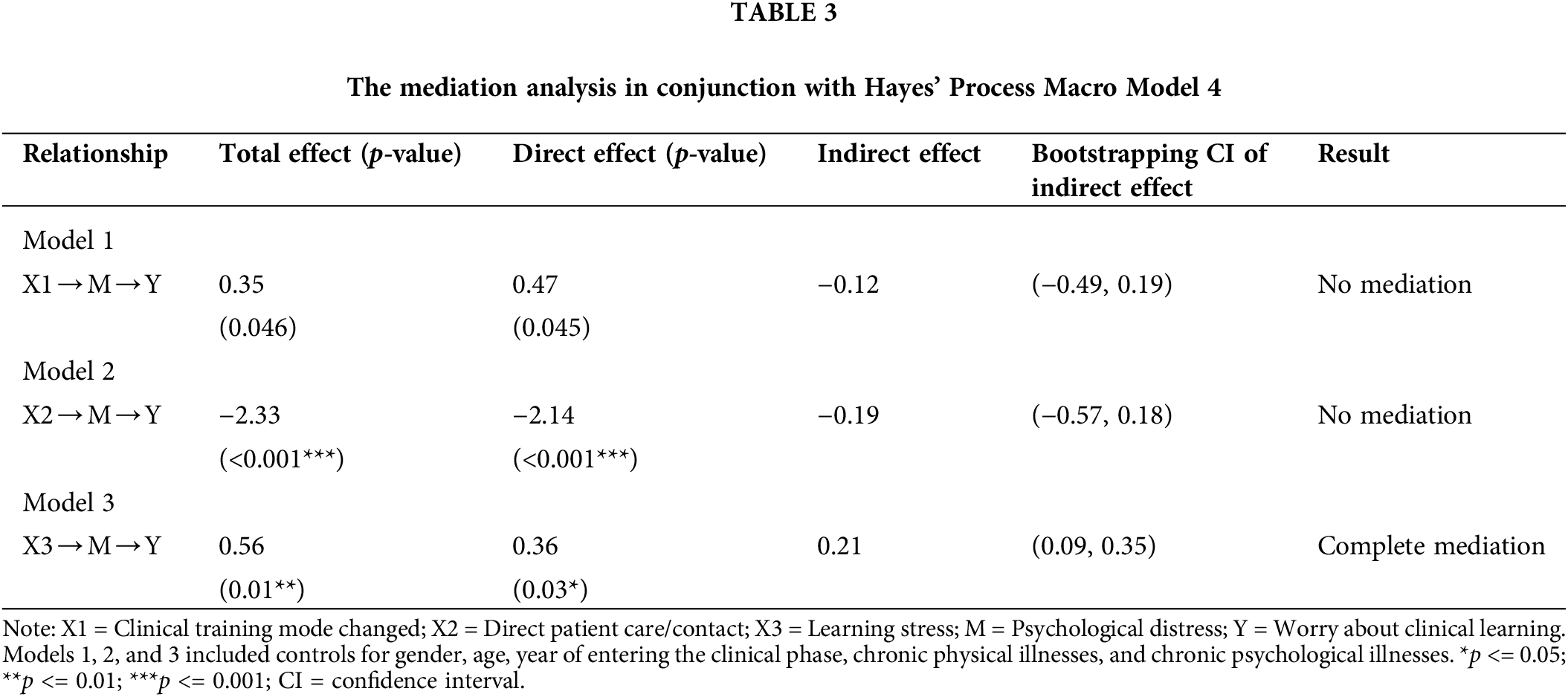
The analysis in Table 3 indicates that while the total effect of clinical training mode change on worry about clinical learning remained nonsignificant, direct patient care/contact had a significant direct effect on worry about clinical learning without mediation (p < 0.001). However, the effect of learning stress on worry about clinical learning was partially mediated by psychological distress, explaining approximately 38% of the total effect (95% CI: [0.09, 0.35]), indicating that increases in learning stress impacted worry about clinical learning directly and indirectly through its negative effect on psychological distress. Moreover, the direct effects (95% CI) were −0.87 (−2.87, 1.14) from clinical training mode changed to psychological distress; −1.37 (−3.74, 0.99) from direct patient care/contact to psychological distress; and 1.56 (0.86, 2.26) from learning stress to psychological distress. The direct effects (95% CI) were 0.14 (0.11, 0.18), 0.14 (0.10, 0.18), and 0.13 (0.10, 0.17) from psychological distress to worry about clinical learning.
Multiple hierarchical regression
Table 4 shows the results of the multiple hierarchical regression analysis. Model A in the multiple hierarchical regression analysis included demographic characteristics (gender, age, year of entering the clinical phase, and chronic physical and psychological illnesses), psychological distress, and clinical training mode change. The overall explanatory variance of these factors for worry about clinical learning was 14%. However, clinical training mode change did not contribute significantly to the explanation (β = 0.043, p = 0.29). Model B added direct patient care/contact, and this added factor showed a significant negative association with worry about clinical learning (β = −0.169, p < 0.001). Although the regression coefficient for the change in clinical training mode slightly increased, it remained nonsignificant (β = 0.056, p = 0.16). The overall explanatory variance increased to 17%.
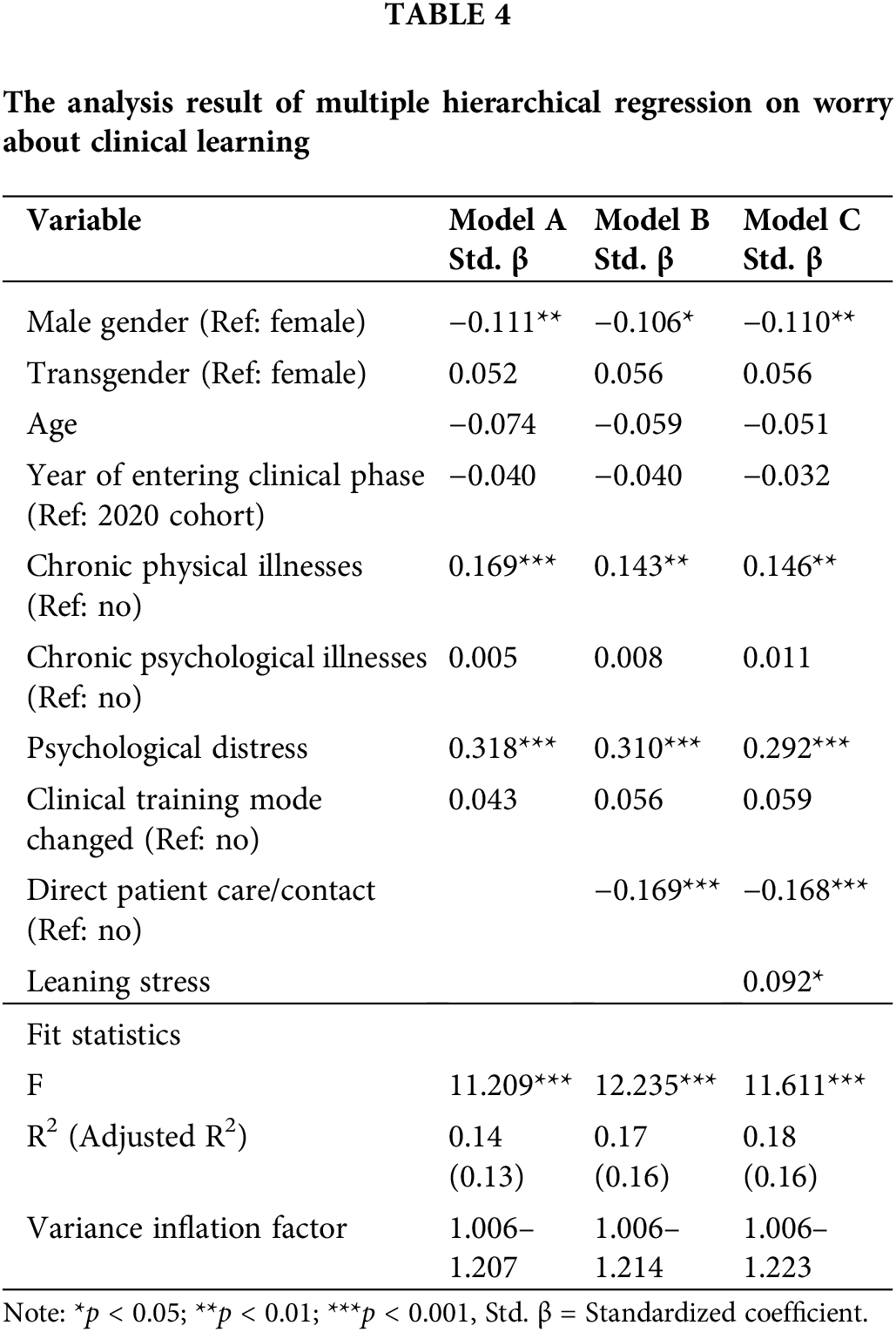
Finally, Model C added learning stress in the regression, and learning stress was significantly associated with worry about clinical learning (β = 0.092, p = 0.02). The regression coefficient for the change in clinical training mode resulted in another slight increase but remained non-significant (β = 0.059, p = 0.14). The association between direct patient care/contact and worry about clinical learning remained similar (β = −0.168, p < 0.001), and the overall explanatory variance slightly increased to 18%.
The present study sought to identify the association between changes in clinical training mode and worry about clinical learning among PGY doctors and allied health students in Taiwan during the COVID-19 pandemic, and assess the role of psychological distress as a mediating variable between learning stress and worry about clinical learning. The findings showed several important insights into how these factors interact and are associated with worry about clinical learning. A notable finding was the significant impact of direct patient care/contact on worry about clinical learning. Participants who had direct patient care/contact during their clinical training exhibited less worry about clinical learning, consistent with the previous research emphasizing the irreplaceable value of practical patient care experiences in medical education [41–43].
These experiences are pivotal for the professional development of students because they provide essential hands-on learning and feedback from patients and instructors, thereby decreasing their worry about clinical learning and enhancing their in-person clinical skills [31]. This aligns with a study conducted by Ho et al. [44], which showed that the arrival of emerging infectious diseases in Taiwan decreased patient visits, reducing opportunities for medical practitioners and students to engage in patient interactions. Hassan et al. highlighted that virtual patients were not sufficient in compensating for the experiential learning provided by actual physical examinations [45].
Moreover, the present study’s findings demonstrated no significant correlation between direct patient care/contact and psychological distress. However, given the cross-sectional, survey-based design, it is important to note that this reflects only a snapshot in time and does not capture longitudinal changes in psychological distress. Consequently, the mediation findings should be interpreted with caution. This may also be attributed to Taiwan’s medical education system’s efforts to maintain the integrity of clinical training in a safe learning environment despite the pandemic. Moreover, public health measures and the discouragement of non-essential patient visits may have limited the cumulative experience gained by students [46]. During the COVID-19 pandemic, technological advancements in Taiwan, such as video calls for teleconsultations, allowed students to capture details such as real facial expressions and tone of voice from actual patients, thereby supplementing the lack of doctor-patient interaction in simulated teaching. This approach sought to alleviate students’ concerns and anxieties regarding their future practice. As indicated by Zweigenthal et al., medical students in South Africa enhanced their skills and confidence in doctor-patient communication through telephone interactions and caring for COVID-19 patients [47].
The present study additionally highlighted the mediating role of psychological distress in the relationship between learning stress and worry about clinical learning. Increased learning stress correlated with increased worry about clinical learning, with part of this correlation explained through the mediating effect of psychological distress. This finding aligns with previous research showing that factors contributing to increased learning stress during the COVID-19 pandemic (such as the substitution and adaptation of online teaching [48–50], enforcement of public health policies, and changes in social networks [51]) can lead to an increase in worry about clinical learning and poorer mental health conditions [52]. Previous studies also suggested that symptoms of depression and anxiety negatively impacted medical self-efficacy and confidence [24,53], which may explain the mediating effect of psychological distress between learning stress and worry about clinical learning.
In the present study, several limitations need to be acknowledged. Firstly, being a cross-sectional study, causal relationships cannot be confirmed even if correlations among variables were observed. Secondly, the retrospective survey method employed in the present study relied on participants’ memory, introducing the possibility of recall bias and potentially compromising the accuracy of the results. Lastly, the survey was conducted through an online platform, possibly biased towards individuals who are users of online platforms. This exclusion of those lacking digital technology resources might overlook individuals facing challenges in the digital learning process, highlighting a limitation in capturing the complete spectrum of experiences.
The present study found that the increased learning stress due to the pandemic was associated with increased psychological distress of medical students, further amplifying the worry about clinical learning. The present study suggested that the COVID-19 pandemic necessitated immediate changes to the clinical training programs for medical students in Taiwan. These changes included alternative teaching methods within restricted environments and reduced clinical practice experiences, which appear to have increased learning stress. Simultaneously, the study demonstrated that interactions with real patients appeared to have significantly helped students reduce their worry about executing clinical tasks. In conclusion, the present study provides novel insights into the impact of the COVID-19 pandemic on medical education in Taiwan. The findings not only aid educational institutions in better navigating similar situations but also establish a rich foundation for future research to further explore the long-term effects of learning environments and mental health on worry about clinical learning.
Acknowledgement: We thank all participants who participated in the present study.
Funding Statement: This research was supported in part by (received funding from) the National Science and Technology Council, Taiwan (NSTC 113-2321-B-006-007) and the E-Da Hospital (EDAHS113037).
Author Contributions: The authors confirm their contribution to the paper as follows: study conception and design: Shikha Kukreti, Min-Chi Hsieh, Ming-Ta Hsieh, Chung-Ying Lin, Nai-Ying Ko; data collection: Min-Chi Hsieh, Ru-Yi Huang, Carol Strong, Jung-Sheng Chen, Ming-Ta Hsieh, Chung-Ying Lin; analysis and interpretation of results: Shikha Kukreti, Min-Chi Hsieh, Musheer A. Aljaberi, I-Ting Hwang, Ming-Ta Hsieh, Mark D. Griffiths, Chung-Ying Lin; draft manuscript preparation: Shikha Kukreti, Min-Chi Hsieh, Ming-Ta Hsieh, Chung-Ying Lin; critically review and edit manuscript: Musheer A. Aljaberi, Ru-Yi Huang, I-Ting Hwang, Carol Strong, Jung-Sheng Chen, Mark D. Griffiths, Chung-Ying Lin, Nai-Ying Ko. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The dataset supporting the present study’s findings are available from the corresponding author upon reasonable request.
Ethics Approval: The survey procedures strictly adhered to ethical principles involving human participants and the Declaration of Helsinki. The National Cheng Kung University Human Research Ethics Committee approved the study protocol (Approval No. NCKU HREC-E-111-325-2) before the authors distributed the online survey. All participantsprovided their informed consent to take part in the study.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives. Best Pract Res Clin Anaesthesiol. 2021;35(3):293–306. doi:10.1016/j.bpa.2020.11.009. [Google Scholar] [PubMed] [CrossRef]
2. Prasetyo YB, Faridi F, Masruroh NL, Melizza N, Kurnia AD, Wardojo SSI, et al. Path analysis of the relationship between religious coping, spiritual well-being, and family resilience in dealing with the COVID-19 pandemic in Indonesia. Asi J Soc Health Behav. 2024;7(1):1–10. doi:10.4103/shb.shb_375_23. [Google Scholar] [CrossRef]
3. Aljaberi MA, Al-Sharafi MA, Uzir MU, Sabah A, Ali AM, Lee K-H, et al. Psychological toll of the COVID-19 pandemic: an in-depth exploration of anxiety, depression, and insomnia and the influence of quarantine measures on daily life. Healthcare. 2023;11(17):2418. doi:10.3390/healthcare11172418. [Google Scholar] [PubMed] [CrossRef]
4. Gupta S, Sahoo S. Pandemic and mental health of the front-line healthcare workers: a review and implications in the Indian context amidst COVID-19. Gen Psychiat. 2020;33(5):e100284. doi:10.1136/gpsych-2020-100284. [Google Scholar] [PubMed] [CrossRef]
5. Aljaberi MA, Alareqe NA, Alsalahi A, Qasem MA, Noman S, Uzir MUH, et al. A cross-sectional study on the impact of the COVID-19 pandemic on psychological outcomes: multiple indicators and multiple causes modeling. PLoS One. 2022;17(11):e0277368. doi:10.1371/journal.pone.0277368. [Google Scholar] [PubMed] [CrossRef]
6. Lai CW. Reflections on medical education in Taiwan brought about by SARS in 2003. udn News. 2020 (In Chinese). Available from: https://health.udn.com/health/story/6631/4421448. [Accessed 2024]. [Google Scholar]
7. Chou HH. New thinking in medical education. Chang Gung Medical News. 2015 (In Chinese). Available from: https://www.cgmh.org.tw/cgmn/category.asp?id_seq=1502001. [Accessed 2024]. [Google Scholar]
8. Chi JJ, Guo WX, Du YT. The Chairman of Taiwan Medical Accreditation Council, Shang-Chun, Chang: higher education innovation does not forget to strengthen the foundation of the whole population to face the challenge of epidemic prevention. 2020 (In Chinese). Available from: https://www.heeact.edu.tw/1151/1165/43078/43083/43106/44292/. [Accessed 2024]. [Google Scholar]
9. Rigby J, Satija B. WHO declares end to COVID global health emergency. London, UK: Reuters; 2023 May 8. Available from: https://www.reuters.com/business/healthcare-pharmaceuticals/covid-is-no-longer-global-health-emergency-who-2023-05-05/. [Accessed 2024]. [Google Scholar]
10. Shrivastava SR, Bobhate PS, Mendhe HG, Badge A. Training medical students in pandemic preparedness: a systematic review. Asian J Soc Health Behav. 2024;7(2):55–9. [Google Scholar]
11. Kaul V, de Moraes AG, Khateeb D, Greenstein Y, Winter G, Chae J, et al. Medical education during the COVID-19 pandemic. Chest. 2021;159(5):1949–60. doi:10.1016/j.chest.2020.12.026. [Google Scholar] [PubMed] [CrossRef]
12. Abiddine FZE, Aljaberi MA, Gadelrab HF, Lin C-Y, Muhammed A. Mediated effects of insomnia in the association between problematic social media use and subjective well-being among university students during COVID-19 pandemic. Sleep Epidemiol. 2022;2:100030. doi:10.1016/j.sleepe.2022.100030. [Google Scholar] [PubMed] [CrossRef]
13. Huang P-C, Lin C-Y, Huang R-Y, Chen J-S, Potenza MN, Strong C, et al. Impact of COVID-19-induced academic stress on insomnia and suicidal ideation among Taiwanese health trainees and junior doctors. Med Sci Monit. 2024;30:e944932. doi:10.12659/MSM.944932. [Google Scholar] [PubMed] [CrossRef]
14. Alvin MD, George E, Deng F, Warhadpande S, Lee SI. The impact of COVID-19 on radiology trainees. Radiology. 2020;296(2):246–8. doi:10.1148/radiol.2020201222. [Google Scholar] [PubMed] [CrossRef]
15. Eleftheriou A, Rokou A, Arvaniti A, Nena E, Steiropoulos P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front Public Health. 2021;9:775374. doi:10.3389/fpubh.2021.775374. [Google Scholar] [PubMed] [CrossRef]
16. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi:10.1001/jamanetworkopen.2020.3976. [Google Scholar] [PubMed] [CrossRef]
17. Aljaberi MA, Lee K-H, Alareqe NA, Qasem MA, Alsalahi A, Abdallah AM, et al. Rasch modeling and multilevel confirmatory factor analysis for the usability of the Impact of Event Scale-Revised (IES-R) during the COVID-19 pandemic. Healthcare. 2022;10(10):1858. doi:10.3390/healthcare10101858. [Google Scholar] [PubMed] [CrossRef]
18. Mandan J, Sidhu HS, Mahmood A. Should a clinical rotation in hematology be mandatory for undergraduate medical students? Adv Med Educ Pract. 2016;7:519–21. doi:10.2147/AMEP. [Google Scholar] [CrossRef]
19. Kim KH. Baccalaureate nursing students’ experiences of anxiety producing situations in the clinical setting. Contemp Nurse. 2003;14(2):145–55. doi:10.5172/conu.14.2.145. [Google Scholar] [PubMed] [CrossRef]
20. Melincavage SM. Student nurses’ experiences of anxiety in the clinical setting. Nurse Educ Today. 2011;31(8):785–9. doi:10.1016/j.nedt.2011.05.007. [Google Scholar] [PubMed] [CrossRef]
21. Abdulghani HM, Al-Drees AA, Khalil MS, Ahmad F, Ponnamperuma GG, Amin Z. What factors determine academic achievement in high achieving undergraduate medical students? A qualitative study. Med Teach. 2014;36:S43–8. doi:10.3109/0142159X.2014.886011. [Google Scholar] [PubMed] [CrossRef]
22. Hammen C. Stress and depression. Annu Rev Clin Psychol. 2005;1(1):293–319. doi:10.1146/annurev.clinpsy.1.102803.143938. [Google Scholar] [PubMed] [CrossRef]
23. Silverstein ST, Kritz-Silverstein D. A longitudinal study of stress in first-year dental students. J Dent Educ. 2010;74(8):836–48. doi:10.1002/jdd.v74.8. [Google Scholar] [CrossRef]
24. Ding Y, Huang L, Feng C, Yang M, Zhang Y. Depression and self-efficacy in medical residents. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2017;42(1):83–7 (In Chinese). [Google Scholar] [PubMed]
25. Xiong H, Yi S, Lin Y. The psychological status and self-efficacy of nurses during COVID-19 outbreak: a cross-sectional survey. Inquiry. 2020;57:0046958020957114. doi:10.1177/0046958020957114. [Google Scholar] [PubMed] [CrossRef]
26. Vizheh M, Qorbani M, Arzaghi SM, Muhidin S, Javanmard Z, Esmaeili M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. 2020;19:1967–78. doi:10.1007/s40200-020-00643-9. [Google Scholar] [PubMed] [CrossRef]
27. Wilcha R-J. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020;6(2):e20963. doi:10.2196/20963. [Google Scholar] [PubMed] [CrossRef]
28. Legido-Quigley H, Mateos-García JT, Campos VR, Gea-Sánchez M, Muntaner C, McKee M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health. 2020;5(5):e251–2. doi:10.1016/S2468-2667(20)30060-8. [Google Scholar] [PubMed] [CrossRef]
29. Cervera-Gasch Á, González-Chordá VM, Mena-Tudela D. COVID-19: are Spanish medicine and nursing students prepared? Nurse Educ Today. 2020;92:104473. doi:10.1016/j.nedt.2020.104473. [Google Scholar] [PubMed] [CrossRef]
30. Swift A, Banks L, Baleswaran A, Cooke N, Little C, McGrath L, et al. COVID-19 and student nurses: a view from England. J Clin Nurs. 2020;29(17–18):3111. [Google Scholar] [PubMed]
31. Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: a systematic review. In Vivo. 2020;34(3 suppl):1603–11. doi:10.21873/invivo.11950. [Google Scholar] [PubMed] [CrossRef]
32. Chilton JM, McNeill C, Alfred D. Survey of nursing students’ self-reported knowledge of Ebola virus disease, willingness to treat, and perceptions of their duty to treat. J Prof Nurs. 2016;32(6):487–93. doi:10.1016/j.profnurs.2016.05.004. [Google Scholar] [PubMed] [CrossRef]
33. Patel R, Wattamwar K, Kanduri J, Nahass M, Yoon J, Oh J, et al. Health care student knowledge and willingness to work in infectious disease outbreaks. Disaster Med Public Health Prep. 2017;11(6):694–700. doi:10.1017/dmp.2017.18. [Google Scholar] [PubMed] [CrossRef]
34. Kukreti S, Padmalatha S, Fu S-H, Chen Y-C. Response to the COVID-19 pandemic in Taiwan. In: Global perspectives of COVID-19 pandemic on health, education, and role of media. Singapore: Springer Nature; 2023. p. 497–511. [Google Scholar]
35. Biggs A, Brough P, Drummond S. Lazarus and Folkman’s psychological stress and coping theory. In: The handbook of stress and health: a guide to research and practice. 2017 Apr 19. p. 349–64. [Google Scholar]
36. Harries AJ, Lee C, Jones L, Rodriguez RM, Davis JA, Boysen-Osborn M, et al. Effects of the COVID-19 pandemic on medical students: a multicenter quantitative study. BMC Med Educ. 2021;21:1–8. [Google Scholar]
37. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–43. doi:10.1016/0005-7967(94)00075-U. [Google Scholar] [PubMed] [CrossRef]
38. Chen I-H, Chen C-Y, Liao X-L, Chen X-M, Zheng X, Tsai Y-C, et al. Psychometric properties of the Depression, Anxiety, and Stress Scale (DASS-21) among different Chinese populations: a cross-sectional and longitudinal analysis. Acta Psychol. 2023;240:104042. doi:10.1016/j.actpsy.2023.104042. [Google Scholar] [PubMed] [CrossRef]
39. Cao C-H, Liao X-L, Gamble JH, Li L-l, Jiang X-Y, Li X-D, et al. Evaluating the psychometric properties of the Chinese Depression Anxiety Stress Scale for Youth (DASS-Y) and DASS-21. Child Adolesc Psychiatr Ment Health. 2023;17(1):106. doi:10.1186/s13034-023-00655-2. [Google Scholar] [PubMed] [CrossRef]
40. Cao C-H, Liao X-L, Jiang X-Y, Li X-D, Chen I-H, Lin C-Y. Psychometric evaluation of the Depression, Anxiety, and Stress Scale-21 (DASS-21) among Chinese primary and middle school teachers. BMC Psychol. 2023;11(1):209. doi:10.1186/s40359-023-01242-y. [Google Scholar] [PubMed] [CrossRef]
41. Wong FKY, Liu H, Wang H, Anderson D, Seib C, Molasiotis A. Global nursing issues and development: analysis of World Health Organization documents. J Nurs Scholarsh. 2015;47(6):574–83. doi:10.1111/jnu.2015.47.issue-6. [Google Scholar] [CrossRef]
42. Barr J, Graffeo CS. Procedural experience and confidence among graduating medical students. J Surg Educ. 2016;73(3):466–73. doi:10.1016/j.jsurg.2015.11.014. [Google Scholar] [PubMed] [CrossRef]
43. Panduragan SL, Abdullah N, Hassan H, Mat S. Level of confidence among nursing students in the clinical setting. Procedia Soc Behav Sci. 2011;18:404–7. doi:10.1016/j.sbspro.2011.05.059. [Google Scholar] [CrossRef]
44. Ho SW, Tasi MC, Huang CY. Qualitative study on the online virtual clinical training during the COVID-19 pandemic. J Taiwan Simul Soc Healthcare. 2020;7(2):4–13 (In Chinese). [Google Scholar]
45. Hassan AB, El-Agroudy A, Shehata MH, Almoawda MA, Atwa HS. Adaptations of clinical teaching during the COVID-19 pandemic: perspectives of medical students and faculty members. Adv Med Educ Pract. 2022;13:883. doi:10.2147/AMEP.S371201. [Google Scholar] [PubMed] [CrossRef]
46. Yu PL, Tsai TC. The paradigm shift of telemedicine under COVID-19 pandemic: the impact of digital technology. J Taiwan Simul Soc Healthcare. 2021;8(1):38–48 (In Chinese). [Google Scholar]
47. Zweigenthal V, Perez G, Wolmarans K, Olckers L. Health Sciences students’ experience of COVID-19 case management and contact tracing in Cape Town, South Africa. BMC Med Educ. 2023;23(1):238. doi:10.1186/s12909-023-04205-4. [Google Scholar] [PubMed] [CrossRef]
48. Zhang J-Y, Shu T, Xiang M, Feng Z-C. Learning burnout: evaluating the role of social support in medical students. Front Psychol. 2021;12:625506. doi:10.3389/fpsyg.2021.625506. [Google Scholar] [PubMed] [CrossRef]
49. Zagury-Orly I, Durning SJ. Assessing open-book examination in medical education: the time is now. Med Teach. 2021;43(8):972–3. doi:10.1080/0142159X.2020.1811214. [Google Scholar] [PubMed] [CrossRef]
50. Dewart G, Corcoran L, Thirsk L, Petrovic K. Nursing education in a pandemic: academic challenges in response to COVID-19. Nurse Educ Today. 2020;92:104471. doi:10.1016/j.nedt.2020.104471. [Google Scholar] [PubMed] [CrossRef]
51. Vala NH, Vachhani MV, Sorani AM. Study of anxiety, stress, and depression level among medical students during COVID-19 pandemic phase in Jamnagar city. Natl J Physiol Pharm Pharmacol. 2020;10(12):1043–5. [Google Scholar]
52. Tariq EF, Sah PK, Malik A. The plight of COVID-19 pandemic on medical students and residency applicants. Ann Med Surg. 2020;60:1–4. doi:10.1016/j.amsu.2020.10.010. [Google Scholar] [PubMed] [CrossRef]
53. Calisi CC. The effects of the relaxation response on nurses’ level of anxiety, depression, well-being, work-related stress, and confidence to teach patients. J Holist Nurs. 2017;35(4):318–27. doi:10.1177/0898010117719207. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools