 Open Access
Open Access
ARTICLE
Prevalence of Anxiety and Associated Factors among University Students: A Cross-Sectional Study in Japan
1 Faculty of Rehabilitation, School of Health Sciences, Fujita Health University, Toyoake, 4701192, Japan
2 Department of Rehabilitation Medicine, National Center for Geriatrics and Gerontology, Obu, 4748511, Japan
* Corresponding Author: Hiroaki Sakurai. Email:
# These authors have contributed equally to this work and share first authorship
International Journal of Mental Health Promotion 2023, 25(7), 855-861. https://doi.org/10.32604/ijmhp.2023.028956
Received 19 January 2023; Accepted 03 April 2023; Issue published 01 June 2023
Abstract
Mental health difficulties can impact students’ motivation, focus, and ability to communicate with others. Students attending medical universities are more likely to experience anxiety, depression, and other mood changes for the first time. However, no study has examined their prevalence among Japanese rehabilitation students. This study investigated the prevalence of anxiety among Japanese rehabilitation students and aimed to identify its predictors. A cross-sectional study was conducted among 148 first-year physical and occupational therapy students at a private medical university in Japan in June 2022. Data on sociodemographic and personal characteristics, such as gender, age, subject major, regular exercise, place of residence, and sleeping hours, were recorded using an original questionnaire. Instruments included the State-Trait Anxiety Inventory, COVID-19 questionnaire, and Beck Depression Inventory–Second Edition (BDI-II). The results indicated that 83 (56%) and 77 (52%) students exhibited state anxiety and trait anxiety symptoms, respectively. Thirty-four (23%) students experienced mild depressive symptoms. Associations were further determined between gender, subject major, handling of stress, loneliness, satisfaction with life, satisfaction with social connections, anxiety about the future, satisfaction with school life, fulfillment of friendships, and depression. Several variables demonstrated a statistically significant association: handling stress (p < 0.05; 95% CI 0.409–2.472), satisfaction with life (p < 0.01; 95% CI 0.500–0.897), anxiety about the future (p < 0.01; 95% CI 1.397–4.087), and depression (total score of BDI-II, p < 0.01; 95% CI 1.555–100.742). Our results emphasize that universities must establish a system for early identification and support of anxiety and depression in students.Keywords
Mental health issues are a significant obstacle for students [1]. Mental health difficulties can impact students’ motivation, focus, and ability to communicate with others. Unlike students majoring in liberal arts, social sciences, and humanities, students pursuing medical professions, such as physical and occupational therapy, are subjected to many stressful events, including numerous classes, long-term clinical training, and national examinations [2]. Students attending medical universities are likely to experience greater changes in mood, including anxiety and depression. Previous studies have shown that undergraduate and graduate students have increased stress levels and signs of mental health problems [3,4]. More recently, the COVID-19 pandemic has significantly impacted students’ mental health [5,6]. In addition, the restrictions imposed on various aspects of university life, such as lectures, meals with friends, and club activities, have sparked concerns about the decline in mental health among students.
According to the 2019 Annual Report of the Center for Collegiate Mental Health, anxiety is the most prevalent mental health problem among university students [7]. Anxiety is a physical reaction to real or imaginary perceived danger caused by a person’s thoughts, beliefs, and emotions [8]. It may have significant consequences for college students, including poor academic performance, dropping out, and suicide [9–11]. However, anxiety has received little attention and is often undetected and undertreated in the general population [12].
Research on anxiety among university students has primarily been conducted among medical students. In a previous study, 33.8% of medical students experienced anxiety, which was significantly higher than its prevalence in the general population [13]. In addition, a systematic review of anxiety among medical students showed an extensive prevalence ranging from 7.7% to 65.5% [14]. Studies on rehabilitation students have also shown a high prevalence of anxiety (50.5% to 69%) [15,16]. However, to the best of our knowledge, there have been no studies regarding the prevalence of anxiety among Japanese rehabilitation students. Mental health effects can vary greatly depending on the country, culture, and environment in which one lives [17]. Previous studies have only considered limited explanatory variables associated with anxiety, such as demographic factors (gender and place of residence) [18]. We hypothesized that anxiety is associated with other factors, such as anxiety about the future, life satisfaction, and stress among rehabilitation students in Japan. The objectives of this study were thus (1) to investigate the prevalence of anxiety among Japanese rehabilitation students, and (2) to identify predictors of anxiety.
A cross-sectional study was conducted in June 2022 on a convenience sample of 148 first-year physical and occupational therapy students (61 men and 87 women) enrolled at Fujita Health University. The students were informed that participation in the study was voluntary, and they were invited to participate. In this study, we aimed to assess the risk of mental health issues among students at the time of university enrollment. Therefore, students in their second year or higher were excluded from the analysis. The inclusion criteria for this study involved individuals who were enrolled in the Department of Rehabilitation at Fujita Health University, were fluent in and able to read Japanese, and were over the age of 18 years. The exclusion criteria comprised individuals with severe mental disorders, such as bipolar disorder. The survey was conducted during a non-stressful study period (i.e., non-examination period) [19].
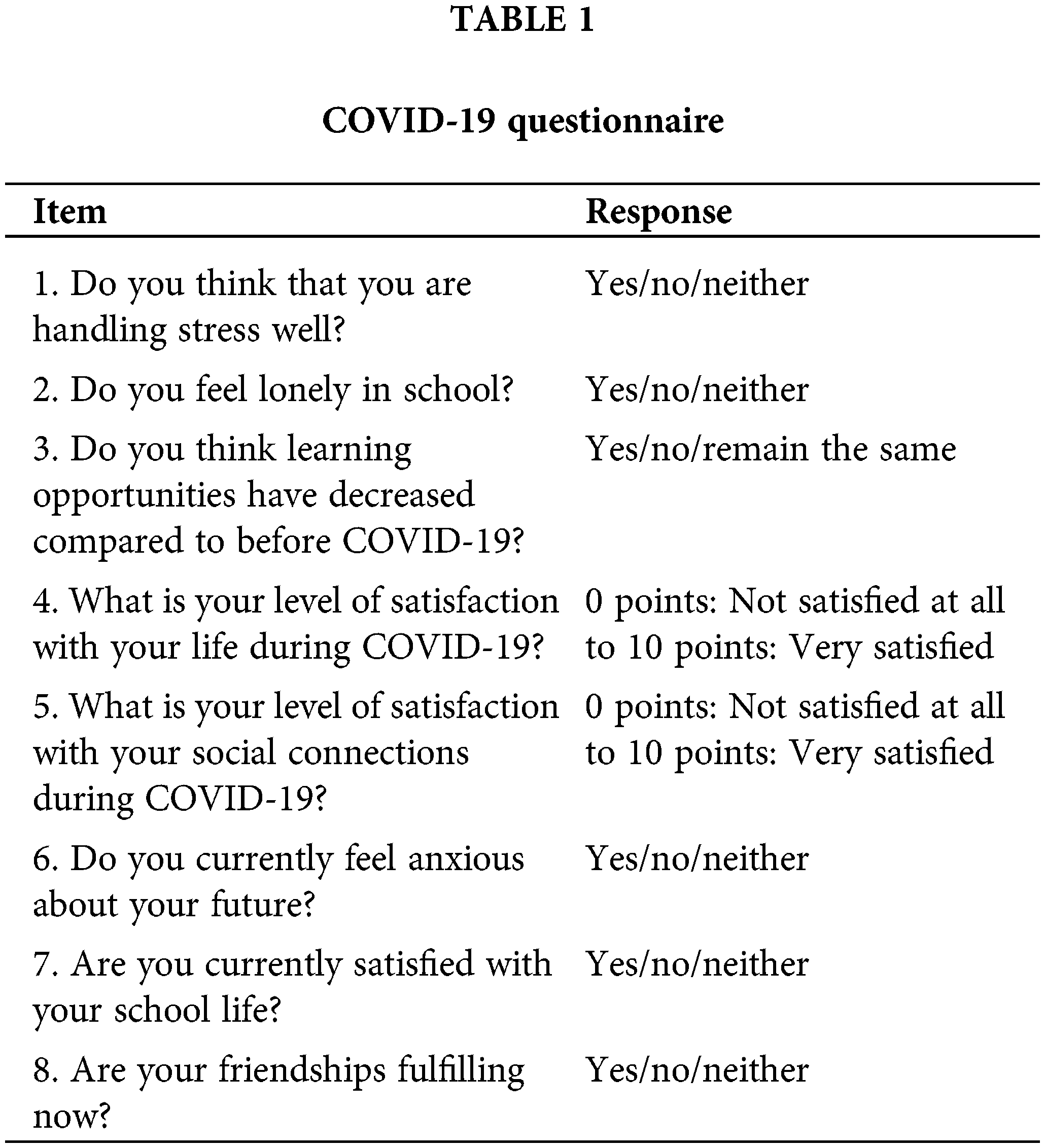
Data on sociodemographic and personal characteristics, such as gender, age, subject major, regular exercise, place of residence, and sleeping hours, were recorded. Anxiety symptoms were assessed using the State-Trait Anxiety Inventory (STAI) [20]. In addition, the COVID-19 questionnaire and Beck Depression Inventory–Second Edition (BDI-II) [21] were used to examine anxiety-related factors. The COVID-19 questionnaire was administered using Google Forms, with items developed following the example of previous studies [22,23]. The contents of the questionnaire are shown in Table 1. For the items in Table 1 that indicate the COVID-19 period (items 4 and 5), the respondents were encouraged to answer the questions according to an image of their post-entry status.
The State-Trait Anxiety Inventory (STAI) is a two-part scale, with 20 items assessing the intensity of state anxiety and trait anxiety frequency [20]. Conventional anxiety tests aim to measure only trait anxiety, but the STAI is a test that can discriminate between trait and state anxiety. This study used the State-Trait Anxiety Inventory-Form JYZ (STAI-JYZ), which is sensitive to cultural factors within Japan [24]. State anxiety reflects a transient response to the anxiety-evoking phenomenon and changes over time. Trait anxiety comprises anxiety that is relatively stable under various situations. Anxiety-presence is when anxiety is present (e.g., loss of confidence), and anxiety-absence is when anxiety is absent (e.g., feeling lucky and fortunate). The STAI-JYZ had a high internal consistency and the Cronbach’s alpha coefficient was in the range of 0.87 to 0.92 for the state anxiety scale, and 0.86 to 0.90 for the trait anxiety scale [24]. In addition, based on the report by Himeno et al., the participants’ anxiety levels were divided into two groups: not having anxiety (men, 20–40 points; women, 20–41 points) and anxiety (men, 41–80 points; women, 42–80 points) [25].
The BDI-II is a widely used 21-item self-report scale for evaluating depressive symptoms [21]. Each item is rated on a Likert scale ranging from 0 to 3, with total scores ranging from 0 to 63. Higher scores indicate a higher level of depressive symptoms. The score is interpreted as no/minimal (0–13), mild (14–19), moderate (20–28), or severe depression (29–63) [21]. This study used an approved Japanese version of the BDI-II, which has been validated and demonstrates reliability with a Cronbach’s alpha value of 0.87 [26]. The widely used Japanese versions of the BDI-II and STAI-JYZ have been standardized and published [27,28]. The participants rated items on a 4-point Likert-scale (1 = “not at all,” 4 = “very much”). The weight of each item was added to obtain the summary score.
Continuous variables were presented as mean ± standard deviation. The percentage of anxiety symptoms and depression was calculated. Logistic regression analysis using the likelihood ratio test was performed using the forwarding selection method to identify factors associated with anxiety symptoms. Logistic regression analysis was conducted to identify current anxiety factors, and state rather than trait anxiety was analyzed. Based on the report by Himeno et al., the objective variable was defined as “0” and “1” for the no anxiety group and anxiety group, respectively (see 2.3 Evaluation tool) [25]. The explanatory variables were gender, subject major, handling stress, loneliness, life satisfaction, satisfaction with social connections, anxiety about the future (including employment and future career paths), school life satisfaction, fulfillment of friendships, and depression. Depression was classified as no depressive symptoms (0–13 points) or depressive symptoms (≥14 points) based on BDI-II scores [21]. The statistical significance level was set at p < 0.05. SPSS Statistics ver. 26.0 (IBM Japan, Tokyo) was used for the analysis.
There were no missing data. No students met the exclusion criteria.
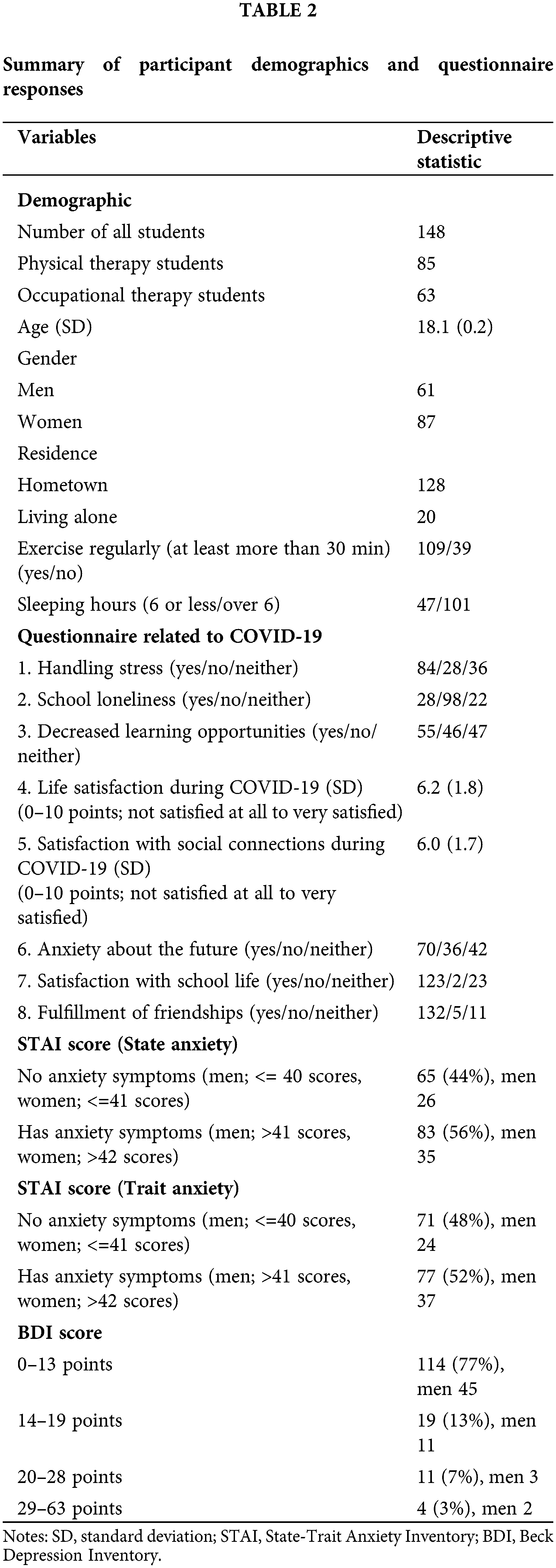
The participants’ sociodemographic and personal characteristics, STAI-JYZ and BDI-II results, and COVID-19 questionnaire results are summarized in Table 2. Based on the STAI-JYZ scores, 83 students (56%, 35 men and 48 women) were classified as having state anxiety symptoms, and 77 students (52%, 37 men and 40 women) demonstrated trait anxiety symptoms.
Logistic regression analysis with STAI-JYZ as the objective variable
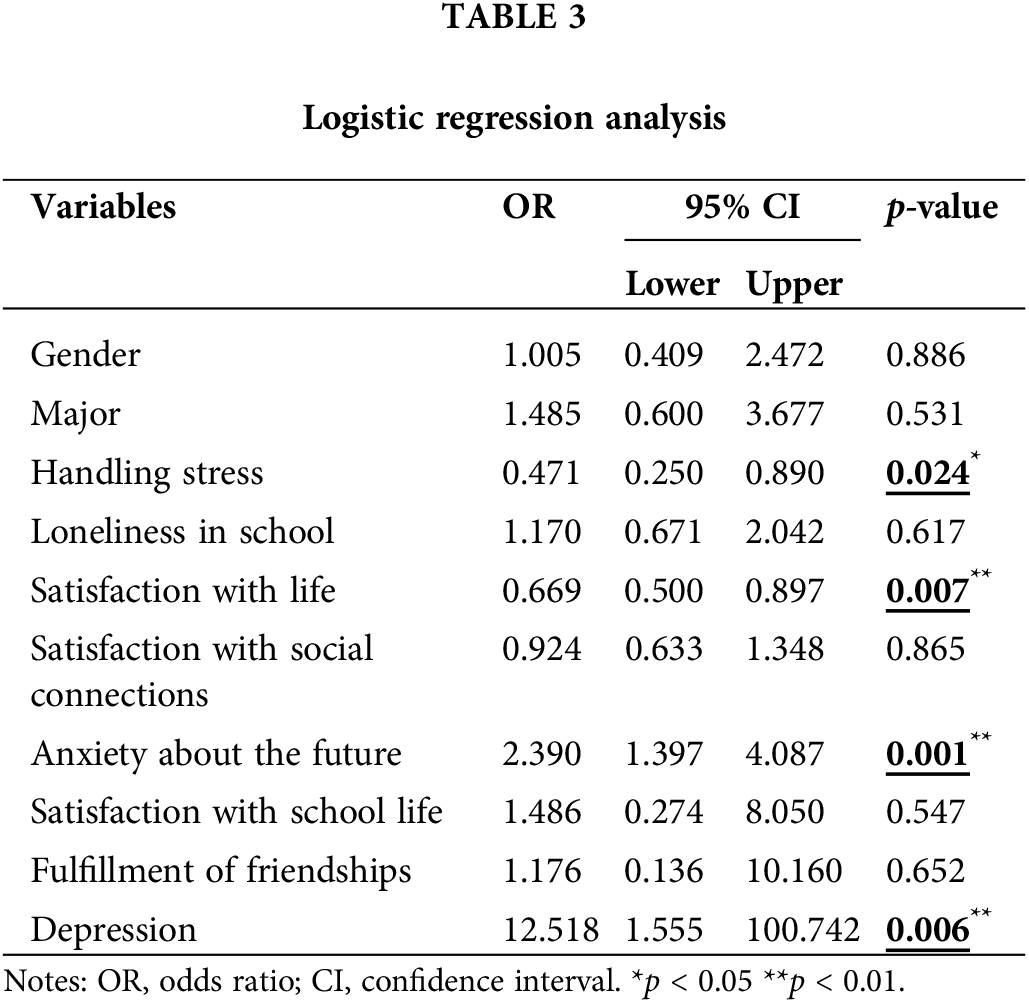
We determined associations between gender, subject major, handling stress, loneliness, satisfaction with life, satisfaction with social connections, anxiety about the future, satisfaction with school life, fulfillment of friendships, and depression (Table 3). Several variables demonstrated a statistically significant association: handling stress (p < 0.05; 95% CI 0.409–2.472), satisfaction with life (p < 0.01; 95% CI 0.500–0.897), anxiety about the future (p < 0.01; 95% CI 1.397–4.087), and depression (total score of BDI-II, p < 0.01; 95% CI 1.555–100.742). Odds ratios showed that students with anxiety were 0.471 times less able to handle stress and 0.669 times less satisfied with their lives than were those without anxiety. Students with anxiety were also 2.390 times more anxious about the future and 12.518 times more likely to report depression than were those without anxiety.
We investigated the rate of anxiety and factors related to anxiety among first-year university students studying rehabilitation. The results showed that approximately half of the sample presented anxiety symptoms. The ability to handle stress, life satisfaction, anxiety about the future, and depressive symptoms were associated with increased anxiety symptoms. To the best of our knowledge, this is the first survey report on anxiety among rehabilitation students in Japan.
The prevalence of anxiety varies by country of residence, ranging from 43% in Europe to 60.8% in Saudi Arabia and 69.3% in Pakistan [29–31]. Among nursing students in Hong Kong, the prevalence of anxiety was 39% [32]. Various other factors have been associated with anxiety, such as urbanicity [33], socioeconomic disadvantage [34], and relationship difficulties [35]. The rates of anxiety symptoms in our study (56% for state anxiety and 52% for trait anxiety) were consistent with those in previous studies [36,37] and higher than those of the general population [38–40]. Thus, understanding the mental health of undergraduate rehabilitation students in Japan is extremely important because the impact on mental health varies greatly depending on the country, culture, and environment in which they live [17]. We believe it is essential to address the mental health issues of Japanese rehabilitation students who aspire to become health professionals, developing effective strategies for managing anxiety symptoms.
Moreover, mental health deterioration is reported to increase as students progress in their academic careers [41,42]. Mental health problems among university students mainly develop before matriculation and are associated with failure to enter university and withdrawal from school [43]. Most students exhibited anxiety (state or trait), resulting in some students to drop out within a few days or months of enrollment, while others showed poor academic performance and high failure rates, leading to mood changes and an increased risk of depression [44–46]. A report on anxiety among first-year university students showed that 47.1% of students had anxiety symptoms, similar to the present study’s findings [47]. Therefore, screening students for mental health risks at the beginning of the university program is crucial, and long-term support may reduce withdrawal and improve their educational and psychosocial functioning.
Previous studies have investigated the factors influencing mental health, such as gender and place of residence; however, many studies have been limited to demographic factors [18]. In the present study, strong predictors of anxiety symptoms included anxiety about the future and depressive symptoms. Feeling anxious after entering university is a common experience for many students. Furthermore, medical universities for physical and occupational therapy expose students to many stressful events, such as numerous classes, long clinical training, and national examinations [2]. Therefore, strong anxiety about the future, alongside symptoms of depression and decreased life satisfaction, may have been identified as factors that predict anxiety. According to a survey assessing anxiety and worries about university life, the most prevalent factors were “finding employment and future career path,” followed by “academics.” Anxiety by the year of study demonstrated that 63.2% of third-year university students, who were closer to entering the job market, were concerned about “employment and future career paths.” Although this percentage was lower among first-year university students, it was still high (31.1%) [48]. These mental health problems are common among new university students and are associated with poor academic performance [1]. Therefore, it is vital to investigate mental health risks immediately after admission to detect and support the signs among new university students. For example, it may be necessary to introduce lectures and curricula to promote mental health from the first year of university, and for students to learn coping behaviors and stress management skills.
In addition, we believe that students with mental health problems require support from medical specialists. However, a previous study reported that approximately 1.5% of all students in Japan used counseling rooms for students [49], indicating that access to psychological support may be insufficient. Moreover, compared to their peers, students with high levels of depression and anxiety symptoms disagreed more with the statements, “I have adequate access to psychological support” and “There is a good program for stress management in my school” [50]. This finding suggests that students with mental health problems do not receive adequate psychological support. Thus, it is essential to monitor the mental health of rehabilitation students regularly and identify individuals who need assistance.
A significant strength of this study was that it was the first to investigate the rate of anxiety symptoms and factors contributing to anxiety among first-year university students in the Faculty of Rehabilitation in Japan. However, this study had several limitations. First, we collected data only from a single university in Japan. Future studies should examine differences among universities and regions to increase the generalizability of the present findings. Increasing the number of cases and collecting data from several universities would enable us to obtain more reliable findings. Second, because this was a cross-sectional study, subsequent progress was not followed. If students with anxiety symptoms can be identified early, then faculty members can provide long-term support to them. In such cases, it may be possible to monitor changes in mental health over a period. Third, since this study was conducted during a non-stressful period when there were few examinations and other events, it is expected that the percentage of anxiety symptoms would increase depending on the time of year in which they are measured. Fourth, we were not able to compare rehabilitation students with general college students. At this point, we cannot determine whether the predictors of anxiety (coping with stress, satisfaction with life, anxiety about the future, and depression) are only characteristic of rehabilitation students. Therefore, it is necessary to survey general college students and compare their results with those of rehabilitation students. Finally, the STAI-JYZ was selected because it was designed to screen for the risk of anxiety symptoms, was suitable for population studies, and is an internationally used assessment. However, other clinician-administered diagnostic procedures should be used to assess the intensity of anxiety symptoms. This study highlights the high prevalence of anxiety symptoms among first-year university students studying rehabilitation in Japan, alongside the need for early detection and support for mental health risks.
This study highlights the high prevalence of anxiety symptoms among first-year rehabilitation university students in Japan and the need for early detection and support regarding mental health risks. Approximately half of the sample presented anxiety symptoms, which were linked with the ability to handle stress, satisfaction with life, anxiety about the future, and depressive symptoms. The findings highlight the importance of addressing mental health issues among rehabilitation students and suggest introducing lectures and curricula to promote mental health from the first year of university. The study also underscores the need to regularly monitor students’ mental health such that they can receive timely support from medical specialists.
Acknowledgement: We would like to thank Fujita Health University for reviewing and approving the study and Editage (www.editage.com) for English language editing.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study design, Y.K., S.K., S.T. and H.S.; data collection, S.S., K.T., K.F. and T.I.; data analysis, Y.K., S.S., K.T. and H.S.; writing—original draft preparation, Y.K. and S.S. All authors have read and agreed to the published version of the manuscript.
Availability of Data and Materials: The datasets generated for this study are available on request from the corresponding author.
Ethics Approval: The study included human participants and was reviewed and approved by the institutional review board of Fujita Health University (approval number: HM21-377), and conducted according to the guidelines of the Declaration of Helsinki. The objectives and procedures of the study were explained to the participants, emphasizing their voluntary participation, anonymity, and confidentiality. In addition, the students were informed of the study’s purpose and the option to withdraw at any time. Written informed consent for participation was not required for this study, in accordance with national legislation and institutional requirements. All participants consented to participate in the study and completed the questionnaires.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Bruffaerts R, Mortier P, Kiekens G, Auerbach RP, Cuijpers P, Demyttenaere K, et al. Mental health problems in college freshmen: prevalence and academic functioning. J Affect Disord [Internet]. 2018;225:97–103. doi:https://doi.org/10.1016/j.jad.2017.07.044. [Google Scholar] [PubMed] [CrossRef]
2. Nishida S, Hashimoto S, Fukuhara K, Tamaru Y, Sugihara K. The state of depression of rehabilitation medical students—from the perspective of learned helplessness. Annual Reports of Faculty of Rehabilitation, Shijonawate Gakuen University [Internet]. 2013;9:27–34. [Google Scholar]
3. Pinder-Amaker S. Introduction innovative and collaborative approaches to college student mental health challenges. Harvard Review of Psychiatry [Internet]. 2012;20(4):171–3. doi:https://doi.org/10.3109/10673229.2012.712835. [Google Scholar] [PubMed] [CrossRef]
4. Stallman HM. Psychological distress in university students: a comparison with general population data. Aust Psychol [Internet]. 2010;45(4):249–57. doi:https://doi.org/10.1080/00050067.2010.482109. [Google Scholar] [CrossRef]
5. Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19impact on education and mental health of students and academic staff. Cureus [Internet]. 2020;12(4):e7541. doi:https://doi.org/10.7759/cureus.7541. [Google Scholar] [PubMed] [CrossRef]
6. Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res [Internet]. 2020;22(9):e21279. doi:https://doi.org/10.2196/21279. [Google Scholar] [PubMed] [CrossRef]
7. Park P. Center for collegiate mental health [Internet]. In: Saad PB, editor. USA: Penn State University; 2019. [Google Scholar]
8. Bassi R, Sharma S, Kaur M. A study of correlation of anxiety levels with body mass index in new MBBS students. Natl J Physiol Pharm Pharmacol [Internet]. 2014;4(3):208–12. doi:https://doi.org/10.5455/njppp.2014.4.080420142. [Google Scholar] [CrossRef]
9. Stewart SM, Lam TH, Betson CL, Wong CM, Wong AM. A prospective analysis of stress and academic performance in the first two years of medical school. Med Educ [Internet]. 1999;33(4):243–50. doi:https://doi.org/10.1046/j.1365-2923.1999.00294.x. [Google Scholar] [PubMed] [CrossRef]
10. Tyssen R, Vaglum P, Gronvold NT, Ekeberg O. Suicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictors. J Affect Disord [Internet]. 2001;64(1):69–79. doi:https://doi.org/10.1016/S0165-0327(00)00205-6. [Google Scholar] [PubMed] [CrossRef]
11. Walkiewicz M, Tartas M, Majkowicz M, Budzinski W. Academic achievement, depression and anxiety during medical education predict the styles of success in a medical career: a 10-year longitudinal study. Med Teach [Internet]. 2012;34(9):e611–9. doi:https://doi.org/10.3109/0142159X.2012.687478. [Google Scholar] [PubMed] [CrossRef]
12. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med [Internet]. 2007;146(5):317–25. doi:https://doi.org/10.7326/0003-4819-146-5-200703060-00004. [Google Scholar] [PubMed] [CrossRef]
13. Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CSH, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Health Res [Internet]. 2019;16(15):2735. doi:https://doi.org/10.3390/ijerph16152735. [Google Scholar] [PubMed] [CrossRef]
14. Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ [Internet]. 2014;48(10):963–79. doi:https://doi.org/10.1111/medu.12512. [Google Scholar] [PubMed] [CrossRef]
15. Ali M, Uddin Z, Amran Hossain KM, Uddin TR. Depression, anxiety, stress, and suicidal behavior among Bangladeshi undergraduate rehabilitation students: an observational study amidst the COVID-19 pandemic. Health Sci Rep [Internet]. 2022;5(2):e549. doi:https://doi.org/10.1002/hsr2.549. [Google Scholar] [PubMed] [CrossRef]
16. Syed A, Ali SS, Khan M. Frequency of depression, anxiety and stress among the undergraduate physiotherapy students. Pak J Med Sci [Internet]. 2018;34(2):468–71. doi:https://doi.org/10.12669/pjms.342.12298. [Google Scholar] [PubMed] [CrossRef]
17. Somers JM, Goldner EM, Waraich P, Hsu L. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry [Internet]. 2006;51(2):100–13. doi:https://doi.org/10.1177/070674370605100206. [Google Scholar] [PubMed] [CrossRef]
18. Chang J, Yuan Y, Wang D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao [Internet]. 2020;40(2):171–6. doi:https://doi.org/10.12122/j.issn.1673-4254.2020.02.06. [Google Scholar] [PubMed] [CrossRef]
19. Silva V, Costa P, Pereira I, Faria R, Salgueira AP, Osta MJ, et al. Depression in medical students: insights from a longitudinal study. BMC Med Educ [Internet]. 2017;17(1):184. doi:https://doi.org/10.1186/s12909-017-1006-0. [Google Scholar] [PubMed] [CrossRef]
20. Spielberger CGR, Lushene R. STAI manual for the State-trait anxiety inventory. In: Self-evaluation questionnaire [Internet]. Consulting Psychologists Press; 1970. [Google Scholar]
21. Beck ATSR, Brown GK. BDI-II, Beck depression inventory manual [Internet]. 2nd ed. San Antonio; 1996. [Google Scholar]
22. Wang X, Hegde S, Son C, Keller B, Smith A, Sasangohar F. Investigating mental health of US college students during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res [Internet]. 2020;22(9):e22817. doi:https://doi.org/10.2196/22817. [Google Scholar] [PubMed] [CrossRef]
23. Cabinet Office. Survey on changes in lifestyle consciousness and behavior under the influence of the COVID-19 pandemic [Internet]; 2020. https://www5.cao.go.jp/keizai2/wellbeing/covid/index.html [Accessed 2022 Oct 31]. [Google Scholar]
24. Hidano NFM, Iwasaki M, Soga S, Spielberger C. Manual for the state-trait anxiety inventory-form JYZ [Internet]. Tokyo: Jitsumu Kyoiku-Shuppan; 2000. [Google Scholar]
25. Himeno CNH, Hamada S, Ikeda H, Kitajiri M, Yamashita T. An investigation of state-trait anxiety inventory (STAI) in dizzy patients. Equilibrium Res [Internet]. 2005;64(4):225–32. doi:https://doi.org/10.3757/jser.64.225. [Google Scholar] [CrossRef]
26. Kojima M, Furukawa TA, Takahashi H, Kawai M, Nagaya T, Tokudome S. Cross-cultural validation of the Beck Depression Inventory-II in Japan. Psychiatry Res [Internet]. 2002;110(3):291–9. doi:https://doi.org/10.1016/S0165-1781(02)00106-3. [Google Scholar] [PubMed] [CrossRef]
27. CHIBA TEST CENTER. 2022. https://www.chibatc.co.jp/cgi/web/index.cgi?c=catalogue-zoom&pk=144 [Accessed 2022 Oct 3]. [Google Scholar]
28. CHIBA TEST CENTER. 2022. https://www.chibatc.co.jp/cgi/web/index.cgi?c=catalogue-zoom&pk=139 [Accessed 2022 Oct 3]. [Google Scholar]
29. Alaqeel MK, Alowaimer NA, Alonezan AF, Almegbel NY, Alaujan FY. Prevalence of irritable bowel syndrome and its association with anxiety among medical students at King Saud bin Abdulaziz University for Health Sciences in Riyadh. Pak J Med Sci [Internet]. 2017;33(1):33–6. doi:https://doi.org/10.12669/pjms.331.12572. [Google Scholar] [PubMed] [CrossRef]
30. Bunevicius A, Katkute A, Bunevicius R. Symptoms of anxiety and depression in medical students and in humanities students: relationship with big-five personality dimensions and vulnerability to stress. Int J Soc Psychiatry [Internet]. 2008;54(6):494–501. doi:https://doi.org/10.1177/0020764008090843. [Google Scholar] [PubMed] [CrossRef]
31. Waqas A, Rehman A, Malik A, Muhammad U, Khan S, Mahmood N. Association of ego defense mechanisms with academic performance, anxiety and depression in medical students: a mixed methods study. Cureus [Internet]. 2015;7(9):e337. doi:https://doi.org/10.7759/cureus.337. [Google Scholar] [PubMed] [CrossRef]
32. Cheung T, Wong SY, Wong KY, Law LY, Ng K, Tong MT, et al. Depression, anxiety and symptoms of stress among baccalaureate nursing students in Hong Kong: a cross-sectional study. Int J Environ Health Res [Internet]. 2016;13(8):779. doi:https://doi.org/10.3390/ijerph13080779. [Google Scholar] [PubMed] [CrossRef]
33. Prina AM, Ferri CP, Guerra M, Brayne C, Prince M. Prevalence of anxiety and its correlates among older adults in Latin America, India and China: cross-cultural study. Br J Psychiatry [Internet]. 2011;199(6):485–91. doi:https://doi.org/10.1192/bjp.bp.110.083915. [Google Scholar] [PubMed] [CrossRef]
34. Kawakami N, Abdulghani EA, Alonso J, Bromet EJ, Bruffaerts R, Caldas-de-Almeida JM, et al. Early-life mental disorders and adult household income in the World Mental Health Surveys. Biol Psychiatry [Internet]. 2012;72(3):228–37. doi:https://doi.org/10.1016/j.biopsych.2012.03.009. [Google Scholar] [PubMed] [CrossRef]
35. Beesdo K, Pine DS, Lieb R, Wittchen HU. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Arch Gen Psychiatry [Internet]. 2010;67(1):47–57. doi:https://doi.org/10.1001/archgenpsychiatry.2009.177. [Google Scholar] [PubMed] [CrossRef]
36. Aktekin M, Karaman T, Senol YY, Erdem S, Erengin H, Akaydin M. Anxiety, depression and stressful life events among medical students: a prospective study in Antalya. Med Educ [Internet]. 2001;35(1):12–7. doi:https://doi.org/10.1046/j.1365-2923.2001.00726.x. [Google Scholar] [PubMed] [CrossRef]
37. Carmona CR, Rojas AMM, Martínez AN, Martínez EPA, García UT. Ansiedad de los estudiantes de una facultad de medicina mexicana, antes de iniciar el internado. Investigación en Educación Médica [Internet]. 2017;6(21):42–6. doi:https://doi.org/10.1016/j.riem.2016.05.004. [Google Scholar] [CrossRef]
38. Gillis M, Haaga D, Ford G. Normative values for the beck anxiety inventory, fear questionnaire, penn state worry questionnaire, and social phobia and anxiety inventory. Psychol Assess [Internet]. 1995;7(4):450–5. doi:https://doi.org/10.1037/1040-3590.7.4.450. [Google Scholar] [CrossRef]
39. Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21construct validity and normative data in a large non-clinical sample. Br J Clin Psychol [Internet]. 2005;44(2):227–39. doi:https://doi.org/10.1348/014466505X29657. [Google Scholar] [PubMed] [CrossRef]
40. Lisspers J, Nygren A, Soderman E. Hospital Anxiety and Depression Scale (HADsome psychometric data for a Swedish sample. Acta Psychiatrica Scandinavica [Internet]. 1997;96(4):281–6. doi:https://doi.org/10.1111/j.1600-0447.1997.tb10164.x. [Google Scholar] [PubMed] [CrossRef]
41. Gold JA, Johnson B, Leydon G, Rohrbaugh RM, Wilkins KM. Mental health self-care in medical students: a comprehensive look at help-seeking. Acad Psychiatry [Internet]. 2015;39(1):37–46. doi:https://doi.org/10.1007/s40596-014-0202-z. [Google Scholar] [PubMed] [CrossRef]
42. Rosal MC, Ockene IS, Ockene JK, Barrett SV, Ma Y, Hebert JR. A longitudinal study of students’ depression at one medical school. Acad Med [Internet]. 1997;72(6):542–6. doi:https://doi.org/10.1097/00001888-199706000-00022. [Google Scholar] [PubMed] [CrossRef]
43. Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, et al. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med [Internet]. 2016;46(14):2955–70. doi:https://doi.org/10.1017/S0033291716001665. [Google Scholar] [PubMed] [CrossRef]
44. García MJS, Delgado MP, María Trinidad Sánchez Núñez JMR, Portas PB. Diferencias de ansiedad y rendimiento académico en el proceso de enseñanza-aprendizaje con créditos ects. Ensayos [Internet]. 2006;21:203–15. [Google Scholar]
45. Garza MDRR, Salazar MFS, Muñoz AM, Rodríguez CER. El estrés en estudiantes de medicina al inicio y final de su formación académica. Revista Iberoamericana de Educação [Internet]. 2014;66:105–22. doi:https://doi.org/10.35362/rie660381. [Google Scholar] [CrossRef]
46. Morales CF, Pérez VB, León SO, Medrano AJ, Aguilar MEU, Guevara-Guzmán R. Síntomas depresivos y rendimiento escolar en estudiantes de Medicina. Salud Mental [Internet]. 2013;36(1):59–65. doi:https://doi.org/10.17711/SM.0185-3325.2013.008. [Google Scholar] [CrossRef]
47. Bayram N, Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Soc Psychiatry Psychiatr Epidemiol [Internet]. 2008;43(8):667–72. doi:https://doi.org/10.1007/s00127-008-0345-x. [Google Scholar] [PubMed] [CrossRef]
48. Nakamura A. Identity of anxiety lurking in the student’s mind. Urban Housing Sci [Internet]. 2017;99(99):54–60. doi:https://doi.org/10.11531/uhs.2017.99_54. [Google Scholar] [CrossRef]
49. Shimodaira A. Characteristics of the utilization situation in the student counseling room. Journal of Yasuda Women’s University [Internet]. 2015;44:53–61. doi:https://doi.org/10.24613/00000057. [Google Scholar] [CrossRef]
50. Mayer FB, Santos IS, Silveira PS, Lopes MHI, de Souza AR, Campos EP, et al. Factors associated to depression and anxiety in medical students: a multicenter study. BMC Med Educ [Internet]. 2016;16(1):282. doi:https://doi.org/10.1186/s12909-016-0791-1. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools