 Open Access
Open Access
ARTICLE
The Influence of Workplace Environment on Mental Health: A Quantitative and Qualitative Investigation in China
1 Department of Outpatient Office, Yongchuan Hospital of Chongqing Medical University, Chongqing, 402160, China
2 Department of Gastrointestinal Surgery, Central Hospital Affiliated to Shandong First Medical University, Jinan, 250113, China
3 Department of Nursing, Central Hospital Affiliated to Shandong First Medical University, Jinan, 250113, China
* Corresponding Author: Jiaqin Qi. Email:
International Journal of Mental Health Promotion 2024, 26(11), 957-966. https://doi.org/10.32604/ijmhp.2024.055468
Received 28 June 2024; Accepted 13 September 2024; Issue published 28 November 2024
Abstract
Background: The demanding nature of nursing, characterized by long hours, high-stress environments, and substantial workloads, can significantly impact nurses’ mental health. However, there are limited studies that assessed the influence of workplace environment on nursing mental health based on both quantitative and qualitative approaches. Methods: This study aims to comprehensively investigate the multidimensional relationship between the workplace environment and nurses’ well-being. This cross-sectional study was based on a sample of 3256 nurses from various healthcare settings in Shandong province, China (2022), who participated in the quantitative phase. For the qualitative phase, a subsample of participants from the quantitative phase was selected (n = 200) using purposive sampling to ensure diversity in terms of age, gender, years of experience, and healthcare settings. The mean age was 35.2 years, with 74% female participants. Results: Significant negative correlations were found between leadership support and mental distress, while workload showed negative associations with General Positive Affect and mental health functioning (p < 0.05). Multiple linear regression demonstrated the predictive power of workplace dimensions on mental health, with leadership support, teamwork, and organizational culture positively associated with mental health functioning (p < 0.05). Thematic analysis underscored the intricate interplay between workplace indicators and mental health dimensions, emphasizing the need for a holistic approach. Conclusion: This study reveals that key workplace factors, including leadership support, teamwork, and organizational culture, play a vital role in enhancing nurse mental health, which is essential for sustaining high-quality patient care and a resilient healthcare workforce.Keywords
The healthcare sector relies significantly on the dedicated and tireless work of nurses, who play an indispensable role in ensuring the well-being of patients [1]. The demands placed on nurses are immense, encompassing a range of responsibilities from delivering critical medical care to providing emotional support [2]. However, the demanding nature of the nursing profession, characterized by long hours, high-stress environments, substantial workloads, and often limited resources, can take a substantial toll on the mental health of nurses [3]. Nurses are pivotal to the healthcare system, acting as the primary caregivers and advocates for patients. Their roles extend beyond medical procedures to include offering comfort and emotional support, education, and acting as a bridge between patients and medical teams [4].
The nursing profession operates within a high-stress environment, frequently encountering emotionally charged situations, managing extended work hours, and often facing resource limitations [5]. These unique challenges can lead to stress, anxiety, depression, and other mental health issues among nurses. The mental well-being of nurses is intrinsically linked to the quality of patient care [6,7]. Stressed and mentally strained nurses may experience reduced job satisfaction, burnout, and decreased performance, ultimately influencing patient outcomes [8]. Hence, the mental health of nurses is of paramount importance for the overall quality of healthcare delivery [8,9].
While some research has explored the mental health of nurses [8,10–12], there is a notable gap in comprehensively understanding how workplace conditions contribute to their mental well-being. Existing studies have often focused on specific aspects or individual factors, providing a fragmented view of this complex issue. Therefore, a comprehensive investigation into the multidimensional relationship between the workplace environment and nurses’ mental health is warranted. This study holds immense significance on multiple fronts. Firstly, it plays a pivotal role in enhancing nurse well-being by delving into the precise workplace factors affecting their mental health. The insights gained from this research can pave the way for targeted interventions and policies, ultimately leading to an improvement in the overall welfare of nurses. Secondly, it directly impacts the quality of patient care [1,13]. A nursing workforce in sound mental health is better equipped to deliver high-quality care to patients [13]. Consequently, the study’s findings have the potential to create a positive ripple effect on patient outcomes. Lastly, the study contributes to the sustainability of the healthcare workforce. In an environment where nurse burnout and turnover rates are alarmingly high, the research lays the foundation for strategies that boost nurse job satisfaction and retention [14]. This, in turn, promotes the long-term sustainability of the nursing workforce, which is indispensable for the effective functioning of the healthcare system [14]. Therefore, this comprehensive study aimed to address a critical gap in the current understanding of nurses’ mental health by examining the complex relationship between the workplace environment and their well-being.
This comprehensive study was conducted in various healthcare settings, including public and private hospitals, clinics, and healthcare facilities, across Shandong province, China between February and September 2022. The study involved a purposive sample of registered nurses employed across different healthcare facilities. To ensure the representation of various healthcare sectors, participants were recruited from public and private hospitals, clinics, and primary care centers. Inclusion criteria encompassed registered nurses actively practicing within the healthcare system, irrespective of their specialization or clinical area, having at least 5 years of work experience, having regular work shifts during the month and not having a record of chronic physical and mental diseases. Recruitment efforts were carried out through collaboration with nursing associations, nursing boards, and healthcare institutions. Information about the study was disseminated via email, nursing forums, and direct communication with nursing managers and administrators. Finally, 3256 nurses agreed to participate in our study and signed the consent form.
For the qualitative phase, a subsample of participants was selected (n = 200) using purposive sampling to ensure diversity in terms of age, gender, years of experience, and healthcare settings. These participants were invited to participate in semi-structured interviews, scheduled at their convenience. The study was approved by Yongchuan Hospital of Chongqing Medical University Ethics committee at the University Chongqing Medical University (IRB number: J-YL.20230104). All participants signed the informed consent in this study.
Workplace environment assessment (WES)
The WES is used in the quantitative phase and consists of 30 items that assess different dimensions of the workplace environment. While the traditional WES by Moos and Insel in 1986 focuses on broader dimensions, we used a version tailored to our study’s needs [15]. Nurses were asked to rate their level of agreement with statements using a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The WES covers various aspects, including leadership support [16], nurse-physician relationships [17], workload [18], teamwork [19], and organizational culture [20]. This validated instrument has been widely utilized in nursing research to evaluate nurses’ perceptions of their work environment. It provides a comprehensive assessment of workplace conditions that can impact nurses’ job satisfaction and mental well-being. In the present study, the reliability coefficient of the WES scale based on Cronbach’s alpha method was 0.89, which indicated the optimal reliability of the scale.
Mental health assessment (MHI)
The MHI is a self-report questionnaire used to assess nurses’ mental health status. It consists of 38 items that inquire about psychological distress, Psychological Well-Being, and overall mental health functioning (i.e.). Participants rate their feelings and experiences over the past month using a Likert scale, with options such as “all of the time,” “most of the time,” “some of the time,” “a little of the time,” and “none of the time.” The MHI covers various domains, including Psychological Distress, Psychological Well-Being, Mental Health Functioning, Anxiety, Depression, General Positive Affect, and Loss of Behavioral/Emotional Control. The term ‘Mental Health Functioning’ was calculated as a composite measure, which includes General Positive Affect, Anxiety, Depression, and potentially Loss of Behavioral/Emotional Control [21–23]. It has demonstrated reliability and validity in measuring mental health outcomes in previous research studies. The Cronbach’s alpha for MHI scale was 0.85 indicating the optimal reliability of the scale.
The quantitative data collection process involved the following steps: (i) Recruitment: Participants were invited to participate in the study through various channels, including email invitations, announcements in nursing associations, and direct communication with healthcare institutions. (ii) Informed Consent: Participants who expressed interest in the study were provided with detailed information about the research on General Positive Affect, including its purpose, procedures, and confidentiality measures. Informed consent was obtained electronically from those willing to participate. (iii) Online Survey: Participants were directed to an online survey platform where they completed the quantitative portion of the study. The survey included the WES and MHI questionnaires. Participants were encouraged to respond honestly and thoughtfully to ensure data accuracy. (iv) Data Storage: All data collected through the online survey were stored securely on a password-protected server. Measures were taken to ensure the confidentiality and anonymity of participants.
Semi-Structured Interviews: The qualitative phase involved conducting semi-structured interviews with a subset of participants selected through purposive sampling. The interview guide was designed to explore nurses’ perceptions and experiences related to their workplace environment and its potential impact on their mental health.
The qualitative data collection process included the following steps: (i) Selection of Participants: A diverse group of nurses was selected for interviews to capture a wide range of perspectives. Participants were chosen based on age, gender, years of experience, and healthcare setting. (ii) Informed Consent: Participants selected for interviews were provided with detailed information about the interview process and its objectives. Informed consent was obtained from each participant before scheduling interviews. (iii) Semi-Structured Interviews: Interviews were conducted via video calls or in-person, depending on participants’ preferences and logistical considerations. The semi-structured format allowed for open-ended questioning, enabling participants to share their experiences and insights in-depth. (iv) Audio Recording and Transcription: All interviews were audio-recorded with participants’ consent. The recordings were transcribed verbatim to facilitate qualitative data analysis. (v) Data Analysis: Thematic analysis was employed to analyze qualitative data. Two researchers independently reviewed and coded the interview transcripts to identify recurring themes and patterns in nurses’ narratives.
The combination of quantitative survey responses and qualitative interview insights allowed for a comprehensive exploration of the relationship between the workplace environment and nurses’ mental health. Triangulation of data from both phases enhanced the study’s validity and provided a richer understanding of the topic.
Quantitative data were analyzed using STATA statistical software version 17.0. A significant level of 0.05 was applied for all statistical analyses. Descriptive statistics, including means, standard deviations, and frequencies, were used to characterize the participants and summarize quantitative variables. Bivariate analyses, such as correlation and multiple linear regression, were employed to explore relationships between workplace environment factors and mental health outcomes. The regression models adjusted for a priori selected covariates including age (years); gender (Female, Male), years of experience (continuous), healthcare setting (Public, Private, Clinic), employment type (Full-time, Part-time), education level (Bachelor, Master, Doctorate), work shift (Day Shift, Night Shift, Rotating Shift), marital status (Single, Married, Divorced/Separated, Widowed), number of children (None, 1 Child, 2 Children). In the correlation analysis between Workplace Environment Assessment and Mental Health Assessment indices (Fig. 1), bold red represents a strong negative correlation between the variables. As the correlation weakens, the color transitions to a lighter red. Yellow indicates a weak positive correlation, which shifts toward green as the correlation strength increases. The darker the green, the stronger the positive correlation.

Figure 1: Correlation matrix of workplace environment assessment and mental health assessment indices.
Qualitative data from interviews were analyzed using thematic analysis. Transcripts were coded independently by two researchers to identify recurrent themes and patterns related to nurses’ perceptions of their workplace environment and its impact on their mental health. The mixed-methods approach involved merging quantitative and qualitative data to provide a comprehensive understanding of the relationship between workplace environment and nurses’ mental health. Triangulation of findings from both data sources enhanced the study’s validity and comprehensiveness.
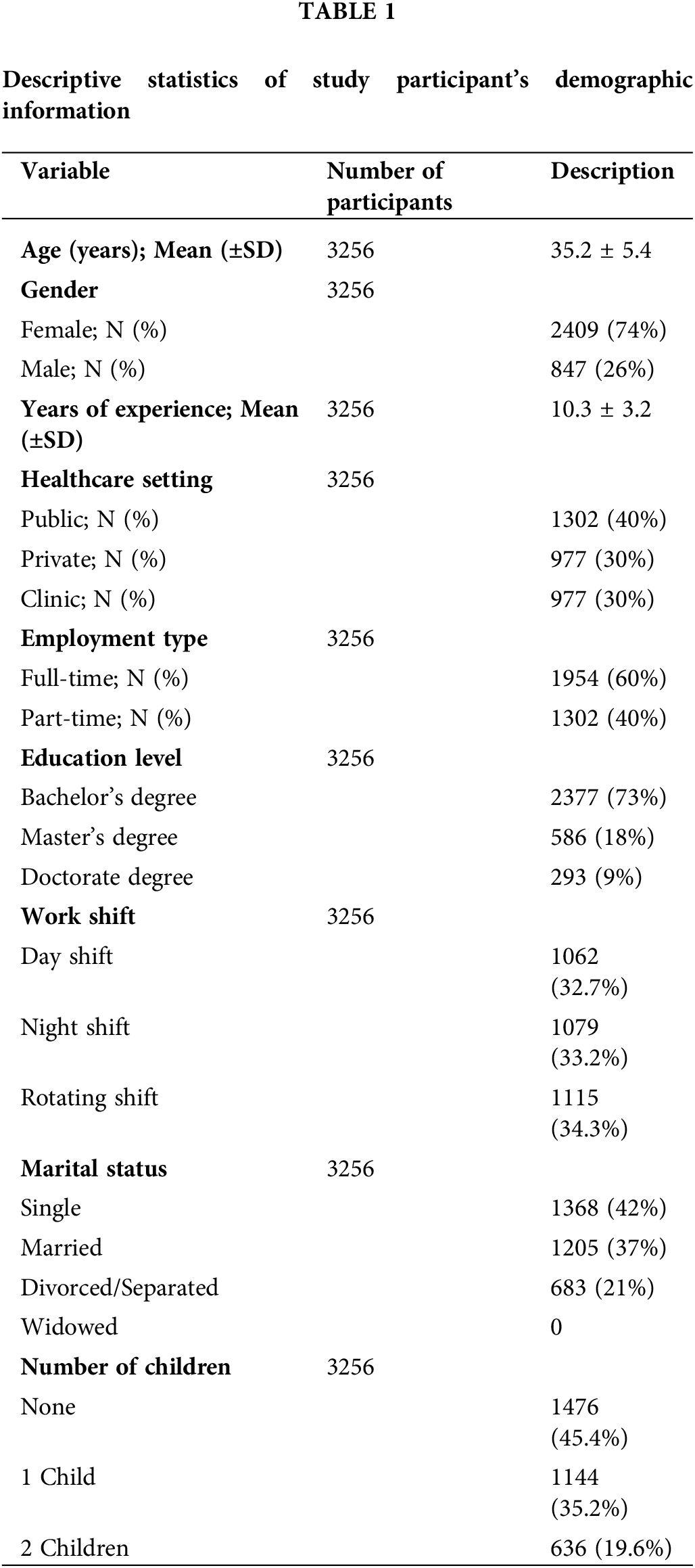
Table 1 summarizes the demographic and employment characteristics of the study participants. The data reveal a diverse sample in terms of age, gender, work experience, and employment settings. The distribution of educational levels, work shifts, and marital status highlights the varied backgrounds of the participants. This overview offers a foundation for understanding the relationships between these characteristics and the workplace and mental health aspects explored in the study. Specific values for these characteristics can be found in Table 1.
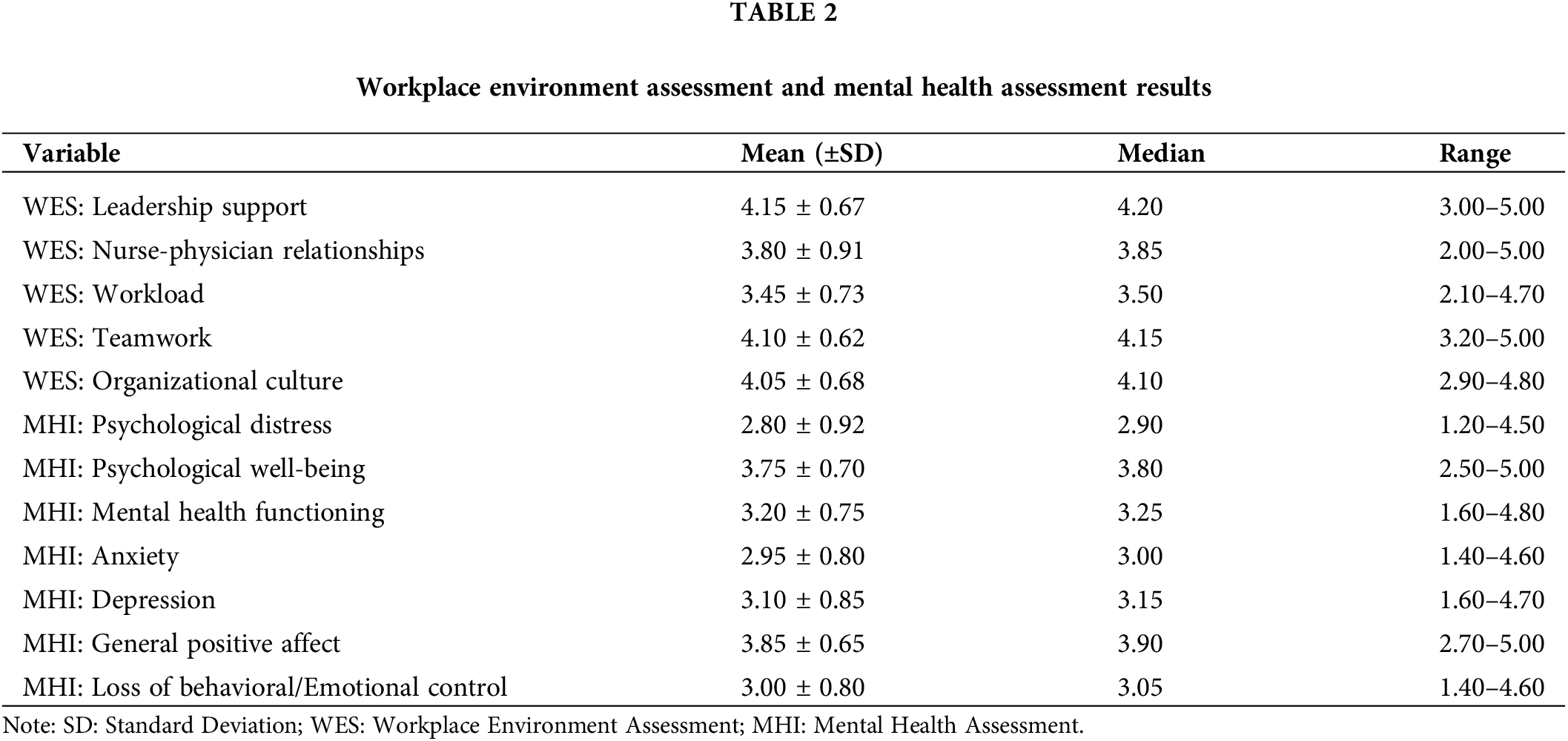
Descriptive statistics for the Workplace Environment Scale and Mental Health Inventory scores are presented in Table 2. For WES, the mean scores (± standard deviation) range from 3.45 to 4.15, indicating nurses’ varying perceptions across dimensions such as leadership support, nurse-physician relationships, workload, teamwork, and organizational culture. In contrast, the MHI data show a range of mean scores from 2.80 to 3.85, reflecting assessments of psychological distress, Psychological Well-Being, and overall mental health functioning. The nurses’ responses reveal a spectrum of experiences, from moderate to high levels, across these diverse domains.
Bivariate analysis (Fig. 1) revealed significant correlations between certain workplace environment dimensions and mental health outcomes. Specifically, “leadership support” showed a strong negative correlation with “Loss of Behavioral/Emotional Control” (r = –0.6) and “anxiety” (r = −0.55) and moderate negative correlation with “psychological distress” (r = −0.45) and “depression” (r = −0.4). Conversely, “Workload” exhibited a strong negative correlation with “General Positive Affect” (r = −0.65) and “mental health function” (r = −0.75), suggesting that higher perceived workload was associated with lower mental health scores. Furthermore, “teamwork” and “organizational culture” were strongly correlated with lower “anxiety”, “depression” and “Loss of Behavioral/Emotional Control” scores.
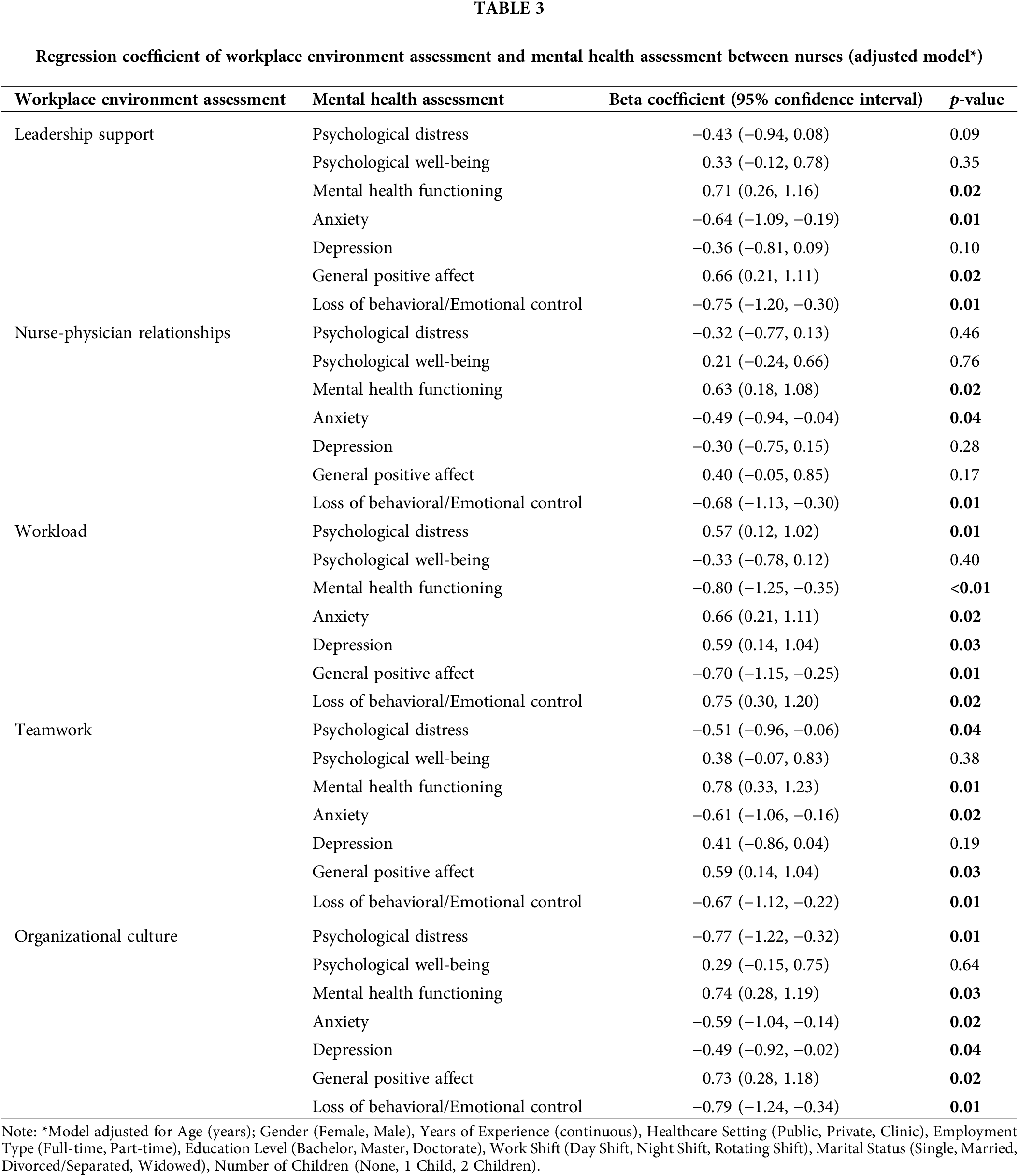
Multiple linear regression (Table 3) was conducted to examine the predictive power of workplace environment dimensions on mental health outcomes while controlling for covariates. In the fully adjusted model, there was a significant positive association between WES indices including “leadership support”, “Nurse-Physician Relationships”, “Teamwork” and “Organizational Culture” with “Mental Health Functioning”. Moreover, these indices were negatively associated with “Anxiety” and “Loss of Behavioral/Emotional Control” in nurses. There was a negative significant association between “workload” with “Mental Health Functioning” (β = −0.80, 95% confidence interval (CI): −1.25, −0.35, p-value < 0.01) and “Positive Affect” (β = −0.70, 95% CI: −1.15, −0.25, p-value = 0.01). Furthermore, “workload” was positively associated with “Psychological Distress”, “Anxiety”, “Depression” and “Loss of Behavioral/Emotional Control” (Table 3).
The thematic analysis of nurses’ perceptions of the workplace environment and mental health revealed several key insights, each playing a significant role in shaping their well-being. Leadership support emerged as critical, with nurses emphasizing the importance of accessible and supportive managers in reducing psychological distress. Clear communication and guidance from leadership not only provided stability but also fostered a sense of security and trust, directly contributing to lower anxiety and depression. This finding underscores the direct correlation between leadership style and mental health, suggesting that enhancing leadership practices could mitigate workplace mental health issues. Nurse-physician relationships also played a vital role, with effective communication and mutual respect closely linked to lower anxiety and depression levels. The quality of interprofessional relationships was found to have a significant impact on mental health, indicating that improving communication and collaboration across disciplines could enhance overall well-being. Workload was identified as a primary stressor with direct implications for mental health, as excessive workloads, particularly when coupled with challenges in maintaining a healthy work-life balance, led to heightened stress and a decline in mental health. This theme highlights the importance of workload management and work-life balance in maintaining mental health, suggesting that organizational interventions aimed at reducing workload or improving work-life balance could be effective strategies. Positive teamwork and collaboration were recognized as protective factors, with strong teamwork providing support and reducing feelings of isolation, thereby contributing to Psychological Well-Being. This finding emphasizes the need for initiatives that promote a collaborative team culture in healthcare settings. Finally, the study found that organizational culture, characterized by supportive values and inclusive practices, significantly shaped nurses’ mental health. A positive organizational culture contributed to Psychological Well-Being and reduced levels of anxiety and depression, suggesting that organizations should prioritize cultivating a supportive and inclusive culture to support staff mental health. Overall, the thematic analysis emphasized the intricate interplay between these workplace indicators and mental health dimensions, indicating that a holistic approach addressing leadership, interprofessional relationships, workload, teamwork, and organizational culture is essential for enhancing nurses’ well-being in healthcare settings.
This study contributes valuable insights into the relationship between the workplace environment and the mental health of nurses, addressing a critical aspect of healthcare that has substantial implications for both professionals and patient outcomes. The comprehensive analysis of demographic and employment characteristics provides a nuanced understanding of the study population, setting the stage for a detailed exploration of workplace and mental health aspects. Notably, the quantitative phase reveals varying perceptions among nurses across dimensions such as leadership support, nurse-physician relationships, workload, teamwork, and organizational culture. The negative correlations between specific workplace environment dimensions, such as leadership support, workload, and mental health outcomes shed light on critical associations. Furthermore, the qualitative phase uncovers the lived experiences of nurses, emphasizing the pivotal role of accessible and supportive leadership, positive nurse-physician relationships, and collaborative teamwork as protective factors for mental well-being. The interplay between these workplace indicators and mental health dimensions underscores the need for a holistic approach in addressing nurses’ well-being.
Comparisons with previous studies
Our study findings bring into line with and extend existing research on the relationship between workplace environment and nurses mental health. Our quantitative results emphasize the significant impact of leadership support on mental health outcomes, underscoring the importance of managerial accessibility and clear communication in reducing psychological distress, which is consistent with previous evidence [24–28]. This resonates with findings from studies such as Sfantou et al., affirming the universal relevance of supportive leadership in healthcare settings [29]. Furthermore, our results of strong negative correlations between workload and General Positive Affect, mental health functioning, and other mental health dimensions add granularity to the literature [30–32]. While previous studies have acknowledged the strain of high workload on nurses, our study illuminates specific dimensions of mental health, contributing novel insights [10]. This aligns with research by Ruggeri et al. [33], but our study goes beyond by examining diverse mental health indicators within a single comprehensive analysis.
The qualitative phase of our study underscores the importance of positive nurse-physician relationships and collaborative teamwork, reinforcing the findings of previous studies [4,34,35]. Effective communication and mutual respect among healthcare professionals have been recognized as essential factors for a harmonious work environment and reduced anxiety and depression among nurses [36]. However, our study extends this understanding by providing nuanced insights into the lived experiences of nurses, emphasizing the multifaceted nature of these relationships in influencing mental well-being [4,34,35].
The negative association between certain workplace dimensions (e.g., leadership support, teamwork, organizational culture) and mental health outcomes makes it straight with previous studies emphasizing the protective role of positive workplace characteristics [37]. Our findings are consistent with the findings of studies such as Paganin et al., but our study contributes by incorporating multiple workplace dimensions simultaneously, providing a more comprehensive understanding of their collective impact on mental health [38,39].
The findings of this study align with and underscore the importance of China’s national initiatives aimed at improving mental health and workforce well-being. China’s National Mental Health Work Plan (2015–2020), along with the Healthy China 2030 blueprint, emphasizes the need to address mental health issues across various sectors, including healthcare [40,41]. These initiatives recognize the critical role of mental health in overall well-being and productivity, particularly among healthcare professionals who are at the frontline of patient care. The study’s results, which highlight significant correlations between workplace environment dimensions and mental health outcomes, resonate with the objectives of China’s national plans. The National Mental Health Work Plan advocates for comprehensive mental health services, which include preventive measures and the promotion of mental health in workplaces [42]. This aligns with our findings that leadership support and positive teamwork are protective factors against mental health challenges. Moreover, the emphasis on reducing workload and improving work-life balance in our study echoes the goals outlined in China’s efforts to improve the work environment and mental health of healthcare workers [43,44]. The National Health Commission’s policies on enhancing the mental well-being of healthcare professionals underscore the need for supportive organizational cultures, which our study also identifies as crucial for reducing anxiety and depression among nurses [45,46].
The biological mechanisms underlying the relationship between the workplace environment and nurses’ mental health are complex and multifaceted. Chronic stress resulting from high workloads and inadequate support systems can lead to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, contributing to conditions like anxiety and depression [47,48]. Moreover, a negative workplace environment may hinder the release of oxytocin, a neuropeptide associated with social bonding and stress reduction [49,50]. Furthermore, the inflammatory response in the body may be triggered by chronic stress, potentially leading to conditions like cardiovascular disease [51,52]. Additionally, the sleep patterns of nurses can be severely disrupted due to irregular shifts and high-stress levels, which can further exacerbate mental health issues [53]. These biological mechanisms emphasize the need for multifaceted interventions that address not only the workplace environment but also individual coping strategies and support systems.
Limitations and future recommendations
Despite the valuable insights gained, this study has limitations. The cross-sectional design limits causal inference, and future longitudinal research could provide a more robust understanding of the dynamic relationship between workplace environment and mental health over time. Additionally, the reliance on self-reported data may introduce response biases, and objective measures or observational data could enhance the study’s validity. The study’s generalizability may be influenced by the specific demographic and employment characteristics of the sample, and future research should aim for diverse and representative samples. Finally, interventions targeting specific workplace dimensions should be explored to assess their effectiveness in improving nurses’ mental health. Future studies could employ experimental designs to evaluate the impact of workplace interventions on both subjective and objective mental health outcomes.
Our study offers a comprehensive exploration of the complex interplay between the workplace environment and nurses mental health, shedding light on critical dimensions that influence the well-being of healthcare professionals. The thorough examination of demographic and employment characteristics establishes a robust foundation for understanding the nuanced experiences of nurses. The quantitative phase reveals diverse perceptions across dimensions such as leadership support, nurse-physician relationships, workload, teamwork, and organizational culture, illustrating the multifaceted nature of their workplace experiences. The negative correlations between specific workplace dimensions and mental health outcomes provide valuable insights into potential areas for targeted interventions. Moreover, the qualitative phase adds depth by uncovering the lived experiences of nurses, emphasizing the pivotal role of accessible leadership, positive nurse-physician relationships, and collaborative teamwork as protective factors for mental well-being. By comparing our findings with existing literature, we affirm and extend established knowledge, offering nuanced insights into the relationship between workplace environment and mental health. Overall, this study contributes a holistic understanding of the challenges and strengths within the healthcare workplace, emphasizing the need for comprehensive interventions to enhance the mental health of nurses and, subsequently, the quality of patient care.
Acknowledgement: We would like to express our sincere gratitude to the nurses who generously shared their experiences, the healthcare institutions for their support, and the research team members for their dedication.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: All authors contributed significantly to the development of this study. Zulian Zhang was responsible for the conceptualization, methodology, formal analysis, and drafting of the original manuscript. Meiyu Yan contributed to data curation, investigation, and provided critical revisions during the review and editing process. Jiaqin Qi supervised the project, managed its administration, and also contributed to the review and editing of the manuscript. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data of this study will be available on request from the corresponding author.
Ethics Approval: The study was approved by Yongchuan Hospital of Chongqing Medical University Ethics Committee at the University Chongqing Medical University (IRB number: J-YL.20230104). All participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Stelnicki AM, Carleton RN, Reichert C. Nurses’ mental health and well-being: COVID-19 impacts. Can J Nurs Res. 2020;52(3):237–9. doi:10.1177/0844562120931623. [Google Scholar] [PubMed] [CrossRef]
2. Sekse RJT, Hunskår I, Ellingsen S. The nurse’s role in palliative care: a qualitative meta-synthesis. J Clin Nurs. 2018;27(1–2):e21–38. doi:10.1111/jocn.13912. [Google Scholar] [PubMed] [CrossRef]
3. Kinman G, Teoh K, Harriss A. The mental health and wellbeing of nurses and midwives in the United Kingdom. 2020. Available from: https://eprints.bbk.ac.uk/id/eprint/40551/1/2020%20-%20The%20Mental%20Health%20and%20Wellbeing%20of%20Nurses%20and%20Midwives%20in%20the%20United%20Kingdom.pdf. [Accessed 2024]. [Google Scholar]
4. Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021;20(1):158. doi:10.1186/s12912-021-00684-2. [Google Scholar] [PubMed] [CrossRef]
5. McGrath A, Reid N, Boore J. Occupational stress in nursing. Int J Nurs Stud. 2003;40(5):555–65. doi:10.1016/S0020-7489(03)00058-0. [Google Scholar] [PubMed] [CrossRef]
6. Kaushik A, Ravikiran SR, Suprasanna K, Nayak MG, Baliga K, Acharya SD. Depression, anxiety, stress and workplace stressors among nurses in tertiary health care settings. Indian J Occup Environ Med. 2021;25(1):27–32. doi:10.4103/ijoem.IJOEM_123_20. [Google Scholar] [PubMed] [CrossRef]
7. Babapour A-R, Gahassab-Mozaffari N, Fathnezhad-Kazemi A. Nurses’ job stress and its impact on quality of life and caring behaviors: a cross-sectional study. BMC Nurs. 2022;21(1):75. doi:10.1186/s12912-022-00852-y. [Google Scholar] [PubMed] [CrossRef]
8. Khamisa N, Peltzer K, Ilic D, Oldenburg B. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. 2015;12(1):652–66. doi:10.3390/ijerph120100652. [Google Scholar] [PubMed] [CrossRef]
9. Mudallal RH, Othman WM, Al Hassan NF. Nurses’ burnout: the influence of leader empowering behaviors, work conditions, and demographic traits. Inquiry. 2017;54:46958017724944. doi:10.1177/0046958017724944. [Google Scholar] [PubMed] [CrossRef]
10. Nagel C, Nilsson K. Nurses’ work-related mental health in 2017 and 2020–a comparative follow-up study before and during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(23):15569. doi:10.3390/ijerph192315569. [Google Scholar] [PubMed] [CrossRef]
11. Ito A, Sasaki M, Yonekura Y, Ogata Y. Impact of organizational justice and manager’s mental health on staff nurses’ affective commitment: a multilevel analysis of the work environment of hospital nurses in Japan-Part II (WENS-J-II). Int J Nurs Stud Adv. 2023;5:100137. doi:10.1016/j.ijnsa.2023.100137. [Google Scholar] [PubMed] [CrossRef]
12. Havaei F, Ma A, Staempfli S, MacPhee M. Nurses’ workplace conditions impacting their mental health during COVID-19: a cross-sectional survey study. Healthcare. 2021;9(1):84. doi:10.3390/healthcare9010084. [Google Scholar] [PubMed] [CrossRef]
13. Hurley J, Lakeman R, Linsley P, Ramsay M, Mckenna-Lawson S. Utilizing the mental health nursing workforce: a scoping review of mental health nursing clinical roles and identities. Int J Ment Health Nurs. 2022;31(4):796–822. doi:10.1111/inm.v31.4. [Google Scholar] [CrossRef]
14. Al Sabei SD, Labrague LJ, Miner Ross A, Karkada S, Albashayreh A, Masroori Al, et al. Nursing work environment, turnover intention, job burnout, and quality of care: the moderating role of job satisfaction. J Nurs Scholarsh. 2020;52(1):95–104. doi:10.1111/jnu.v52.1. [Google Scholar] [CrossRef]
15. Moos RH. Work environment scale manual. Consulting Psychologists Press; 1986. [Google Scholar]
16. Laschinger HKS, Wong CA, Greco P. The impact of staff nurse empowerment on person-job fit and work engagement/burnout. Nurs Adm Q. 2006;30(4):358–67. doi:10.1097/00006216-200610000-00008. [Google Scholar] [PubMed] [CrossRef]
17. Borkowski N, Meese KA. Organizational behavior in health care. Jones & Bartlett Learning; 2020. [Google Scholar]
18. Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93. doi:10.1001/jama.288.16.1987. [Google Scholar] [PubMed] [CrossRef]
19. King HB, Battles J, Baker DP, Alonso A, Salas E, Webster J, et al. TeamSTEPPS™: team strategies and tools to enhance performance and patient safety. In: Henriksen K. et al. editors. Advances in patient safety: new directions and alternative approaches (vol. 3: performance and toolsRockville, MD, USA: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
20. Schein EH. Organizational culture and leadership. Hoboken, NJ, USA: John Wiley & Sons; 2010. vol. 2. [Google Scholar]
21. Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. J Consult Clin Psychol. 1983;51(5):730. doi:10.1037/0022-006X.51.5.730. [Google Scholar] [PubMed] [CrossRef]
22. Larson JS. The MOS 36-item short form health survey: a conceptual analysis. Evaluat Health Profess. 1997;20(1):14–27. doi:10.1177/016327879702000102. [Google Scholar] [PubMed] [CrossRef]
23. Hendryx MS, Ahern MM. Mental health functioning and community problems. J Community Psychol. 1997;25(2):147–57. doi:10.1002/(ISSN)1520-6629. [Google Scholar] [CrossRef]
24. Dextras-Gauthier J, Gilbert MH, Dima J, Adou LB. Organizational culture and leadership behaviors: is manager’s psychological health the missing piece? Front Psychol. 2023;14:1237775. doi:10.3389/fpsyg.2023.1237775. [Google Scholar] [PubMed] [CrossRef]
25. Volpi L, Giusino D, Pietrantoni L, De Angelis M. Does organizational commitment to mental health affect team processes? a longitudinal study. J Healthc Leadersh. 2023;15:339–53. doi:10.2147/JHL.S429232. [Google Scholar] [PubMed] [CrossRef]
26. Kelly RJ, Hearld LR. Burnout and leadership style in behavioral health care: a literature review. J Behav Health Serv Res. 2020;47(4):581–600. doi:10.1007/s11414-019-09679-z. [Google Scholar] [PubMed] [CrossRef]
27. Farahnak LR, Ehrhart MG, Torres EM, Aarons GA. The influence of transformational leadership and leader attitudes on subordinate attitudes and implementation success. J Leadership Organizat Stud. 2020;27(1):98–111. doi:10.1177/1548051818824529. [Google Scholar] [CrossRef]
28. Chen X, Masukujjaman M, Al Mamun AGao J, Makhbul KMZ. Modeling the significance of work culture on burnout, satisfaction, and psychological distress among the Gen-Z workforce in an emerging country. Human Soc Sci Commun. 2023;10(1):828. doi:10.1057/s41599-023-02371-w. [Google Scholar] [CrossRef]
29. Sfantou DF, Laliotis A, Patelarou AE, Sifaki-Pistolla D, Matalliotakis M, Patelarou E. Importance of leadership style towards quality of care measures in healthcare settings: a systematic review. Healthcare. 2017;5(4):73. doi:10.3390/healthcare5040073. [Google Scholar] [PubMed] [CrossRef]
30. Hoobler JM, Rospenda KM, Lemmon G, Rosa JA. A within-subject longitudinal study of the effects of positive job experiences and generalized workplace harassment on well-being. J Occup Health Psychol. 2010;15(4):434–51. doi:10.1037/a0021000. [Google Scholar] [PubMed] [CrossRef]
31. Lingard H, Turner M. Measuring sense of place in project environments to promote positive mental wellbeing. Int J Proj Manag. 2023;41(6):102503. doi:10.1016/j.ijproman.2023.102503. [Google Scholar] [CrossRef]
32. Xi N, Chen J, Gama F, Riar M, Hamari J. The challenges of entering the metaverse: an experiment on the effect of extended reality on workload. Inf Syst Front. 2023;25(2):659–80. [Google Scholar] [PubMed]
33. Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18(1):192. doi:10.1186/s12955-020-01423-y. [Google Scholar] [PubMed] [CrossRef]
34. Rogers L, De Brún A, McAuliffe E. Exploring healthcare staff narratives to gain an in-depth understanding of changing multidisciplinary team power dynamics during the COVID-19 pandemic. BMC Health Serv Res. 2023;23(1):419. doi:10.1186/s12913-023-09406-7. [Google Scholar] [PubMed] [CrossRef]
35. Farhadie A, Elahi N, Jalali R. Nurses’ and physicians’ experiences of the pattern of their professional relationship with each other: a phenomenological study. J Qualit Res Health Sci. 2017;6(2):201–13. [Google Scholar]
36. Rosen MA, DiazGranados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, et al. Teamwork in healthcare: key discoveries enabling safer, high-quality care. Am Psychol. 2018;73(4):433–50. doi:10.1037/amp0000298. [Google Scholar] [PubMed] [CrossRef]
37. Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open. 2017;7(11):e017708. doi:10.1136/bmjopen-2017-017708. [Google Scholar] [PubMed] [CrossRef]
38. Peng X. Advancing workplace civility: a systematic review and meta-analysis of definitions, measurements, and associated factors. Front Psychol. 2023;14:1277188. [Google Scholar] [PubMed]
39. Paganin G, De Angelis M, Pische E, Violante FS, Guglielmi D, Pietrantoni L. The impact of mental health leadership on teamwork in healthcare organizations: a serial mediation study. Sustainability. 2023;15(9):7337. doi:10.3390/su15097337. [Google Scholar] [CrossRef]
40. Xiong W, Phillips MR. Translated and annotated version of the 2015–2020 national mental health work plan of the people’s Republic of China. Shanghai Arch Psychiatr. 2016;28(1):4–17. doi:10.11919/j.issn.1002-0829.216012. [Google Scholar] [PubMed] [CrossRef]
41. 2030 planning outline. Beijing: China State Council; 2016. [Google Scholar]
42. Xiao Y, Chen TT, Du N. Challenges facing China’s mental health services in the context of COVID-19. Gen Hosp Psychiatry. 2022;79(2):191–2. doi:10.1016/j.genhosppsych.2022.10.007. [Google Scholar] [PubMed] [CrossRef]
43. Liang D, Mays VM, Hwang WC. Integrated mental health services in China: challenges and planning for the future. Health Policy Plan. 2018;33(1):107–22. doi:10.1093/heapol/czx137. [Google Scholar] [PubMed] [CrossRef]
44. Tang N, Thomson LE. Workplace violence in Chinese hospitals: the effects of healthcare disturbance on the psychological well-being of Chinese healthcare workers. Int J Environ Res Public Health. 2019;16(19):3687. doi:10.3390/ijerph16193687. [Google Scholar] [PubMed] [CrossRef]
45. Shi Y, Xue H, Ma Y, Wang L, Gao T, Shi L, et al. Prevalence of occupational exposure and its influence on job satisfaction among Chinese healthcare workers: a large-sample, cross-sectional study. BMJ Open. 2020;10(4):e031953. doi:10.1136/bmjopen-2019-031953. [Google Scholar] [PubMed] [CrossRef]
46. Guo Y, Hu S, Liang F. The prevalence and stressors of job burnout among medical staff in Liaoning, China: a cross-section study. BMC Public Health. 2021;21(1):777. doi:10.1186/s12889-021-10535-z. [Google Scholar] [PubMed] [CrossRef]
47. Koinis A, Giannou V, Drantaki V, Angelaina S, Stratou E, Saridi M. The impact of healthcare workers job environment on their mental-emotional health. coping strategies: the case of a local general hospital. Health Psychol Res. 2015;3(1):1984. doi:10.4081/hpr.2015.1984. [Google Scholar] [PubMed] [CrossRef]
48. Coelho D, Yamaguchi S, Harb A, Souza-Talarico JN. Effort-reward and overcommitment at work and psychiatric symptoms in healthcare professionals: the mediation role of allostatic load. Compreh Psychoneuroendocrinol. 2024;17:100225. [Google Scholar]
49. Takayanagi Y, Onaka T. Roles of oxytocin in stress responses, allostasis and resilience. Int J Mol Sci. 2021;23(1):150. doi:10.3390/ijms23010150. [Google Scholar] [PubMed] [CrossRef]
50. Gordon I, Martin C, Feldman R, Leckman JF. Oxytocin and social motivation. Dev Cogn Neurosci. 2011;1:471–93. doi:10.1016/j.dcn.2011.07.007. [Google Scholar] [PubMed] [CrossRef]
51. Liu YZ, Wang YX, Jiang CL. Inflammation: the common pathway of stress-related diseases. Front Hum Neurosci. 2017;11:316. doi:10.3389/fnhum.2017.00316. [Google Scholar] [PubMed] [CrossRef]
52. Lagraauw HM, Kuiper J, Bot I. Acute and chronic psychological stress as risk factors for cardiovascular disease: insights gained from epidemiological, clinical and experimental studies. Brain Behav Immun. 2015;50:18–30. doi:10.1016/j.bbi.2015.08.007. [Google Scholar] [PubMed] [CrossRef]
53. Al-Hrinat J, Al-Ansi AM, Hendi A, Adwan G, Hazaimeh M. The impact of night shift stress and sleep disturbance on nurses quality of life: case in Palestine Red Crescent and Al-Ahli Hospital. BMC Nurs. 2024;23(1):24. doi:10.1186/s12912-023-01673-3. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools