 Open Access
Open Access
ARTICLE
Protecting Protectors: Smartphone-Based Cognitive Behavioral Therapy for Mental Health in the Chinese Police
1 Social Management Department, Shaanxi Police College, Xi’an, 710021, China
2 School of Psychology, Shaanxi Normal University, Xi’an, 710061, China
3 Department of Psychiatry, The Second Xiangya Hospital of Central South University, Changsha, 410011, China
4 School of Education, Shaanxi Normal University, Xi’an, 710061, China
* Corresponding Author: Zheng Zhang. Email:
(This article belongs to the Special Issue: Exploring anxiety, stress, depression, addictions, executive functions, mental health, and other psychological and socio-emotional variables: psychological well-being and suicide prevention perspectives)
International Journal of Mental Health Promotion 2024, 26(11), 925-934. https://doi.org/10.32604/ijmhp.2024.056444
Received 23 July 2024; Accepted 15 October 2024; Issue published 28 November 2024
Abstract
Background: The mental health challenges faced by police officers due to high-stress work environments necessitate effective interventions. Cognitive-behavioral therapy (CBT) has shown promise in addressing mental health issues, and this study aims to evaluate the efficacy of smartphone-based cognitive-behavioral therapy (SCBT) in improving mental health outcomes among police officers. This intervention could provide a reference for enhancing mental health literacy and resilience in this population. Methods: A randomized controlled trial (RCT) design was employed, involving 291 police officers who were randomly assigned to either the SCBT intervention group (n = 145) or the control group (n = 146). Participants completed pre- and post-intervention assessments using the Symptom Checklist-90 (SCL-90), which measures multiple psychological symptoms including somatization, obsessive-compulsiveness, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Statistical analyses were conducted to examine group differences in symptom severity and effect sizes. Results: Post-intervention results indicated significant reductions in somatization, obsessive-compulsiveness, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism, with large effect sizes observed in the intervention group. Notably, the intervention group showed significantly greater improvements compared to the control group, particularly in overall psychological distress as measured by the total SCL-90 score. However, significant reductions in interpersonal sensitivity and paranoid ideation were also observed in the control group, suggesting external factors may have influenced these dimensions. Conclusion: SCBT demonstrated efficacy in reducing psychological distress among police officers, offering a flexible and accessible mental health intervention. However, challenges such as high dropout rates and the complex, dynamic nature of mental health warrant further investigation. Future studies should explore targeted interventions for specific behavioral issues and consider SCBT as a supplementary tool alongside traditional psychotherapy.Keywords
Nomenclature
| SCL-90 | Symptom Checklist-90 |
| SOM | Somatization |
| OC | Obsessive-compulsive disorder |
| IS | Interpersonal sensitivity |
| DEP | Depression |
| ANX | Anxiety |
| HOS | Hostility |
| PHOB | Phobic anxiety |
| PAR | Paranoia |
| PSY | Psychoticism |
| SCBT | Smartphone-based cognitive behavioral therapy |
The mental health crisis within the law enforcement community is a significant concern [1]. Police personnel worldwide have a high prevalence of mental health problems, including depression (14.6%), posttraumatic stress disorder (14.2%), and generalized anxiety disorder (9.6%) [2,3]. These alarming statistics highlight urgent mental health challenges. The demanding nature of police work, which involves exposure to violence, high-stress scenarios, and constant engagement with societal issues, significantly exacerbates mental health issues [4]. As first responders to violent and traumatic incidents, police officers experience profound psychological impacts that lead to severe mental health conditions that affect their physical health, increase the risks of self-harm or suicide, and impair job performance [5].
The unique pressures faced by the Chinese police force are primarily characterized by direct and frequent exposure to negative societal incidents, such as crime and violence. Excessive police work, the dangerous nature of the work itself and the irregularity of work shifts cause the majority of public security police to experience extreme fatigue and high pressure, which impose significant psychological burdens [6]. In addition, China’s political and organizational structure, which requires absolute loyalty to the Party and the state, places high demands on the police, who must use cognitive resources for self-supervision. Additionally, because of the influence of Confucian culture, police officers are positioned not only as law enforcers but also as societal role models to maintain social harmony and moral standards [7]. People have high expectations of the public security police, which amplifies their psychological stress due to the expectation that they must demonstrate superior moral and ethical conduct in their duties [8].
This combination of unique pressures poses a significant threat to the mental health of police officers, which manifests in a greater prevalence of psychological issues such as depression, anxiety, and occupational burnout and an increased risk of suicide compared to police forces in other cultural contexts [9]. These unique stressors necessitate the development of culturally sensitive intervention measures to effectively address these mental health challenges [10]. Designing mental health interventions for Chinese police officers requires consideration of these unique cultural and political factors as well as the use of comprehensive and multilayered strategies to ensure the effectiveness and cultural appropriateness of the interventions. This includes providing support from specially trained mental health professionals, establishing a stigma-free work environment, and developing mental health resources and programs that specifically cater to the needs of Chinese police officers [11].
Addressing these mental health concerns is crucial not only for the well-being of officers but also to alleviate the extensive social and economic burdens they pose [12]. Mental health problems within the police force adversely impact organizational effectiveness, escalate healthcare expenses, and induce productivity losses [13]. Law enforcement officers worldwide face significant mental health challenges due to their exposure to violence and trauma [14]. This leads to increased risks of depression, alcohol-use disorders, and trauma-related symptoms, often resulting in early disability retirement [15,16]. Comprehensive mental health support systems and strategies that are specifically designed for the law enforcement sector are vital to enhance officers’ quality of life and maintain the operational integrity of law enforcement bodies, which are crucial for societal stability and safety.
Cognitive Behavioral Therapy (CBT) is widely recognized as an effective approach for managing various mental health conditions. Beck [17] outlines a comprehensive framework for CBT, emphasizing the importance of case conceptualization, treatment planning, and session structuring. By utilizing core cognitive, behavioral, and experiential techniques, therapists can effectively engage patients and address both cognitive distortions and maladaptive behaviors. This structured approach makes CBT particularly suitable for interventions aimed at high-stress populations, such as police officers, where relapse prevention and patient engagement are critical [17].
Smartphone-based cognitive behavioral therapy (SCBT) represents a significant advancement in addressing mental health issues within police forces by providing a robust alternative to conventional interventions such as counseling, peer support, stress management workshops, and critical incident stress debriefing [18]. While traditional methods play a crucial role in providing coping mechanisms and support networks, they often encounter limitations due to stigma, fear of professional repercussions, and a one-size-fits-all approach that may not meet specific individual needs [19,20]. SCBT, in contrast, offers enhanced accessibility, allowing officers to discreetly engage with therapeutic content on their terms and reducing concerns related to stigma and confidentiality [21]. The personalized nature of the intervention, which is facilitated through customized modules and interactive features, allows for more precise targeting of the cognitive and behavioral patterns associated with stress and trauma [22]. Additionally, SCBT leverages a data-driven framework to continuously monitor progress and refine therapeutic strategies to ensure optimal outcomes. This approach not only aligns with the unique demands of law enforcement personnel but also bridges the gap between the need for mental health support and the utilization of such services [23].
The study aims to explore the effectiveness of SCBT in improving the mental health of police officers. Given the high prevalence of psychological distress, such as depression, anxiety, and post-traumatic stress disorder (PTSD) within the police population, this research employs a randomized controlled trial (RCT) to evaluate whether SCBT, as a convenient psychological intervention, can effectively alleviate these symptoms. By comparing the changes in mental health between the intervention group and the group receiving standard support, focusing on dimensions such as somatization, obsessive-compulsive symptoms, anxiety, and depression, the study seeks to validate the therapeutic impact of SCBT.
Police officers were recruited through an announcement by the Political Department of the Public Security Bureau to participate in a 6-week online self-help psychological counseling program. A total of 401 officers enrolled, and after screening, 371 participants (297 males, 74 females, aged 22 to 58) were deemed eligible and voluntarily signed informed consent forms. The inclusion criteria were: ① grassroots officers aged ≥22 years; ② subjective belief of needing self-help counseling; ③ mean scores on more than 3 factors of the SCL-90 exceeding 2; ④ access to a computer or cell phone; ⑤ agreement to participate continuously for 6 weeks. Exclusion criteria included: ① undergoing psychotherapy or taking psychiatric medication; ② experiencing suicidal ideation (referred to medical services); ③ inability to guarantee sufficient time; ④ pregnant, planning pregnancy, or breastfeeding. The survey was conducted from July to December 2022 (Fig. 1).
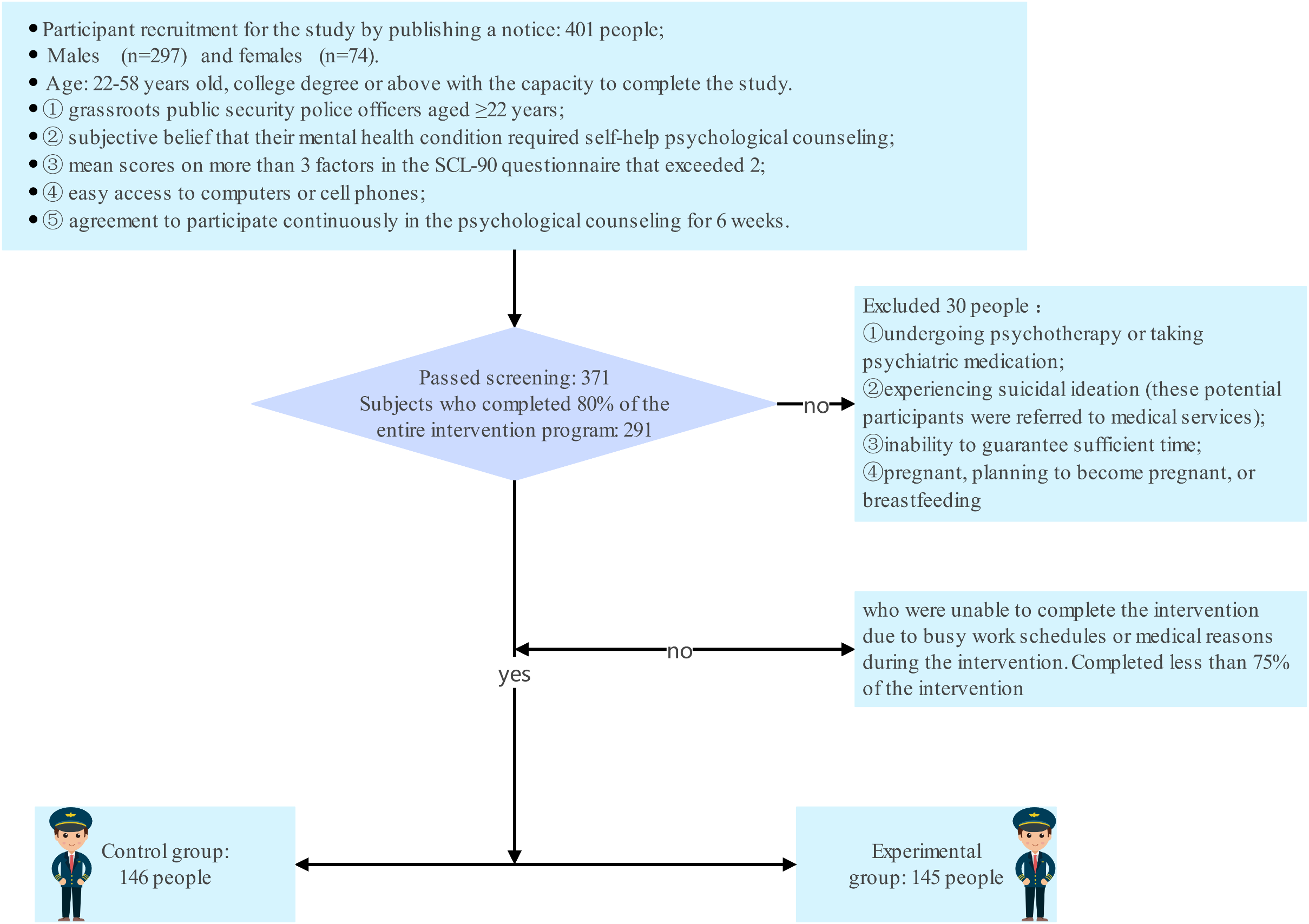
Figure 1: Research flow chart.
A RCT was conducted to test the hypothesis that SCBT could improve the mental health of police officers. Participants were randomly assigned (1:1) using a computer-generated number table to either the SCBT intervention group or a control group receiving standard support. To ensure fairness and reduce selection bias, group assignment was handled by an independent third party, with participants unaware of their allocation.
The SCBT group underwent a program tailored to address the unique stressors of police work, while the control group received basic mental health education, including stress management resources and mental health hotline information. Pre- and post-intervention assessments focused on depression, anxiety, stress, and suicidal ideation. The study aimed to provide empirical evidence of SCBT’s effectiveness as a psychological intervention for high-stress professions like law enforcement.
This RCT employed a 6-week intervention using a dedicated online platform supported by psychological counseling. Informed by CBT principles, the intervention aimed to improve the mental health of public security police officers during the pandemic response.
The intervention program, based on a manual addressing the physical and mental health of public security personnel during pandemics, was designed using CBT principles, specifically strategies from CBT Made Simple [24]. It included case conceptualization, structured treatment planning, and cognitive-behavioral techniques to address negative thought patterns. Key components included behavioral activation, homework assignments, setting realistic goals, cognitive restructuring, and promoting mental health awareness. These strategies were tailored to enhance mental resilience and coping skills, particularly for high-stress roles like law enforcement. The program was evaluated and refined by three experienced counselors to ensure relevance and effectiveness, and was delivered via a dedicated online platform for accessibility.
The content was based on the “Public Security Police Auxiliary Police Epidemic Response Physical and Mental Health Handbook” by the Ministry of Public Security [25]. A dedicated WeChat public account disseminated weekly course content and was designed to fit into the participants’ fragmented schedules. The intervention comprised three phases: psychological education (Session 1), cognitive education and behavioral training (Sessions 2–5), and consolidation and prevention (Session 6). Each phase addressed specific aspects of mental health improvement (Table 1).
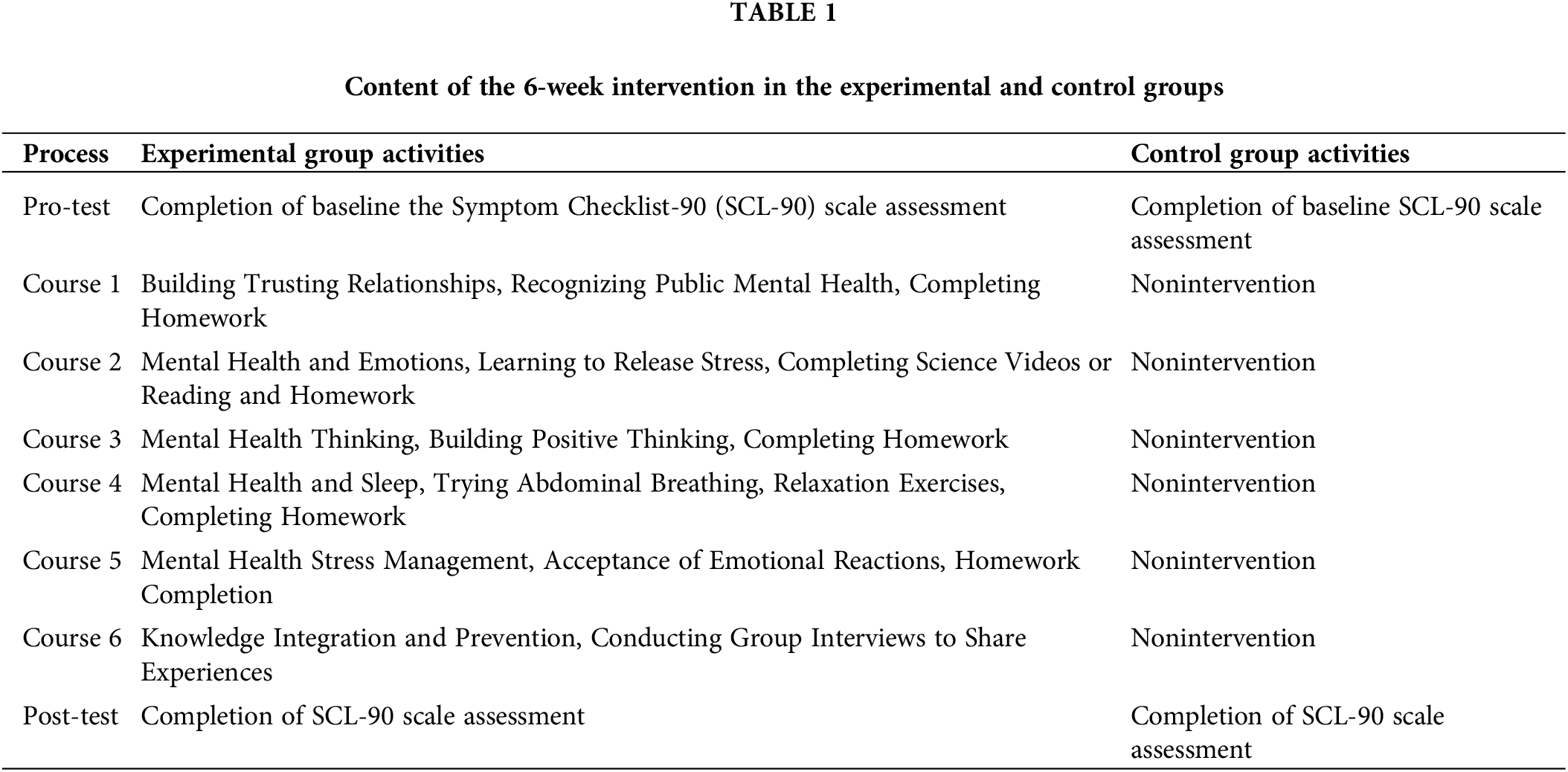
Content of the 6-week intervention is designed following the principles of CBT, as outlined by Beck in Cognitive Therapy: Basics and Beyond. The program focuses on stress management, emotional regulation, and positive thinking by utilizing core CBT strategies such as cognitive restructuring, behavioral activation, and relaxation techniques, which have been proven effective in improving mental health outcomes in high-stress populations [26].
Phase 1 (Session 1): Focus on building trust, understanding public mental health, and homework assignments.
Phase 2 (Sessions 2–5): Emphasis on mental health awareness, stress management, positive thinking, family dynamics, self-expression, and behavioral interactions such as hugs and massages.
Phase 3 (Session 6): Consolidation of learned concepts, group interviews for experience sharing, and encouragement of self-training and emotional regulation.
Before the intervention, the participants were briefed on platform use and intervention logistics, including the module completion time and weekly content engagement (30–50 min). Online counseling support was available 1–2 times weekly for approximately 50 min per session and was provided by counsellors with advanced psychology degrees and CBT training (See Fig. 2).
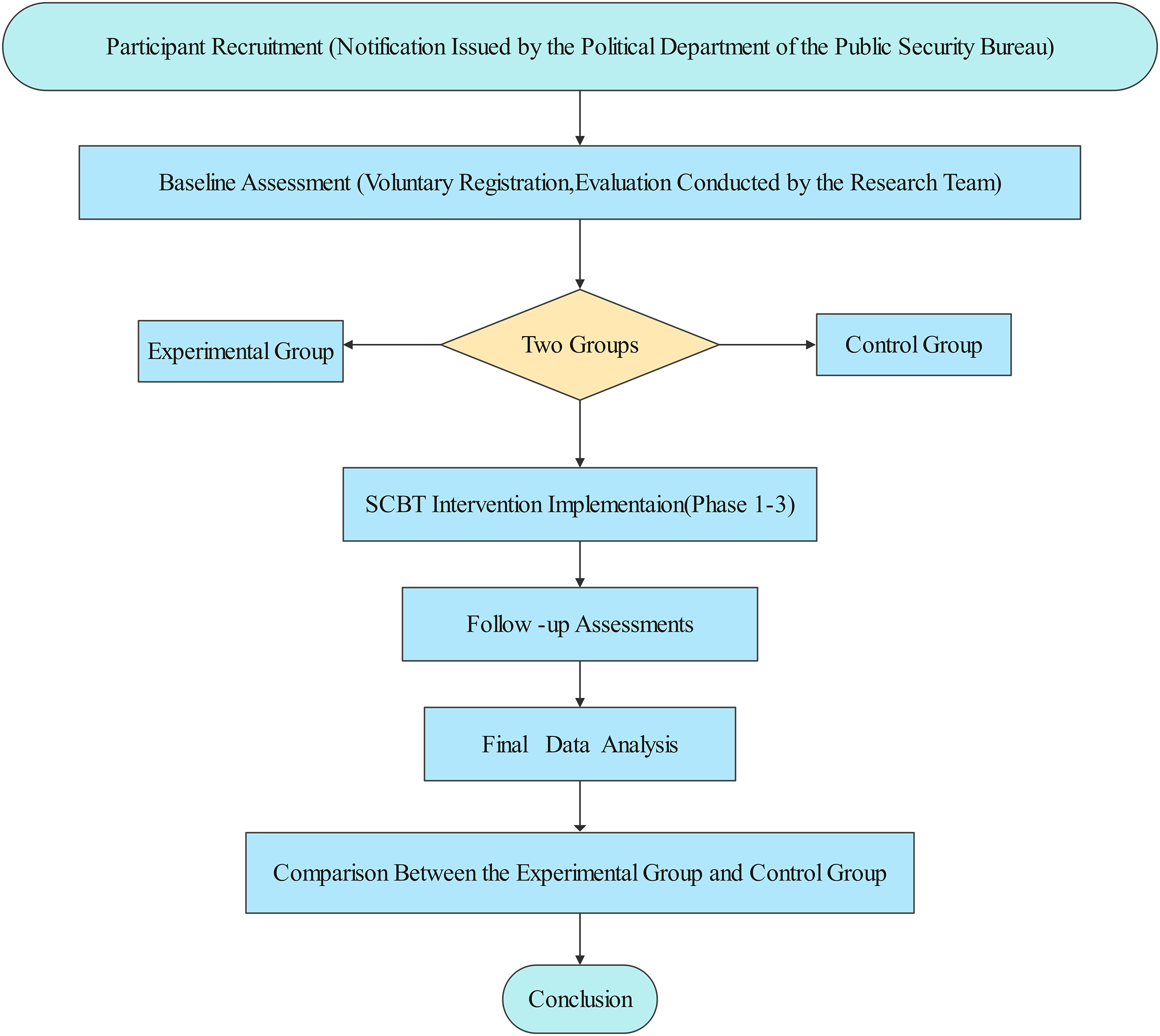
Figure 2: Flowchart of the SCBT intervention process.
SCL-90, developed by Derogatis in 1975, is a self-report inventory designed to assess psychological symptoms in individuals aged 16 and older [27,28]. The SCL-90 is a commonly used psychological assessment tool that evaluates a wide range of psychological symptoms, including depression, anxiety, obsessive-compulsive symptoms, and hostility. These dimensions are highly relevant to the high-stress work environment of police officers, making it an effective tool for assessing their mental health. Several studies have validated the SCL-90’s applicability in Chinese populations, confirming its reliability and validity. This demonstrates that the scale can accurately reflect mental health issues within the Chinese cultural context, particularly in high-risk, high-stress professions like policing [2,29]. It comprises 90 items across 10 dimensions, such as somatization, obsessive-compulsivity, interpersonal sensitivity, depression, and anxiety, each rated on a scale from 1 (“not at all”) to 5 (“extremely severe”). The SCL-90 is noted for its high internal consistency (with Cronbach’s alpha typically over 0.70) and validated structure, making it a reliable tool for diagnosing psychological conditions and evaluating outcomes in clinical and research settings [2,29–32].
This study was approved by the Ethics Committee of Shaanxi Police College (Approval No. 20220619). All participants signed the informed consent in this study. All subjects received a detailed description of the purpose of the investigation and the entire study procedure. All procedures were performed in accordance with the guidelines of our institutional ethics committee, and the principles of the Declaration of Helsinki were followed throughout.
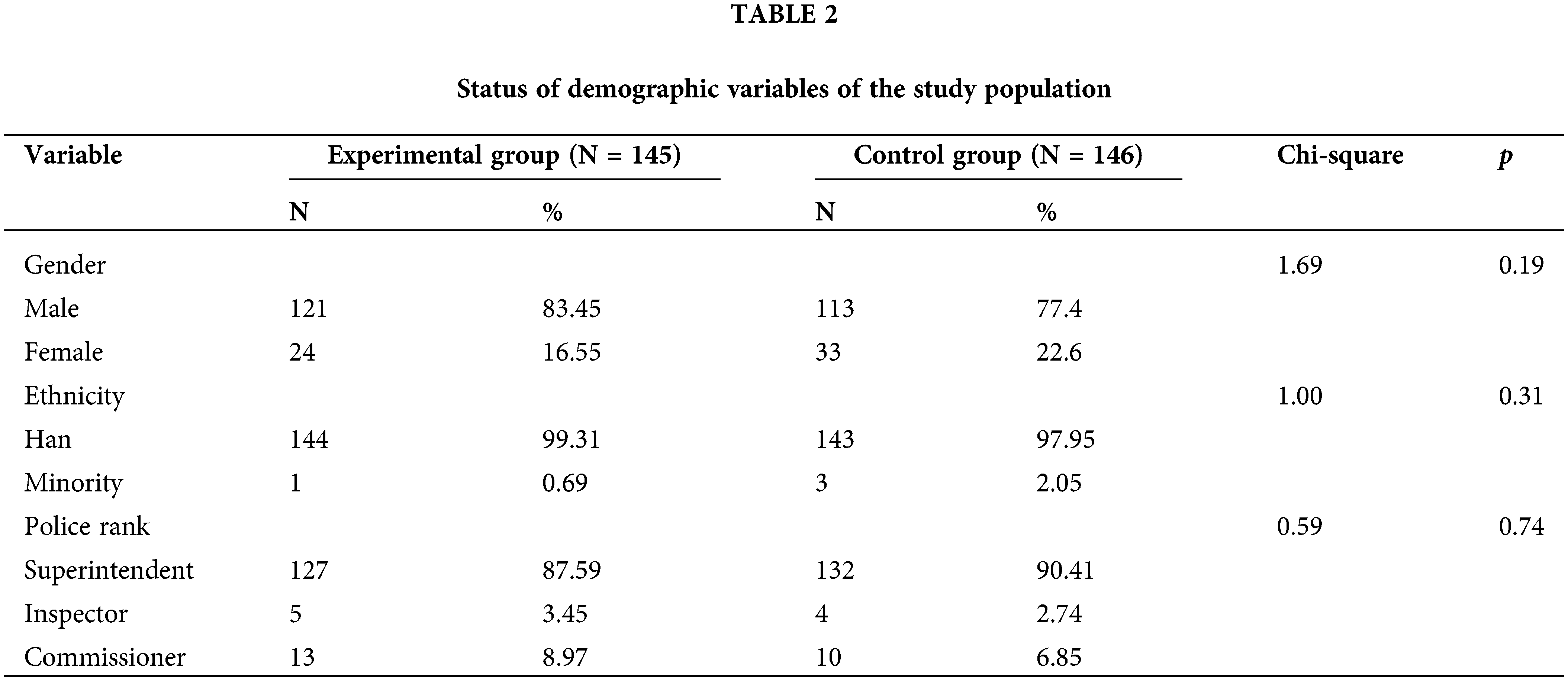
To ensure the statistical power and reliability of our findings, sample size calculations were meticulously performed prior to data collection. These calculations were grounded in established statistical parameters: an alpha level of 0.05, a power of 0.90, and an expected medium effect size (Cohen’s |δ|) of 0.5. For the independent-samples t-test, a minimum sample size of 84 participants was identified as necessary to detect the anticipated effect size with 90% power. Similarly, the paired-samples t-test required a minimum of 44 participants to achieve the same level of statistical power for within-subject comparisons. Our study’s participant recruitment exceeded these calculated thresholds, ensuring ample statistical power to substantiate the hypothesized effects. This approach affirms the adequacy of our sample size and enhances the credibility and generalizability of our results (Table 2).
All statistical analyses were conducted using JASP 0.16 software. Descriptive statistics were used to summarize the demographic characteristics of the participants. To test for significant differences, independent-sample t-tests were employed, with a significance level set at p < 0.05.
Distribution of demographic variables
The chi-square test results indicated no significant differences between the experimental and control groups in terms of gender, ethnicity, or job level distribution. This suggests a balanced allocation of these important covariates across both groups, establishing a homogeneous baseline for further analysis.
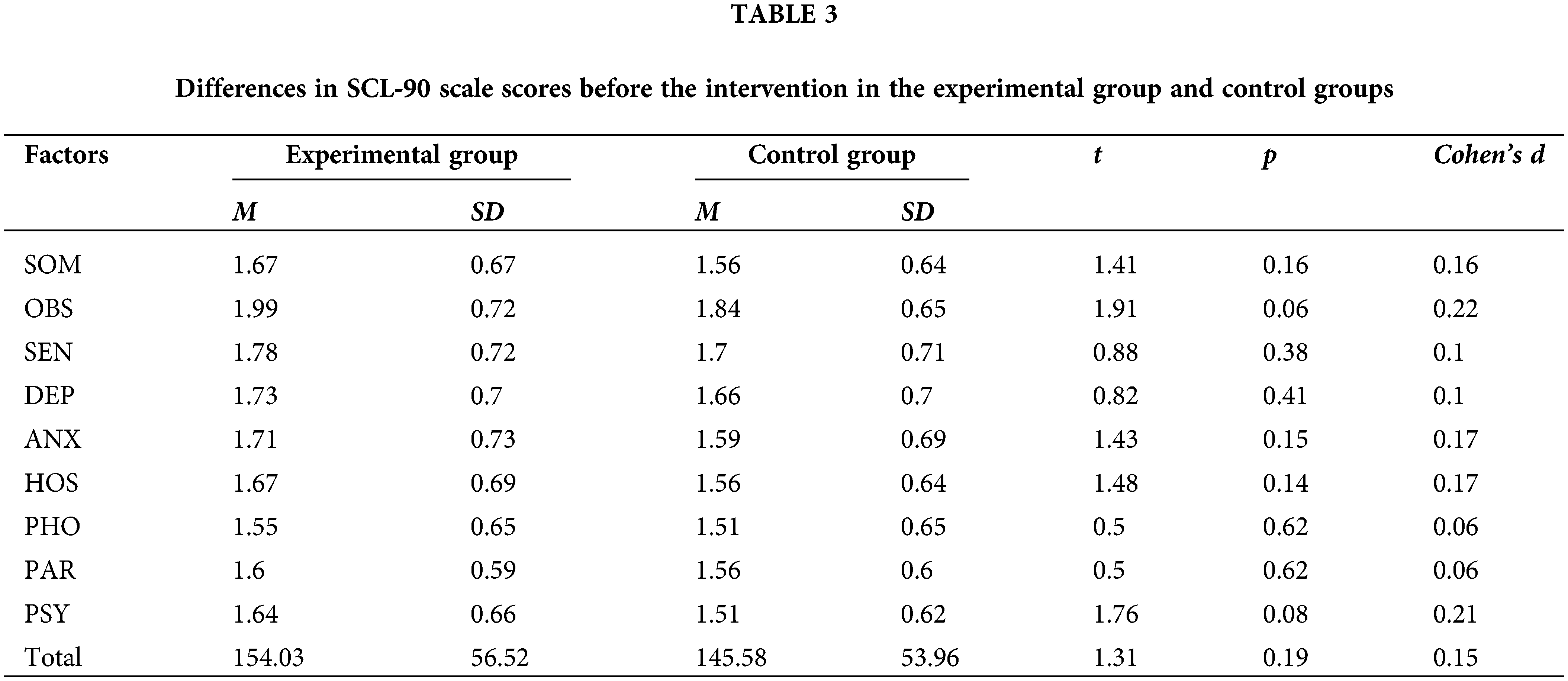
The baseline data revealed no significant differences between the control and experimental groups at the initial assessment (T1), especially in their scores across all dimensions of SCL-90. This equivalence underscores a critical premise for the effectiveness of subsequent interventions, indicating that any differences observed postintervention can be attributed directly to the effects of the intervention itself rather than to preexisting discrepancies (Table 3).
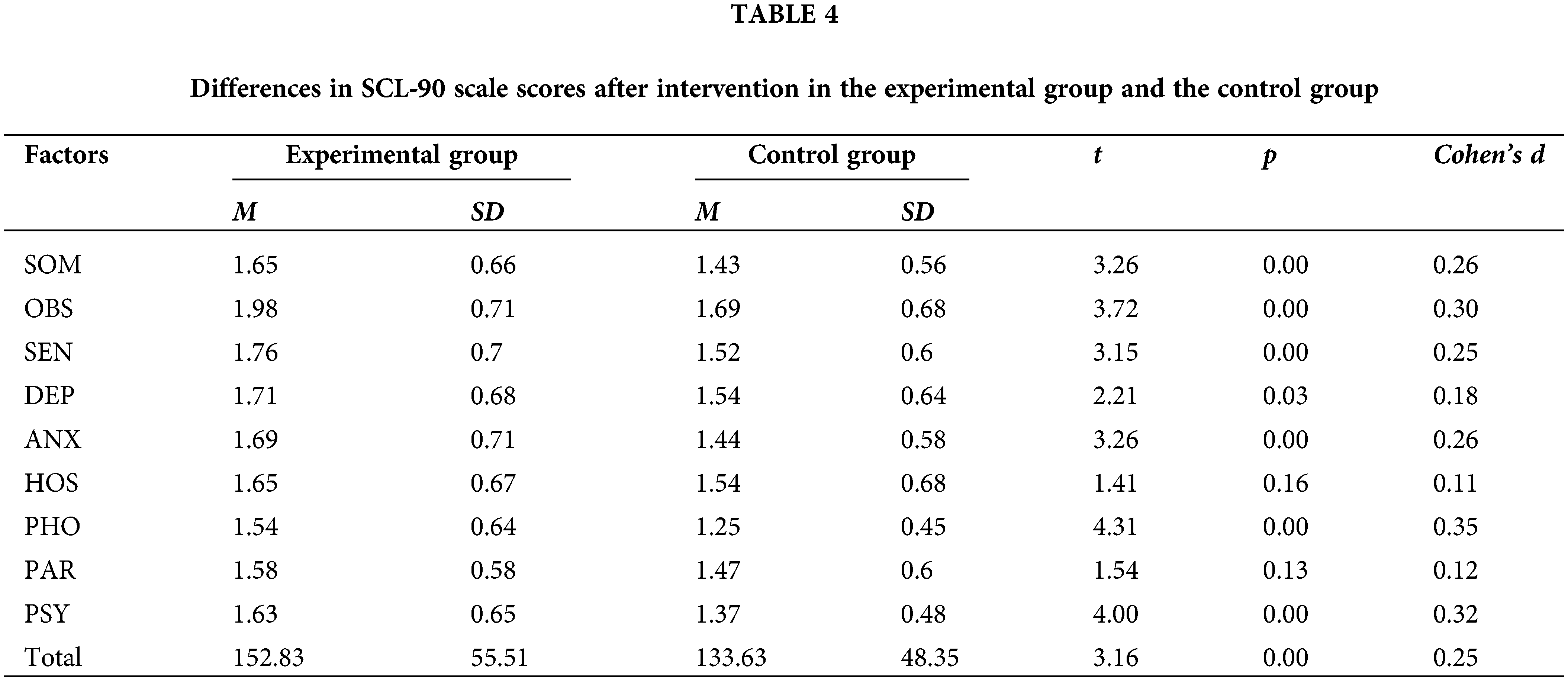
The follow-up data revealed significant differences between the groups postintervention (T2), with the experimental group showing notable improvements in SOM, OBS, ANX, PHO, PSY, and overall scores compared to those of the control group. These findings affirm the intervention’s impact on these specific psychological domains, highlighting significant improvements or changes in the experimental group (Table 4).
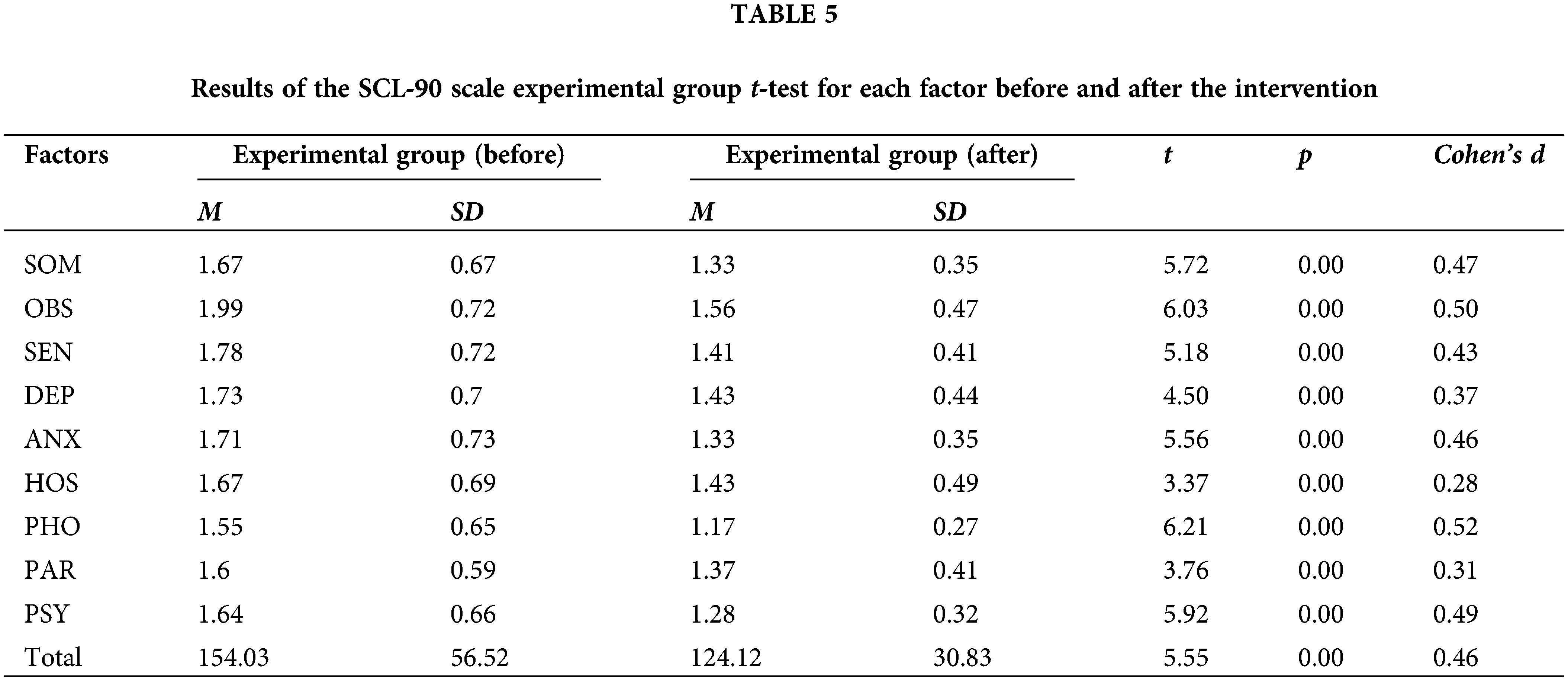
Furthermore, within the experimental group, notably positive outcomes were observed, including enhancements in all symptoms and overall scores. These outcomes underscore the effectiveness of the experimental intervention in improving a spectrum of psychological symptoms, demonstrating its potential as a targeted approach to mental health improvement (Table 5).
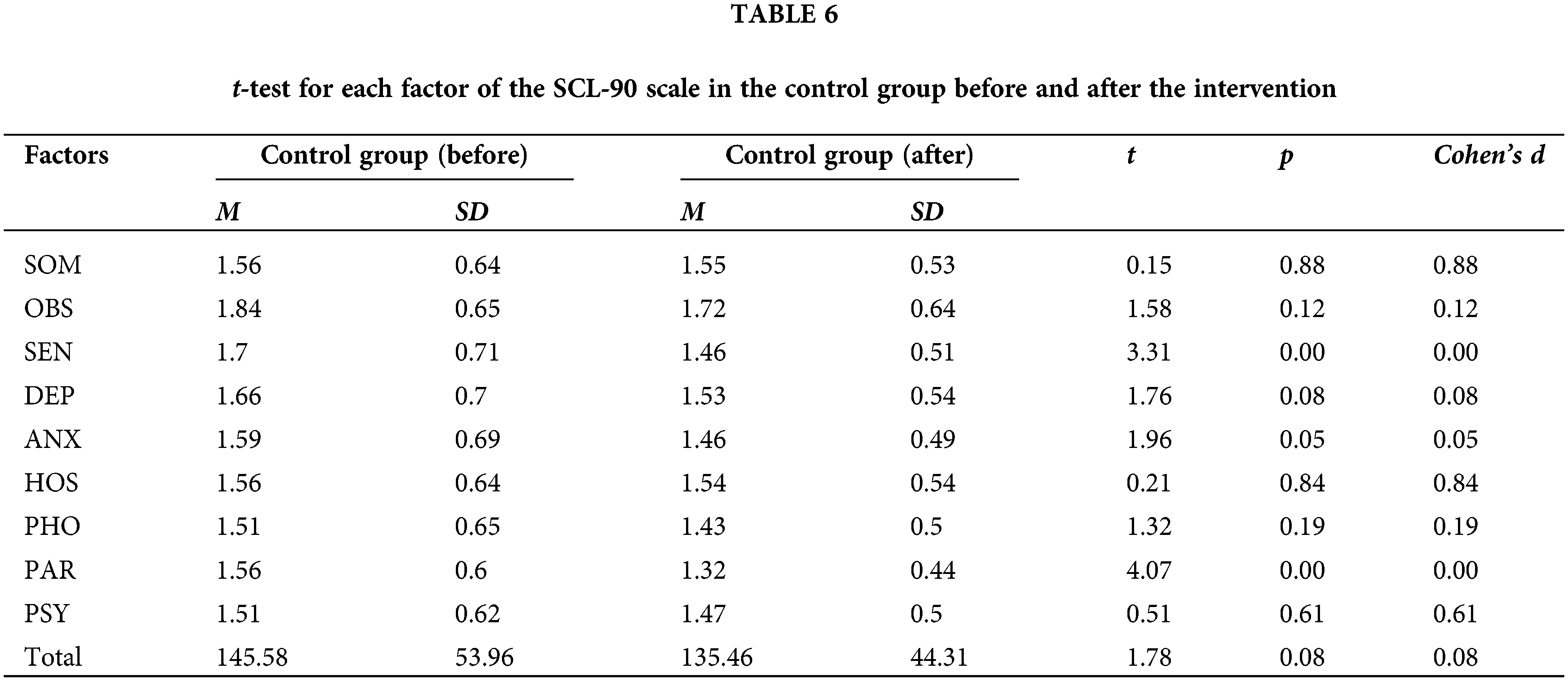
The significant differences observed in interpersonal sensitivity (SEN) and paranoid ideation (PAR) between the pre- and post-intervention measurements in the control group present a challenge for interpreting the results (Table 6).
In this study, we observed a high dropout rate, primarily due to the work demands of police officers during the COVID-19 pandemic. Many participants had to remain on call at all times, which prevented them from completing the intervention as planned. We recognize that this dropout rate may introduce potential bias, affecting the representativeness and external validity of the study results.
To address this challenge, we implemented several measures to mitigate the impact of bias. In our data analysis, we applied appropriate statistical methods to account for the missing data caused by the dropout. Additionally, we compared the characteristics of retained participants with those who dropped out to assess whether the dropout introduced any systematic bias into the study outcomes. Nevertheless, we acknowledge that the dropout rate may still affect the generalizability of the results, and future research should consider designing more flexible interventions to accommodate the unique demands of high-stress occupations.
This study found that the SCBT-based intervention had a positive impact on certain mental health indicators, such as the SOM, OBS, SEN, DEP, ANX, PHO, and PSY factors, although it did not demonstrate significantly higher improvements across all measures. This may be related to individual differences among participants, the duration of the intervention, or the intervention model [33,34].This finding highlights the importance of culturally specific interventions tailored to the unique mental health characteristics of police officers within the Chinese cultural context. The pressures and challenges faced by Chinese police officers are distinct from those encountered by police forces in other cultural settings, including high work intensity, a profound sense of responsibility for social stability and harmony, and the requirement of absolute loyalty to the Party and the state.
Developing and implementing intervention measures that specifically address the unique psychological stresses and cultural background of Chinese police officers is crucial [35]. The SCBT intervention designed in this study took these cultural characteristics and specific sources of stress into account to provide a flexible intervention method that respects cultural sensitivities while adapting to the work rhythm of police officers, thus offering an effective mental health support scheme for Chinese police. This approach not only helps police officers better manage and alleviate the stresses of work and life but also serves as a valuable reference for designing more culturally adaptive mental health interventions in the future.
Similar to previous studies, the results of our RCT substantiated the hypothesis that SCBT can significantly improve mental health outcomes among police officers [36]. Notably, the experimental group showed considerable improvements in several mental health dimensions, including somatization, obsessive-compulsive disorder, anxiety, phobic anxiety, psychoticism, and overall scores, as measured by SCL-90. These findings highlight the effectiveness of the SCBT intervention in alleviating the psychological burdens of law enforcement officers, thereby enhancing their psychological well-being and operational effectiveness [22,37].
However, the impact of the intervention was nuanced, with unexpected findings in the control group for interpersonal sensitivity and paranoid ideation, suggesting that external factors might also significantly influence these specific dimensions of mental health. This observation highlights the complexity of mental health dynamics within the law enforcement context and underscores the need for a multifaceted approach to mental health interventions that accounts for external influences and individual differences.
The discreet and flexible nature of smartphone-based interventions combined with the customization and interactivity offered by SCBT provides a promising avenue to address the mental health needs of this high-risk group. The study’s methodological rigor, including the use of a RCT design and comprehensive mental health outcome assessment using the SCL-90, enhances the credibility and generalizability of our findings. SCBT, as a flexible and easily scalable intervention, is particularly suitable for situations where face-to-face psychological counseling is not feasible, such as for high-stress, time-constrained professional groups like police officers [38–40].
Sample Representativeness and Generalizability: The study’s sample is drawn from a specific police population in a particular region, which may limit its representativeness. As a result, the findings may not be applicable to other professions, regions, or cultural contexts. Future research should aim to include a more diverse sample to enhance the generalizability of the results across various settings.
Short-Term Intervention and Dropout Rate: The intervention lasted for a relatively short period of six weeks, and the high dropout rate due to the demanding nature of police work may introduce systematic bias. This limits the ability to assess the long-term effects of the intervention and affects the overall robustness of the results. Extending the duration of the intervention and including follow-up assessments would provide a better understanding of the long-term impact. Additionally, implementing strategies to improve participant retention could mitigate this limitation.
In conclusion, our study offers valuable insights into the effectiveness of SCBT to improve the mental health of law enforcement officers. While the intervention showed significant benefits across several key mental health areas, the complex interaction of individual and external factors highlights the need for ongoing research to refine and optimize mental health interventions for this critical population. Future studies should investigate the mechanisms behind the observed changes in mental health outcomes, the long-term effects of SCBT, and how these interventions can be integrated into broader mental health support strategies for law enforcement personnel.
Acknowledgement: The authors would like to thank Xianyang Public Security Bureau and Yangling Model District Public Security Bureau for assistance and guidance in this research.
Funding Statement: This work was supported by the Shaanxi Police Officers’ Vocational College Scientific Research Project (grant number YJKY202310).
Author Contributions: The authors confirm contribution to the paper as follows: Huiting Zou and Zheng Zhang researched literature and conceived the study. Peng Chen and Huiting Zou were involved in protocol development, gaining ethical approval, patient recruitment and data analysis. Huiting Zou and Zheng Zhang wrote the first draft of the manuscript. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data will be provided upon request to the corresponding author.
Ethics Approval: This study was approved by the Ethics Committee of Shaanxi Police College (Approval No. 20220619). All participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Campbell J, Ahalt C, Hagar R, Arroyo W. Building on mental health training for law enforcement: strengthening community partnerships. Int J Prison Health. 2017;13(3–4):207–12. doi:10.1108/IJPH-10-2016-0060. [Google Scholar] [PubMed] [CrossRef]
2. Li YQ, Ren ZH, Jiang GR. A meta-analysis of the mental health status of police officers in Chinese public security agencies. Adv Psychol Sci. 2016;24(5):692–706 (In Chinese). doi:10.3724/SP.J.1042.2016.00692. [Google Scholar] [CrossRef]
3. Syed S, Ashwick R, Schlosser M, Jones R, Rowe S, Billings J. Global prevalence and risk factors for mental health problems in police personnel: a systematic review and meta-analysis. Occup Environ Med. 2020;77(11):737–47. doi:10.1136/oemed-2020-106498. [Google Scholar] [PubMed] [CrossRef]
4. Van DV, Peter G, Kleber RJ, Grievink L, Yzermans JC. Confrontations with aggression and mental health problems in police officers: the role of organizational stressors, life-events and previous mental health problems. Psychol Trauma Theory Res Pract Policy. 2010;2(2):135–44. doi:10.1037/a0019158. [Google Scholar] [CrossRef]
5. Van der Velden PG, Rademaker AR, Vermetten E, Portengen MA, Yzermans JC, Grievink L. Police officers: a high-risk group for the development of mental health disturbances? A cohort study. BMJ Open. 2013;3(1):e001720. doi:10.1136/bmjopen-2012-001720. [Google Scholar] [PubMed] [CrossRef]
6. Jetelina KK, Molsberry RJ, Gonzalez JR, Beauchamp AM, Hall T. Prevalence of mental illness and mental health care use among police officers. JAMA Netw Open. 2020;3(10):e2019658. doi:10.1001/jamanetworkopen.2020.19658. [Google Scholar] [PubMed] [CrossRef]
7. Jiao AY. Police and culture: a comparison between China and the United States. Police Q. 2001;4:156–85. doi:10.1177/109861101129197789. [Google Scholar] [CrossRef]
8. Wang J, Liu S. Ordering power under the party: a relational approach to law and politics in China. Asian J Law Soc. 2019;6(1):1–18. doi:10.1017/als.2018.40. [Google Scholar] [CrossRef]
9. Zhu X, Xia M, Hu Y, Zhang L, Lu Y, Zhang Y, et al. Mental status and psychological needs of Chinese police officers in a highly impacted city during the COVID-19 Pandemic. Int J Ment Health Promot. 2020;22(3):149–57. doi:10.32604/IJMHP.2020.011097. [Google Scholar] [CrossRef]
10. Wang Y, Zheng L, Hu T, Zheng Q. Stress, burnout, and job satisfaction. Public Personnel Manage. 2014;43(3):325–39. doi:10.1177/0091026014535179. [Google Scholar] [CrossRef]
11. Chen IH, Lin CY, Zheng X, Griffiths MD. Assessing mental health for China’s police: psychometric features of the self-rating depression scale and symptom checklist 90-revised. Int J Environ Res Public Health. 2020;17(8):2737. doi:10.3390/ijerph17082737. [Google Scholar] [PubMed] [CrossRef]
12. Patterson GT. Mental stress and workers’ compensation claims among police officers. J Workplace Rights. 2011;14(4):441–55. [Google Scholar]
13. Buys CRaN. Managing occupational stress injury in police services: a literature review. Int Public Health J. 2013;5:413–25. [Google Scholar]
14. Stogner J, Miller BL, McLean K. Police stress, mental health, and resiliency during the COVID-19 Pandemic. Am J Crim Justice. 2020;45(4):718–30. doi:10.1007/s12103-020-09548-y. [Google Scholar] [PubMed] [CrossRef]
15. Price M. Psychiatric disability in law enforcement officers. Behav Sci Law. 2017;35(2):113–23. doi:10.1002/bsl.v35.2. [Google Scholar] [CrossRef]
16. Mumford EA, Liu W, Taylor BG. Profiles of US law enforcement officers’ physical, psychological, and behavioral health: results from a nationally representative survey of officers. Police Q. 2021;24:357–81. doi:10.1177/1098611121991111. [Google Scholar] [CrossRef]
17. Beck JS. Cognitive behavior therapy: basics and beyond. 2nd ed. USA: Guilford Publications; 2020. [Google Scholar]
18. Marciniak MA, Shanahan L, Rohde J, Schulz A, Wackerhagen C, Kobylinska D, et al. Standalone smartphone cognitive behavioral therapy-based ecological momentary interventions to increase mental health: narrative review. JMIR Mhealth Uhealth. 2020;8(11):e19836. doi:10.2196/19836. [Google Scholar] [PubMed] [CrossRef]
19. Mcaleer S. E-learning and traditional approaches in psychotherapy education. Arch Psychiat Psych. 2015;17(4):48–52. doi:10.12740/APP/60644. [Google Scholar] [PubMed] [CrossRef]
20. Rief W. Moving from tradition-based to competence-based psychotherapy. BMJ Ment Health. 2021;24(3):115–20. [Google Scholar]
21. Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiat. 2017;16(3):287–98. doi:10.1002/wps.v16.3. [Google Scholar] [CrossRef]
22. Hrynyschyn R, Dockweiler C. Effectiveness of smartphone-based cognitive behavioral therapy among patients with major depression: systematic review of health implications. JMIR Mhealth Uhealth. 2021;9(2):e24703. doi:10.2196/24703. [Google Scholar] [PubMed] [CrossRef]
23. Linardon J, Torous J, Firth J, Cuijpers P, Messer M, Fuller-Tyszkiewicz M. Current evidence on the efficacy of mental health smartphone apps for symptoms of depression and anxiety. A meta-analysis of 176 randomized controlled trials. World Psychiat. 2024;23(1):139–49. doi:10.1002/wps.21183. [Google Scholar] [PubMed] [CrossRef]
24. Gillihan SJ. Cognitive behavioral therapy made simple: 10 strategies for managing anxiety, depression, anger, panic, and worry. Hachette, UK: Althea Press; 2020. [Google Scholar]
25. Group. PIaP. Handbook on physical and mental health of public security police in response to the epidemic. Police Station Work. 2020;8–16. [Google Scholar]
26. Beck JS. Cognitive therapy for challenging problems. New York, NY, USA: The Guilford Press; 2005. doi:10.1037/e679642007-001. [Google Scholar] [CrossRef]
27. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Mod Probl Pharmacopsychiatry. 1974;7(1):1–15. [Google Scholar]
28. Tong H. A 20-year study of the SCL-90 scale and its norm changes. Psychol Sci. 2010;33(4):928–30+1 (In Chinese). [Google Scholar]
29. Wei G. Mental health and role conflict among police officers: an empirical study of police officers in Fuzhou. J Chin People’s Public Secur Univ (Soc Sci Ed). 2011;27(3):108–12 (In Chinse). [Google Scholar]
30. Chen X, Zhang L, Peng Z, Chen S. Factors influencing the mental health of firefighters in Shantou City, China. Psychol Res Behav Manag. 2020;529–36. [Google Scholar]
31. Bonache JS, Costa BF, Hoshino MT, Ludwig L, de Oliveira MAB, Emerick GL. Occupational evaluation of federal highway police officers exposed to cholinesterase inhibiting insecticides. J Occup Environ Med. 2023;65(10):e660–7. doi:10.1097/JOM.0000000000002937. [Google Scholar] [PubMed] [CrossRef]
32. Preti A, Carta MG, Petretto DR. Factor structure models of the SCL-90-R: replicability across community samples of adolescents. Psychiat Res. 2019;27:491–8. [Google Scholar]
33. Gómez-Cambronero A, Casteleyn S, Bretón-López J, García-Palacios A, Mira A. A smartphone-based serious game for depressive symptoms: protocol for a pilot randomized controlled trial. Internet Interv. 2023;32:100624. doi:10.1016/j.invent.2023.100624. [Google Scholar] [PubMed] [CrossRef]
34. Castro O, Mair JL, Salamanca-Sanabria A, Alattas A, Keller R, Zheng SL, et al. Development of “LvL UP 1.0”: a smartphone-based, conversational agent-delivered holistic lifestyle intervention for the prevention of non-communicable diseases and common mental disorders. Front Digit Health. 2023;5:1039171. doi:10.3389/fdgth.2023.1039171. [Google Scholar] [PubMed] [CrossRef]
35. Santa Maria A, Wörfel F, Wolter C, Gusy B, Rotter M, Stark S, et al. The role of job demands and job resources in the development of emotional exhaustion, depression, and anxiety among police officers. Police Q. 2017;21(1):109–34. [Google Scholar]
36. Koppers D, Van H, Peen J, Alberts J, Dekker J. The influence of depressive symptoms on the effectiveness of a short-term group form of schema cognitive behavioural therapy for personality disorders: a naturalistic study. BMC Psychiat. 2020;20(1):271. doi:10.1186/s12888-020-02676-z. [Google Scholar] [PubMed] [CrossRef]
37. Auerbach RP, Srinivasan A, Kirshenbaum JS, Mann JJ, Shankman SA. Geolocation features differentiate healthy from remitted depressed adults. J Psychopathol Clin Sci. 2022;131(4):341–9. doi:10.1037/abn0000742. [Google Scholar] [PubMed] [CrossRef]
38. Lukas CA, Eskofier B, Berking M. A gamified smartphone-based intervention for depression: randomized controlled pilot trial. JMIR Ment Health. 2021;8(7):e16643. doi:10.2196/16643. [Google Scholar] [PubMed] [CrossRef]
39. Goldberg SB, Baldwin SA, Riordan KM, Torous J, Dahl CJ, Davidson RJ, et al. Alliance with an unguided smartphone app: validation of the digital working alliance inventory. Assessment. 2022;29(6):1331–45. doi:10.1177/10731911211015310. [Google Scholar] [PubMed] [CrossRef]
40. Zhang C, Liu YX, Guo XM, Liu YN, Shen Y, Ma J. Digital cognitive behavioral therapy for insomnia using a smartphone application in China a pilot randomized clinical trial. JAMA Netw Open. 2023;6(3):e234866. doi:10.1001/jamanetworkopen.2023.4866. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools