 Open Access
Open Access
ARTICLE
Moderating Mechanism in the Relationship between Social Isolation and Mental Health among College Students during High-Risk Period of COVID-19 Transmission in Hubei, China
1 International College, Krirk University, Bangkok, 10220, Thailand
2 Chinese International College, Dhurakij Pundit University, Bangkok, 10210, Thailand
3 Wei Gong Memorial Hospital, Toufen City, Miaoli County, 351011, Taiwan
* Corresponding Authors: Chia Feng Tu. Email: ,
International Journal of Mental Health Promotion 2023, 25(2), 193-206. https://doi.org/10.32604/ijmhp.2022.022130
Received 22 February 2022; Accepted 29 August 2022; Issue published 02 February 2023
Abstract
This study explored the effect of perceived social isolation on the mental health of college students during the high-risk period of COVID-19 transmission in Hubei, China and the role of social support from online friends in alleviating this effect. The questionnaire responses of 213 college students from four universities in Hubei were included. Measurement and structural models were constructed using structural equation modeling. The findings revealed that perceived social isolation while under home quarantine was a negative predictor of the mental health of college students in Hubei. Low social support from online friends may lead to a relatively strong relationship between perceived social isolation and mental health in these college students, whereas high social support from online friends may lead to a relatively weak relationship between perceived social isolation and mental health.Keywords
Each individual has a crucial role in preventing coronavirus disease 2019 (COVID-19); one of the tools used to prevent the transmission of COVID-19 has been quarantines, particularly during periods when the risk of transmission of the disease is high [1]. After COVID-19 rapidly broke out in Wuhan City, Hubei Province, China on January 23, 2020, the city was blockaded [2]. From January 24, 2020, to March 23, 2020, a strict home quarantine policy was implemented across Hubei Province [3,4]. An investigation into the effect of the prolonged home quarantine on the psychological condition of the residents of Hubei, who could not venture freely outside of their homes for a period of more than 2 months, was warranted. The residents felt social isolation because they had lost face-to-face social contact with other people [3–5].
In general, people are adapted to receiving stimuli from the environment and interacting with others; therefore, the social isolation perception of prolonged (i.e., 24 h or more) home quarantine with a lack of environmental stimuli and social interaction may lead to feelings of stress, anxiety, and anger [5–8]. This claim, namely that the perceived social isolation of home quarantine is associated with declining mental health, has been supported by other studies and has been shown to be especially true in the case of college students [9,10].
While under home quarantine, college students in Hubei received social support from parents and online friends, and this may have reduced the negative effect of their social isolation perception [5,6,8,11–13]. Normally, an individual adapts his or her attitude and behavior to the external environment [14]. The amount of social support received by an individual affects his or her stress level and mental health, and according to stress buffering theory, affects the relationship between perceived social isolation and mental health [9,11,15,16].
The current study discussed the effect of perceived social isolation of home quarantine on the mental health of college students in Hubei and the role of social support from parents and online friends in alleviating this effect. The study provided recommendations to Chinese university staff and counselors on how to support and preserve the mental health of students who were experiencing social isolation.
1.1 Current Research and Research Hypothesis
Social isolation has been defined as perceived inadequate quality and quantity of social contact with others; having inadequate social relationships influences mental health outcomes [17]. Perceived social isolation can result from living in a confined environment for a prolonged period of time without sufficient social contact and environmental stimuli [5,18], resulting in a series of poor mental health symptoms, such as considerable anxiety and stress [5,6,18]. Moreover, perceived social isolation can negatively affect an individual’s psychological functioning [19], giving rise to a potential for severe mental illness and an increased risk for suicide [17,20]. In particular, the level of perceived social isolation while under home quarantine during the COVID-19 pandemic was a predictor of poor mental health outcomes in college students who did not have pre-existing mental health problems [9,10]. Accordingly, this study proposed the following research hypothesis:
H1: Perceived social isolation negatively predicts mental health among college students in Hubei.
To cope with mental health problems while under home quarantine during the COVID-19 pandemic, college students obtained social support from family and online friends [11–13]. Whether from parents or online friends, social support can be psychological or material. Psychological support mainly allows individuals to experience a sense of care and belonging, whereas material support allows individuals to solve problems and obtain financial assistance [21]. A large amount of social support with stress-buffering effects can help prevent young adults from developing poor mental health [12,22,23]. For instance, social support from parents might help college students avoid developing poor mental health during the COVID-19 pandemic [12]; social support from online friends might help individuals avoid the negative effect of social isolation perception on their mental health while under quarantine [13]. Therefore, this study proposed the following research hypotheses:
H2a: Social support from parents positively predicts mental health among college students in Hubei.
H2b: Social support from online friends positively predicts mental health among college students in Hubei.
The differences in social support levels are caused by a moderating mechanism [15,16], which is emphasized under stress buffering theory, revealing that the negative effect of stress is mitigated by involving problem-solving strategies in social support systems and thereby reducing stress reactions to protect mental health [15]. However, the level of social support appears to have strong effects on the relationship of social isolation with mental health [16]; for instance, strong social support results in a weaker stress–mental health relationship, whereas weak social support results in a stronger stress–mental health relationship [15,16]. In this study, college students who were under home quarantine obtained social support mainly from parents and online friends [11,24]. Receiving a large amount of social support while under home quarantine in a confined environment that otherwise lacks opportunities for social contact enriches environmental stimuli and provides a stress buffer [5,6,8,15,24], thereby ameliorating the effect of perceived social isolation on mental health (i.e., significant stress and anxiety). By contrast, receiving a small or insufficient amount of social support from parents and online friends may enhance the negative effect [5–7,11,15]. Therefore, differences in the amount of social support may result in differences in the intensity of the effect between perceived social isolation and mental health in college students. Therefore, this study proposed the following moderation hypotheses:
H3a: Social support from parents moderates the relationship between perceived social isolation and mental health among college students in Hubei.
H3b: Social support from online friends moderates the relationship between perceived social isolation and mental health among college students in Hubei.
The current hypothetical model (Fig. 1) was constructed on the basis of previous studies and related theories. Social isolation and mental health were considered to underlie the main effect. Social support from parents and online friends was considered to exert a positive effect on mental health and the moderators of the main effect.
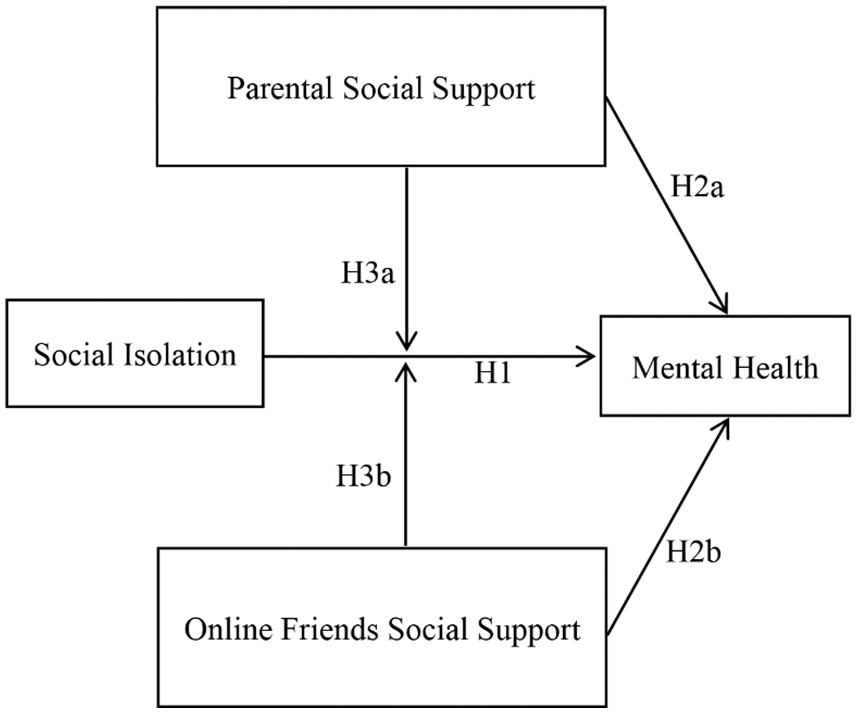
Figure 1: Hypothetical model
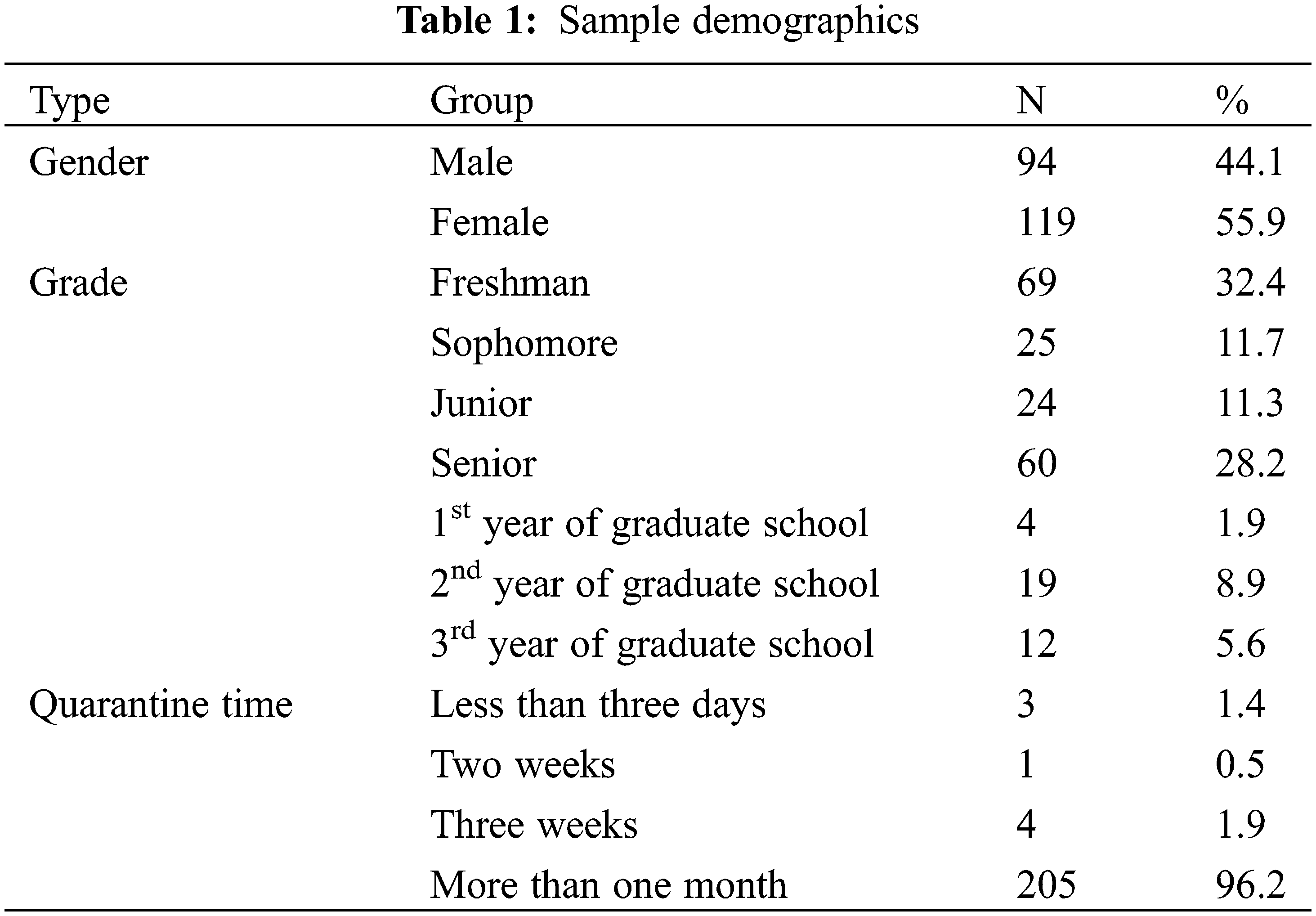
Considering the infection risk and restrictions on leaving the house, 346 online questionnaires were sent to students of four universities by university counselors in Hubei from 10–19 March, 2020, on WeChat. In all, 97.7% of participants reported living with their parents while under home quarantine. The participants had the study purpose explained to them first, and then they were asked to provide online written informed consent. Participation was voluntary, and all data were handled confidentially. Moreover, to encourage participation, five disposable masks were provided to each participant as a gift, which could be collected from a specific store. Only individuals who had access to both offline social support (from parents) and online social support (from online friends) during their home quarantine were included. Eventually, 213 valid samples were obtained; all of which were provided by college students in Hubei who lived with their parents while under home quarantine. The participant demographic characteristics are presented in Table 1.
This study measured three interrelated concepts developed by theory and supported by research, and their scales were scored on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree) and defined as follows:
(1) Social Isolation: Social isolation is a feeling without sufficient social communication and social support that worsens health-related quality of life and mental health [17,18]. The degree of social isolation was measured on a six-item questionnaire, comprising three reverse and three forward questions [18].
(2) Social Support: Social support is a psychological protective factor associated with cope stress and anxiety; its protective mechanism appears in the process of interaction with friends and parents [15,16,25]. Here, the degree of social support from parents and online friends was measured on an 18-item questionnaire [25] comprising eight questions related to psychological and material social support from parents and ten questions related to support from online friends. Here, an online friend was defined as any object that was interacted with through the Internet, and thus included both real-life and online-only friends.
(3) Mental Health: Mental health represents the degree of satisfaction with life, level of life meaning, ability to focus on thinking and learning, and satisfaction with self-appearance; here, the degree of mental health was measured on a six-item questionnaire [26].
Here, structural equation modeling was used to construct measurement and structural models for the current college students [27–30].
Original data were collated in SPSS and valid samples were executed using AMOS. Consequently, a measurement model was constructed and its reliability and validity were estimated through confirmatory factor analysis (CFA). First, the sample normality [27,31,32], and Cronbach’s alpha coefficient of the questionnaire item categories were calculated. Second, the model fit, factor loading, and variance of these categories were determined. The model fit indices included χ2, χ2/df, root mean square residual (RMR), standardized root mean square residual (SRMR), goodness-of-fit (GFI), comparative fit index (CFI), normed fit index (NFI), incremental fit index (IFI), Tucker-Lewis Index (TLI) and parsimony-adjusted normed fit index (PNFI) [27,30,33,34]. Finally, the convergent validity of the questionnaire was explained by calculating the composite reliability (CR) and average variance extracted (AVE), whereas their discriminant validity was revealed using the square root of the AVE and correlation coefficient of the two variables.
A structural direct effect model, constructed according to the current hypothesis model, was used for testing variable relationships. In addition, multigroup analysis was used to compare the different structural models for testing the moderating effects [35,36].
In this study, the relationship with parents and the relationship with online friends were considered and discussed separately because parental support and online friends’ support have different effects. In brief, direct effect models were constructed on the basis of social isolation, two social support types, and mental health for verifying H1, H2a, and H2b, and multigroup analysis was employed for verifying H3a and H3b. Default and test models were constructed for evaluating moderating effects. The chi-square difference, which was the indicator of the moderating effect, reached a significant difference between the default and test models [35,36]. The default and test models were constructed on the basis of the main effect of social isolation and mental health; high and low social support groups were divided according to mean social support scores [37]. The high and low groups were constructed for the main effect in the default model and were estimated freely; the model path coefficients of the high and low social support groups for the main effect in the test model were limited to equal each other [35,36]. Thus, a comparison of the model structural parameters of the default and test models was performed under different conditions by multigroup analysis [35,36]. If the chi-square difference of the two models reached significance, the test model of equal path coefficients was rejected, indicating that the main effect has different path coefficients according to the default level of social support. Therefore, a moderating effect is supported.
The measurement model was constructed after the questionnaire items were correctly coded (Fig. 2). According to the results of factor loadings per variable, items in the measurement model were deemed suitable and retained only when their loading was >0.50. Finally, after the invalid items (including three items from the social isolation questionnaire items with low factor loadings of 0.13, 0.14, and 0.39 and one item with a factor loading of 0.15, from the mental health questionnaire items) were removed, only 26 valid items remained (Table 2), and these were used subsequently.
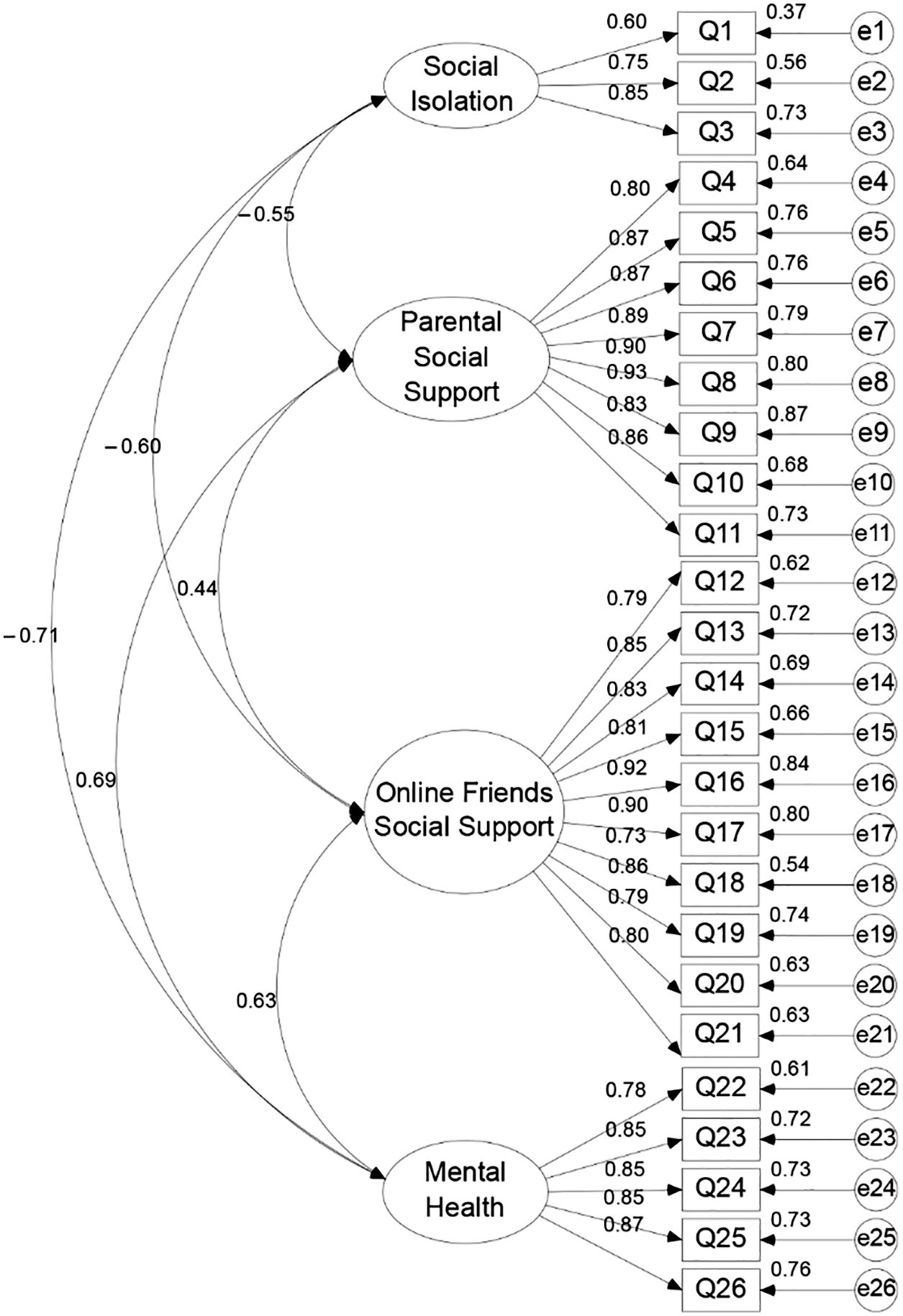
Figure 2: Measurement model
In this study, the univariate and multivariate normality tests indicated normal distribution. The absolute skewness and kurtosis values were in the range of 0.03–1.17 and 0.01–1.00, respectively [31], and the Mardia coefficient was 360.29 (i.e., lower than p(p + 2) = 728) [27,32]. Moreover, the Cronbach’s alpha values were 0.77, 0.96, 0.96, and 0.92 for questionnaire items on social isolation, social support from parents, social support from online friends, and mental health, respectively (Table 3).
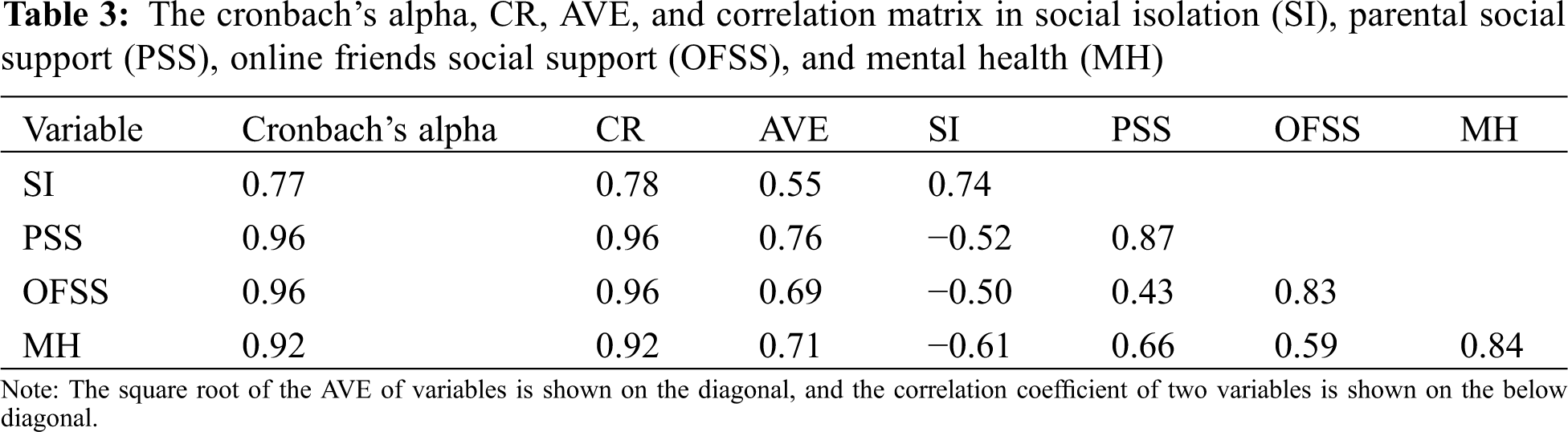
The convergent and discriminate validity, as explained through construct validity, was verified using CFA: the factor loadings were 0.60–0.93 (Fig. 2) and no variance was negative in the parameters [33,34]—all had significant t values. Moreover, the model fit indices demonstrated an acceptable fit: χ2 = 994.33 (p < 0.001), χ2/df = 3.39, RMR = 0.07, SRMR = 0.05, CFI = 0.87, NFI = 0.87, IFI = 0.87, and PNFI = 0.75 [27,30]. Finally, the CR and AVE of all variables were in the range of 0.78–0.96 and from 0.55–0.76, respectively (Table 3). Taken together, the results indicated that the current measurement model has reasonable reliability and convergent validity with internal consistency. Because correlation coefficients of the two variables were less than their corresponding square roots of AVEs (Table 3), the current model also has discriminant validity.
Finally, to reduce the common method variance (CMV) caused by self-reporting during the measurement process, specific instructions for separating variables (e.g., “The following topics are to understand your feelings during quarantine”) and the reverse question method were employed for the social isolation items [38]. Moreover, the single factor model containing 26 items demonstrated model fit: χ2 = 2,949.69 (p < 0.001), χ2/df = 9.87, RMR = 0.26, GFI = 0.31, CFI = 0.52, NFI = 0.50, IFI = 0.53, and PNFI = 0.46. Therefore, the results indicated the absence of any serious CMV in the current questionnaire [39].
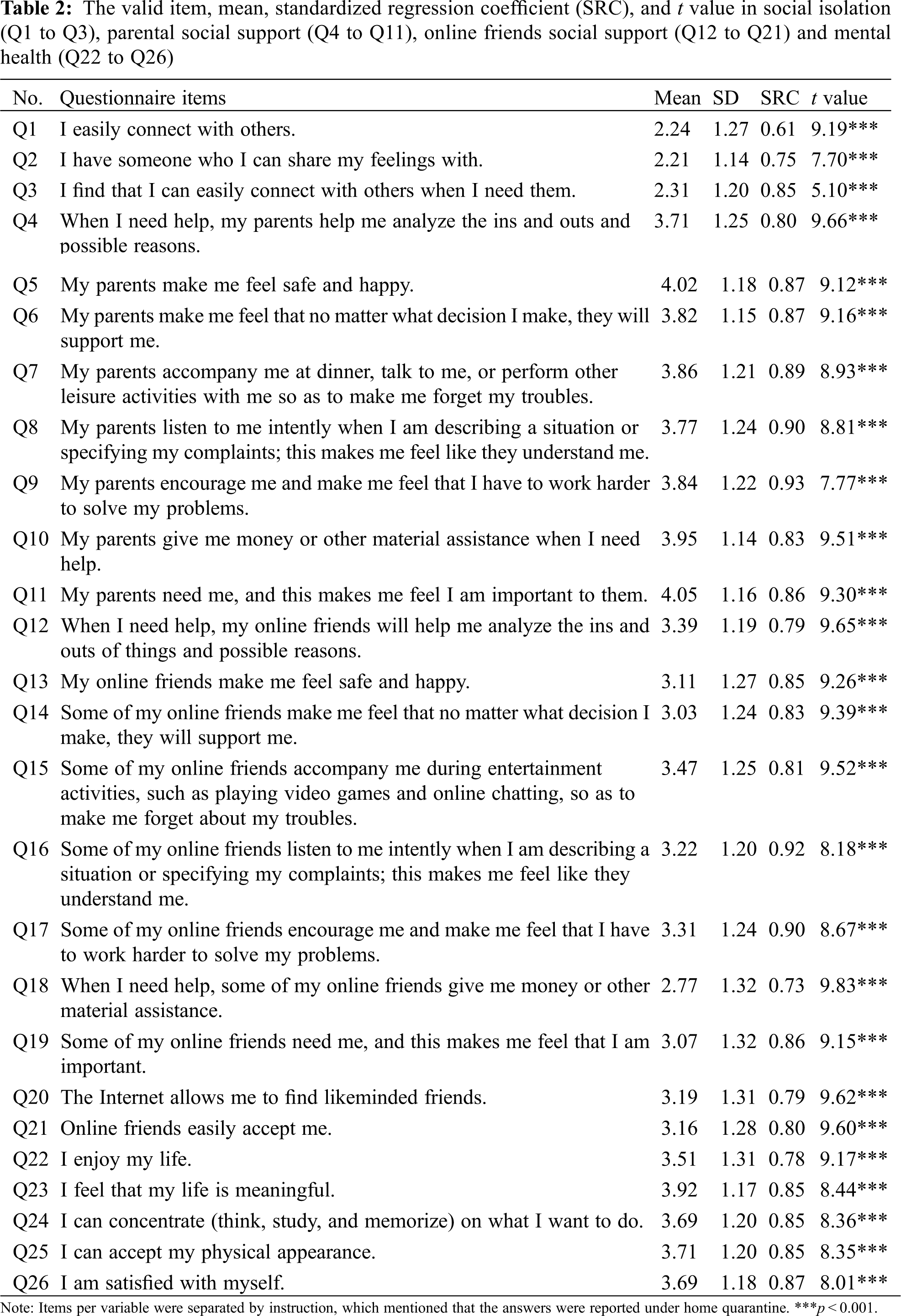
3.1.1 Moderating Effect of Parental Social Support
First, a structural direct effect model was constructed (Fig. 3). Standardized regression coefficients of all items ranged from 0.62 to 0.93; furthermore, the model fit demonstrated that the direct effect model was reasonable for our samples: χ2 = 359.02 (p < 0.001), χ2/df = 3.56, GFI = 0.83, RMR = 0.06, CFI = 0.92, NFI = 0.89, IFI = 0.92, and PNFI = 0.75 [27,30]. The path coefficients of social isolation (γ = −0.48, p < 0.001) and parental social support (γ = 0.43, p < 0.001) for mental health reached statistical significance (Fig. 3).
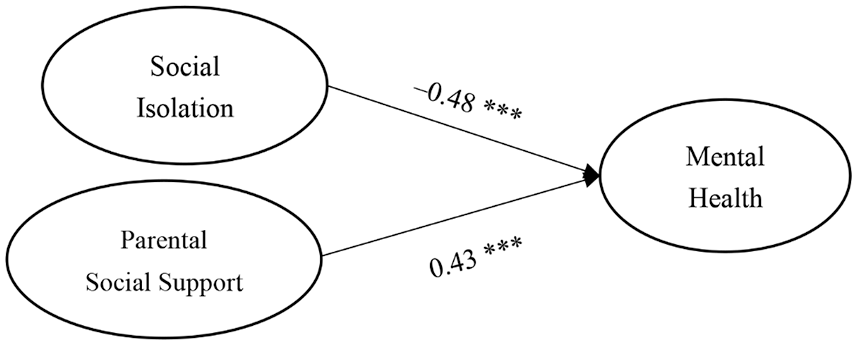
Figure 3: Direct effects of social isolation and parental social support on mental health
Note: ***p < 0.001.
Second, for multigroup analysis for the moderating role of parental social support, the mean scores of the scale for social support from parents were divided into high and low social support groups [35–37]. The high social support group demonstrated scores that were above average, indicating that individuals perceived that they can easily obtain mental and physical supports from parents, whereas the low social support group demonstrated contrary results [21]. Consequently, the number of individuals in the high and low social support groups was 117 and 96, respectively.
Third, the default model demonstrated acceptable fit: χ2 = 174.03 (p < .001), χ2/df = 4.58, GFI = 0.83, RMR = 0.09, CFI = 0.85, NFI = 0.82, IFI = 0.85, and PNFI = 0.55. Moreover, the test model demonstrated reasonable fit: χ2 = 177.29 (p < 0.001), χ2/df = 4.47, GFI = 0.83, RMR = 0.09, CFI = 0.85, NFI = 0.82, IFI = 0.85, and PNFI = 0.57. However, the fit of these models indicated the default model fit was not visibly superior to that of the test model. Simultaneously, the chi-square difference test confirmed that the fit between the default and test models did not have a significant difference in the chi-square value (Δχ2 (1) = 0.27, p > 0.05), thereby indicating that social support from parents did not moderate the social isolation–mental health relationship in the current college students [35,36]. Hypotheses H1 and H2a were accepted, but hypothesis H3a was rejected.
3.1.2 Moderating Effect of Social Support from Online Friends
First, a direct effect model was constructed on the basis of social isolation, social support from online friends, and mental health (Fig. 4); the standardized regression coefficients of all items ranged from 0.62 to 0.92; the model demonstrated a reasonable fit: χ2 = 532.89 (p < 0.001), χ2/df = 4.04, CFI = 0.88, RMR = 0.07, NFI = 0.85, IFI = 0.88, TLI = 0.86, and PNFI = 0.73 [27,30]. The path coefficients of social isolation (γ = −0.51, p < 0.001) and social support from online friends (γ = 0.33, p < 0.001) on mental health all reached statistical significance (Fig. 4).
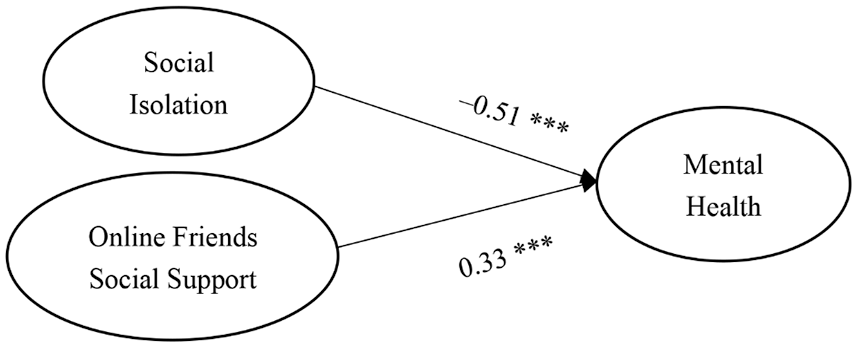
Figure 4: Direct effects of social isolation and online friends social support on mental health
Note: ***p < 0.001.
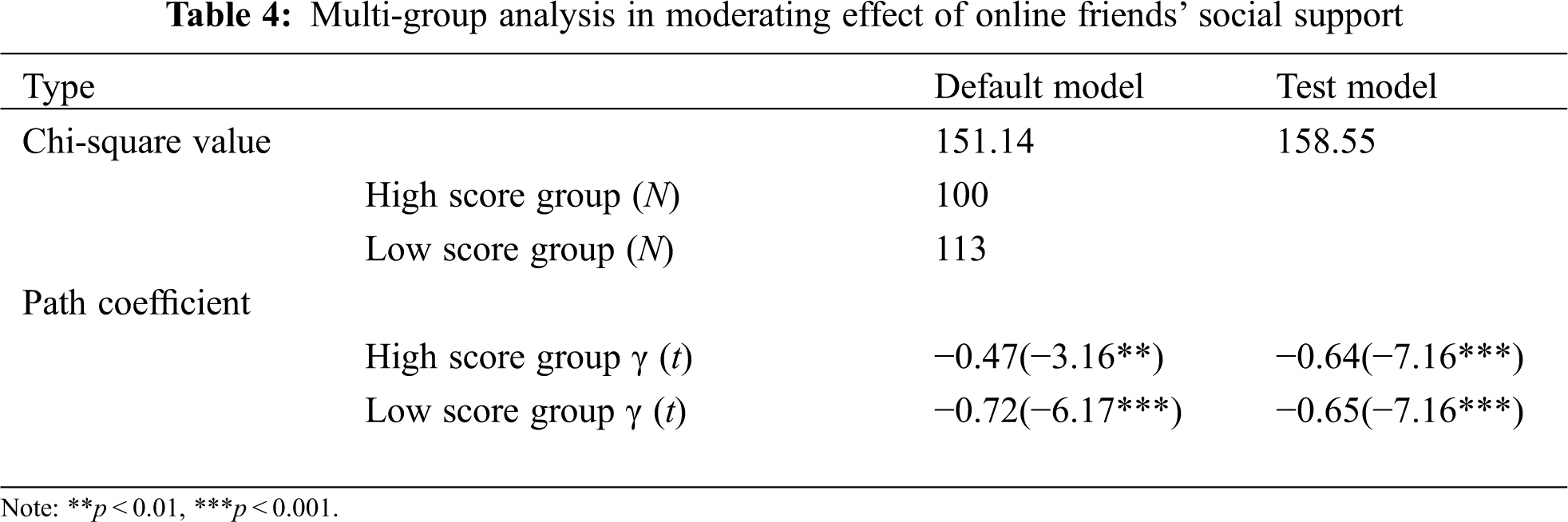
Second, the moderating effect of social support from online friends was confirmed using multigroup analysis, where the number of individuals in the high and low social support groups were 100 and 113, respectively.
Third, the default model demonstrated acceptable fit: χ2 = 151.137 (p < 0.001), χ2/df = 3.98, GFI = 0.85, RMR = 0.08, CFI = 0.88, NFI = 0.85, IFI = 0.88, and PNFI = 0.58. Moreover, the test model demonstrated reasonable fit: χ2 = 158.55 (p < 0.001), χ2/df = 4.07, GFI = 0.85, RMR = 0.11, CFI = 0.87, NFI = 0.84, IFI = 0.87, and PNFI = 0.59. These fit indices demonstrated that the fit of the default model was slightly superior to that of the test model. Next, the chi-square difference test revealed a significant difference between the default and test model fit (Δχ2 (1) = 7.42, p < 0.01); therefore, social support from online friends moderated the social isolation–mental health relationship in the current college students. Hypotheses H1, H2b, and H3b were accepted.
Fourth, this moderating effect was resolved by path coefficients and t values [35]. Here, in the default model, social isolation in the high (t = −3.16, p < 0.01) and low (t = −6.17, p < 0.001) online friends social support groups negatively and significantly affected mental health (Table 4). However, the level of social support from online friends created a moderating effect in the relationship between social isolation and mental health. In the low social support group, social isolation negatively affected mental health (γ = −0.72, p < 0.001) more strongly than it did in the high social support group (γ = −0.47, p < 0.01).
Hypotheses H1, H2a, H2b, H3a, and H3b were verified. The results for H1, H2a, and H2b were consistent with those of previous studies—verified on the basis of the direct effect models in this study (Figs. 3 and 4, respectively). Thus, perceived social isolation of home quarantine had a negative effect on the mental health of college students in Hubei [9,10,17], and social support from parents and online friends had a positive effect on the mental health of college students in Hubei [11,22,23]. Furthermore, H3b was accepted, but H3a was rejected. In accordance with the stress buffering theory [15,16], social support from online friends moderated the relationship between perceived social isolation and mental health; however, social support from parents did not. This difference in outcomes demonstrates that social support from online friends may be more important than social support from parents [12,13]. The results of H3b were verified in a multigroup analysis. The high online friends social support group exhibited a relatively weak relationship between perceived social isolation and mental health, whereas the low online friends social support group exhibited a relatively strong relationship between perceived social isolation and mental health.
According to the results of hypotheses H1, H2b, and H3b, this research shows that social support from online friends was essential for the mental health of college students in Hubei who were under home quarantine. The perceived social isolation of home quarantine may result in poor mental health [9,10], possibly because college students in Hubei were quarantined in confined environments for a prolonged period, leading to feelings of anxiety and stress [5,6]. Receiving social support from online friends may act as a stress buffer that helps prevent college students in Hubei from developing poor mental health [13]. The moderating role of social support from online friends in the relationship between social isolation and mental health was shown to be strong. According to stress buffering theory, social support from online friends is considered a stress buffer and facilitates the development of problem-solving strategies [15]. This buffering effect enhanced or reduced adaptation to the circumstances of home quarantine depending on the amount of social support received from online friends [14,15]. Consequently, while under home quarantine, college students who receive sufficient social support from online friends may avoid the negative effect of perceived social isolation on mental health. Furthermore, an absence of sufficient social support from online friends may enhance the negative effect of perceived social isolation on the mental health of the college students [5–8,17,19]. Therefore, social support from online friends may improve the mental health of college students in Hubei who are under home quarantine.
This study revealed that perceived social isolation negatively predicted mental health among college students in Hubei who were under home quarantine during the COVID-19 pandemic. Furthermore, it showed that social support from online friends moderated this relationship: the relationship between perceived social isolation and mental health becomes stronger when social support is more abundant.
This study discussed the theoretical interpretation of how social support from online friends moderates the relationship between perceived social isolation and mental health while under home quarantine. This research can help psychological researchers understand the moderating mechanism of social support from online friends and the importance of social support from online friends for the mental health of college students who are under home quarantine.
Home quarantine of people who have had close contact with COVID-19, and especially college students [40], has become a standard policy procedure for reducing the spread of COVID-19 [41]. This study mainly revealed that perceived social isolation of home quarantine negatively predicted the mental health of college students in Hubei [9,10,17]. Social support from online friends was a buffer against deteriorations in mental health among college students in Hubei who were under home quarantine [13]. Receiving sufficient social support from online friends reduced the negative effect of perceived social isolation on mental health, and insufficient social support from online friends enhanced the negative effect of perceived social isolation on mental health [5–8,17,19]. This study makes the following three recommendations to Chinese university staff, counselors, and the government on how to support and preserve the mental health of students who are experiencing the social isolation of home quarantine. First, university staff should establish a team of counselors to provide psychological crisis and intervention support. Second, these counselors should play the role of online friends providing support to college students who are developing poor mental health due to perceiving social isolation while under home quarantine. Finally, the Chinese government should be cautious in implementing epidemic prevention policies such as home quarantine. If social isolation perception increases, young people may be at risk of social withdrawal. Strong social support systems that include parents and social contact through the Internet may help reduce the phenomenon of social withdrawal among young people [42,43]. The Chinese government can refer to other countries when designing epidemic prevention policies.
5.2 Limitations and Future Directions
This study used a relatively small sample, which may be the reason the model fits were not perfect. Future studies should use larger sample sizes, particularly when multiple conditions are to be sampled. The use of quarantines as a pandemic response tool has been expanding in China and also in various other countries; thus, follow-up research on social isolation is warranted.
In this study, the Cronbach’s alpha was α = 0.77. This could be because this study only used three social isolation measurement items to measure social isolation. Follow-up research on social isolation should consider using more measurement items.
The correlational findings of this study do not imply causation. The findings of this study only explained the potential importance of social support from online friends for the mental health of college students in Hubei who are under home quarantine. The findings of this study can be used as a reference for future research on social isolation.
Acknowledgement: The authors would like to thank all the colleagues, students, editors, and reviewers who contributed to this study.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Zhu, P., Tan, X. (2021). Is compulsory home quarantine less effective than centralized quarantine in controlling the COVID-19 outbreak? Evidence from Hong Kong. Sustainable Cities and Society, 74, 103222. DOI 10.1016/j.scs.2021.103222. [Google Scholar] [CrossRef]
2. Du, Z., Wang, L., Cauchemez, S., Xu, X., Wang, X. et al. (2020). Risk for transportation of 2019 novel Coronavirus disease from Wuhan to other cities in China. Emerging Infectious Diseases, 26(5), 1049–1052. DOI 10.3201/eid2605.200146. [Google Scholar] [CrossRef]
3. Chen, Y., Wang, Y., Wang, H., Hu, Z., Hua, L. (2020). Controlling urban traffic-one of the useful methods to ensure safety in Wuhan based on COVID-19 outbreak. Safety Science, 131, 104938. DOI 10.1016/j.ssci.2020.104938. [Google Scholar] [CrossRef]
4. Ji, T., Chen, H. L., Xu, J., Wu, L. N., Li, J. J. et al. (2020). Lockdown contained the spread of 2019 novel coronavirus disease in Huangshi City, China: Early epidemiological findings. Clinical Infectious Diseases, 71(6), 1454–1460. DOI 10.1093/cid/ciaa390. [Google Scholar] [CrossRef]
5. Zuckerman, M., Persky, H., Link, K. E., Basu, G. K. (1968). Experimental and subject factors determining responses to sensory deprivation, social isolation, and confinement. Journal of Abnormal Psychology, 73(3), 183–194. DOI 10.1037/h0025748. [Google Scholar] [CrossRef]
6. Davis, J. M., McCourt, W. F., Courtney, J., Solomon, P. (1961). Sensory deprivation: The role of social isolation. Archives of General Psychiatry, 5(1), 84–90. DOI 10.1001/archpsyc.1961.01710130086010. [Google Scholar] [CrossRef]
7. Hossain, M. M., Sultana, A., Purohit, N. (2020). Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. Epidemiology and Health, 42, e2020038. DOI 10.4178/epih.e2020038. [Google Scholar] [CrossRef]
8. Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S. et al. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. DOI 10.1016/S0140-6736(20)30460-8. [Google Scholar] [CrossRef]
9. Hamza, C. A., Ewing, L., Heath, N. L., Goldstein, A. L. (2021). When social isolation is nothing new: A longitudinal study on psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Canadian Psychology, 62(1), 20–30. DOI 10.1037/cap0000255. [Google Scholar] [CrossRef]
10. Pancani, L., Marinucci, M., Aureli, N., Riva, P. (2021). Forced social isolation and mental health: A study on 1,006 Italians under COVID-19 lockdown. Frontiers in Psychology, 12, 663799. DOI 10.3389/fpsyg.2021.663799. [Google Scholar] [CrossRef]
11. Zhang, J., Wu, W., Zhao, X., Zhang, W. (2020). Recommended psychological crisis intervention response to the 2019 novel Coronavirus pneumonia outbreak in China: A model of West China Hospital. Precision Clinical Medicine, 3(1), 3–8. DOI 10.1093/pcmedi/pbaa006. [Google Scholar] [CrossRef]
12. Zhen, L., Nan, Y., Pham, B. (2021). College students coping with COVID-19: Stress-buffering effects of self-disclosure on social media and parental support. Communication Research Reports, 38(1), 23–31. DOI 10.1080/08824096.2020.1870445. [Google Scholar] [CrossRef]
13. Juvonen, J., Schacter, H. L., Lessard, L. M. (2021). Connecting electronically with friends to cope with isolation during COVID-19 pandemic. Journal of Social and Personal Relationships, 38(6), 1782–1799. DOI 10.1177/0265407521998459. [Google Scholar] [CrossRef]
14. Bandura, A., Walters, R. H. (1977). Social learning theory, vol. 1. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
15. Cohen, S., Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. DOI 10.1037/0033-2909.98.2.310. [Google Scholar] [CrossRef]
16. Lakey, B., Orehek, E. (2011). Relational regulation theory: A new approach to explain the link between perceived social support and mental health. Psychological Review, 118(3), 482–495. DOI 10.1037/a0023477. [Google Scholar] [CrossRef]
17. Wang, J., Lloyd-Evans, B., Giacco, D., Forsyth, R., Nebo, C. et al. (2017). Social isolation in mental health: A conceptual and methodological review. Social Psychiatry and Psychiatric Epidemiology, 52(12), 1451–1461. DOI 10.1007/s00127-017-1446-1. [Google Scholar] [CrossRef]
18. Hawthorne, G. (2006). Measuring social isolation in older adults: Development and initial validation of the friendship scale. Social Indicators Research, 77(3), 521–548. DOI 10.1007/s11205-005-7746-y. [Google Scholar] [CrossRef]
19. Ali, A., Kohun, F. (2007). Dealing with social isolation to minimize doctoral attrition-a four stage framework. International Journal of Doctoral Studies, 2, 33–49. DOI 10.28945/56. [Google Scholar] [CrossRef]
20. Ma, J., Batterham, P., Calear, A. L., Sunderland, M. (2019). The development and validation of the thwarted belongingness scale (TBS) for interpersonal suicide risk. Journal of Psychopathology and Behavioral Assessment, 41(3), 456–469. DOI 10.1007/s10862-019-09721-6. [Google Scholar] [CrossRef]
21. Tomaka, J., Thompson, S. E., Palacios, R. (2006). The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. Journal of Aging and Health, 18(3), 359–384. DOI 10.1177/0898264305280993. [Google Scholar] [CrossRef]
22. Reid, G. M., Holt, M. K., Bowman, C. E., Espelage, D. L., Green, J. G. (2016). Perceived social support and mental health among first-year college students with histories of bullying victimization. Journal of Child and Family Studies, 25(11), 3331–3341. DOI 10.1007/s10826-016-0477-7. [Google Scholar] [CrossRef]
23. Hefner, J., Eisenberg, D. (2009). Social support and mental health among college students. American Journal of Orthopsychiatry, 79(4), 491–499. DOI 10.1037/a0016918. [Google Scholar] [CrossRef]
24. Wang, G. H., Zhang, Y. T., Zhao, J., Zhang, J., Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet, 395(10228), 945–947. DOI 10.1016/S0140-6736(20)30547-X. [Google Scholar] [CrossRef]
25. Yeh, Y. C., Ko, H. C., Wu, J. Y. W., Cheng, C. P. (2008). Gender differences in relationships of actual and virtual social support to internet addiction mediated through depressive symptoms among college students in Taiwan. Cyber Psychology & Behavior, 11(4), 485–487. DOI 10.1089/cpb.2007.0134. [Google Scholar] [CrossRef]
26. Zhang, C. H., Cheng, Y. F., Chin, H. C., Lee, H. N. (2013). A study on the test of validity and reliability of WHOQOL-BREF when it was applied to adults with severe visual impairments. Bulletin Educational Psychology, 44, 521–536. [Google Scholar]
27. Bollen, K. A. (1989). Structural equations with latent variables. New York, NY: Wiley. [Google Scholar]
28. Byrne, B. B. (2010). Structural equation modeling using AMOS: Basic concepts, applications, and programming. 2nd edition. New York, NY: Routledge. [Google Scholar]
29. Kline, R. B. (2010). Principles and practice of structural equation modelling. 3rd edition. New York, NY: Guilford. [Google Scholar]
30. Schumacker, R. E., Lomax, R. G. (2004). A beginner’s guide to structural equation modelling. 2nd edition. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
31. Bollen, K. A., Long, J. S. (1993). Testing structural equation models, vol. 154. Newbury Park, CA: SAGE. [Google Scholar]
32. Raykov, T., Marcoulides, G. A. (2008). An introduction to applied multivariate analysis. New York, NY: Taylor & Francis. [Google Scholar]
33. Bagozzi, R. P., Yi, Y. (2012). Specification, evaluation, and interpretation of structural equation models. Journal of the Academy of Marketing Science, 40(1), 8–34. DOI 10.1007/s11747-011-0278-x. [Google Scholar] [CrossRef]
34. Fornell, C., Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18(1), 39–50. DOI 10.2307/3151312. [Google Scholar] [CrossRef]
35. Paulssen, M., Roulet, R., Wilke, S. (2014). Risk as moderator of the trust-loyalty relationship. European Journal of Marketing, 48(5), 964–981. DOI 10.1108/EJM-11-2011-0657. [Google Scholar] [CrossRef]
36. Rodríguez, N. G., Pérez, M. J. S., Gutiérrez, J. A. T. (2008). Can a good organizational climate compensate for a lack of top management commitment to new product development? Journal of Business Research, 61(2), 118–131. DOI 10.1016/j.jbusres.2007.06.011. [Google Scholar] [CrossRef]
37. Cauce, A. M., Felner, R. D., Primavera, J. (1982). Social support in high-risk adolescents: Structural components and adaptive impact. American Journal of Community Psychology, 10(4), 417–428. DOI 10.1007/BF00893980. [Google Scholar] [CrossRef]
38. Peng, T. K., Kao, Y. T., Lin, C. C. (2006). Common method variance in management research: Its nature, effects, detection, and remedies. Journal of Management, 23(1), 77–98. [Google Scholar]
39. Verhagen, T., van Dolen, W. (2011). The influence of online store beliefs on consumer online impulse buying: A model and empirical application. Information & Management, 48(8), 320–327. DOI 10.1016/j.im.2011.08.001. [Google Scholar] [CrossRef]
40. Chang, B., Hou, J. (2022). The association between perceived risk of COVID-19, psychological distress, and internet addiction in college students: An application of stress process model. Frontiers in Psychology, 13, 898203. DOI 10.3389/fpsyg.2022.898203. [Google Scholar] [CrossRef]
41. Centers for Disease Control and Prevention (2022). Public health guidance for potential COVID-19 exposure associated with travel. https://www.cdc.gov/coronavirus/2019-ncov/php/risk-assessment.html. [Google Scholar]
42. Tateno, M., Teo, A. R., Ukai, W., Kanazawa, J., Katsuki, R. et al. (2019). Internet addiction, smartphone addiction, and Hikikomori trait in Japanese young adult: Social isolation and social network. Frontiers in Psychiatry, 10, 455. DOI 10.3389/fpsyt.2019.00455. [Google Scholar] [CrossRef]
43. Teo, A. R. (2010). A new form of social withdrawal in Japan: A review of Hikikomori. International Journal of Social Psychiatry, 56(2), 178–185. DOI 10.1177/0020764008100629. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools