 Open Access
Open Access
ARTICLE
Break Free from Depression: Implementation and Outcomes of a School-Based Depression Awareness Program
1 Department of Psychiatry, Boston Children’s Hospital/Harvard Medical School, Boston, MA, 02115, USA
2 Boston Public Schools, Boston, MA, 02115, USA
3 Graduate School of Social Service, Fordham University, Bronx, NY, 10023, USA
* Corresponding Author: Amy J. Kaye. Email:
International Journal of Mental Health Promotion 2023, 25(10), 1103-1115. https://doi.org/10.32604/ijmhp.2023.030185
Received 01 April 2023; Accepted 08 June 2023; Issue published 03 November 2023
Abstract
The objective of this study was to evaluate the impact of Break Free from Depression (BFFD), a school-based depression awareness curriculum, in comparison to a wait list control group. A total of 13 eighth grade classrooms participated in either an intervention or control group and completed pre-, post-, and three-month follow-up surveys. Students participating in BFFD (N = 6 classrooms, 166 students) demonstrated enhanced knowledge of and more adaptive attitudes towards depression compared to the control group (N = 7 classrooms, 155 students). Participants in the BFFD intervention also demonstrated increases in their confidence in knowing how to seek help for depression and in their intent to seek this help if needed. Slight decreases were found at a three-month follow-up in all scales except for intent to seek help. BFFD was effective regardless of gender, ethnicity, or identification as a member of the LGBTQ community. There was a delayed effect on measured constructs for Black students with gains apparent at three-month follow-up. The findings demonstrated that BFFD had a small but significant positive impact on students’ knowledge, skills, and attitudes in seeking support for themselves and for others when faced with signs of depression. The implementation of depression awareness curricula in schools hold promise in promoting student mental health, and it is important to consider factors that might have an impact on outcomes.Keywords
The prevention and early intervention of depression among adolescents are critical to their overall health and wellbeing. In 2020, 17% of U.S. adolescents experienced at least one major depressive episode in the past year [1]. Over 31% of youth ages 14–18 reported feeling sad or hopeless almost every day for two or more consistent weeks to the point that they stopped doing some usual activities [2]. The COVID-19 pandemic saw depression prevalence rates increase, with 31% of parents of girls and 18% of parents of boys reporting that they witnessed new or worsening symptoms of depression in their teen [3]. Despite the high prevalence of depressive symptoms, the majority of youth do not receive appropriate treatment [1]. When left untreated, symptoms of depression can become risk factors for self-harm and/or suicidal ideation/attempts [4]. Among youth ages 14–18 years, suicide is the second leading cause of death [2]. Almost 19% reported seriously considering suicide between 2018 and 2019, and 9% made an attempt. These numbers were the highest among females, Black youth, and lesbian, gay, and bisexual youth [5]. Higher levels of depression among youth have been associated with academic challenges, school dropout, physical fighting, interpersonal challenges, substance use, and unemployment [6,7].
Adolescents experience physiological and societal stressors that can contribute to depressive symptoms, including physical health and genetic vulnerabilities, difficulties with family and peers, social determinants of health, and experiences of marginalization and discrimination based on diverse social identities (e.g., race, gender, sexual orientation, religion) [8,9]. For many, school presents additional stressors due to expectations surrounding academic progress, extracurricular involvement, and social pressures. During the school year, adolescents report higher stress levels than adults [10]. With the COVID-19 pandemic, many adolescents faced added stress and depression related to remote learning, isolation, and uncertainty about their post-secondary school options [11]. When this stress goes unmanaged or untreated, it can lead to feelings of overwhelm and depression among adolescents [11].
Prevention and early intervention of depression in schools
Schools provide the opportunity for all students to access early intervention services for depression, as well as a unique place to implement universal social and emotional learning (SEL) curricula to teach young people healthy coping strategies that can prevent the development of mental health challenges like depression. SEL is aimed at ensuring all students have the opportunity to learn, develop, and practice social-emotional competencies found to be critical for enhanced development [12]. The benefits of SEL include improved interpersonal relationships, increased high school graduation rates, and increased readiness for college and post-secondary options [13].
Given that awareness is an important precursor of prevention, there is a critical need for SEL awareness curricula focused on depression. While some universal curricula currently exist, many depression programs for secondary schools are targeted for only a select number of students, too brief to provide all necessary psychoeducation, too long to be feasibly implemented to all students in a school/grade, and/or not yet empirically validated for a wide range of students. While some school-based universal depression curricula have demonstrated reductions in students’ symptoms of depression [14], few have examined their impact on students’ awareness and understanding of depression, including knowledge and skills. This is particularly important for prevention, as many students participating in universal depression prevention programs will not endorse clinical or subclinical symptoms of depression at a given time. Instead, measuring students’ acquisition of knowledge about depression and the skills needed to seek help and cope with symptoms may be measurable outcomes that better apply to all students and are critical to the prevention and early intervention of depression.
Two school-based universal depression programs that have previously explored impact on students’ knowledge and skills are Signs of Suicide (SOS) [15] and the Adolescent Depression Awareness Program (ADAP) [16,17]. Signs of Suicide is a universal program that aims to provide psychoeducation and screen for depression and suicidal thoughts in one session [15]. Program evaluation efforts have indicated significant increases in students’ knowledge and adaptive attitudes about depression and suicide with significant reductions in self-reported suicide attempts [18]. In contrast to SOS’s one session, ADAP is a three-session depression education curriculum [16]. Students participating in this program demonstrated significant gains in knowledge and help-seeking attitudes compared to a control group [16,17]. The current study expands on this literature by investigating both the immediate and longer-term effectiveness of a school-based awareness program that is comprehensive and feasible, Break Free from Depression (BFFD) [19].
Developed by Boston Children’s Hospital Neighborhood Partnerships, BFFD [19] is a four-session manualized school-based universal awareness curriculum designed to be used in grades 8–12. The program goals are to (a) increase adolescents’ knowledge about depression and suicide, (b) enhance their ability to recognize it in themselves and in their friends, (c) increase their skills and strategies for finding help, and (d) achieve high program satisfaction. Each session is 45–60 min and combines didactic presentations, interactive activities, and opportunities for discussion. Sessions are designed to be taught by trained school personnel such as psychologists, social workers, school counselors, adjustment counselors, school nurses, community mental health providers partnered with high schools, other mental health professionals, and health/wellness teachers. The cornerstone of the curriculum is a documentary that focuses on adolescents, not actors, talking about their real struggles with depression and suicide in their own words. BFFD components are outlined in Table 1. A series of training videos are available for free online (https://www.childrenshospital.org/programs/boston-childrens-hospital-neighborhood-partnerships-program/tap-online-trainings/break-free-depression-program), sharing how school personnel can facilitate the curriculum’s four modules in their school or community. Following completion of the online training, individuals have online access to and can download all materials needed to implement the curriculum, including session outlines, handouts, and the documentary.
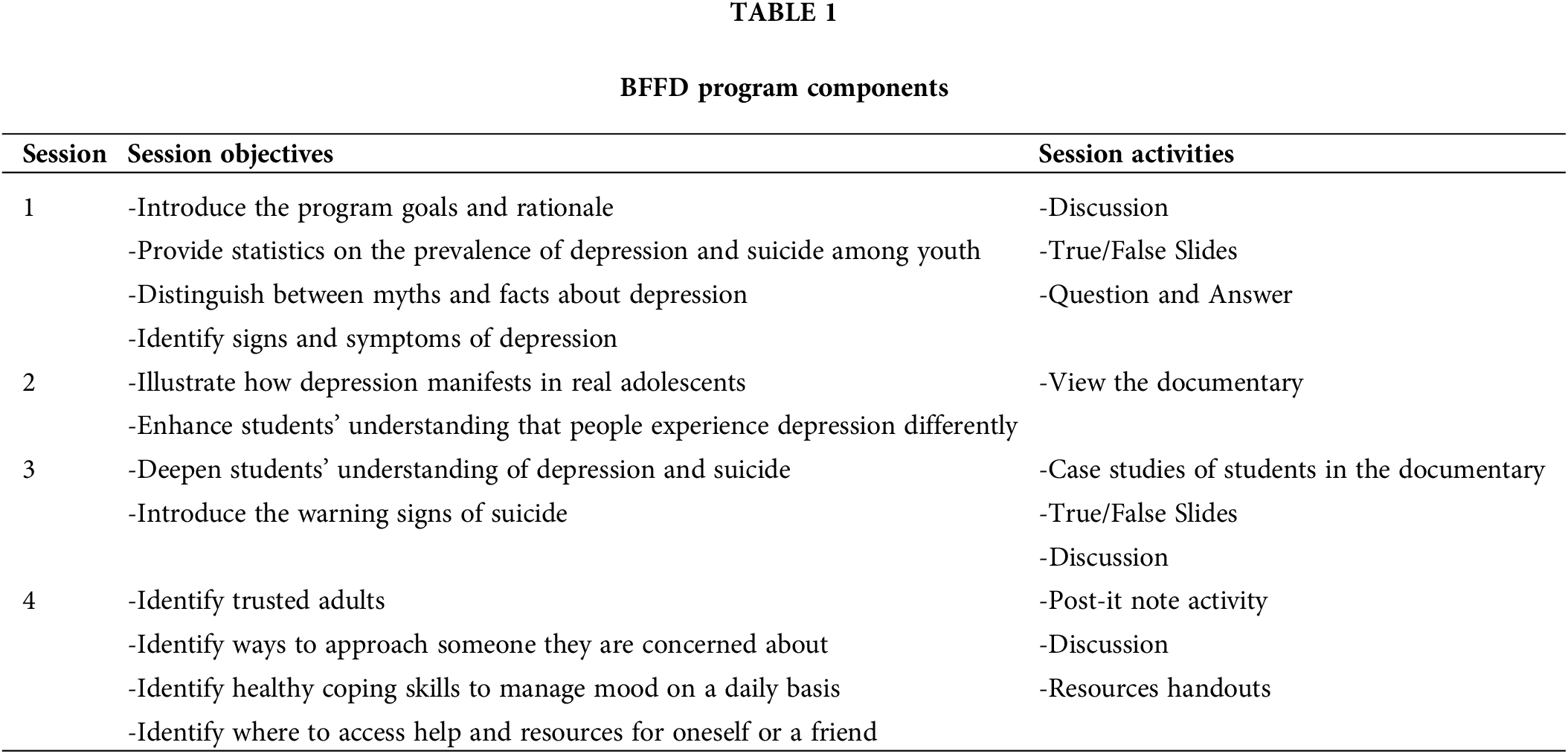
To date, BFFD has reached over 30,000 students in over 30 states. Safety and feasibility evaluations have demonstrated that (1) the curriculum content is accurate, as assessed by content experts; (2) the curriculum content does not induce unintended distress; and (3) the curriculum is feasible to be delivered in a variety of high school settings [19]. Early program evaluations of BFFD have demonstrated that program participation is associated with increases in knowledge about depression and suicide, decreases in stigmatizing attitudes about depression and suicide, and increases in self-efficacy for identifying and seeking support for signs of depression. In addition, at post-survey, program participants demonstrated high student satisfaction, with over 80% of students consistently reporting that they would recommend the curriculum to a friend [19,20]. While these program evaluation efforts have demonstrated BFFD’s initial promise, more rigorous research is necessary in order to build the evidence base of BFFD.
The present study extends the results of previous program evaluations by comparing BFFD to a waitlist control group. The primary goal was to evaluate the impact of the BFFD program on students’ knowledge of and attitudes towards depression, as well as their self-efficacy and behavioral intent for help-seeking as it relates to depression in themselves and others, in comparison to a wait list control group. The secondary goal was to explore participant satisfaction with the program.
The study took place at an urban high school located in Northeastern U.S. In the year the study was conducted, the student body was 45% White, 30% Asian, 13% Hispanic, 8% Black, and 4% identify as other. Although a public school for 7th to 12th grade students, the school requires a competitive score on a standardized examination as part of the admission process. Similar schools are referred to in the literature as high achieving schools (HAS), high performing schools, or selective schools. HAS are defined as schools with high standardized test scores, numerous academic and extracurricular options, and graduates who attend the nation’s “top-tier” universities [21]. Such schools have been found to be nurturing environments for students’ growth, with strong connections between students and teachers, high expectations for student effort, and significant support for post-secondary planning [22]. In addition to the many stressors adolescents face, students attending HAS may face unique stressors associated with academically-advanced course loads, including increased homework and test preparation, increased focus on college readiness and acceptance, increased stress related to family’s academic expectations, and decreased time available for extracurriculars and social activity [23].
While students in HAS report several stressors, they also endorse the ability to cope with these stressors and maintain their well-being with the proper skills and supports [24]. Strategies previously found to be helpful for adolescents in advanced academic courses include seeking family and peer support, maintaining habits that promote physical health, and engaging in extracurriculars and interests outside of academic responsibilities [23,24]. Moreover, coping strategies have been found to moderate the influence of perceived academic stress on life satisfaction and internalizing distress. This public school benefits from access to an array of academic, athletic, and social/extra-curricular enrichment opportunities for its students due to the strong ongoing involvement and financial support of its alumni association. Furthermore, the school has developed a robust academic and mental health support infrastructure. Comprehensive social-emotional supports include universal prevention programs, small group interventions, and a strong partnership with onsite embedded clinicians from the nearby hospital’s Department of Psychiatry & Behavioral Sciences who work as a team with the onsite full time district-employed clinicians (clinical coordinator, school psychologist). Academic supports are also extensive, including peer tutoring, after-school tutoring, teacher office hours, and additional executive functioning workshops and supports.
The current study employs a prospective cohort design with a comparison waitlist control condition. Randomization was not possible due to curricular and schedule considerations. Passive consent letters were sent to guardians of all eighth grade students at the school, and less than 2% of guardians requested that their child opt out of participation in either the intervention, the research surveys, or both. The six eighth grade classrooms scheduled to complete BFFD as part of their curriculum in the fall participated in the Intervention condition, while the seven classrooms completing BFFD as part of their curriculum in the spring participated in the Control condition. The same facilitators (four White females, one Black male) implemented all interventions in the classroom. All facilitators were mental health clinicians (two social workers, two psychologists, one psychology fellow) from the partnering nearby hospital who had completed the online training. Three of the five facilitators are also authors on this paper and supported data collection and evaluation. There are no known systematic differences in the ways in which students were assigned to classrooms or in the way in which classrooms scheduled BFFD implementation. We hypothesized that students enrolled in a classroom assigned to the Intervention condition would score higher on outcomes of knowledge, attitudes, self-efficacy, behavioral intent to seek help, and help-seeking behavior relative to counterparts assigned to a Control classroom.
All student participants in the Intervention group (n = 166) completed a survey at: (a) the beginning of the first BFFD classroom session (i.e., “pre-survey”), (b) the end of the fourth and last classroom session (i.e., “post-survey”), and (c) the beginning of a regular Health classroom session three months following the post-survey (i.e., “follow-up survey”). Participants in the Control group (n = 155) completed the survey at the same time points in their regular Health classroom session. Surveys were the same for both the Intervention and Control groups except that the Control group survey did not include the satisfaction questions (see below for further details about items).
Pre-, post-, and follow-up surveys were matched based on students’ month and day of birth, which they were asked to indicate at each time point. This information was used only to match their surveys at each time point and was not used to match surveys to students’ names. No other identifying information was collected. Results shared in the present study include only those participants with a matching pre-, post-, and follow-up survey.
Pre-, post-, and follow-up survey items for both intervention and control groups
Each survey at pre-, post-, and follow-up included items comprising the following subscales.
Eight true or false items assessed students’ knowledge about depression and suicide (e.g., “Depression is a biological illness;” “Being depressed changes the way you think about solving problems in your life”). The percentage of items answered correctly was calculated to form the Knowledge subscale score.
Attitudes, self-efficacy, and behavioral intent
A 14-item scale with three subscales was designed for use in this study. Within the Attitudes subscale, five questions assessed students’ ideas and beliefs related to depression and suicide (e.g., “Teens who are depressed are just being dramatic”). Within the Self-Efficacy subscale, an additional five questions assessed the extent to which students felt confident that they would know what to do if either they or a friend were depressed or having suicidal thoughts (e.g., “I would know how to talk to a friend who I thought was depressed;” “I know different strategies I can use to help myself deal with sad or stressful situations”). Finally, within the Behavioral Intent subscale, four items assessed the extent to which students would seek support from an adult and/or encourage their friend to do so if they or their friend were depressed or having suicidal thoughts (e.g., “I would tell an adult if I was feeling really down or depressed;” “I would encourage a friend who was feeling really down or depressed to get help from an adult”). On each item within these three subscales, students responded on a 4-point Likert scale ranging from 1 = “Strongly Disagree” to 4 = “Strongly Agree.” Responses to items within each subscale were averaged to form each subscale score.
At the end of the post- and follow-up surveys only, participants responded either “yes” or “no” to the question, “Do you know someone, including yourself, who sought help from an adult because of the Break Free from Depression program?”
At the end of the post-survey in the Intervention condition only, seven additional items assessed students’ satisfaction with the BFFD program. One question assessed overall ratings of the program on a 4-point Likert scale ranging from “Not Good” to “Excellent.” Five items assessed specific aspects of satisfaction (e.g., “The activities and presentation held my attention”) on a 4-point Likert scale ranging from 1 = “Strongly Disagree” to 4 = “Strongly Agree.”
Study staff were trained to be aware of and to briefly assess need for support amongst any Intervention or Control group students who became visibly distressed during any sessions. Based on self-report of study staff following each session, only one student in the Intervention group and no students in the Control group were in need of this type of support. Additionally, the Student Assistance Request Form (SARF) was a required exit ticket at each of the curriculum sessions for the Intervention group and at each of the assessment sessions for the Control group. The SARF provided students an opportunity to seek help directly by requiring them to check one of three boxes indicating whether they would like to talk with someone right away, would like to set up a time to talk to someone, or did not need support at this time. Student support staff at the school in turn followed up with students requesting support. Throughout the course of the study, one student from the Control group and 16 students from the Intervention group received support via SARF follow up.
At the end of each curriculum session, study staff completed a Fidelity Checklist. The Fidelity Checklist outlines each component of each curriculum session as described in the BFFD Manual. Study staff indicated whether the component was implemented as intended, as well as included any notes about adaptations made. Average fidelity across sessions was 99%, with the majority of sessions rated at 100% fidelity. Notes regarding modifications made were largely related to needing to move through content more quickly and review responses to discussion questions as a whole group instead of small groups as a result of time limitations (e.g., when class period was shortened by 5 min due to school schedule) and/or technical challenges (e.g., challenges with a slide projector).
Knowledge, attitudes, self-efficacy, and behavioral intent
To explore the effectiveness of the BFFD program in building knowledge, attitudes, self-efficacy, and behavioral intent, data were analyzed using a Multilevel Random Coefficient Model (MRCM) with each time slope being modeled as a indicator variable in the absence of an intercept term [25]. Initially a series of unconditional models [26,27] were fit to the data for each dependent variable to satisfy prerequisites of multilevel models, in that ample variability within persons existed that necessitated the measurement of individual person slopes. The mean at pre-survey was captured by the intercept term in the model, and two slopes, a linear and a quadratic, were modeled as varying randomly across persons to estimate the trajectories of change for both groups (intervention and control) over time. The first model tested, termed the null or unconditional model, evaluated whether ample variability of individuals over time existed that necessitated the modeling of individual person trajectories over time.
Level-1
Outcomeij = β0j (Grand Mean) + rij
Level-2
β0j = γ00 + u0j with i denoting the number of observations (i.e., pre-survey, post-survey, follow-up survey) for j individuals. Each outcome variable is predicted by an intercept term β0j which is the within-person mean and a residual term rij, which is the error term around that mean estimate. At level-2, the term γ00 reflects the mean of the person scores across the three time points and the error term u0j reflects how that mean estimate γ00 varies across persons (with person being the random effect).
From the unconditional model posited above, several prerequisites to multilevel modeling effects were evaluated. First, the Intra-Class Correlation (ICC) coefficient was estimated [25,26] to test for the presence of variability at each level in the analysis. The coefficient is estimated as the ratio of the between-level variance
Subsequently, the following structural model was fit to the data to test the hypothesis that mean levels of the dependent variables over the three time points are predicted by the intervention.
Level-1
Outcomeij = β0j (Intercept) + β1j (Linear Slope) + β2j (Quadratic Slope) + rij
Level-2
β0j = γ00 + γ01 (Intervention) + u0j
β1j = γ10 + γ11 (Intervention) + u1j
β2j = γ20 + γ21 (Intervention) + u2j
with the terms β0j, β1j and β2j reflecting intercept terms of the pre-survey mean, the linear slope and the quadratic slope, and the terms γ01, γ11, and γ21 reflecting the difference between intervention and control groups. Because all effects due to the intervention were significant, subsequent evaluation of the contribution of the covariates to intervention effectiveness were conducted within the Intervention group only. For example, in order to test the effects of gender on intervention efficacy, the following model was fit to the data.
Effects of intervention by group (e.g., gender)
Level-1
Outcomeij = β0j (Intercept) + β1j (Linear Slope) + β2j (Quadratic Slope) + rij
Level-2
β0j = γ00 + γ01 (Females) + u0j
β1j = γ10 + γ11 (Females) + u1j
β2j = γ20 + γ21 (Females) + u2j
with the terms β0j, β1j and β2j reflecting intercept terms of the pre-survey mean, the linear slope and the quadratic slope, and the terms γ01, γ11, and γ21 reflecting the difference between males and females (termed cross-level interactions). Similar models were utilized for the difference between LGBTQ and non LGBTQ participants and across race and ethnicity for which additional indicator variable terms were included to reflect identification with five groups for which there was a meaningful sample size sufficient for both statistical and practical significance (Black, Asian, White, Multiracial, and Hispanic).
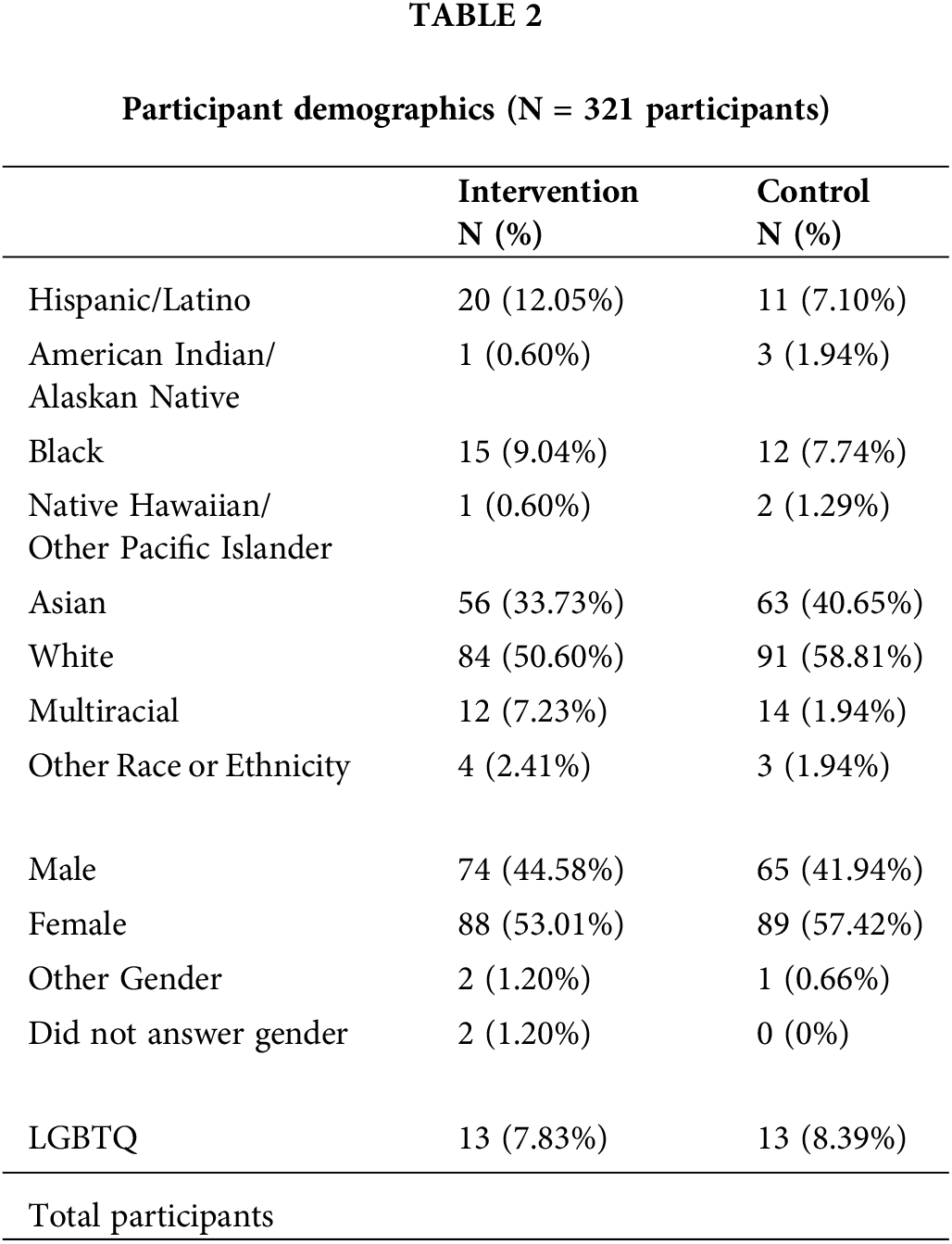
Participants in the present study include a total of 321 eighth grade students (166 in the Intervention group, 155 in the Control group). This represents approximately 83% of the total eighth grade student population at the school. Participant demographics, self-reported at the end of the pre-survey, are presented in Table 2. Participants responded to an item asking them to “check all that apply” with regard to their race and ethnicity. They also responded either “yes” or “no” indicating, “Do you identify as LGBTQ?” There were no statistically significant differences in demographics by condition.
Prerequisite analyses to multilevel models
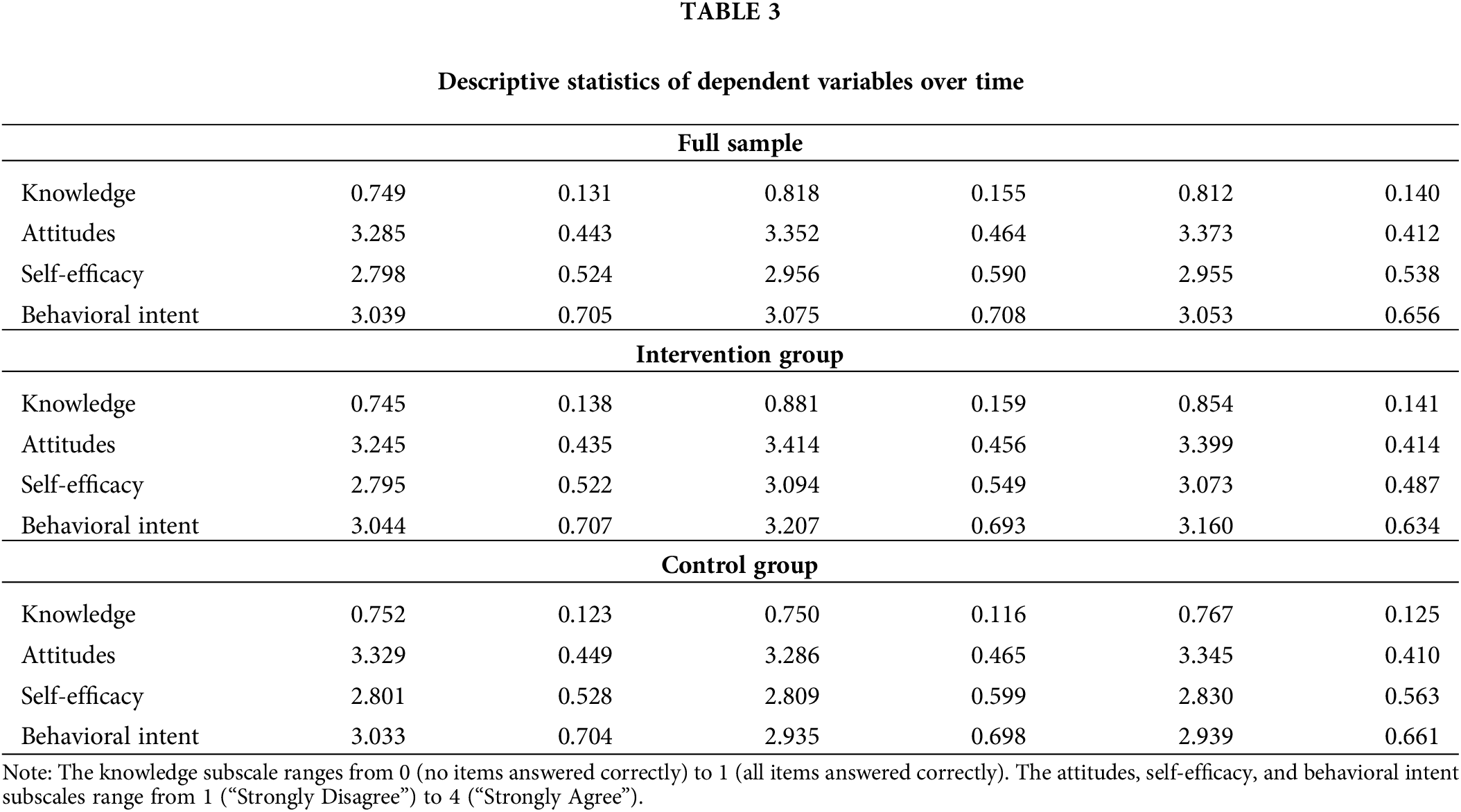
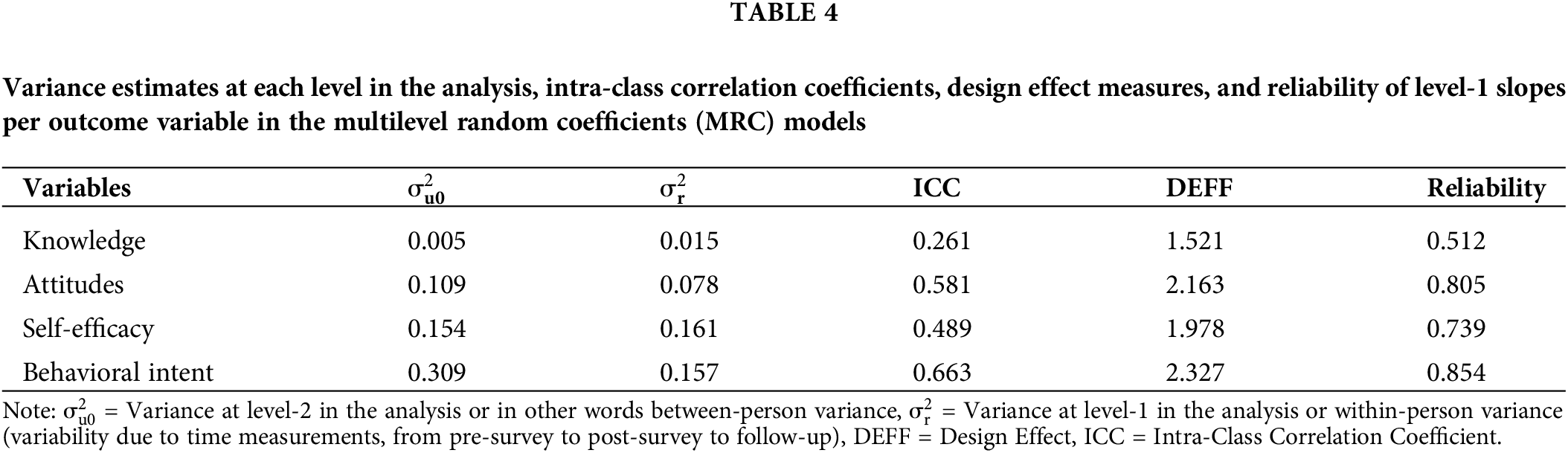
Descriptive statistics for each of the dependent variables: Knowledge, Attitudes, Self-Efficacy, and Behavioral Intent are presented in Table 3. Table 4 presents the results from the prerequisite analyses with the three last column findings indicating that modeling random effects was the proper choice with these data. Specifically, the ICCs suggested the existence of large amounts of variability over time that warranted the need to model individuals’ behavior randomly. The design effect estimates were also close to the value of 2, which, as recommended by Muthen et al. [28], necessitate the modeling of effects as random. Last, reliability was greater than the worrisome estimate of 0.1, suggesting that the trajectories of behavioral change over time varied significantly across individuals, again validating the use of the multilevel approach.
Was the intervention effective overall?
Results indicated that the Intervention group had a significant linear positive trajectory on Knowledge (b = 0.217, p < 0.001; See Fig. 1), Attitudes (b = 0.222, p < 0.001; See Fig. 2), Self-Efficacy (b = 0.441, p < 0.001; See Fig. 3), and Behavioral Intent (b = 0.205, p < 0.05; See Fig. 4), representing a pre- to post-survey improvement in each of these subscales. Maintenance of that significant positive linear slope was attained whenever the quadratic term was not significantly different from zero. This was true only for the Behavioral Intent subscale (b = −0.066, p = 0.120), indicating that the full benefits of the intervention for Behavioral Intent from pre- to post-survey were maintained at follow-up survey. For the Knowledge, Attitudes, and Self-Efficacy subscales, however, the quadratic slope was negative and significant, suggesting a decline in the intervention benefits at the third time point [Knowledge (b = −0.082, p < 0.05); Attitudes (b = −0.080, p < 0.05); Self-Efficacy (b = −0.149, p < 0.05)]. Baseline (i.e., pre-survey) point estimates were contrasted to those at follow-up survey to explore whether this decline reflected a return to baseline levels. Results using chi-square difference tests indicated that despite the decrease from post-survey to follow-up survey, significant differences remained between baseline (i.e., pre-survey) and follow-up survey for the Knowledge [MDIFF = −0.104, χ2 (1) = 58.113, p < 0.001], Attitudes [MDIFF = −0.124, χ2 (1) = 17.458, p < 0.001], and Self-Efficacy [MDIFF = −0.286, χ2 (1) = 33.593, p < 0.001] subscales. In other words, there remained a significant benefit of the intervention on all subscale scores at follow-up survey.
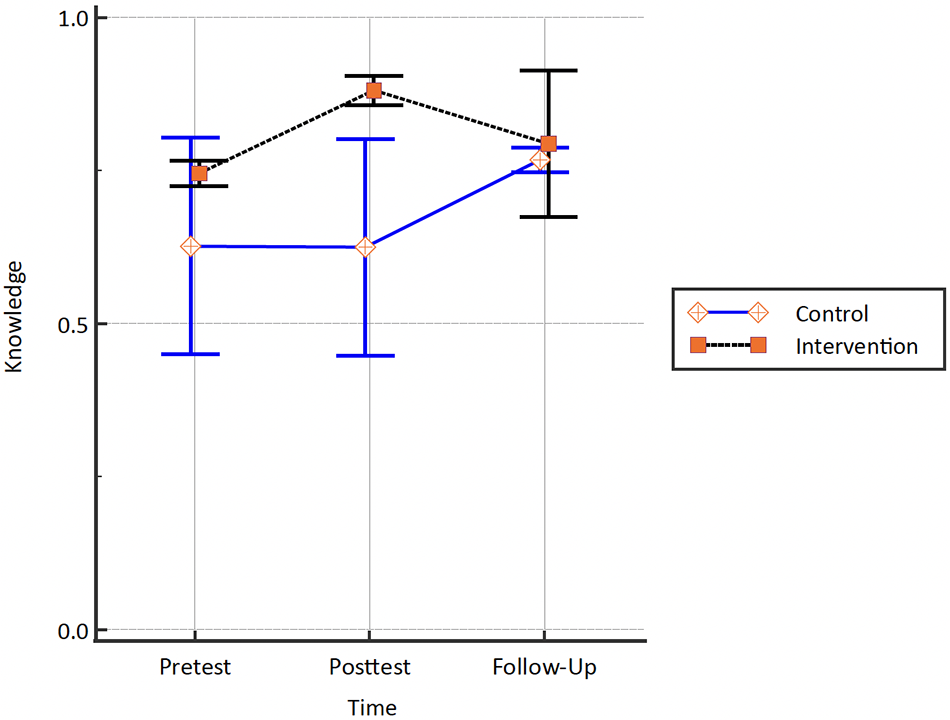
Figure 1: Change in knowledge for intervention and control groups.
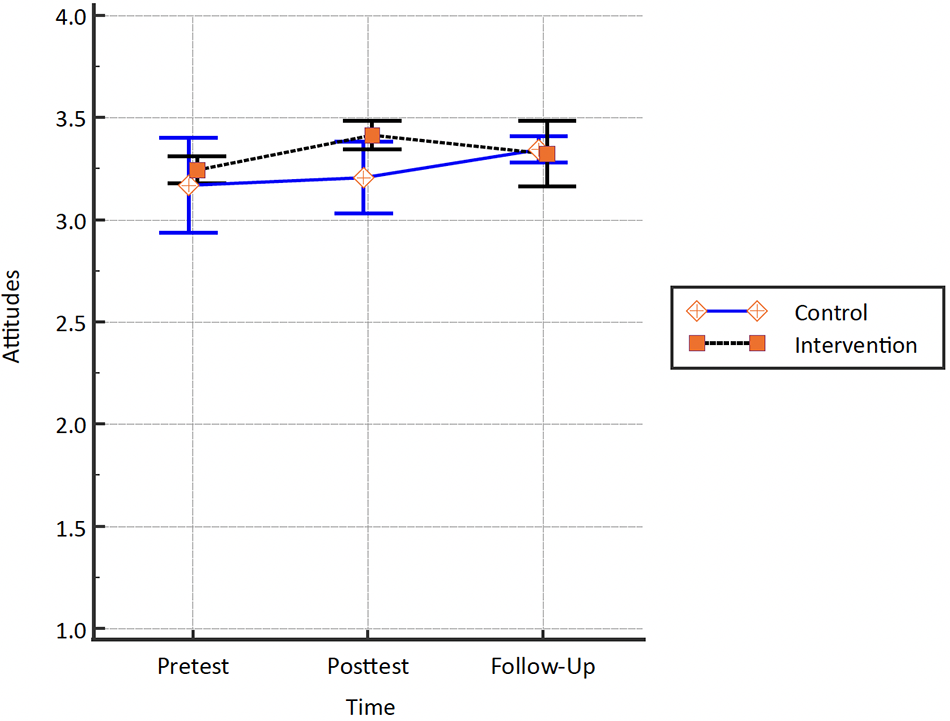
Figure 2: Change in attitudes for intervention and control groups.
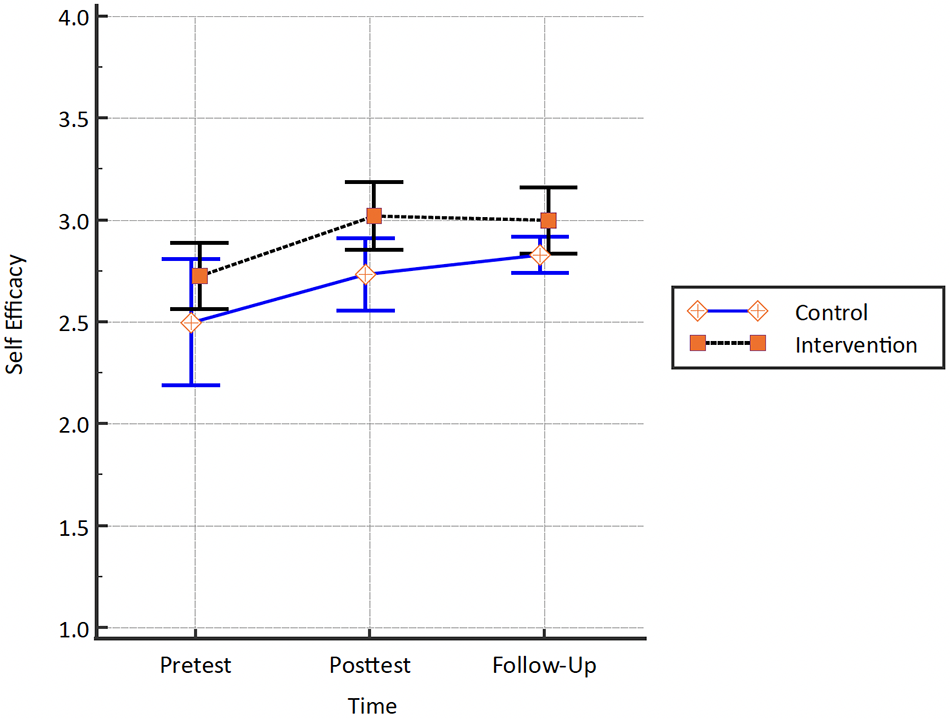
Figure 3: Change in self-efficacy for intervention and control groups.
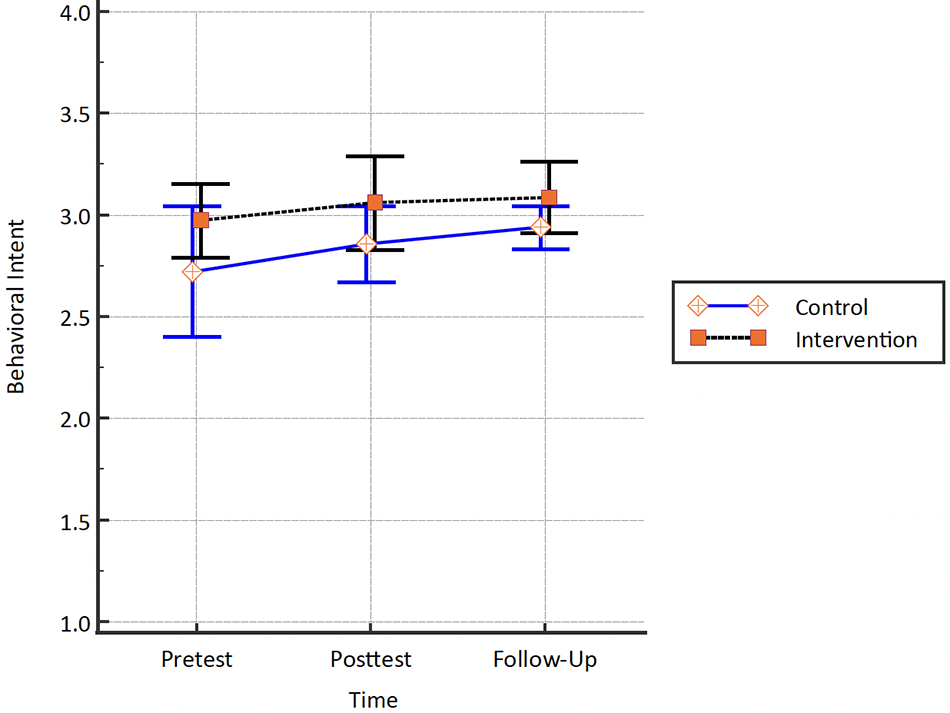
Figure 4: Change in behavioral intent for intervention and control groups.
Was the intervention differentially effective for different groups?
There were no significant differences between males and females across linear or quadratic terms for any of the dependent variables (i.e., Knowledge, Attitudes, Self-Efficacy, Behavioral Intent). The only difference observed in gender was with regard to the intercept term for Attitudes. Specifically, females had significantly higher Attitudes subscale ratings at baseline (i.e., pre-survey) compared to males (Intercept for Females = 3.379, p < 0.001, Intercept for Males = 3.162). There were no significant differences in dependent variables for students identifying as LGBTQ and those not identifying as LGBTQ, with a similar pattern of the curves across the two groups.
For ethnicity, we were cognizant that the small sample sizes would likely evidence themselves with Type-II errors. Results pointed to the support of null hypotheses only across dependent variables, indicating no significant differences between students identifying as Hispanic or Latinx and those identifying as not Hispanic or Latinx.
Several findings emerged with regard to race, which will be important to interpret in the context of the unique nature of the study’s population, including small sample sizes for some racial groups and a unique school context. First, the linear trajectory for Black students’ responses was significantly lower than the trajectory of the rest of the group (b = −0.262, p < 0.05); however, this group had a significant positive quadratic slope. In other words, there was no increase observed on outcomes of interest from pre- to immediate post-survey, but there was a significant increase by follow-up, as if the intervention had delayed effects (b = 0.117, p < 0.05). There was no significant deviation from the grand linear and quadratic slopes described above for any of the other racial groups. However, students identifying as Asian and White reported significantly lower Attitudes ratings at baseline (i.e., pre-survey). A similar pattern was observed for the Behavioral Intent subscale, with students identifying as Asian having significantly lower behavioral intent ratings at the beginning of the study. No other significant differences were evidenced at baseline.
Descriptive statistics and chi-square tests were utilized to explore reports of help-seeking between the Intervention and Control groups. In the Intervention group, 5.45% of participants at post-survey and 4.91% of participants at follow-up indicated that they knew someone, including themselves, who had sought adult support as a result of BFFD. In the Control group, 0.67% at post-survey and 3.27% at follow-up indicated the same. Chi-square tests revealed a significantly higher percentage of students in the Intervention group reported that they knew someone who had received help at post-survey (Χ2 (1, 314) = 4.362, p = 0.037), but this difference was no longer significant by follow-up (Χ2 (1, 316) = 0.203, p = 0.653).
Descriptive statistics were utilized to explore satisfaction with the BFFD program at post-survey for those in the Intervention group. High satisfaction was achieved with average ratings in the “Agree” range (M = 2.68 to 3.26) across items. Highest agreement was seen on items indicating that BFFD is a good way to learn about depression and suicide, that the documentary was a helpful piece of the program, and that participants learned new information about depression and suicide. Most participants rated BFFD overall as “Good” (50.92%) or “Excellent” (14.11%), with fewer students rating BFFD as “Okay” (31.9%) or “Not Good” (3.07%). Table 5 presents participants’ average satisfaction with BFFD for the 163 participants (98% of total sample) who completed these items.
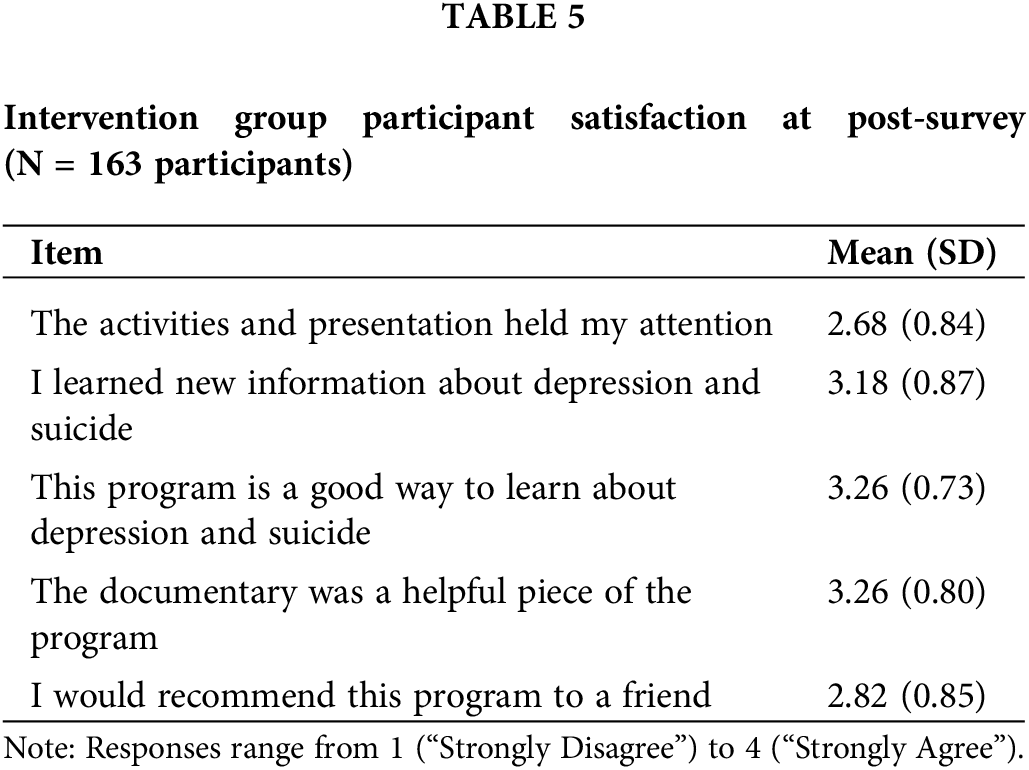
Mann-Whitney U Tests were utilized to explore satisfaction by gender, sexual orientation, ethnicity, and race for those races for which there was a meaningful sample size (i.e., Black, Asian, White, Multiracial). Black students rated their overall satisfaction with BFFD higher (M = 3.15) than students not identifying as Black (M = 2.73) (Mann-Whitney U = 677, z = −0.200, p = 0.045). Results revealed no other statistically significant differences.
Building on emerging evidence generated through open trials of BFFD, this is the first evaluation of BFFD that employs a more rigorous design including a comparison group. Following participation in BFFD, this sample of eighth grade students demonstrated both enhanced knowledge of and more adaptive attitudes towards depression beyond that of a waitlist Control group. Additionally, students demonstrated increases in both their confidence in knowing how to seek help for depression, as well as in their intent to seek this help if needed. Full improvements in intent to seek help persisted into the three month follow up despite declines for knowledge, attitudes, and confidence in knowing how to seek help. Break Free From Depression was equally effective regardless of gender, identification as a member of the LGBTQ community, and ethnicity. With regard to race, there was a reported delayed effect of BFFD on measured constructs for Black students. Although statistically significant improvement in knowledge, attitudes, and help-seeking were not seen at immediate post-survey, improvements were seen by the three month follow-up. It is important to note that some baseline (i.e., pre-survey) differences were seen across gender and race in some of the outcome variables. Despite these differences, differences in the effectiveness of BFFD were not seen. Furthermore, approximately 64% of participants rated BFFD as good or excellent, with participants agreeing, on average, that the program was helpful in learning about depression.
Although changes from pre- to post-survey were statistically significant, they were modest with small effect sizes. There are many possible reasons for this related to the context in which the intervention was provided. In targeting all students within a grade, universal SEL programming like BFFD reaches students with a wide range of baseline knowledge, attitudes, and behaviors related to depression. In doing so, the intervention is broader, and outcomes observed include those who might start at lower baseline levels as well as those who might start at higher baseline levels. On a related note, the school at which this intervention was provided has robust behavioral health supports and suicide prevention programming in order to provide continuity of supports across the time students are enrolled at the school. As such, it is possible that students started at a higher baseline than students might in another school, which could lead to less robust changes over time, or students could be impacted by other systemic factors that limit the magnitude of the impact.
Despite small effects, by examining immediate post-survey results, the findings of the present study build upon the limitations of previous studies that looked only at long term follow-ups. Instead of administering an immediate post-survey, these programs administered post-surveys at a three-month follow-up (i.e., SOS) [30] or a six-week and four-month follow-up to focus specifically on what information was retained (i.e., ADAP) [17,31]. Similar to BFFD, significant increases in knowledge and help-seeking behavior after SOS and ADAP were reported at all follow-up periods [31]. It is possible that the reductions in knowledge, attitudes, and help-seeking self-efficacy three months after participating in BFFD are at least in part due to some expected loss in retention of knowledge and help-seeking strategies that may also have been seen in the other interventions had there been an immediate post-survey. Despite these reductions, increases in intent to seek help, a crucial aspect of prevention, persisted.
Conclusions cannot be drawn based on the differences in baseline and immediate post-survey results between different groups. Here, present findings are compared to past research findings to shed light on further needed exploration into adolescents’ perspectives. When examining differences in knowledge, attitudes, and help-seeking across gender and race compared to previous studies, results from previous studies are mixed and reflect the heterogeneity and intersecting factors that may contribute to adolescents’ views on depression and mental health. Similar to results described in this study, Aseltine and colleagues (2007) found that there were no significant gender differences in reported knowledge and attitudes on depression three months after students participated in SOS. In contrast, findings from the ADAP demonstrated that female students reported higher depression literacy and lower stigma toward depression than male students at the four month follow-up [32]. Previous research has found that females, on average, report less internalized stigma about depression and mental health and therefore may be more willing to seek information about depression and help for themselves or others [33]. This may help to explain the gender difference in baseline scores on attitudes toward depression in the current study, and results from the post-survey are encouraging in suggesting that males’ attitudes toward depression improved to similar levels as females’ following BFFD.
More exploration is needed to better understand the relations between adolescents’ perspectives on depression, depression prevention curricula, and racial identities, among other critical and intersecting aspects of adolescents’ identities and lives. In the current study, Asian and White students reported less adaptive attitudes toward depression at baseline on average, and Asian students, on average, reported significantly lower behavioral intention to seek help than other racial groups. Some previous findings are in line with the current study’s findings [34,35], and some studies have found different results when it comes to attitudes toward depression and seeking help among different racial and ethnic groups [36,37]. It is known that factors impacting adolescents’ attitudes toward depression and help seeking include previous experiences with mental health systems, perceived self-stigma, family and cultural beliefs, and availability of appropriate, accessible, and affirming services [37]. All individuals benefit from programming that reflects their cultural experience and therefore may be more likely to seek support when that support is culturally relevant [38,39]. For example, some previous literature suggests that Asian adolescents and their families may be more likely to seek support from peers, medical professionals, religion, and family [40]. Similarly, Black Americans have previously reported being more likely to seek help from religion and loved ones [41]. Specific examination of mental health and help-seeking intent among Black adolescents at a high-achieving public secondary school found that Black students reported, on average, being unlikely to seek mental health support at school despite 33% reporting internalizing symptoms of distress and only 11% receiving care in or outside of school [42]. Furthermore, findings from Lu [36] indicate that, compared to White adolescents, Black adolescents may express more somatic symptoms of distress and be less apt to report depressive symptoms or suicidal ideation even in the midst of a suicide crisis [36]. Differences in symptom presentation and help seeking behavior among Black adolescents may have impacted students’ experience in BFFD.
Although modest, the present study’s findings suggest the need for ongoing investigation into depression awareness programming like BFFD. Given the emergence and prevalence of depression among youth, schools provide an ideal setting for delivering awareness and prevention programs that can alter or mitigate the trajectory of depression among youth. Several meta-analyses [43,44] have found that prevention programs for depression have a small but significant effect on reducing and preventing depression symptoms compared to the control group. However, less is known about student knowledge and attitudes as they relate to these programs. Examining knowledge and attitudes is critical given that it is not expected that all students participating in universal programs would report depression symptoms at baseline. BFFD’s focus on these outcomes provides evidence of the importance of providing students with knowledge about depression and help-seeking strategies in order to prevent future symptoms of depression and other negative long-term outcomes.
Akin to Werner-Seidler and colleagues’ [44] meta-analysis of school-based depression and anxiety prevention programs for young people, this study’s results contribute to the literature suggesting that school-based awareness programs have the potential to promote youth mental health in important ways. Although the changes from pre- to post-test are modest, similar modest results have been found with regard to other prevention programming, particularly in the areas of suicide and obesity [45,46]. Among the reasons suggested for this include implementation challenges [46], including variability in facilitators, that might have obscured more significant changes from pre- to post-test. As such, further research is needed to better understand potential variability within outcomes. Although variability within outcomes could suggest the need to focus on those populations who are most at risk, it could also be that those who are most at risk might not show those same benefits in the context of a targeted program. Targeted programs have greater accessibility barriers and do not have the same potential to impact other important aspects of the school environment and school climate that might go unmeasured in studies like the present one.
Programs like BFFD have the potential to equip adolescents with tools such as increased awareness and knowledge about the etiology and symptoms of depression, more adaptive attitudes toward depression, and expansion of help-seeking and coping strategies to help them better recognize whether they or a friend are at risk for developing depression. In turn, these acquired skills can help adolescents better navigate how to and who to ask for help when in need, as well as how to best cope with some of the symptoms they experience. In the long term, depression awareness programs such as BFFD can decrease the number of teenagers who are suffering in silence and thus increase the number of youth who are appropriately diagnosed and treated, as research shows that 57% of adolescents experiencing depressive disorders go undiagnosed and untreated [1]. Developing culturally responsive depression awareness and prevention curricula is especially critical for students of color who may be more vulnerable to developing mental health disorders due to experiencing higher levels of external stressors and less likely to receive culturally relevant services [47–50].
In coordination with the evidence base on depression prevention programming more broadly, the findings of this investigation suggest consideration of federal and state wide policies and guidance surrounding the implementation of awareness programs like BFFD in high schools by integrating them in schools’ health and wellness curricula and devoting the time to train health teachers to teach them with fidelity. It is also important to note this in light of the COVID-19 pandemic that has set the stage for the proliferation of risk factors commonly associated with the emergence and development of depressive and anxiety disorders in youth, such as increased social isolation, rise in the number of hours spent using social media, frequent and at times chronic exposure to media as a whole, and multiplication of losses experienced (loss of loved ones to death, loss of routine, loss of hobbies/interest, loss of financial stability, etc.) [51]. Even more so amidst the pandemic, federal and state policies on the school-based integration and implementation of mental health awareness programs such as BFFD are paramount in identifying and helping adolescents in need.
Limitations and future research
There are some limitations that highlight the importance of future research in this area. First, due to logistical barriers, classrooms were not randomly assigned to the intervention or control group within the present study. In turn, there is a possibility that there were differences between the Intervention and Control groups that were not randomly distributed and thus resulted in systematic differences in these groups that could artificially inflate and/or obscure the impact of the intervention. For example, the classrooms that implemented BFFD in the Fall as part of the Intervention group did so due to their willingness to modify their schedule to integrate BFFD earlier in the year. It could be that those Health teachers in the Intervention group were in some way different than those in the Control group (e.g., more or less comfortable with mental health topics, more or less busy), which could have an impact on the results.
Additionally, we recognize that the student and school sample used in this study is unique. Given the nature of the enrollment and admission process at the HAS where the study was conducted, the student population and the overall school experience may not be reflective of the general student population, although literature suggests that a depression awareness curriculum may be important for students in HAS settings [52]. Furthermore, the participant sample consisted of a disproportionately high percent of White and Asian students. Over half of the student sample population identified as White compared to less than twenty percent who identified as Black and Latinx. These demographics are not representative of the greater school district to which the school belongs, making broader implications difficult.
Finally, in order to further strengthen the cultural relevance of depression awareness and prevention curricula, it will be critical to help adolescents understand how culture, as defined by the set of values, attitudes, beliefs, and behaviors internalized from one’s family and ethnic background [49,50], can have a significant influence on the manifestation of depression and on how individuals cope and navigate these symptoms. It could be that limitations in the cultural significance could also be impacting the magnitude of the results. Programs should aim to develop materials that are optimally culturally relevant to Black, Indigenous, People of Color (BIPOC) students in order to help increase their effectiveness and satisfaction with BIPOC youth. Depression curricula must address the impact of racial trauma on BIPOC students’ vulnerability to develop depressive disorders. For example, didactic materials could be modified to include information demonstrating how the impact of racial trauma stemming from accrued experiences of micro-aggressions, discrimination, systemic racism, racial profiling, and stereotype threat can erode the mental well-being and self-esteem of BIPOC individuals by increasing their vulnerabilities to symptoms such as hypervigilance to threat, flashbacks, nightmares, avoidance, suspiciousness, and somatic expressions such as headaches and heart palpitations [53]. Moreover, adding a section that engages students to learn and discuss different strategies to best navigate and heal from racial trauma could also be quite beneficial to the emotional well-being of BIPOC students. Future research should also examine whether there is a significant difference in the effectiveness and significance of an awareness curriculum for BIPOC students when these aforementioned elements are added and made salient in the program.
Despite these limitations, current study findings provide insight into depression awareness curricula and important evidence of BFFD as a valuable school-based awareness program. The findings of this study indicate how mental health prevention programs should aim to increase student knowledge, adaptive attitudes, and help-seeking as a means to promote mental health awareness and coping strategies among young people in a school setting.
Acknowledgement: We are incredibly grateful to the students, educators, school professionals, administrators, and the entire school community for the time, energy, and resources dedicated to this effort. Their steadfast dedication to promoting mental health is what makes efforts like this one successful. We also thank the additional clinicians who implemented the intervention described in this paper, Lisa Katerman Dean, MSW, LICSW and Isaac Woods, PhD, as well as our research data coordinators who supported literature review, data collection, and data entry over the years, Maureen Burns, Vincent Donofrio, Madeline Ganz, Rachel Takes, and Sarah Weidman.
Funding Statement: Finally, we thank the Sidney A. Swensrud Foundation for their generous financial support without which we would not have been able to do this work.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: A. Kaye, V. Prosper, V. Pejic, K. Capraro, A. Ross, K.M. Dennery, D. DeMaso; data collection: A. Kaye, V. Pejic, K. Capraro; analysis and interpretation of results: G. Sideridis, A. Kaye, K. Moffa, V. Pejic, K. Capraro; draft manuscript preparation: A. Kaye, V. Prosper, K. Moffa, V. Pejic, K. Capraro, G. Sideridis. All authors reviewed the results, edited the draft manuscript, and approved the final version of the manuscript.
Availability of Data and Materials: The data and materials underlying this article will be shared on reasonable request to the corresponding author.
Ethics Approval: This study was approved by the Boston Children’s Hospital Institutional Review Board (IRB).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: results from the 2020 national survey on drug use and health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Available from: https://www.samhsa.gov/data/. [Accessed 2021]. [Google Scholar]
2. Centers for Disease Control and Prevention. Youth risk behavior survey: Data summary and trends report 2009–2019. Available from: https://www.cdc.gov/healthyyouth/data/yrbs/pdf/YRBSDataSummaryTrendsReport2019-508.pdf. [Accessed 2020]. [Google Scholar]
3. C.S. Mott Children’s Hospital. How the pandemic has impacted teen mental health. Available from: https://mottpoll.org/reports/how-pandemic-has-impacted-teen-mental-health. [Accessed 2021]. [Google Scholar]
4. Carballo JJ, Llorente C, Kehrmann L, Flamarique I, Zuddas A, Purper-Ouakil D, et al. Psychosocial risk factors for suicidality in children and adolescents. Eur Child Adoles Psy [Internet]. 2020;29(6):759–76. doi:https://doi.org/10.1007/s00787-018-01270-9. [Google Scholar] [PubMed] [CrossRef]
5. Ivey-Stephenson AZ, Demisse Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, et al. Suicidal ideation and behaviors among high school students—youth risk behavior survey, United States, 2019. Morb Mortal Wkly Rep Suppl [Internet]. 2020;69(1):47–55. doi:https://doi.org/10.15585/mmwr.su6901a6. [Google Scholar] [PubMed] [CrossRef]
6. Kim YK, Sanders JE, Makubuya T, Yu M. Risk factors of academic performance: experiences of school violence, school safety concerns, and depression by gender. Child Youth Care For [Internet]. 2020;49(5):725–42. doi:https://doi.org/10.1007/s10566-020-09552-7. [Google Scholar] [CrossRef]
7. Quiroga CV, Janosz M, Bisset S, Morin AJS. Early adolescent depression symptoms and school dropout: mediating processes involving self-reported academic competence and achievement. J Educ Psychol [Internet]. 2013;105(2):552–60. doi:https://doi.org/10.1037/a0031524. [Google Scholar] [CrossRef]
8. Saleem FT, Anderson RE, Williams M. Addressing the myth of racial trauma: developmental and ecological considerations for youth of color. Clin Child Fam Psych [Internet]. 2020;23(1):1–14. doi:https://doi.org/10.1007/s10567-019-00304-1. [Google Scholar] [PubMed] [CrossRef]
9. Rice F, Eyre O, Riglin L, Potter R. Adolescent depression and the treatment gap. Lancet Psychiatry [Internet]. 2017;4(2):86–7. doi:https://doi.org/10.1016/S2215-0366(17)30004-4. [Google Scholar] [PubMed] [CrossRef]
10. American Psychological Association. Stress in America: are teens adopting adults’ stress habits? Available from: https://www.apa.org/news/press/releases/stress/2013/stress-report.pdf. [Accessed 2014]. [Google Scholar]
11. American Psychological Association. Stress in America 2020: a national mental health crisis. Available from: https://www.apa.org/news/press/releases/stress/2020/sia-mental-health-crisis.pdf. [Accessed 2020]. [Google Scholar]
12. Collaborative for Academic, Social, and Emotional Learning. Fundamentals of SEL. Available from: https://casel.org/fundamentals-of-sel/. [Google Scholar]
13. Greenberg MT, Domitrovich CE, Weissberg RP, Durlak JA. Social and emotional learning as a public health approach to education. Future Child [Internet]. 2017;27(1):13–32. doi:https://doi.org/10.1353/foc.2017.0001. [Google Scholar] [CrossRef]
14. Feiss R, Dolinger S, Merritt M, Reiche E, Martin K, Yanes JA, et al. A systematic review and meta-analysis of school-based stress, anxiety, and depression prevention programs for adolescents. J Youth Adolesc [Internet]. 2019;48(9):1668–85. doi:https://doi.org/10.1007/s10964-019-01085-0. [Google Scholar] [PubMed] [CrossRef]
15. Aseltine RH, DeMartino R. An outcome evaluation of the SOS suicide prevention program. Am J Public Health [Internet]. 2004;94(3):446–51. doi:https://doi.org/10.2105/AJPH.94.3.446. [Google Scholar] [PubMed] [CrossRef]
16. Ruble AE, Leon PJ, Gilley-Hensley L, Hess SG, Swartz KL. Depression knowledge in high school students: effectiveness of the adolescent depression awareness program. J Affect Disord [Internet]. 2013;150(3):1025–30. doi:https://doi.org/10.1016/j.jad.2013.05.033. [Google Scholar] [PubMed] [CrossRef]
17. Swartz KL, Kastelic EA, Hess SG, Cox TS, Gonzales LC, Mink SP, et al. The effectiveness of a school-based adolescent depression education program. Health Educ Behav [Internet]. 2010;37(1):11–22. doi:https://doi.org/10.1177/1090198107303313. [Google Scholar] [PubMed] [CrossRef]
18. Aseltine Jr RH, James A, Schilling EA, Glanovsky J. Evaluating the SOS suicide prevention program: a replication and extension. BMC Public Health [Internet]. 2007;7(161):471. doi:https://doi.org/10.1186/1471-2458-7-161. [Google Scholar] [PubMed] [CrossRef]
19. Reilly N, Proper V, Jordan M, Feigenberg L, Capraro K. Break free from depression. Boston: Boston Children’s Hospital; 2016. [Google Scholar]
20. Boston Children’s Hospital Neighborhood Partnerships. Annual report 2020. Available from: https://www.childrenshospita’l.org/sites/default/files/media_migration/78e7ffcd-b671-4034-a9be-8d14ce0b6a1e.pdf [Accessed 2020]. [Google Scholar]
21. Luthar SS, Kumar NL. Youth in high-achieving schools: challenges to mental health and directions for evidence-based interventions. In: Leschied AW, Saklofske DH, Flett GL, editors, Handbook of school-based mental health promotion: an evidence-informed framework for implementation. New York: Springer; 2018. p. 441–58. [Google Scholar]
22. Allensworth EM, Moore PT, Sartain L, de la Torre M. The educational benefits of attending higher performing schools: evidence from Chicago high schools. Educ Eval Policy Anal [Internet]. 2017;39(2):175–97. doi:https://doi.org/10.3102/0162373716672039. [Google Scholar] [CrossRef]
23. Milburn KM. Experiences of high-achieving high school students who have taken multiple advanced placement courses. [Unpublished doctoral dissertation]. Drake University. Available from: dd2011KMM.pdf. [Accessed 2011]. [Google Scholar]
24. Suldo SM, Shaunessy E, Hardesty R. Relationships among stress, coping, and mental health in high-achieving high school students. Psychol Schools [Internet]. 2008;45(4):273–90. doi:https://doi.org/10.1002/(ISSN)1520-6807. [Google Scholar] [CrossRef]
25. Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods: advanced quantitative techniques in the social sciences series [Internet]. 2nd ed. Thousand Oaks: Sage; 2002. [Google Scholar]
26. Maas CJ, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodol [Internet]. 2005;1(3):86–92. doi:https://doi.org/10.1027/1614-2241.1.3.86. [Google Scholar] [CrossRef]
27. Nezlek JB. Multilevel random coefficient analyses of event-and interval-contingent data in social and personality psychology research. Pers Soc Psychol Bull [Internet]. 2001;27(7):771–85. doi:https://doi.org/10.1177/0146167201277001. [Google Scholar] [CrossRef]
28. Muthen BO, Satorra A. Complex sample data in structural equation modeling. Sociol Methodol [Internet]. 1995;25:267–316. doi:https://doi.org/10.2307/271070. [Google Scholar] [CrossRef]
29. Spybrook J, Raudenbush S, Liu X, Congdon R, Martinez A. Optimal design for longitudinal and multilevel research: documentation for the “Optimal Design” software. Available from: http://www.wtgrantfoundation.org. [Accessed 2006]. [Google Scholar]
30. Schilling EA, AseltineJr RH, James A. The SOS suicide prevention program: further evidence of efficacy and effectiveness. Prev Sci [Internet]. 2016;17(2):157–66. doi:https://doi.org/10.1007/s11121-015-0594-3. [Google Scholar] [PubMed] [CrossRef]
31. Beaudry MB, Swartz K, Miller L, Schweizer B, Glazer K, Wilcox H. Effectiveness of the adolescent depression awareness program (ADAP) on depression literacy and mental health treatment. J School Health [Internet]. 2019;89(3):165–72. doi:https://doi.org/10.1111/josh.12725. [Google Scholar] [PubMed] [CrossRef]
32. Townsend L, Musci R, Stuart E, Heley K, Beaudry MB, Schweizer B, et al. Gender differences in depression literacy and stigma after a randomized controlled evaluation of a universal depression education program. J Adolesc Health [Internet]. 2019;64(4):472–7. doi:https://doi.org/10.1016/j.jadohealth.2018.10.298. [Google Scholar] [PubMed] [CrossRef]
33. Latalova K, Kamaradova D, Prasko J. Perspectives on perceived stigma and self-stigma in adult male patients with depression. Neuropsych Dis Treat [Internet]. 2014;10:1399–405. doi:https://doi.org/10.2147/NDT. [Google Scholar] [CrossRef]
34. Moses T. Stigma and self-concept among adolescents receiving mental health treatment. Am J Orthopsychiatry [Internet]. 2009;79(2):261–74. doi:https://doi.org/10.1037/a0015696. [Google Scholar] [PubMed] [CrossRef]
35. Wang C, Cramer KM, Cheng H, Do KA. Associations between depression literacy and help-seeking behavior for mental health services among high school students. School Ment Health [Internet]. 2019;11(4):707–18. doi:https://doi.org/10.1007/s12310-019-09325-1. [Google Scholar] [CrossRef]
36. Lu W. Adolescent depression: national trends, risk factors, and healthcare disparities. Am J Health Behav. [Internet]. 2019;43(1):181–94. doi:https://doi.org/10.5993/AJHB.43.1.15. [Google Scholar] [PubMed] [CrossRef]
37. Lu W, Todhunter-Reid A, Mitsdarffer ML, Muñoz-Laboy M, Yoon AS, Xu L. Barriers and facilitators for mental health service use among racial/ethnic minority adolescents: a systematic review of literature. Front Public Health [Internet]. 2021;9:641605. doi:https://doi.org/10.3389/fpubh.2021.641605. [Google Scholar] [PubMed] [CrossRef]
38. BarreraJr M, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psych [Internet]. 2013;81(2):196–205. doi:https://doi.org/10.1037/a0027085. [Google Scholar] [PubMed] [CrossRef]
39. Kalibatseva Z, Leong FTL. A critical review of culturally sensitive treatments for depression: recommendations for intervention and research. Psychol Serv [Internet]. 2014;11(4):433–50. doi:https://doi.org/10.1037/a0036047. [Google Scholar] [PubMed] [CrossRef]
40. Lei N, Pelliteri J. Help-seeking and coping behaviors among Asian Americans: the roles of Asian values, emotional intelligence, and optimism. Asian Am J Psychol [Internet]. 2017;8(3):224–34. doi:https://doi.org/10.1037/aap0000086. [Google Scholar] [CrossRef]
41. Taylor RE, Kuo BCH. Black American psychological help-seeking intention: an integrated literature review with recommendations for clinical practice. J Psychother Integr [Internet]. 2018;29(4):325–37. doi:https://doi.org/10.1037/int0000131. [Google Scholar] [CrossRef]
42. Goodwin AKB, Chen GL, Long ACJ. Mental health, well-being, and help-seeking in schools among black adolescents: the role of discrimination in high-achieving academic settings. Psychol Schools [Internet]. 2021;58(9):1690–707. doi:https://doi.org/10.1002/pits.22523. [Google Scholar] [CrossRef]
43. Johnstone KM, Kemps E, Chen J. A meta-analysis of universal school-based prevention programs for anxiety and depression in children. Clin Child Fam Psych [Internet]. 2018;21(4):466–81. doi:https://doi.org/10.1007/s10567-018-0266-5. [Google Scholar] [PubMed] [CrossRef]
44. Werner-Seidler A, Perry Y, Calear AL, Newby JM, Christensen H. School-based depression and anxiety prevention programs for young people: a systematic review and meta-analysis. Clin Psychol Rev [Internet]. 2017;51(1):30–47. doi:https://doi.org/10.1016/j.cpr.2016.10.005. [Google Scholar] [PubMed] [CrossRef]
45. Miller DN. Suicide prevention programs in the schools: a review and public health perspective. School Psychol Rev [Internet]. 2009;38(2):168–88. doi:https://doi.org/10.1080/02796015.2009.12087830. [Google Scholar] [CrossRef]
46. Thomas H. Obesity prevention programs for children and youth: why are their results so modest? Health Educ Res [Internet]. 2006;21(6):783–95. doi:https://doi.org/10.1093/her/cyl143. [Google Scholar] [PubMed] [CrossRef]
47. Jones SC, Anderson RE, Metzger IW. Standing in the gap: the continued importance of culturally competent therapeutic interventions for black youth. Evid-Based Pract Child Adolesc Ment [Internet]. 2020;5(3):327–39. doi:https://doi.org/10.1080/23794925.2020.1796546. [Google Scholar] [CrossRef]
48. Antonio MC, Chung-Do DrPH JJ. Systematic review of interventions focusing on Indigenous adolescent mental health and substance use. Am Indian Alsk Native Ment Health Res [Internet]. 2015;22(3):36–46. doi:https://doi.org/10.5820/aian.2203.2015.36. [Google Scholar] [PubMed] [CrossRef]
49. Ford-Paz RE, Reinhard C, Kuebbeler A, Contreras R, Sánchez B. Culturally tailored depression/suicide prevention in Latino youth: community perspectives. J Behav Health Serv Res [Internet]. 2015;42(4):519–33. doi:https://doi.org/10.1007/s11414-013-9368-5. [Google Scholar] [PubMed] [CrossRef]
50. Brown C, Maggin DM, Buren M. Systematic review of cultural adaptations of school-based social, emotional, and behavioral interventions for students of color. Educ Treat Child [Internet]. 2008;41(4):431–56. doi:https://doi.org/10.1353/etc.2018.0024. [Google Scholar] [CrossRef]
51. de Miranda DM, da Silva Athanasio B, Oliveira ACS, Simoes-e-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disast Risk Re [Internet]. 2020;51:101845. doi:https://doi.org/10.1016/j.ijdrr.2020.101845. [Google Scholar] [PubMed] [CrossRef]
52. Luthar SS, Suh BC, Ebbert AC, Kumar NL. Students in high-achieving schools: perils of pressures to be “standouts”. Advers Resil Sci [Internet]. 2020;1(2):135–47. doi:https://doi.org/10.1007/s42844-020-00009-3. [Google Scholar] [CrossRef]
53. Comas-Díaz L, Hall GN, Neville HA. Racial trauma: theory, research, and healing: introduction to the special issue. Am Psychol [Internet]. 2019;74(1):1–5. doi:https://doi.org/10.1037/amp0000442. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools