 Open Access
Open Access
ARTICLE
Do Public Health Events Promote the Prevalence of Adjustment Disorder in College Students? An Example from the COVID-19 Pandemic
College of Economics, Hangzhou Dianzi University, Hangzhou, 310018, China
* Corresponding Author: Rong Fu. Email:
International Journal of Mental Health Promotion 2024, 26(1), 21-30. https://doi.org/10.32604/ijmhp.2023.041730
Received 04 May 2023; Accepted 17 July 2023; Issue published 05 February 2024
Abstract
COVID-19, as one of the most serious sudden public health problems in this century, is a serious threat to people’s mental health. College students, as a vulnerable group, are more likely to develop mental health problems. When the body is unable to adapt to new changes in the environment, the main mental health problem that arises is adjustment disorder. The aim of this study was to assess the prevalence and influencing factors of adjustment disorder among college students during the COVID-19 outbreak in China. Cross-sectional data collected by web-based questionnaires were obtained through convenience sampling and snowball sampling between March 07, 2023 and March 14, 2023. The online self-report questionnaire included measures of demographic characteristics, the International Adjustment Disorder Questionnaire (IADQ), and the Influencing Factors Scale. Data were analyzed through structural equation modeling. A total of 394 valid samples (55.33% female) were collected in this study, approximately 75.63% of college students had a confirmed diagnosis of COVID-19 and 28.68% of college students had an adjustment disorder. There was no significant difference between the different demographic characteristics and the prevalence of adjustment disorder, and almost all demographic characteristics had a high prevalence of adjustment disorder. Structural equation modeling revealed that physiological impact ( = 0.077), psychological impact ( = 0.626) and potential impact ( = 0.106) of the sudden COVID-19 outbreak had a significant positive effect on the prevalence of adjustment disorder. The prevalence of adjustment disorder among college students is increased under the outbreak of COVID-19. The government should provide psychosocial support and mental health services for college students while also paying attention to potential factors such as stressors to reduce the adverse effects of outbreaks.Keywords
In December 2019, the Chinese Health Authority notified the World Health Organization (WHO) of several cases of pneumonia of unknown etiology in Wuhan, Hubei Province, central China [1], which later became known as COVID-19. COVID-19 is gradually becoming a global outbreak epidemic due to its rapid transmission, widespread infection, and difficulty in control [2]. On January 30, 2020, the World Health Organization classified COVID-19 as an international public health emergency [3], making it the most serious public health issue of the century [4]. As the lethality of the Omicron variant decreased and vaccination coverage increased [5], on December 7, 2022, the Joint Prevention and Control Mechanism of the State Council announced ten new measures to further optimize COVID-19 prevention and control (hereafter referred to as the ten new measures) [6,7]. Due to the further liberalization of COVID-19 prevention and control, Omicron infection has since spread rapidly in China, forming a new wave [8]. The number of new COVID-19 infections per day in China is shown in Fig. 1, with the vertical dashed line indicating the date December 07, 2022.
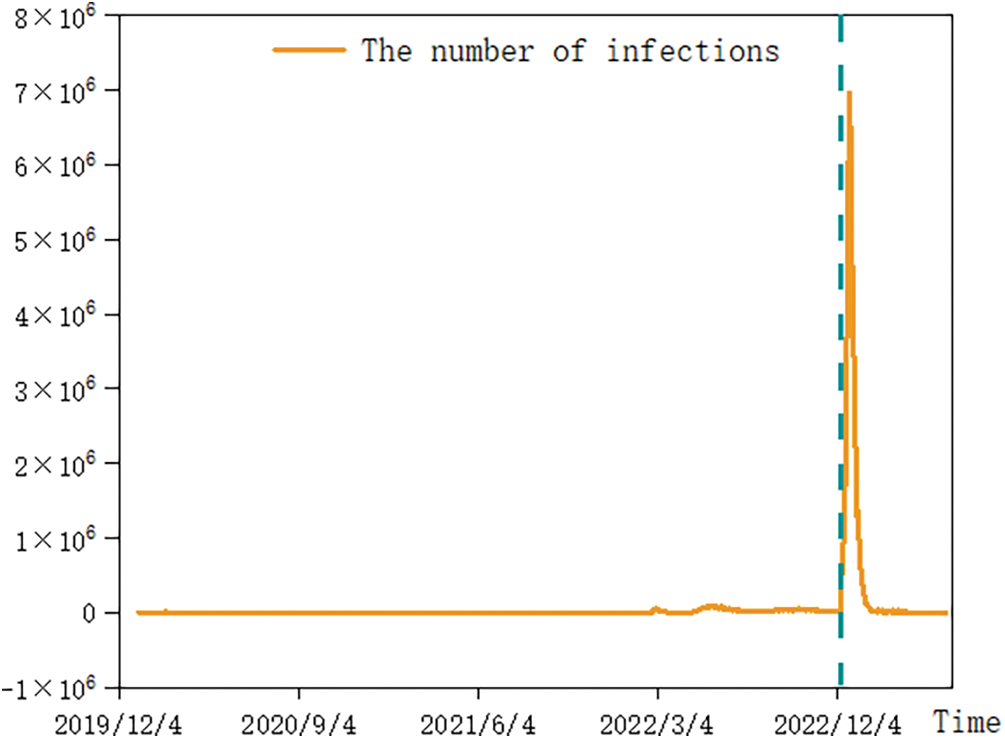
Figure 1: Daily number of COVID-19 infections in China.
Because of the suddenness, complexity and unpredictability of public health emergencies, the masses fail to correctly understand, prevent and dispose of the event after it occurs. It is easy to cause mass behavior that affects social order, which leads to panic and anxiety spread among the general public [9]. Thus, the psychological health of the masses is seriously affected [10]. One of these mental health outcomes may be the creation of adjustment disorder (AjD) [11]. Adjustment disorder is a common psychological disorder in the population. Adjustment disorder is a maladaptive response to an identifiable psychosocial stressor or multiple stressors, usually within 1 month of the onset of the stressor. The disorder is characterized by preoccupation with the stressor or its consequences and failure to adapt to the stressor [12].
The COVID-19 pandemic is a stressful health event that triggers maladaptive reactions in the form of adjustment disorder [11]. When the human body is unable to adapt to new changes in the environment, a series of abnormal physiological and psychological reactions will occur, such as neurological reactions, endocrine reactions or in the psychological anxiety, fear and other emotional reactions [13]. Although all populations are affected, college students are among the most severely affected by COVID-19 [14–16]. Related studies have shown a higher prevalence of adjustment disorder in adolescents [17]. On the one hand, it is because college students are in the active period of physical and mental development. It is a special group of society. Faced with the double pressure of epidemic and academics, college students are more likely to have negative emotions. Thus, they develop bad habits of life and exercise, and their physical fitness decreases [2]. On the other hand, college students are more prone to mental health problems due to the uncertainty of academic success, future career and social life under public health emergencies [18]. During the COVID-19 pandemic, 20–40% of Chinese college students were vulnerable to severe psychological problems [19], with a significant increase in the overall prevalence of anxiety and depressive symptoms [20]. As the COVID-19 pandemic continues, the initial shock gradually emerges in the form of chronic stress, posing a significant challenge to the mental health of college students [21].
The COVID-19 pandemic has created a large number of stressors in the population. Governments have taken many isolation measures in response to the COVID-19 outbreak, such as lockdowns, home quarantines, travel restrictions, and physical distance [22], which have had a significant physiological impact. While these isolation measures slow down the spread of COVID-19, they also cause a certain amount of psychological stress to the population [23], which leads to a high incidence of psychological problems such as depression, anxiety, panic, fear, and insomnia [9,24–27]. In addition, psychological effects such as fear of infectious diseases and grieving the loss of loved ones from the world can exacerbate the impact on adjustment disorder [28,29]. As the peak period passed, the physiological impact of COVID-19 on the masses gradually decreased [30], but the sudden change in the epidemic environment still had a potential impact on the psychology of the masses. The extent to which individuals are exposed to information about the spread of the COVID-19 pandemic, for example, can further increase their stress response and thus also increase symptoms of adjustment disorder [31].
There have been literature reports on the mental health condition of college students during the COVID-19 epidemic in China, but no investigation has been conducted on the adjustment disorder of college students in the later stages of the COVID-19 epidemic in China, especially after the implementation of the ten new measures of the COVID-19 wave. Therefore, this study aims to analyze the situation of adjustment disorder among college students under the COVID-19 wave after the implementation of the ten new measures and the factors influencing it. Since the COVID-19 pandemic has greatly affected the lives of the population [32] and has a direct psychological impact [33] as well as a potential impact [34], this study investigates the impact of “physiological impact”, “psychological impact” and “potential impact” of the COVID-19 pandemic on “adjustment disorder” and proposes the following hypotheses:
H1: Physiological impact has a positive effect on adjustment disorder.
H2: Psychological impact has a positive effect on adjustment disorder.
H3: Potential impact has a positive effect on adjustment disorder.
The number of infections gradually peaked in about 1 month after the implementation of the ten new measures, so the data from this time period can reflect the authenticity and reliability of students’ status when coping with unexpected events, highlighting the significance of this study. In addition, to our knowledge, no study has investigated adjustment disorder among college students during the COVID-19 epidemic. We introduced the International Adjustment Disorder Questionnaire and integrated it with the Chinese context to measure the influences of adjustment disorder, which is novel.
For socio-demographic factors, researchers collected demographic information as needed for the survey, including questions on gender, grade level, poor student, only child, personality, physical status, living alone, and being infected with COVID-19.
For the assessment of adjustment disorder and its influencing factors, this study translated Shevlin’s International Adjustment Disorder Questionnaire (IADQ) into a Chinese version after adaptation to assess whether participants had adjustment disorder [35]. Since the implementation of the ten new measures leading to the COVID-19 pandemic was already a stressful event, only whether it caused adjustment disorder was considered. In terms of influences that contribute to adjustment disorder, researchers assessed changes in human behavior as a result of the COVID-19 pandemic [36], and then assessed the factor of physiological impact using “impact on daily life”, “impact on school work” and “impact on offline social activities”. Dragan indicated in previous studies that most participants perceived the COVID-19 pandemic as a highly stressful situation and that anxiety was the strongest predictor of adjustment disorder symptoms [37], so the researchers combined the 7-item Generalized Anxiety Disorder scale (GAD-7) and modified it to assess psychological impact as a factor [38]. The researchers combined previous pre-surveys with the actual situation in China to assess the potential impact of “fear of (re)infection with COVID-19”, “fear of lack of treatment drugs”, “fear of potential sequelae of COVID-19” and “fear that COVID-19 will persist”. A 5-point Likert scale was used for each item, with 1 corresponding to complete non-compliance and 5 corresponding to complete compliance, with compliance increasing from 1 to 5. The determination of the presence of adjustment disorder was the same as that of Shevlin et al. [35]. In this study, the Cronbach’s alpha coefficients for “physiological impact”, “psychological impact” and “potential impact” were 0.751, 0.899 and 0.893.
In this study, a combination of convenience sampling and snowball sampling was used to collect sample data. The questionnaires were first entered into the “Wenjuanxing” platform, and then based on the principle of convenience sampling, the counselors distributed the questionnaires to college students’ WeChat groups. At the same time, students were invited to forward the questionnaire based on the snowball sampling principle. The questionnaire was distributed from March 07, 2023 to March 14, 2023. A total of 427 questionnaires were collected, 33 invalid questionnaires were excluded, and the remaining 394 questionnaires were used as the original data samples for later data analysis, with an effective rate of 92.3%.
Statistical models and data analysis
Structural equation modeling is a model analysis method used to analyze causal relationships. The method is mainly performed by integrating two statistical methods: factor analysis and path analysis. By analyzing and testing the relationships among the latent variables, observed variables and error variables in the model, multiple effects of numerous independent variables on the dependent variable are obtained. This study uses structural equation modeling to explore the relationships among the variables.
In this study, SPSS 19.0 and AMOS 26.0 were used for statistical analysis. First, descriptive statistics were used to summarize the demographic characteristics of the participants. Second, the reliability of the scale was examined by using three indicators: Cronbach’s alpha coefficient, the composite reliability (CR), and the average variance extracted (AVE). And the discriminant validity of the scale was further measured by the average variance extracted. Structural equation modeling was used to explore the relationship between the variables, and this study relied primarily on the indicators proposed by Jackson to assess the model fit [39]. Finally, a path analysis was conducted to explore the relationship between physiological impact, psychological impact, and potential impact on adjustment disorder.
Description of sample feature distribution
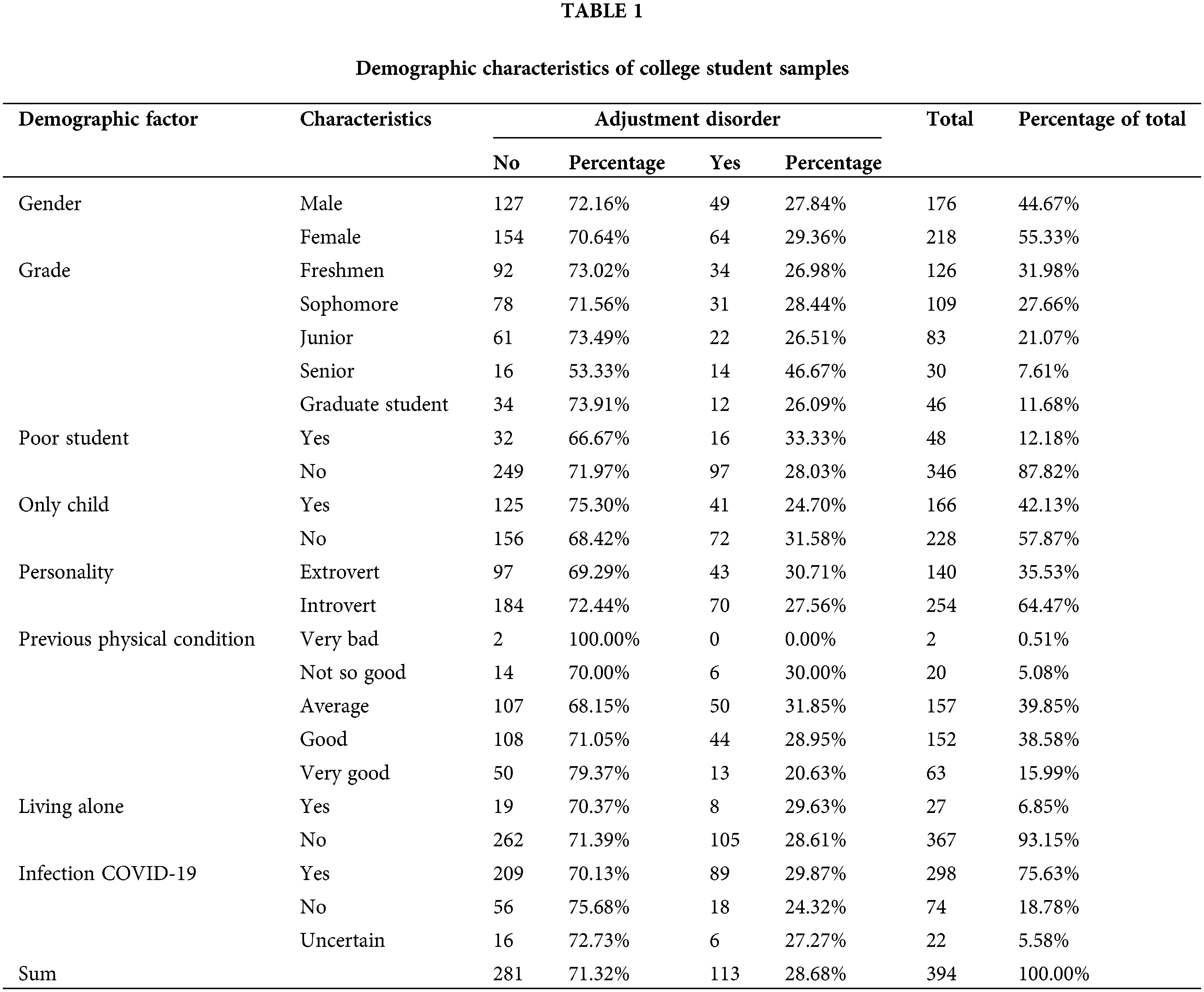
The demographic characteristics of the study sample are shown in Table 1. Among the 394 participants, there were slightly more females (55.33%) than males (44.67%). In terms of grade level, freshmen (31.98%) were the most numerous, with sophomores (27.66%), juniors (21.07%), graduate students (11.68%), and seniors (7.61%) in decreasing order of magnitude. There were far more non-poor students (87.82%) than poor students (12.18%), slightly fewer only children (42.13%) than non-only children (57.87%), and slightly fewer extroverts (35.53%) than introverts (64.47%). Before the implementation of the ten new measures, the majority of participants felt in fair (39.85%) and fairly good (38.58%) health, some felt very good (15.99%), and a few felt not so good (5.08%) and very bad (0.51%). In the COVID-19 wave after the implementation of the ten new measures, only a small percentage of participants were living alone (6.85%). COVID-19 was diagnosed in 298 of all participants (75.63%), 56 were not infected with COVID-19 (18.78%), and 22 were unsure if they were infected (5.58%). Of all participants, 113 were detected with adjustment disorder (28.68%) and 281 had no adjustment disorder (71.32%). The percentage of adjustment disorder was around 30% for all characteristics except for the grade level of seniors (46.67%) and the physical condition of very bad (0%).
Reliability and validity analysis
Measurement model testing requires testing the reliability and validity of the scales. In this study, three indicators, the Cronbach’s alpha coefficient, CR, and AVE, were used to conduct reliability tests. The agreement between the question items of the measured variables is generally considered acceptable when the CR value is greater than 0.7, the AVE value is greater than 0.5, and the Cronbach’s alpha value is greater than 0.7 [40]. The values of Cronbach’s alpha coefficient, CR and AVE calculated in this study are shown in Table 2. For the three factors of “ physiological impact ”, “psychological impact” and “potential impact”, the Cronbach’s alpha coefficients were all greater than 0.7, CR values were all greater than 0.7, and AVE values were all greater than 0.5, indicating that the scale used in this study had good internal consistency and the reliability was acceptable.
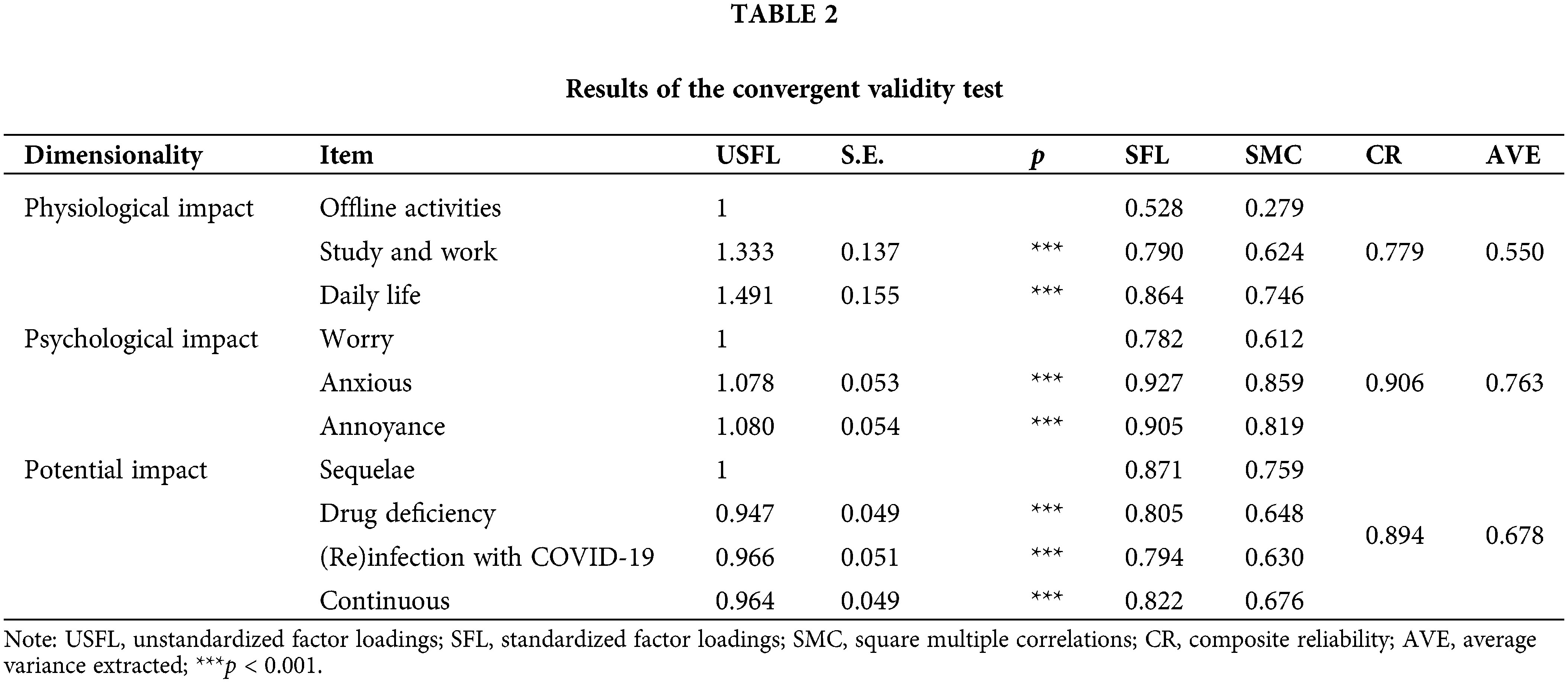
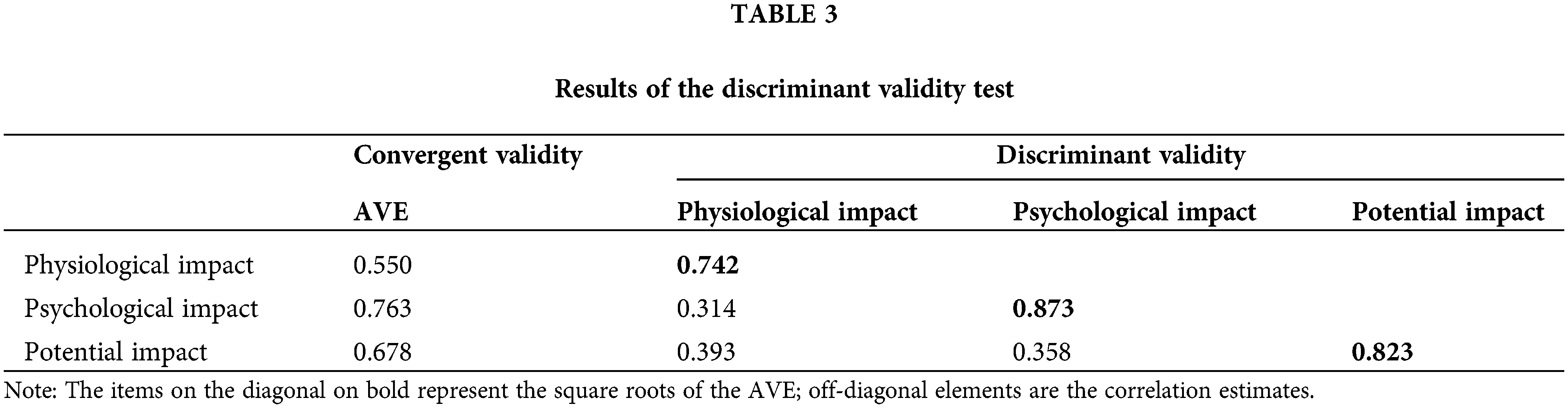
The validity tests are divided into convergent validity and discriminant validity. According to the criteria proposed by Fornell et al., when the CR value is greater than 0.7 and the AVE value is greater than 0.5, it indicates a high convergent validity of the variables [40]. As can be seen from Table 2, all variables have CR values greater than 0.7 and AVE values greater than 0.5, indicating that the convergent validity of each variable meets the requirements. Discriminant validity refers to low correlations and significant differences between latent variables, and it can be assessed by comparing the magnitude of the square root of the AVE with the correlation coefficient between the variables. According to the standard proposed by Fornell and Larcker, if the correlation coefficient between a variable and other variables is less than the square root of the AVE of the variable, it indicates that the variable has good discriminative validity [40]. The discriminant validity indicators calculated in this study are shown in Table 3. The data in bolded font in Table 3 are the square root of the AVE, which are all greater than all values in the column in which they are located, and therefore the discriminant validity of the measurement model in this study is appropriate.
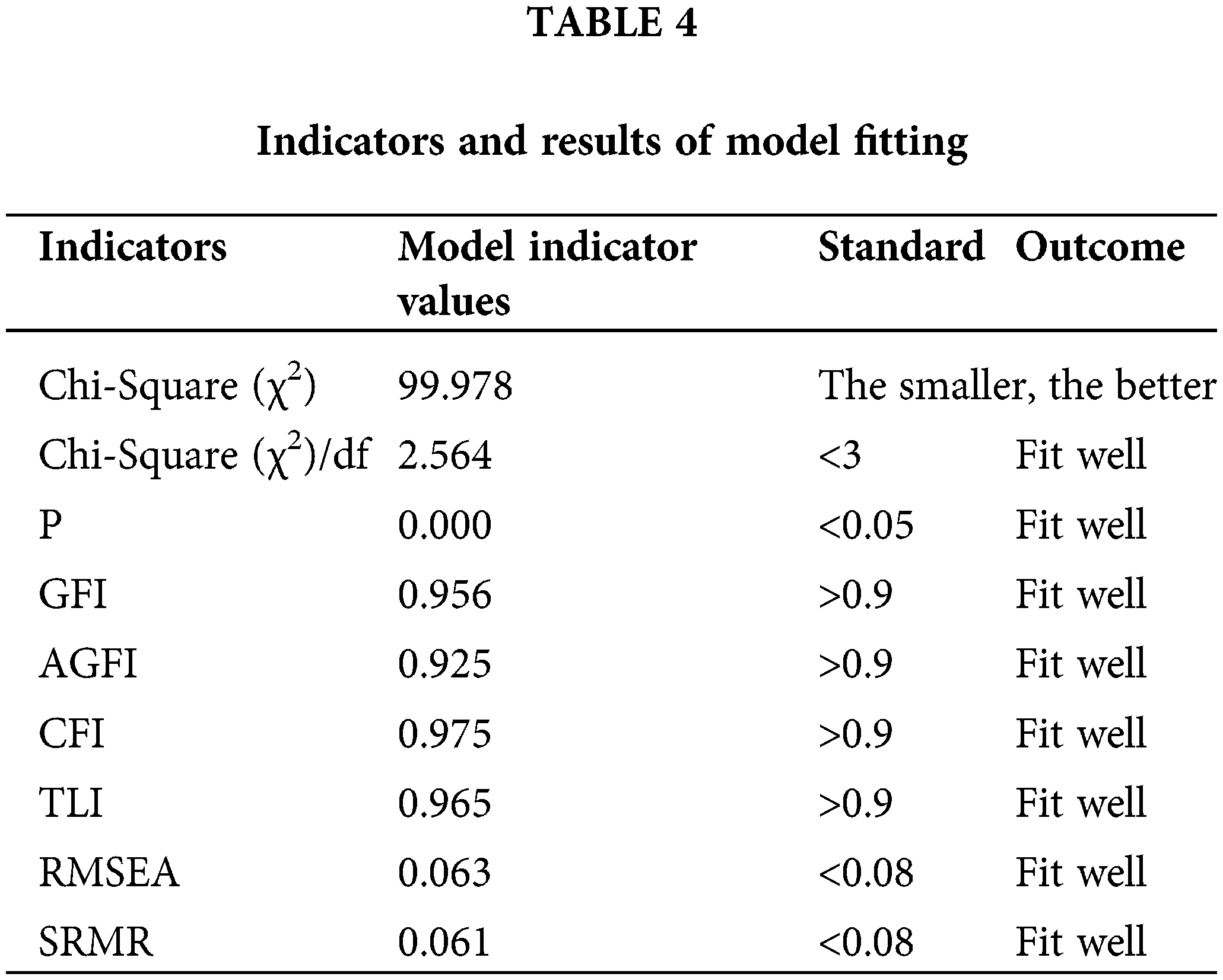
In this study, the results are reported in terms of the fit indices obtained from the study of Jackson [39]. The goodness of fit of a model can be assessed in terms of its Chi-Square (χ2), Relative Chi-Square (χ2/df), p-value, Goodness of Fit Index (GFI), Adjusted Goodness of Fit Index (AGFI), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Square of Error Approximation (RMSEA), Standardized Root Mean Square Residual (SRMR). The actual values of the model fit indices compared with the recommended values are shown in Table 4. As can be seen from Table 4, the actual values of all fitted indicators meet the judgment criteria proposed by Bagozzi [41]. Therefore, the model has a good fit.
This study uses structural equation modeling to perform path analysis and hypothesis verification for the three hypotheses proposed earlier, and the final path coefficients are shown in Fig. 2. The path coefficients between the independent and dependent variables are the values indicated on the connecting lines in Fig. 2. The parameter estimates and hypothesis testing results of the model are shown in Table 5.
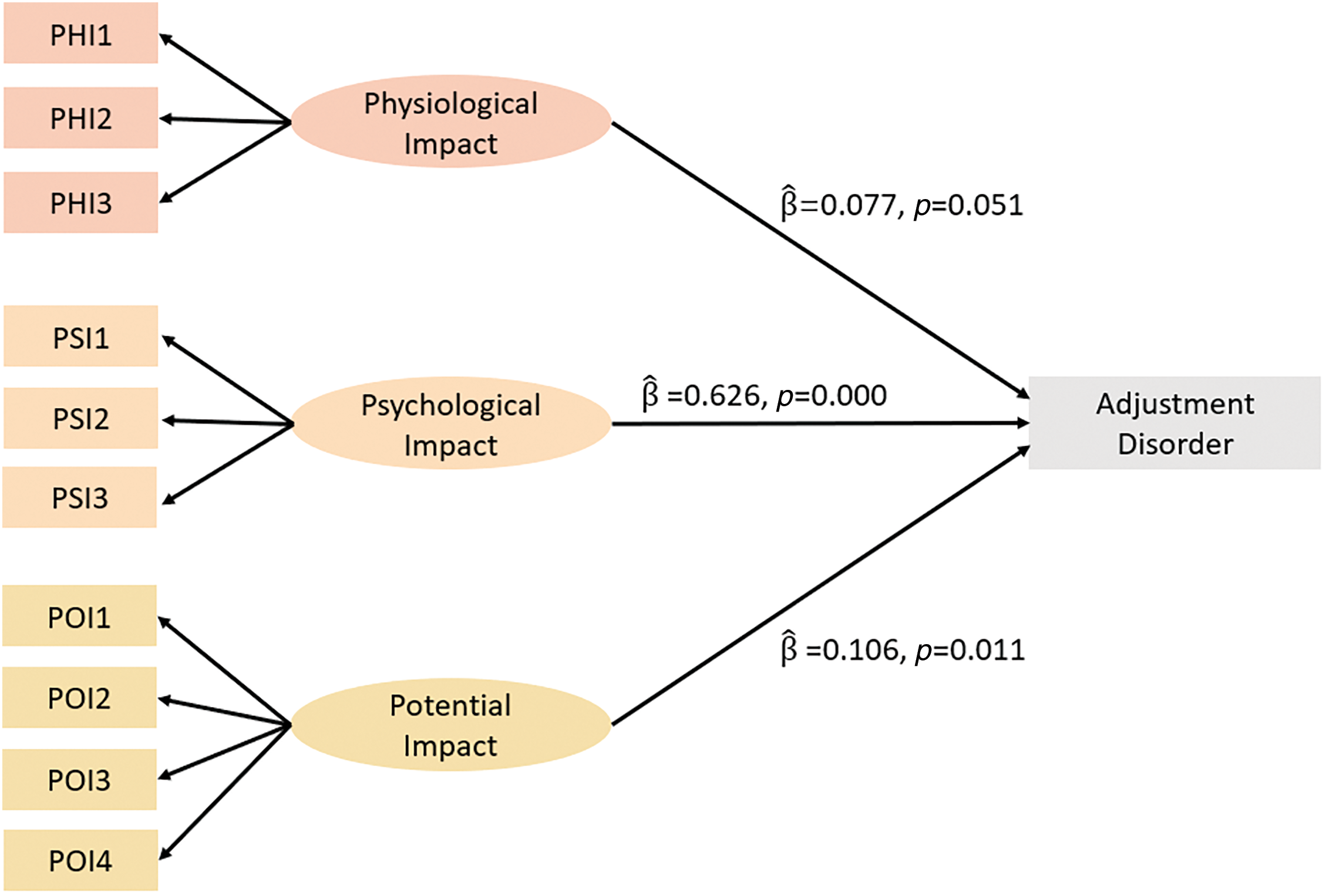
Figure 2: Structural equation modeling of physiological impact, psychological impact, and potential impact on adjustment disorder.
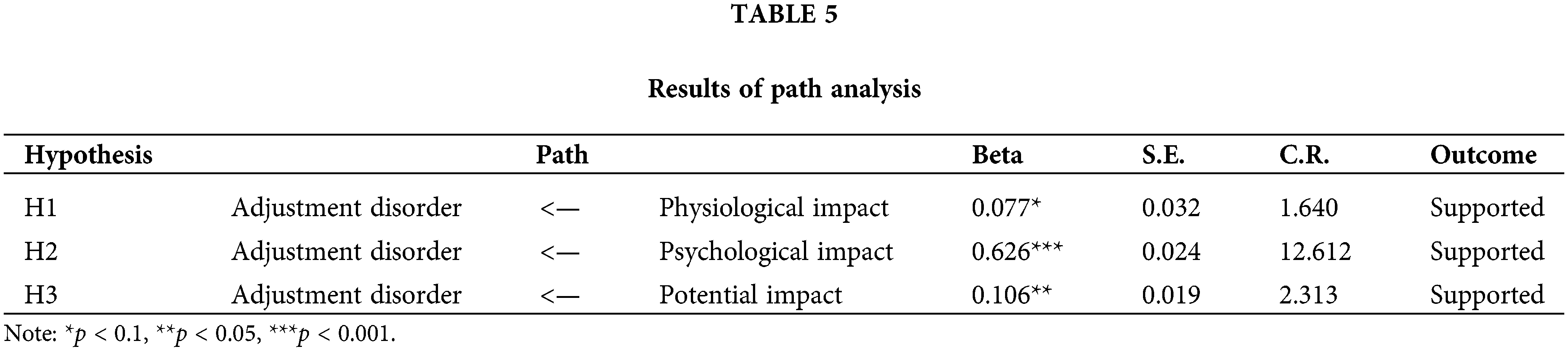
Analysis of Table 5 shows that physiological impact (
This exploratory study investigated the prevalence of adjustment disorder and its influencing factors among college students in the wave of COVID-19 after the implementation of the ten new measures. This study revealed that 75.63% of college students in this wave had a confirmed diagnosis of COVID-19, 28.68% of college students in this wave had an adjustment disorder. In addition, physiological impact, psychological impact and potential impact all had a significant positive effect on adjustment disorder.
Analysis of the prevalence of adjustment disorder
Until now, only a few studies have investigated the prevalence of adjustment disorder during the COVID-19 pandemic. Rossi conducted a study in Italy during the initial phase of the COVID-19 outbreak and reported a slightly higher prevalence of adjustment disorder at 22.9% [42]. By surveying a large sample of Poles, Dragan found that during the first weeks of the COVID-19 pandemic and embargo, the Polish population had high rates of mental ill health, with 14% meeting diagnostic criteria for adjustment disorder after excluding other mental illnesses [37]. Lotzin studied adjustment disorder in 11 European countries during the first year of the COVID-19 epidemic and showed a self-reported prevalence of 18.2% for possible adjustment disorder [28]. The descriptive statistical analysis of this study shows that the prevalence of adjustment disorder in the COVID-19 wave after the implementation of the ten new measures was 28.68%, which is much higher than the prevalence of adjustment disorder during the COVID-19 pandemic studied above and the 7% prevalence of adjustment disorder at the time of Shevlin’s first survey [35]. This demonstrates that the wave of COVID-19 brought about by the implementation of the ten new measures contributed significantly to the prevalence of adjustment disorder among college students. This is also consistent with college students being more susceptible to the effects of the COVID-19 pandemic [43] and having a higher prevalence of mental health problems than the general population [44].
Analysis of factors influencing adjustment disorder
Since the target population of this study was college students, we designed a survey with characteristics corresponding to the actual situation of college students. However, our study showed that we did not find any of these characteristics associated with higher prevalence of adjustment disorder, regardless of gender, grade, poor students, only child, personality, physical condition, living alone, or infection with COVID-19. Taking gender as an example, all three earlier studies showed a positive association between female gender and self-reported symptoms of adjustment disorder during the initial phase of the COVID-19 pandemic [28,37,42]. Lotzin argues that as primary caregivers of children and older family members, women may bear an additional burden and therefore have a higher prevalence of adjustment disorder [28]. However, the respondents in this study were college students with no additional family burden, and there was no difference between genders. In addition, Jamshaid’s study found that COVID-19 exerted equal stress on students’ mental health and exacerbated their depression and anxiety equally regardless of gender [45], which may explain the fact that college students’ gender was not associated with a higher prevalence of adjustment disorder. Among the grade characteristics, although the statistical results showed that the effect of grade on the prevalence of adjustment disorder was not significant (χ2 = 5.263, p = 0.261), the prevalence of adjustment disorder was significantly higher in the senior year (46.67%) than in other grades. This may be due on the one hand to the small sample size (n = 30), and on the other hand to the fact that they are in a period of transition in their life stage, with concerns about adapting to a new social and geographical environment after graduation and confusion about the future [46]. This is similar to the results of Dafogianni’s study [47]. As for other characteristics, the possible explanation is that the massive liberalization after the implementation of the ten new measures led to a new wave of COVID-19, and a large number of people, including students, were infected with COVID-19. In the social environment of that time, everyone could be infected. Stress factors such as the sudden and dramatic increase in the risk of being infected, the surrounding family and friends infected with COVID-19, the fear of COVID-19 infection and the possibility of losing family/friends caused a high psychological burden for all college students without discrimination [48,49], resulting in a high prevalence of adjustment disorder across the different study characteristics.
Our study showed that the physiological impact (
Adjustment disorder is considered a sub-comprehensive mental disorder [50] that occurs in a variety of stressful situations and is a common mental illness [51]. It is mainly influenced by psychological factors [52], and sudden outbreaks can have a negative psychological impact on college students and even produce some mental health symptoms [53]. This is in line with the fact that psychological effects are significant and have the greatest impact. Jannini also confirmed in a previous study that psychological factors such as depression, anxiety and stress symptoms are closely related [52]. The physiological effects brought about during the COVID-19 pandemic, such as lifestyle changes, may have led to increased exposure of college students to related stressors [17], thus contributing to some extent to the prevalence of adjustment disorder. In addition, there are potential impacts of a sudden COVID-19 outbreak. Factors such as uncertainty about the development of the outbreak [54] and fear of infection and transmission of the virus [55] may continue to cause stress among college students, increasing the risk of poor health in both the short and long term [34], which promotes the prevalence of adjustment disorder. This is consistent with Lotzin’s finding that individuals may experience more psychological distress and AjD symptoms when faced with a long-term COVID-19 pandemic [28]. Due to the psychological vulnerability of college students, any disturbance can have a profound long-term impact on the lives of individuals [56]. Therefore, in the face of public health emergencies, while providing psychosocial support and mental health services for college students to cope with the physical and mental health effects of diseases [18,57], it is also necessary to pay attention to potential factors such as stressors of college students [13], so as to reduce the adverse effects of public health emergencies.
Only a few studies have investigated the prevalence of adjustment disorder during the COVID-19 pandemic, and the influencing factors were mainly studied by demographic characteristics. We fill this study by introducing the International Adjustment Disorder Questionnaire and incorporating the Chinese context to explore the influences of adjustment disorder among college students facing public health emergencies. Moreover, the larger sample size and the sampling time frame corresponding to the peak of the COVID-19 pandemic after the implementation of the ten new measures are strengths of this study. However, some limitations may affect the generalizability of the findings reported in this study. The use of convenience sampling in this study limits the ability to provide a perfect representation of the population and may introduce systematic errors, so caution should be exercised when generalizing to the general population. In addition, most of the items addressing impact factors were self-constructed and not psychometrically tested. Finally, because public health events occur suddenly, we cannot assess the psychological status of individuals prior to the outbreak of a disaster. Future studies could use random sampling and incorporate more established impact factor scales to better generalize the findings.
This exploratory study analyzed the prevalence and influencing factors of adjustment disorder among college students facing public health emergencies, which may help to identify influencing factors to be explored in future studies, and made some suggestions on how the government can safeguard the mental health of college students.
This study showed that college students under the sudden COVID-19 epidemic had a higher prevalence of adjustment disorder among the surveyed college students, and there was no significant difference in the prevalence of adjustment disorder between different demographic characteristics. The physiological impact, psychological impact, and potential impact of the outbreak COVID-19 were all significantly positive, with the psychological impact being the greatest. The government should provide psychosocial support and mental health services for college students while also paying attention to potential factors such as stressors in order to reduce the adverse effects of sudden outbreaks.
Acknowledgement: We would like to thank the participants who filled out the online questionnaire.
Funding Statement: This research was funded by the National Social Science Fund of China (Grant No. 20BTJ005).
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Rong Fu; data collection: Rong Fu; analysis and interpretation of results: Luze Xie; draft manuscript preparation: Luze Xie. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data can be obtained by contacting the authors.
Ethics Approval: Ethical review and approval for research with human participants was not required in accordance with local legislative and institutional requirements. Written informed consent for participation was not required for this study in accordance with national legislation and institutional requirements.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Harapan H, Itoh N, Yufika A, Winardi W, Keam S, Te H, et al. Coronavirus disease 2019 (COVID-19a literature review. J Infect. 2020;13(5):667–73. [Google Scholar]
2. Xue Y, Pyong KH, Oh SS, Tao Y, Liu T. Analysis of the Impacts on the psychological changes of Chinese returning college students after the outbreak of the 2019 coronavirus disease. Front. 2022;10:916407. [Google Scholar]
3. Eurosurveillance Editorial Team. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill. 2020;25(5):pii=200131e. doi:https://doi.org/10.2807/1560-7917.ES.2020.25.5.200131e. [Google Scholar] [PubMed] [CrossRef]
4. Karimi A, Tabatabaei SR, Shiva F, Hoseinialfatemi SM. COVID-19 or influenza, or both? A comparison and algorithmic approach to management. Jundishapur J Microbiol. 2021;13(12):e112121. doi:https://doi.org/10.5812/jjm.112121. [Google Scholar] [CrossRef]
5. Xinhua. Xinhua Commentary: is China really ill-prepared for its new phase of COVID response? Available from: https://english.news.cn/20230120/23ddb76dee964dd6a9f934e507ae4bae/c.html. [Accessed 2023]. [Google Scholar]
6. Xinhua. China Focus: China releases measures to optimize COVID-19 response. Available from: https://english.news.cn/20221111/d4399114a082438eaac32d08a02bf58d/c.html. [Accessed 2022]. [Google Scholar]
7. Xinhua. China Focus: COVID-19 response further optimized with 10 new measures. Available from: https://english.news.cn/20221207/ca014c043bf24728b8dcbc0198565fdf/c.html. [Accessed 2022]. [Google Scholar]
8. Leung K, Lau EHY, Wong CKH, Leung GM, Wu JT. Estimating the transmission dynamics of SARS-CoV-2 Omicron BF.7 in Beijing after adjustment of the zero-COVID policy in November–December 2022. Nat Med. 2023;29(3):579–82. [Google Scholar] [PubMed]
9. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psych. 2020;33(2):e100213. [Google Scholar]
10. Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510–2. doi:https://doi.org/10.1056/NEJMp2008017. [Google Scholar] [PubMed] [CrossRef]
11. Mahat-Shamir M, Pitcho-Prelorentzos S, Kagan M, Kestler-Peleg M, Lavenda O. Adjustment disorder in the face of COVID-19 outbreak: the impact of death anxiety, media exposure, fear of contagion and hypochondriasis symptoms. Omega (Westport). 2021;87(4):1189–206. doi:https://doi.org/10.1177/00302228211034372. [Google Scholar] [PubMed] [CrossRef]
12. World Health Organization. ICD-11 for mortality and morbidity statistics. Available from: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/264310751. [Accessed 2023]. [Google Scholar]
13. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287(10224):112934. [Google Scholar] [PubMed]
14. Zhou SJ, Wang LL, Qi M, Yang XJ, Gao L, Zhang SY, et al. Depression, anxiety, and suicidal ideation in Chinese university students during the COVID-19 pandemic. Front Psychol. 2021;12:669833. [Google Scholar] [PubMed]
15. Penner F, Hernandez Ortiz J, Sharp C. Change in youth mental health during the COVID-19 pandemic in a majority Hispanic/Latinx US sample. J Am Acad Child Adolesc Psychiatry. 2021;60(4):513–23. [Google Scholar] [PubMed]
16. Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819–820. [Google Scholar] [PubMed]
17. Abe K, Daniunaite I, Truskauskaitė-Kunevičienė I, Sugimura K, Zelviene P, Hihara S, et al. Cross-cultural comparison of ICD-11 adjustment disorder prevalence and its risk factors in Japanese and Lithuanian adolescents. Brain Sci. 2022;12(9):1172. [Google Scholar] [PubMed]
18. Browning MHEM, Larson LR, Sharaievska I, Rigolon A, McAnirlin O, Mullenbach L, et al. Psychological impacts from COVID-19 among university students: risk factors across seven states in the United States. PLoS One. 2021;16(1):e0245327. [Google Scholar] [PubMed]
19. Cao H, Zhang HW, Yang L, Li L, Wang JZ, Zada B, et al. Analysis of the mediating effect of risk perception on the relationship between time perception and mental health of college students during the COVID-19 epidemic. Front. 2021;12:749379. [Google Scholar]
20. Zhang Y, Bao X, Yan J, Miao H, Guo C. Anxiety and depression in chinese students during the COVID-19 pandemic: a meta-analysis. Front. 2021;9:697642. [Google Scholar]
21. Sun YY, Zhu SY, ChenHuang G, Zhu LY, Yang SH, Zhang XC, et al. COVID-19 burnout, resilience, and psychological distress among Chinese college students. Front. 2022;10:1009027. [Google Scholar]
22. Wasserman D, van der Gaag R, Wise J. The term physical distancing is recommended rather than social distancing during the COVID-19 pandemic for reducing feelings of rejection among people with mental health problems. Eur Psychiatr. 2020;63(1):e52. [Google Scholar] [PubMed]
23. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. [Google Scholar] [PubMed]
24. Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. 2020;89:531–42. [Google Scholar]
25. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. [Google Scholar] [PubMed]
26. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and Initial validation. Int J Ment Health Addict. 2022;20(3):1537–45. [Google Scholar] [PubMed]
27. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–20. [Google Scholar] [PubMed]
28. Lotzin A, Krause L, Acquarini E, Ajdukovic D, Ardino V, Arnberg F, et al. Risk and protective factors, stressors, and symptoms of adjustment disorder during the COVID-19 pandemic–first results of the ESTSS COVID-19 pan-European ADJUST study. Eur J Psychotraumatol. 2021;12(1):1964197. [Google Scholar] [PubMed]
29. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277(1):55–64. [Google Scholar] [PubMed]
30. Xinhua. China reports declining critical COVID-19 cases as peaks pass. Available from: https://english.news.cn/20230115/6dfa4992461f4481a8c9faeb13e344cc/c.html. [Accessed 2023]. [Google Scholar]
31. Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39(5):355–7. [Google Scholar] [PubMed]
32. Ke D, Chen W. Comparative study on residents’ health-promoting lifestyle and life satisfaction in wuhan before and after the COVID-19 pandemic. Front. 2022;10:820499. [Google Scholar]
33. Ferrucci R, Averna A, Marino D, Reitano MR, Ruggiero F, Mameli F, et al. Psychological impact during the first outbreak of COVID-19 in Italy. Front. 2020;11:559266. [Google Scholar]
34. Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ. 2020;17(22):8479. [Google Scholar]
35. Shevlin M, Hyland P, Ben-Ezra M, Karatzias T, Cloitre M, Vallières F, et al. Measuring ICD-11 adjustment disorder: the development and initial validation of the international adjustment disorder questionnaire. Acta Psychiatr Scand. 2020;141(3):265–74. [Google Scholar] [PubMed]
36. Zhang N, Jia W, Lei H, Wang P, Zhao P, Guo Y, et al. Effects of human behavior changes during the coronavirus disease 2019 (COVID-19) pandemic on influenza spread in Hong Kong. Clin Infect Dis. 2021;73(5):e1142–50. [Google Scholar] [PubMed]
37. Dragan M, Grajewski P, Shevlin M. Adjustment disorder, traumatic stress, depression and anxiety in Poland during an early phase of the COVID-19 pandemic. Eur J Psychotraumatol. 2021;12(1):1860356. [Google Scholar] [PubMed]
38. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092. [Google Scholar] [PubMed]
39. Jackson DL, Gillaspy JA, Purc-Stephenson R. Reporting practices in confirmatory factor analysis: an overview and some recommendations. Psychol Methods. 2009;14(1):6–23. [Google Scholar] [PubMed]
40. Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39–50. [Google Scholar]
41. Bagozzi RP, Yi Y, Phillips LW. Assessing construct validity in organizational research. Adm Sci Q. 1991;36(3):421. [Google Scholar]
42. Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. 2020;11:790. [Google Scholar]
43. Tsaava M, Oniani N, Eliozishvili M, Sakhelashvili I, Tkemaladze N, Aladashvili T, et al. Age-based differences in sleep quality, pre-sleep arousal, and psychosocial factors during the second wave lockdown of the COVID-19 pandemic in Georgia—a higher vulnerability of younger people. Int J Environ. 2022;19(23):16221. [Google Scholar]
44. Stallman HM. Psychological distress in university students: a comparison with general population data. Aust Psychol. 2010;45(4):249–57. [Google Scholar]
45. Jamshaid S, Bahadar N, Jamshed K, Rashid M, Imran Afzal M, Tian L, et al. Pre- and post-pandemic (COVID-19) mental health of international students: data from a longitudinal study. Psychol Res Behav. 2023;16:431–46. [Google Scholar]
46. Acharya L, Jin L, Collins W. College life is stressful today–emerging stressors and depressive symptoms in college students. J Am Coll Health. 2018;66(7):655–64. [Google Scholar] [PubMed]
47. Dafogianni C, Pappa D, Mangoulia P, Kourti FE, Koutelekos I, Dousis E, et al. Anxiety, stress and the resilience of university students during the first wave of the COVID-19 pandemic. Healthcare. 2022;10(12):2573. [Google Scholar] [PubMed]
48. Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2020;22(9):e22817. [Google Scholar] [PubMed]
49. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. 2020;14(1):20. [Google Scholar]
50. Israelashvili M. Should adjustment disorder be conceptualized as transitional disorder? In pursuit of adjustment disorders definition. J Ment Health. 2012;21(6):579–88. [Google Scholar] [PubMed]
51. Myung W, Na KS, Ham BJ, Oh SJ, Ahn HW, Jung HY. Decreased medial frontal gyrus in patients with adjustment disorder. J Affect Disord. 2016;191(1083–1090):36–40. [Google Scholar] [PubMed]
52. Jannini TB, Rossi R, Socci V, Reda F, Pacitti F, Di Lorenzo G. Psychometric and factorial validity of the international adjustment disorder questionnaire (IADQ) in an Italian sample: a validation and prevalence estimate study. Clin Psychol Psychoth. 2023;30(2):436–45. [Google Scholar]
53. Sankhi S, Marasine NR. Impact of COVID-19 pandemic on mental health of the general population, students, and health care workers: a review. Europasian J Med Sci. 2020;2:64–72. doi:https://doi.org/10.46405/ejms.v2i2.131. [Google Scholar] [CrossRef]
54. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. [Google Scholar] [PubMed]
55. Cowie H, Myers C. The impact of the COVID-19 pandemic on the mental health and well-being of children and young people. Child Soc. 2021;35(1):62–74. [Google Scholar] [PubMed]
56. Patsali ME, Mousa DPV, Papadopoulou EVK, Papadopoulou KKK, Kaparounaki CK, Diakogiannis I, et al. University students’ changes in mental health status and determinants of behavior during the COVID-19 lockdown in Greece. Psychiatry Res. 2020;292(5):113298. [Google Scholar] [PubMed]
57. Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. 2020;29:e181. [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools