 Open Access
Open Access
REVIEW
Meaning in Life and Mental Health Issues in Older Adults: A Meta-Analysis
1 School of Public Management, Inner Mongolia University, Hohhot, 010021, China
2 School of Psychological and Cognitive Sciences and Beijing Key Laboratory of Behavior and Mental Health, Peking University, Beijing, 100091, China
3 The Third Hospital of Beijing Chaoyang District, Beijing, 100091, China
4 School of Economics and Management, Center for China Social Trust Research, and Institute of Psychological and Cognitive Sciences, Fuzhou University, Fuzhou, 350108, China
* Corresponding Author: Yiqun Gan. Email:
International Journal of Mental Health Promotion 2023, 25(9), 971-984. https://doi.org/10.32604/ijmhp.2023.029155
Received 04 February 2023; Accepted 16 May 2023; Issue published 10 August 2023
Abstract
This study aims to be the first to use meta-analysis to explore the relationship between meaning in life (MIL) and mental health issues among older adults. A meta-analysis was conducted using six databases, resulting in 16 studies with 5,074 participants in total. The “metacor” and “forestplot” packages in R-Studio were used for data analysis. The total effect was calculated using a random-effects model, with I² = 86% in the heterogeneity test. The results showed a moderate negative correlation between MIL and mental health issues among older adults, with an average effect of −0.37. Five potential moderating variables were examined: the conceptualization of MIL (value vs. purpose), region (Asian vs. Western countries), residence status (community vs. nursing home vs. hospital), types of mental health issues, and evaluation methods (clinical vs. non-clinical). The first four had no significant moderating effect. The mean correlation coefficients between mental health issues and value/purpose were −0.49/−0.33; the mean correlation coefficients in Asian countries and Western countries were −0.48 and −0.34; the mean correlation coefficients among participants living in community/nursing home/mixed status were −0.33/−0.40/−0.40; the mean correlation coefficients between MIL and depression/others were −0.37/−0.35; however, the negative relationship between MIL and mental health issues was stronger when non-clinical evaluations (self-report only) were used. Specifically, the mean correlation coefficient for non-clinical evaluations was −0.42 and for clinical evaluations was −0.29. This study is the first meta-analysis to identify the negative correlation between older adults’ MIL and mental health issues. Significant moderating effects of evaluation methods were found.Keywords
Current mental health status of older adults
The global population is aging rapidly [1]. From 2015 to 2050, the world’s population over 60 years of age is expected to increase from 12% to 22%, and the absolute number will rise from 900 million to 2 billion. Related to these trends, about 15% of people in this age group suffer from mental disorders, which poses unprecedented significant challenges for most countries. Consequently, nations must ensure that their health and social systems are well prepared to cope with this demographic shift [2].
A mental health issue refers to a mental health problem or mental illness caused by biological, psychological, and/or social factors. It is a broad concept that includes different types of psychological disorders and problems that interfere with cognitive, social, or emotional aspects of functioning. Previous studies have examined mental health issues such as depression, anxiety, stress, self-injury, schizophrenia, sleep disorders, and eating disorders [3–7]. According to the WHO report, among older adults over 60 years of age worldwide, the most common mental health issues are depression, anxiety, and substance abuse, with depression being the most prevalent. The incidence of depression was 7%, followed by anxiety (3.8%) and substance abuse (1%). However, substance abuse problems among older adults are often overlooked or misdiagnosed. In addition, approximately 25% of deaths from self-harm are among people aged 60 years or older [8].
Geriatric depression is known to be one of the most common mental health issues in adults over 60 years of age [9]. For older adults, concerns about declining health, possible economic problems, age discrimination, loneliness, the possibility of dying, and the death of friends and significant others could lead to depression [10,11]. Anxiety is also one of the most common mental health issues among older adults [12]. Studies on anxiety-related factors in older adults have shown that cognitive impairment, chronic medical conditions, negative perceptions about health, functional limitations, and female gender increase the risk of having an anxiety disorder [13]. Lastly, loneliness is a major mental health issue among older adults [14]. The level of loneliness reported by older adults was relatively higher than that reported by the youth population [15]. Given these major mental health issues, the current study conducted an analysis of studies that focused on depression, anxiety, substance abuse, self-harm, and loneliness in older adults. This study aims to explore the effect of meaning in life (MIL) on mental health issues through meta-analysis. As mental health is important to successful aging [16], the study will provide a theoretical and practical basis for preventing mental health issues and promoting successful aging.
MIL and mental health among older adults
Meaning in life as an “umbrella term” contains some other narrower constructs. From the perspective of measurement, the “two-dimensional model” of meaning proposed by Steger et al. is widely recognized, which divides meaning in life into “search for meaning” and “presence of meaning” [17]. Heintzelman and King summarized the three core components of meaning in life from the levels of cognition, emotion and motivation, respectively: coherence, significance and purpose [18]. In this meta-analysis, the definition of meaning in life is consistent with the meta-analysis of C, that is, meaning in life includes two dimensions: order and purpose [19].
MIL has a protective function against negative mental health states [20], and a lack of MIL has been positively associated with depression, despair, and self-reported health problems and negatively associated with mental health [21]. Old age is a mentally and physically stressful stage of life. Older adults may experience stress from various sources such as stress-related events [22], health problems [23], loss of a spouse or a friend [24], or self-management [25]. All of these may awaken different needs and present different adaptive challenges for older adults. Fortunately, MIL can act as a resource that can cushion the effect of mental and physical stress in old age.
However, research on the relationship between MIL and older adults’ mental health issues has been inconsistent. Some studies have shown that older adults who have a sense of MIL are less likely to be depressed [26,27] or experience anxiety [28]. On the other hand, in a five-year longitudinal study, MIL was found to have no protective effect against depression in very old adults [29]. The relationship between MIL and mental health issues may vary with different psychological, physiological, and social environments. Therefore, it is necessary to conduct a meta-analysis of the relationship and explore the possible moderating mechanism.
MIL is an important factor in promoting positive emotions and well-being [30]. Thus, MIL is a powerful predictor of successful aging and emotional and physical well-being [28]. Studies have found a positive correlation between MIL and overall psychological well-being in older adults [28,31], and older adults who had MIL tended to have better physical [32] and mental health [26] compared to those who had less sense of MIL. In terms of negative outcomes, a lack of MIL has been related to depression [29], despair and health issues [21], risk of mild cognitive impairment [33], and premature mortality [34]. The correlation curve of age and MIL is similar to the “J” distribution, which is initially lower in youth but gradually gets higher around middle age, and finally shows the strongest correlation in old age [35], which explains why there is a particular need to examine MIL in older adults. Meta-analytic studies have verified a positive correlation between MIL and positive health outcomes [36,37]; however, there is a lack of meta-analysis on the relationship between MIL and negative health outcomes in older adults. This study aimed to address this gap in the literature.
Moderators in the relationship between MIL and mental health issues among older adults
As an umbrella term, MIL contains other narrower constructs [19], which makes it more difficult to define accurately. Based on the meaning-making model proposed by Park [38], this study conceptualized MIL as (1) the value (or meaningfulness) of life, comprising beliefs about the world, self, and relationships between them, or (2) one’s life’s goals and purposes. Frankl [39] pointed out that the ultimate MIL lies in the sense of serving a more ambitious and transcendent goal. Some theoretical models suggest that MIL consists of three components: a sense of harmony, purpose, and meaning [40].
Some studies defined MIL as a purpose and investigated its relationship with mental health and subjective well-being [15,28,41]. However, Homan et al. [42] considered having a sense of MIL is part of well-being, reflecting its meaning and value connotation. Therefore, this study explored whether there are differences in the value vs. purpose dimensions of MIL in their relation to mental health issues in older adults. This is an important distinction in understanding the underlying mechanisms in this relationship.
The relationship between MIL and mental health issues may be related to the different types of mental health issues among older adults. The present study focused on depression, anxiety, and other issues such as suicide and loneliness to explore whether there are differences in the relationship between MIL and mental health based on the type of issue.
Culture in different regions may play an essential role in the relationship between MIL and mental health, as it can strongly influence individual values, expectations, and needs [43]. MIL depends mainly on cultural and ethnic contexts [44]. Culture provides individuals with a theory of what the world looks like, including what makes sense and how to gain meaning [45]. Indeed, cross-cultural differences in the association between meaning and psychological well-being have been found [46].
Older adults in Asia live in collectivistic cultures, while in Western countries, they live in individualistic cultures [47]. Because individualistic culture construes the self as an independent individual, individualism tends to increase self-evaluation [48]. Collectivistic culture construes the self as interdependent, that individuals exist in relation to others, and therefore people tend to criticize themselves [49]. Given this conceptualization of cultures, we speculated that culture influences the formation of values, meaning, and memorable experiences, which would affect the relationship between MIL and mental health. However, there is a lack of cross-cultural research on MIL and the mental health issues of older adults. Therefore, it is necessary to explore the moderating effects of culture.
Various studies have confirmed that the residence status of older adults affects their mental health. Living in nursing homes or communities for older people can affect their mental and spiritual health, as well as their search for MIL [50]. Although no differences were found in the prevalence of depression in older adults living in nursing homes or community dwellings [50,51], institutionalized older adults were found to have higher levels of spirituality than those living in the community [52]. In addition, single older adults living in community dwellings were found to have a higher willingness to “search for the MIL” than the “presence of MIL” [50]. However, it is not clear whether different residence statuses have different effects on the relationship between MIL and mental health issues in older adults.
Assessment of mental health issues
The way mental health issues are assessed could be a possible moderator [19]. In the present study, the evaluation methods in the reviewed studies were divided into clinical and non-clinical methods. The clinical method combined a self-report scale and face-to-face diagnostic interview, making it more professional and rigorous. The non-clinical method involved only a self-report scale. Even with the risk of subjectivity, most evaluations were conducted in a non-clinical way, mainly because of their convenience and low cost [53]. Self-reported mental health issues may depend on individuals’ self-evaluation, cognition, and goals, which are involved in MIL [54]. Therefore, this study explores whether method of evaluation moderates the relationship.
This study aimed to explore the relationship between MIL and mental health issues among the older adults through a meta-analysis. Several moderators were involved: the conceptualization of MIL (value vs. purpose), regions (Asian vs. Western countries), residence status (community vs. nursing home vs. hospital), evaluation methods (clinical vs. non-clinical), and types of mental health issues.
The research question of this meta-analysis is, to what extent is the MIL related to mental health issues in the older adults, and whether the conceptualization of MIL, culture, residence status, evaluation methods and types of mental health issues play a moderating role?
This study was registered on the OSF (osf.io/4cs6y). Inclusion criteria were changed from registration to study completion. The dependent variables selected at registration were mental health, depression, anxiety, substance abuse, and self-harm. The dependent variable of “mental health” was removed during the study because mental health is a positive psychological dimension, while the other dependent variables are negative dimensions. To make the research question clearer and focus on the relationship between older adults’ MIL and mental health issues, in addition to mental disorder, several common mental health issues were added as dependent variables in this study, including loneliness, distress and stress.
In this meta-analysis, the inclusion criteria were as follows. First, the mean age of the participants had to be greater than 60 years. If the study included multiple groups, it should have at least one group that included participants aged 60 or older. Second, the participants had no severe cognitive problems or deficits. Third, the independent variable was MIL. Lastly, dependent variables included common mental health issues in older people, including depression, anxiety, substance abuse, self-traumatic behavior, and loneliness.
When the study involved the evaluation of two or more mental health issues in the same article, the study was included, but different mental health issues were calculated separately in data coding and analysis. For research types, experimental studies, cross-sectional surveys, longitudinal surveys, and interventions were included. Other criteria included peer-reviewed articles written in English. We wrote to authors to request the full-text articles that we could not retrieve online. We were unable to include articles in which we did not get a reply after making two requests.
This study was conducted per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [55]. Six electronic databases were searched to ensure the comprehensiveness of the literature: APA PsycArticles, APA PsycInfo, Medline, Psychology, Behavioral Sciences Collection, and Web of Science.
For database retrieval strategies, the search keywords for older adults were as follows: “old people” OR “older adult” OR “elderly” OR “aged people” OR “senior citizens” OR “old population.” For the search of MIL, the keywords were as follows: “meaning” OR “meaning of life” OR “MIL” OR “sense of meaning” OR “global beliefs” OR “purpose in life” OR “life purpose.” For the mental health issues of older adults, the keywords were as follows: “mental disorder” OR “depression” OR “anxiety” OR “substance use” OR “substance abuse” OR “self-harm” OR “loneliness” OR “distress” OR “stress.” The articles selected were published from January 1990 to January 2020 and were peer-reviewed and written in English. In the first stage, there were 1,185 articles regarding MIL and common mental health issues of older adults. Of the 1,185 articles, 206 duplicates were excluded, leaving 979 in total. Endnote X9 was used for document management.
In the second stage, three of the authors independently viewed the titles and abstracts of articles for literature screening to confirm the potential targeted studies. When the authors did not meet a consensus on whether the articles met the screening criteria, the consensus method was used to discuss and judge the article. Ultimately, 71 articles containing keywords regarding MIL and mental health issues of older adults were selected.
In the third stage, to ensure the comprehensiveness of the retrieval, the authors sifted through the remaining articles’ references according to inclusion and exclusion criteria and added 14 more articles. Three of the authors (those who participated in the second stage) read the full text separately to determine whether the 85 articles satisfied the inclusion criteria and included studies that analyzed the correlation coefficient between MIL and mental health issues. Eighteen articles met all inclusion criteria.
In the last stage, two articles were excluded because of their low quality (see below for quality assessment criteria), and thus we used 16 articles for data encoding and analysis. Due to the long period involved in conducting the study and writing the paper, to avoid omissions during this period, we conducted a supplementary search in April 2023. No additional qualified articles were found in the six databases among articles. Fig. 1 illustrates the screening process, and the process and results of the systematic review are reported in the PRISMA format [55].
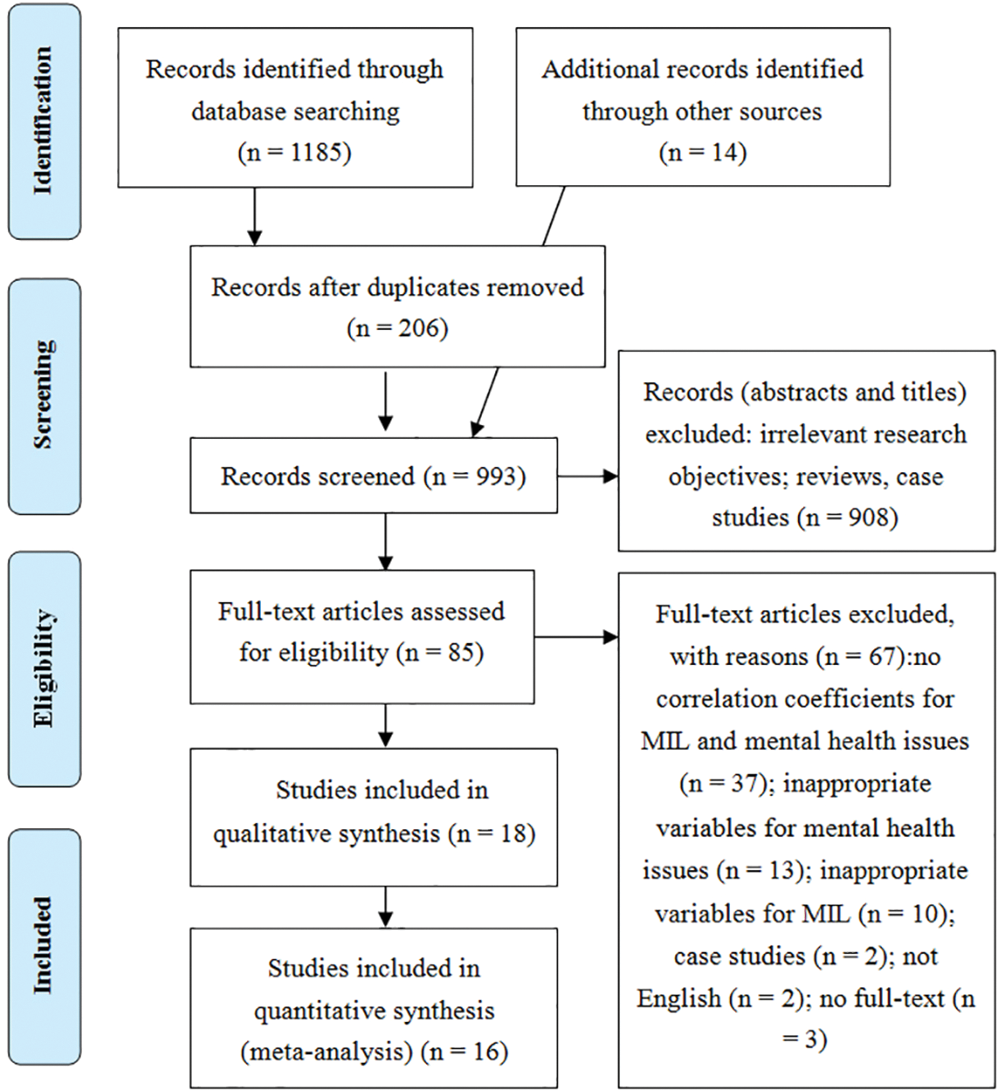
Figure 1: The flow chart of the selection process.
To account for the risk of bias in individual studies, the standard quality assessment criteria determined the methodological quality of the included studies [56], and the following quality criteria were used:
(a) Sufficiently described research questions
(b) Appropriate research design
(c) Described the appropriate method for selecting participants
(d) Sufficiently described the characteristics of participants
(e) Had well defined measures
(f) Justified analytic methods
(g) Results reported in sufficient detail
(h) Supporting conclusions
Quality assessment was conducted independently by three authors. The response scale for quality assessment was yes (2 points), partial (1 point), and no (0 points). Studies that met the threshold of 65% of the maximum score were included (moderate to high quality; min = 68.5%, max = 100%, SD = 7.98, M = 88.62) [56]. Cohen’s κ coefficient was moderate and ranged from 0.25 to 1 (M = 0.623) with all ps < 0.05, indicating acceptable concordance.
Defining and coding of variables
For this study, the independent and dependent variables were encoded in the following manner: (1) the definition of MIL is consistent with Park’s concept of MIL and was defined as the belief that one’s life is valuable/meaningful or purposeful [19]; (2) mental health issues included depression, anxiety, substance abuse, self-harm [2], loneliness [15], distress, and stress [57].
To explore the factors influencing the relationship between MIL and mental health issues, the following moderating variables were coded: conceptual dimension of MIL, the types and evaluation of mental health issues, participants’ geographic location, and participants’ residence status.
Based on Czekierda’s definition of MIL [19], we coded it into two dimensions: value and purpose. “Value” is an individual’s beliefs regarding the world’s rules. If MIL was measured by knowledge regarding oneself and one’s relationship with the world, it was coded as “meaning-value.” “Purpose” is the worth and motivational characteristic of MIL. If MIL was measured by the individual’s life goal or purpose, it was coded as “meaning-purpose.” If more than 50% of the items in the measuring tool were related to themes such as “life has value,” “significance,” and “meaningful,” its conceptual dimension was considered “meaning-value.” Correspondingly, if more than 50% of the items in the measuring tool were related to themes such as “goal,” “purpose,” “future plan,” and “aim,” its conceptual dimension was considered “meaning-purpose.” There was no tool with an even number of items in both categories.
Although there were many keywords related to mental health issues in document retrieval, the ones included in the final 16 articles for analysis were depression, anxiety, and loneliness. Some articles measured depression and anxiety among the same participants. In such articles, the correlations between MIL, depression, and anxiety were calculated separately [28]. Then, only the correlation coefficient between MIL and anxiety was used, and the mental health issue was coded as anxiety. Since we wanted to compare the results of different mental health issues as comprehensively as possible, and the vast majority of mental health issues are depression, when there are two or more dependent variables, only the dependent variable that is not depression is retained.
The residence status of the sample was divided into three categories: community, nursing home, and hospital. If participants lived at home, they were coded as a “community” sample. If they lived in a nursing home or a welfare institution, they were coded as “nursing home.” They were coded as “hospital” if the participants were hospitalized during the study. If there was more than one type of residence, it was coded as “mixed.”
The geographic region in which the study was conducted was categorized as Asian or Western countries to explore whether there were significant differences in the relationship between MIL and mental health among older adults in different regions and cultural orientations.
Evaluation methods used to assess mental health were classified into clinical or non-clinical according to how the researchers specified and confirmed the mental health issue. For example, if the researcher(s) only used a scale to specify the issue and did not include a clinical diagnosis, it was coded as “non-clinical” [58]. Correspondingly, if the study indicated that a diagnostic evaluation was performed, it was coded as “clinical” [59].
The three authors performed data extraction to ensure that at least two people read each article. If the extracted data were inconsistent, the authors read and discussed it again, eventually achieving a consensus.
Meaning-value. Meaning-value scales included the following measures: Sources of MIL Profile [SOMP; 60], MIL Scale [61], Schedule for MIL Evaluation [SMiLE; 62], a shortened version of the MIL Scale devised by Krause [32], Experienced MIL Scale [EMIL; 63], a composite index of the Life Attitude Profile [LAP; 64], two interview questions [65], and a composite index of the Life Purpose subscale of the LAP [LAP; 64].
Meaning-purpose. Meaning-purpose scales included the following measures: Purpose of Life Scale [66], Chinese Purpose in Life Scale [67], Purpose in Life Test [68,69], and MIL Questionnaire [MLQ; 17].
Instruments used in studies classified as non-clinical. The scales used in the non-clinical studies included the following: Beck Depression Inventory [70], 4-item Geriatric Depression Scale [71], 15-item Geriatric Depression Scale [72], 15-item short version of the Geriatric Depression Rating Scale [GDRS; 73], Chinese version of the Geriatric Depression Scale [74], Zung Self-Rating Depression Scale [75], 14-item Hospital Anxiety and Depression Scale [76], seven items from the CES-D [77], UCLA Loneliness Scale [78], Patient Health Questionnaire-9 [PHQ-9; 79], and Perceived MIL subscale of the Geriatric Suicide Ideation Scale [21].
Instruments used in studies classified as clinical. The clinical studies used the Diagnostic and Statistical Manual of Mental Disorders-IV [DSM-IV; 80] and the Composite International Diagnostic Interview 65+ [CIDI65+; 81].
The “metacor” and “forestplot” software packages in R-Studio were used for data analysis. The primary analysis focused on estimating the combined effect size and heterogeneity using the random-effects model method [82]. The Pearson correlation coefficient was considered to indicate the effect size initially; when the original text did not report a Pearson correlation, the indicated index was converted to a Pearson correlation coefficient according to Card’s method [83]. His book details the formula for calculating Pearson r from the effect size in the primary study. In a study that contained multiple correlation coefficients, the coefficients were combined, and then the total effect size was obtained using the method described by Borenstein et al. [84]. Therefore, according to this procedure, the correlation coefficient was converted into Fisher’s z to demonstrate the final result’s combined total effect size.
This study ensured that the internal consistency reliability coefficient of the articles included was greater than 0.60. Q-statistics to minimize the measurement error, which can evaluate the dispersion of effects in the χ2 distribution [85], were used to evaluate the heterogeneity of data included in the meta-analysis. I² was also adopted to evaluate the heterogeneity of the data, to measure the observed percentage of variability due to heterogeneity between the research results rather than accidental effects [84]. The effect at each level was calculated to examine moderating effects. The meta-regression method was used to adjust the variation between the groups. A funnel chart test (see Fig. 2) and Egger’s test were conducted to investigate possible asymmetry in publishing bias.
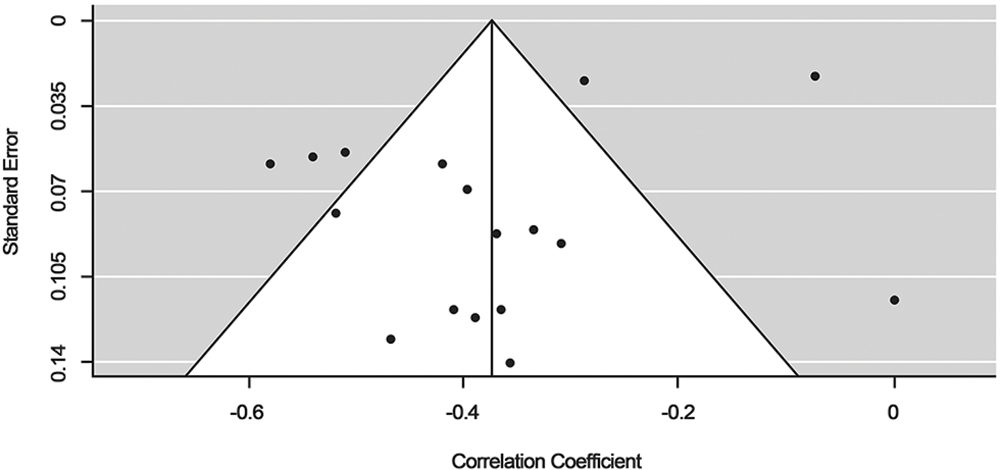
Figure 2: Funnel plot of the distribution of the effects.
Table 1 presents the sample characteristics, variables, and measurements for 17 sample groups from the 16 studies included in the meta-analysis. One of the studies demonstrated two correlations between MIL and mental health issues, one for older adults living in the community and one for those living in institutions [26].
The sample sizes ranged from 40 to 2,045, with a total of 5,074 participants for the 16 studies. The average age ranged from 66.98 to 91.3. There were five longitudinal follow-up surveys and 11 cross-sectional studies. One study was experimental [27], and there were no intervention studies. In 82.3% (k = 14) of the studies, the dependent variable was depression, 5.8% (k = 1) were concerned with anxiety, and 11.8% (k = 2) examined loneliness among older adults.
The total effect was calculated using a random-effects model, with I² = 86% in the heterogeneity test. The total effect of MIL on mental health was −0.37 (95% confidence interval [CI] [−0.451, −0.296], p < 0.001, k = 17, tau² = 0.020). This is considered to be a moderate effect size [95]. This result indicates that older people’s MIL was moderately and negatively correlated with mental health issues. Fig. 3 shows the effect size and the corresponding forest plot with a 95% CI of each study.
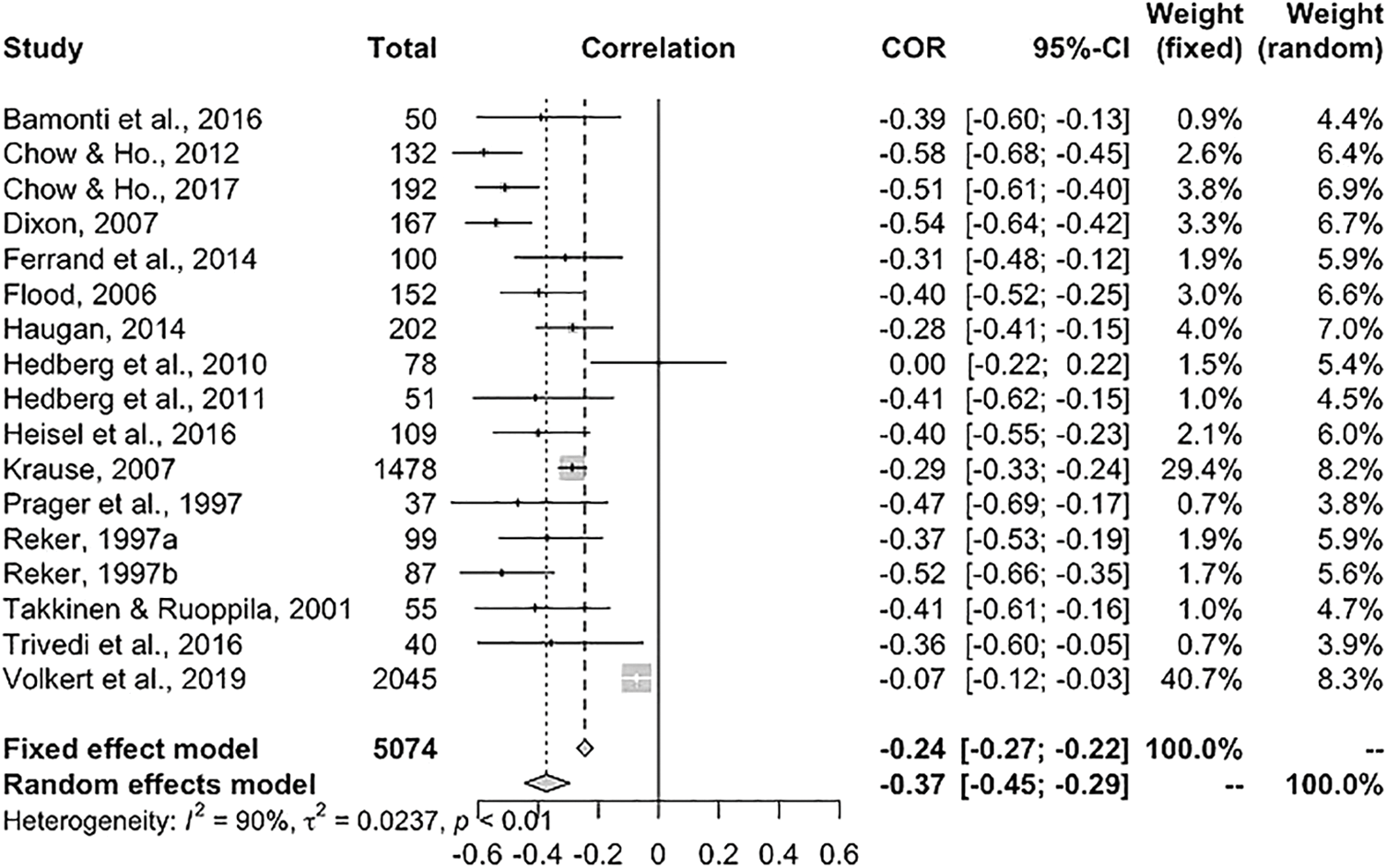
Figure 3: Distribution of effects of meaning in life and mental health issues in older adults.
To test whether the results were affected by publication bias (interdisciplinary study risk), a funnel plot, regression test, and rank test were used to calculate bias. The Reg-test suggested good symmetry of the funnel plot (z = −0.248, p = 0.804). The rank test was performed using the rank correlation test of the funnel plot. The results also showed good symmetry (Kendall’s tau = 0.191, p = 0.308).
Studies were classified into two categories to test the moderating effect of the value vs. purpose dimension in the relationship between MIL and mental health issues: (1) viewing MIL as value and significance and (2) viewing MIL as a life goal or purpose in life. Approximately 35.3% (k = 6) were encoded as “purpose,” while the remaining 64.7% (k = 11) were encoded as “value.” The moderation analysis showed no significant difference in the correlations of the different conceptualizations of MIL and mental health issues (p = 0.69), the mean correlation coefficients between mental health issues and value/purpose were −0.49/−0.33.
Different mental health issues, including depression, anxiety, and loneliness, did not significantly moderate the correlation. Because most articles (k = 14) had depression as a dependent variable, the moderating effect of depression was compared with other mental health issues, but no significant difference was observed (p = 0.98). The mean correlation coefficients between MIL and depression/others were −0.37/−0.35.
The studies were classified into two categories to examine the moderating effect of the region: (1) Western countries, including the United States, Canada, France, Norway, Sweden, Germany, Italy, Switzerland, Spain, and Finland (k = 13); and (2) Asian countries, including Israel and China (k = 4). The statistical results showed that there was no significant difference between Asian and Western countries (p = 0.52). The mean correlation coefficients in Asian countries and Western countries were −0.48 and −0.34.
Residence status in the 16 studies included living in the community (k = 10), a nursing home (k = 2), and mixed residence status (k = 4) (one study did not report the Residence status of the participants). The pairwise comparison showed no significant moderating effects were observed (ps > 0.05). The mean correlation coefficients among participants living in community/nursing home/mixed status were −0.33/−0.40/−0.40.
With regard to evaluation methods, 35.3% used methods that involved clinical diagnosis (n = 6), whereas 64.7% involved non-clinical evaluations (k = 11). The results showed a significant moderating effect on the correlation between MIL and mental health issues (p = 0.049, SE = −0.16); the negative relationship between MIL and mental health issues was stronger when non-clinical evaluations (self-report only) were used. Specifically, the mean correlation coefficient for non-clinical evaluations was −0.42 and for clinical evaluations was −0.29.
The overall association of MIL with negative mental health outcomes
Previous studies have focused on the association of MIL with positive mental health outcomes, such as subjective well-being and life satisfaction [28,30,96–99]. The present study focused on the relationship between MIL and negative mental health outcomes and was the first meta-analysis to explore this relationship among older adults. There was a moderate negative correlation between MIL and mental health issues, indicating that the lack of a sense of MIL can be detrimental to the mental health of older adults. Successful aging is difficult for older adults who lack MIL. Thus, it would be an important area to address through psychological interventions.
The negative predictive effect of MIL on mental health problems in the elderly is consistent with expectations, and the test of moderating variables is crucial in explaining the mechanism of the relationship between the two. Specifically, it includes the conceptualization of MIL (value/purpose), the region in which the study was conducted (Asian/Western), participants’ residence status (community/nursing home/hospital), the evaluation method of mental health issues (clinical/non-clinical), and type of mental health issue.
Moderating effects of the concept of MIL and types of mental health issues
The moderating effect of the conceptualization of MIL (value/purpose) was not significant. This is consistent with the original assumptions proposed by Park et al. [100] that different aspects of MIL do not have different effects on outcome variables. Furthermore, in a meta-analysis of the relationship between MIL and physical health, it was noted that different aspects of MIL were not significantly different in their correlation with physical health [19]. Thus, they had the same association with the negative mental health outcomes of older adults. In future studies, the mechanism of the value and purpose dimensions of MIL on mental health issues of older adults can be further explored.
This study did not find any differences in the effects of MIL on different mental health issues. The reason could be related to the fact that the literature selected for this research was mostly depression-related studies, lacking other mental health issues (such as substance abuse, self-harm, and posttraumatic stress disorder). However, there were consistent correlations between MIL and different types of mental health issues. Older adults who lack MIL tend to suffer from depression, anxiety, and other negative psychological outcomes. These findings deepen our understanding of the mechanisms affecting the mental health of older adults. It is suggested that practitioners pay attention to and promote MIL for older adults to prevent the occurrence of mental health issues.
The moderating effect of culture
There was no moderating effect of culture (Asian countries vs. Western countries) on the relationship between MIL and mental health issues in older adults. It can be inferred that the correlation represents a pan-cultural phenomenon. This differs from a previous study that found differences in the relationship between MIL and psychological well-being in Eastern vs. Western countries, with young adults as participants [46].
Terror management theory holds that meaning and significance are components of self-esteem, which is essential for buffering the profound sources of anxiety. It works for people at all levels of development and across all cultures [101]. Some theories about universal psychological needs suggest that levels of meaning may be consistent across cultures [102]. MIL was significantly associated with mental health issues; therefore, this correlation in the two types of cultures, as represented in the studies’ geographic regions, had equal significance. Effects of “presence of meaning” and “searching for meaning” on the mental health issues of older adults in different cultures is an area for future research investigation.
The moderating effect of residence status
The moderating effect of residence status on MIL and mental health issues in older adults was not significant. However, in the studies included in this analysis, residential information about the participants was limited. Most articles described only whether the study was conducted in the community or a nursing home, and some articles did not mention where the participants were recruited from. Therefore, this study could only encode the residential situation as “community,” “nursing home,” “hospital,” “mixed,” or “unknown.” According to a study that examined the association of area-level demographic factors and mood disorder prevalence in a large sample of UK residents, no significant association between resident status and functional mental health [103] was seen. However, older adults living alone were found to be at risk of poor mental health [104], reporting higher depressive symptoms than those living with their spouse [105]. Thus, in terms of the mental health of older adults, living alone as opposed to living with others, especially a spouse, may be more important than where they live. In future research, mental health issues related to older adults living alone, with their spouse, children, or other older adults should be considered. The relationship between MIL and mental health issues of older adults in urban and rural area also needs to be further explored [106].
The moderating effect of the evaluation method
The method of evaluation or assessment used to examine the relationship between MIL and mental health issues showed a significant difference between studies that used self-report assessments compared to those that included a clinical diagnosis. Specifically, the negative correlation was significantly higher in studies that only used self-report instruments. One possible reason for the stronger non-clinical estimation effect is common method variance. Self-rated measurements depend on individual subjectivity, such as personal goals, self-evaluation, interpersonal relationships, coping styles, and people’s search for beliefs and action results [54,107]. Although we summarized the measurements for MIL and mental health issues separately, some items in the scales may contain both meaning and conceptual structures of mental health issues (e.g., the item, “My personal existence is very purposeful and meaningful” may access both meaning and depression).
An alternative explanation for this significant moderator is the reliability and validity of self-report assessment tools, which tend to be more standardized than an unstructured clinical interview [19,36]. Clinical diagnosis based on an unstructured interview depends on the experience and competence of the practitioner. As such, “diagnostic overshadowing” and misdiagnosis sometimes affect the accuracy of the diagnosis [108,109], which could potentially impact the correlation between MIL and mental health issues. The results have important implications for the diagnosis of older adults’ mental health issues for practitioners; both in-person diagnostic interviews and subjective self-report assessments are indispensable.
The mental health of older adults is a globally concerning issue; mental health issues such as depression and anxiety are prevalent [8]. It is critical to identify the preventative factors for mental health issues among older adults, take preventive measures, and develop appropriate interventions. This meta-analysis has the following theoretical and practical implications.
With regard to theoretical significance, this study used meta-analysis to identify a moderate negative association between MIL and mental health issues in older adults. The association did not differ significantly across mental health issues. At the same time, this correlation is pan-cultural and is not affected by residential conditions. This result is a comprehensive summary of the existing relevant studies, we confirm that enhancing MIL plays important role in promoting older adults’ mental health.
These results have important practical significance. Older adults should take an active approach to increasing their MIL, setting goals for the future, and identifying what they value in life. Family members and communities can encourage older adults to engage in activities that enhance their MIL. This will reduce the likelihood of them suffering from depression, anxiety and other psychological issues, which consequently reduce the burden on families and society. In addition, the correlation was stronger for non-clinical evaluation than for clinical diagnosis. This reminds practitioners realize that the older adults have a relatively strong assessment of the severity of their mental health issues. Then should pay attention to the comprehensive use of assessment methods, and guide the older adults to have a more objective cognition of their own mental health situation.
Our study has a few limitations: First, as most of the studies reviewed in this meta-analysis used a correlational research design, causality in the relationships found cannot be inferred. Additional variables could jointly affect MIL and mental health, such as the evaluation of stressful life events and whether they are threatening or uncontrollable [38], thereby affecting the correlation between MIL and mental health issues. Second, the types of mental health issues were not balanced. Most studies selected depression as a mental health variable, and only a few studies were concerned about anxiety and loneliness in older adults. Similarly, the conceptualization of MIL (value vs. purpose) was not balanced, either. Most studies included in this review focused on purpose in life; therefore, the moderation analysis may also have had relatively low power, affected the accuracy of estimates and limited the likelihood of detecting significant differences. Thus, the related conclusions are preliminary, and further exploration is needed.
This study found a moderate negative correlation between MIL and mental health issues among older adults. The evaluation method used to assess mental health issues played a significant role in moderating this negative relationship. The negative correlation between MIL and mental health issues was significantly higher in non-clinical assessment than in clinical assessment. The correlation between MIL and mental health issues did not differ significantly in terms of the conceptualization of MIL, region of participants, type of mental health issues, or residence status.
Funding Statement: This research was funded by a research Grant 32171076 from National Social Sciences Foundation of China and 20BSH139 from National Social Sciences Foundation of China.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Wang S. Spatial patterns and social-economic influential factors of population aging: a global assessment from 1990 to 2010. Soc Sci Med [Internet]. 2020;253:112963. doi:https://doi.org/10.1016/j.socscimed.2020.112963. [Google Scholar] [PubMed] [CrossRef]
2. WHO. Ageing and health. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. [Accessed 2018]. [Google Scholar]
3. Pluddemann A, Flisher AJ, McKetin R, Parry C, Lombard C. Methamphetamine use, aggressive behavior and other mental health issues among high-school students in Cape Town, South Africa. Drug Alcohol Depen [Internet]. 2010;109(1–3):14–9. doi:https://doi.org/10.1016/j.drugalcdep.2009.11.021. [Google Scholar] [PubMed] [CrossRef]
4. Bernstein CM, Stockwell MS, Gallagher MP, Rosenthal SL, Soren K. Mental health issues in adolescents and young adults with type 1 diabetes: prevalence and impact on glycemic control. Clin Pediatr [Internet]. 2013;52(1):10–5. doi:https://doi.org/10.1177/0009922812459950. [Google Scholar] [PubMed] [CrossRef]
5. Eleftheriades R, Fiala C, Pasic MD. The challenges and mental health issues of academic trainees. F1000Research [Internet]. 2020;9:104. doi:https://doi.org/10.12688/f1000research.21066.1. [Google Scholar] [PubMed] [CrossRef]
6. Cauli O, Navarro-Martínez R, Fernández-Garrido J. Special issue “Mental health issues and quality of life in older individuals”. Life [Internet]. 2021;11(3):221. doi:https://doi.org/10.3390/life11030221. [Google Scholar] [PubMed] [CrossRef]
7. Stanley SH, Ferguson L, Velayudhan A. The physical health wellness clinic model of care for patients with mental health issues who are ‘hard to engage’. Australasian Psychiatry Bulletin of the Royal Australian and New Zealand College of Psychiatrist [Internet]. 2020;28(3):303–6. doi:https://doi.org/10.1177/1039856219891596. [Google Scholar] [PubMed] [CrossRef]
8. WHO. Mental health of older adults. https://www.who.int/en/news-room/fact-sheets/detail/mental-health-of-older-adults. [Accessed 2017]. [Google Scholar]
9. Volkert J, Schulz H, Harter M, Wlodarczyk O, Andreas S. The prevalence of mental disorders in older people in Western countries—A meta-analysis. Ageing Res Rev [Internet]. 2013;12(1):339–53. doi:https://doi.org/10.1016/j.arr.2012.09.004. [Google Scholar] [PubMed] [CrossRef]
10. Estebsari F, Dastoorpoor M, Khalifehkandi ZR, Nouri A, Mostafaei D, Hosseini M, et al. The concept of successful aging: a review article. Current Aging Sci [Internet]. 2020;13(1):4–10. doi:https://doi.org/10.2174/1874609812666191023130117. [Google Scholar] [PubMed] [CrossRef]
11. Molavi R, Alavi M, Keshvari M. Relationship between general health of older health service users and their self-esteem in Isfahan in 2014. Iran J Nurs Res [Internet]. 2015;20(6):717–22. doi:https://doi.org/10.4103/1735-9066.170009. [Google Scholar] [PubMed] [CrossRef]
12. Sousa CM, Goncalves M, Machado J, Efferth T, Greten HJ. Effects of qigong on performance-related anxiety and physiological stress functions in transverse flute music schoolchildren: a feasibility study. J Chin Integr Med [Internet]. 2012;10(8):858–65. doi:https://doi.org/10.3736/jcim20120805. [Google Scholar] [PubMed] [CrossRef]
13. Wolitzky-Taylor KB, Castriotta N, Lenze EJ, Stanley MA, Craske MG. Anxiety disorders in older adults: a comprehensive review. Depress Anxiety [Internet]. 2010;27(2):190–211. doi:https://doi.org/10.1002/da.20653. [Google Scholar] [PubMed] [CrossRef]
14. Dykstra PA. Older adult loneliness: myths and realities. Eur J Ageing [Internet]. 2009;6(2):91–100. doi:https://doi.org/10.1007/s10433-009-0110-3. [Google Scholar] [PubMed] [CrossRef]
15. Ferreira-Alves J, Magalhães P, Viola L, Simoes R. Loneliness in middle and old age: demographics, perceived health, and social satisfaction as predictors. Arch Gerontol Geriat [Internet]. 2014;59(3):613–23. doi:https://doi.org/10.1016/j.archger.2014.06.010. [Google Scholar] [PubMed] [CrossRef]
16. Windsor TD. Persistence in goal striving and positive reappraisal as psychosocial resources for ageing well: a dyadic analysis. Aging Ment Health [Internet]. 2009;13(6):874–84. doi:https://doi.org/10.1080/13607860902918199. [Google Scholar] [PubMed] [CrossRef]
17. Steger MF, Frazier P, Oishi S, Kaler M. The meaning in life questionnaire: assessing the presence of and search for meaning in life. J Couns Psychol [Internet]. 2006;53(1):80–93. doi:https://doi.org/10.1037/0022-0167.53.1.80. [Google Scholar] [CrossRef]
18. Heintzelman SJ, King LA. Life is pretty meaningful. Am Psychol [Internet]. 2014;69(6):561–74. doi:https://doi.org/10.1037/a0035049. [Google Scholar] [PubMed] [CrossRef]
19. Czekierda K, Banik A, Park CL, Luszczynska A. Meaning in life and physical health: systematic review and meta-analysis. Health Psychol Rev [Internet]. 2017;11(4):387–418. doi:https://doi.org/10.1080/17437199.2017.1327325. [Google Scholar] [PubMed] [CrossRef]
20. Halama P, Bakosová K. Meaning in life as a moderator of the relationship between perceived stress and coping. Stud Psychol [Internet]. 2009;51(2/3):143. [Google Scholar]
21. Heisel MJ, Flett GL. The development and initial validation of the geriatric suicide ideation scale. Am J Geriatr Psychiatry [Internet]. 2006;14(9):742–51. doi:https://doi.org/10.1097/01.JGP.0000218699.27899.f9. [Google Scholar] [PubMed] [CrossRef]
22. Stawski RS, Sliwinski MJ, Smyth JM. Stress-related cognitive interference predicts cognitive function in old age. Psychol Aging [Internet]. 2006;21(3):535–44. doi:https://doi.org/10.1037/0882-7974.21.3.535. [Google Scholar] [PubMed] [CrossRef]
23. Steinert A, Steinert A, Haesner M, Haesner M. Stress in retired adults–stressors, symptoms and coping strategies. Ageing Int [Internet]. 2019;44(2):129–40. doi:https://doi.org/10.1007/s12126-018-9327-9. [Google Scholar] [CrossRef]
24. Hahn EA, Cichy KE, Small BJ, Almeida DM. Daily emotional and physical reactivity to stressors among widowed and married older adults. J Gerontol B Psychol Sci Soc Sci [Internet]. 2013;69B(1):19–28. doi:https://doi.org/10.1093/geronb/gbt035. [Google Scholar] [PubMed] [CrossRef]
25. Corbett T, Cummings A, Calman L, Farrington N, Fenerty V, Foster C, et al. Self-management in older people living with cancer and multi-morbidity: a systematic review and synthesis of qualitative studies. Psycho-Oncol [Internet]. 2020;29(10):1452–63. doi:https://doi.org/10.1002/pon.5453. [Google Scholar] [PubMed] [CrossRef]
26. Reker GT. Personal meaning, optimism, and choice: existential predictors of depression in community and institutional elderly. The Gerontologist [Internet]. 1997;37(6):709–16. doi:https://doi.org/10.1093/geront/37.6.709. [Google Scholar] [PubMed] [CrossRef]
27. Trivedi SC, Subramanyam AA, Kamath RM, Pinto C. Study of spirituality in elderly with subjective memory complaints. J Geriatr Psych Neur [Internet]. 2016;29(1):38–46. doi:https://doi.org/10.1177/0891988715598235. [Google Scholar] [PubMed] [CrossRef]
28. Haugan G. Meaning-in-life in nursing-home patients: a correlate with physical and emotional symptoms. J Clin Nurs [Internet]. 2014;23(7–8):1030–43. doi:https://doi.org/10.1111/jocn.12282. [Google Scholar] [PubMed] [CrossRef]
29. Hedberg P, Gustafson Y, Alex L, Brulin C. Depression in relation to purpose in life among a very old population: a five-year follow-up study. Aging Ment Health [Internet]. 2010;14(6):757–63. doi:https://doi.org/10.1080/13607861003713216. [Google Scholar] [PubMed] [CrossRef]
30. George LS, Park CL. The multidimensional existential meaning scale: a tripartite approach to measuring meaning in life. J Posit Psychol [Internet]. 2016;12(6):613–27. doi:https://doi.org/10.1080/17439760.2016.1209546. [Google Scholar] [CrossRef]
31. Steger MF, Oishi S, Kashdan TB. Meaning in life across the life span: levels and correlates of meaning in life from emerging adulthood to older adulthood. J Posit Psychol [Internet]. 2009;4(1):43–52. doi:https://doi.org/10.1080/17439760802303127. [Google Scholar] [CrossRef]
32. Krause N. Stressors arising in highly valued roles, meaning in life, and the physical health status of older adults. J Gerontol B [Internet]. 2004;59(5):S287–97. doi:https://doi.org/10.1093/geronb/59.5.S287. [Google Scholar] [PubMed] [CrossRef]
33. Boyle PA, Buchman AS, Barnes LL, Bennett DA. Effect of a purpose in life on risk of incident alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiat [Internet]. 2010;67(3):304–10. [Google Scholar] [PubMed]
34. Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosom Med [Internet]. 2009;71(5):574–9. doi:https://doi.org/10.1097/PSY.0b013e3181a5a7c0. [Google Scholar] [PubMed] [CrossRef]
35. Krause N, Rainville G. Age differences in meaning in life: exploring the mediating role of social support. Arch Gerontol Geriatr [Internet]. 2020;88(6):104008. doi:https://doi.org/10.1016/j.archger.2020.104008. [Google Scholar] [PubMed] [CrossRef]
36. Solares C, Dobrosavljevic M, Larsson H, Cortese S, Andershed H.The mental and physical health of older offenders: A systematic review and meta-analysis. Neurosci Biobehav Rev [Internet]. 2020;(118):440–50. [Google Scholar]
37. Li JB, Dou K, Liang Y. The relationship between presence of meaning, search for meaning, and subjective well-being: a three-level meta-analysis based on the meaning in life questionnaire. J Happiness Stud [Internet]. 2021;22(1):467–89. doi:https://doi.org/10.1007/s10902-020-00230-y. [Google Scholar] [CrossRef]
38. Park CL. Making sense of the meaning literature: an integrative review of meaning making and its effects on adjustment to stressful life events. Psychol Bulletin [Internet]. 2010;136(2):257–301. doi:https://doi.org/10.1037/a0018301. [Google Scholar] [PubMed] [CrossRef]
39. Frankl VE. Man’s search for meaning [Internet]. New York: Washington Square Press/Pocket Books; 1985. [Google Scholar]
40. Hill PL, Burrow AL, Sumner R, Young RK. Life Is pretty meaningful and/or purposeful? On conflations, contexts, and consequences. Am Psychol [Internet]. 2015;70(6):574–5. [Google Scholar] [PubMed]
41. Musich S, Wang SS, Kraemer S, Hawkins K, Wicker E. Purpose in life and positive health outcomes among older adults. Popul Health Manag [Internet]. 2018;21(2):139–47. doi:https://doi.org/10.1089/pop.2017.0063. [Google Scholar] [PubMed] [CrossRef]
42. Homan KJ, Boyatzis CJ. Religiosity, sense of meaning, and health behavior in older adults. Int J Psychol Relig [Internet]. 2010;20(3):173–86. doi:https://doi.org/10.1080/10508619.2010.481225. [Google Scholar] [CrossRef]
43. Markus HR, Kitayama S. Culture and the self: implications for cognition, emotion, and motivation. Psychol Rev [Internet]. 1991;98(2):224–53. doi:https://doi.org/10.1037/0033-295X.98.2.224. [Google Scholar] [CrossRef]
44. Reker GT. Theoretical perspective, dimensions, and measurement of existential meaning. In: Reker GT, Chamberlain K, editors. Exploring existential meaning: Optimizing human development across the life span [Internet]. Thousand Oaks, CA: Sage Publications; 2000. p. 39–58. [Google Scholar]
45. Kitayama S, Markus HR. The pursuit of happiness and the realization of sympathy: cultural patterns of self, social relations, and well-being. In: Diener E, Suh EM, editors. Culture and subjective well-being [Internet]. Cambridge, MA: The MIT Press; 2000. p. 113–61. [Google Scholar]
46. Steger MF, Kawabata Y, Shimai S, Otake K. The meaningful life in Japan and the United States: levels and correlates of meaning in life. J Res Pers [Internet]. 2008;42(3):660–78. doi:https://doi.org/10.1016/j.jrp.2007.09.003. [Google Scholar] [CrossRef]
47. de Cristofaro V, Pellegrini V, van Zomeren M. The relation between syetem justification and collective action in individualistic versus collectivistic European countries. TPM-Test Psychom Methodol Appl Psychol [Internet]. 2022;29(1):55–70. [Google Scholar]
48. Heine SJ, Kitayama S, Lehman DR. Cultural differences in self-evaluation: Japanese readily accept negative self-relevant information. J Cross Cult Psychol [Internet]. 2001;32(4):434–43. doi:https://doi.org/10.1177/0022022101032004004. [Google Scholar] [CrossRef]
49. Heine SJ, Lehman DR, Markus HR, Kitayama S. Is there a universal need for positive self-regard? Psychol Rev [Internet]. 1999;106(4):766–94. doi:https://doi.org/10.1037/0033-295X.106.4.766. [Google Scholar] [PubMed] [CrossRef]
50. Aydın A, Işık A, Kahraman N. Mental health symptoms, spiritual well-being and meaning in life among older adults living in nursing homes and community dwellings. Psychogeriatr [Internet]. 2020;20(6):833–43. doi:https://doi.org/10.1111/psyg.12613. [Google Scholar] [PubMed] [CrossRef]
51. Demir G, Nsal A, Gürol A, Oban A. Study of prevalence of depression among elders living at nursing home and house. University Journal of Health Sciences [Internet]. 2013;2(1):1–12. [Google Scholar]
52. Tiwari S, Singh R, Chand H. Spirituality and psychological wellbeing of elderly of Uttarakhand: a comparative study across residential status. J Psychol [Internet]. 2016;7(2):112–8. doi:https://doi.org/10.1080/09764224.2016.11907851. [Google Scholar] [CrossRef]
53. Muckler FA, Seven SA. Selecting performance measures: “objective” versus “subjective” measurement. Hum Factors [Internet]. 2016;34(4):441–55. doi:https://doi.org/10.1177/001872089203400406. [Google Scholar] [CrossRef]
54. Schlenker BR, Leary MR. Social anxiety and self-presentation: a conceptualization model. Psychol Bull [Internet]. 1982;92(3):641–69. doi:https://doi.org/10.1037/0033-2909.92.3.641. [Google Scholar] [PubMed] [CrossRef]
55. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med [Internet]. 2009;6(7):e1000097. doi:https://doi.org/10.1371/journal.pmed.1000097. [Google Scholar] [PubMed] [CrossRef]
56. Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers. Canada: Alberta Heritage Foundation for Medical Research Edmonton; 2004. [Google Scholar]
57. Feng D, Ji L, Xu L. Mediating effect of social support on the association between functional disability and psychological distress in older adults in rural China: does age make a difference? PLoS One [Internet]. 2014;9(6):e100945. doi:https://doi.org/10.1371/journal.pone.0100945. [Google Scholar] [PubMed] [CrossRef]
58. Chow EOW, Ho HCY. The relationship between psychological resources, social resources, and depression: results from older spousal caregivers in Hong Kong. Aging Ment Health [Internet]. 2012;16(8):1016–27. doi:https://doi.org/10.1080/13607863.2012.692769. [Google Scholar] [PubMed] [CrossRef]
59. Volkert J, Harter M, Dehoust MC, Ausin B, Canuto A, Da Ronch C, et al. The role of meaning in life in community-dwelling older adults with depression and relationship to other risk factors. Aging Ment Health [Internet]. 2019;23(1):100–6. doi:https://doi.org/10.1080/13607863.2017.1396576. [Google Scholar] [PubMed] [CrossRef]
60. Reker GT, Wong PTP. Aging as an individual process: toward a theory of personal meaning. In: Birren JE, Bengston VL, editors. Emergent theories of aging. New York, NY: Springer; 1988. p. 214–46. [Google Scholar]
61. Warner SC, Williams JI. The meaning in life scale: determining the reliability and validity of a measure. J Chron Dis [Internet]. 1987;40(6):503–12. doi:https://doi.org/10.1016/0021-9681(87)90007-5. [Google Scholar] [PubMed] [CrossRef]
62. Fegg MJ, Kramer M, L’Hoste S, Borasio GD. The schedule for meaning in life evaluation (SMiLEvalidation of a new instrument for meaning-in-life research. J Pain Symptom Manag [Internet]. 2008;35(4):356–64. doi:https://doi.org/10.1016/j.jpainsymman.2007.05.007. [Google Scholar] [PubMed] [CrossRef]
63. Heisel MJ. Assessing experienced meaning in life among older adults: the development and initial validation of the EMIL. Int Psychogeriatr [Internet]. 2009;21:S172–3. [Google Scholar]
64. Reker GT, Peacock EJ. The Life Attitude Profile (LAPa multidimensional instrument for assessing attitudes toward life. Can J Beh Sci [Internet]. 1981;13(3):264–73. doi:https://doi.org/10.1037/h0081178. [Google Scholar] [CrossRef]
65. Takkinen S, Ruoppila I. Meaning in life as an important component of functioning in old age. Int J Aging Hum Dev [Internet]. 2001;53(3):211–31. doi:https://doi.org/10.2190/H6H6-YAT0-181Y-5BR3. [Google Scholar] [PubMed] [CrossRef]
66. Ferrand C, Martinent G, Durmaz N. Psychological need satisfaction and well-being in adults aged 80 years and older living in residential homes: using a self-determination theory perspective. J Aging Stud [Internet]. 2014;30(3):104–11. doi:https://doi.org/10.1016/j.jaging.2014.04.004. [Google Scholar] [PubMed] [CrossRef]
67. Shek DTL. Reliability and factorial structure of the Chinese version of the purpose in life questionnaire. J Clin Psychol [Internet]. 1988;44(3):384–92. doi:https://doi.org/10.1002/(ISSN)1097-4679. [Google Scholar] [CrossRef]
68. Crumbaugh JC. Cross-validation of purpose-in-life test based on Frankl’s concepts. J Indiv Psychol [Internet]. 1968;24(1):74–81. [Google Scholar]
69. Crumbaugh JC, Henrion R. The PIL test: administration, interpretation, uses theory and critique. The International Forum of Logotherapy [Internet]. 1988;11(2):76–88. [Google Scholar]
70. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiat [Internet]. 1961;4(6):561–71. doi:https://doi.org/10.1001/archpsyc.1961.01710120031004. [Google Scholar] [PubMed] [CrossRef]
71. Chen R, Copeland J. Epidemiology of depression: prevalence and incidence. In: Abou-Saleh MT, Katona C, Kumar A, Chichester [Internet]. UK: John Wiley & Sons, Ltd.; 2010. p. 479–88. [Google Scholar]
72. Sheikh JI, Yesavage JA. 9/Geriatric depression scale (Gds) recent evidence and development of a shorter version. Clin Gerontologist [Internet]. 1986;5(1–2):165–73. doi:https://doi.org/10.1300/J018v05n01_09. [Google Scholar] [CrossRef]
73. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiat Res [Internet]. 1983;17(1):37–49. doi:https://doi.org/10.1016/0022-3956(82)90033-4. [Google Scholar] [PubMed] [CrossRef]
74. Lee H-CB, Chiu HFK, Kwok WY, Leung CM, Kwong PK, Chung DWS, et al. Chinese elderly and the GDS short form: a preliminary study. Clin Gerontologist [Internet]. 1993;14(2):27–62. [Google Scholar]
75. Zung WWK, Zung WW. A self-rating depression scale. Arch Gen Psychiat [Internet]. 1965;12(1):63–70. doi:https://doi.org/10.1001/archpsyc.1965.01720310065008. [Google Scholar] [PubMed] [CrossRef]
76. Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J (Clinical Research ed.) [Internet]. 1986;292(6516):344. doi:https://doi.org/10.1136/bmj.292.6516.344. [Google Scholar] [PubMed] [CrossRef]
77. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psych Meas [Internet]. 1977;1(3):385–401. doi:https://doi.org/10.1177/014662167700100306. [Google Scholar] [CrossRef]
78. Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. J Pers Assess [Internet]. 1978;42(3):290–4. doi:https://doi.org/10.1207/s15327752jpa4203_11. [Google Scholar] [PubMed] [CrossRef]
79. Williams N. PHQ-9. Occupational Medicine [Internet]. 2014;64(2):139–40. [Google Scholar]
80. American Psychiatric Association, A. Diagnostic and statistical manual of mental disorders. BMC Med [Internet]. 2013;17:133–7. [Google Scholar]
81. Wittchen HU, Strehle J, Gerschler A, Volkert J, Dehoust MC, Sehner S, et al. Measuring symptoms and diagnosing mental disorders in the elderly community: the test-retest reliability of the CIDI65. Int J Meth Psych Res [Internet]. 2015;24(2):116–29. doi:https://doi.org/10.1002/mpr.1455. [Google Scholar] [PubMed] [CrossRef]
82. Field AP, Gillett R. How to do a meta-analysis. Brit J Math Stat Psy [Internet]. 2010;63(3):665–94. doi:https://doi.org/10.1348/000711010X502733. [Google Scholar] [PubMed] [CrossRef]
83. Mike WL, Cheung. Applied meta-analysis for social science research. Structural Equation Modeling: A Multidisciplinary Journal [Internet]. 2013;20(4):704–7. [Google Scholar]
84. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. 1. Aufl. 1st ed. Somerset: Wiley; 2009. [Google Scholar]
85. Cochran WG. Some methods for strengthening the common χ2 Tests. Biometrics [Internet]. 1954;10(4):417–451. doi:https://doi.org/10.2307/3001616. [Google Scholar] [CrossRef]
86. Bamonti P, Lombardi S, Duberstein PR, King DA, van Orden KA. Spirituality attenuates the association between depression symptom severity and meaning in life. Aging Ment Health [Internet]. 2016;20(5):494–9. doi:https://doi.org/10.1080/13607863.2015.1021752. [Google Scholar] [PubMed] [CrossRef]
87. Chow EOW. The role of meaning in life: mediating the effects of perceived knowledge of stroke on depression and life satisfaction among stroke survivors. Clin Rehabil [Internet]. 2017;31(12):1664–73. doi:https://doi.org/10.1177/0269215517708604. [Google Scholar] [PubMed] [CrossRef]
88. Dixon AL. Mattering in the later years_older adults’ experiences of mattering to others, purpose in life, depression, and wellness. Adultspan J [Internet]. 2007;6(2):83–95. doi:https://doi.org/10.1002/(ISSN)2161-0029. [Google Scholar] [CrossRef]
89. Flood M. Exploring the relationships between creativity, depression, and successful aging. Act Adapt Aging [Internet]. 2006;31(1):55–71. [Google Scholar]
90. Hedberg P, Brulin C, Alex L, Gustafson Y. Purpose in life over a five-year period: a longitudinal study in a very old population. Int Psychogeriatr [Internet]. 2011;23(5):806–13. doi:https://doi.org/10.1017/S1041610210002279. [Google Scholar] [PubMed] [CrossRef]
91. Crumbaugh JC, Maholick LT. Manual of instructions for the purpose in life test [Internet]. Murfreesboro, TN: Psychometric Affiliates; 1981. [Google Scholar]
92. Heisel MJ, Neufeld E, Flett GL. Reasons for living, meaning in life, and suicide ideation: investigating the roles of key positive psychological factors in reducing suicide risk in community-residing older adults. Aging Ment Health [Internet]. 2016;20(2):195–207. doi:https://doi.org/10.1080/13607863.2015.1078279. [Google Scholar] [PubMed] [CrossRef]
93. Krause N. Evaluating the stress-buffering function of meaning in life among older people. J Aging Health [Internet]. 2007;19(5):792–812. doi:https://doi.org/10.1177/0898264307304390. [Google Scholar] [PubMed] [CrossRef]
94. Prager E, Bar-Tur L, Abramowici I. The Sources of Meaning Profile (SOMP) with aged subjects exhibiting depressive symptomatology. Clin Gerontologist [Internet]. 1997;17(3):25–39. doi:https://doi.org/10.1300/J018v17n03_04. [Google Scholar] [CrossRef]
95. Cohen J. Statistical power analysis for the behavioral sciences [Internet]. 2nd ed. Hillsdale, N.J: L. Erlbaum Associates; 1988. [Google Scholar]
96. Krause N. Meaning in life and mortality. J Gerontol B Psychol Sci Soc Sci [Internet]. 2009;64(4):517–27. doi:https://doi.org/10.1093/geronb/gbp047. [Google Scholar] [PubMed] [CrossRef]
97. Brassai L, Piko BF, Steger MF. Meaning in life: is it a protective factor for adolescents’ psychological health? Int J Behav Med [Internet]. 2011;18(1):44–51. doi:https://doi.org/10.1007/s12529-010-9089-6. [Google Scholar] [PubMed] [CrossRef]
98. Brandstätter M, Baumann U, Borasio GD, Fegg MJ. Systematic review of meaning in life assessment instruments. Psycho-Oncol [Internet]. 2012;21(10):1034–52. doi:https://doi.org/10.1002/pon.2113. [Google Scholar] [PubMed] [CrossRef]
99. Steger MF, Fitch-Martin AR, Donnelly J, Rickard KM. Meaning in life and health: proactive health orientation links meaning in life to health variables among american undergraduates. J Happiness Stud [Internet]. 2015;16(3):583–97. doi:https://doi.org/10.1007/s10902-014-9523-6. [Google Scholar] [CrossRef]
100. Park CL, Folkman S. Meaning in the context of stress and coping. Rev Gen Psychol [Internet]. 1997;1(2):115–44. doi:https://doi.org/10.1037/1089-2680.1.2.115. [Google Scholar] [CrossRef]
101. Ryan RM, Deci EL. Avoiding death or engaging life as accounts of meaning and culture: comment on Pyszczynski et al. (2004). Psychol Bull [Internet]. 2004;130(3):473–7. [Google Scholar] [PubMed]
102. Hofer J, Busch H, Au A, Poláčková Šolcová I, Tavel P, Wong TT. For the benefit of others: generativity and meaning in life in the elderly in four cultures. Psychol Aging [Internet]. 2014;29(4):764–75. doi:https://doi.org/10.1037/a0037762. [Google Scholar] [PubMed] [CrossRef]
103. Wainwright NWJ, Surtees PG. Places, people, and their physical and mental functional health. J Epidemiol Community Health (1979) [Internet]. 2004;58(4):333–9. doi:https://doi.org/10.1136/jech.2003.012518. [Google Scholar] [PubMed] [CrossRef]
104. Oh DH, Park JH, Lee HY, Kim SA, Choi BY, Nam JH. Association between living arrangements and depressive symptoms among older women and men in South Korea. Soc Psych Psych Epid [Internet]. 2015;50(1):133–41. doi:https://doi.org/10.1007/s00127-014-0904-2. [Google Scholar] [PubMed] [CrossRef]
105. Honjo K, Tani Y, Saito M, Sasaki Y, Kondo K, Kawachi I, et al. Living alone or with others and depressive symptoms, and effect modification by residential social cohesion among older adults in Japan: the JAGES longitudinal study. J Epidemiol [Internet]. 2018;28(7):315–22. doi:https://doi.org/10.2188/jea.JE20170065. [Google Scholar] [PubMed] [CrossRef]
106. Shou J, Du Z, Wang H, Ren L, Liu Y, Zhu S. Quality of life and its contributing factors in an elderly community-dwelling population in Shanghai, China. Psychogeriatr [Internet]. 2018;18(2):89–97. doi:https://doi.org/10.1111/psyg.12288. [Google Scholar] [PubMed] [CrossRef]
107. Czellar S. Self-presentational effects in the implicit association test. J Consum Psychol [Internet]. 2006;16(1):92–100. doi:https://doi.org/10.1207/s15327663jcp1601_11. [Google Scholar] [CrossRef]
108. Kostov CE, Rees CE, Gormley GJ, Monrouxe LV. I did try and point out about his dignity’: a qualitative narrative study of patients and carers’ experiences and expectations of junior doctors. BMJ Open [Internet]. 2018;8(1):e017738. doi:https://doi.org/10.1136/bmjopen-2017-017738. [Google Scholar] [PubMed] [CrossRef]
109. van der Heiden C, Muris PEHM, van der Molen HT, Methorst G. Generalized anxiety disorder: clinical presentation, diagnostic features, and guidelines for clinical practice. J Clin Psychol [Internet]. 2011;67(1):58–73. doi:https://doi.org/10.1002/jclp.20743. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF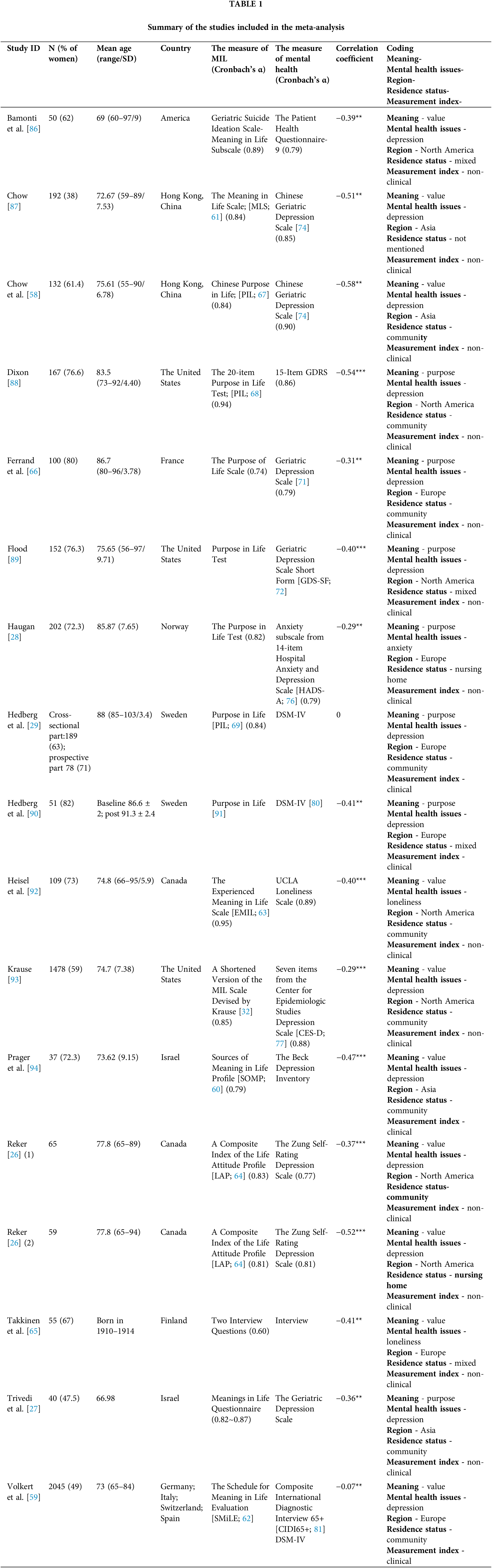
 Downloads
Downloads
 Citation Tools
Citation Tools