 Open Access
Open Access
ARTICLE
Reciprocal Association between Psychological Distress and PTSD and Their Relationship with Pre-Displacement Stressors among Displaced Women
1
Faculty of Humanities, North-West University, Mafikeng Campus, 34151, South Africa
2 Department of Psychiatry & Behavioural Sciences, Jane & Terry Semel Institute for Neuroscience & Human Behaviour, University
of California Los Angeles, Los Angeles, 90095, USA
* Corresponding Author: Babatola D. Olawa. Email:
International Journal of Mental Health Promotion 2023, 25(5), 699-710. https://doi.org/10.32604/ijmhp.2023.026852
Received 28 September 2022; Accepted 12 December 2022; Issue published 28 April 2023
Abstract
It is established in the psychological literature that pre-displacement stressors, PTSD symptoms, and psychological distress are associated among internally displaced persons. However, existing studies have not demonstrated the mechanism underlying these associations. This study compared two explanatory models; one with PTSD symptoms severity explaining the indirect association between pre-displacement stressors and psychological distress, and the other with psychological distress explaining the indirect relationship between pre-displacement stressors and PTSD symptoms severity. In a cross-sectional design, 631 women (Mean age = 31.18 ± 8.59) were conveniently and purposely selected from the displaced women harboured in two camps in Borno State, Nigeria, due to the Boko-Haram insurgency. Data were collected utilizing structured questionnaires and subjected to path analyses. Results demonstrated that PTSD symptoms severity and psychological distress indirectly explained their respective and independent association with pre-displacement stressors. However, PTSD symptoms had a statistically larger standardized indirect effect size, greater indirect effect percentage, and bigger kappa-squared (k2) effect size than psychological distress. PTSD symptoms and psychological distress may have a reciprocal influence on each other from pre-displacement stressors. However, PTSD symptoms can better explain the association between pre-displacement stressors and psychological distress than the other way around. These outcomes have important implications for the psychological treatment of displaced persons.Keywords
Globally, post-traumatic stress disorder symptomatology is shown to be highly prevalent among individuals exposed to violent attacks. However, prevalence figures have not been uniformly reported and seem dependent on regional differences, the specific population affected, and the type of trauma exposure. In a recent review of the world epidemiology of PTSD and exposure to traumatic events, Bromet et al. [1] reported different prevalence rates for high-risk samples (e.g., veterans and active-duty soldiers) in the developed world (17%–20%), high-stressed areas in less-developed regions (18%–37%), specific individuals exposed to rape (65%), physical abuse (48.5%) and torture (62%). Among internally displaced persons (IDPs) in sub-Saharan Africa, Owoaje et al. [2] estimated figures ranging between 42%–54%, while studies among IDPs in Nigeria provided rates between 63%–78% [3–5].
Although less reported among IDPs and refugees, psychological distress, which includes severe depression, anxiety/insomnia, social dysfunction, and somatic symptoms [6], is also shown to be common among the displaced population. For example, in a systematic review of 38 studies spanning 21 countries with a total adult sample of 39,518 refugees and IDPs, Morina et al. [7] showed that rates for anxiety (1%–81%) and depression (5%–80%) could be relatively as high as PTSD (3%–88%). Similarly, in a systematic review of 29 articles involving 16,010 refugees displaced by war, a prevalence of 23%–80% was found for depression, unspecified anxiety (20.3%–88%), and PTSD (4.4%–86%) [8]. Owoaje et al. [2] further provided the prevalence of depression (31%–67%) among displaced persons in sub-Saharan Africa.
PTSD symptoms and psychological distress among displaced persons are shown to be mainly initiated by pre-displacement stressors or traumatic events resulting from exposure to violence and conflicts. For example, traumatic events such as exposure to assault and threat to life, or witnessing horrors involving the violent death of family members or friends are significant predictors of PTSD symptoms and psychological distress among Syrian war refugees residing in Turkey and Sweden [9]. Hollifield et al. [10] demonstrated that war and non-war trauma (e.g., disaster, sexual assault, and crime) were predictive of mental health outcomes, including PTSD, anxiety, and depression. Gerber et al. [11] also indicated that the number of potentially traumatic events predicted an increase in distress tolerance difficulties, the severity of depressive symptoms, and the manifestation of PTSD symptoms in a sample of women seeking treatment in a community mental health setting. Similar findings were replicated among Syrian refugees, where several traumatic event types were associated with increased probable PTSD and depression [12]. There is a greater risk of psychological distress and higher severity of PTSD symptoms with increased exposure to traumatic events [13].
Although studies have examined the impact of pre-displacement stressors on psychological distress and PTSD symptoms, there is a need to understand how these stressors impact the reciprocal relationship between psychological distress and PTSD symptoms. It has been demonstrated that greater PSTD levels may predict increased psychological distress [14–16], and a history of psychological distress may predict increased PTSD [17,18]. Research has also shown that PTSD is usually comorbid with psychological distress [19,20]. The reciprocal relationship between psychological distress and PTSD has been demonstrated in some theoretical models. For example, Briere’s self-trauma model [21] suggested that PTSD resulting from past trauma impacts psychological distress by causing emotional dysregulation and distorted cognition. Dysfunctional thinking emanating from previous trauma can significantly affect subjective internal states, culminating in post-psychological distress [21,22]. Other models [18,23] have suggested that vulnerability to psychological distress in the face of trauma may predispose the manifestation of PTSD symptoms.
Regarding the more appropriate pathway by which these two mental health outcomes are associated with each other from pre-displacement stressors, it is essential to test a bi-directional framework, where PTSD symptom is specified to indirectly explain the relationship between pre-displacement stressors and psychological distress and another in which psychological distress indirectly explains the association between pre-displacement stressors and PTSD. Accordingly, the principal aim of this study is to examine and compare the magnitude by which PTSD symptoms and psychological distress indirectly explain their respective associations with pre-displacement stressors in a sample of displaced women in North-East Nigeria.
The following research questions are put forward:
(1) Is the relationship between pre-displacement stressors and psychological distress indirectly explained by PTSD symptoms? Or:
(2) Does psychological distress indirectly explain the relationship between pre-displacement stressors and PTSD?
(3) If (1) and (2) are confirmed, which of the two models has a better indirect effect magnitude using kappa-squared (k2) effect size [24], standardized indirect effects, and the percentage of the indirect effect within the total effect?
Study outcomes will extend our knowledge of a more explanatory model by which the reciprocal relationship between PTSD symptoms and psychological distress is associated with pre-displacement stressors.
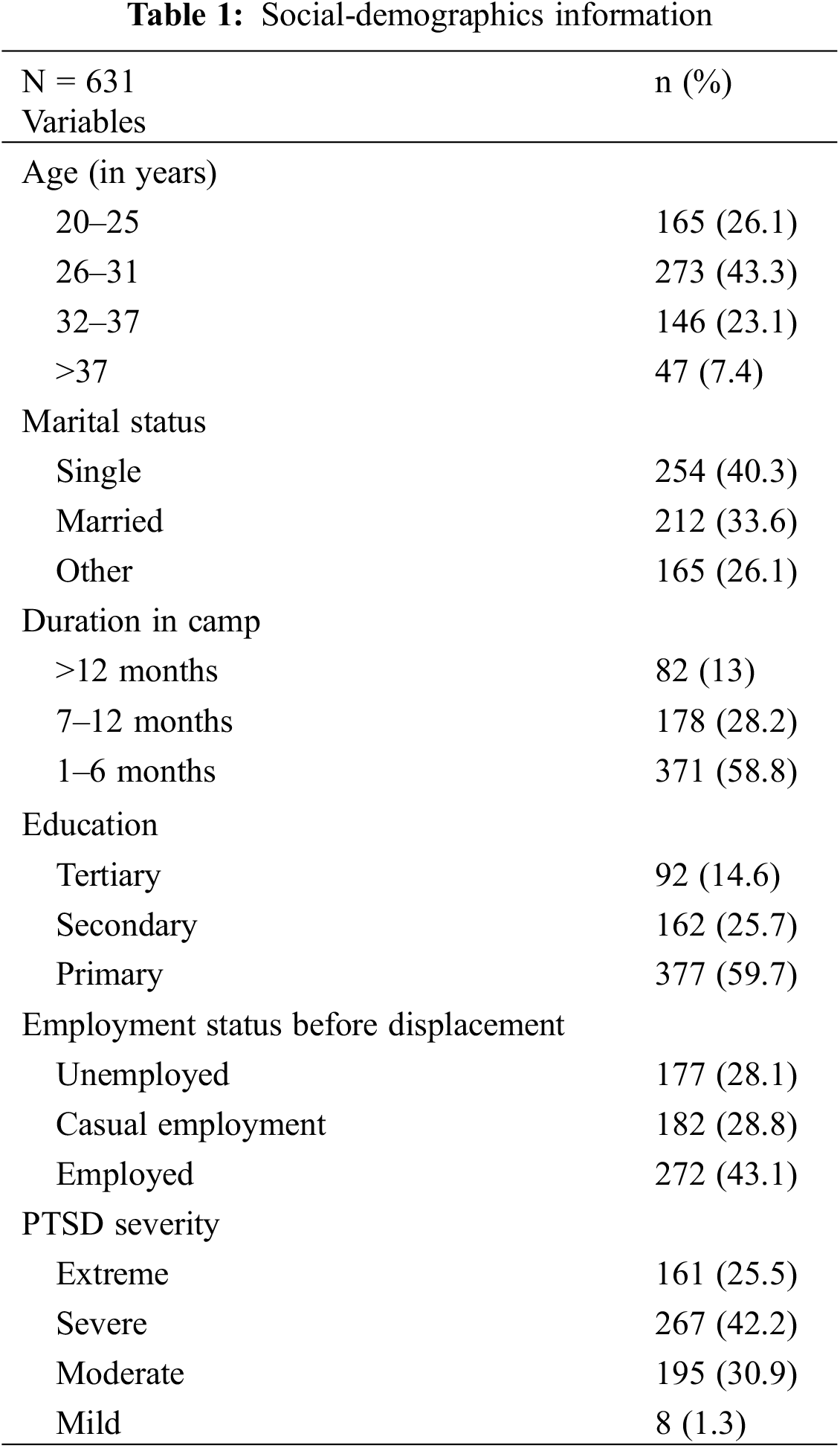
By utilizing the cross-sectional survey design, we conveniently and purposely selected 631 women (Mean age = 31.18 ± 8.59) from the population of IDPs harboured in Mongonu and Baga camps, Borno State, due to the Boko-Haram insurgency in North-East Nigeria. Both camps were established in 2015 due to the rising number of individuals displaced during this period. Inclusion criteria were being female, being able to understand the English language, and being over 18 years of age. We purposively selected women because they constitute the larger proportion of displaced persons and their children are worst afflicted by the insurgency [25]. Table 1 shows that the majority of displaced women in this sample were below the age of 40 (93.2%, n = 588), single (40.3%, n = 254), have had six years of formal education (59.7%, n = 377), were employed before displacement (43.1%, n = 272), and have stayed only up to 6 months in a camp (58.8%, n = 371). By utilizing the DSM 5 clinical trials method of classifying the severity of PTSD symptoms [26], we found 68% and 32%, respectively, for severe/extreme and mild/moderate PTSD symptoms. Using the cut-off criteria of 12 as obtained in the World Health Organisation (WHO) study of mental illness in general health care [27], we found all participants to be positive on psychological distress (M = 24.20 ± 4.85) with minimum and maximum scores of 13 and 33, respectively.
Ethical approval to conduct the study was provided by Government Authorities in Mongonu and Baga camps after being satisfied with the ethical research procedures. Administration of research instruments was accomplished during leisure periods in the camps of individual IDPs with the support of four trained research assistants. We obtained informed consent, assured the confidentiality of the data obtained, and made participants aware of their ability to withdraw at any data collection stage. We projected the recruitment of 700 participants but were able to administer instruments to 657 women based on inclusion criteria and willingness to participate in the study. Instruments were retrieved immediately after completion. However, we discarded a total of 26 cases during data analysis as a result of considerable missing data.
Demographic information: This was measured using a semi-structured questionnaire requiring information on marital status, age, educational level, duration of stay in the camp, and status of employment before migrating to the camp.
Post-traumatic Stress Disorder (PTSD) symptoms: The Severity of Post-traumatic Stress Symptoms—Adult [26] was used in assessing PTSD symptoms. It is an APA-approved instrument for assessing the severity of PTSD symptoms among adults (18+) with a history of exposure to traumatic and highly stressful conditions [26]. The nine items on the scale were scored using a 5-point scale ranging from ‘not at all’ (0) to ‘extremely’ (4). Based on the APA recommendation, the severity of PTSD symptoms can be classified as 0 (none), 1 (mild), 2 (moderate), 3 (severe) and 4 (extreme) after calculating an average score for the nine items [26].
Sample items are: “Feeling very emotionally upset when something reminded you of a stressful experience?” and “Being ‘super alert,’ on guard, or constantly on the lookout for danger?” This study obtained an internal consistency coefficient of .83 for the SPSS-A. In addition, the measurement model provided an absolute fit for the latent construct of PTSD symptoms severity, χ2 (17) = 17.80, p = .40; SRMR = .02, RMSEA = .01 [90% CI = (.00, .04)] and CFI = .99. High scores reflect a high severity of PTSD symptoms.
Psychological Distress: We assessed psychological distress using the General Health Questionnaire (GHQ-12) developed by Goldberg and Williams [27]. The GHQ-12 is designed to assess the presence of psychological distress. GHQ-12 was rated on a 5-point scale ranging from never (1) to very frequently (5). However, in order to calculate the psychological distress prevalence in line with Goldberg et al. [28], we collapsed the scoring into a 4-point scale ranging from never (0) to frequently/very frequently (3). Sample items are: “Thinking of self as worthless?” and “Loss of sleep over worry?” The scale is valid and reliable in measuring psychological distress within the Nigerian context [29,30]. Higher scores reflect greater psychological distress.
Pre-displacement stressors (PDS): We assessed PDS by utilizing the Pre-Migration Difficulties Checklist (PDC) developed by Idemudia et al. [31]. The PMDC is a 22-item checklist scored on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree) and designed for use among migrants to measure the experience of stress and adverse life events associated with victimization, physical and sexual abuse, human rights violation, violence, and conflicts, before and after migration. Sample items are: “I had a threat to my life”, “I almost died”, and “I was beaten and harassed.” Idemudia et al. [31] reported adequate content validity and reliability coefficient for the checklist in a sample of displaced Zimbabweans in South Africa. We also obtained an excellent internal consistency coefficient of .88 for the checklist in this study. The PDC scores were subjected to a confirmatory factor analysis (CFA) to examine whether they fittingly measure the construct of pre-migration stressors. Outcomes of CFA showed that the measurement model adequately fitted the latent construct of pre-migration stressors, χ2 (149) = 525.03, p < .01, RMSEA = .06 [(90% CI = .06, .07)], SRMR = .07, CFI = .93. High scores denote an increased level of pre-displacement stressors.
Descriptive statistics Pearson’s correlations and point-biserial correlations were conducted with the aid of IBM SPSS software (Version 20.0), while path analyses were performed using IBM SPSS AMOS (version 26.0). We generated two models. Model 1 tested the indirect role of PTSD symptoms severity in the relationship between pre-displacement stressors and psychological distress. Model 2 examined the indirect role of psychological distress in the relationship between pre-displacement stressors and PTSD symptom severity. In both models, we controlled the influence of socio-demographics of marital status, education, and duration in camp. Data distribution on all variables was moderately normal given that skewness values were in the range of −1 and 1 [32], and thus allowed us to use maximum likelihood as the estimation method for path analyses. In addition, we replaced missing scores with mean values since missing data on individual cases did not exceed 15% [33].
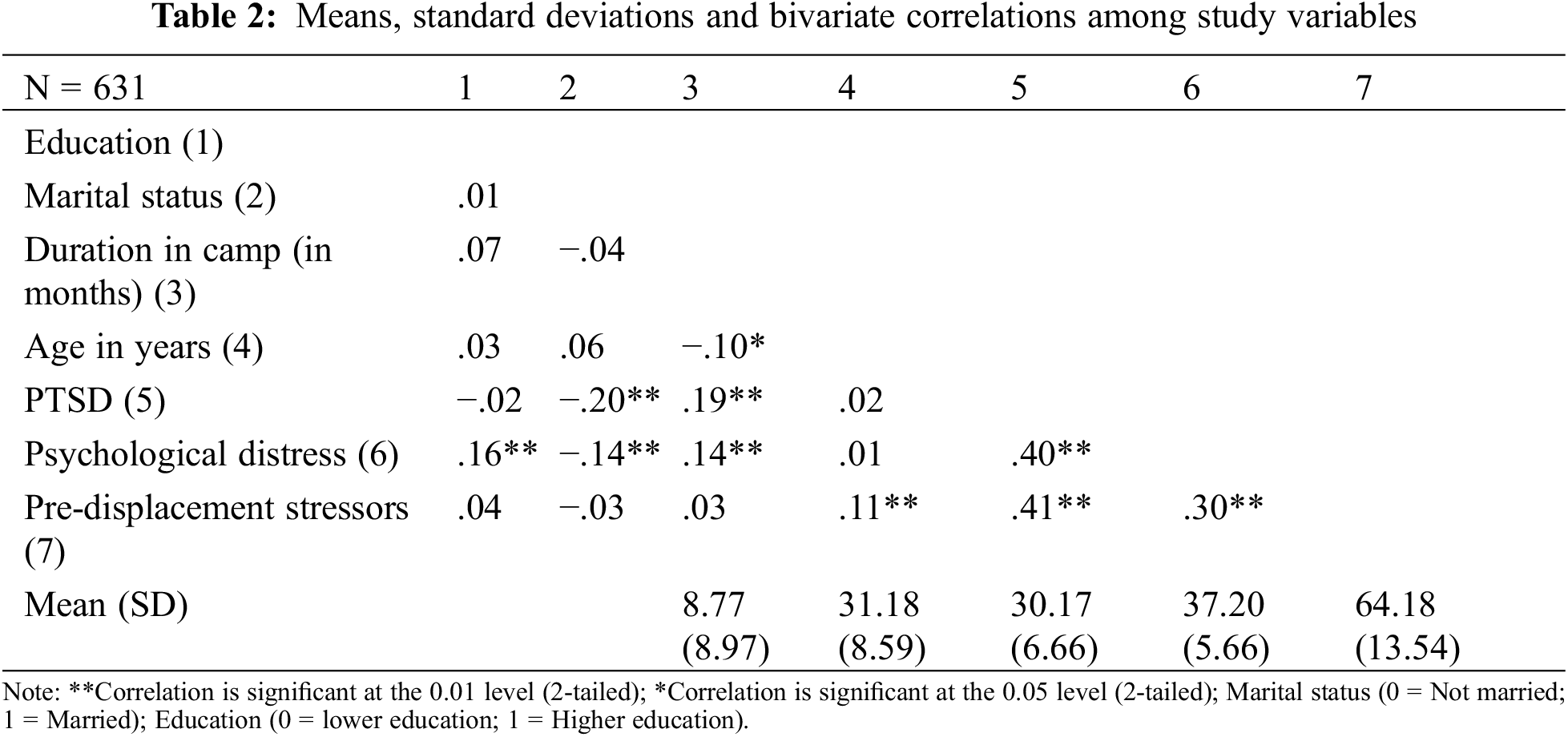
Table 2 shows that all socio-demographics except age (r = .02, p = .79) were significantly associated with psychological distress. Longer duration in camp (r = .14, p < .001), being unmarried (rpb = −.14, p < .001) and having higher education (rpb = .16, p < .001) were associated with psychological distress. In addition, longer duration in camp (r = .19, p < .001) and being unmarried (rpb = −.14, p < .001) were associated with PTSD symptoms severity while education (r = −.02, p = .67) and age (r = .02, p = .79) did not. The main study variables were significantly associated in the expected direction. Pre-displacement stressor was significantly and positively associated with psychological distress (r = .30, p < .001) and PTSD symptoms (r = .41, p < .001). Psychological distress and PTSD symptoms were also positively associated (r = .40, p < .001).
3.2 Indirect Relationship between Pre-Displacement Stressors and Psychological Distress by PTSD Symptoms
Fig. 1 presents the indirect role of PTSD on the relationship between pre-displacement stressors and psychological distress with standardized estimates. Table 3 displays the unstandardized direct, indirect, and total effects, the k2 effect size, and the percentage of indirect effect within the total effect. The direct effects of pre-displacement stressors on psychological distress (b = .07, p < .001) and PTSD symptom severity (b = .20, p < .001) were both significant. The direct effect of PTSD symptoms severity on psychological distress was also significant (b = .26, p < .001). In addition, the total effect was significant (b = .12, p < .001). The control variables of duration in camp (b = .17, p < .001) and marital status (b = −.19, p < .001) were significant on PTSD symptoms severity, while education (b = .15, p < .001) and marital status (b = −.07, p = .046) were significant on psychological distress, as shown in their standardized values.
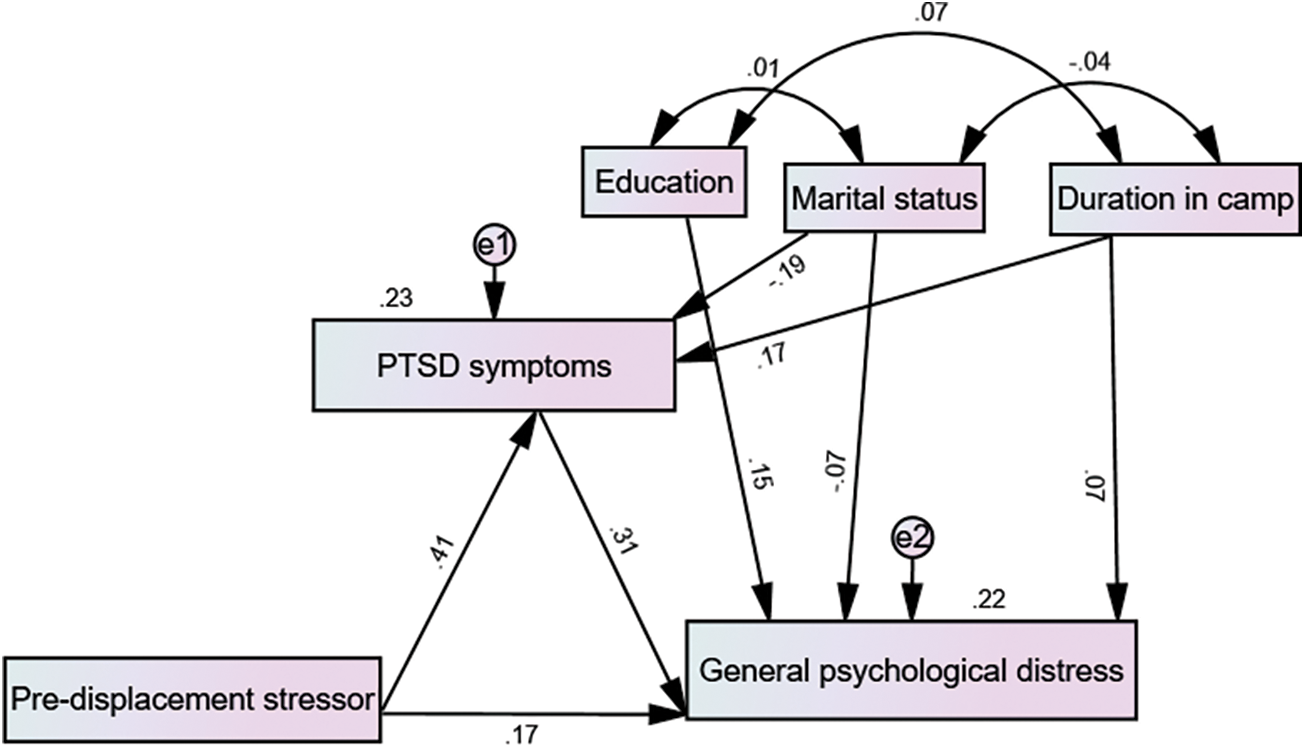
Figure 1: Model showing the mediating role of PTSD symptoms with standardized estimates
The indirect role of the severity of PTSD symptoms on the association between pre-displacement stressors and psychological distress was significant, given that the 95% bias-corrected confidence interval for indirect effect did not pass through zero (b = .05 [.04, .07]). Since the direct effect of pre-displacement stressors on psychological distress (b = .07) was still significant, we conclude that PTSD has a partial indirect role in the relationship between pre-displacement stressors and psychological distress.
3.3 Indirect Relationship between Pre-Displacement Stressors and PTSD Symptoms by Psychological Distress
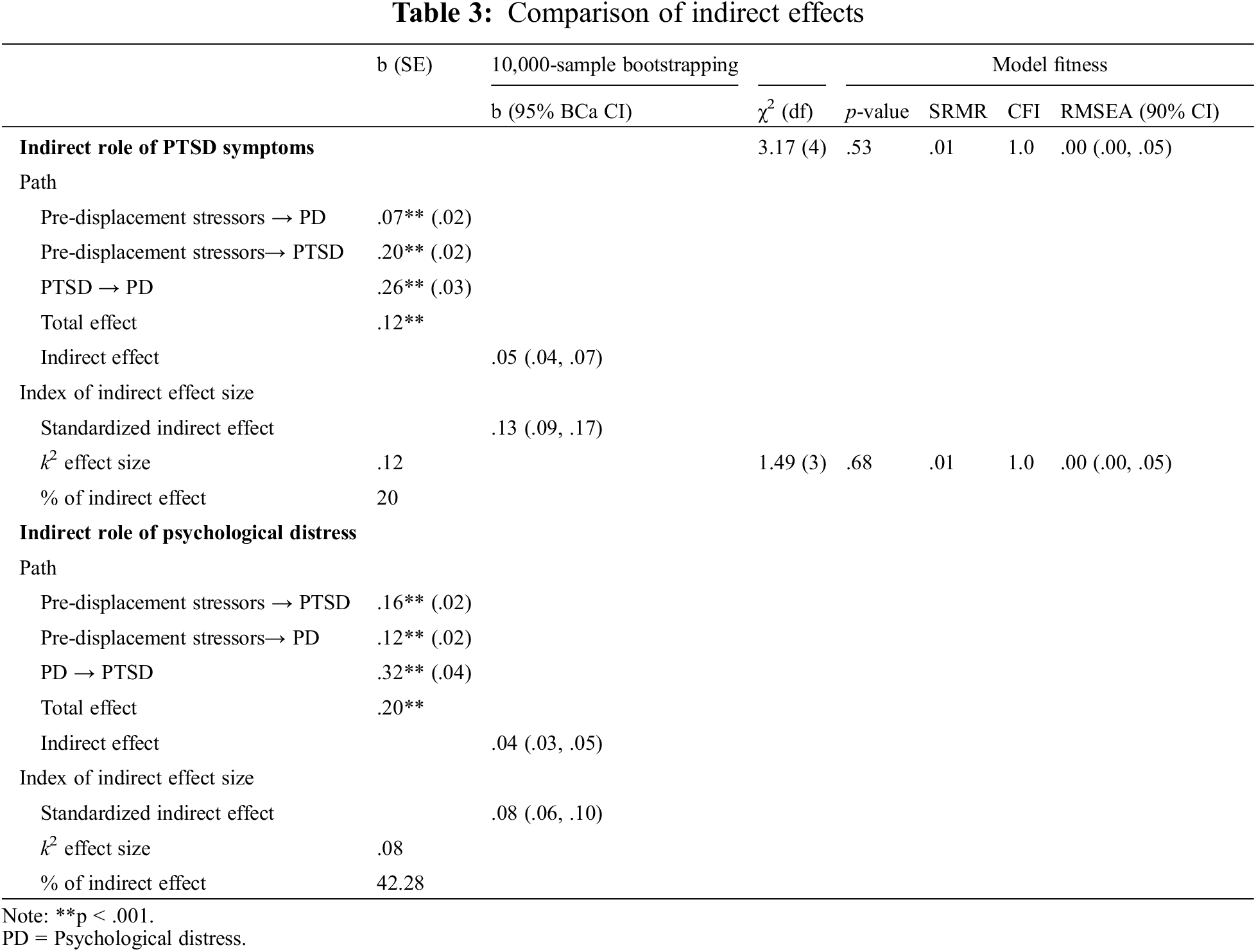
Fig. 2 presents the indirect role of psychological distress on the relationship between pre-displacement stressors and PTSD symptoms with standardized estimates. As shown in Table 3, the unstandardized direct effect of pre-displacement stressors on PTSD symptoms (b = .16, p < .001) and psychological distress (b = .12, p < .001) were both significant. The unstandardized direct effect of psychological distress on PTSD symptoms was also significant (b = .32, p < .001). In addition, the unstandardized total effect was significant (b = .20, p < .001). The control variables of duration in camp (b = .14 vs. b = .12), marital status (b = −.16 vs. b = −.13), and education (b = −.08 vs. b = .14) were all significant on PTSD symptoms and psychological distress, respectively.
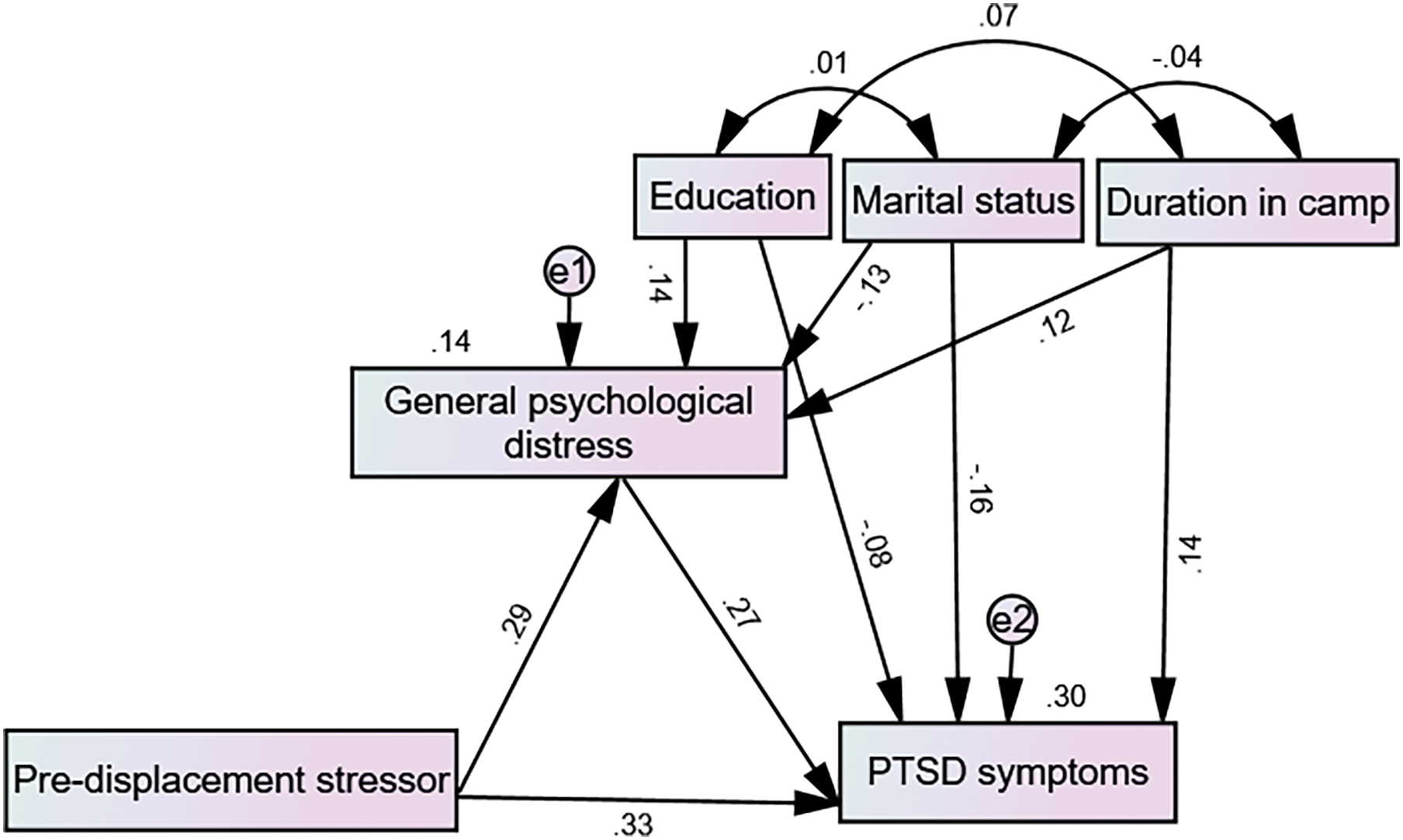
Figure 2: Model showing the indirect role of general psychological distress with standardized estimates
The indirect role of psychological distress on the association between pre-displacement stressors and severity of PTSD symptoms was significant, given that the 95% bias-corrected confidence interval for indirect effect did not pass through zero (b = .04 [.03, .05]). Therefore, since the direct effect of pre-displacement stressors on PTSD symptoms is significant, we conclude that psychological distress partially and indirectly explains the relationship between pre-displacement stressors and PTSD symptom severity.
3.4 Comparing the Indirect Effects of PTSD Symptoms and Psychological Distress
As indicated in Table 3, the standardized indirect effect of pre-displacement stressors on psychological distress through PTSD symptoms is higher compared to the standardized indirect effect of pre-displacement stressors on PTSD symptoms through psychological distress (β = .13 [.09, .17] vs. β = .08 [.06, .10]). To evaluate the statistical difference between the standardized indirect effect through PTSD symptoms (SI-PTSD) and the standardized indirect effect through psychological distress (SI-PD), half of the mean of the overlapping confidence intervals (.015) was added to the SI-PTSD beta weight lower bound score (.09), equaling .105 [34]. Since the SI-PD upper band score of .10 is lower than .105, it can be established that the difference between SI-PTSD and SI-PD beta weights (Δb = 0.05) was statistically significant. Thus, SI-PTSD is larger than SI-PD (p < .05). In addition, the percentage of the indirect effect within the total effect is greater via PTSD (42.28%) than via psychological distress (20%). This is also corroborated by the greater k2 effect size (.12) via PTSD symptoms compared to the k2 effect size (.08) via psychological distress. However, both effect sizes are moderate according to the criteria of [35].
It is known that pre-displacement stressors and exposure to war trauma have a significant impact on the severity of PTSD symptoms and psychological distress among displaced persons [9,10]. However, existing studies have not demonstrated whether pre-displacement stressors impact psychological distress through PTSD symptoms or whether pre-displacement stressors impact PTSD symptoms through psychological distress. Therefore, by utilizing a bi-directional framework, this study examined the indirect role of PTSD on the relationship between pre-displacement stressors and psychological distress and the indirect role of PTSD symptoms severity on the relationship between pre-displacement stressors and psychological distress. Besides, we also examined the roles of some socio-demographic variables on both severity of PTSD symptoms and psychological distress and specified them as control variables.
Our results confirmed previous findings showing that pre-displacement stressors are associated with PTSD symptoms and psychological distress among the displaced population [13,9]. Similar to the outcomes of previous works [14–16], our results showed a significant and positive relationship between psychological distress and PTSD symptoms. Results further suggested that longer duration in camp and being single predicted higher levels of PTSD symptoms severity and psychological distress. Also, the influence of educational status varied on PTSD symptoms severity and psychological distress. Higher education predicted lower PTSD symptom severity and increased psychological distress. IDPs with higher education may feel more distressed because the current displacement has perhaps thwarted their ambitious goals, terminated their employment, and driven them to underutilization of their skills and potential.
On the other hand, higher education may contribute to personal resources to lower PTSD symptom severity. Present findings corroborate the results of past studies showing that longer duration in camp [36], lower education [9], and single status [37] may predispose higher PTSD symptoms among trauma-affected individuals. More recently, the association between singlehood and increased psychological distress among displaced persons is attested to in the literature [38].
Regarding the study’s primary research questions, we established evidence for a bi-directional association between PTSD symptom severity and psychological distress in relation to pre-displacement stressors. Specifically, results showed that PTSD symptom severity has an indirect role in the relationship between pre-displacement stressors and psychological distress, and psychological distress has an indirect role in the relationship between pre-displacement stressors and PTSD symptom severity. In addition, although both models have moderate k2 effect sizes, we found that PTSD has a bigger k2 effect size compared to psychological distress. The comparison of standardized indirect effect values also confirmed this difference. In addition, the percentage of the indirect effect within the total effect is greater for PTSD than psychological distress.
These findings confirm that PTSD symptoms severity and psychological distress have a bi-directional relationship [16,18,20]. In addition, outcomes imply that PTSD symptom severity can partly explain the mechanism through which pre-displacement stressors impact psychological distress and that psychological distress can partly explain how pre-displacement stressors impact PTSD symptoms severity. However, PTSD symptoms severity may explain these mechanisms better.
Results should be interpreted with caution due to some limitations. The use of a cross-sectional design limits making a concluding direction of causality among study variables [39]. Longitudinal designs are needed to imply such a conclusion [40]. Also, generalizing results to other displaced persons, including men, children, adolescents, and those who do not understand the use of the English language, may be limited, given that our sample consisted only of adult women who understood the English language. Prospective studies in this area should adopt samples with more characteristics.
Moreover, PTSD was not diagnosed in this study; instead, we assessed the severity of PTSD symptoms. Hence, our models focused on the association between PTSD symptoms severity and psychological distress. Future bi-directional models may specifically associate actual diagnoses of PTSD and psychological distress with pre-displacement stressors.
This study established that PTSD symptom severity plays an indirect role between pre-displacement stressors and psychological distress, and psychological distress indirectly explains the relationship between pre-displacement stressors and the severity of PTSD symptoms. Although both PTSD symptom severity and psychological distress indirectly explain their relations with pre-displacement stressors, it is suggested that the indirect role of PTSD symptom severity is more robust than that of psychological distress. Findings imply that treatment targeting mental health problems from pre-displacement stressors among displaced women can proceed by initially managing psychological distress to aim for a reduction in PTSD symptoms or by initial management of PTSD symptoms to promote a reduction in psychological distress. However, initial management of PTSD symptoms can foster a better prognosis in the remission of psychological distress than the other way around.
Acknowledgement: We thank the National Institutes of Health (NIH)/Fogarty International Centre for supporting this study. Many appreciations to all the participants that took part in this study.
Funding Statement: This study was funded by the National Institutes of Health (NIH)/Fogarty International Centre (5D43TW007278-13).
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: ESI, BDO, GW and NW; data collection: ESI; analysis and interpretation of results: BDO, draft manuscript preparation: ESI and BDO. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data will be made available upon reasonable request.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Bromet, E., Karam, E., Koenen, K., Stein, D. (2018). The global epidemiology of trauma exposure and posttraumatic stress disorder. In: Bromet, E., Karam, E., Koenen, K., Stein, D. (Eds.Trauma and posttraumatic stress disorder: Global perspectives from the WHO world mental health surveys, pp. 1–12. Cambridge: Cambridge University Press. https://doi.org/10.1017/9781107445130.002 [Google Scholar] [CrossRef]
2. Owoaje, E. T., Uchendu, O. C., Ajayi, T. O., Cadmus, E. O. (2016). A review of the health problems of the internally displaced persons in Africa. Nigerian Postgraduate Medical Journal, 23, 161–171. https://doi.org/10.4103/1117-1936.196242 [Google Scholar] [PubMed] [CrossRef]
3. Taru, M. Y., Bamidele, L. I., Makput, D. M., Audu, M. D., Philip, T. F. et al. (2018). Post-traumatic stress disorder among internally displaced victims of Boko haram terrorism in North-Eastern Nigeria. Jos Journal of Medicine, 12(1), 8–15. [Google Scholar]
4. Chukwuorji, J. C., Ifeagwazi, C. M., Eze, J. E. (2019). Event centrality influences post-traumatic stress disorder symptoms via core beliefs in internally displaced older adults. Aging & Mental Health, 23(1), 113–121. https://doi.org/10.1080/13607863.2017.1396580 [Google Scholar] [PubMed] [CrossRef]
5. Aluh, D., Okoro, R., Zimboh, A. (2019). The prevalence of depression and post-traumatic stress disorder among internally displaced persons in Maiduguri, Nigeria. Journal of Public Mental Health, 19(2), https://doi.org/10.1108/JPMH-07-2019-0071 [Google Scholar] [CrossRef]
6. Goldberg, D. (1978). Manual of the general health questionnaire. Windsor, UK: NFER-Nelson. [Google Scholar]
7. Morina, N., Akhtar, A., Barth, J., Schnyder, U. (2018). Psychiatric disorders in refugees and internally displaced persons after forced displacement: A systematic review. Frontiers Psychiatry, 9, 433. https://doi.org/10.3389/fpsyt.2018.00433 [Google Scholar] [PubMed] [CrossRef]
8. Bogic, M., Njoku, A., Priebe, S. (2015). Long-term mental health of war-refugees: A systematic literature review. BMC International Health and Human Rights, 15, 29. https://doi.org/10.1186/s12914-015-0064-9 [Google Scholar] [PubMed] [CrossRef]
9. Chung, M. C., AlQarnib, N., AlMazroueib, M., Muhairib, S. A., Shakrac, M. et al. (2018). The impact of trauma exposure characteristics on post-traumatic stress disorder and psychiatric co-morbidity among Syrian refugees. Psychiatry Research, 259(1), 310–315. https://doi.org/10.1016/j.psychres.2017.10.035 [Google Scholar] [PubMed] [CrossRef]
10. Hollifield, M., Warner, T. D., Krakow, B., Westermeyer, J. (2018). Mental health effects of stress over the life span of refugees. Journal of Clinical Medicine, 7(2), 25. https://doi.org/10.3390/jcm7020025 [Google Scholar] [PubMed] [CrossRef]
11. Gerber, M. M., Frankfurt, S. B., Contractor, A. A., Oudshoorn, K., Dranger, P. et al. (2018). Influence of multiple traumatic event types on mental health outcomes: Does count matter? Journal of Psychopathology and Behavioral Assessment, 40(4), 645–654. https://doi.org/10.1007/s10862-018-9682-6 [Google Scholar] [CrossRef]
12. Mahmood, H. N., Ibrahim, H., Goessmann, K., Ismail, A. A., Neuner, F. (2019). Post-traumatic stress disorder and depression among Syrian refugees residing in the Kurdistan region of Iraq. Conflict and Health, 13, 51. https://doi.org/10.1186/s13031-019-0238-5 [Google Scholar] [PubMed] [CrossRef]
13. Kanesarajah, J., Waller, M., Zheng, W. Y., Dobson, A. J. (2016). Unit cohesion, traumatic exposure and mental health of military personnel. Occupational Medicine, 66(4), 308–315. https://doi.org/10.1093/occmed/kqw009 [Google Scholar] [PubMed] [CrossRef]
14. Maselesele, V. M., Idemudia, E. S. (2013). The role of social support in the relationship between mental health and post-traumatic stress disorder amongst orthopaedic patients. Curationis, 36(1). https://doi.org/10.4102/curationis.v36i1.122 [Google Scholar] [PubMed] [CrossRef]
15. Slanbekova, G., Chung, M. C., Abildina, S., Sabirova, R., Kapbasova, G. et al. (2017). The impact of coping and emotional intelligence on the relationship between post-traumatic stress disorder from past trauma, adjustment difficulty, and psychological distress following divorce. Journal of Mental Health, 26(4), 334–341. https://doi.org/10.1080/09638237.2017.1322186 [Google Scholar] [PubMed] [CrossRef]
16. Fang, S., Chung, M. C. (2019). The impact of past trauma on psychological distress among Chinese students: The roles of cognitive distortion and alexithymia. Psychiatry Research, 271(3), 136–143. https://doi.org/10.1016/j.psychres.2018.11.032 [Google Scholar] [PubMed] [CrossRef]
17. Silverman, J. J., Singh, N. N., Carntanico, S. J., Lindstrom, K. A., Best, A. M. et al. (1999). Psychological distress and symptoms of post-traumatic stress disorder in Jewish adolescents following brief exposure to concentration camps. Journal of Child and Family Studies, 8(1), 71–78. https://doi.org/10.1023/A:1022998611853 [Google Scholar] [CrossRef]
18. Breslau, N., Troost, J. P., Bohnert, K., Luo, Z. (2013). Influence of predispositions on post-traumatic stress disorder: Does it vary by trauma severity? Psychological Medicine, 43(2), 381–390. https://doi.org/10.1017/S0033291712001195 [Google Scholar] [PubMed] [CrossRef]
19. McFarlane, A. C. (2000). Post-traumatic stress disorder: A model of the longitudinal course and the role of risk factors. Journal of Clinical Psychiatry, 61(5), 15–20. [Google Scholar] [PubMed]
20. Flory, J. D., Yehuda, R. (2015). Co-morbidity between post-traumatic stress disorder and major depressive disorder: Alternative explanations and treatment considerations. Dialogues in Clinical Neuroscience, 17(2), 141–150. https://doi.org/10.31887/DCNS.2015.17.2/jflory [Google Scholar] [CrossRef]
21. Briere, J. (1996). A self-trauma model for treating adult survivors of severe child abuse. In: Briere, J., Berliner, L., Bulkley, J. A., Jenny, C., Reid, T. (Eds.The APSAC handbook on child maltreatment, 2nd edition, pp. 140–157. Newbury Park, CA: Sage Publications. [Google Scholar]
22. Briere, J. (2002). Treating adult survivors of severe childhood abuse and neglect: Further development of an integrative model. In: Myers, L., Berliner, L., Briere, J., Hendrix, C. T., Reid, T. et al. (Eds.The APSAC handbook on child maltreatment, 2nd edition, pp. 175–203. Newbury Park, CA: Sage Publications. [Google Scholar]
23. Berntsen, D., Rubin, D. C., Johansen, M. K. (2008). Contrasting models of post-traumatic stress disorder: Reply to monroe and mineka. Psychological Review, 115(4), 1099–1106. https://doi.org/10.1037/a0013730 [Google Scholar] [PubMed] [CrossRef]
24. Preacher, K. J., Kelley, K. (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16(2), 93–115. https://doi.org/10.1037/a0022658 [Google Scholar] [PubMed] [CrossRef]
25. Adimula, R. A., Ijere, I. N. (2018). Psycho-social traumatic events among women in Nigeria. Madridge Journal of AIDS, 2(1), 17–28. https://doi.org/10.18689/mja-1000104 [Google Scholar] [CrossRef]
26. Kilpatrick, D. G., Resnick, H. S., Friedman, M. J. (2013). Severity of posttraumatic stress symptoms—adult. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM5_Severity-of-Posttraumatic-Stress-Symptoms-Adult.pdf [Google Scholar]
27. Goldberg, D., Williams, P. (1988). A user’s guide to the general health questionnaire. Windsor, UK: NFER-Nelson. [Google Scholar]
28. Goldberg, D. P., Gater, R., Sartorius, N., Ustun, T. B., Piccinelli, M. et al. (1997). The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychological Medicine, 27(1), 191–197. https://doi.org/10.1017/S0033291796004242 [Google Scholar] [PubMed] [CrossRef]
29. Guruje, O., Obikoya, B. (1990). The GHQ-12 as a screening tool in a primary care setting. Social Psychiatry and Psychiatric Epidemiology, 25(5), 276–280. https://doi.org/10.1007/BF00788650 [Google Scholar] [PubMed] [CrossRef]
30. Olawa, B. D., Idemudia, E. S., Umeh, C. S. (2019). The association between psychological commitments to team and mental health of football fans within an academic setting. Journal of Happiness Studies, 21(5), 1549–1559. https://doi.org/10.1007/s10902-019-00142-6 [Google Scholar] [CrossRef]
31. Idemudia, E. S., William, J. K., Boehnke, K., Wyatt, G. (2013). Gender differences in trauma and post-traumatic stress symptoms among displaced Zimbabweans in South Africa. Journal of Traumatic Stress Disorders and Treatment, 2(3). https://doi.org/10.4172/2324-8947.1000110 [Google Scholar] [PubMed] [CrossRef]
32. Blanca, M. J., Arnau, J., López-Montiel, D., Bono, R., Bendayan, R. (2013). Skewness and kurtosis in real data samples. Methodology, 9(2), 78–84. https://doi.org/10.1027/1614-2241/a000057 [Google Scholar] [CrossRef]
33. Hair, J. F., Black, W. C., Babin, B. J., Anderson, R. E. (2010). Multivariate data analysis, 7th edition. Englewood Cliffs: Prentice Hall. [Google Scholar]
34. Cumming, G. (2009). Inference by eye: Reading the overlap of independent confidence intervals. Statistics in Medicine, 28(2), 205–220. https://doi.org/10.1002/sim.3471 [Google Scholar] [PubMed] [CrossRef]
35. Cohen, J. (1988). Statistical power analysis for the behavioral sciences, 2nd edition. Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers. [Google Scholar]
36. Fino, E., Mema, D., Russo, P. M. (2020). War trauma exposed refugees and post-traumatic stress disorder: The moderating role of trait resilience. Journal of Psychosomatic Research, 129(9), 109905. https://doi.org/10.1016/j.jpsychores.2019.109905 [Google Scholar] [PubMed] [CrossRef]
37. Richardson, J. D., Naifeh, J. A., Elhai, J. D. (2007). Post-traumatic stress disorder and associated risk factors in Canadian peacekeeping veterans with health-related disabilities. The Canadian Journal of Psychiatry, 52(8), 510–518. https://doi.org/10.1177/070674370705200809 [Google Scholar] [PubMed] [CrossRef]
38. Walther, L., Fuchs, L. M., Schupp, J., von Scheve, C. (2020). Living conditions and the mental health and well‐being of refugees: Evidence from a large‐scale German survey. Journal of Immigrant and Minority Health, 22(5), 903–913. https://doi.org/10.1007/s10903-019-00968-5 [Google Scholar] [PubMed] [CrossRef]
39. Wang, X., Cheng, Z. (2020). Cross-sectional studies: Strengths, weaknesses, and recommendations. Chest, 158(1S), S65–S71. https://doi.org/10.1016/j.chest.2020.03.012 [Google Scholar] [PubMed] [CrossRef]
40. Caruana, E. J., Roman, M., Hernández-Sánchez, J., Solli, P. (2015). Longitudinal studies. Journal of Thoracic Disease, 7(11), E537–E540. https://doi.org/10.3978/j.issn.2072-1439.2015.10.63 [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools