 Open Access
Open Access
ARTICLE
The Relationship between Depression and Negative Cognitive Bias in Late Pregnancy Women and Its Influencing Factors
1 Department of Maternal, Child and Adolescent Health, School of Public Health, Anhui Medical University, Hefei, 230032, China
2 Department of Anhui Provincial Key Laboratory of Population Health and Aristogenics, Anhui Medical University, Hefei, 230032, China
3 Department of Patient Service Center, The People’s Hospital of Yingshang, Fuyang, 236200, China
* Corresponding Author: Jiahu Hao. Email:
(This article belongs to the Special Issue: Exploring anxiety, stress, depression, addictions, executive functions, mental health, and other psychological and socio-emotional variables: psychological well-being and suicide prevention perspectives)
International Journal of Mental Health Promotion 2024, 26(12), 1009-1016. https://doi.org/10.32604/ijmhp.2024.056235
Received 17 July 2024; Accepted 24 October 2024; Issue published 31 December 2024
Abstract
Objective: In recent years, psychological problems in pregnant women have become an important public health problem. Depression is a common psychological problem during pregnancy. At present, most studies focus on prenatal depression in pregnant women, and there is a lack of relevant studies on prenatal negative cognition and its relationship with depression. This study aims to examine the relationship between depression and negative cognitive bias in women in late pregnancy and identify the influencing factors. Methods: A total of 829 women in late pregnancy were recruited from a tertiary hospital between April 2023 and October 2023. The survey included the General Information Questionnaire for Women in Late Pregnancy, the Negative Cognitive Processing Bias Scale, and the Edinburgh Postpartum Depression Scale. Descriptive statistics and the χ2 test were employed for univariate analysis of depression among these women. Pearson correlation analysis assessed the relationship between depression scores and negative cognitive bias scores. Multiple linear regression analysis, with depression as the dependent variable, was used to identify the influencing factors of depression in late pregnancy. Results: The detection rate of depression was 26.3%. Planned pregnancy emerged as a protective factor against depression in the third trimester (OR = 0.481). Conversely, negative life events during pregnancy and negative memory bias were identified as significant risk factors (OR = 2.880, 1.146). Conclusion: The prevalence of depression in the third trimester is notably high, with pronounced negative memory bias. Healthcare providers should prioritize the mental health of pregnant women, particularly those with deep and repetitive recollections of negative events, by enhancing psychological monitoring and treatment.Keywords
Depression, a prevalent psychological disorder, ranks as the second-largest global health issue [1]. Prenatal depression lacks a unified definition. However, based on DSM-5 diagnostic criteria, researchers [2] described it as a persistent low mood, inability to adjust to pregnancy-induced changes, feelings of loneliness and isolation, and loss of social functioning, with symptoms persisting for more than two weeks. Reports on the incidence of prenatal depression in China vary widely, ranging from 7% to 36.8% [3,4].
Negative cognitive bias, characterized by a predisposition to focus on, remember, and interpret information negatively, comprises four components: negative attentional bias, negative memory bias, negative interpretational bias, and negative rumination bias [5,6]. This cognitive trait has garnered substantial attention in psychology research globally. Domestic scholars have extensively explored the causes, effects, and intervention strategies of negative cognition [7]. Studies have examined its relationship with mental health issues such as depression and anxiety disorders, finding that negative cognition is a core feature of these conditions, adversely affecting emotions, behavior, and physiological health [8,9]. This study aims to investigate the relationship between depression and negative cognitive bias in women during late pregnancy and analyze the influencing factors. The objective is to assist healthcare professionals in identifying high-risk groups for negative psychological states during late pregnancy, thereby promoting maternal and infant health.
The study involved 829 pregnant women who attended prenatal examinations at the obstetrics outpatient department from April 2023 to October 2023. Following informed consent, participants completed a questionnaire survey. Inclusion criteria included: ① informed consent; ② gestational age ≥28 weeks; and ③ singleton pregnancy. Exclusion criteria comprised: ① inability to cooperate; ② known history of mental illness or severe physical disease; and ③ multiple pregnancies. A total of 900 questionnaires, encompassing the General Information Questionnaire for Women in Late Pregnancy, Edinburgh Postnatal Depression Scale (EPDS), and Negative Cognitive Processing Bias Questionnaire (NCPBQ), were distributed. After excluding invalid and inconsistent responses, 829 valid questionnaires were retained, resulting in an effective response rate of 92.1%. The study has been approved by the Medical Ethics Committee of Yingshang County People’s Hospital Clinical research subject approval Medical ethics Review document (IRB number 2024-10). Written consent was acquired from the participants.
General information questionnaire
A General Information Questionnaire for Women in Late Pregnancy was developed after a comprehensive review of relevant literature [2–4] and an analysis of epidemiological factors influencing depression during pregnancy. The primary variables assessed include age, pregnancy and childbirth status, educational level, occupation, spouse’s educational level, pregnancy knowledge acquisition, negative life events, adverse obstetric history, planned pregnancy, prenatal exercise habits, monthly per capita household income, expectations regarding fetal gender, marital relationship, relationship with mother-in-law, dietary habits, and presence of complications.
The EPDS is extensively used to evaluate the severity of postpartum depression symptoms and has been proven effective in screening for prenatal depression [10]. The scale comprises 10 items categorized into three sections: emotional absence, anxiety, and depression. Each item is rated on a 4-point scale (0 to 3) based on symptom severity, with total scores ranging from 0 to 30. Higher scores denote more severe depression. In China, the EPDS was revised by Guo et al. in 2009 [11], achieving a Cronbach’s alpha coefficient of 0.76. This version is widely adopted in clinical practice and research for assessing depression in the perinatal population. In this study, a total score of ≥10 was considered indicative of a positive depression screening, suggesting a depressive state.
Feng et al. [12,13] identified negative cognitive processing bias as a cognitive trait, characterized by a preference for processing negative information. This encompasses four dimensions: negative attention bias, negative memory bias, negative interpretation bias, and negative rumination bias. The reliability analysis of the questionnaire demonstrated a Cronbach’s alpha coefficient of 0.893 and a split-half reliability coefficient of 0.866. The NCPBQ comprises 24 items: 6 items assess negative memory bias (score range: 6–24), and 5 items each measure the other three dimensions (score range: 5–20 each). Additionally, 2 lie-detection items and 1 self-evaluation item for response attitude are included. The total score for the scale ranges from 24 to 96, with higher scores indicating more severe negative cognitive processing bias.
Data were entered into an Excel database and meticulously verified. Statistical analysis was conducted using SPSS 26.0 software. The employed statistical methods included descriptive analysis, chi-square (χ2) test, t-test, and binary logistic regression for multivariate analysis. Odds ratios (OR) and 95% confidence intervals (95% CI) were calculated, with a p-value < 0.05 considered statistically significant.
Prior to the survey, obstetric nurses and two questionnaire administrators received training. The survey was administered using a one-on-one approach, allowing administrators to provide immediate clarification for any participant inquiries. Questionnaires were collected on-site, reviewed for accuracy, and then entered into an Excel sheet.
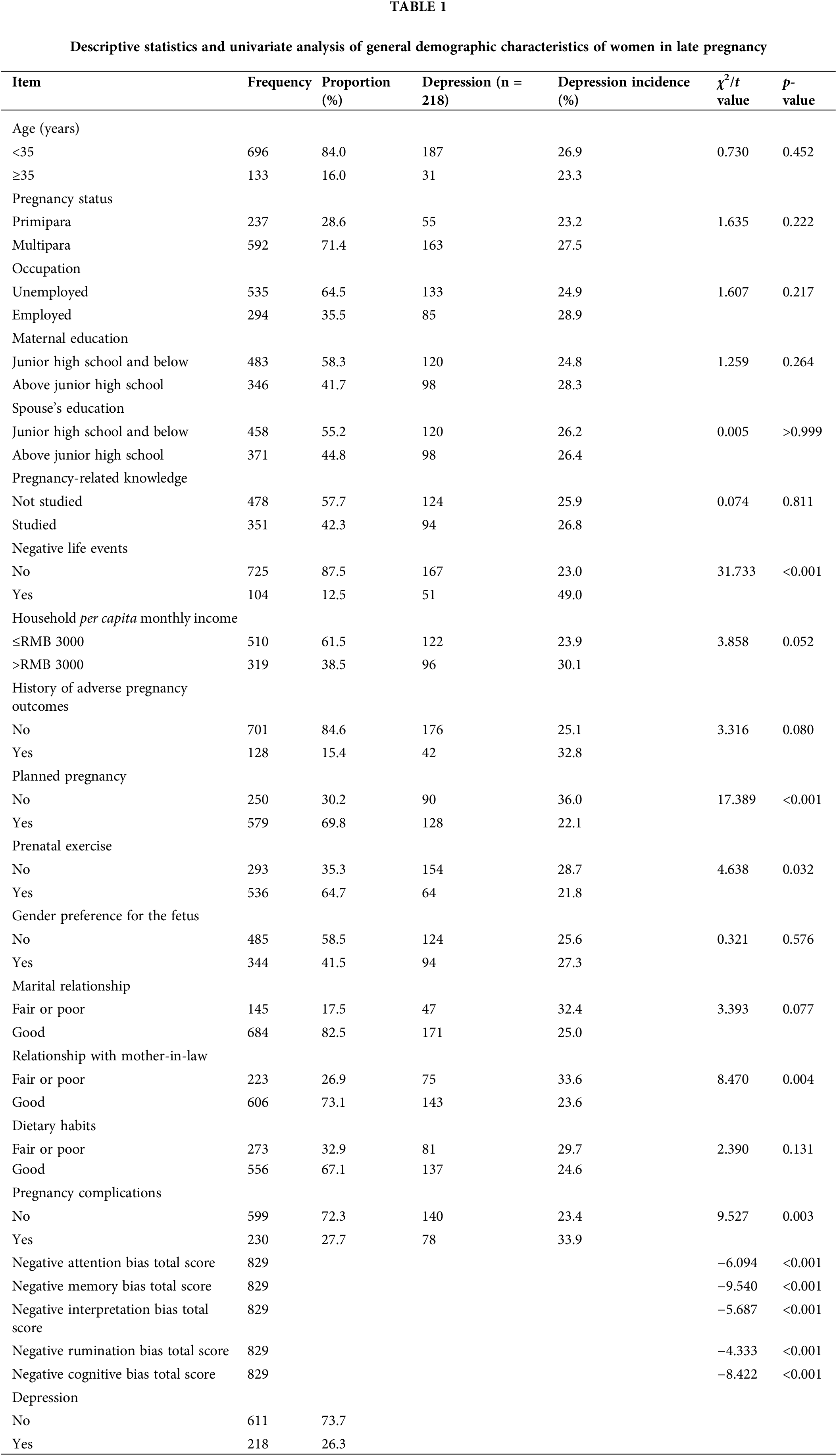
Pregnant women were categorized by age into childbearing age (<35 years) and elderly gravida (≥35 years). In this study, the oldest participant was 43 years old, and the youngest was 16, with 60% aged between 24 and 32 years. Other covariables are shown in Table 1.
Analysis of influencing factors on depression in late pregnancy
The completed general survey data for women in late pregnancy totaled 829 forms, as detailed in Table 1. Univariate analysis revealed that experiencing negative life events, whether the pregnancy was planned, prenatal exercise habits, the relationship with the mother-in-law, and the presence of complications were statistically significant factors (p < 0.05). Other variables showed no statistical significance (p > 0.05), as shown in Table 1.
t-test analysis indicated that pregnant women with depression in late pregnancy exhibited negative cognitive biases across all four dimensions: negative attentional bias, negative memory bias, negative interpretation bias, and negative rumination bias.
Correlation analysis between depression and negative cognitive bias in late pregnancy
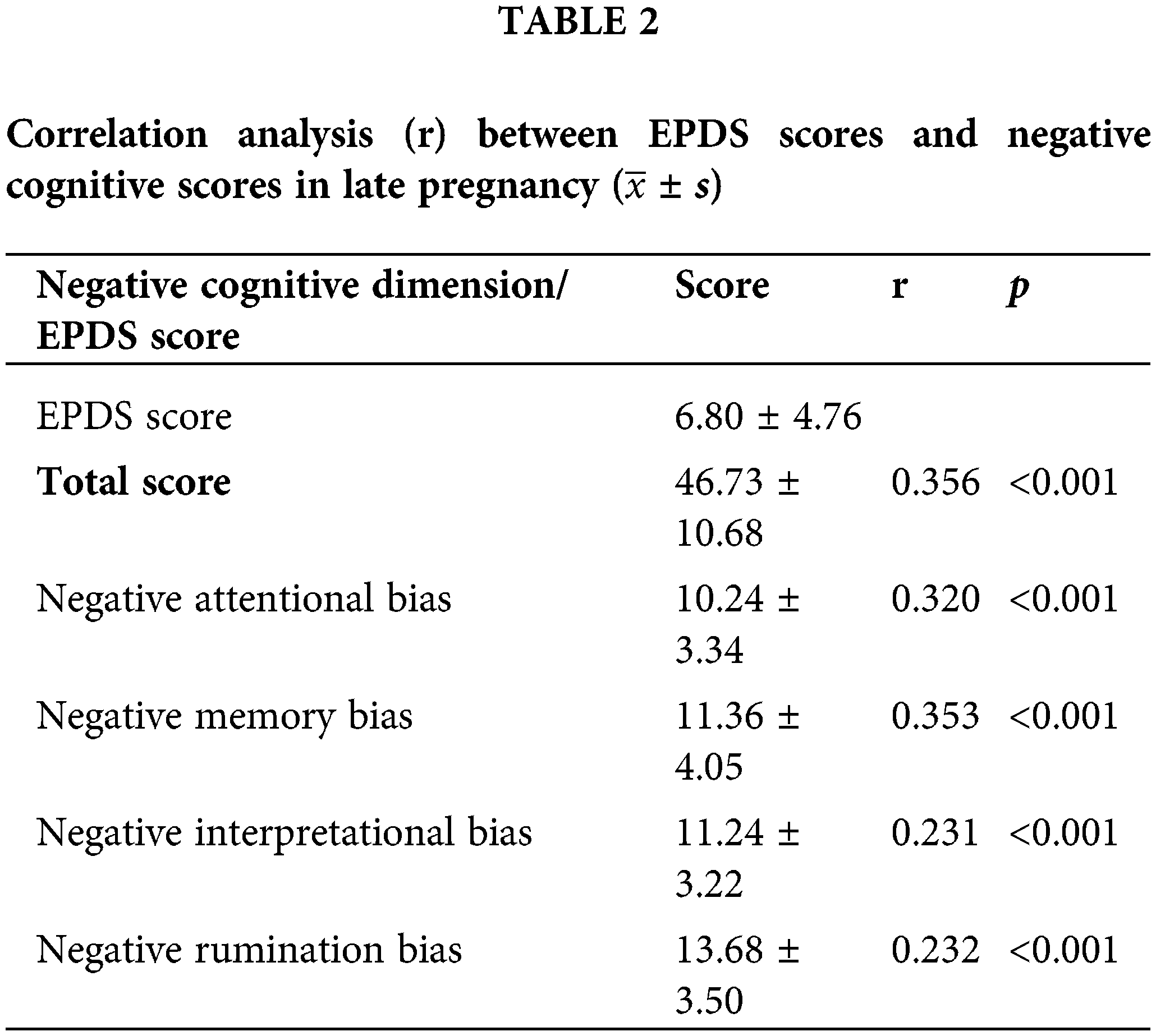
Pearson correlation analysis indicated that the mean EPDS score of pregnant women (6.80 ± 4.76) had statistically significant positive correlations with the mean score of negative cognitive bias (46.73 ± 10.68) and its four dimensions: negative attention bias (10.24 ± 3.34), negative memory bias (11.36 ± 4.05), negative interpretation bias (11.24 ± 3.22), and negative rumination bias (13.68 ± 3.50). The correlation coefficients were r = 0.356, 0.320, 0.353, 0.231, and 0.232, respectively (all p < 0.001). Detailed results are provided in Table 2.
Logistic regression analysis of influencing factors for depression in women during late pregnancy
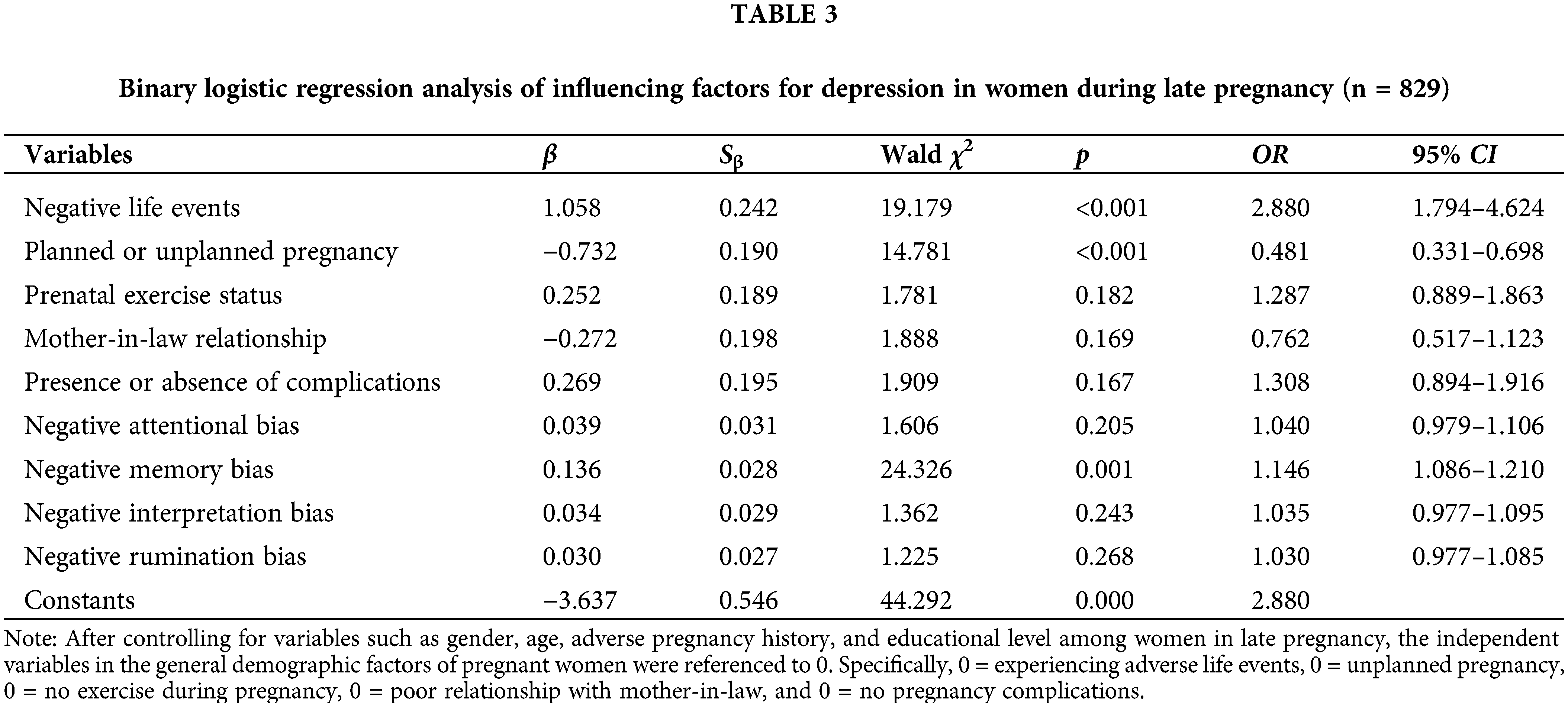
A binary logistic regression analysis was performed with depression status as the dependent variable and statistically significant variables from the univariate analysis, along with negative cognitive bias, as independent variables. The results indicated that planned pregnancy served as a protective factor against depression in late pregnancy (OR = 0.481). Conversely, experiencing negative life events during pregnancy and negative memory bias, a dimension of negative cognitive processing bias were identified as risk factors for depression in late pregnancy (OR = 2.880 and 1.146, respectively). As shown in Table 3.
Analysis of depression prevalence and influencing factors in women during late pregnancy
In the current era of rapid globalization and socioeconomic progress, the material foundation of humanity has become more abundant and stable, leading to a global increase in psychological disorders. Recently, there has been a growing focus on prenatal depression in both domestic and international reports. However, most previous research has concentrated on postpartum depression, with relatively few studies addressing prenatal depression, particularly in late pregnancy. Late pregnancy is a critical period when female organ function reaches its gestational peak, and childbirth is imminent. Factors such as hormonal changes, physical transformations, and concerns about the newborn can contribute to the onset and exacerbation of depressive symptoms [14]. In this study, 829 pregnant women were examined, among whom 218 were identified as having depression in late pregnancy (EPDS score ≥10), yielding a detection rate of 26.3%. This result aligns with Zhou et al.’s [15] findings of 26.9% but is lower than Chen et al.’s [16] reported 32.2%. It exceeds the depression rates observed in Suzhou (15.9%) [17] and Beijing (20%) [18] for late pregnancy. Bisetegn et al.’s research [19] revealed depression prevalence rates of 9.2%, 7.4%, and 15.5% in early, middle, and late pregnancy, respectively. Zhang et al.’s study [20] reported depression detection rates of 5.97%, 8.51%, and 15.56% for early, middle, and late pregnancy, respectively, indicating that late pregnancy depression rates surpass those of early and mid-pregnancy. Variability in reported depression detection rates across regions can be attributed to differences in research tools, assessment criteria, cultural contexts, living environments, family atmospheres, and individual variations. The 26.3% detection rate of depression in late pregnancy observed in this study significantly exceeds the incidence of other pregnancy-related complications. Without timely intervention, this could potentially lead to adverse effects on both mother and child.
Risk factors for depression in women during late pregnancy
Negative life events, including work-related stress, strained interpersonal relationships, loss of loved ones, and adverse pregnancy history, can trigger anxiety and depression in pregnant women. These stressors demand significant coping resources, and prolonged exposure can harm both physical and mental health [21]. This study found a positive correlation between experiencing negative life events during pregnancy and the occurrence of depression in late pregnancy. Pregnant women who experienced negative life events were 2.88 times more likely to develop depression than those who did not. Xu et al. [22] also identified negative life events during pregnancy as an independent risk factor for depression, consistent with the present findings. However, their research reported a higher risk, with a 4.02-fold increase in depressive symptoms. Biaggi et al. [23] found that negative life events such as domestic violence, childhood or pregnancy abuse, divorce, or loss of a close relative are closely associated with prenatal depression. Xu Yao’s study similarly highlighted the strong link between prenatal depression and negative life events. Increased psychological sensitivity and vulnerability during pregnancy can amplify the impact of negative events, leading to heightened negative emotions and behaviors, and exacerbating adverse psychological reactions. Therefore, healthcare professionals should assess the association between depressive symptoms and life events experienced by pregnant women and develop personalized intervention measures to promote psychological well-being.
In the field of negative cognition, negative attention bias is a core component of cognitive models. This bias refers to the inability to appropriately allocate attention to emotional cues. While most individuals focus on positive stimuli, susceptible individuals often excessively attend to negative stimuli, lacking selective attention to positive or neutral stimuli [24]. During late pregnancy, individuals frequently remember and recall negative experiences or aspects of events [24], leading to a negative cognitive processing bias in memory processing among pregnant women, who are considered a susceptible population. These findings suggest that cognitive therapy could be an effective intervention for pregnant women prone to repetitive thinking, rumination, and negative emotions, potentially preventing the exacerbation of depressive symptoms.
Protective factors against depression in late pregnancy
Unplanned pregnancy refers to an unexpected conception that occurs without prior planning or preparation by the couple, often causing confusion, anxiety, or stress. This study found that planned pregnancy is negatively correlated with depression in late pregnancy, indicating a higher depression rate among women with unplanned pregnancies. Conducted in a county town in Northern Anhui Province, the study highlighted the influence of regional, cultural, and economic factors on thinking patterns. Modern families often plan for childbearing; hence, unplanned pregnancies, as unexpected events, may result in insufficient support and care from husbands or mothers-in-law, leading to feelings of being unwanted and undervalued. This emotional isolation can increase the likelihood of developing depressive symptoms. Xu et al. [22] identified unplanned pregnancy as an independent risk factor for depression in late pregnancy (OR = 1.38). Families experiencing unplanned pregnancies often lack financial readiness and knowledge about pregnancy, disrupting family order and life plans. Zhu et al. [25] found unplanned pregnancy to be an independent risk factor for prenatal depression in Tianjin, while Yang et al.’s [26] survey in the Pearl River Delta region confirmed it as a major factor influencing depression among first-time pregnant women. These findings suggest the importance of medical staff providing comfort, guidance, and encouragement to pregnant women and their families to promote a positive attitude toward the baby’s arrival. Offering relevant medical knowledge and advice can help families understand pregnancy risks and precautions, protecting the health of both mother and fetus. Encouraging informed decision-making and planning among pregnant women and their spouses ensures appropriate arrangements and preparations, including financial, career, and family planning aspects.
At the same time, medical staff should regularly assess the psychological status of pregnant women, and provide timely psychological support. Psychological monitoring of pregnant women during pregnancy can follow both population-wide strategies and high-risk population strategies. The whole population strategy is to evaluate the mental health level, especially depression, of all pregnant women at different regular prenatal checkups and gestational weeks during pregnancy. The high-risk population strategy is to provide early intervention and closer testing for pregnant women with low negative cognitive bias and a high risk of depression. High-risk factors include low cultural level, poor economic conditions, strained mother-in-law and daughter-in-law relationship, unplanned pregnancy, low education level, low social support, adverse pregnancy history, pregnancy complications, and negative memory bias in this study [15,17,25,27]. For pregnant women with high-risk factors, early intervention can be carried out by establishing psychological testing clinics and maternity schools.
Positive correlation between negative cognition and depression in late pregnancy
The study results indicate a significant positive correlation between maternal depression in late pregnancy and negative memory bias. Higher scores in negative memory bias correspond to higher rates of depression, consistent with previous research [28,29]. It has been reported that individuals with depression exhibit excessive negativity in autobiographical memory, tending to recall more self-related sad events when recollecting personal experiences [30].
Analyzing the causes among the pregnant women in this group, those experiencing depression may exhibit cognitive narrowing, extremism, and obsessive thinking after encountering pathological, physiological, or psychological stress. Following stressful events, individuals might excessively emphasize potential negative consequences, leading to persistent anxiety and behavioral disorders. This aligns with findings from a study of 829 women in late pregnancy, which identified negative life events and pregnancy complications as independent risk factors for depression. Literature [31] indicated that cognitive factors play a crucial role in the development of depression as an affective disorder. External information and life events influence an individual’s emotions only through subjective cognitive appraisal. Distorted cognition or systematically negative biases inevitably lead to an accumulation of negative emotions. Pregnant women may involuntarily engage in repetitive thinking about stressful events, often with obsessive-compulsive characteristics. This process can hinder adaptive coping strategies and impede adjustment. Subsequently, pregnant women may involuntarily recall or experience sudden intrusive thoughts of distressing situations or content that persist. Negative memory bias can adversely affect pregnant women’s mental health, potentially leading to emotional disorders, anxiety, and depression. This underscores the importance of identifying and managing negative cognitive biases in mental health. Additionally, these findings suggest valuable recommendations for healthcare professionals. Psychological interventions such as cognitive behavioral therapy or mindfulness-based therapy could help pregnant women identify and modify negative cognitions, thereby improving their mental health.
Research has found that coping strategies such as sitting meditation and mindfulness yoga can improve pregnant women’s mindfulness awareness, prevent or alleviate prenatal anxiety, and improve their mental health during pregnancy [32–34]. This also provides good advice for medical staff to use cognitive behavioral therapy and mindfulness therapy in psychotherapy to help pregnant women identify and change negative cognition.
This study explored the relationship between pregnancy depression and negative cognitive bias from a psychological perspective, providing empirical evidence for theoretical research on psychological interventions during the perinatal period. However, this study also had certain limitations. It investigated the real psychological state of women during pregnancy in representative counties and districts in Northern Anhui, China. However, China is a multi-ethnic country with cultural differences between the North and South. A study conducted only in one hospital can only reflect the research results of a middle population, and there are limitations in the sample size. Subsequent studies would focus on expanding the sample size to meet sample diversity; This article was a survey based on a scale and can only be used for screening depressive symptoms, not for diagnosing depression.
In conclusion, a high prevalence of depression was detected among women in late pregnancy in the northern Anhui region of China, with a significant positive correlation to negative cognitive bias. Depressive symptoms in late pregnancy were closely associated with negative memory bias. When depression occurs in late pregnancy, pregnant women tend to exhibit negative cognitive bias, further exacerbating their depressive state. Specifically, this study found that negative memory bias in pregnant women intensified depressive symptoms. Consequently, healthcare professionals should regularly assess the psychological state of pregnant women and provide timely psychological support. Establishing a trusting relationship is crucial to help pregnant women navigate this unique period, ensuring the health of both mother and infant during the perinatal period.
Acknowledgement: We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Funding Statement: The authors did not receive specific funding for this study.
Author Contributions: The authors confirm their contribution to the paper as follows: study conception and design: Yuchen Ye; data collection: Dadi Wu; analysis and interpretation of results: Yuchen Ye, Jiahu Hao; draft manuscript preparation: Yuchen Ye. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
Ethics Approval: The study has been approved by the Medical Ethics Committee of Yingshang County People’s Hospital Clinical Research Subject Approval Medical Ethics Review document (IRB number 2024-10). Written consent was acquired from the participants.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. Dennis CL, Ross LE, Grigoriadis S. Psychosocial and psychological interventions for treating antenatal depression. Cochrane Database Syst Rev. 2007;18(3):CD006309. doi:10.1002/14651858.CD006309.pub2. [Google Scholar] [PubMed] [CrossRef]
2. Xiao X, Zhu S, Zhang H, Liu H. Concept analysis of prenatal depression. J Nurs. 2017;24(19):18–23. [Google Scholar]
3. Liu Y, Liu J, Wu YS, Chen YL, Ren SS, Shang YW, et al. Neuronal autophagy in depression and regulatory effect of traditional Chinese medicine: a review. Chin J Exp Tradit Med Formulae. 2021;27(16):218–26 (In Chinese). [Google Scholar]
4. Yang YH, Huang X, Sun MY, Yang L, Zheng RM. Analysis of depression status transition at different time points and influencing factors of persistent depression among Chinese pregnant and postpartum women. Chin J Epidemiol. 2022;43(1):58–64 (In Chinese). doi:10.3760/cma.j.cn112338-20210628-00502. [Google Scholar] [CrossRef]
5. Beckat. The evolution of the cognitive model of depresion and its neurobiological correlates. Am J Psychiat. 2008;165(8):969–77. doi:10.1176/appi.ajp.2008.08050721. [Google Scholar] [PubMed] [CrossRef]
6. Everaert J. Interpretation of ambiguity in depression. Curr Opin Psychol. 2021;41:9–14. doi:10.1016/j.copsyc.2021.01.003. [Google Scholar] [PubMed] [CrossRef]
7. Yan XY, Feng ZZ. Reliability and validity evaluation of the negative cognitive processing bias questionnaire in military personnel. Acta Acad Med Mil Tertiae. 2018;40(18):1619–23. [Google Scholar]
8. Zheng X, Wu SM, Liu LF. The relationship between optimism and depression in college students: a chain mediation of negative cognitive bias and negative affect. Psychol Explor. 2024;44(1):66–73. [Google Scholar]
9. Huang X, Fu FH, Zeng ZY, E MY, Tan XH. The influence of negative cognitive processing bias on social anxiety in college students: the mediating role of fear of positive evaluation. PSY. 2022;15(20):50–3. [Google Scholar]
10. Fu XY, Chen X, Zhang YZ. Analysis of the cut-off value of Edinburgh postnatal depression scale in screening for prenatal depression in late pregnancy. Chin J Clin Obstetrics GynEcol. 2018;19(5):453–4 (In Chinese). [Google Scholar]
11. Guo XJ, Wang YQ, Liu Y, Chen J, Pu XF. Study on the cut-off value of Edinburgh postnatal depression scale in screening for prenatal depression in late pregnancy. Chin J Nurs. 2009;44(9):808–10 (In Chinese). [Google Scholar]
12. Feng R, Li KL, Li ZS, Feng ZZ. Development and application of a questionnaire on negative cognitive processing bias in adolescents. Acta Acad Med Mil Tertiae. 2024;46(2):196–202. [Google Scholar]
13. Zhang R. Development and application of the negative cognitive processing bias questionnaire (Master’s Thesis). Third Military Medical University: China; 2015. [Google Scholar]
14. Feng YH, Yue HX, Zhan YL, Shi YJ, Chen YL, Wang YW, et al. Study on mental health status of pregnant women and its influencing factors in the third trimester. Chin J Epidemiol. 2021;42(5):853–8 (In Chinese). doi:10.3760/cma.j.cn112338-20200827-01102. [Google Scholar] [PubMed] [CrossRef]
15. Zhou XL, Liu H, Li XH, Zhang SM, Li F, Zhao ZL. Investigation on depression status and its influencing factors among women in middle and late pregnancy in Shaanxi province. Chin Nurs Manag. 2019;19(7):1005–11 (In Chinese). [Google Scholar]
16. Chen CR, Wu YQ, Wang YQ. Study on influencing factors of prenatal depression in pregnant women. MCHCC. 2009;24(25):3553–4. [Google Scholar]
17. Fan J, Kong LH, Wang XY, Yang Y, Sun Y, Li XH. Investigation on depressive mood and its influencing factors among pregnant women in Suzhou. J Psychiat. 2021;34(3):221–5. [Google Scholar]
18. Xu YQ, Wang XR, Wang ZX, Chen X, Liu XW, Zhao H. Investigation on the incidence and risk factors of perinatal depression in Beijing area. Chin J Health Psychol. 2024;32(1):47–51 (In Chinese). [Google Scholar]
19. Bisetegn TA, Mihretie G, Muche T. Prevalence and predictors of depression among pregnant women in Debretabor town, northwest Ethiopia. PLoS One. 2016;11(9):0161108. doi:10.1371/journal.pone.0161108. [Google Scholar] [PubMed] [CrossRef]
20. Zhang SY, Dai XF, Yang JP, Sun XY, Lin RJ. Analysis of depression and its influencing factors in pregnant women at different stages of pregnancy. Chin Gen Pract Nurs. 2021;19(7):965–8 (In Chinese). [Google Scholar]
21. Luo XY, Jiao GS, Xiu LY, Chen JT, Li WF. The relationship between life events, social support and mental health and well-being during pregnancy. Chin J Health Psychol. 2020;28(12):1761–6 (In Chinese). [Google Scholar]
22. Xu Y, Xiao CQ, Zhou YL, Li JH, Liu F, Wang ZJ. Analysis of depression status and influencing factors in pregnant women. J Pract Med. 2023;39(4):493–8. [Google Scholar]
23. Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Dis. 2016;191:62–77. doi:10.1016/j.jad.2015.11.014. [Google Scholar] [PubMed] [CrossRef]
24. Miao K. Study on the neural structural and functional characteristics of negative cognitive processing bias in individuals with depressive symptoms (Master’s Thesis). Army Medical University of the Chinese People’s Liberation Army: Chongqing, China; 2023. [Google Scholar]
25. Zhu RX, Bao XY, Fan J, Li Y, Jin XZ. Analysis of influencing factors of prenatal depression. Chin J Fam Plan. 2020;28(6):807–10+814. [Google Scholar]
26. Yang WJ, Chen Y, Xiao CQ, Li MM, Hu WX, Gao YM, et al. Investigation and analysis of depressive mood in first-time pregnant women in the Pearl river delta region. Nurs J Chin PLA. 2020;37(4):41–5 (In Chinese). [Google Scholar]
27. Liao YJ, Chen SY, Deng XY, Gan YQ, Han SL, Tan XL, et al. Construction and validation of a simple model for predicting prenatal depression risk. Sichuan Mental Health. 2023;36(5):466–72 (In Chinese). [Google Scholar]
28. Wang LL, Zhao J. Effects of late pregnancy depression on neonatal neurobehavioral development. Chin J Pract Nerv Dis. 2017;20(16):94–6 (In Chinese). [Google Scholar]
29. Luo SJ, Yang WH, Mo ZW, Wang QP. Effects of depressive mood in late pregnancy on neonatal neurobehavioral development. Chin Cont Med Edu. 2021;13(1):120–3 (In Chinese). [Google Scholar]
30. Williams JM, Barnhofer T, Crane C, Herman D, Raes F, Watkins E, et al. Autobiographical memory specificity and emotional disorder. Psychol Bull. 2007;133(1):122–48. doi:10.1037/0033-2909.133.1.122. [Google Scholar] [PubMed] [CrossRef]
31. Yan X, Zhang R, Feng ZZ. Development of the negative cognitive processing bias questionnaire. Acta Acad Med Mil Tertiae. 2017;39(23):2329–34. [Google Scholar]
32. Isgut M, Smith AK, Reimann ES, Kucuk O, Ryan J. The impact of psychological distress during pregnancy on the developing fetus: biological mechanisms and the potential benefits of mindfulness interventions. J Perinat Med. 2017;45(9):999–1011. doi:10.1515/jpm-2016-0189. [Google Scholar] [PubMed] [CrossRef]
33. Yuan PP. The effect of cognitive-behavioral intervention on negative emotions in emergency patients with threatened miscarriage. Pract J Gynecol Endocrinol. 2024;11(12):144–6. [Google Scholar]
34. Liu LJ, Han B, Liu C, Zhang R, Wang X. Research progress on the intervention effect and mechanism of yoga on prenatal depression. China Sports Sci Technol. 2023;59(1):44–50 (In Chinese). [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools