 Open Access
Open Access
ARTICLE
The Relationship between Mental Disorders and Personality of Outpatients in a Psychiatric Clinic in Nanjing, China
1 Department of Epidemiology and Biostatistics, School of Public Health, Southeast University, Nanjing, 210009, China
2 Medical Statistics and Analysis Center, Nanjing Drum Tower Hospital, Nanjing University Medical School, Nanjing, 210008, China
3 Department of Clinical Psychology, Nanjing Drum Tower Hospital, Nanjing University Medical School, Nanjing, 210008, China
* Corresponding Authors: Qiuyun Cao. Email: ; Bingwei Chen. Email:
(This article belongs to the Special Issue: Mental Health and Social Development)
International Journal of Mental Health Promotion 2023, 25(12), 1287-1302. https://doi.org/10.32604/ijmhp.2023.042584
Received 05 June 2023; Accepted 06 September 2023; Issue published 29 December 2023
Abstract
Psychosis has increasingly become a social problem, emphasizing the need to understand the relationship between mental disorders and personality. This study aimed to investigate the relationship between mental disorders and personality among psychiatric outpatients based on real-world data. Symptom Checklist 90 (SCL-90) and Eysenck Personality Questionnaire (EPQ) were used to evaluate the personality and psychopathological symptoms of patients (n = 8409) in the Psychiatric Outpatient Department at Nanjing Drum Tower Hospital. t-test was used to compare scores between patients and national norms. Pearson’s correlation coefficient and path analysis were used to explore the relationship between mental health status and personality. The correlation coefficient between the neuroticism (N) score and each factor score of the SCL-90 test, as well as the correlation between psychoticism (P) and hostility and paranoia, exceeded 0.4. Path analysis revealed that the standardized path coefficients of N score and SCL-90 were all higher than 0.4. In addition, the standardized path coefficient of hostility and paranoia on P score were 0.313 and 0.280, respectively. Interpersonal sensitivity, depression and obsessive-compulsive symptoms were affected by extraversion (E) score, with standardized path coefficients of −0.149, −0.138, and −0.105, respectively. The path analysis also showed the direct and indirect effects of age, gender, education, and marital status on SCL-90. Patients characterized as melancholic had higher scores in all factors of SCL-90. In conclusion, mental health was related to personality traits of neuroticism, psychoticism and introversion.Keywords
Mental disorder is a significant contributor to the global burden of disease [1,2]. With population growth and aging, the focus of public health concerns has shifted from communicable diseases to non-communicable diseases. This shift has further increased the disease burden of mental disorders, especially in middle-income countries [3]. According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Illness (DSM-5), mental disorder is defined as a syndrome characterized by significant impairment of personal cognitive functioning, emotional regulation or behavior, which reflects the potential mental disorder in psychological, biological and developmental processes [4]. In 2019, the China Mental Health Study published the results of a cross-sectional survey on the prevalence of mental illnesses in 157 nationally representative population disease monitoring stations across 31 provinces. The study revealed an increasing trend in the prevalence of mental disorders, confirming the severity of the disease burden [5]. Based on the reported data, severe depression and anxiety disorder have emerged as the most common mental diseases in China [6].
Personality is a relatively stable cognitive and behavioral characteristic among individuals, which is considered to be a bridge between disease and normal social function and has a significant impact on mental health [7]. Personality stability is the result of the interaction between individuals and their environment [8] and it has the cumulative continuity principle of personality development [9]. This principle reflects the outcome of personality development and maturity over time. Personality is believed to influence social functioning, the occurrence of common mental disorders, and the course and remission of psychopathological syndromes [10]. Therefore, early characterization of personality could potentially help identify people who are more susceptible to severe mental disorders [11]. Increased neuroticism and depressive coping style as well as reduced self-esteem and mastery collectively denoted as personality deviance were considered to be significantly related to the ongoing expression of vulnerability for depression. The change in the severity of depressive symptoms and the severity of personality deviance is synchronous [12]. Specific consideration of personality is important when providing and distributing mental health services.
Symptom Checklist-90 (SCL-90) and Eysenck Personality Questionnaire (EPQ) are widely used in psychiatry to evaluate the symptoms of mental disorders and personality traits, respectively, and they have strong reliability and validity [13–15]. Some scholars have conducted SCL-90 and EPQ tests for psychiatric patients to investigate the characteristics of patients with various symptoms. A study from a public psychiatric hospital in Mexico found that psychiatry residents exhibited more frequent or severe interpersonal sensitivity, depression, obsessive-compulsive, and somatic worries compared to the general Mexican population [16]. Recently, Chen et al. [17] used a 30-day timely return visit rate was used to investigate psychiatric outpatients and found showed that patients with high scores on SCL-90 phobic anxiety and EPQ psychoticism had poor initial adherence.
Traditional studies of the relationship between EPQ and SCL-90 included Pearson correlation analysis [18] and partial correlation analysis [19]. However, these methods have less research on the relationship between SCL-90 and EPQ scale items. Path analysis can deal with the relationship between complex variables, and can show advantages when the number of variables is large and the correlation between variables is complex. It allows researchers not only to examine the direct impact of a predictor on a dependent variable but also to observe other types of relationships, including indirect effects [20]. Chen et al. [21] used Path analysis to investigate the relationship between EPQ and total mean score of SCL90 among parents of burn hospitalized children. They found that the most influential factors on the total score were the P-dimension score and the age of the child. İnak et al. [22] used a structural equation model to investigate the impact of the 10-items. Personality Inventory on SCL-90-R scores and the impact of SCL-90-R on nonverbal immediate behavior to examine the relationships between Big Five personality traits, psychopathology, and nonverbal immediacy behaviors.
In this study, the personality characteristics and mental disorders of outpatients in the Psychiatry Department in Drum Tower of Nanjing Hospital, Nanjing University Medical School, were investigated using the SCL-90 and EPQ. Correlation analysis was used to explore the relationship between personality and mental disorders. Path analysis was used to explore the relationship between SCL-90 items and EPQ dimensions, including direct and indirect effects of variables. This study aimed to provide personalized prevention for mental disorders of different personality groups, as well as early detection and treatment of mental disorders.
This retrospective study was based on real-world data from Nanjing Drum Tower Hospital, Nanjing University Medical School. The participants were first-visit outpatients between June 2014 and May 2019, regardless of age and gender. The patients’ chief complaints included symptoms of insomnia, anxiety, depression, compulsion, panic attack, and social phobia, as well as physical symptoms that were not abnormal during the examination, such as headache, back pain, palpitation, chest tightness, nausea, abdominal distension, fatigue and other symptoms. EPQ and SCL-90 were tested simultaneously. Data such as age, gender, marital status and education were obtained from the medical records. This study was approved by the ethics committee of Nanjing Drum Tower Hospital (approval no. 2021-096-01).
SCL-90, a psychiatric self-report list, is the most widely used outpatient examination scale for mental disorders and other mental diseases in worldwide, with high reliability and validity [23,24]. From the aspects of personal feelings, emotions, thinking, consciousness, behavior, living habits, interpersonal relationship, diet and sleep, the SCL-90 can assess and evaluate whether a person may have some mental disorder related to psychological symptoms and their severity. SCL-90 has a comprehensive description of the psychological symptoms of psychosis as well as the capacity to observe and distinguish the specific mental symptoms. It has been proven to be a vital and effective tool in the identification of primary health care and psychiatric symptoms, measurement and analysis of the overall psychological distress of subjects, detection of changes and reflection of symptom characteristics and comparison of intervention effects in mental and neuropsychiatric diseases [25].
SCL-90 contains 10 self-assessment dimensions and 90 self-report items [26]. The 10 self-assessment factors are somatization, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, terror, paranoia, psychoticism and others. Each self-report item is scored on a scale of 1–5. SCL-90 assesses the mental health status of the subjects based on the total symptom score index and factor score. The more severe the frequency and intensity of the symptoms corresponding to the factor, the higher the score of some factors. The national norm of SCL-90 was obtained from the survey of healthy populations in 13 regions in China (n = 1338) [27].
EPQ is a self-assessment scale developed by well-known psychologist Eysenck et al. [28]. The questionnaire consists of four dimensions: extraversion (E), neuroticism (N), psychoticism (P), and lying (L). According to Eysenck’s theory, extraversion is characterized by good communication, a desire for stimulation and adventure, and being easy to be impulsive; neuroticism is characterized by a high degree of negative effects, such as depression and anxiety; and psychoticism is independent of neuroticism and has the characteristics of stubbornness, which are manifested as loneliness, difficulty in adapting to the external environment and strong aggression [29].
The revised EPQ questionnaire contains 88 items, all of which are answered with “yes” and “no”. The national norm of EPQ was obtained from a survey conducted including 13 provinces in 6 regions of China (n = 2517). The original EPQ score were converted to standard score (T-scores) based on the national norm score grouped by age and gender [14].
If the standard score is between 43.3 and 56.7, the personality characteristics of this dimension are of intermediate type. The standard score of tendency type is between 38.5 and 43.3 or 56.7 and 61.5. The standard score of the typical type is less than 38.5 or greater than 61.5.
In the EPQ questionnaire survey, we use a standard score of 50 as the boundary. A higher score on the E dimension indicates a more significant tendency towards extroversion, while a higher P score indicates greater emotional instability. In Eysenck’s two-dimensional model of personality theory, temperament is classified into four types based on EPQ scores: introverted-unstable, introverted-stable, extroverted-unstable and extroverted-stable, corresponding to, melancholic, phlegmatic, choleric, and sanguineous, respectively. These types reflect the comprehensive effect of psychic temperament and introverted and extroverted personality [30]. Choleric, also known as leadership temperament, is characterized by individuals who are confident, decisive, and aggressive. Sanguineous, also known as lively temperament, refers to individuals who are outgoing, optimistic, and have cheerful and easy-going behavior. Phlegmatic, also known as steady temperament, is characterized by individuals who are thick, steady, and meticulous in their actions. Melancholic is also known as the quiet temperament, which refers to individuals with introverted, quiet, and cautious behavior.
SAS 9.4 was used to analyze data. Continuous variables were described using mean and standard deviation (SD). Categorical variables were expressed using frequency and percentage. Differences in factors of SCL-90 and EPQ tests between the patients and national norms were compared using t-test. One-way variance analysis (ANOVA) was used to compare the differences in SCL-90 scores among four different temperament groups of psychiatric outpatients, Bonferroni post hoc test was used if significant differences were found. The differences between the two groups were expressed using the mean and Bonferroni-adjusted 95% confidence interval (CI). Pearson’s correlation analysis and path analysis were used to investigate the relationship between mental disorders and personality types. We present Person correlation coefficient and 95% CI to account for correlation analysis. A p-value of <0.05 was considered statistically significant.
Basic characteristics of the participants
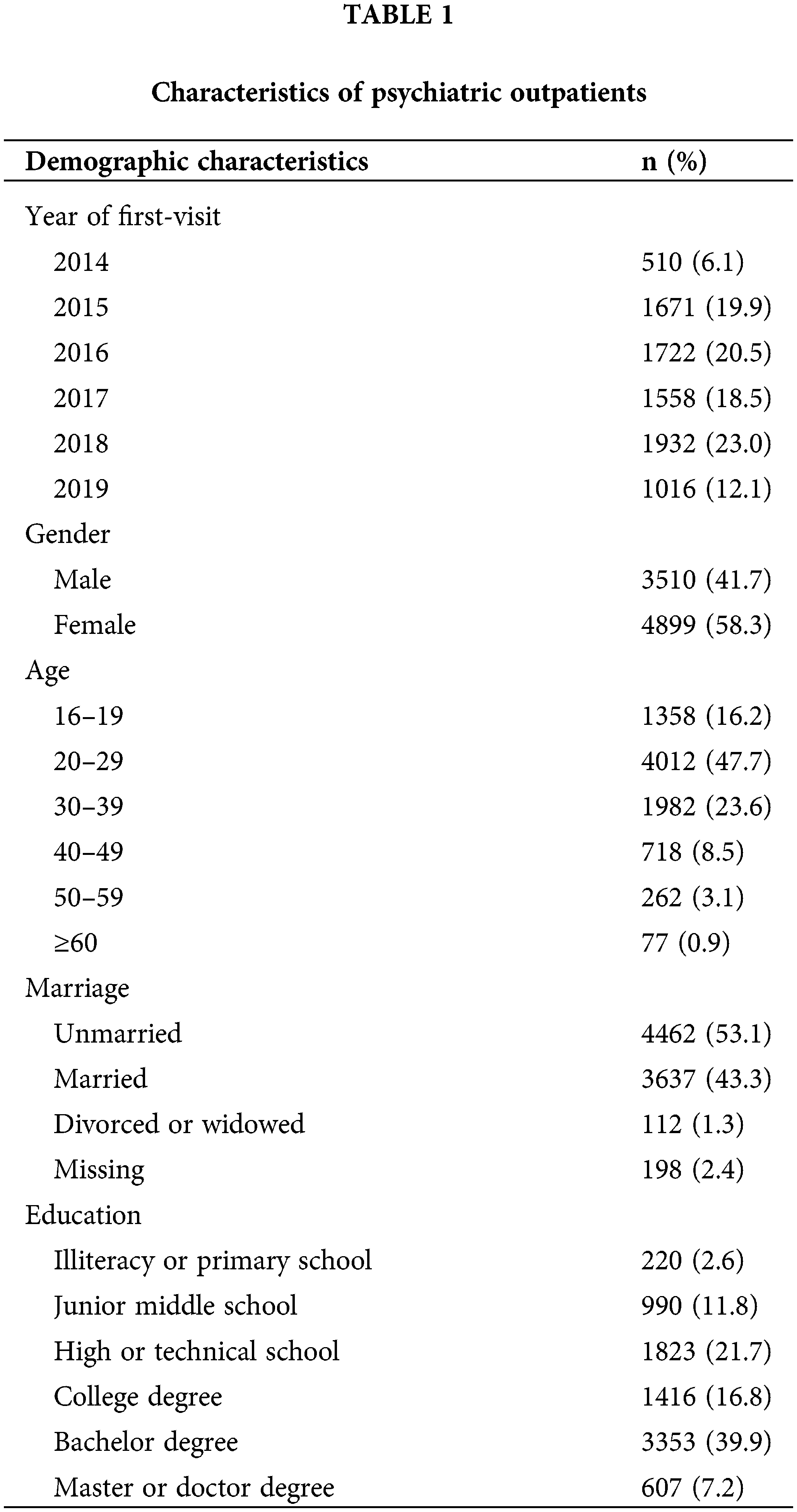
During the period from June 2014 to May 2019, a total of 8,762 first-visit outpatients received SCL-90 and EPQ tests on the same day. Of these, 353 patients with a high degree of concealment were excluded (if the L score in the EPQ test was greater than 61.5). Finally, 8,409 patients (average age 28.46 ± 9.62 years old) were included in the analysis. There were 3,510 males and 4,899 females. Table 1 summarizes the demographic characteristics of the study population.
Reliability analysis of SCL-90 and EPQ
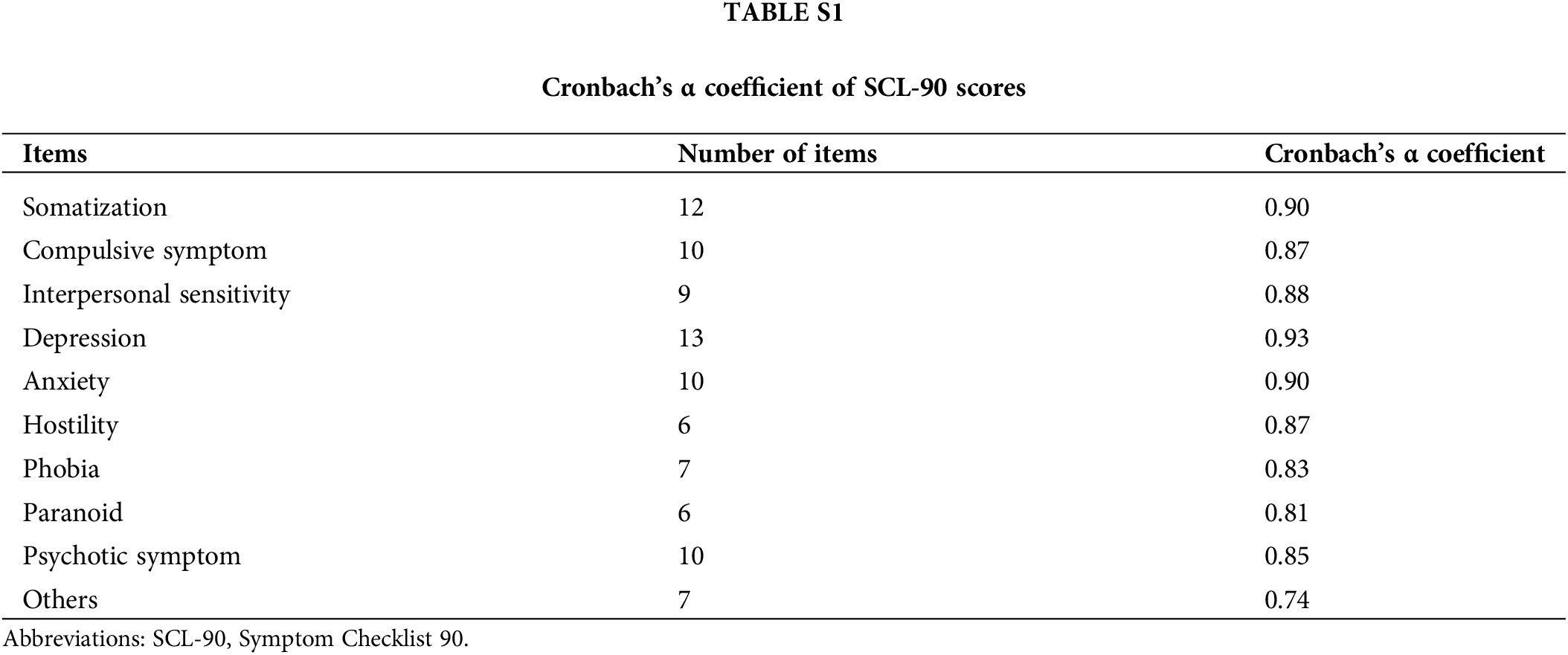
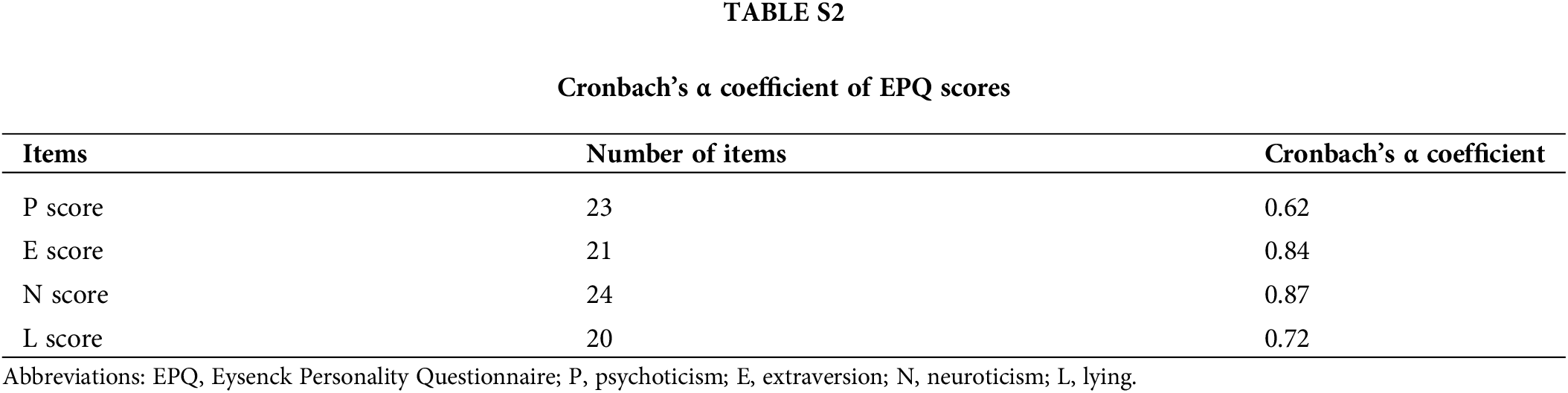
Cronbach’s alpha was used to independently analyze internal consistency across all domains. Cronbach’s α of SCL-90 ranged from 0.74 to 0.93 and for EPQ, it ranged from 0.62 to 0.87. Suppl. Tables S1 and S2 show detailed Cronbach’s α coefficients for each dimension, demonstrating that internal consistency was acceptable.
SCL-90 scores of psychiatric outpatients
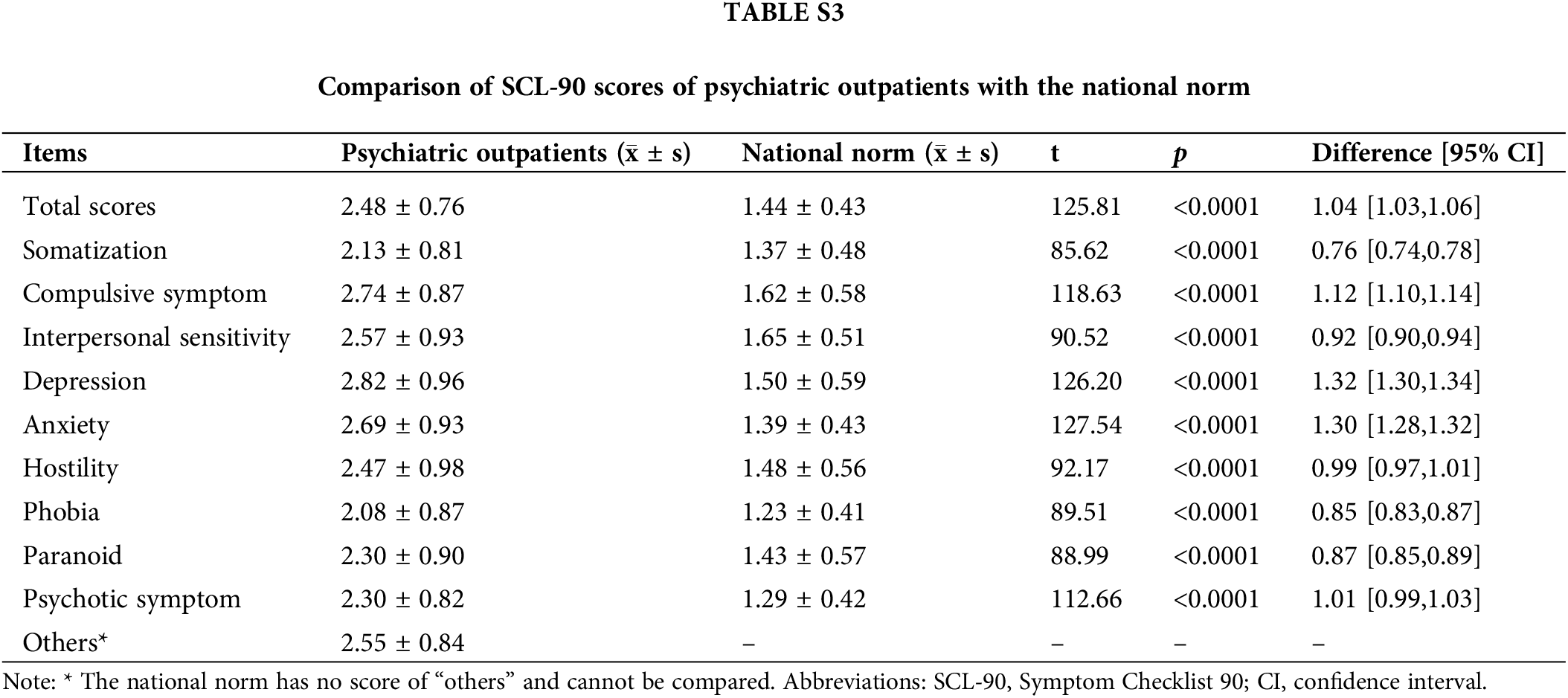
As is shown in Fig. 1 and Suppl. Table S3, the t-test revealed that the total average score and factor scores of SCL-90 in psychiatric outpatients were significantly higher than those in the national norm (p < 0.001) [27].
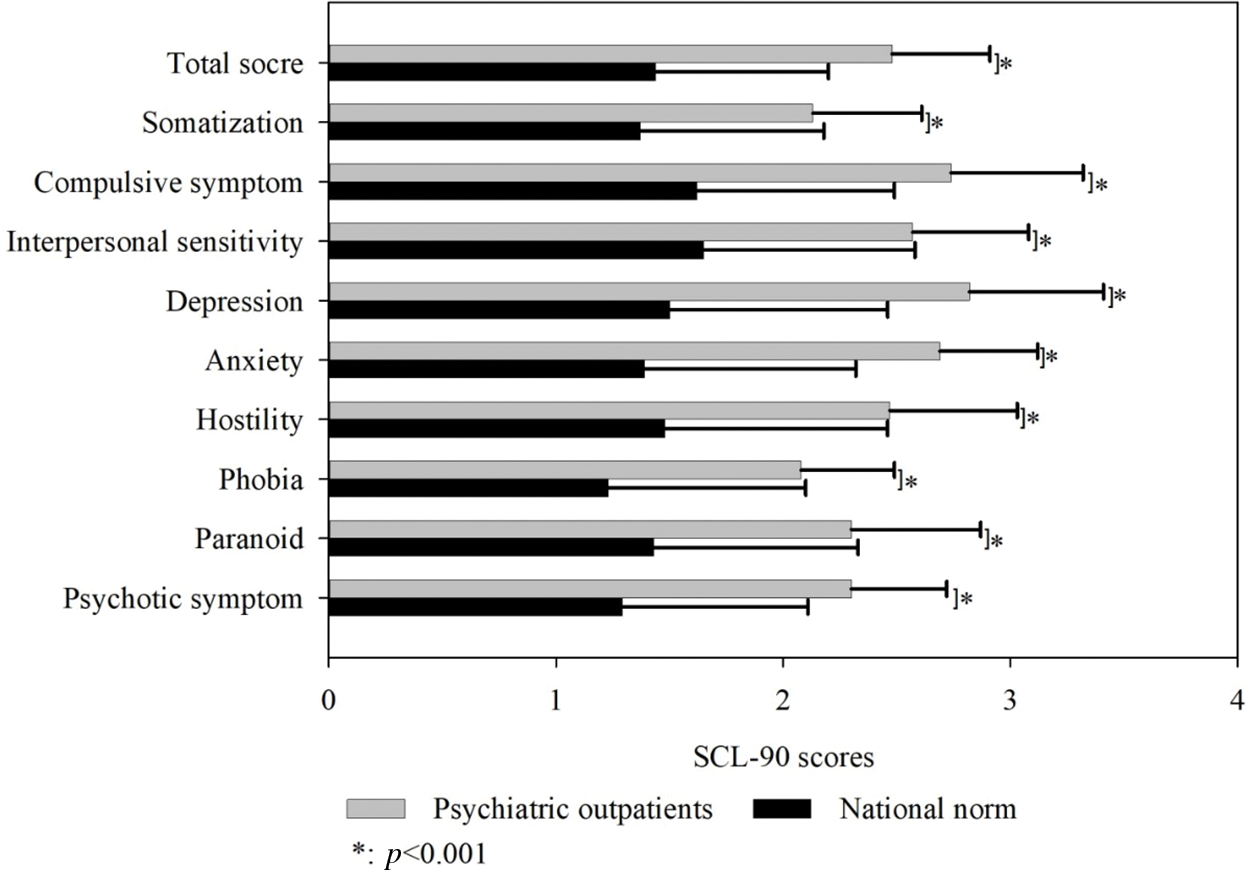
Figure 1: Comparison of SCL-90 scores of psychiatric outpatients with the national norm (
EPQ scores of psychiatric outpatients
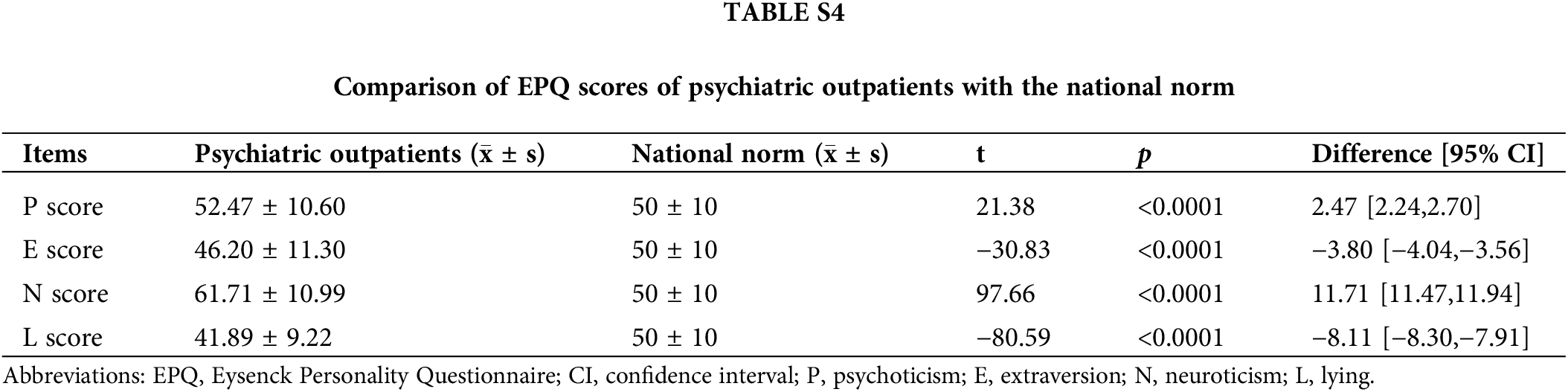
The composition of the scores of each dimension of the EPQ scale for patients is shown in Fig. 2. t-test results comparing EPQ scores of the patients to the national norms are shown in Fig. 3 and Suppl. Table S4. Compared to the national norms, the P and N scores were significantly higher, whereas the E score was significantly lower.
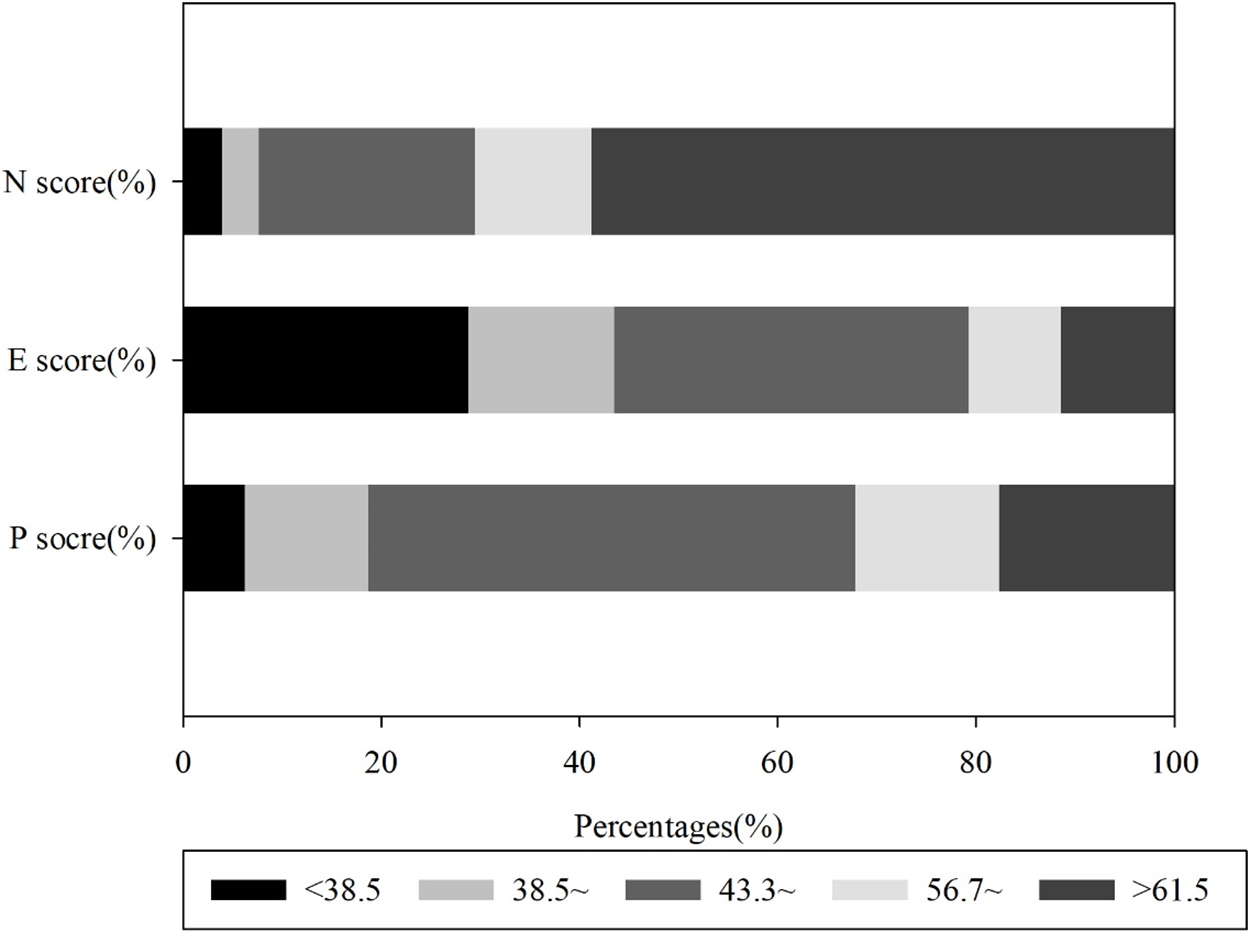
Figure 2: Distribution of EPQ scores in each dimension of psychiatric outpatients.
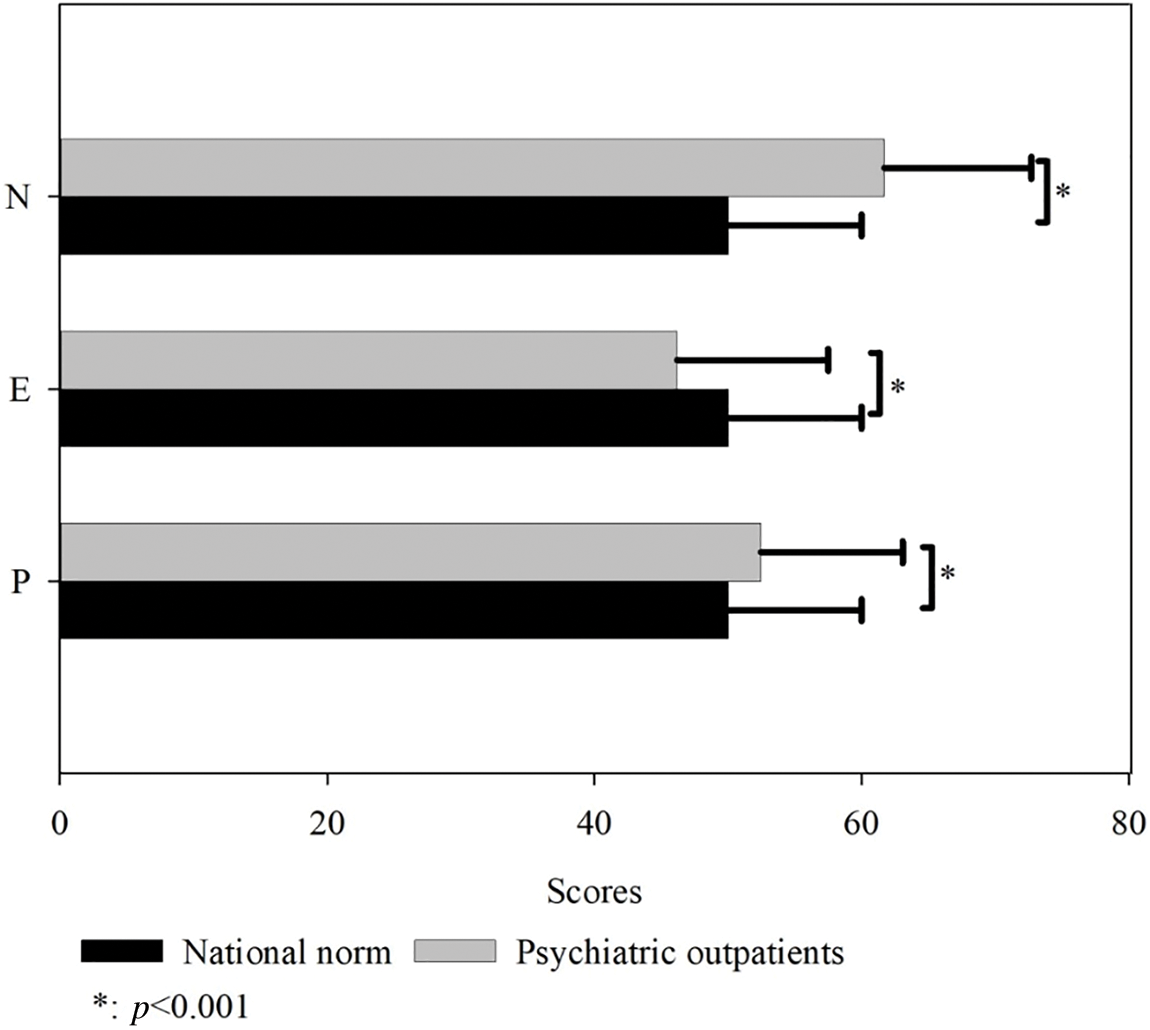
Figure 3: Comparison of EPQ scores of psychiatric outpatients with the national norm (
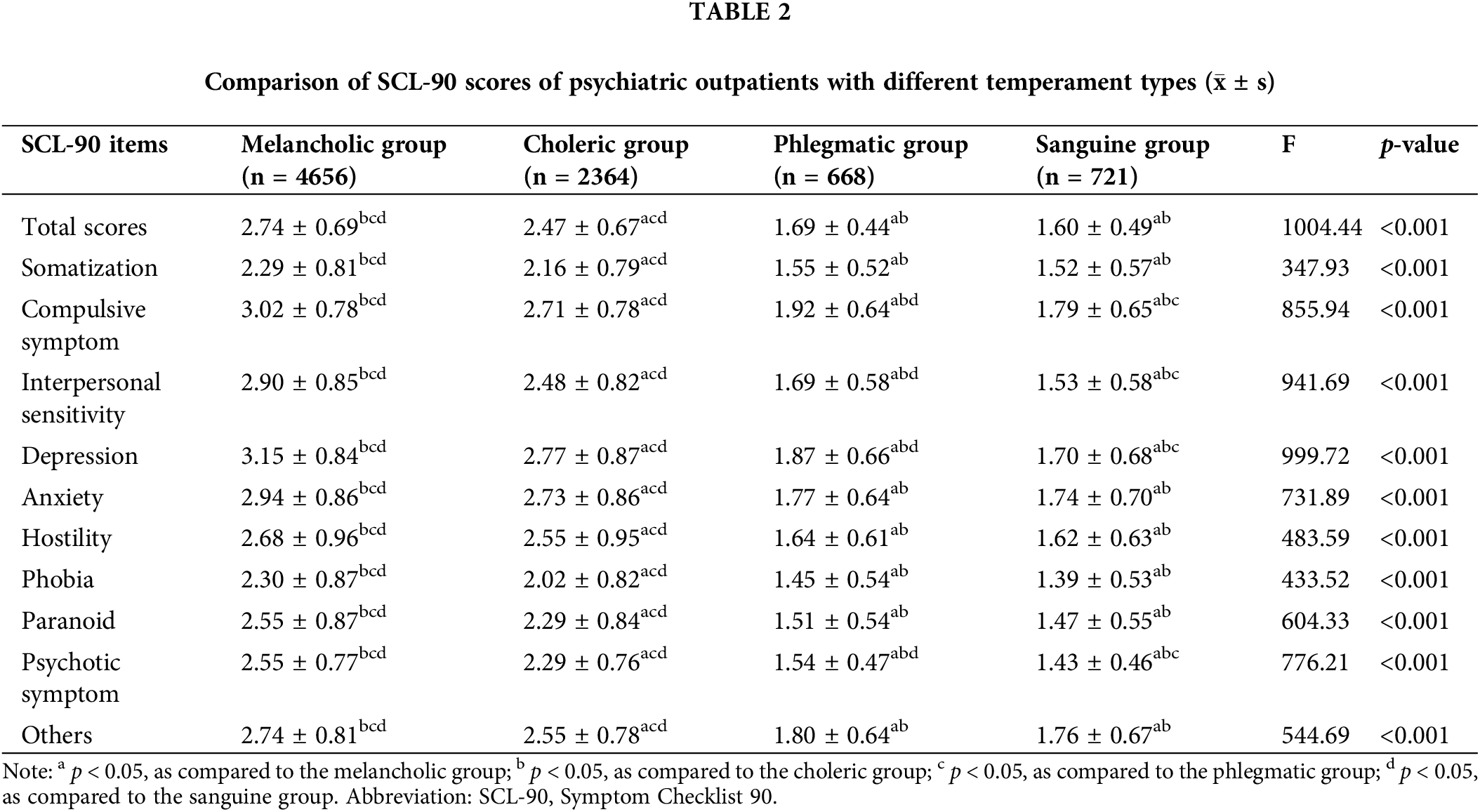
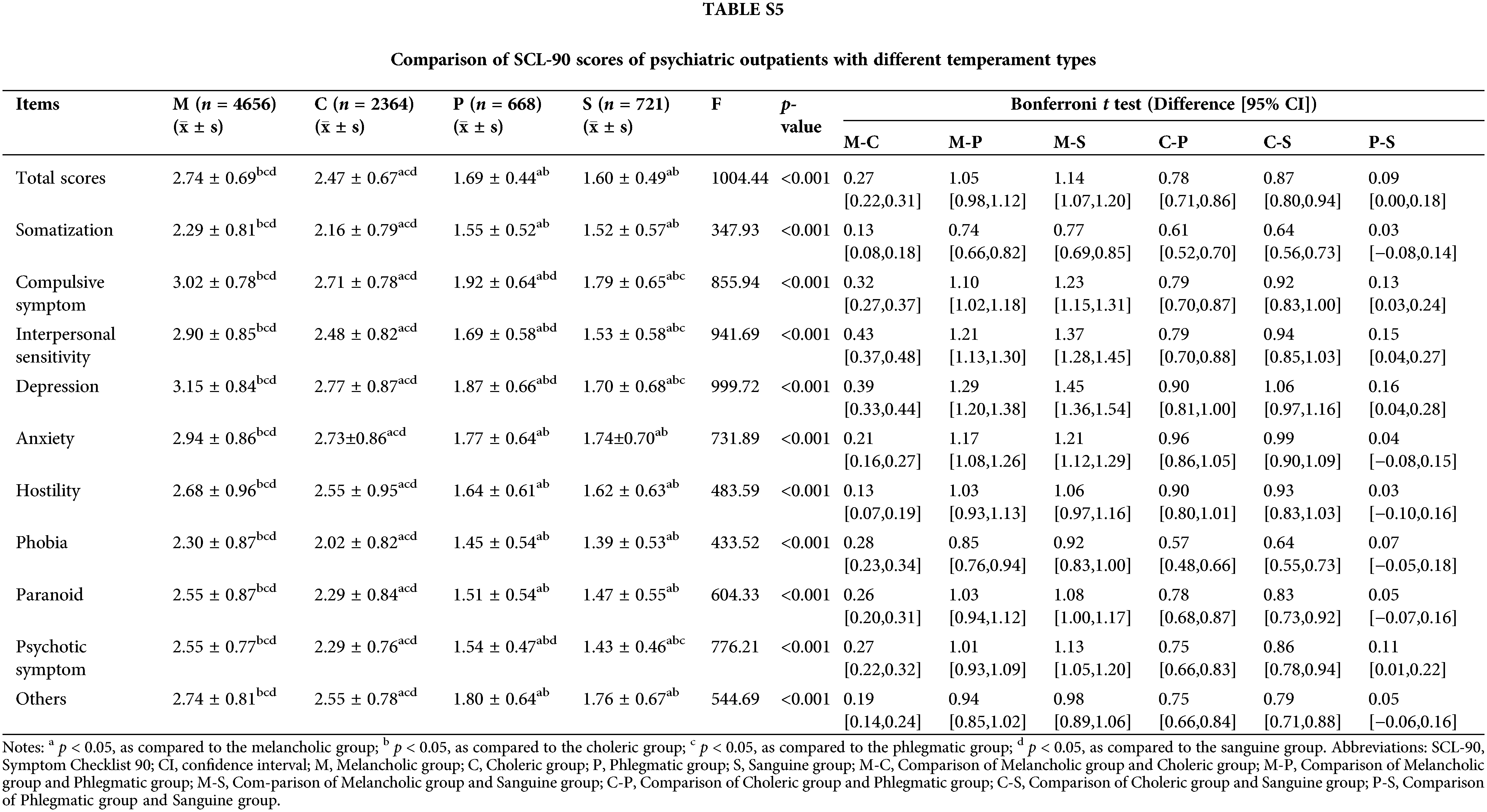
Comparison of SCL-90 scores of psychiatric outpatients with different temperament types
One-way ANOVA showed the statistically significant differences in temperament among the four groups of patients (p < 0.001). Each factor had a higher score in patients with a melancholic temperament as shown in Table 2. Suppl. Table S5 describes the difference and its Bonferroni-adjusted 95% CI between the two groups.
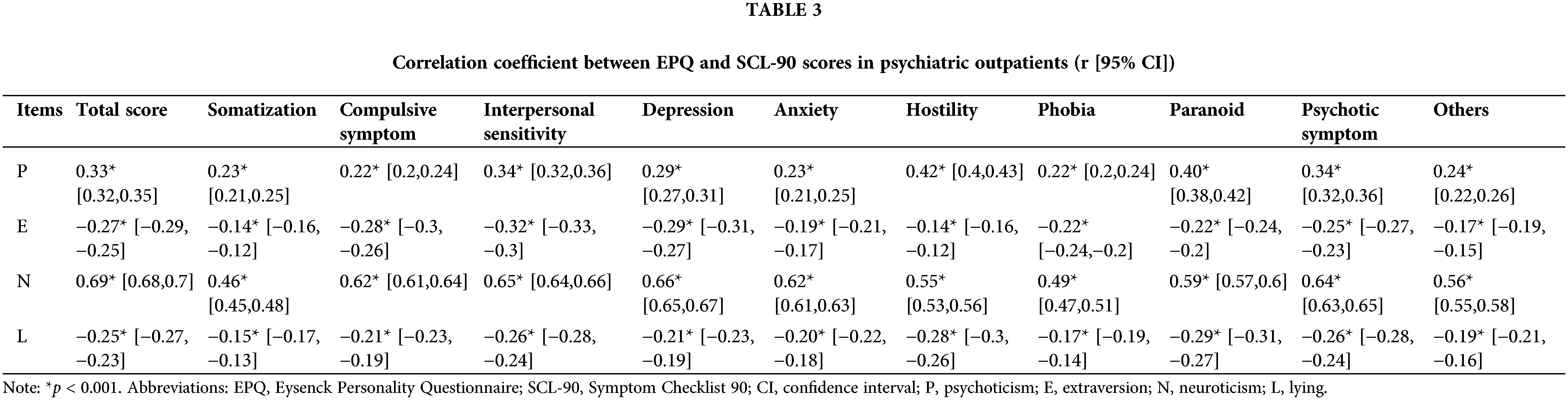
Correlation between EPQ and SCL-90 scores
Pearson’s correlation matrix showed that the total average score and each factor score of SCL-90 were positively correlated with the P score and N score, but negatively correlated with the E score (p < 0.001). The correlation coefficient between the N score and total score, compulsive symptom, interpersonal sensitivity, depression, anxiety, psychotic symptom was 0.69, 0.62, 0.65, 0.66, 0.62 and 0.64, respectively, indicating a strong association. The correlation coefficient between the N score and somatization, hostility, phobia, paranoid and other factors were 0.46, 0.55, 0.49, 0.59, and 0.56, respectively, indicating a moderate association. The correlation between the P score and hostility and paranoia was 0.42 and 0.40, respectively. The correlation coefficients and the 95% CI of EPQ and SCL-90 are shown in Table 3.
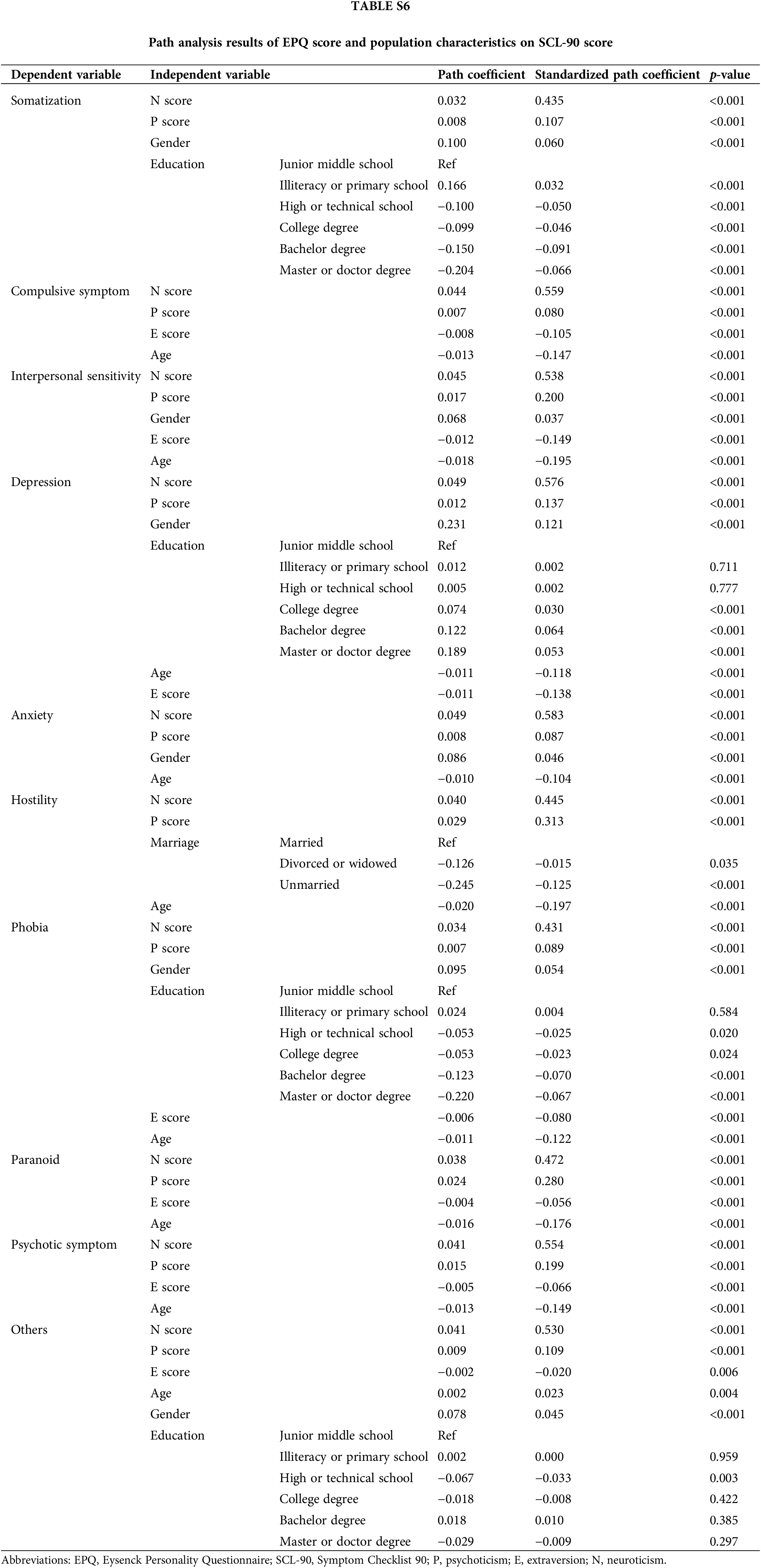
Path analysis of SCL-90 and EPQ scores
The path analysis model was established by considering 10 factors of SCL-90 as endogenous (dependent) variables and 3 factors of EPQ (N, E and P), along with age, gender, marital status and education as exogenous (independent) variables. The model also accounted for the correlation among the 10 factors of SCL-90 and the 3 factors of EPQ. The model fit the data well, with a goodness of fit index (GFI) of 0.9920, an adjusted goodness of fit index (AGFI) of 0.9722, a comparative fit index (CFI) of 0.9938, root mean square error of approximation (RMSEA) of 0.0335, and a standardized root mean square residual (SRMR) of 0.0240.
Supp. Table S6 shows the detailed path coefficients and Fig. 4 shows the path analysis diagram. Due to the large number of paths in the graph, Fig. 4 includes only partial paths with absolute path coefficients greater than or equal to 0.1.
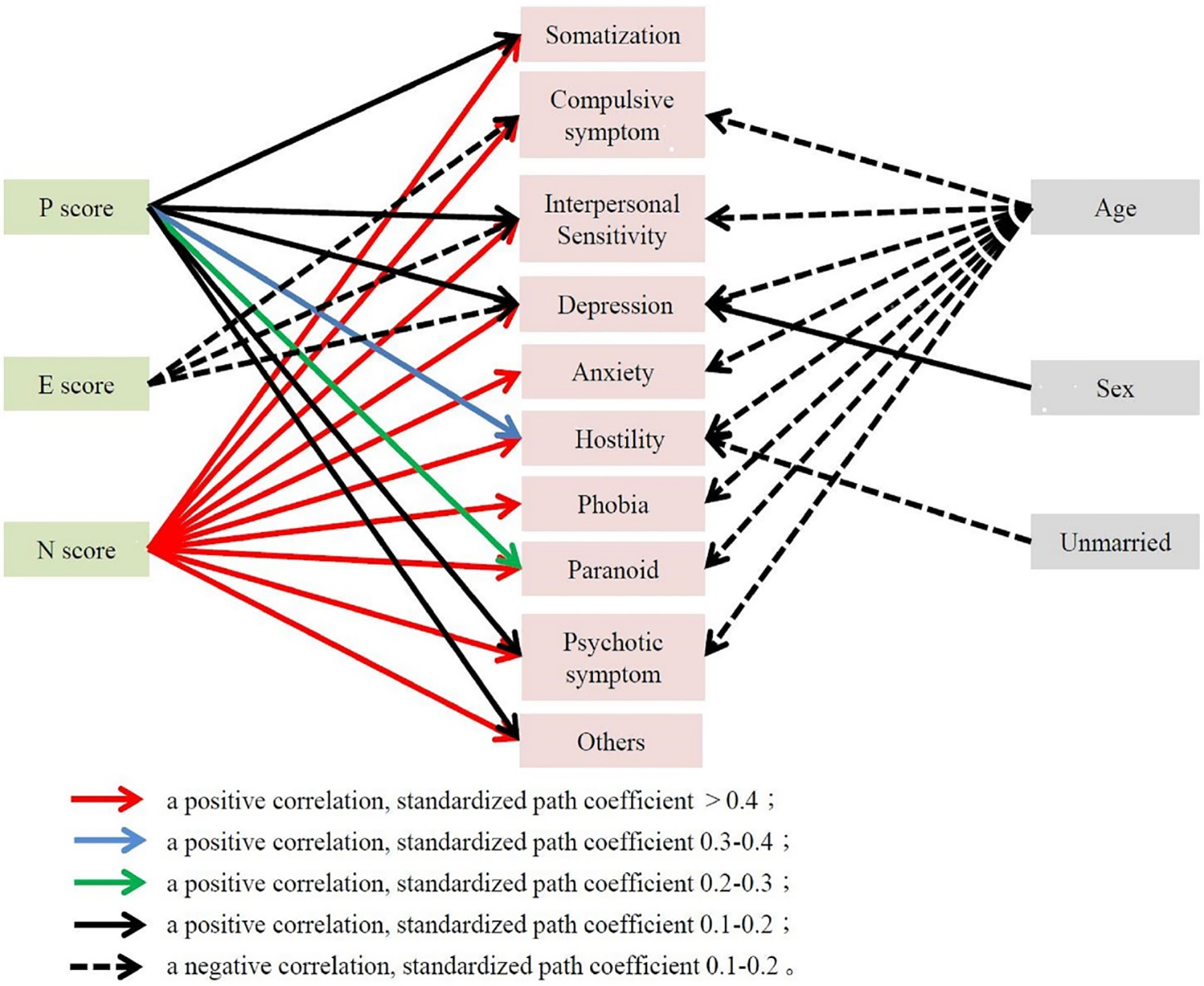
Figure 4: Path analysis diagram of the effects of EPQ scores and population characteristics on SCL-90 scores.
The results revealed that N scores had a significant effect on somatization, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, phobia, paranoia, psychotic symptom and others, with standardized path coefficients were all greater than 0.4. The standardized path coefficient of hostility and paranoia on P scores were 0.313 and 0.280, respectively. Interpersonal sensitivity, depression and obsessive-compulsive symptoms were influenced by E scores, with standardized path coefficients of −0.149, −0.138, and −0.105, respectively.
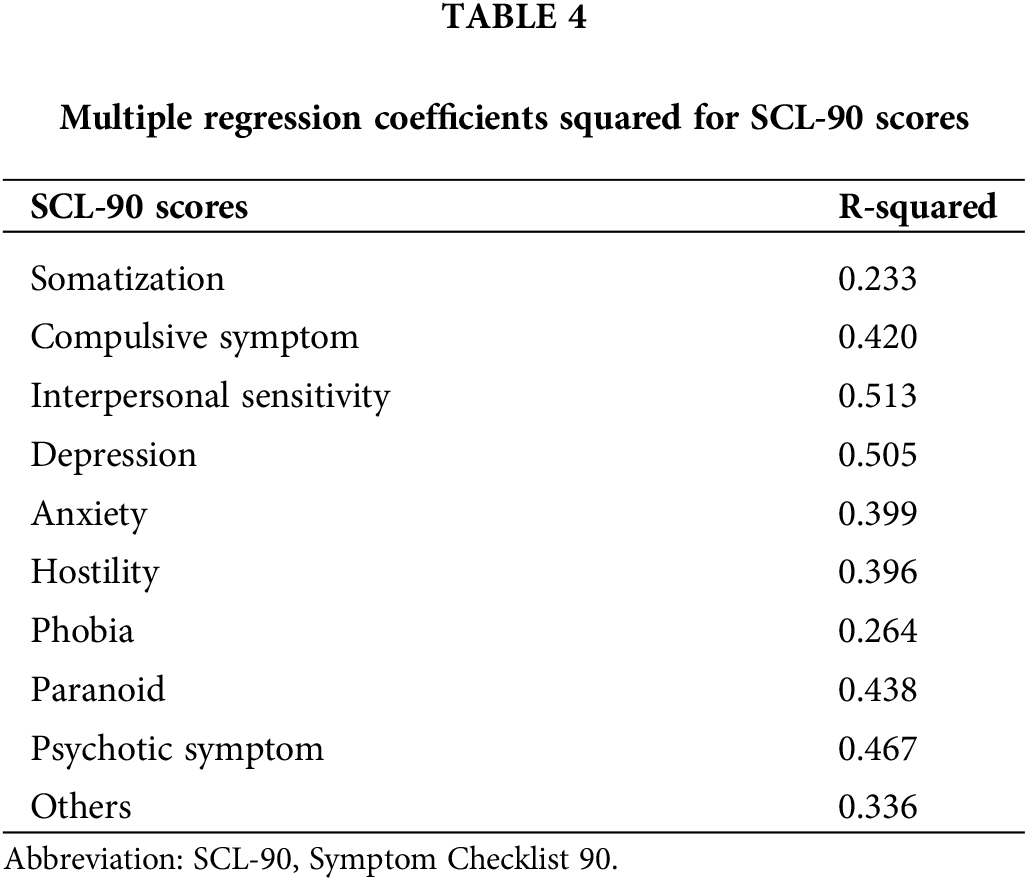
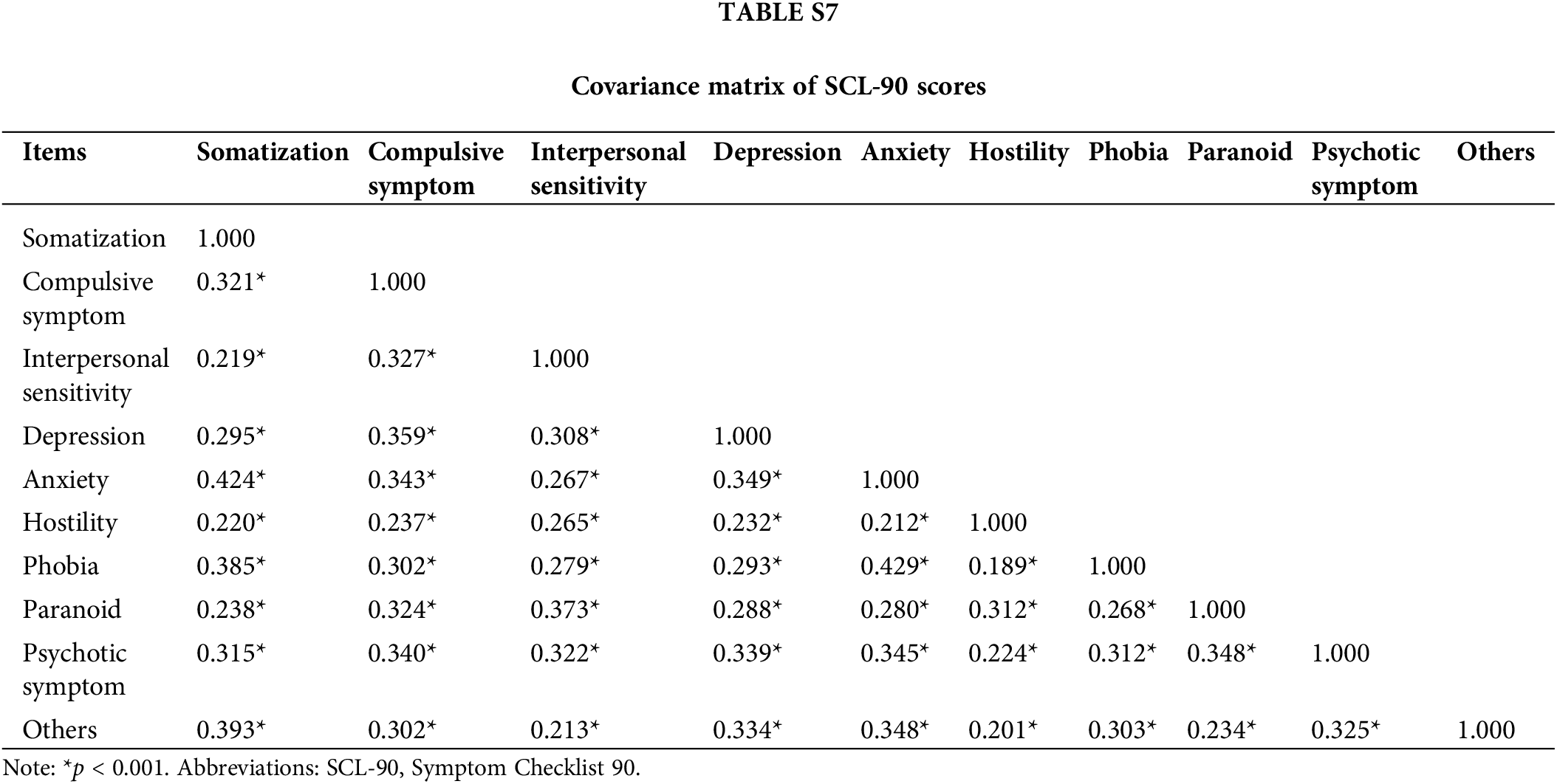
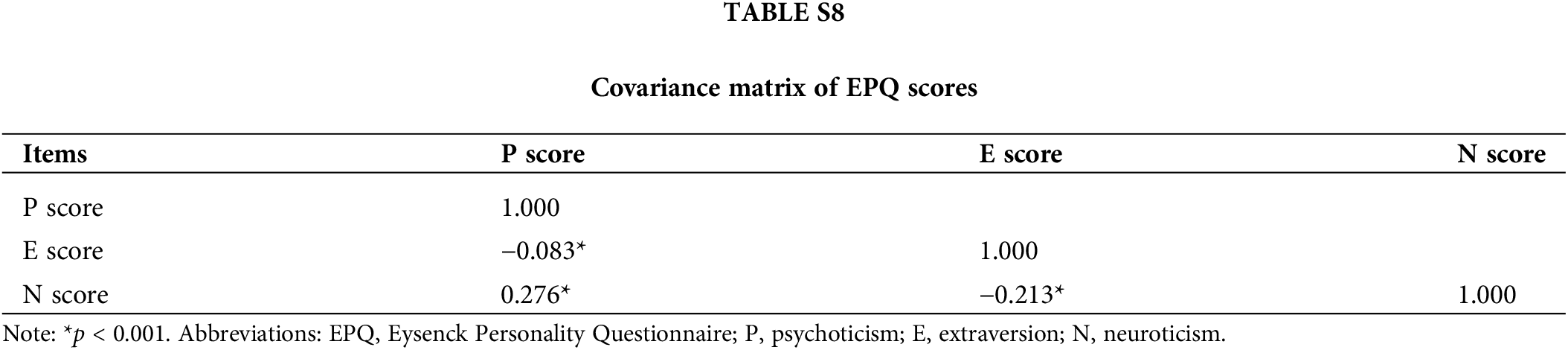
The correlation coefficient matrix of SCL-90 and EPQ indicated that the correlations among SCL-90 factors were strong, whereas the correlations among EPQ dimensions were relatively weak (detailed correlation coefficients are presented in Supp. Tables S7 and S8). Table 4 shows that the path analysis model had a higher explanatory power for interpersonal sensitivity and depression (R2 = 0.513, 0.505) but was weaker for somatization and phobia (R2 = 0.233, 0.264).
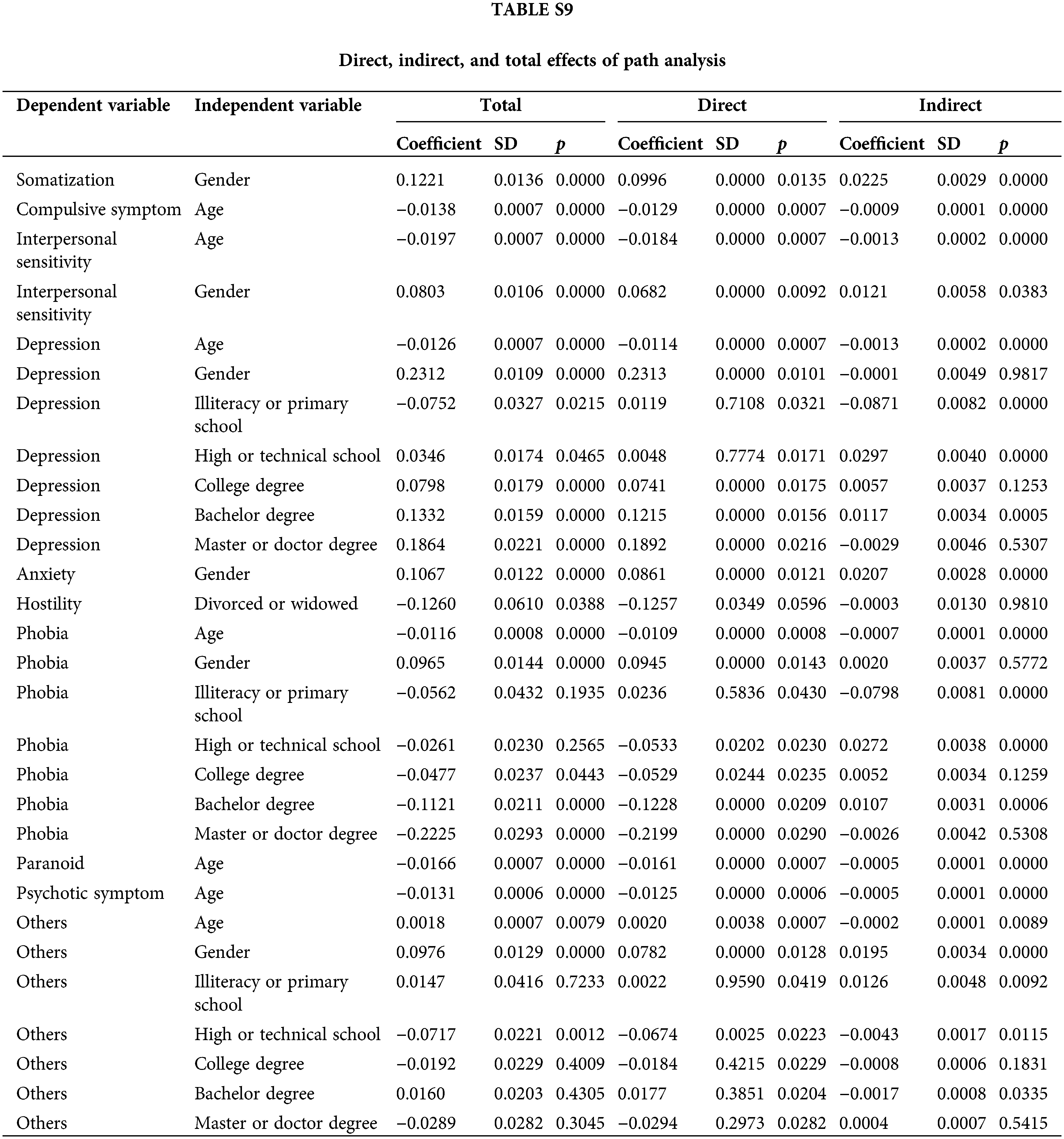
Supp. Table S9 shows the direct, indirect, and overall effects of the parameters influencing the risk of SCL-90. The results indicated that direct effects accounted for more than 80% of the overall effects in all paths, while indirect effects accounted for only a small proportion. The indirect effect of gender on somatization accounted for 18% of the overall effect, while the indirect effect on others accounted for 20%.
Symptom of patients with mental disorders
Perceptible signs of mental disorders usually include pains, fevers, weaknesses, irritability, depression, sleep disorders, cognitive disorders, and other types of dysfunctions [31,32]. In this study, psychiatric outpatients were examined using SCL-90, examine and subjective symptoms were extensively described. We found that the total average score of SCL-90 and the scores of each factor in psychiatric outpatients were significantly higher than the national norm (p < 0.001). This indicated that psychiatric outpatients had a higher tendency in aspects including somatization, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, terror, paranoid ideation, and psychosis.
Somatization is generally considered to be the expression of physical symptoms that cannot be medically explained, reflecting stress and pain, and usually indicating the maladjustment psychological reaction to stress. This connection between somatization and depressive symptoms can explain the association between the two [33]. Defazio et al. [34] reported that the severity of somatization symptoms positively correlated with the score of anxiety and depression scale in patients with functional dyskinesia. Another study observed a high incidence of mental disorders in the Israeli population, with a relatively high rate of depression, generalized anxiety disorder, somatization disorder and neurasthenia [35].
Obsessive-compulsive symptoms are usually characterized by repetitive and distressing thoughts that are difficult to control and can impact social functionality [36,37]. Obsessive-compulsive disorder is often associated with depression, reduced mental function, and even a certain suicidal tendency [38]. Sancak et al. [39] found that more than 40% of schizophrenia patients exhibit apparent obsessive-compulsive symptoms.
Interpersonal sensitivity is internally related to the lack of social functioning. Masillo et al. [40] found that the scores of interpersonal sensitivity measurement and global function: social and role scale of 39 adolescents with ultra-high risk mental state were higher than those of the control group, indicating a worse function in interpersonal consciousness and timidity.
Compulsion and anxiety are often accompanied by hostile thinking [41], with paranoia as the main manifestation.
Relationship between psychological status and personality traits of psychiatric outpatients
In this study, psychiatric outpatients exhibited introversion, psychoticism, and neuroticism. The correlation coefficient between the total average score of the SCL-90 test and each factor score of the EPQ test revealed that neuroticism, introversion, and psychoticism had a significant negative impact on the psychological status of psychiatric outpatients. This finding is consistent with the results of numerous existing studies [42–44]. Psychoticism, neuroticism, and introversion are predictors of adverse psychological reactions [45,46].
Neuroticism had a standardized path coefficient of greater than 0.4 for all factors of SCL-90. Pearson’s correlation matrix showed a correlation coefficient of higher than 0.6 between the N score and total score, compulsive symptom, interpersonal sensitivity, depression, anxiety, and psychotic symptom, indicating a strong association. Reportedly, individuals with high neuroticism scores are more likely to experience moodiness and feelings of anxiety, worry, fear, anger, frustration, envy, jealousy, pessimism, guilt, depressed mood, and loneliness [47]. In addition, neuroticism is thought to be related to shifts in attention and biased negative emotional stimuli, lower stress tolerance, and increased negative emotional experience [48]. More psychological symptoms will result from high neuroticism. Neurotic personality traits make people overly detail-oriented and always strive for perfection, blame others for their worries, which can lead to tensions and conflicts in their relationships [49]. Hippocampal dysfunction is considered the pathological basis of high neuroticism, which may be related to trauma and post-traumatic stress disorder (PTSD), as well as the sensitive psychological state of interpersonal relationships [50]. In the SCL-90 test, the factor “others” reflects the diet and sleep status and shows a strong correlation with the N score. Studies have found that patients with functional dyspepsia have higher N scores in the EPQ test [51]. Furthermore, neurotic symptoms are also associated with the nightmare frequency [52]. The psychological status of patients with depressive and choleric temperaments, characterized by emotional instability, is of greater concern compared to patients with stable temperaments [53]. These studies align with our findings.
People with psychotic personalities are known for their cold and strange demeanor, making it difficult for them to adapt to interpersonal communication and social situations. In addition, these individuals are usually stubborn and tend to be hostile towards people around them, making them more prone to encountering challenging life events [54]. As a result, their psychological state is often at the stress level, leading to impaired cortical function and causing emotional changes [55]. Consequently, patients with psychoticism are more likely to exhibit hostility and obsessive-compulsive symptoms, with standardized path coefficients of hostility and paranoia on psychoticism are greater than 0.280.
Extraversion shows weak negative path coefficients for interpersonal sensitivity, depression and obsessive-compulsive symptoms. Noticeable personality traits associated with extrovert tendency types are highly correlated with interpersonal sensitivity and anxiety symptoms. Patients with mental disorders who have introverted personalities struggle with communication and self-confidence [56]. When faced with social stress, such as pressure, they tend to blame themselves, and their interpersonal sensitivity becomes apparent. In times of adversity, introverts find it challenging to take positive measures, making them susceptible to suffering and feeling overwhelmed by negative emotions [57–59].
In Eysenck’s two-dimensional model of personality theory, temperament is classified into four types based on EPQ scores: depressive temperament, mucinous temperament, bilious temperament, and pluripotent temperament. These classfications reflect the comprehensive influence of the N and E dimensions. Patients with higher phlegmatic and sanguine temperaments tend to have stronger emotional stability and are better equipped to cope with stress. On the other hand, the psychological status of patients with depressive and choleric temperaments, characterized by emotional instability, is more concerning compared to stable patients. This observation aligns with the results of the correlation analysis in our study.
The results of the path analysis revealed that gender indirectly affects symptoms of mental disorders. Previous studies focused on the direct effect of gender on SCL-90 scores and consistently found that female patients tend to score higher than male patients in all aspects of the SCL-90 (p < 0.001). This suggested that female patients are more likely to exhibit severe psychological states, especially concerning depression and somatization, with stronger negative tendencies. These differences may be attributed to physiological and social factors, as women are more susceptible to psychological, social, and occupational impairment, leading to increased psychological stress [60].
In clinical practice, the patient’s neuroticism score reflects their emotional stability, while the psychoticism score helps evaluate their interpersonal interaction. Psychotherapy and/or drug treatments for each patient are selected primarily based on the severity of SCL-90 symptoms. During treatment, physicians consider the EPQ personality characteristics to adjust the way of communicating with the patient, providing targeted psychotherapy. Individuals with prominent psychoticism and neuroticism personality characteristics require heightened attention to psychological symptoms to detect early symptoms and provide appropriate interventions.
This study has a few limitations. First is the absence of data on the clinical classification of patients with mental disorders, as well as the treatment modalities received and the effects of treatment. Second, the validation of personalized treatment plans based on different personality characteristics requires further investigation. Further studies should be conducted to understand the impact of personality traits on the mental health of patients with mental disorders.
This study describes the personality characteristics and SCL-90 scores of psychiatric outpatient patients. Pearson’s correlation analysis shows that mental disorders are associated with personality traits of neuroticism, psychoticism and introversion, particularly with neurotic personality traits being more prominent. Patients with a melancholic temperament exhibit more severe physical symptoms. The path analysis provides a clearer demonstration of the relationship between each dimension of EPQ and the ten items in SCL-90, revealing the direct and indirect effects of age, gender, education, and marital status. To enhance social functioning, appropriate guidance should be provided to individuals with neuroticism, psychoticism, introversion, and depressive temperament at an early stage. Negative emotions should be addressed promptly. Providing necessary and suitable medical and social psychological intervention for individuals with diverse personality characteristics holds great significance in the clinical practice of psychiatry.
Acknowledgement: The authors would like to thank Professor Qiao-Hong Chen at California State University, Fresno, for proofreading this paper.
Funding Statement: This work was supported by a grant from the Health Commission of Nanjing (Grant Number: ZKX22019), China.
Author Contributions: The authors confirm contribution to the paper as follows: conceptualization, Y.Z., B.X., Q.C. and B.C.; formal Analysis, Y.Z., B.X., S.C. and B.C.; writing—original draft preparation, Y.Z.; writing—review and editing, G.M., B.C. and Q.C.; funding acquisition, B.X., Q.C. and B.C. All authors have read and agreed to the published version of the manuscript.
Availability of Data and Materials: The data used to support the findings of this study are available from the corresponding author upon request.
Ethics Approval: The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Nanjing Drum Tower Hospital (2021-096-01).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–50. [Google Scholar] [PubMed]
2. Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. [Google Scholar] [PubMed]
3. Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLoS One. 2015;10(2):e0116820. [Google Scholar] [PubMed]
4. Nuckols CC, Nuckols CC. The diagnostic and statistical manual of mental disorders (DSM-5). Philadelphia: American Psychiatric Association; 2013. [Google Scholar]
5. Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–24. [Google Scholar] [PubMed]
6. Baxter AJ, Charlson FJ, Cheng HG, Shidhaye R, Ferrari AJ, Whiteford HA. Prevalence of mental, neurological, and substance use disorders in China and India: a systematic analysis. Lancet Psychiatry. 2016;3(9):832–41. [Google Scholar] [PubMed]
7. Fagerberg T, Söderman E, Gustavsson JP, Agartz I, Jönsson EG. Thirteen-year follow-up of long-term treated psychotic disorder: personality aspects. Nord J Psychiatry. 2022;76(5):386–93. [Google Scholar] [PubMed]
8. Roberts BW, Mroczek D. Personality trait change in adulthood. Curr Dir Psychol Sci. 2008;17(1):31–5. [Google Scholar] [PubMed]
9. Caspi A, Roberts BW, Shiner RL. Personality development: stability and change. Annu Rev Psychol. 2005;56:453–84. [Google Scholar] [PubMed]
10. Hengartner MP. The detrimental impact of maladaptive personality on public mental health: a challenge for psychiatric practice. Front Psychiatry. 2015;6:87. [Google Scholar] [PubMed]
11. Santesteban-Echarri O, MacQueen G, Goldstein BI, Wang J, Kennedy SH, Bray S, et al. Personality and risk for serious mental illness. Early Interv Psychiatry. 2021;15(1):133–9. [Google Scholar] [PubMed]
12. Ormel J, Oldehinkel AJ, Vollebergh W. Vulnerability before, during, and after a major depressive episode: a 3-wave population-based study. Arch Gen Psychiatry. 2004;61(10):990–6. [Google Scholar] [PubMed]
13. Bonicatto S, Dew MA, Soria JJ, Seghezzo ME. Validity and reliability of symptom checklist ‘90 (SCL90) in an Argentine population sample. Soc Psychiatry Psychiatr Epidemiol. 1997;32(6):332–8. [Google Scholar] [PubMed]
14. Gong Y. Eysenck personality questionnaire revised in china. Inf Psychol Sci. 1984;4:13–20+67. [Google Scholar]
15. Hardt J, Gerbershagen HU, Franke P. The symptom check-list, SCL-90-R: its use and characteristics in chronic pain patients. Eur J Pain. 2000;4(2):137–48. [Google Scholar] [PubMed]
16. Mesa Ríos FJ, Muñoz Mdel C. Screening for psychopathology symptoms in Mexican psychiatry residents. Acad Psychiatry. 2011;35(6):370–72. [Google Scholar]
17. Chen M, Zhou L, Ye L, Lin G, Pang Y, Lu L, et al. Initial adherence by psychiatric outpatients in a general hospital and relevant personal factors. BMC Psychiatry. 2022;22(1):1–9. [Google Scholar]
18. Zhang L, Liu X, Zheng GJ, Zhou L, Lin DY, Wang XD, et al. Eysenck personality and psychosocial status of adult patients with malocclusion. Asian Pac J Trop Med. 2012;5(2):151–6. [Google Scholar] [PubMed]
19. Cao YP, Zhang YL, Chang DF, Yang SC, Wang GQ. Correlations between self-reported symptoms and psychosocial factors of perpetrators with domestic violence in China: a population-based sample. Chin Med J (Engl). 2011;124(4):546–50. [Google Scholar] [PubMed]
20. Menard S. Path analysis. In: Salkind NJ (ed.) Encyclopedia of research design. Thousand Oaks, CA: Sage; 2019. p. 1018–22. [Google Scholar]
21. Chen S, Jiang Q, Zhang Y, Zeng C. Use of symptom checklist 90 for exploring psychological factors among the parents of children hospitalized for burn injuries in Shanghai: a cross-sectional study. Sci Rep. 2022;12(1):21039. [Google Scholar] [PubMed]
22. İnak S, Okray Z. Structural equation model of personality traits, psychopathology, and nonverbal immediacy behavior. Alpha Psychiatry. 2021;22(1):19–24. [Google Scholar] [PubMed]
23. Hafkenscheid A. Psychometric evaluation of the symptom checklist (SCL-90) in psychiatric inpatients. Pers Individ Differ. 1993;14(6):751–6. [Google Scholar]
24. Prinz U, Nutzinger D, Schulz H, Petermann F, Braukhaus C, Andreas S. The symptom-check-list-90-R (SCL-90-R) and the short versions of the SCL-90-R: psychometric analyses of inpatients with mental disorders. Phys Med Rehabil Kurortmed. 2008;18(6):337–43. [Google Scholar]
25. Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale--preliminary report. Psychopharmacol Bull. 1973;9(1):13–28. [Google Scholar] [PubMed]
26. Derogatis L. SCL-90-R: administration, scoring of procedures manual-II for the revised version and other instruments of the psychopathology rating scale series. Towson: Clinical Psychometric Research. 1992:1–16. [Google Scholar]
27. Wang JH, Zhang FG, Song LL. The preliminary analysis for evaluation results of SCL-90 in China normal. Chin J Nerv Ment Dis. 1986;12:260–63. [Google Scholar]
28. Eysenck SB, Eysenck HJ. The questionnaire measurement of psychoticism. Psychol Med. 1972;2(1):50–5. [Google Scholar] [PubMed]
29. Eysenck SB, Eysenck HJ. The measurement of psychoticism: a study of factor stability and reliability. Br J Soc Clin Psychol. 1968;7(4):286–94. [Google Scholar] [PubMed]
30. Howart E. Mood differences between the four Galen personality types: choleric, sanguine, phlegmatic melancholic. Pers and Individ Differ. 1988;9(1):173–5. [Google Scholar]
31. Goossens PJ, Hartong EG, Knoppert-van der Klein EA, van Achterberg T. Self-reported psychopathological symptoms and quality of life in outpatients with bipolar disorder. Perspect Psychiatr Care. 2008;44(4):275–84. [Google Scholar] [PubMed]
32. Häfner H. Psychische krankheit-ein mehrregionenbegriff. Fortschr Der Neurol Psychiatr. 2019;87(12):685–94. [Google Scholar]
33. Dreher A, Hahn E, Diefenbacher A, Nguyen MH, Böge K, Burian H, et al. Cultural differences in symptom representation for depression and somatization measured by the PHQ between Vietnamese and German psychiatric outpatients. J Psychosom Res. 2017;102:71–7. [Google Scholar] [PubMed]
34. Defazio G, Pastore A, Pellicciari R, Pierri G, Gigante AF, Fabio G, et al. Personality disorders and somatization in functional and organic movement disorders. Psychiatry Res. 2017;257:227–9. [Google Scholar] [PubMed]
35. Laufer N, Zilber N, Jecsmien P, Maoz B, Grupper D, Hermesh H, et al. Mental disorders in primary care in Israel: prevalence and risk factors. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1539–54. [Google Scholar] [PubMed]
36. Jansen M, Overgaauw S, De Bruijn ERA. Social cognition and obsessive-compulsive disorder: a review of subdomains of social functioning. Front Psychiatry. 2020;11:118. [Google Scholar] [PubMed]
37. Amianto F, Secci I, Arletti L, Davico C, Abbate Daga G, Vitiello B. Obsessive-compulsive symptoms in young women affected with anorexia nervosa, and their relationship with personality, psychopathology, and attachment style. Eat Weight Disord. 2022;27(3):1193–207. [Google Scholar] [PubMed]
38. Klenfeldt IF, Karlsson B, Sigström R, Bäckman K, Waern M, Östling S, et al. Prevalence of obsessive-compulsive disorder in relation to depression and cognition in an elderly population. Am J Geriatr Psychiatry. 2014;22(3):301–8. [Google Scholar] [PubMed]
39. Sancak B, Özgen Hergül G. Obsessive-compulsive symptoms in schizophrenia patients and their first-degree relatives and the association with subclinical psychotic symptoms. Nord J Psychiatry. 2022;76(4):307–15. [Google Scholar] [PubMed]
40. Masillo A, Valmaggia LR, Saba R, Brandizzi M, Lindau JF, Solfanelli A, et al. Interpersonal sensitivity and functioning impairment in youth at ultra-high risk for psychosis. Eur Child Adolesc Psychiatry. 2016;25(1):7–16. [Google Scholar] [PubMed]
41. Tellawi G, Williams MT, Chasson GS. Interpersonal hostility and suspicious thinking in obsessive-compulsive disorder. Psychiatry Res. 2016;243(3):295–302. [Google Scholar] [PubMed]
42. Sharma SC. Generalized anxiety disorder and personality traits. Kathmandu Univ Med J (KUMJ). 2003;1(4):248–50. [Google Scholar] [PubMed]
43. Rosmalen JG, Neeleman J, Gans RO, de Jonge P. The association between neuroticism and self-reported common somatic symptoms in a population cohort. J Psychosom Res. 2007;62(3):305–11. [Google Scholar] [PubMed]
44. Al-Turkait FA, Ohaeri JU. Relationship of personality traits with anxiety, depressive and ptsd symptomatology and academic performance. Experience with an Arab college student sample. J Med Liban. 2016;64(2):100–6. [Google Scholar] [PubMed]
45. Fullana MA, Mataix-Cols D, Trujillo JL, Caseras X, Serrano F, Alonso P, et al. Personality characteristics in obsessive-compulsive disorder and individuals with subclinical obsessive-compulsive problems. Br J Clin Psychol. 2004;43(4):387–98. [Google Scholar] [PubMed]
46. Zhang F, Baranova A, Zhou C, Cao H, Chen J, Zhang X, et al. Causal influences of neuroticism on mental health and cardiovascular disease. Hum Genet. 2021;140(9):1267–81. [Google Scholar] [PubMed]
47. Thompson ER. Development and validation of an international English big-five mini-markers. Pers Individ Differ. 2008;45(6):542–48. [Google Scholar]
48. Canli T. Functional brain mapping of extraversion and neuroticism: learning from individual differences in emotion processing. J Pers. 2004;72(6):1105–32. [Google Scholar] [PubMed]
49. Widiger TA, Oltmanns JR. Neuroticism is a fundamental domain of personality with enormous public health implications. World Psychiatry. 2017;16(2):144–5. [Google Scholar] [PubMed]
50. Ning L, Guan S, Liu J. Impact of personality and social support on posttraumatic stress disorder after traffic accidents. Med (Baltim). 2017;96(34):e7815. [Google Scholar]
51. Filipović BF, Randjelovic T, Ille T, Markovic O, Milovanović B, Kovacevic N, et al. Anxiety, personality traits and quality of life in functional dyspepsia-suffering patients. Eur J Intern Med. 2013;24(1):83–6. [Google Scholar] [PubMed]
52. Berquier A, Ashton R. Characteristics of the frequent nightmare sufferer. J Abnorm Psychol. 1992;101(2):246–50. [Google Scholar] [PubMed]
53. Junqian M. Stress: friend or enemy?. J Educ Soc Res. 2014;4(6):275. [Google Scholar]
54. Rapinesi C, Kotzalidis GD, Del Casale A, Ferrone M, Vento A, Callovini G, et al. Depressive symptoms, temperament/character, and attention deficit/hyperactivity disorder traits in medical students seeking counseling. Psychiatr Danub.2018;30(3):305–9. [Google Scholar] [PubMed]
55. Sperandeo R, Monda V, Messina G, Carotenuto M, Maldonato NM, Moretto E, et al. Brain functional integration: an epidemiologic study on stress-producing dissociative phenomena. Neuropsychiatr Dis Treat. 2018;14:11–9. [Google Scholar] [PubMed]
56. de Goma IA, Moneva JC. Introvert–extrovert personality types and self-confidence—A case study from Philippines. IRA-Intern J Educ & Multidisc Stud. 2020;16(1):68. [Google Scholar]
57. Grav S, Stordal E, Romild UK, Hellzen O. The relationship among neuroticism, extraversion, and depression in the HUNT study: in relation to age and gender. Issues Ment Health Nurs. 2012;33(11):777–85. [Google Scholar] [PubMed]
58. Lischetzke T, Eid M. Why extraverts are happier than introverts: the role of mood regulation. J Pers. 2006;74(4):1127–61. [Google Scholar] [PubMed]
59. Ku LC, Chan SH, Lai VT. Personality traits and emotional word recognition: an ERP study. Cogn Affect Behav Neurosci. 2020;20(2):371–86. [Google Scholar] [PubMed]
60. Dekker J, Koelen JA, Peen J, Schoevers RA, Gijsbers-van Wijk C. Gender differences in clinical features of depressed outpatients: preliminary evidence for subtyping of depression? Women Health. 2007;46(4):19–38. [Google Scholar] [PubMed]
Supplementary Materials
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools