 Open Access
Open Access
ARTICLE
Relation between Interparental Conflict and Non-Suicidal Self-Injury in Adolescents: Mediating Role of Alexithymia and Moderating Role of Resilience
College of Educational Science, Shenyang Normal University, Shenyang, 110034, China
* Corresponding Author: Ye Zhang. Email:
(This article belongs to the Special Issue: Exploring anxiety, stress, depression, addictions, executive functions, mental health, and other psychological and socio-emotional variables: psychological well-being and suicide prevention perspectives)
International Journal of Mental Health Promotion 2024, 26(10), 837-846. https://doi.org/10.32604/ijmhp.2024.053586
Received 05 May 2024; Accepted 10 August 2024; Issue published 31 October 2024
Abstract
Background: Adolescents frequently engage in Non-Suicidal Self-Injury (NSSI), with recent trends indicating an increase in this behavior. At the same time, Chinese adolescents have a higher incidence of NSSI than Western adolescents. Therefore, it is necessary to explore the relationship between interparental conflict and NSSI among adolescents within the context of Chinese families. Methods: The research sample comprised 755 senior high school students (46.62% male; age M = 16.82, SD = 0.94 years) who completed the Interparental Conflict Child Perception Scale (CPIC), Adolescent Self-Injury Behavior Questionnaire (ASHS), Toronto Alexithymia Scale-20 (TAS-20), and Scale of Adolescent Resilience (RSCA). Results: Findings suggest that interparental conflict is a significant positive predictor of NSSI (r = 0.22, p < 0.01). Alexithymia mediates the relation between interparental conflict and NSSI (effect size = 0.09, 95% CI [0.05, 0.13]). Additionally, resilience moderates both the direct relation (β = −0.08, p < 0.05) and the latter half of the mediating pathway (β =−0.08, p < 0.05) in the moderated mediation model. Conclusion: This study indicates that interparental conflict have an impact on adolescents’ NSSI in Chinese families, and alexithymia and resilience play important roles in the relationship. These findings offer valuable guidance for the prevention and intervention efforts targeting NSSI among adolescents in China and in similar family contexts.Keywords
Non-suicidal self-injury (NSSI) involves the intentional and repeated damage to one’s own body without the purpose of ending one’s life [1]. This behavior not only inflicts immediate physical harm but also negatively affects social relationships because of its unhealthy nature [2]. Additionally, NSSI can be a precursor to future suicidal behaviors [3]. Adolescence, a period of profound physical and psychological transformation, is marked by heightened emotional volatility and a great tendency toward extreme actions [4]. A study indicates that in Western countries, the prevalence of NSSI in adolescents is usually between 17% and 31%, whereas in China, it is 27.4%, which is higher than the general level in Western countries [5]. Cultural variations, particularly the emphasis on collectivism in Chinese society vs. the individualism prevalent in Western cultures, lead to different familial structures and values. In China, the nuclear family maintains strong ties with the extended family, whereas Western societies tend to focus more on the autonomous nuclear family. Within Chinese families, the parent-child relationship is often the focal point, with children being regarded as the essence of the family’s continuity. Conversely, Western families typically prioritize the spousal relationship. As a result, the mental and physical health of Chinese adolescents is inextricably linked to their family environment. In recent years, the literature on NSSI among Chinese adolescents has increased dramatically, with most publications in local journals, highlighting a need for more articles with international influence in the future [5]. Therefore, exploring the generation and prevention mechanism of NSSI among Chinese adolescents is of great importance in promoting their physical and mental health. This study explores whether children’s perceived interparental conflict affects their NSSI, thereby providing feasible ideas for the prevention and radical treatment of NSSI starting from the Chinese family environment.
Interparental conflict and NSSI
Interparental conflict involves verbal or physical aggression between parents perceived by children within the family, often stemming from disagreements or other issues [6]. According to ecological system theory, the family, as the immediate environment for living and communication, is most closely connected to an individual [7]. It serves as not only a provider for the basic needs of human life and growth but also a foundation for emotional support, profoundly affecting the physical and psychological development of each family member [8]. A harmonious parental relationship is essential for cultivating positive psychological traits in adolescents [9]. The quality of the parental relationship directly influences the parents’ psychological state, which indirectly affects the development of their children. Parental marital conflict is a crucial factor contributing to emotional issues in adolescents [10]. The spill-over hypothesis suggests that when the conflict in the marital subsystem “spills over” into the parent-child subsystem, it disrupts the normal parent-child interaction patterns and leads to adaptive challenges for the children [11]. Interparental conflict diminishes the intimacy between children and parents [12] and introduces negative emotional experiences for children, which are predictive of NSSI in adolescence [13]. Children may resort to NSSI to alleviate or extinguish negative emotions and as an attempt to garner parental attention or seek assistance [14].
The environmental function model suggests that NSSI is a response to a complex interplay of situational triggers, emotional states, personal cognition, and the outcomes associated with NSSI [15]. Interparental conflict can create a family environment leading to negative emotional experiences for children, which are conducive to NSSI. Alexithymia is a personality construct marked by an inability to recognize and articulate emotions, a propensity for external processing, and a neglect of one’s inner world [16]. It may act as a negative cognitive influence driving individual toward NSSI. This trait complicates integrating and expressing negative emotions, leaving them disjointed and unexplained, thereby heightening cognitive distress [17]. Alexithymia is strongly linked to negative emotional issues such as anxiety and depression and is a critical risk factor for maladaptive behaviors [18]. High levels of alexithymia can lead to a spectrum of behavioral problems and hinder healthy adolescent development [19], including instances of aggression and NSSI [20–22]. Moreover, the emergence of alexithymia is shaped by multiple factors, including family dynamics, educational settings, cultural norms, and social interactions [23,24]. Adolescents who have endured traumatic experiences often exhibit high levels of alexithymia [25]. Prolonged exposure to interparental conflict can cause adolescents to internalize their parents’ negative emotional expressions, which can then influence the development of their self-esteem and emotional resilience [26]. Insecure parent-child relationships and strained marital bonds can compromise children’s ability to express themselves verbally and increase the likelihood of alexithymia [27].
The compensation model suggests that during stressful situations that impair an individual’s crisis cooping ability, personal characteristics and environmental resources can act as moderating factors, thereby preventing the crisis from having a catastrophic impact on the individual [28]. Given the variability of personality traits, when certain characteristics are detrimental to healthy development, other traits that positively influence an individual’s mental and physical health can offset these deficiencies. Resilience is a psychological ability that enables individuals to adjust their psychological states in time to cope with and overcome difficulties in the face of adverse internal and external factors [29]. It is a crucial moderating variable that can reduce the negative effects of risk factors on individuals [30]. Adolescents who lack parental care often experience instability in parent-child relationships, a low sense of security, and poor psychological adaptability [31,32]. In risky environments, resilience enables individuals to adjust their cognition and emotions efficiently, enhancing their ability to adapt [33]. Those with higher resilience exhibit less negative thinking [34] and a greater capacity for negative adaptation [35], correspondingly reducing problem behaviors [36]. Individuals with alexithymia struggle to regulate and integrate negative emotions or self-soothe, making them more susceptible to vulnerability. Those with severe alexithymia are at a higher risk of psychological disorders and engage in self-injury and suicide at a greater rate [37]. Resilience is a critical resource that enables individuals to emerge from traumatic experiences [38]. Individuals with low resilience are likely to develop mental disorders such as depression and anxiety and engage in NSSI [39–41].
Although the extensive literature on adolescent NSSI has consistently demonstrated that its occurrence is multifactorial, current research perspectives remain less comprehensive and can benefit from further elaboration. Firstly, empirical evidence generally supports the notion that interparental conflict positively predicts NSSI among adolescents. Adolescents are often portrayed as passive participants in this dynamic who are powerless to change. Adolescents possess relatively sophisticated cognitive abilities akin to adults, making them acutely sensitive to interparental discord. Before the NSSI occurred, they made corresponding psychological efforts to avoid hurting themselves. Secondly, researches have predominantly focused on the familial environment, neglecting the broader societal context. Within the collectivist culture of Chinese families, the familial unit is only one part of a larger social fabric. The societal responsibilities and norms that distinguish Chinese and Western family dynamics suggest that the implications of varying social contexts on adolescent NSSI have not been adequately explored.
This study offers two primary contributions to the field. First, this study emphasizes the subjective efforts that individuals make to become resilient. Confronted with life’s inevitable challenges and setbacks, an individual’s psychological makeup and their ability to cope with adversity are pivotal. For those with alexithymia, the adverse effects of inescapable interparental conflict can be profound. However, robust resilience can internalize transient negative emotions, considerably diminishing the likelihood of progressing to NSSI.
Second, this study broadens the scope beyond the confines of the family environment. It explores the influence of the familial atmosphere on adolescent NSSI within the societal context of Chinese culture, as viewed through the lens of cultural psychology. China is a quint quintessential exponent of collectivist culture, where the bonds between individuals, families, and the broader society are tight knit. Consequently, the parent-child relationship exerts a substantial influence on children’s engagement in NSSI. Hence, we start our investigation by examining traditional family dynamics in China, with the objective of offering a cross-cultural perspective on the interplay between families and parenting concerns across a spectrum of collectivist societies. This study constructs a moderated mediation model (Fig. 1), grounded in the environmental function model and compensation model. It takes a holistic approach to understanding the mechanisms linking interparental conflict with NSSI. It also examines the mediating effects of alexithymia and the moderating influence of resilience within this process. The objective is to provide a theoretical foundation and empirical evidence to underpin the prevention and intervention strategies for NSSI among Chinese adolescents.
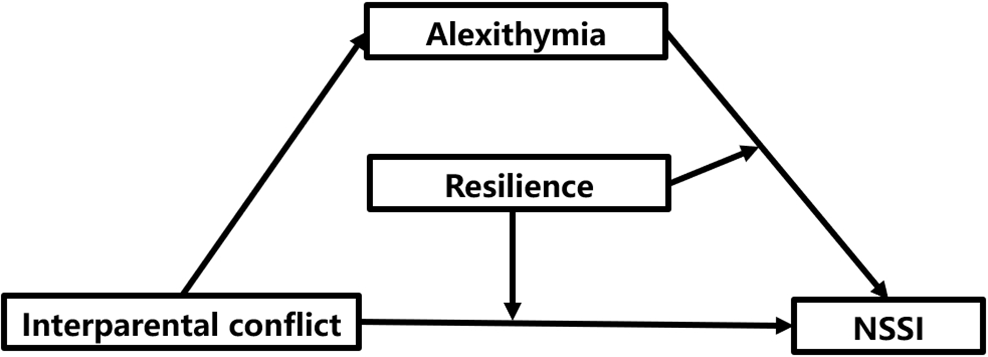
Figure 1: Theoretical model.
Based on the arguments outlined above, we propose the following hypotheses:
Hypothesis 1 (H1): Interparental conflict significantly positively predicts NSSI.
Hypothesis 2 (H2): Alexithymia mediates the relation between interparental conflict and NSSI.
Hypothesis 3a (H3a): Resilience moderates the relation between interparental conflict and NSSI. The positive predictive effect of interparental conflict on NSSI is more significant in individuals with lower levels of resilience than in those with higher levels.
Hypothesis 3b (H3b): Resilience moderates the relation between alexithymia and NSSI. The positive predictive effect of alexithymia on NSSI is more significant in individuals with lower levels of resilience than in those with higher levels.
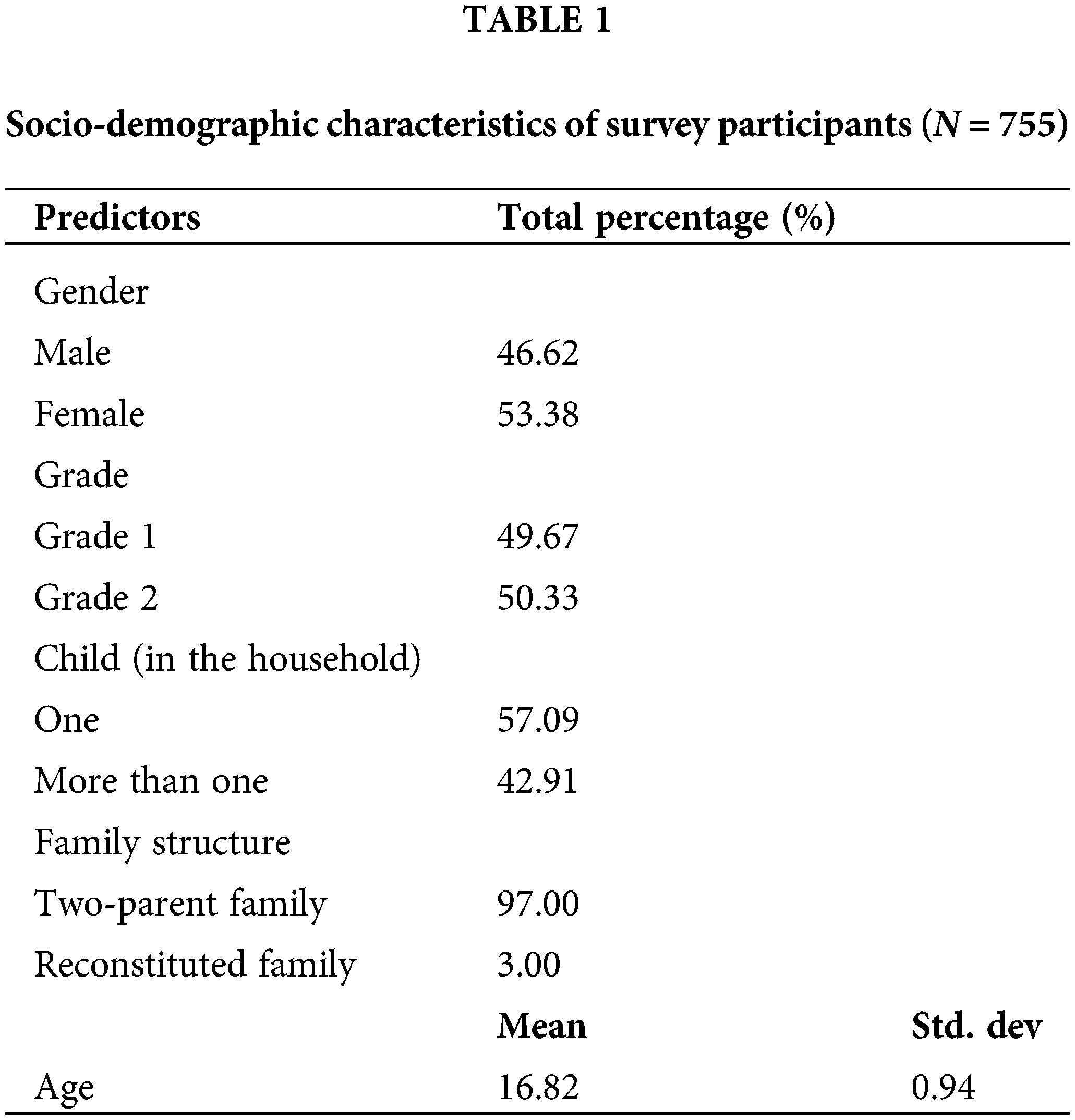
Students from the first and second grades of two senior high schools in Liaoning Province in China were selected using cluster sampling between 30 September 2023 and 15 October 2023, with an effort to recruit an equal number of male (46.62%) and female (53.38%) participants. Their ages ranged from 14 to 18 years, with a mean age of 16.82 years (SD = 0.94). Detailed socio-demographic characteristics of the respondents are presented in Table 1.
Prior to their completion, all participants received detailed instructions. A classroom teacher oversaw the questionnaire administration, and they ensured that the participants finished within a 20-min time frame. Upon collection, questionnaires from students in single-parent families, as well as those that were incomplete or filled out in a patterned manner, were excluded. A total of 820 questionnaires were distributed, and 755 students completed the survey qualifiedly, resulting in a response rate of 92.07%. This present study complied with the Helsinki Declaration and its relevant all other amendments to collect data from human participants. The Ethical Committee of the College of Educational Science, Shenyang Normal University, Shenyang, China has approved the study (No. 2023015). All participants signed the informed consent in this study.
All experimental data were gathered using a comprehensive questionnaire that included demographic inquiries and four sub-questionnaires. These sub-questionnaires were randomly ordered to assess children’s perceptions of interparental conflict, their history of engaging in self-injury and the severity thereof, and their levels of alexithymia and resilience. Following localization, all sub-questionnaires demonstrated robust reliability and validity. The specifics are outlined below.
Interparental conflict was measured using the conflict characteristics subscale of the Interparental Conflict Child Perception Scale (CPIC) [42]. The scale contains two dimensions of conflict degree and conflict resolution, with a total of 18 items. Using a 5-point Likert Scale (from “1 = strongly disagree” to “5 = totally agree”), a higher total score indicates a higher level of interparental conflict. In the present study, the CPIC had good model fits (Cronbach’s α = 0.82, χ2 = 558.63, df = 113, CFI = 0.93, TLI = 0.91, RMSEA = 0.07, SRMR = 0.07).
NSSI was evaluated using the Adolescent Self-Injury Behavior Questionnaire (ASHS) [43], which comprises 19 items. The questionnaire was divided into two parts to measure the frequency and degree of NSSI. The existence of NSSI was defined by the product of these two parts. NSSI does not exist if the product is 0, otherwise NSSI exists. The frequency of NSSI was scored on a 4-point Likert Scale (from “0 = does not occur” to “3 = more than five times”), and the degree of NSSI was scored on a 5-point Likert Scale (from “0 = does not occur” to “4 = extremely severe”). In the present study, the ASHS had good model fits (Cronbach’s α = 0.98, χ2 = 341.91, df = 70, CFI = 0.99, TLI = 0.97, RMSEA = 0.07, SRMR = 0.02).
Alexithymia was measured using the localized version of the Toronto Alexithymia Scale-20 (TAS-20) [44], which includes three dimensions—emotion recognition, emotion description, and extroverted thinking—with a total of 20 items. Using a 5-point Likert Scale (from “1 = strongly disagree” to “5 = totally agree”), a higher total score means a higher level of alexithymia. In the present study, the TAS-20 had good model fits (Cronbach’s α = 0.85, χ2 = 576.56, df = 154, CFI = 0.92, TLI = 0.90, RMSEA = 0.06, SRMR = 0.06).
To assess one’s resilience, the Scale of Adolescent Resilience (RSCA) [45] was used, which has 27 questions divided into two factors: individual power and support. These two factors were measured from different sources of resilience. Individual power includes three factors: goal focus, emotional control, and positive cognition. Support includes two factors: family support and interpersonal assistance. Using a 5-point Likert Scale (from “1 = strongly disagree” to “5 = totally agree”), a higher total score means a higher level of resilience. In the present study, the RSCA had good model fits (Cronbach’s α = 0.89, χ2 = 830.91, df = 238, CFI = 0.93, TLI = 0.90, RMSEA = 0.06, SRMR = 0.08).
In this study, the independent variable was interparental conflict and the dependent variable was NSSI. The socio-demographic controls included gender, grade, age, number of children in the household, and family structure. Age was used as a continuous variable. Gender, grade, number of children, and family structure were coded into dummy variables with the following categories: female (reference: male); Grade 1 (reference: Grade 2); one child in the household (reference: more children), and two-parent family (reference: reconstituted family).
Initially, the reliability and validity of the four sub-questionnaires were assessed individually. “Harman’s single factor test” and the “control for the effects of an unmeasured latent factor (ULMC)” were then employed to examine the presence of common method bias. The collected data were analyzed comprehensively using SPSS 25.0, which included controlling for demographic variables as covariates. Required statistical analyses were performed on interparental conflict, alexithymia, resilience, and NSSI (H1). Finally, the theoretical model constructed in this study was validated by Process (a plug-in installed in SPSS 25.0). In the first phase, Process Model 4 combined with the bootstrap method was used to test the mediating role of alexithymia (H2). In the second phase, Process Model 15 was utilized to assess the moderating role of resilience (H3a and H3b). The moderating mediating effect was further examined through simple slope analysis. The p < 0.05 was considered statistically significant.
Harman single factor test and the controlling for the effects of an Unmeasured Latent Methods factor (ULMC) were used to examine common method bias in the data. First, the results of the Harman single-factor test extracted 14 factors whose characteristic roots were greater than 1. The first factor explained 22.40% of the variation, below the 40% threshold. Subsequently, based on related trait factors (interparental conflict, alexithymia, NSSI, and resilience), all items were taken as indicators of global method factors, and a two-factor model was established and compared with the model containing only trait factors. The results showed no significant difference between the two models (ΔCFI = 0.071, ΔTLI = 0.056, ΔRMSEA = 0.017, ΔSRMR = 0.017). No obvious common method bias is noted in the study.
The results showed that 587 high school students had never committed NSSI, accounting for 77.75% of the total. A total of 168 high school students had attempted NSSI at least once, accounting for 22.25% of the total. The mean value, standard deviation, and correlation coefficient of each variable are shown in Table 2. Interparental conflict was significantly positively associated with alexithymia (r = 0.45, p < 0.01) and NSSI (r = 0.22, p < 0.01). Resilience was significantly negatively associated with interparental conflict (r = −0.47, p < 0.01), NSSI (r = −0.18, p < 0.01), and alexithymia (r = −0.67, p < 0.01).
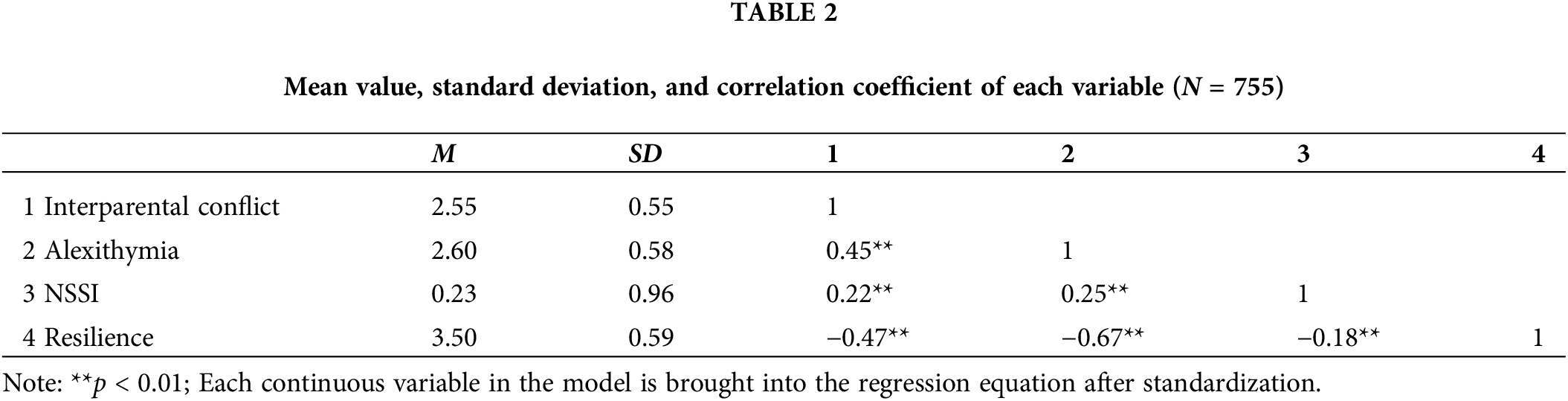
The mediation effect of alexithymia between interparental conflict and NSSI was tested by Process Model 4 while controlling for demographic variables such as gender and grade. The results are shown in Table 3. Interparental conflict significantly positively predicted NSSI (β = 0.21, t = 5.89, p < 0.01), verifying H1. Interparental conflict significantly positively predicted alexithymia (β = 0.46, t = 13.93, p < 0.01). After controlling the interparental conflict, alexithymia positively predicted NSSI significantly (β = 0.19, t = 4.83, p < 0.01). After adding the mediation variable, we found that interparental conflict could still significantly positively predict NSSI (β = 0.12, t = 3.14, p < 0.01). The standard regression coefficient decreased from 0.21 to 0.12, that is, the influence of interparental conflict on NSSI became smaller.
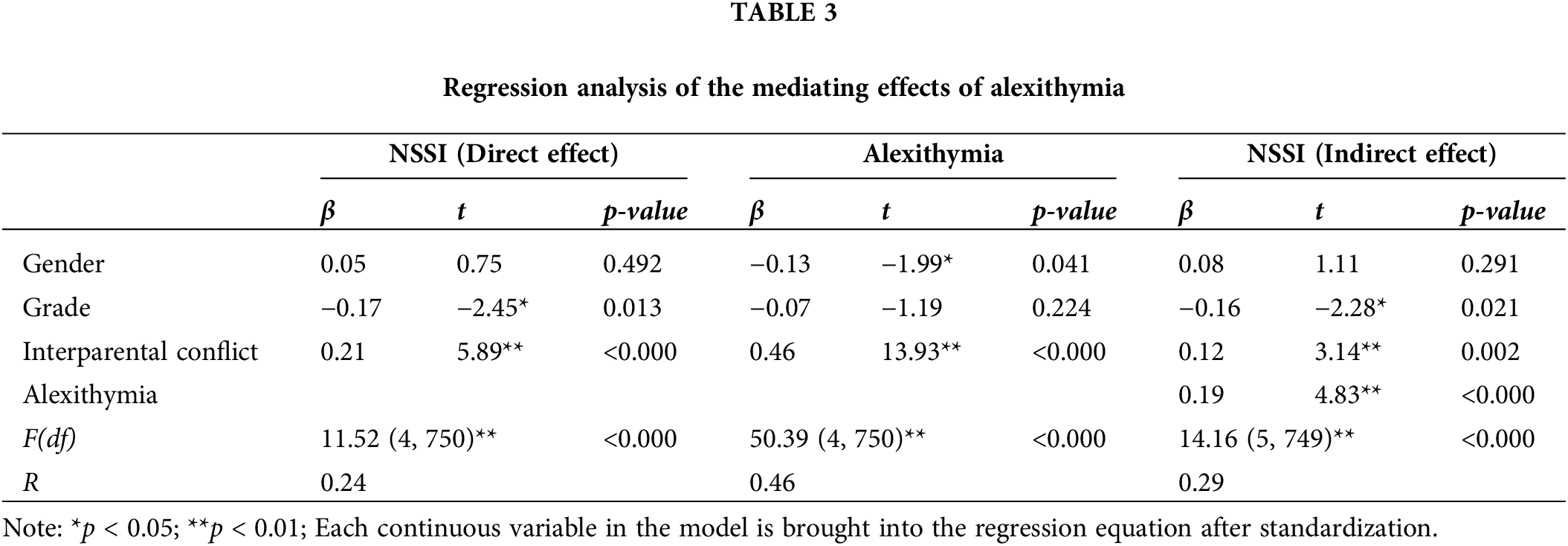
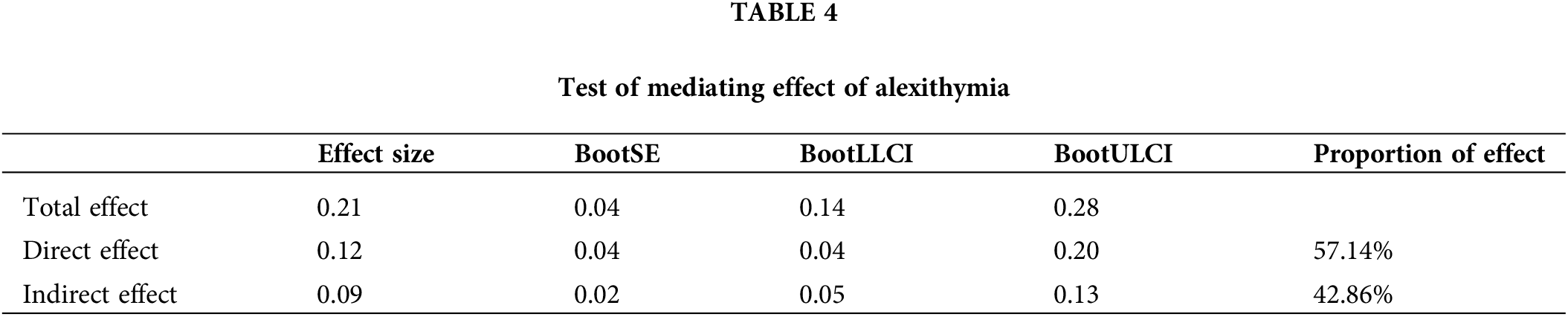
Bootstrap was used to test the proportion of direct and indirect effects, and the results are shown in Table 4. The total effect value was 0.21. The direct effect of interparental conflict on NSSI was 0.12, accounting for 57.14% of the total effect. The indirect effect was 0.09, accounting for 42.86% of the total effect. The upper and lower limits of the 95% confidence interval of the direct effect of NSSI (CI = [0.04, 0.20]) and the mediating effect of alexithymia (CI = [0.05, 0.13]) excluded 0. This outcome indicates that alexithymia partially mediated the prediction of interparental conflict on NSSI, thereby verifying H2.
Process Model 15 was used to test the moderating role of resilience in this moderated mediation model, and the results are shown in Table 5. The interaction between interparental conflict and resilience had a significant predictive effect on NSSI (β = −0.08, p < 0.05). This result indicates that resilience moderated the relation between interparental conflict and NSSI, 95% CI [−0.147, −0.003] excluded 0, verifying H3a. The interaction between alexithymia and resilience had a significant predictive predicted effect on NSSI (β = −0.08, p < 0.05). Therefore, resilience moderated the relationship between alexithymia and NSSI, 95% CI [−0.151, −0.013] excluded 0, verifying H3b.
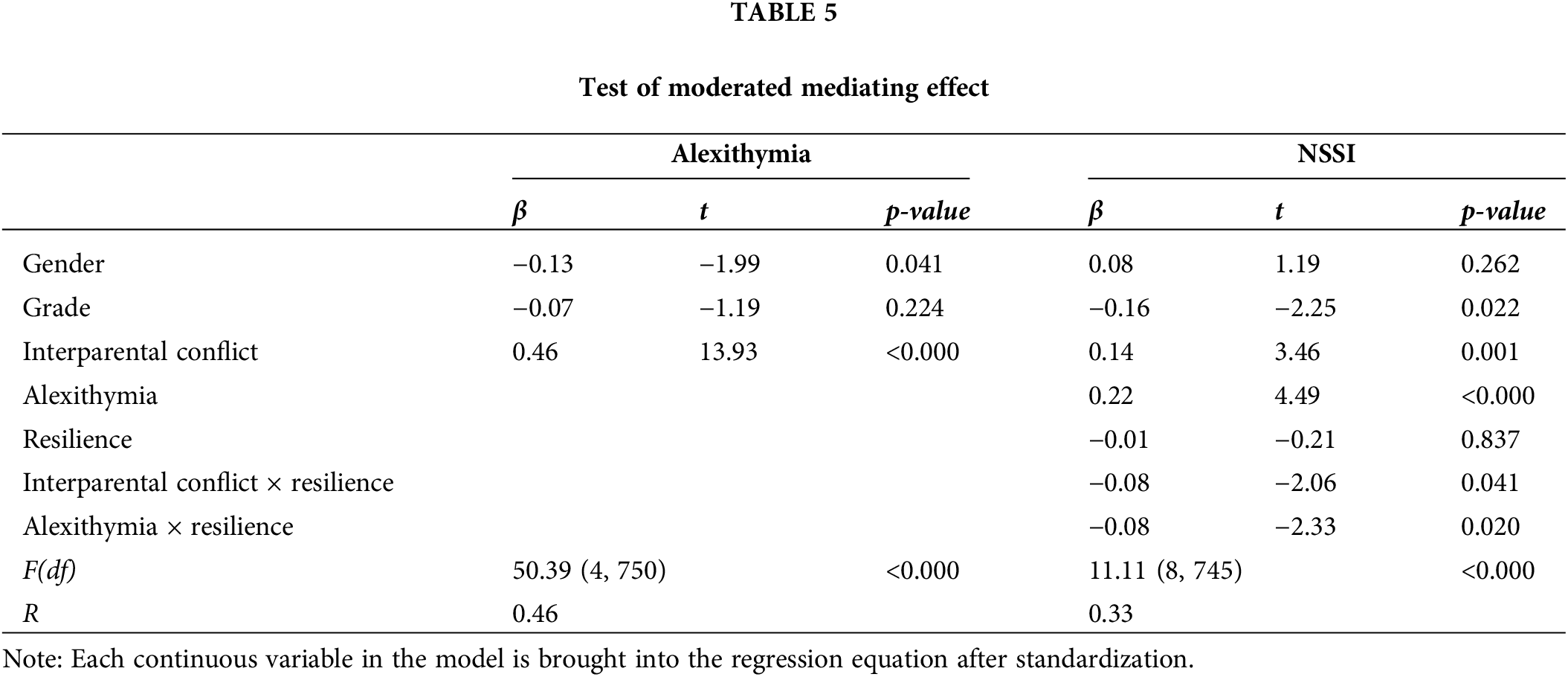
Simple slope analysis was used to further test the moderating effect of resilience. According to the average resilience score, the subjects were divided into high resilience group (M + 1SD) and low resilience group (M − 1SD). In the low resilience group, interparental conflict predicted NSSI more significantly (β = 0.22, p < 0.01). With the improvement of resilience level, interparental conflict cannot significantly predict NSSI (β = 0.07, p > 0.05). Only when the level of resilience is low, interparental conflict can positively predict the NSSI of adolescents (Fig. 2). In the low resilience group, the predictive effect of alexithymia on NSSI is more significant. (β = 0.14, p < 0.05). With the improvement of resilience level, the predictive effect of alexithymia on NSSI gradually decreases (β = 0.06, p < 0.05) (Fig. 3).
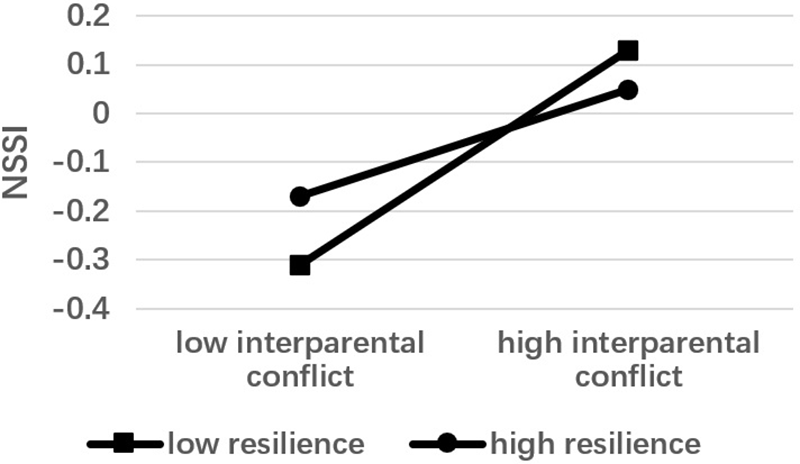
Figure 2: Moderation of resilience between interparental conflict and NSSI.
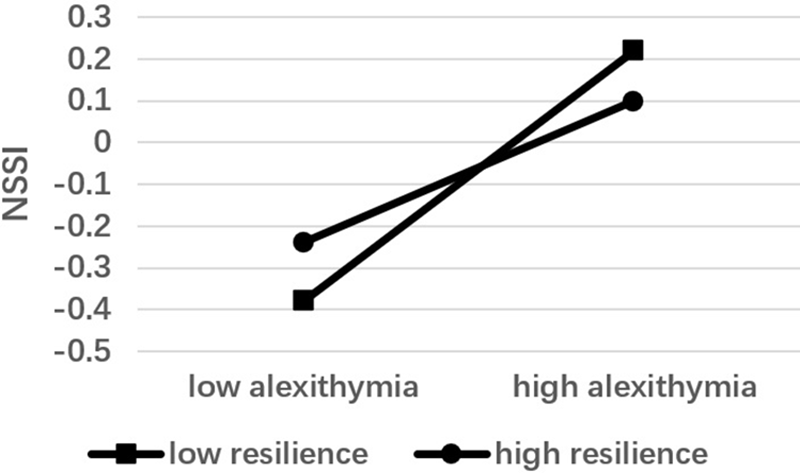
Figure 3: Moderation of resilience between alexithymia and NSSI.
This cross-sectional study aims to investigate the influence of interparental conflict on adolescents’ NSSI within the context of Chinese families. The internal operational mechanism is examined by considering the mediating role of alexithymia and the moderating role of resilience. To our knowledge, there have been no prior studies that have modeled or explored the relationship among these factors. Lastly, this study provides an explanation for why Chinese adolescents may be more susceptible to NSSI compared to their Western counterparts and suggests effective interventions.
The results of this study show that interparental conflict positively predicts NSSI of seniohigh school students, which is consistent with previous research results [46]. According to NSSI’s environmental function model, an individual’s living environment is conceptualized as a system. NSSI is a means for self-injurers to restore balance within the system or to express the distress caused by a malfunctioning system [15]. A dysfunctional system often results in negative emotional states such as restlessness, depression, and anxiety, while giving rise to various psychological issues that self-injury may temporarily alleviate [47]. Among the environmental factors, the family environment is a predominant influence on self-injury behavior [48]. Dysfunctional family dynamics considerably elevate the incidence of NSSI in adolescents [49], with interparental conflict being a key indicator of family dysfunction [50].
Moreover, the findings indicate that alexithymia partially mediates the relation between interparental conflict and NSSI in adolescents. In other words, interparental conflict not only has a direct predictive effect on NSSI, but also can indirectly predict NSSI through alexithymia. As children mature, they become increasingly attuned to the dynamics of their parents’ relationship, particularly during adolescence. The quality of the parent-child relationship greatly influences the physical and psychological development of adolescents [51]. According to the emotion-regulating function of self-injury behavior, self-injury is considered an inappropriate strategy for individuals to express and manage intense negative emotions [52]. Adolescents exposed to frequent and severe family conflicts often lack emotional security and lack the skills to express and cope with emotions effectively. They typically experience greater distress and pressure compared to children from stable families [49]. In such contexts, interparental conflict can lead teenagers to experience intense negative emotions [53], and they are more prone to emotional management issues, which can lead to the development of alexithymia. If the perceived level of conflict exceeds their threshold for tolerance, prolonged suppression of negative emotions without appropriate outlets can result in elevated levels of alexithymia. As a result, their likelihood of engaging in negative behaviors such as NSSI increases. The high correlation observed between alexithymia and NSSI [54] enables effective differentiation between individuals who engage in NSSI and those who do not. This finding validates the mediating path of the model and is consistent with the existing literature.
Another important aim of this study is to elucidate the moderating role of resilience in the model. Firstly, the results uncovered that resilience moderates the relationship between interparental conflict and NSSI among adolescents. With an increase in resilience levels, the strength of the positive association between interparental conflict and NSSI in this demographic tends to diminish. Given their propensity toward impulsive actions [55] adolescents are particularly vulnerable to engaging in self-injury as a maladaptive strategy to restore equilibrium within the family system when it is disturbed or when familial relationships are strained [56]. This phenomenon is particularly pronounced in individuals with low resilience [57]. Therefore, high levels of resilience not only reduce the likelihood that adolescents will resort to self-harm but also provide the necessary psychological support as they cope with environmental risks. During their development, high levels of resilience may be a key factor in promoting positive mental health [58]. Secondly, resilience moderates the relationship between alexithymia and NSSI. Central to alexithymia is a difficulty in regulating emotions [59]. Adolescents experiencing alexithymia opt for internal inhibitory strategies when confronting negative emotions [60]. Consequently, alexithymia is often associated with NSSI [61]. Research has agreed that a high resilience level is an important positive predictor of mental health [62]. Additionally, it is a pivotal factor in the ability to manage emotions [63]. Individuals with higher levels of resilience are more prone to select appropriate coping strategies when faced with by negative emotional experiences, enabling them to navigate challenges effectively and avoid unnecessary harm.
Combining the results of this study with existing literature, it is revealed why Chinese adolescents tend to have higher rates of self-harm than adolescents in Western cultures. According to the concept of “the basic triangle of the Chinese family”, the family is the primary unit comprising conjugal and parent-child relationships. The father, mother, and children form this foundational triangular structure, which shapes the fundamental framework and subsequent development of family dynamics. In this marital arrangement, two interrelated social relationships are simultaneously established: the couple relationship and the parent-child relationship. These relationships are interdependent: the couple’s relationship is based on the parent-child relationship as the premise, and the parent-child relationship is based on the couple’s relationship as a necessary condition. Consequently, children in Chinese families not only assume their roles but also serve as a crucial link between the couple, indicating that they often carry a heavier burden. The presence of alexithymia within individuals and interparental conflict within the family environment amplifies the pressure on children within the context of a closely-knit cultural framework.
NSSI serves as a critical risk factor for heightened suicide risk among Chinese adolescents. However, there is a paucity of clinical intervention methods specifically tailored to NSSI [64]. Currently, the evidence supporting the efficacy of traditional psychotropic medications in treating adolescent is insufficient. Psychotherapy and psychological interventions are the predominant approaches in clinical practice [65]. Studies of adult Dialectical Behavior Therapy (DBT) have shown a low dropout rate and effective reduction of suicide attempts and self-injury behaviors, which has prompted its adaptation for adolescent NSSI patients [66]. Cognitive behavioral interventions based on DBT have been identified as an effective strategy for addressing NSSI among adolescents in China. Combined with the positive predictive effect of interparental conflict on adolescents’ NSSI, this study encourages the use of DBT in multi-family groups. This approach leverages the strong family bonds prevalent in Chinese culture to reduce interparental conflict and build a more harmonious family environment. It enables parents to act as coaches, summarizing and reinforcing the DBT skills they have learned for their children. This optimization will make it easier for adolescents to understand and participate in treatment, reducing the likelihood of alexithymia occurring and developing. Moreover, according to the results of this study, improving the level of resilience in NSSI patients should be included as part of the training.
The study is not without limitations, so the findings should be approached with a degree of caution. Firstly, this study only discussed environmental factors among the various influencing factors that affect adolescents’ NSSI. However, recent research has emphasized that externalizing behaviors are influenced by a combination of genetic predispositions, environmental factors, and individual development. Future research could explore the interaction of the three on NSSI. Secondly, cross-sectional design is limited in examining dynamic individual development. To gain a deeper understanding, future studies can utilize longitudinal designs to explore the relationship between family factors and NSSI in adolescents. Thirdly, this study only examined the parent-child relationship in the family system. In fact, relevant variables such as family income, parents’ educational level, and parenting style are equally important. Controlling for these factors in future research can lead to more precise conclusions.
This present study aims to contribute to the literature on interparental conflict and NSSI by establishing a moderated mediation model. The study reveals a positive correlation between interparental conflict and adolescents’ NSSI in Chinese family contexts. Additionally, it demonstrates the mediating role of Alexithymia and the moderating role of resilience. Based on the results, it is suggested that Chinese adolescents are more susceptible to developing NSSI compared to their Western counterparts due to the influence of family dynamics, and recommendations for intervention and treatment of NSSI are provided. The results of this study can help mental health and behavioral professionals design rational intervention programs and provide a reference for adolescent educators in similar cultural contexts.
Acknowledgement: The authors would like to acknowledge all the anonymous participants in the research.
Funding Statement: This research was supported by the National Social Science Foundation of China (BHA240105).
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Lu Jia, Ye Zhang, Sijia Yu; data collection: Sijia Yu; analysis and interpretation of results: Lu Jia; draft manuscript preparation: Lu Jia, Ye Zhang. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data is available on request from the corresponding author.
Ethics Approval: The Ethical Committee of College of Educational Science, Shenyang Normal University, Shenyang, China has approved the study (No. 2023015). All participants signed the informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Nock MK. Self-injury. Annu Rev Clin Psychol. 2010;6(1):339–63. doi:10.1146/annurev.clinpsy.121208.131258. [Google Scholar] [CrossRef]
2. Yang Q, Xie R, Li J, Zhang R, Ding W, Li W. The mutual relationship between self-compassion, perceived social support, and adolescent NSSI: a three-wave longitudinal study. Mindfulness. 2023;14(8):1940–50. doi:10.1007/s12671-023-02169-6. [Google Scholar] [CrossRef]
3. Forster M, Grigsby TJ, Gower AL, Mehus CJ, McMorris BJ. The role of social support in the association between childhood adversity and adolescent self-injury and suicide: findings from a statewide sample of high school students. J Youth Adolesc. 2020;49:1195–208. [Google Scholar]
4. Green KH, van de Groep S, Sweijen SW, Becht AI, Buijzen M, de Leeuw RN, et al. Mood and emotional reactivity of adolescents during the COVID-19 pandemic: short-term and long-term effects and the impact of social and socioeconomic stressors. Sci Rep. 2021;11(1):11563. doi:10.1038/s41598-021-90851-x. [Google Scholar] [CrossRef]
5. Qu D, Wen X, Liu B, Zhang X, He Y, Chen D, et al. Non-suicidal self-injury in Chinese population: a scoping review of prevalence, method, risk factors and preventive interventions. Lancet Reg Health West Pac. 2023;37:100794. [Google Scholar]
6. Buehler C, Anthony C, Krishnakumar A, Stone G, Gerard J, Pemberton S. Interparental conflict and youth problem behaviors: a meta-analysis. J Child Fam Stud. 1997;6(2):233–47. doi:10.1023/A%3A1025006909538. [Google Scholar] [CrossRef]
7. Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1997;32(7):513. doi:10.1037/0003-066X.32.7.513. [Google Scholar] [CrossRef]
8. Kong J, Moorman SM, Martire LM, Almeida DM. The role of current family relationships in associations between childhood abuse and adult psychological functioning. J Gerontol B. 2019;74(5):858–68. [Google Scholar]
9. Saadati N, Parsakia K. The predictive role of parents’ marital relationship quality on the adolescents’ psychological capital. J Adolesc Youth Psychol Stud. 2023;4(8):139–46. [Google Scholar]
10. Bozyiğit T, Mamatoğlu N. The mediating role of adolescent emotion regulation in the relationship between parental marital conflict resolution styles and adolescent conflict resolution behaviors. Hacet Univ Egit Fak. 2022. doi:10.16986/huje.2021073520. [Google Scholar] [CrossRef]
11. Katz LF, Gottman JM. Spillover effects of marital conflict: in search of parenting and coparenting mechanisms. New Dir Child Adolesc Dev. 1996;1996(74):57–76. doi:10.1002/CD.23219967406. [Google Scholar] [CrossRef]
12. Xiang J, Jin L, Qian H, Wang GH, Shu C. The influence of interpersonal relationship on non-suicidal self-injury behavior in adolescents with depression. Neural Inj Funct Recons. 2022;17:444–8. [Google Scholar]
13. Kaess M, Eppelmann L, Brunner R, Parzer P, Resch F, Carli V, et al. Life events predicting the first onset of adolescent direct self-injurious behavior—a prospective multicenter study. J Adolesc Health. 2020;66(2):195–201. doi:10.1016/j.jadohealth.2019.08.018. [Google Scholar] [CrossRef]
14. Esposito C, Bacchini D, Affuso G. Adolescent NSSI and its relationships with school bullying and peer rejection. Psychiatry Res. 2019;274:1–6. doi:10.1016/j.psychres.2019.02.018. [Google Scholar] [CrossRef]
15. Carr EG. The motivation of self-injurious behavior: a review of some hypotheses. Psychol Bull. 1977;84(4):800. doi:10.1037/0033-2909.84.4.800. [Google Scholar] [CrossRef]
16. Taylor GJ. Recent developments in alexithymia theory and research. Can J Psychiat. 2000;45(2):134–42. doi:10.1177/070674370004500203. [Google Scholar] [CrossRef]
17. Prino LE, Longobardi C, Fabris MA, Parada RH, Settanni M. Effects of bullying victimization on internalizing and externalizing symptoms: the mediating role of alexithymia. J Child Fam Stud. 2019;28(9):2586–93. doi:10.1007/s10826-019-01484-8. [Google Scholar] [CrossRef]
18. Kmieciak R. Alexithymia, social inhibition, affectivity, and knowledge hiding. J Knowl Manag. 2022;26(11):461–85. [Google Scholar]
19. Li Y, Yue P, Zhang M. Alexithymia and internet addiction in children: meaning in life as mediator and reciprocal filial piety as moderator. Psychol Res Behav Manag. 2023;16:3597–606. [Google Scholar]
20. Zhang B, Zhang W, Sun L. Relationship between alexithymia, loneliness, resilience and non-suicidal self-injury in adolescents with depression: a multi-center study. BMC Psychiatr. 2023;23(1):1–11. [Google Scholar]
21. Janik McErlean AB, Lim LXC. Relationship between parenting style, alexithymia and aggression in emerging adults. J Fam Econ Iss. 2020;41(6):853–74. doi:10.1177/0192513X19886647. [Google Scholar] [CrossRef]
22. Li X, Li B, Lu J, Jin L, Xue J, Che X. The relationship between alexithymia, hostile attribution bias, and aggression. Pers Indiv Differ. 2020;159(19):109869. doi:10.1016/j.paid.2020.109869. [Google Scholar] [CrossRef]
23. Wang Z, Goerlich KS, Luo YJ, Xu P, Aleman A. Social-specific impairment of negative emotion perception in alexithymia. Soc Cogn Affect Neurosci. 2022;17(4):387–97. doi:10.1093/scan/nsab099. [Google Scholar] [CrossRef]
24. Wang X, Li X, Guo C, Hu Y, Xia L, Geng F, et al. Prevalence and correlates of alexithymia and its relationship with life events in Chinese adolescents with depression during the COVID-19 pandemic. Front Psychiatr. 2021;12:774952. doi:10.3389/fpsyt.2021.774952. [Google Scholar] [CrossRef]
25. Feyzioğlu A, Taşlıoğlu Sayıner AC, Özçelik D, Tarımtay Altun F, Budak EN. The mediating role of early maladaptive schemas in the relationship between early childhood trauma and alexithymia. Curr Psychol. 2023;42(21):17851–61. doi:10.1007/s12144-022-02988-1. [Google Scholar] [CrossRef]
26. Schermerhorn AC. Associations of child emotion recognition with interparental conflict and shy child temperament traits. J Soc Pers Relat. 2019;36(4):1343–66. doi:10.1177/0265407518762606. [Google Scholar] [CrossRef]
27. Costa AP, Steffgen G, Vögele C. The role of alexithymia in parent-child interaction and in the emotional ability of children with autism spectrum disorder. Autism Res. 2019;12(3):458–68. doi:10.1002/aur.2061. [Google Scholar] [CrossRef]
28. Garmezy N, Masten AS, Tellegen A. The study of stress and competence in children: a building block for developmental psychopathology. Child Dev. 1984;55(1):97–111. doi:10.2307/1129837. [Google Scholar] [CrossRef]
29. Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Soc Behav Personal. 2007;35(1):19–30. doi:10.2224/SBP.2007.35.1.19. [Google Scholar] [CrossRef]
30. Masten AS. Ordinary magic: resilience in development. Guilford Pub. 2015. doi:10.5860/choice.187892. [Google Scholar] [CrossRef]
31. Chen M, Sun X, Chen Q, Chan KL. Parental migration, children’s safety and psychological adjustment in rural China: a meta-analysis. Trauma Violence Abus. 2020;21(1):113–22. doi:10.1177/1524838017744768. [Google Scholar] [CrossRef]
32. Mao M, Zang L, Zhang H. The effects of parental absence on children development: evidence from left-behind children in China. Int J Env Res Pub He. 2020;17(18):6770. doi:10.3390/ijerph17186770. [Google Scholar] [CrossRef]
33. Chen S, Bonanno GA. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol Trauma. 2020;12(S1):S51. doi:10.1037/tra0000685. [Google Scholar] [CrossRef]
34. Crucian N. The fake news phenomenon in the context of the covid-19 pandemic. the perception of romanian students. J Media Res Revista de Stud Media. 2023;16(46):28–45. [Google Scholar]
35. Xu M, Yang X. The influence of parents’ support of rural left-behind students acting on the passive adaptation: the mediating effect of mental resilience. Educ Measurem Eval. 2020;2:59–64. [Google Scholar]
36. Sher L. Primary and secondary resilience to stress-related disorders and suicidal behavior. Aust N Z J Psychiatr. 2020;54(1):108–8. doi:10.1177/0004867419876698. [Google Scholar] [CrossRef]
37. Zhou H, Hu Y, Cheng X, Sun X. Resilience as mediator in relation to parental attachment and posttraumatic stress disorder in adolescents following the Yancheng tornado. Clin Child Psychol Psychiatr. 2023;28(4):1408–19. doi:10.1177/13591045231160639. [Google Scholar] [CrossRef]
38. Zang X, Li T, Li M, An Y, Cheng X, Jin J. Resilience mediates the relationship between parental attachment and posttraumatic growth in adolescents: a longitudinal study. Disaster Med Public. 2023;17:e381. doi:10.1017/dmp.2023.43. [Google Scholar] [CrossRef]
39. Gonçalves S, Vieira AI, Machado BC, Bessa C. Non-suicidal self-injury in Portuguese college students: relationship with emotion regulation, resilience and self-compassion. Curr Psychol. 2024;43(9):7877–86. [Google Scholar]
40. Lyu C, Ma R, Hager R, Porter D. The relationship between resilience, anxiety, and depression in Chinese collegiate athletes. Front Psychol. 2022;13:921419. doi:10.3389/fpsyg.2022.921419. [Google Scholar] [CrossRef]
41. Zhang J, Yang Z, Wang X, Li J, Dong L, Wang F, et al. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: a cross-sectional study. J Clin Nurs. 2020;29(21–22):4020–402. [Google Scholar]
42. Chi L, Xin Z. The revision of children’s perception of marital conflict scale. Chin Ment Health J. 2002;17(8):554–6 (In Chinese). [Google Scholar]
43. Feng Y. The relation of adolescents’ self-harm behaviors, individual emotion characteristics and family environment factors. Central China Normal University: China; 2008. [Google Scholar]
44. Yi J, Yao S, Zhu X. The Chinese version of the TAS-20: reliability and validity. Chin Ment Health J. 2003;17(11):763–7 (In Chinese). [Google Scholar]
45. Hu YQ, Gan YQ. Development and psychometric validity of the resilience scale for Chinese adolescents. Acta Psychol Sin. 2008;40(8):902–12. doi:10.3724/SP.J.1041.2008.00902. [Google Scholar] [CrossRef]
46. Dhir R. Influence of parental and peer relationships on non-suicidal self-injury in adolescents. Int J Indian Psychol. 2020;8(3):30. [Google Scholar]
47. Hauber K, Boon A, Vermeiren R. Non-suicidal self-injury in clinical practice. Front Psychol. 2019;10:424130. [Google Scholar]
48. Wang D, Ma Z, Fan Y, Chen H, Liu W, Zhang Y, et al. Associations between family function and non-suicidal self-injury among Chinese urban adolescents with and without parental Migration. Child Psychiatr Hum Develop. 2023;54:1–11. [Google Scholar]
49. Boyes ME, Mah MA, Hasking P. Associations between family functioning, emotion regulation, social support, and self-injury among emerging adult university students. J Child Fam Stud. 2023;32(3):846–57. doi:10.1007/s10826-022-02516-6. [Google Scholar] [CrossRef]
50. Davies PT, Pearson JK, Cao VT, Sturge-Apple ML. Family-level antecedents of children’s patterns of reactivity to interparental conflict: testing the reformulation of emotional security theory. Dev Psychol. 2023;59(1):99. doi:10.1037/dev0001497.supp. [Google Scholar] [CrossRef]
51. Fosco GM, Weymouth BB, Feinberg ME. Interparental conflict, family climate, and threat appraisals: early adolescent exposure and young adult psychopathology risk. J Fam Psychol. 2023;37(5):731. doi:10.1037/fam0001096. [Google Scholar] [CrossRef]
52. Gratz KL. Risk factors for and functions of deliberate self-harm: an empirical and conceptual review. Clin Psychol-Sci Pr. 2003;10(2):192. doi:10.1093/CLIPSY.BPG022. [Google Scholar] [CrossRef]
53. Wang J, Liu N, Tao L. Interparental conflict affects adolescents’ anxiety and depression: self-esteem as a mediator. China J Health Psychol. 2020;28(11):1714–8 (In Chinese). [Google Scholar]
54. Liu J, Zhao K, Kang W, Tong S, Xu Y, Jin W, et al. The association of borderline personality features and self-injury among adolescents with non-suicidal self-injury: the mediating role of alexithymia. Psychol Res Behav Manag. 2023;16:1741–54. [Google Scholar]
55. McHugh CM, Lee RSC, Hermens DF, Corderoy A, Large M, Hickie IB. Impulsivity in the self-harm and suicidal behavior of young people: a systematic review and meta-analysis. J Psychiatr Res. 2019;116(3):51–60. doi:10.1016/J.JPSYCHIRES.2019.05.012. [Google Scholar] [CrossRef]
56. Chen X. Research on the intervention methods of adolescents’ non-suicidal self-injury behavior. Lect Not Educ Psychol Public Media. 2023;6(1):465–71. doi:10.54254/2753-7048%2F6%2F20220436. [Google Scholar] [CrossRef]
57. Mao C, Lin M, Shen S, Li Y, Xie Z, Li P. Latent profiles of emotion regulation strategies associated with alexithymia, nonsuicidal self-injury and resilience among nursing students. Stress Health. 2022;38(1):69–78. doi:10.1002/smi.3075. [Google Scholar] [CrossRef]
58. Zhang L, Meiai C, Benxian Y, Zhang Y. Aggression and non-suicidal self-injury among depressed youths: the mediating effect of resilience. Iran J Public Health. 2021;50(2):288. [Google Scholar]
59. Norman H, Oskis A, Marzano L, Coulson M. The relationship between self-harm and alexithymia: a systematic review and meta-analysis. Scand J Psychol. 2020;61(6):855–76. doi:10.1111/sjop.12217. [Google Scholar] [CrossRef]
60. Luo H, Gong X, Chen X, Hu J, Wang X, Sun Y, et al. Exploring the links between alexithymia and cognitive emotion regulation strategies in internet addiction: a network analysis model. Front Psychol. 2022;13:938116. [Google Scholar]
61. Wolff JC, Thompson E, Thomas SA, Nesi J, Bettis AH, Ransford B, et al. Emotion dysregulation and non-suicidal self-injury: a systematic review and meta-analysis. Eur Psychiat. 2019;59:25–36. doi:10.1016/j.eurpsy.2019.03.004. [Google Scholar] [CrossRef]
62. Yıldırım M, Arslan G, Wong PT. Meaningful living, resilience, affective balance, and psychological health problems among Turkish young adults during coronavirus pandemic. Curr Psychol. 2022;41(11):7812–23. [Google Scholar]
63. Zhang JY, Ji XZ, Fan YN, Cui YX. Emotion management for college students: effectiveness of a mindfulness-based emotion management intervention on emotional regulation and resilience of college students. J Nerv Ment Dis. 2022;210(9):716–22. doi:10.1097/NMD.0000000000001484. [Google Scholar] [CrossRef]
64. Nguyen TP, Lerch S, Maggetti A, Reichl C, Tarokh L, Kaess M. The relationship between sleep disturbance and self-harming behaviours in high-risk clinical adolescents. J Psychiatr Res. 2023;158:81–7. doi:10.1016/j.jpsychires.2022.12.034. [Google Scholar] [CrossRef]
65. Qin Y, Liu J, Wu DM. Research progress on online disclosure of non-suicidal self-injury among adolescents. Chin J Sch Health. 2022;43(10):1596–600 (In Chinese). [Google Scholar]
66. Syed S, Kingsbury M, Bennett K, Manion I, Colman I. Adolescents’ knowledge of a peer’s non-suicidal self-injury and own non-suicidal self-injury and suicidality. Acta Psychiatr Scand. 2020;142(5):366–73. doi:10.1111/acps.13229. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools