 Open Access
Open Access
ARTICLE
Can Social Support be Protective against Depressive Symptoms in Adolescents from 24 Low- and Middle-Income Countries?
1
School of Government, Institute of Urban Governance, Shenzhen University, Shenzhen, 518052, China
2
Body-Brain-Mind Laboratory School of Psychology, Shenzhen University, Shenzhen, 518052, China
* Corresponding Author: Tianyou Guo. Email:
International Journal of Mental Health Promotion 2023, 25(3), 375-387. https://doi.org/10.32604/ijmhp.2022.021505
Received 18 January 2022; Accepted 19 April 2022; Issue published 21 February 2023
Abstract
Background: Adolescents are highly vulnerable to depressive symptoms worldwide partially because of limited social supports. However, it still remains largely unknown regarding the associations between social support(s) and depressive symptoms among adolescents living in low- and middle-income countries (LMICs). The aim of this study aimed to explore the associations between different types of social support and depressive symptoms in adolescents from LMICs. Methods: Data were retrieved from the Global School-based Health Survey (GSHS) in which 92,551 adolescents (50.6% females) were included with mean of 15.6 years. Depressive symptoms in the past one month as the dependent variable were measured in combination with social support (was measured by “During the past 30 days, how often were most of the students in your school kind and helpful?”). Multivariable logistic regression and meta-analysis of country-wise estimates were performed to investigate the associations between social support and depressive symptoms, and the heterogeneity of the associations across the countries, respectively. Results: The prevalence of depressive symptoms was 30.9% of adolescents from LMICs. Peer support and parental connectedness were two major factors that were significantly associated with depression symptoms in adolescents. However, the associations of peer support and parental connectedness with depressive symptoms were significant in males and females, respectively. The country-wise analysis indicated that varied inconsistency (small to large) across the associations of peer support and parental connectedness with depressive symptoms in adolescents. Conclusion: Results in this study provides multi-national evidence of the protective roles of social support against depressive symptoms among adolescents. However, the association between social support and depression symptoms may be moderated by sex and types of social support. Although we found that social support may be an important protective factor against depressive symptoms in adolescents from LMICs, specifically designed interventions should be implemented based on sex difference and country difference.Keywords
Depressive symptoms are widely prevalent mental health issues that affect roughly 270 million people across different age groups worldwide [1]. Depressive symptoms are mainly characterized by constant sadness, lacking of interest or pleasure in previously meaningful or enjoyable activities, feelings of tiredness and guilty, reduced activities, insufficiency of energy, and poor concentration [2], which have become the fourth major disease globally [3]. According to the World Health Organization (WHO), depressive symptoms will become the second primary disease by 2030 [1]. Data shows that approximately 20% of population would undergo depressive symptoms at least one time in their lifetime, and the recurrence rate exceeds 80 percent [4]. Nearly two thirds of people with depressive symptoms are more likely have a higher suicidal tendency [5]. Studies found that the incidence of depressive symptoms surged in adolescence [6,7], especially in low-and-middle income countries (LMICs), and the prevalence rates was surprisingly reported as 28% [8]. Depressive symptoms were associated with multiple adverse outcomes, including cognitive impairment, functional impairment, suicide, decreased academic performance, deteriorating social relationships with family and friends and inability to participate in various activities [9,10]. Depressive symptoms in adolescence can be a strong predictor of the risk of depression in adulthood [7,11,12]. According to a meta-analysis including 17 studies depressive symptoms in adolescents increased the risk of depression in adults, and adolescents with depressive symptoms were 2.78 (1.97, 3.93) times more likely to suffer depression during adulthood [12]. Owing to adverse effects of depressive symptoms on physical and mental health in adolescents, preventing and controlling depressive symptoms during adolescence is a key across the world.
Depressive symptoms are influenced by a variety of variables. It has been increasingly accepted that depressive symptoms are a result of deficient social support that refers to the concern and support that people feel from others [13,14]. Social support mainly consisted of peer support and parental support, as well as some other kinds of support from teachers and communities [15,16]. Consistently compelling evidence showed an inverse link between social support and depressive symptoms [17–21]. For example, a study from South Asia showed that social support is a determinant factor of adolescents’ mental health. This study emphasized the importance of parental support and close friends in establishing adolescents’ mental health research and intervention [19]. Gao et al. [22] conducted a questionnaire survey on 521 boarding school students (51.1% female) in 2015 and found that more peer support was associated with fewer depressive symptoms. A meta-analysis compared peer support intervention to traditional behavioral therapy for depressive symptoms by pooling seven studies and the results showed that peer support help reduce the risk of depressive symptoms. Moreover, the levels of parental involvement play an important role in preventing depressive symptoms during adolescence. Cong et al. [23] used data from a large longitudinal research and found that positive parental involvement in early life were related to the reduced risk of depressive in young adults [24]. A cross-sectional study covering 1306 adolescents from China found that high level of parental support was associated with better well-being and lower level of depressive symptoms [25]. Tazvin et al. [26] investigated the relationship between styles of parental involvement and presence of depression, and found that the degree of parental connectedness was correlated with depressive symptoms and anxiety in adolescence. Macalli et al. [27] conducted a longitudinal large-scale study (N = 4,463 students aged between 18 to 24 years) and found that lower levels of parental support were associated with higher suicidal behaviors and major depressive symptoms. Adults with depressive symptoms also described their parents giving more rejection, less connectedness and over-supervision, and feeling less warmth during their adolescence [28].
Previous studies have stressed the importance of various kinds of social support in reducing the risk of depressive symptoms. However, there remains some gaps in the previous research. First, most of the relevant studies were limited to the samples from Western or developed countries and paid insufficient attention to adolescents in LMICs. Differences in economic status among countries could lead to changes in mental health of adolescents, with adolescents from low-income countries more likely to suffer from depressive symptoms [7]. On this regard, focusing on the association between social support and depressive symptoms in adolescents from LMICs is urgently required for better understanding on depression preventions. Second, previous studies did not include enough control variables, which may result in null findings. To better understand the associations between social support and depressive symptoms, addressing this issue, like controlling some significant variables, is needed. Specifically, previous studies omitted the variables of physical activity [29–31] and sedentary behavior [31] that have been considered as essential factors related with depressive symptoms. Finally, to date, most of the previous research on the associations between social support and depression in adolescents was conducted in single country. There are no integrated studies based on multiple countries, limiting our understanding of the relationship between social support and depressive symptoms in a wider range of populations. The role of social support in relieving depressive symptoms may vary because of different countries’ cultures, social circumstance, parenting styles. Consequently, a multinational study would enable researchers to gain insights into the relationship between social support and depressive symptoms, thereby promoting adolescent mental health at a global perspective.
In order to address the mentioned-above gaps in the literature, the study aimed to explore the associations between social support and depressive symptoms covering a total sample size of 92, 551 adolescents in 24 LMICs while taking into account some control variables such as eating behaviors, loneliness, anxiety.
The Global School-based Student Health Survey (GSHS) is a publicly available dataset in which researchers can perform data analysis to determine risk and protective factors of major non-infectious illnesses (details can be found from https://extranet.who.int/ncdsmicrodata/index.php/catalog/GSHS and http://www.cdc.gov/gshs). Likewise, procedures of data collection were clearly described in previous studies [32–34]. Of note, data were weighted for non-response and probability selection. Country survey including the main variables (active school travel and depressive symptoms) were finally selected. Given that the data were collected every 4 or 5 years, the latest dataset was used for data analysis of this study (years: 2003–2012).
Social support (exposure variables)
We used peer support and parental involvement as indicators of social support. Peer support was measured by a single-item question: “During the past 30 days, how often were most of the students in your school kind and helpful?” The answers had five categorizations: (1) always, (2) most of the time, (3) sometimes, (4) rarely, and (5) never. The categorizations of ‘Always’ and ‘most of time’ indicated having peer support, in line with previous studies [35].
Three single-items questions were used to measure parental involvement as follow: (1) ‘During the past 30 days, how often did your parents or guardians check to see if your homework was done?’ reflects parental supervision; (2) ‘During the past 30 days, how often did your parents or guardians understand your problems and worries?’ represents parental connections; (3) ‘During the past 30 days, how often did your parents or guardians really know what you were doing with your free time?’ indicates parental bonding. All the three questions had same responses, including (1) always, most of the time, sometimes, rarely, and never. For each question response, ‘Always’ and ‘most of time’ indicated having parental involvement(s), in accordance with previous studies [35].
Depression symptoms (outcome variable)
Likewise, a single-item question was used to measure depressive symptoms: “During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing your usual activities?” Participants were provided with Yes (reflecting depressive symptoms) and No (has no depressive symptoms), which is in line with previous studies [6,32].
Control variables
Based on previous studies, some factors associated with social support and depressive symptoms, such as eating behavior [36], loneliness, anxiety [37], physical activity [38,39], sedentary behavior [6], which were considered as control variables in the statistical analysis. We also controlled for demographic variables such as socioeconomic status, sex, age. For socioeconomic status, a single-item question was used to measure food security during the past one month: How often did you go hungry because there was not enough food in your home?” [6,40,41]. The answers consisted of always, most of the time, sometimes, rarely, and never.
All the statistical analyses were conducted with STATA 16.1 (Stata Corp, College Station, Texas). The prevalence of social support and depressive symptoms by gender and country was also calculated. Multivariable logistic regression analysis (SPSS) was carried out to determine the association between social support and depressive symptoms (overall, by sex and country). The variables of social support and depressive symptoms were binary. The regression was adjusted for sex, age, eating behavior, loneliness, anxiety, sedentary behavior, physical activity and food insecurity, as well as country, with the exception of the sex-stratified and country-wise analyses which were not adjusted for sex and country, respectively.
The value of Higgin’s I2 statistic based on country-wise estimates (R) was used to measure the level of between-country heterogeneity: (1) <40% = negligible; (2) 40%–60% = moderate heterogeneity). A pooled estimate was computed with the random-effects model. All variables were included in the regression analyses as categorical variables with the exception of age and physical activity (both as continuous variables). Less than 4.5% of the data were missing for all the variables used in the analysis. Complete case analysis was performed. Taylor linearization methods were used in all analyses to explain the sample weighting and complex study design. Results from the logistic regression analyses are presented as odds ratios with 95% confidence intervals (CIs), with the statistical significance level of p < 0.05.
A total of 92,551 adolescents aged 11–16 years old from 24 countries and 5 regions were enrolled in this study. The mean age was 15.6 years (standard deviation: 1.3) and girls accounted for 50.6%. The overall prevalence of peer support (reporting ‘always’ or ‘most of time’) was 40.5%. The prevalence of peer support varied across the included countries (range 11.5% [Uruguay] to 65.1% [Sri Lanka]). The overall prevalence of parental supervision, parental connectedness and parental bonding were 38.9% (country differences: from 21.0% [Uruguay] to 63.6% [Sri Lanka]), 38.8% (country differences: from 7.9% [Uruguay] to 62.1% [India]), 46.2% (country differences: from 30.2% [Philippines] to 69.0% [Myanmar]), respectively. The overall prevalence of depressive symptom was 30.9% (country differences: from 11.6% [Uruguay] to 53.3% [Zambia]). More details can be seen in Table 1.
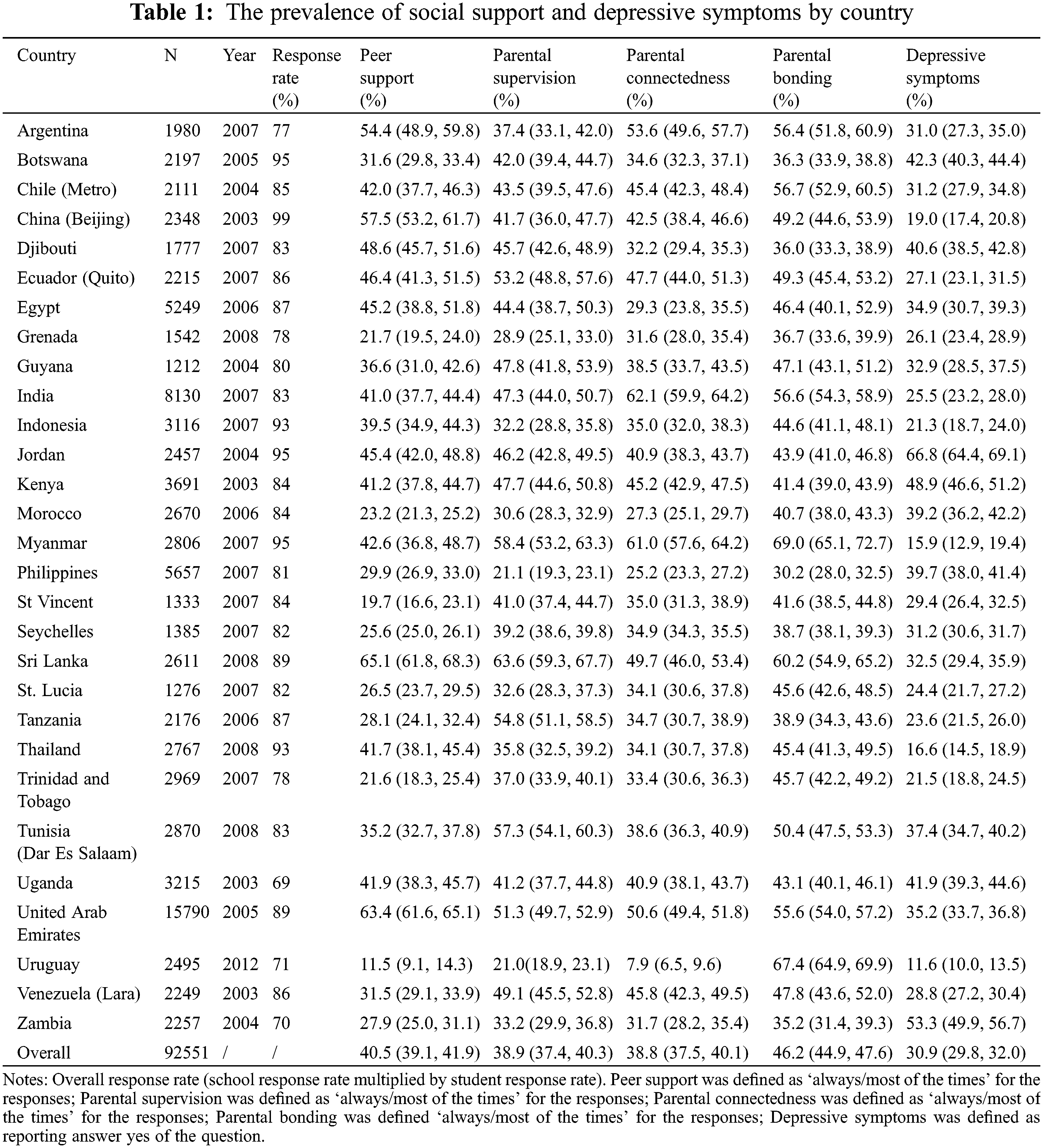
The prevalence of depressive symptoms by different levels of various kinds of social support is shown in Figs. 1–4. Overall, the prevalence of depressive symptoms by parental supervision, parental connectedness and parental bonding decreased (regardless of sex). However, the prevalence of depression symptoms by peer support did not show such a generally downward trend. There was a turning point of the prevalence of depressive symptoms between peer support with most of time and that with always (see Figs. 1–4).
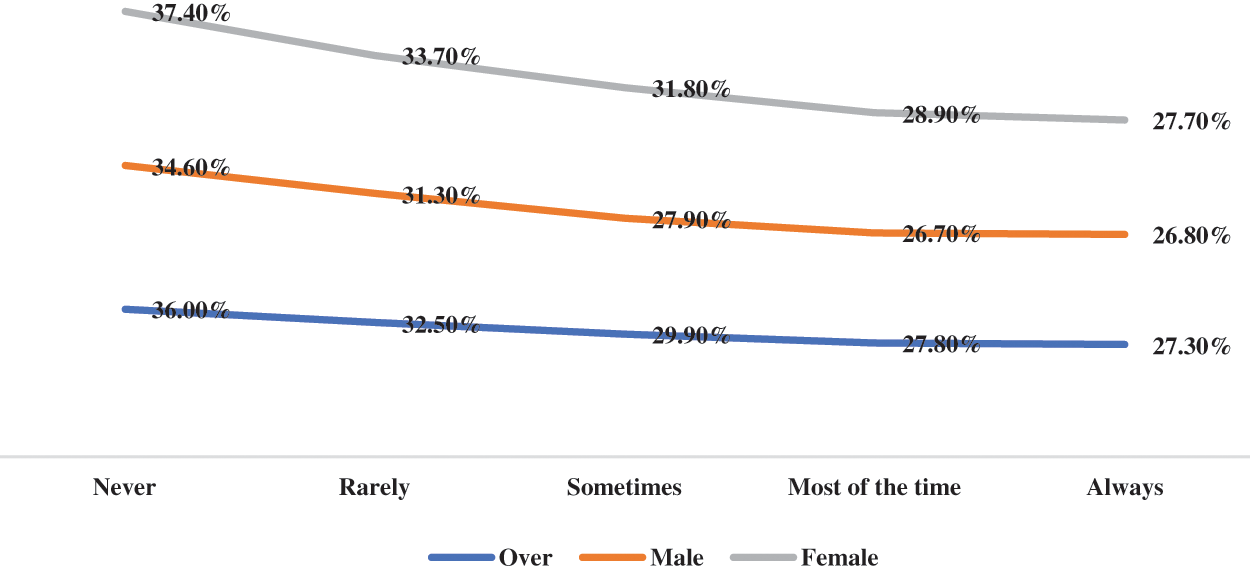
Figure 1: The prevalence of depressive symptoms by parental supervision
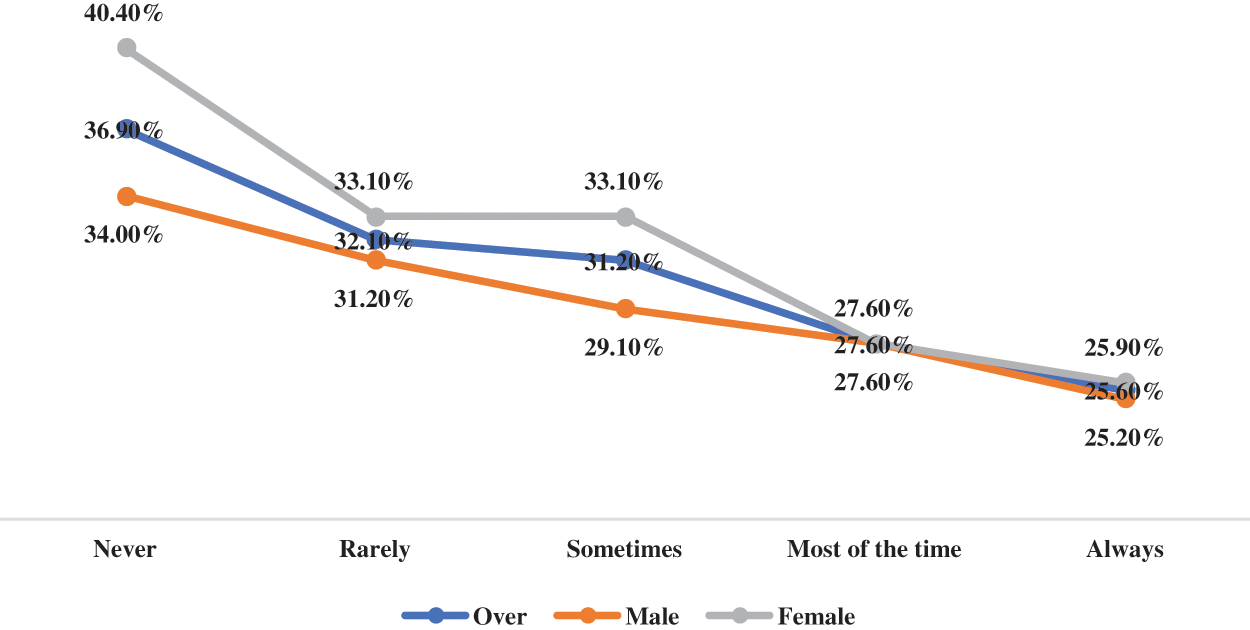
Figure 2: The prevalence of depressive symptoms by parents understand
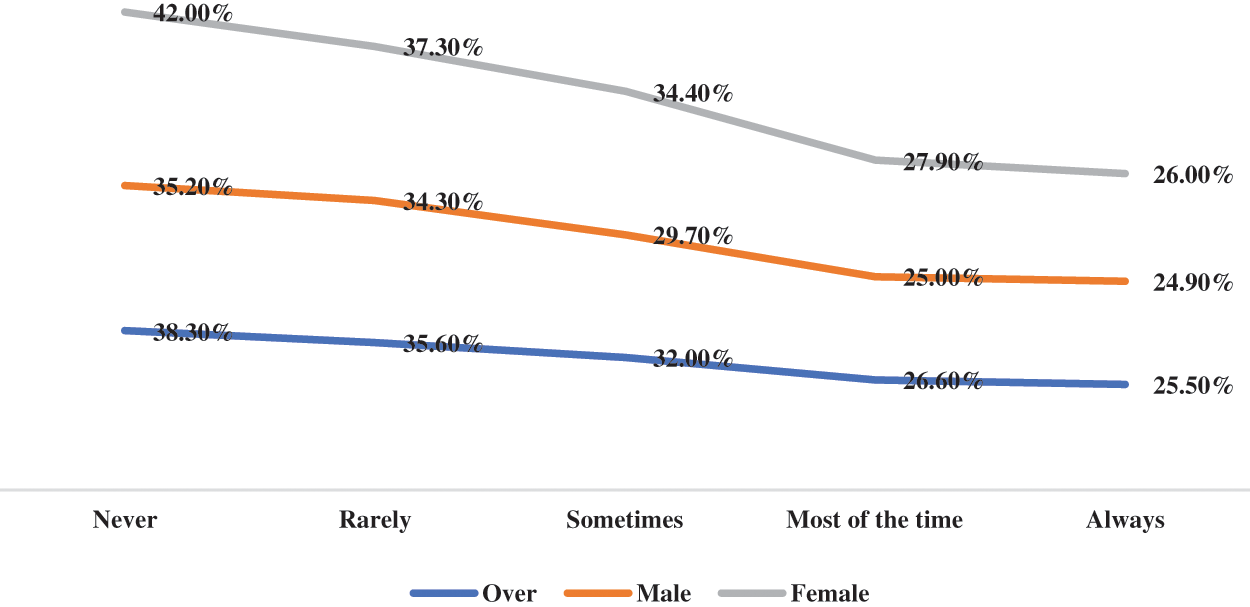
Figure 3: The prevalence of depressive symptoms by parent know
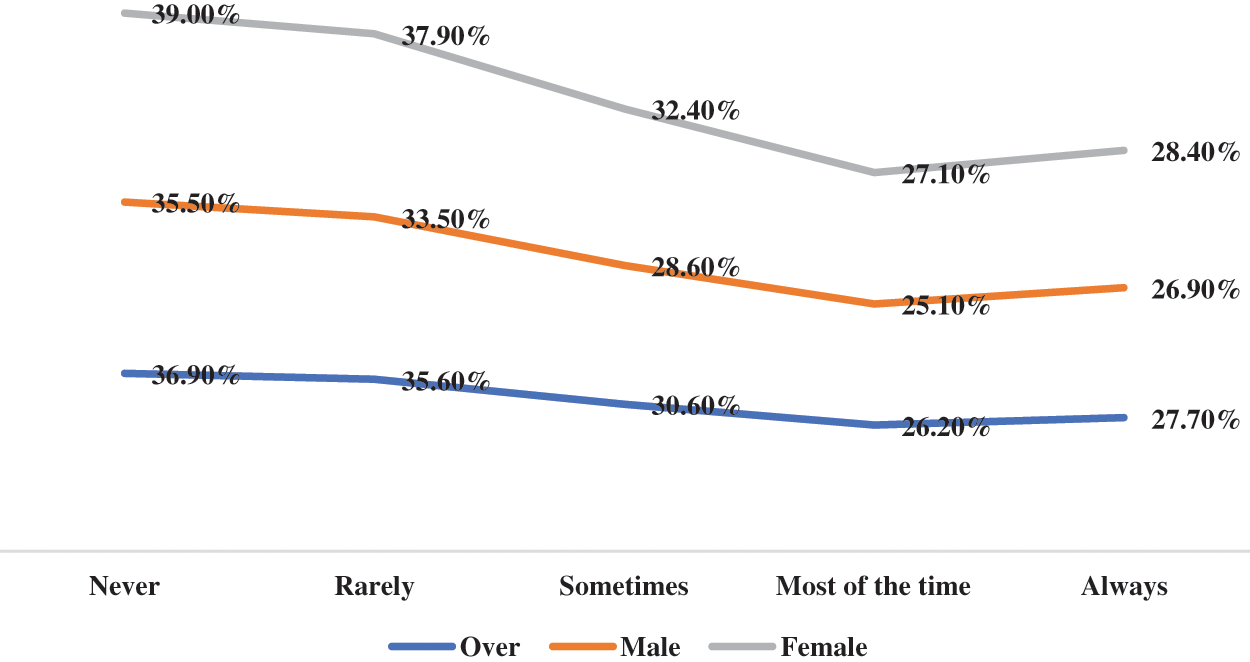
Figure 4: The prevalence of depressive symptoms by peer support
Multivariate logistic regression results show the associations between various kinds of social support and depressive symptoms (Table 2). Specifically, compared with adolescent who reported no peer support, having more peer support was less likely to report depressive symptoms (OR for sometimes = 0.85, 95% CI: 0.78–0.94; OR for most of the time = 0.76, 95% CI: 0.68–0.86; OR for always = 0.86, 95% CI: 0.78–0.96). The similar trend was also observed in male adolescents instead of their counterparts. Regarding parental supervision, there were no significant trend in association between more parental supervisions and lower odds for depressive symptoms regardless of sex. Relative to adolescents who report no parental connectedness, those who report rarely, sometimes, most of the time and always had lower likelihood for depressive symptoms (OR for rarely = 0.89, 95% CI: 0.79–0.98; OR for sometimes = 0.88, 95% CI: 0.81–0.96; OR for most of the time = 0.88, 95% CI: 0.79–0.98; OR for always = 0.87, 95% CI: 0.79–0.97). This significant trend was also found in female adolescents rather than males. For parental bonding, except for male adolescents, those who report ‘always’ had lower odds for depressive symptoms (OR for overall sample = 0.82, 95% CI: 0.73–0.92; OR for female adolescents = 0.84, 95% CI: 0.79, 95% CI: 0.68–0.91).
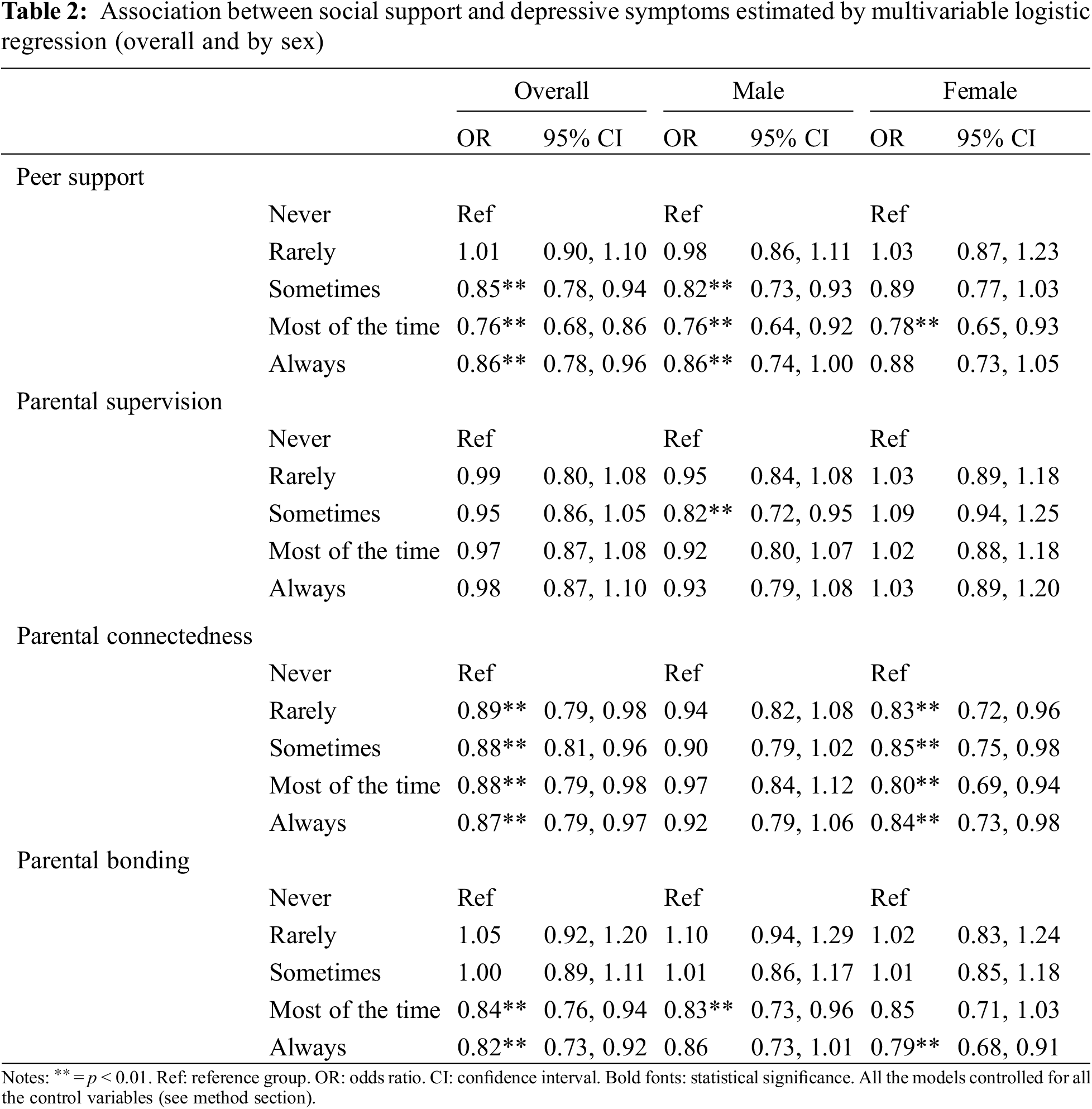
Table 3 shows country-wise and pooled estimates of the associations between peer support and depressive symptoms in adolescents (overall and by sex) examined separately for different kinds of social support (except for parental supervision because of non-significant from regression). Compared to adolescents who reported no peer support, high levels of peer support (OR = 0.86; 95% CI = 0.82–0.91) was associated with a lower risk of depressive symptoms. These results were found among males and females. For overall (I2 = 52%, p < 0.01) and male (I2 = 38%, p < 0.01), a low level of between-country heterogeneity was observed, but the level was high for female (I2 = 70%, p < 0.01). Similar to parental bonding, parental connectedness for high level (OR = 0.88, 95% CI = 0.84–0.92, p < 0.01), compared to no parental connectedness, was associated with a lower risk of depressive symptoms. A low level of between-country heterogeneity was observed for overall (I2 = 34%, p < 0.01), a moderate level of heterogeneity among male (I2 = 57%, p < 0.01) and female (I2 = 59%, p < 0.01). Parental bonding of high level (OR = 0.81, 95% CI = 0.76–0.86, p < 0.01), compared to no parents bonding, was associated with a lower risk of depression symptoms. A low level of between-country heterogeneity was found among male (I2 = 33%), but not among the overall (I2 = 77%) and female (I2 = 80%, p < 0.01).
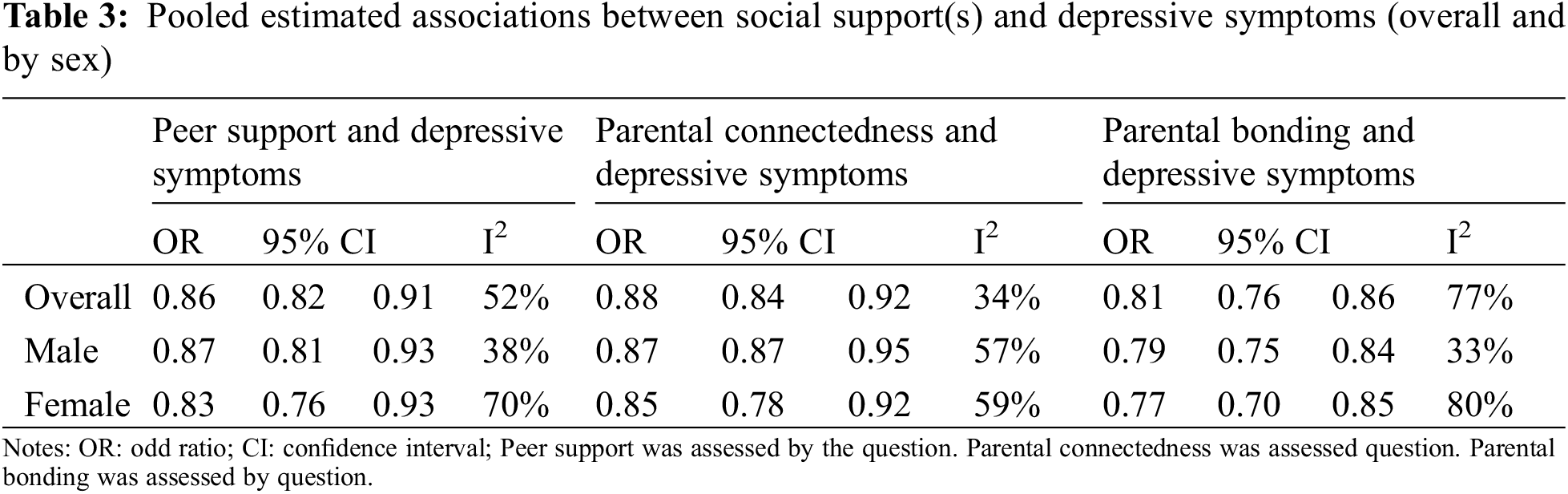
To the authors’ knowledge, the current study is the largest epidemiological study investigating the associations between social support(s) and depressive symptoms among 92, 551 adolescents aged 11–16 years from 24 LMICs covered by 5 WHO regions. After adjusting sex, age, food insecurity, eating behavior, loneliness, anxiety, physical activity, sedentary behavior, this cross-sectional study found that higher levels of peer support were negatively associated with depressive symptoms, especially in male adolescents. There was no significant association between parental supervision and depressive symptoms. higher levels of parental connectedness were negatively associated with depressive symptoms, particularly in female adolescents. Parental bonding was negatively and significantly associated with depressive symptoms. As for the associations between social support and depressive symptoms, differentiated country-wise relations varied by sex and social supports was also observed. The current study has essential and practical meaningfulness in depression prevention for adolescents from LMICs, through which stresses the importance of social support.
In the current study, peer support as a correlate of depressive symptoms in adolescents from LMICs was unfavorably associated with depressive symptoms. Put another word, sufficient peer supports would be a beneficial approach to lower the odds for depressive symptoms in adolescents from LMICs. During adolescence, peers can provide emotional and other kinds of supports, like oral encouragements and comfort, which in turn helps reduce adolescents’ negative moods including depressive symptoms [42]. Our study finding on the association between peer support and depressive symptoms is consistent with many studies [18,19,22,43]. Recently, a meta-analysis including trials using peer support as depressive symptoms interventional strategies has suggested that peer support interventions help reduce depressive symptoms [44]. The results of the present study again stress the importance of peer support in preventing or reducing depressive symptoms, especially in LMICs, because those who are living LMICs are more likely to suffer to depressive symptoms [45,46]. Of note, it should be mentioned that there was a somewhat noticeable sex-differentiation in the associations between peer support and depressive symptoms. Possible reasons may concern the sex-specific trajectories of depressive symptoms during adolescence and females’ reactions to peer support [42–44]. However, more studies are encouraged to explore the sex-differentiation in the associations between peer support and depressive symptoms in adolescents. As for the pooled estimated associations across countries, the study found that country-differentiation in the association between peer support and depressive symptoms varied greatly sex. Specifically, there was a small difference in males but a large difference in females across countries. This implies that the association between peer support and depressive symptoms in females should be considered cautiously based on different countries’ contextual factors.
Parental connectedness was also negatively associated with depressive symptoms in our multiple-nation study, which implies that stronger parental connectedness may result in decreased depressive symptoms in adolescents from LMICs. This research finding is consistent with many previously published research [47,48]. However, the significant association between parental connectedness and depressive symptoms was not observed in boys. This research finding, to our knowledge, is not supported by other previous research because of paucity of data based on adolescents from LIMCs. Possible reasons for this research finding may include that boys were more independent from parents during their adolescents compared with their counterparts. However, for girls, they need more parental supports from multidimensional aspects, which suggests that parental connectedness would play an important role in reduce depressive symptoms [47,49]. Noticeably, the current study found that moderate inconsistency on the association between parental connectedness and depressive symptoms in adolescents regardless of sex. This research finding implies that it is necessary to focus national and contextual differences when designing and implementing relevant interventions aiming at reducing depressive symptoms through peer support and parental connectedness.
Practical implications
Based on the mentioned-above research findings, the current study, building on the evidence from multiple nations, stresses the potential roles of social support on reducing depressive symptoms, especially by peer support and parental connectedness. Of note, it should be mentioned that when designing interventions or policies aiming for depression prevention, sex difference must be taken into consideration. For male adolescents, fulfilling the roles of peer support might be a more effective approach; while for female adolescents, making full of use of parental connectedness could be a better way. Another implication involves country difference, which implies that using peer support and parental connectedness for depression prevention in adolescents should be based on country specific culture, social norms and other imperative considerations. So, the effectiveness of peer support and parental connectedness on depression prevention in adolescents must be varied across the different countries, and the specific adaptations of intervention in different countries are encouraged strongly.
Study strengths and limitations
Although the study includes a large number of sample sizes from over 20 countries, and took into account multiple confounding factors (e.g., eating behavior, sedentary behavior, physical activity), it should be explained in light of some limitations. First, since the GSHS study is a cross-sectional data base, this study could not predict causality between social support and depressive symptoms. Longitudinal studies are strongly recommended to better understand the observed associations for causality inferences. Second, self-reported measures were used in this study, which are prone to result in recall bias and measurement errors owing to social desirability or other personal considerations. In addition, the current data included only adolescents in schools, and information from adolescents who were unable to attend school or who had dropped out was not included. Finally, this study did not find reasons for the differences in the relationship between social support and depression across countries, it may be a direction of future research.
The current offer evidence that social supports could be regard as correlate of depressive symptoms in adolescents based on multiple LMICs across the world. Of note, some specific types of social support, like peer support and parental connectedness, were two mainly significant correlates of depressive symptoms, which may be essential to depression prevention and interventions of adolescents from LMICs. Future longitudinal research is required to further explore the causal association between social support and depressive symptoms and outline potential mechanisms as well as exploring culturally specific variations. The findings of our study can also help to inform depression prevention but should be operationalized with cautions in different LMICs owing to the varied and noticeable country-wise inconsistency.
Funding Statement: This project was supported by National Natural Science Foundation of China (31871115).
Author Contributions: HW: Manuscript writing-original draft preparation; TG: Supervision, methodology, analysis, validation; ZY: editing; All authors: review and editing.
Availability of Data and Materials: The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Approval: The studies involving human participants were reviewed and approved by Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. World Health Organization (2020). Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. World Health Organization. https://apps.who.int/iris/handle/10665/331490. [Google Scholar]
2. Wang, P. S. (2007). Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. The Lancet, 370, 841–850. DOI 10.1016/S0140-6736(07)61414-7. [Google Scholar] [CrossRef]
3. Smith, K. (2014). Mental health: A world of depression. Nature, 515, 180–181. DOI 10.1038/515180a. [Google Scholar] [CrossRef]
4. Gotlib, I. H., Hamilton, J. P. (2008). Neuroimaging and depression: Current status and unresolved issues. Current Directions in Psychological Science, 17, 159–163. DOI 10.1111/j.1467-8721.2008.00567.x. [Google Scholar] [CrossRef]
5. Ledford, H. (2014). Medical research: If depression were cancer. Nature, 515, 182–184. DOI 10.1038/515182a. [Google Scholar] [CrossRef]
6. Vancampfort, D. (2018). Sedentary behavior and depressive symptoms among 67,077 adolescents aged 12–15 years from 30 low- and middle-income countries. International Journal of Behavioral Nutrition and Physical Activity, 15(1), 73. DOI 10.1186/s12966-018-0708-y. [Google Scholar] [CrossRef]
7. Costello, E. J., Egger, H., Angold, A. (2005). 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. Journal of the American Academy of Child and Adolescent Psychiatry, 44(10), 972–986. DOI 10.1097/01.chi.0000172552.41596.6f. [Google Scholar] [CrossRef]
8. Yatham, S. (2018). Depression, anxiety, and post-traumatic stress disorder among youth in low and middle income countries: A review of prevalence and treatment interventions. Asian Journal of Psychiatry, 38, 78–91. DOI 10.1016/j.ajp.2017.10.029. [Google Scholar] [CrossRef]
9. Keenan-Miller, D., Hammen, C. L., Brennan, P. A. (2007). Health outcomes related to early adolescent depression. Journal of Adolescent Health, 41(3), 256–262. DOI 10.1016/j.jadohealth.2007.03.015. [Google Scholar] [CrossRef]
10. Lepine, J. P., Briley, M. (2011). The increasing burden of depression. Neuropsychiatric Disease and Treatment, 7(Suppl 1), 3–7. [Google Scholar]
11. Johnson, D. (2018). Adult mental health outcomes of adolescent depression: A systematic review. Depression and Anxiety, 35(8), 700–716. DOI 10.1002/da.22777. [Google Scholar] [CrossRef]
12. Clayborne, Z. M., Varin, M., Colman, I. (2019). Systematic review and meta-analysis: Adolescent depression and long-term psychosocial outcomes. Journal of the American Academy of Child & Adolescent Psychiatry, 58, 72–79. DOI 10.1016/j.jaac.2018.07.896. [Google Scholar] [CrossRef]
13. George, L. K. (1989). Social support and the outcome of major depression. The British Journal of Psychiatry, 154, 478–485. DOI 10.1192/bjp.154.4.478. [Google Scholar] [CrossRef]
14. Stice, E., Ragan, J., Randall, P. (2004). Prospective relations between social support and depression: differential direction of effects for parent and peer support? Journal of Abnormal Psychology, 113(1), 155–159. DOI 10.1037/0021-843X.113.1.155. [Google Scholar] [CrossRef]
15. Sarason, I. G. (1983). Assessing social support: The social support questionnaire. Journal of Personality & Social Psychology, 44(1), 127–139. DOI 10.1037/0022-3514.44.1.127. [Google Scholar] [CrossRef]
16. Cohen, S., Gottlieb, B. H., Underwood, L. G. (2000). Social relationships and health. In: Cohen, S., Underwood, L. G., Gottlieb, B. H. (Eds.Social support measurement and intervention: A guide for health and social scientists, pp. 3–25. Oxford University Press, USA. [Google Scholar]
17. Cheng, Y., Li, X., Lou, C., Sonenstein, F. L., Kalamar, A. et al. (2014). The association between social support and mental health among vulnerable adolescents in five cities: Findings from the study of the well-being of adolescents in vulnerable environments. Journal of Adolescent Health, 55(6 Suppl), S31–S38. DOI 10.1016/j.jadohealth.2014.08.020. [Google Scholar] [CrossRef]
18. Adamczyk, K., Segrin, C. (2015). Perceived social support and mental health among single vs. partnered Polish young adults. Current Psychology, 34(1), 82–96. [Google Scholar]
19. Murshid, N. J. C., Shaanta, Y. S. (2017). Review, parents, friends, and depression: A multi-country study of adolescents in South Asia. Children and Youth Services Review, 79, 160–165. DOI 10.1016/j.childyouth.2017.06.018. [Google Scholar] [CrossRef]
20. Alsubaie, M. M., Stain, H. J., Webster, L. A. D., Wadman, R. (2019). The role of sources of social support on depression and quality of life for university students. International Journal of Adolescence and Youth, 24(4), 484–496. DOI 10.1080/02673843.2019.1568887. [Google Scholar] [CrossRef]
21. Osborn, T. L., Venturo-Conerly, K. E., Wasil, A. R., Schleider, J. L., Weisz, J. R. (2019). Depression and anxiety symptoms, social support, and demographic factors among Kenyan high school students. Journal of Child and Family Studies, 29(5), 1432–1443. DOI 10.1007/s10826-019-01646-8. [Google Scholar] [CrossRef]
22. Gao, J. L., Wang, L. H., Yin, X. Q., Hsieh, H. F., Rost, D. H. et al. (2019). The promotive effects of peer support and active coping in relation to negative life events and depression in Chinese adolescents at boarding schools. Current Psychology, 40, 2251–2260. [Google Scholar]
23. Pfeiffer, P. N., Heisler, M., Piette, J. D., Rogers, M. A., Valenstein, M. (2011). Efficacy of peer support interventions for depression: A meta-analysis. General Hospital Psychiatry, 33(1), 29–36. DOI 10.1016/j.genhosppsych.2010.10.002. [Google Scholar] [CrossRef]
24. Cong, X., Hosler, A. S., Tracy, M., Appleton, A. A. (2020). The relationship between parental involvement in childhood and depression in early adulthood. Journal of Affective Disorders, 273(1), 173–182. DOI 10.1016/j.jad.2020.03.108. [Google Scholar] [CrossRef]
25. Wang, Z., Kouvonen, A., Satka, M. (2018). Parental social support and adolescent well-being: A cross-sectional study in China. Child Indicators Research, 12, 299–317. [Google Scholar]
26. Tazvin, I., Mahmood, Z. (2009). Relationship between perceived parenting styles and levels of depression, anxiety, and frustration tolerance in female students. Pakistan Journal of Psychological Research, 24, 63–78. [Google Scholar]
27. Macalli, M., Cote, S., Tzourio, C. (2020). Perceived parental support in childhood and adolescence as a tool for mental health screening in students: A longitudinal study in the i-Share cohort. Journal of Affective Disorders, 266(1), 512–519. DOI 10.1016/j.jad.2020.02.009. [Google Scholar] [CrossRef]
28. Adubale, A. A. (2017). Parenting styles as predicators of anxiety and depression of in-school adolescents in Nigeria. Africa Education Review, 14(3–4), 111–121. DOI 10.1080/18146627.2016.1264864. [Google Scholar] [CrossRef]
29. Martinsen, E. W. (2009). Physical activity in the prevention and treatment of anxiety and depression. Nordic Journal of Psychiatry, 62(Suppl 47), 25–29. [Google Scholar]
30. Mckercher, C. M., Schmidt, M. D., Sanderson, K. A., Patton, G. C., Dwyer, T. et al. (2009). Physical activity and depression in young adults. American Journal of Preventive Medicine, 36(2), 161–164. DOI 10.1016/j.amepre.2008.09.036. [Google Scholar] [CrossRef]
31. Schuch, F., Vancampfort, D., Firth, J., Rosenbaum, S., Ward, P. (2017). Physical activity and sedentary behavior in people with major depressive disorder: A systematic review and meta-analysis. Journal of Affective Disorders, 225, 79. DOI 10.1016/j.jad.2017.08.001. [Google Scholar] [CrossRef]
32. Chen, S. T., Guo, T., Yu, Q., Stubbs, B., Clark, C. et al. (2021). Active school travel is associated with fewer suicide attempts among adolescents from low-and middle-income countries. International Journal of Clinical and Health Psychology, 21(1), 100202. [Google Scholar]
33. Liu, S. A., Chen, S.T., Stubbs, B., Yu, Q., Griffiths, M. et al. (2020). Association between active school travel and depressive symptoms among 51,702 adolescents in 26 low-and middle-income countries. International Journal of Mental Health Promotion, 23(2), 141–153. DOI 10.32604/IJMHP.2021.016274. [Google Scholar] [CrossRef]
34. Zhang, Y., Chen, S., Wang, C., Zhang, X., Zou, L. (2021). Does more sedentary time associate with higher risks for sleep disorder among adolescents? A pooled analysis. Frontiers in Pediatrics, 9, 603177. DOI 10.3389/fped.2021.603177. [Google Scholar] [CrossRef]
35. Khan, S. R., Uddin, R., Mandic, S., Khan, A. (2020). Parental and peer support are associated with physical activity in adolescents: Evidence from 74 countries. International Journal of Environmental Research and Public Health, 17(12), 4435. DOI 10.3390/ijerph17124435. [Google Scholar] [CrossRef]
36. Lopresti, A. L., Hood, S. D., Drummond, P. D. (2013). A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. Journal of Affective Disorders, 148(1), 12–27. DOI 10.1016/j.jad.2013.01.014. [Google Scholar] [CrossRef]
37. Fleming, L. C., Jacobsen, K. H. (2009). Bullying and symptoms of depression in chilean middle school students. Journal of School Health, 79(3), 130–137. DOI 10.1111/j.1746-1561.2008.0397.x. [Google Scholar] [CrossRef]
38. McKercher, C. M., Schmidt, M. D., Sanderson, K. A., Patton, G. C., Dwyer, T. (2009). Physical activity and depression in young adults. American Journal of Preventive Medicine, 36(2), 161–164. DOI 10.1016/j.amepre.2008.09.036. [Google Scholar] [CrossRef]
39. McKenzie, L. E., Polur, R. N., Wesley, C., Allen, J. D., McKeown, R. E. (2013). Social contacts and depression in middle and advanced adulthood: Findings from a US national survey, 2005–2008. International Journal of Social Psychiatry, 59(7), 627–635. DOI 10.1177/0020764012463302. [Google Scholar] [CrossRef]
40. Koyanagi, A., Oh, H., Carvalho, A. F., Smith, L., Haro, J. M. (2019). Bullying victimization and suicide attempt among adolescents aged 12–15 years from 48 countries. Journal of the American Academy of Child and Adolescent Psychiatry, 58(9), 907–918.e4. DOI 10.1016/j.jaac.2018.10.018. [Google Scholar] [CrossRef]
41. Koyanagi, A., Stubbs, B., Oh, H., Veronese, N., Smith, L. (2019). Food insecurity (hunger) and suicide attempts among 179,771 adolescents attending school from 9 high-income, 31 middle-income, and 4 low-income countries: A cross-sectional study. Journal of Affective Disorders, 248, 91–98. DOI 10.1016/j.jad.2019.01.033. [Google Scholar] [CrossRef]
42. Shore, L., Toumbourou, J. W., Lewis, A. J., Kremer, P. (2018). Longitudinal trajectories of child and adolescent depressive symptoms and their predictors–A systematic review and meta-analysis. Child and Adolescent Mental Health, 23(2), 107–120. DOI 10.1111/camh.12220. [Google Scholar] [CrossRef]
43. Vaughan, C. A., Foshee, V. A., Ennett, S. T. (2010). Protective effects of maternal and peer support on depressive symptoms during adolescence. Journal of Abnormal Child Psychology, 38(2), 261–272. DOI 10.1007/s10802-009-9362-9. [Google Scholar] [CrossRef]
44. Pfeiffer, P. N., Heisler, M., Piette, J. D., Rogers, M. A. M., Valenstein, M. (2011). Efficacy of peer support interventions for depression: A meta-analysis. General Hospital Psychiatry, 33(1), 29–36. DOI 10.1016/j.genhosppsych.2010.10.002. [Google Scholar] [CrossRef]
45. Jeon, G. S., Ha, Y., Choi, E. (2013). Effects of objective and subjective socioeconomic status on self-rated health, depressive symptoms, and suicidal ideation in adolescents. Child Indicators Research, 6(3), 479–492. DOI 10.1007/s12187-013-9180-z. [Google Scholar] [CrossRef]
46. Duinhof, E. L., Smid, S. C., Vollebergh, W. A. M., Stevens, G. W. J. M. (2020). Immigration background and adolescent mental health problems: The role of family affluence, adolescent educational level and gender. Social Psychiatry and Psychiatric Epidemiology, 55(4), 435–445. DOI 10.1007/s00127-019-01821-8. [Google Scholar] [CrossRef]
47. Boutelle, K., Eisenberg, M. E., Gregory, M. L., Neumark-Sztainer, D. (2009). The reciprocal relationship between parent-child connectedness and adolescent emotional functioning over 5 years. Journal of Psychosomatic Research, 66(4), 309–316. DOI 10.1016/j.jpsychores.2008.10.019. [Google Scholar] [CrossRef]
48. Ackard, D. M., Neumark-Sztainer, D., Story, M., Perry, C. (2006). Parent-child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine, 30(1), 59–66. DOI 10.1016/j.amepre.2005.09.013. [Google Scholar] [CrossRef]
49. Matlin, S. L., Molock, S. D., Tebes, J. K. (2011). Suicidality and depression among african american adolescents: The role of family and peer support and community connectedness. American Journal of Orthopsychiatry, 81(1), 108–117. DOI 10.1111/j.1939-0025.2010.01078.x. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools