 Open Access
Open Access
ARTICLE
The Impact of COVID-19 on the Mental-Emotional Wellbeing of Primary Healthcare Professionals: A Descriptive Correlational Study
1
The Nethersole School of Nursing, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, 518172, China
2
School of Nursing and Midwifery, College of Health, Medicine and Wellbeing, University of Newcastle, Callaghan, New South
Wales, 2325, Australia
3
School of Nursing, Tung Wah College, Hong Kong, 200051, China
4
Alice Lee Centre for Nursing Studies, National University of Singapore, 079903, Singapore
5
Tung Wah College, Hong Kong, 200051, China
* Corresponding Author: Regina Lai-Tong Lee. Email:
International Journal of Mental Health Promotion 2023, 25(3), 327-342. https://doi.org/10.32604/ijmhp.2022.026388
Received 02 September 2022; Accepted 21 November 2022; Issue published 21 February 2023
Abstract
The present study aimed to examine work environment related factors and frontline primary healthcare professionals’ mental-emotional wellbeing during the COVID-19 pandemic in school communities of Hong Kong. A total of 61 (20%) school health nurses (frontline primary healthcare professionals) participated in a cross-sectional online survey from March to June 2020. Outcomes of mental-emotional health were measured using the Mental Health Continuum-Short Form (14-item scale with three subscales related to emotional, social and psychological wellbeing); the Perceived Stress Scale (10-item scale with two subscales related to perceived helplessness and lack of self-efficacy; and the Coping Orientation to Problems Experienced Inventory (Brief COPE), a 28-item inventory with two subscales related to adaptive and maladaptive strategies. Almost half (42.6%) of participants experienced mental health problems. Those employed in government subsidized schools had signifi- cantly lower scores in mental health wellbeing than those who worked in private schools. Factors relating to increased mental health problems included lack of emotional support, inadequate training relating to infection prevention and control measures, disengagement and self-blame. A variety of factors influencing school health nurses’social, emotional and psychological wellbeing in their work environment during the COVID-19 pandemic were also reported. The mental-emotional wellbeing of school nurses may relate to their subjective feeling of loneliness as participants were the sole frontline primary healthcare professional working in the school community during the COVID-19 pandemic. Study findings provide relevant evidence for management teams to build a culture of psychological and social support into workplace policies and procedures. Continuous staff development and adequate social support are important to promote the mental-emotional wellbeing of primary healthcare professionals in school communities as they play a significant role in safeguarding resources during pandemics.Keywords
The global COVID-19 pandemic has caused many disruptive events in healthcare systems. As the pandemic progressed, a global ‘call for action’ was announced to build resilient healthcare systems, grounded in primary healthcare [1]. Since January 2019, COVID-19 case numbers have continued to increase worldwide, with the number of COVID-19 cases still rapidly rising in South Africa, Brazil, the United States and the United Kingdom. As of 19 April 2022, 500,186,525 cumulative cases of COVID-19 were recorded, including 6,190,349 deaths reported to the World Health Organization (WHO) [2]. At the same time in Hong Kong, 1,540,803 cumulative cases of COVID-19 were recorded, including 9,690 deaths [3]. The COVID-19 pandemic has caused tremendous long-term effects on physical, social and psychological aspects of life resulting in symptoms of anxiety, panic, distress and feelings of uncertainty, tension and pandemic fatigue [4–6]. Stress is another effect of the COVID-19 pandemic. Stress may be caused by physical demands on the body or social and environmental conditions that are potentially harmful, beyond control and exceed an individual’s coping resources. Stressful conditions and environments may affect psychological responses resulting in depression, anxiety, insomnia, decreased coping abilities and loss of control [7,8]. The effects of stress stemming from the COVID-19 pandemic may be commonly observed in primary healthcare providers as they care for infected patients in acute care settings, but equally shoulder the worry of becoming infected with the virus themselves and further transmitting the virus to their family members and loved ones [7,9]. By the same token, the effects of stress may be observed in primary healthcare professionals (PHPs) [10,11] working in settings such as school communities and community health centres [12]. A recent qualitative study reported PHPs experienced work-related stress symptoms such as depression, anxiety and tension during the COVID-19 pandemic due to working independently without any healthcare support in the community [8]. Additionally, healthcare resources and supplies for treating, managing and preventing the COVID-19 virus that are distributed into acute care settings rather than into school communities and community health centres may also result in increases levels of stress in PHPs.
Perceived stressors healthcare providers experience during daily work routines may affect physical health and mental wellbeing [13,14]. A study conducted in Wuhan, China reported 45% and 60% of frontline healthcare workers experience symptoms of depression and anxiety respectively when caring for hospitalized patients diagnosed with COVID-19 [15]. A study conducted in Spain, reported high prevalence rates of psychological issues, with 67.55%, 55.89% and 62.99% of healthcare workers expressing anxiety, depression and stress, respectively [6]. An Italian study, conducted during the early stages of the pandemic, found healthcare providers experienced high levels of work-related stress and pressure resulting from the pandemic [16]. Furthermore, a review of literature highlights that the COVID-19 pandemic has substantially affected the psychological wellbeing of frontline hospital staff, with nursing staff at a higher risk of adverse mental health outcomes compared to other medical staff [10,17].
Numerous studies only report the effects of COVID-19 on the mental wellbeing of hospital staff in acute care settings, ignoring staff working in school communities [17–19]. Aside from acute care settings, PHPs in school communities (including school nurses and school doctors), and primary healthcare providers working in diverse primary healthcare settings have also been overlooked in terms of research and the impact and effect of the COVID-19 pandemic. This may come as a surprise due to their significant role in fighting against COVID-19 with limited supplies and resources within communities. Their limited access to supplies and resources may lead to high levels of stress [20,21]. In primary healthcare settings, PHPs are known to play an essential role as ‘gatekeepers’ of health information and have efficiently implemented strategies to reduce the spread of COVID-19, particularly in school settings (including international schools where students often come from different cultures; and special schools where students have intellectual disabilities). A recent qualitative study examining the experiences of PHPs reported that PHPs felt very stressed and expressed many challenges were added to their existing roles during the COVID-19 pandemic [4]. Unfortunately, limited studies examining mental wellbeing and coping strategies used by PHPs working in these settings during the COVID-19 pandemic exist, warranting further investigation. Additionally, there are limited studies investigating the effects of associated factors on PHPs’ mental health outcomes during the COVID-19 pandemic, also leading to a need for further investigation.
Currently, there is a global need to build resilient healthcare systems grounded in primary healthcare to promote mental health and wellbeing for PHPs by strengthening their capacity building and integrating mental health policies in the workplace [22]. Objectives and strategies for developing mental health policies and the implementation of staff training in primary healthcare settings include: (1) strengthening mental health policies, legislation and plans via increasing awareness of the burden associated with mental health problems and engaging the commitment of governments to reduce this burden; (2) improving the technical capacity of countries to create, review and develop mental health policies, legislation and plans; and (3) developing and disseminating advocacy and policy resources. This can improve PHPs’ efficacy and quality of life by reducing their psychological distress. However, before developing effective approaches and building resilience programs to support PHPs working in school communities, it is important to understand specific sources of anxiety and fear [18]. Exploring the psychological distress and social burdens experienced by PHPs during this pandemic is vital to provide an increased level of understanding of their perceptions, stress and concerns. Increased understanding may provide new critical information that administrative departments and systems may implement to improve supportive mechanisms for PHPs during future infectious disease outbreaks. Thus, the present study aimed to examine the work environment-related factors and effects of the COVID-19 pandemic on PHPs’ mental wellbeing and their stress coping strategies in communities and tertiary education institutes within primary healthcare settings in Hong Kong.
This study adopted a cross-sectional, descriptive correlational design using an electronic survey to investigate mental health status and the relationship between demographic variables, perceived stress and coping strategies in PHPs currently working in primary healthcare settings of Hong Kong, China. The Strengthening the Reporting of Observational Studies in Epidemiology checklist was used as the framework to report the study’s findings [23].
2.2 Participants and Study Setting
Purposive sampling was used. PHPs in school communities were invited to complete an online survey between March and June 2020. A total of N = 61 PHPs were recruited from government-subsided schools, private kindergartens, private schools and tertiary education institutes in Hong Kong via primary healthcare professional bodies. Approximately 300 PHPs currently work in school communities, community healthcare centres and tertiary education institutes (which are considered as primary healthcare settings in Hong Kong). The sample size of N = 61 thus represents 20% of the professional group. Inclusion criteria included: (1) voluntary participation; (2) currently employed PHPs; and (3) PHPs who were able to speak and understand English and Cantonese. Exclusion criteria included: (1) non-PHPs engaged in other positions including management, teaching and scientific research; and (2) PHPs who did not speak and understand English and Cantonese.
This study investigated the effects of the COVID-19 pandemic on mental wellbeing, along with coping strategies in PHPs’ currently working in communities and tertiary education institutes (known as primary healthcare settings in Hong Kong). This cross-sectional study was conducted between March and June 2020. A total of 61 (20% of the total nursing population employed within Hong Kong schools) school health nurses completed in the 15-minute online survey (developed using SurveyMonkey, an electronic data collection program). Once ethical approval had been obtained from the Research Committee of the Professional Association (Ref 2020/003), the online survey was emailed to school health nurses currently working in government-subsided schools, private schools, kindergartens and tertiary education institutes. The online survey was also circulated via email through the communication platform ‘Professional Association’. The online survey was also distributed via emails to affiliated schools in Hong Kong, and via facebook, twitter and other social media networking sites. The participant information sheet and consent form were placed before the first page of the survey. Participants were asked to read the information sheet, which detailed the aim of the study and outlined information regarding confidentiality, anonymity and voluntary participation in the study.
Data were collected using validated and structured questionnaires including demographic data, the 10-item Perceived Stress Scale (PSS-10) [24], the Brief COPE inventory [25] and the Mental Health Continuum Short Form (MHC-SF) [26]. Demographic data collected included gender, age, educational level, income, years of work experience, nationality, caring for patients with COVID-19, training on infection control and available resources for fighting against COVID-19.
The PSS-10 [24] measures levels of perceived stress. It comprises 10 questions, with total perceived stress scores ranging from 0 to 40, with higher scores indicating higher levels of stress. Total scores are grouped into three levels of stress: low (scores ranging from 0 to 13), moderate (scores ranging from 14 to 26) and high (scores ranging from 27 to 40). The PSS-10 is a reliable and validated tool which has been widely used by college students and staff. Cronbach’s alpha of the PSS-10 was evaluated at >0.70, with test-retest reliability of the PSS-10 meeting the criterion of >0.70 [24].
The Brief COPE inventory [25] is an abbreviated version of the Coping Orientation to Problems Experienced (COPE) inventory. It measures how individuals cope with a wide range of adversity including natural disasters. It consists of 28 items that measure 14 factors of two items each, which correspond to a Likert scale ranging from 0 (‘I have not been doing this at all’) to 3 (‘I have been doing this a lot’). The Brief COPE inventory is validated tool and used most frequently for measuring coping strategies. There are two subcategories defined within the inventory: (1) adaptive coping includes eight factors (instrumental support, acceptance, planning, emotional seeking support, reframing, active coping, religion and humour); and (2) maladaptive coping, which includes six factors (self-distraction, self-blame, denial, behavioural disengagement, substance use and negative thinking). Cronbach’s alpha of adaptive and maladaptive coping strategies was 0.81 and 0.88, respectively [27].
The MHC-SF [26] measures the degree to which life has been experienced as unpredictable, uncontrollable and overloaded. It is a 14-item scale measuring emotional wellbeing comprising three subscales: (1) three items for emotional wellbeing (happy, interested in life and satisfied); (2) six items for psychological wellbeing (one item from each of the six dimensions); and (3) five items for social wellbeing (one item from each of the five dimensions) [26]. Total scores on the MHC-SF range from 0 to 70, with higher scores indicating higher levels of wellbeing. Scores may be categorised as flourishing, moderate and languishing. Categories used in this study were flourishing and non-flourishing. Confirmatory factor analysis confirmed the three-factor structure in emotional, psychological and social subscales [26]. These subscales correlated well with the corresponding aspects of wellbeing and functioning, showing convergent validity [28].
Descriptive statistics, including the mean, standard deviation and percentage, were used to summarise the demographic, perceived stress, coping and mental wellbeing variables. The mental wellbeing scale included social, emotional and psychological subscales. An independent sample t-test was used to examine the differences between mean scores of the three domains (i.e., social, emotional and psychological) of mental health status across demographic variables. Pearson’s correlation coefficient was used to examine the linear relationship of the PSS-10 and Brief COPE inventory domains within the three subscales pertaining to participants mental health status. Variables with p < 0.1 (t-test or correlation analysis) were selected as independent variables (multiple linear regression) to explore the association of these variables to the three subscales of mental health statuses. The backward selection method was used to identify the model of best fit. Regression coefficients and 95% confidence intervals were computed. Statistical significance was defined at the 5% level. All computations were computed using IBM SPSS [29].
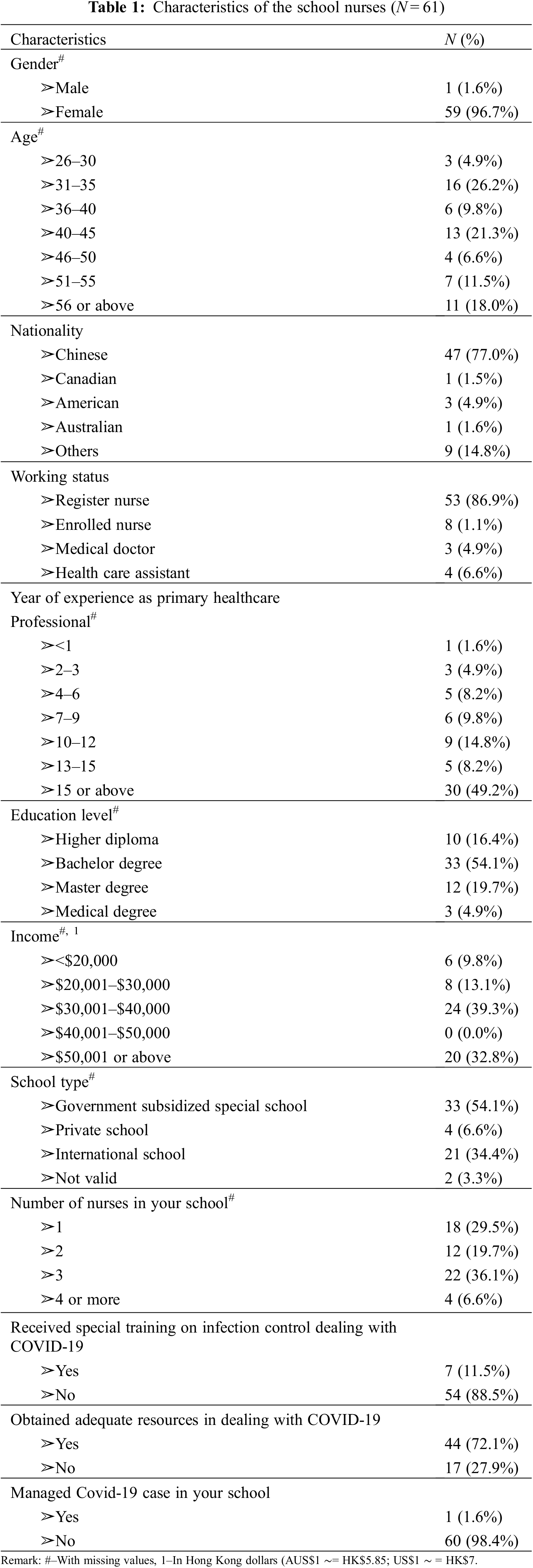
A total of 61 respondents (20%) completed the online survey, corresponding to a response rate of 61%. There were no missing data among the responses to main outcome variables. Table 1 describes the sample in terms of demographics, resources and training completed regarding COVID-19. Respondents included: 59 females (96.7%), with 42 (68.9%) aged below 50 years and 47 (77.0%) Chinese people; 53 (86.9%) registered nurses, of which 44 (72.1%) had 10 or more years of work experience as nurses; and 33 (54.1%) staff from government-subsidised special schools (72.1%) with monthly salaries of HK$30,000 (approximately US$3800) or above. More than half of respondents (44%, 72.1%) implied they obtained adequate resources for dealing with the COVID-19 pandemic. Only seven (11.5%) reported receiving special training for infection control when dealing with COVID-19 (see Table 1).
3.1 Scores of Perceived Stress, Coping Strategies and Mental Wellbeing Measurements by Demographic Variables
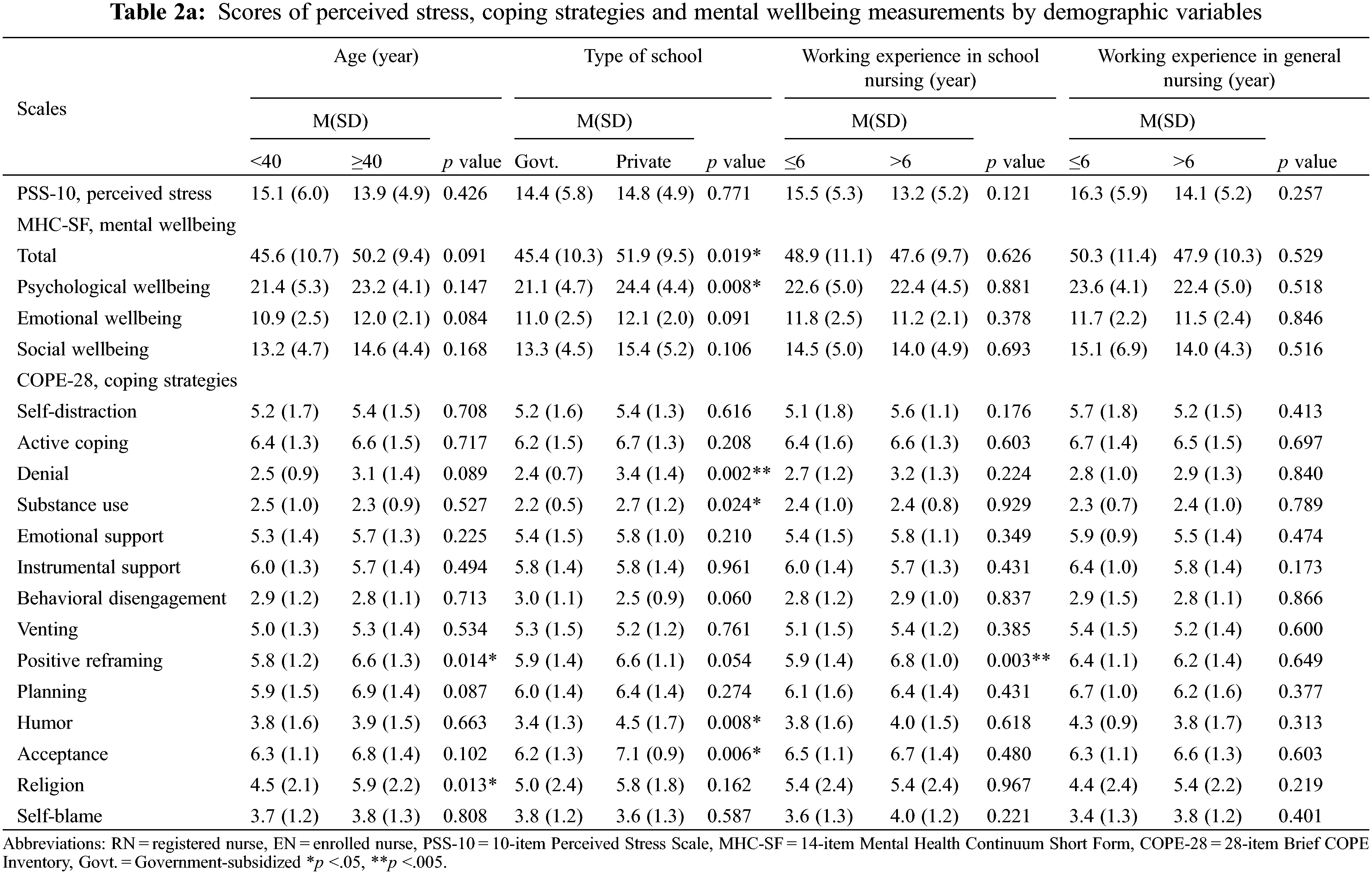
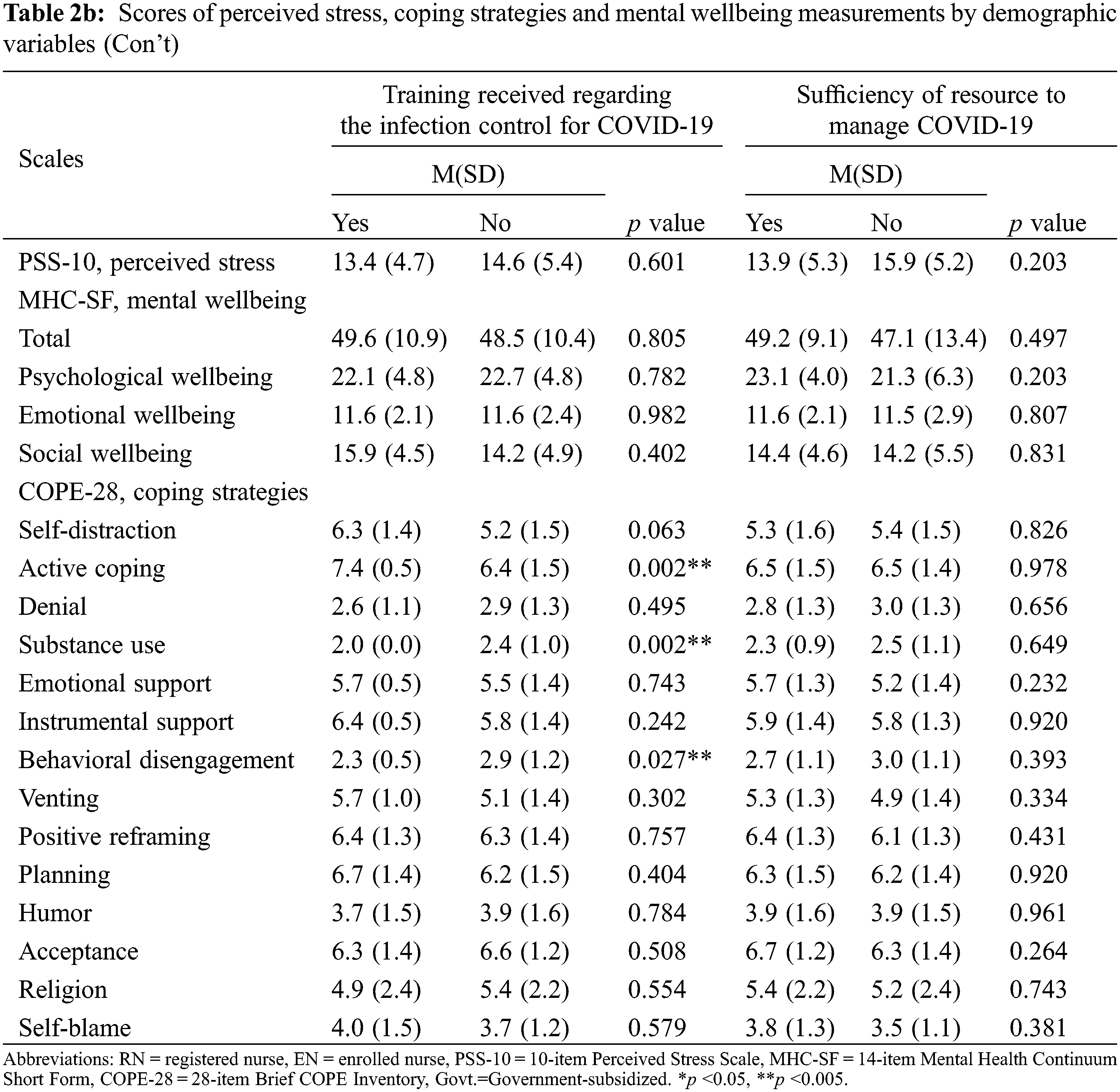
In Table 2, scores for religious coping behaviour in those respondents aged 40 years or above was significantly higher than the younger respondents (p = 0.013). The total score for mental wellbeing in the MHC-SF (p = 0.019) and the psychological wellbeing subscale (p = 0.008) were significantly higher among the school health nurses working in private schools than those working in government-subsidised schools. The Brief COPE behaviour scores for humour, acceptance, denial and substance use among those school health nurses working in private international schools were significantly higher than those working in government-subsided special schools (p < 0.05). Coping behavioural scores for positive reframing (p = 0.043) among those school health nurses who had more than six years of work experience in primary healthcare settings was significantly higher than those who had less than six years of work experience in the primary healthcare settings. Among those who had reportedly received infection control training, the scores for active coping and emotional support were significantly higher (p = 0.002), and the scores for substance use (p = 0.002) and behavioural disengagement (p = 0.027) were significantly lower than those who had received no training (p < 0.05).
3.2 Mean Score Differences of Demographic Variables among Social, Emotional and Psychological Wellbeing for the Mental Health Continuum Short Form
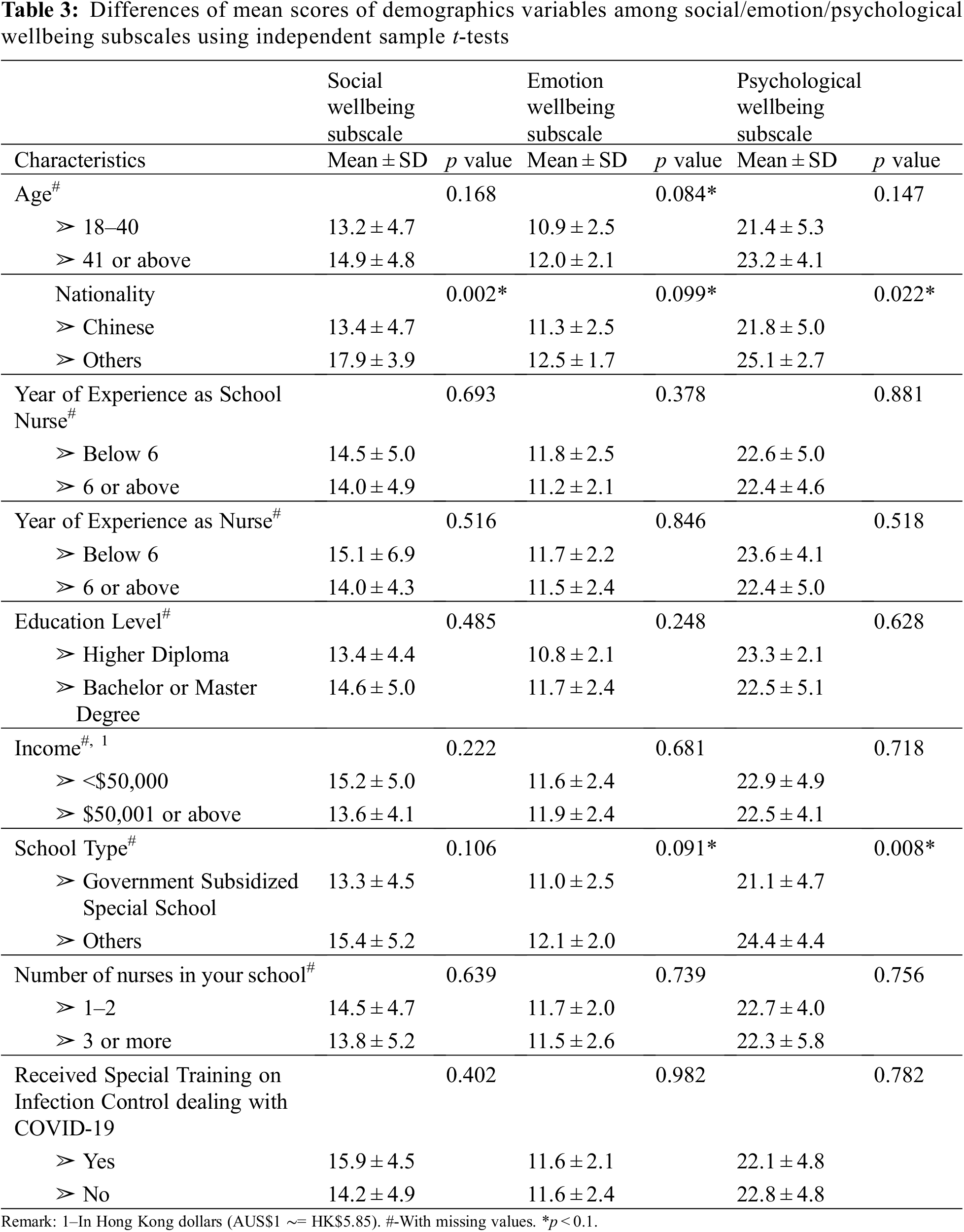
Table 3 shows the results of the independent sample t-tests for the characteristics of each of two groups on the three subscales (social, emotional and psychological wellbeing) of mental health statuses using the MHC-SF across different demographic variables. The emotional wellbeing subscale (p = 0.084) of the age group, the social (p = 0.002), emotional (p = 0.099) and psychological (p = 0.022) wellbeing subscales for nationality, and the social (p = 0.091) and psychological (p = 0.008) wellbeing subscales for the school types (work environment) were significant to the respondents’ mental health statuses. Chinese school health nurses and those who worked in government-subsidised special schools had significantly lower scores for their mental health statuses than those who worked in private schools in the primary healthcare setting.
Mean and standard deviation scores for the PSS-10 and the Brief COPE inventory subscales are presented in Table 4. The mean score for PSS-10 was 14.4 (SD = 5.3), considered a moderate level of perceived stress according to scoring ranges of the PSS-10 [24]. More than half (57.4%) of respondents’ report a flourishing mental health status, and nearly half (42.6%) were non-flourishing due to mental health conditions.
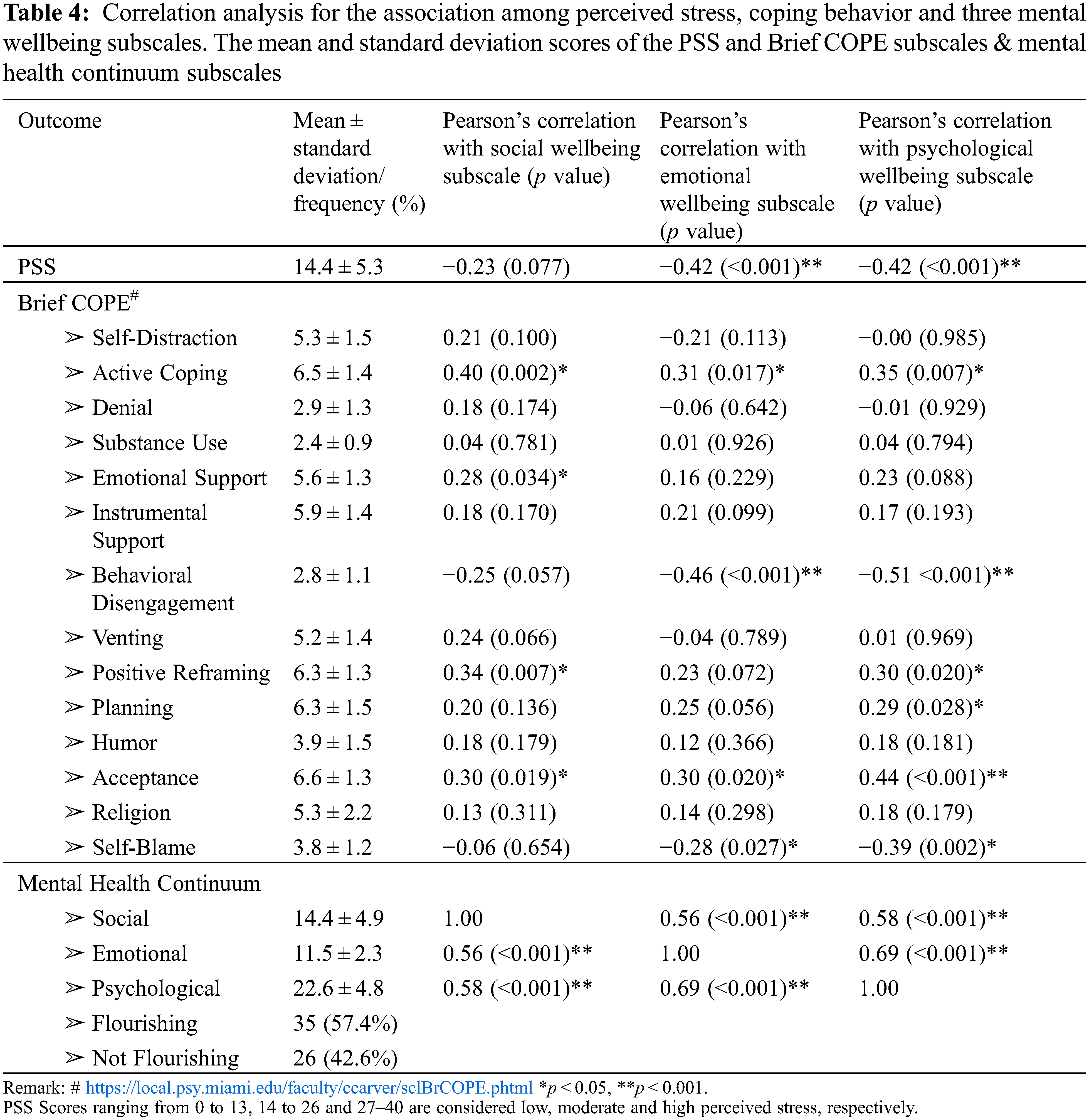
The results of the correlation analysis for the associations among perceived stress, coping behaviours and the three wellbeing subscales of the MHC-SF are presented in Table 4. Perceived stress was significantly negatively correlated with the emotional wellbeing subscale (r = −0.42, p < 0.001) and psychological wellbeing subscale (r = −0.42, p < 0.001) for the MHC-SF.
For the adaptive coping strategies, active coping was positively correlated with the social wellbeing subscale (r = 0.40, p < 0.002), emotional wellbeing subscale (r = 0.31, p < 0.017) and psychological wellbeing subscale (r = 0.35, p < 0.007) for the MHC-SF. Acceptance was also positively correlated with the social (r = 0.30, p < 0.019), emotional (r = 0.30, p < 0.020) and psychological (r = 0.44, p < 0.001) wellbeing subscales. Positive reframing was positively correlated with the social (r = 0.34, p < 0.007) and psychological wellbeing subscales. The emotional support subscale (r = 0.28, p < 0.034) was correlated with the social subscale, and planning (r = 0.29, p < 0.028) was correlated with the psychological wellbeing subscale.
For maladaptive coping strategies, behavioural disengagement (r = −0.46, p < 0.001) and self-blame (r = −0.28, p < 0.027) were negatively correlated with the emotional wellbeing subscale for the MHC-SF. Similarly, behavioural disengagement (r = −0.51, p < 0.001) and self-blame (r = −0.39, p < 0.002) were negatively correlated with the psychological wellbeing subscale.
Results from regression analysis are shown in Table 5. Perceived stress (b = −0.414, 95% CI: −0.629, −0.200), emotional support (b = 1.553, 95% CI: 0.723, 2.383) and nationality (b = 6.195, 95% CI: 3.384, 9.005) were significantly associated with the social wellbeing subscale. Perceived stress (b = −0.178, 95% CI: −0.282, −0.074), behavioural disengagement (b = −0.703, 95% CI: −0.191, −0.216) and nationality (b = 1.507, 95% CI: 0.221, 2.793) were significantly associated with the emotional wellbeing subscale. Perceived stress (b = −0.270, 95% CI: −0.454, −0.086), behavioural disengagement (b = −1.463, 95% CI: −2.614, −0.312), planning (b = 0.842, 95% CI: 0.188, 1.495), self-blame (b = −1.075, 95% CI: −1.975, −0.174) and school type (b = 2.094, 95% CI: 0.178, 4.010) were significantly associated with the psychological wellbeing subscale for the MHC-SF.
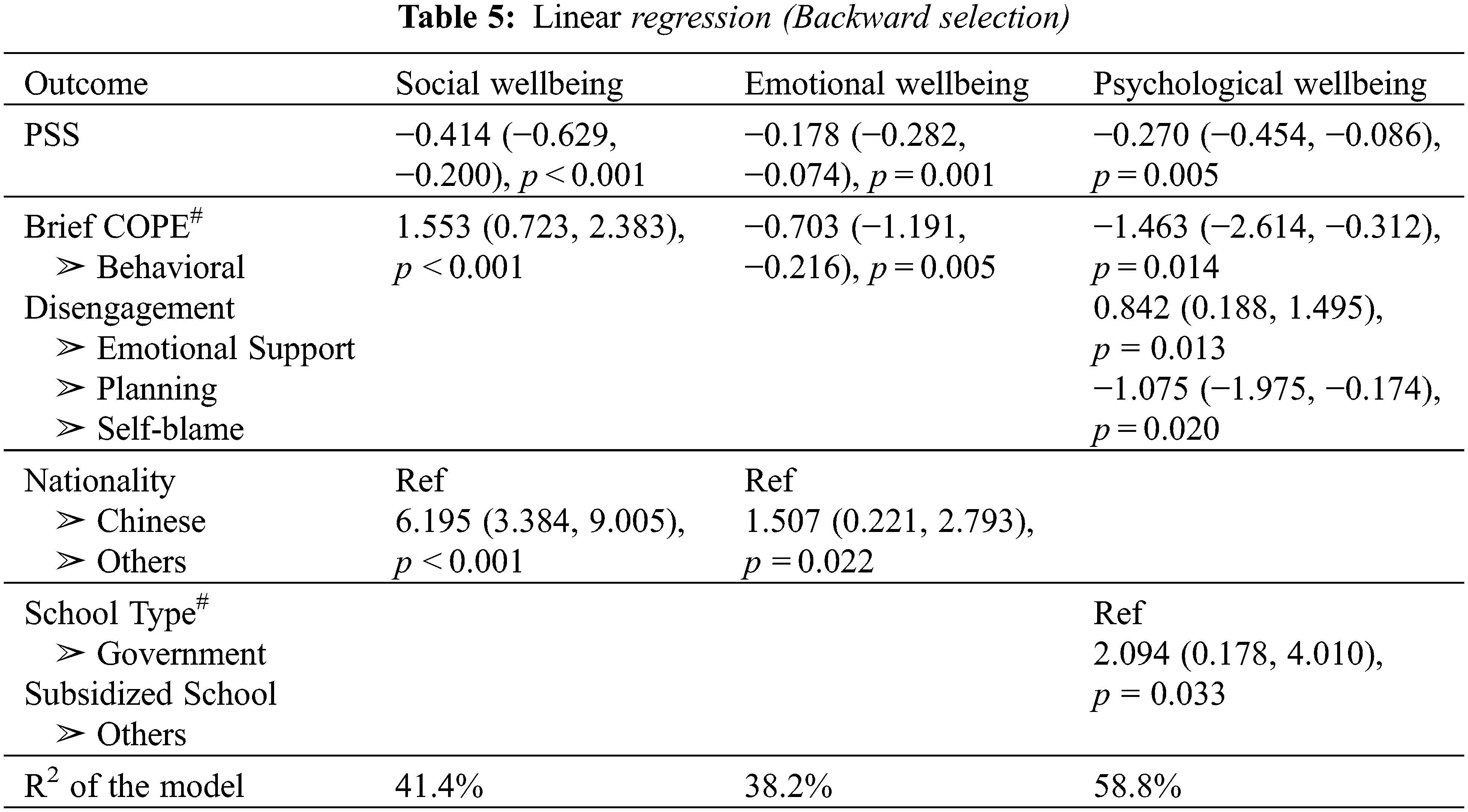
The PSS-10 and subscales of the Brief COPE inventory show high levels of significant correlations (p < 0.01) with the global MHC-SF. Regarding subscales, active coping had significant and positive correlations with the social (p < 0.01) and emotional (p < 0.05) wellbeing subscales. Moreover, positive reframing and acceptance had positive associations with all the subscales for the MHC-SF (p < 0.05). Conversely, behavioural disengagement and perceived stress were significantly negatively correlated with the emotional and psychological wellbeing subscales (p < 0.05). Additionally, self-blame was significantly negatively correlated with the psychological wellbeing subscale (p < 0.01).
Three limitations should be considered when interpreting our study findings. Firstly, the study used an online survey, cross-sectional study design and therefore, no causation between variables can be reported. Second, the study sample size represents only 20% of the total population of PHPs in Hong Kong. Our findings may not be generalisable to other professional healthcare groups in the primary healthcare setting of communities in Hong Kong. Thirdly, school health nurses composed the main portion of PHPs in this community health study. Further research studies should recruit other PHPs, such as allied health professionals, to examine how different demographics and work-related factors may affect changes in the PSS-10, Brief COPE inventory and mental wellbeing. Despite these limitations, these findings provide preliminary data regarding the effects of COVID-19 on PHPs’ mental wellbeing for guiding future studies to plan relevant interventions and training programs for reducing stress and promoting wellbeing.
This study investigated mental health status and its relationship between demographic variables, perceived stress and coping strategies among PHPs including school health nurses working in Hong Kong communities during the COVID-19 pandemic. Results suggest the impact of COVID-19 on the mental-emotional wellbeing of school health nurses may be related to their subjective feelings of loneliness, with worries and uncertainties in fighting against the COVID-19 pandemic as the sole PHP working in the school community. The mean score of the PSS-10 was 14.4, indicating low to moderate levels of stress in this study (see Table 4). More than half (57.4%) of respondents’ report a flourishing mental health status, and nearly half (42.6%) reporting non-flourishing mental health conditions. Fears of uncertainty or becoming infected with the COVID-19 virus were at the forefront of the psychological challenges faced by school health nurses. Chinese school health nurses were found to have lower mental wellbeing scores compared to other nationalities, and those working in government-subsidised special schools had significantly lower scores in the psychological domain. These differences could be related to the availability of resources, support systems, personal coping skills and cultural diversity. As PHPs live in an increasingly multicultural society, school management teams should be aware of cultural differences when coping with stress. Thus, occupational health policies should address those differences to improve employee care.
Workplace policies and occupational health services provided in the workplace to address the healthcare needs of working populations have been identified as an important component of public health strategies [30]. These services can contribute significantly to other government initiatives, such as reducing health inequalities, reducing social exclusion and sickness absence and protecting and promoting the health of the working population. Occupational health services can also help reduce the overall burden of ill health.
This study demonstrates that respondents have experienced low to moderate stress levels related to the availability of emotional support and adequate supplies of personal protective equipment in their work environment during the COVID-19 pandemic. This finding is similar to study findings reported by Kelbiso et al., that poor working environments and stress symptoms were the determinants of healthcare workers’ quality of life [30]. Another study also found that longer exposures to work-related stress would more severely affect the physical and mental wellbeing of primary healthcare workers [31].
The results indicate that respondents’ mental wellbeing was negatively correlated with perceived stress, suggesting that higher levels of perceived stress were associated with lower levels of mental health. A systematic review of the psychological effects of COVID-19 among healthcare professionals found that frontline primary healthcare providers had an increased risk of stress-related disorders, depression and anxiety [32]. Psychosocial supports and intervention strategies are essential for reducing stress and mental health risks. Moreover, workplace support systems and occupational health policies should be designed and integrated into staff development and training programs to promote the mental wellbeing of primary healthcare providers [33].
Results suggest that the impact of COVID-19 on the mental-emotional wellbeing of PHPs could be related to their subjective feeling of loneliness with worries and uncertainties in fighting against the COVID-19 pandemic as the sole PHP working in the community. Our study findings indicate that active coping has significant positive correlations with social and emotional wellbeing. Moreover, positive reframing and acceptance have positive associations with all subscales of the MHC-SF. Emotional support was positively correlated with the social domain of mental health, and planning was positively correlated with the psychological domain of mental health. These findings suggest that mental wellbeing positively correlates with adaptive coping. Barbore and colleagues also found that a positive attitude in the workplace is a protective factor against distress [16]. A systematic review indicated that healthcare professionals use adaptive coping strategies such as acceptance, resilience, active coping and positive framing [33]. Thus, adaptive coping with a positive attitude enables a person to positively interpret a negative situation and contribute to better mental health.
Conversely, the present study findings indicate behavioural disengagement and self-blame have significantly negative correlations with psychological wellbeing. A previous study showed that avoidance coping strategies were associated with higher levels of distress [34]. These findings suggest that schools and institution management teams in the primary healthcare settings should address the potential risk factors that may lead to PHPs adopting negative coping strategies such as self-blame, behaviour disengagement and avoidance. Providing training and resources for developing adaptive coping strategies would promote the mental health outcomes of primary healthcare providers. Additional training is necessary for primary healthcare professionals to prepare for this outbreak and promote preparedness and efficacy in crisis management in the primary healthcare settings in the communities of Hong Kong. To develop effective approaches to support PHPs, it is essential to understand their specific source of stress and how they cope with them. PHPs’ stress levels have often been overlooked in the literature because PHPs’ work is often hidden in the primary healthcare setting in communities [35], especially during the COVID-19 pandemic when the literature has focused on the stress levels of frontline healthcare providers in acute hospital settings. PHPs are often self-reliant, and they do not ask for help especially when they experience high level of stress stemming from the work environment. These preliminary findings provide relevant data for primary healthcare management teams and health planners to develop workplace policies and practices with adequate training/professional development, counselling services and supportive work environments to enhance PHPs’ mental wellbeing and safety. Future research focuses on exploring the psychological distress and social burdens experienced by PHPs during this pandemic is vital to provide an increased level of understanding of their perceptions, stress and concerns.
Increased understanding may also provide new critical information that administrative departments and systems may implement to improve supportive mechanisms for PHPs during future infectious disease outbreaks and future research directions to support mental health needs of PHPs. Cultural diversity should also be considered on the mental-emotional health outcomes among primary healthcare workforce in future research.
In summary, primary healthcare organisations, such as healthcare centres and schools within the Hong Kong community, need to comprehensively strategize ways to establish workplace health policies and provide safe work environments to reduce work-related stress, which may affect the mental wellbeing and work productivity of PHPs. Relevant training and adequate resources for adopting more positive coping mechanisms, such as positive reframing and active coping for dealing with stress resulting from pandemic outbreaks, should be provided in workplace policies and clinical practice guidelines. Cultural diversity must be considered in future mental health nursing research, especially because of the migration of nurses in the global nursing workforce.
Acknowledgement: This project was supported by the Hong Kong School Nurses Association. The authors thank the individuals who participated in this research.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: Conceptualization; methodology: RLL., ACT., SWC., WTC.; formal analysis: WWT., RLL., ACT.; writing, editing, reviewing: RLL., ACT., SWC., WTC., WWT., HYC., CYC.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Levine, O., Gawande, A., Lagomarshino, G., Kelley, E., Pearson, L. et al. (2020). A safer world starts with strong primary healthcare. The BMJ Opinion. [Google Scholar]
2. World Health Organization (WHO) (2022). WHO coronavirus (COVID-19) dashboard. https://covid19.who.int/. [Google Scholar]
3. Government of Hong Kong. Latest situation of coronavirus disease (COVID-19) in Hong Kong 2022. https://chp-dashboard.geodata.gov.hk/covid-19/en.html. [Google Scholar]
4. Lee, R. L. T., West, S., Tang, A. C. Y., Cheng, H. Y., Chong, C. Y. Y. et al. (2021). A qualitative exploration of the experiences of school nurses during COVID-19 pandemic as the frontline primary health care professionals. Nursing Outlook, 69(3), 399–408. DOI 10.1016/j.outlook.2020.12.003. [Google Scholar] [CrossRef]
5. Lu, W., Wang, H., Lin, Y., Li, L. (2020). Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Research, 288, 12936. DOI 10.1016/j.psychres.2020.112936. [Google Scholar] [CrossRef]
6. Odriozola-González, P., Planchuelo-Gómez, Á., Irurtia, M. J., Rodrigo de, L. G. (2022). Psychological symptoms of the outbreak of the COVID-19 confinement in Spain. Journal of Health Psychology, 27(4), 825–835. DOI 10.1177/1359105320967086. [Google Scholar] [CrossRef]
7. Sovold, L. E., Naslund, J. A., Kousoulis, A. A., Saxena, S., Qoronfleh, M. W. et al. (2021). Prioritizing the mental health and well-being of healthcare workers: An urgent global public health priority. Frontier Public Health, 9, 679397. DOI 10.3389/fpubh.2021.679397. [Google Scholar] [CrossRef]
8. Chair, S. K., Chien, W. T., Liu, T., Lam, L., Cross, W. et al. (2021). Psychological distress, fear and coping strategies among Hong Kong people during the COVID-19 pandemic. Current Psychology. DOI 10.1007/s12144-021-02338-7. [Google Scholar] [CrossRef]
9. Vizheh, M., Qorbani, M., Arzaghi, S. M., Muhidin, S., Javanmard, Z. et al. (2020). The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. Journal of Diabetes and Metabolism Disorders, 19(2), 1967–1978. DOI 10.1007/s40200-020-00643-9. [Google Scholar] [CrossRef]
10. Adams, J. G., Walls, R. M. (2020). Supporting the health care workforce during the COVID-19 global epidemic. The Journal of the American Medical Association, 323(15), 1439–1440. DOI 10.1001/jama.2020.3972. [Google Scholar] [CrossRef]
11. Dai, Y., Hu, G., Xiong, H., Qiu, H., Yuan, X. (2020). Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. medRxiv. https://www.medrxiv.org/content/10.1101/2020.03.03.20030874v1. [Google Scholar]
12. Lee, R. L. T. (2011). The role of school nurses in delivering accessible health services for primary and secondary school students in Hong Kong. Journal of Clinical Nursing, 20(19–20), 2968–2977. DOI 10.1111/j.1365-2702.2011.03782.x. [Google Scholar] [CrossRef]
13. Cebello, M., Izquierdo, A., Leal, I. (2020). Loneliness and not living alone is what impacted on the healthcare professional’s mental health during the COVID-19 outbreak in Spain. Health and Social Care in the Community, 30, 968–975. DOI 10.1111/hsc.13260. [Google Scholar] [CrossRef]
14. Piazza, J., Charles, S. T., Sliwinski, M. J. (2013). Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioural Medicine, 45(1), 110–120. DOI 10.1007/s12160-012-9423-0. [Google Scholar] [CrossRef]
15. Lai, J., Ma, S., Wang, Y. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. DOI 10.1001/jamanetworkopen.2020.3976. [Google Scholar] [CrossRef]
16. Babore, A., Lombardi, L., Viceconti, M. L., Pignataro, S., Marino, V. (2020). Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Research, 293, 113366. DOI 10.1016/j.psychres.2020.113366. [Google Scholar] [CrossRef]
17. Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D. et al. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry, 7(4), e15–e16. DOI 10.1016/S2215-0366(20)30078-X. [Google Scholar] [CrossRef]
18. De Kock, J. H., Latham, H. A., Leslie, S. J., Grindle, M., Munoz, S. A. et al. (2021). A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological well-being. BMC Public Health, 21(1), 104. DOI 10.1186/s12889-020-10070-3. [Google Scholar] [CrossRef]
19. Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J. et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. The Journal of the American Medical Association Network Open, 3(3), e203976. DOI 10.1001/jamanetworkopen.2020.3976. [Google Scholar] [CrossRef]
20. Liu, Y., Chen, H., Zhang, N., Wang, X., Fan, Q. et al. (2021). Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. Journal of Affective Disorders, 278, 144–148. DOI 10.1016/j.jad.2020.09.004. [Google Scholar] [CrossRef]
21. Shanafelt, T., Ripp, J., Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. The Journal of the American Medical Association, 323(21), 2133–2134. DOI 10.1001/jama.2020.5893. [Google Scholar] [CrossRef]
22. Friedli, L. (2009). Mental health, resilience and inequalities. In: World Health Organization regional office for Europe. Denmark: Scherfigsvej Copenhagen. https://apps.who.int/iris/handle/10665/107925. [Google Scholar]
23. von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C et al. (2014). Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. International Journal of Surgery, 12(12), 1495–1499. DOI 10.1016/j.ijsu.2014.07.013. [Google Scholar] [CrossRef]
24. Lee, E. H. (2012). Review of the psychometric evidence of the perceived stress scale. Asian Nursing Research, 6(4), 121–127. DOI 10.1016/j.anr.2012.08.004. [Google Scholar] [CrossRef]
25. Carver, C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief. International Journal of Behavioral Medicine, 4(1), 92–100. DOI 10.1207/s15327558ijbm0401_6. [Google Scholar] [CrossRef]
26. Keyes, C. L. M. (2002). The mental health continuum: From languishing to flourishing in life. Journal of Health and Social Behavior, 43, 207–222. DOI 10.2307/3090197. [Google Scholar] [CrossRef]
27. Moran, C., Landero, R., González, M. (2010). COPE-28: A psychometric analysis of the Spanish version of the brief COPE. Universitas Psychologica, 9(2), 543–552. DOI 10.11144/Javeriana.upsy9-2.capv. [Google Scholar] [CrossRef]
28. Lamers, S. M., Westerhof, G. J., Bohlmeijer, E. T., Klooster, P. M., Keyes, C. L. (2011). Evaluating the psychometric properties of the mental health continuum-short form (MHC-SF). Journal of Clinical Psychology, 67(1), 99–110. DOI 10.1002/jclp.20741. [Google Scholar] [CrossRef]
29. Nunnally, J. C., Bernstein, I. J. (1994). Psychometric theory. 3rd editionNew York: McGraw-Hill. [Google Scholar]
30. Kelbiso, L., Belay, A., Woldie, M. (2017). Determinants of quality of work life among nurses working in hawassa town public health facilities, South Ethiopia: A cross-sectional study. Nursing Research and Practice, 5181676. DOI 10.1155/2017/5181676. [Google Scholar] [CrossRef]
31. Koinis, A., Giannou, V., Drantaki, V., Angelaina, S., Stratou, E. et al. (2015). The impact of healthcare workers job environment on their mental-emotional health. coping strategies: The case of a local general hospital. Health Psychology Research, 3(1), 1984. DOI 10.4081/hpr.2015.1984. [Google Scholar] [CrossRef]
32. Ruotsalainen, J. H., Verbeek, J. H., Mariné, A., Serra, C. (2015). Preventing occupational stress in healthcare workers. Cochrane Database Systemic Review, 8(12), CD002892. DOI 10.1002/14651858.CD002892.pub4. [Google Scholar] [CrossRef]
33. Cabarkapa, S., Nadjidai, S. E., Murgier, J., Ng, C. H. (2020). The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain, Behavior, & Immunity-Health, 8, 100144. DOI 10.1016/j.bbih.2020.100144. [Google Scholar] [CrossRef]
34. Tindle, R., Hemi, A., Moustafa, A. A. (2022). Social support, psychological flexibility and coping mediate the association between COVID-19 related stress exposure and psychological distress. Scientific Reports, 12, 8688. DOI 10.1038/s41598-022-12262-w. [Google Scholar] [CrossRef]
35. Lee, R. L. T. (2011). The role of school nurses in delivering accessible health services for primary and secondary school students in Hong Kong. Journal of Clinical Nursing, 20(19–20), 2968–2977. DOI 10.1111/j.1365-2702.2011.03782.x. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools