 Open Access
Open Access
ARTICLE
Cross-Sectional Associations of Lifestyle Behaviors with Depressive Symptoms in Adolescents
1 Division of Physical Education and Sport, Henan Institute of Technology, Xinxiang, 45300, China
2 School of Physical Education and Sport, Shanghai Normal University, Shanghai, 20000, China
* Corresponding Author: Jiayi Gu. Email:
International Journal of Mental Health Promotion 2023, 25(1), 139-152. https://doi.org/10.32604/ijmhp.2022.022123
Received 22 February 2022; Accepted 25 March 2022; Issue published 29 November 2022
Abstract
This study aimed to examine the associations between lifestyle behaviors and depressive symptoms in adolescents. Self-reported data from the 2019 Youth Risk Behavior Survey (YRBS) was analyzed. Depressive symptoms were set as the outcome variable. Movement variables (physical activity, muscle-strengthening exercise, physical education attendance, sports team participation, television watching, video or computer games, and sleep), eating behaviors (fruit intake, vegetable intake, milk intake, and eating breakfast or not), and substance use (alcohol use and cigarette use) were included as explanatory variables. Binary logistic regression was used to explore the associations between lifestyle behaviors and depressive symptoms after adjusting for sex, age, grade, race, and weight status. Of 13,677 participants who completed the investigation, girls were more than boys (50.3% vs. 48.6%). The proportion of participants in grades 9, 10, 11, and 12 was 26.6, 27.2, 24.3, and 20.8, respectively. Of them, the prevalence of depressive symptoms was 36.0% (weighted%: 36.7% [35.1%, 38.3%]). Among all the lifestyle behaviors included, participating in no sports teams (OR = 1.53 [1.32, 1.77]), spending more than 2 h in video or computer games (OR = 1.64 [1.40, 1.92]), sleeping less than 8 h nightly (OR = 1.79 [1.45, 2.20]), not eating breakfast (OR = 1.56 [1.37, 1.78]), alcohol use (OR = 1.74 [1.49, 2.02]), and cigarette use (OR = 1.83 [1.42, 2.37]) were associated with higher odds of depressive symptoms. To reduce depressive symptoms in adolescents, interventions can consider encouraging adolescents to engage in team sports activity, limit time for video or computer games, sleep enough, regularly eat breakfast, and avoid using alcohol and cigarette. Future studies are encouraged to verify our research findings by using a more improved study design.Keywords
Depression has been a serious mental health problem that gives a huge burden on the whole society [1]. Similarly, adolescent depression is a common emotional disorder that results in interest loss, sleep deprivation, excessive substance use, and feelings of hopelessness [1,2]. Data suggests that depression is a major mental health disorder in the world [2,3]. In the US, depression diagnosed among youth increased from 8.7% in 2005 to 11.3% in 2014 [4]. More seriously, about 15% of adolescents in the US were diagnosed with severe depression [5]. 7.1%–19.4% of adolescents in 11 European countries are screened as having depressive symptoms [6]. According to the latest World Health Organization, depression is the fourth leading cause of illness and disability among those aged 15–19 years and the fifteenth among those aged 10–14 years (World Health Organization, 2018). These data show that depression has been a prevalent mental illness in adolescents in the world, which must be paid sufficient attention to addressing this mental health problem. In addition, evidence has confirmed the adverse effects of depression on overall development and health in adolescents, such as social [7] and cognitive impairments [8], school dropout [9], unhealthy behaviors [10,11], and subsequent higher risks for cardiovascular diseases [12]. From a public health perspective, it is necessary to reduce the burdens of depression in adolescents by understanding the associated factors and implementing efficient interventions.
Lifestyle behaviors are considered as important correlates of depression in adolescents [13]. Increasing studies reported that lifestyle behaviors could be factors of depression in adolescents [14–19]. For example, Vancampfort et al. [20] found that more sitting time was positively associated with higher risks of depression symptoms. One systematic review also suggested that screen time was positively associated with depression in adolescents [15]. Biddle et al.’s [21] systematic review indicated that physical activity was a protective factor in developing depression in adolescents. These two kinds of lifestyle behaviors have been studied in previous studies. In addition to these movement activities, some studies have explored the associations between eating behaviors and depression in adolescents. A meta-analysis demonstrated that increasing fruit and vegetable intake may be associated with lower risks for depression [22]. In adolescents, studies have confirmed that sufficient fruit and vegetable intake is a negative factor in depression [23]. This research finding was supported by another multiple-country research [24]. Recent studies also reveal the negative association between breakfast behavior and depression in adolescents [25,26]. Moreover, as an increasing number of adolescents are using substance, like alcohol and cigarettes, studies have suggested the negative effects of substance use on depression [10,11,13,27–30]. The above evidence suggested that improving lifestyle behaviors would be an optimal approach to reducing the odds of depression.
However, some research gaps remain across the previous literature. Addressing these gaps would be more conducive to producing more meaningful insights into depression prevention in children and adolescents. One major research gap is that previous research cannot be done at a nationally representative level owing to limited data sources or collection. This gap inhibits researchers to understand the association between lifestyle behavior and depression at a population level, limiting the efficiency of populational level interventions. Another is that previous studies failed to examine the associations between multiple lifestyle behaviors and depressive symptoms in one study. Examining various lifestyle behaviors can help determine one’s specific association with depressive symptoms. Indeed, including lifestyle behaviors as much as possible in research on depression is of great importance to determine different lifestyle behaviors’ roles in improving mental health. However, to our knowledge, such studies remain scanty, which is encouraged to conduct to determine different lifestyle behaviors’ roles in depression prevention.
To address these research gaps, this study aims to explore the associations between lifestyle behaviors (e.g., movement behaviors, eating behaviors, and substance use) and depression in adolescents using a nationally representative sample from the 2019 US Youth Risk Behavior Survey (YRBS).
2.1 Study Design and Participants
We used data from the YRBS 2019 cycle to achieve our research aims. A cluster sampling design was utilized to generate a nationally representative sample of schoolers from 9–12 grades.
Based on student sex, race/ethnicity, and grade, weight was applied to each respondent to adjust for nonresponse and oversampling of minority students. The overall weights were scaled so that the weighted count of students equals the total sample size, and the weighted proportions of students in each grade match the national population proportions. The YRBS survey has been approved by Institutional Review Board at the Centre for Disease Control of the US. 13,872 study participants completed the questionnaire in the 2019 YRBS survey, of which 13,677 cases can be analyzed. The overall response rate of the 2019 YRBS survey was 60.3%, calculated by the school response rate (75.1%) × the student response rate (80.3%).
Depressive symptoms were assessed by the item question “During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities?” Responses were yes or no. Study participants answering yes were treated as having depressive symptoms. This item has been used to measure depressive symptoms in some published studies. Although there are limitations to measuring depressive symptoms with a single item, the presence of depressive mood and deterioration of functioning on most days during a period of two weeks can suggest the possible occurrence of depressive episodes [31,32]. YRBS questionnaire has shown acceptable reliability and validity among adolescents [33].
2.2.2 Lifestyle Behavior Factors (Explanatory Variables)
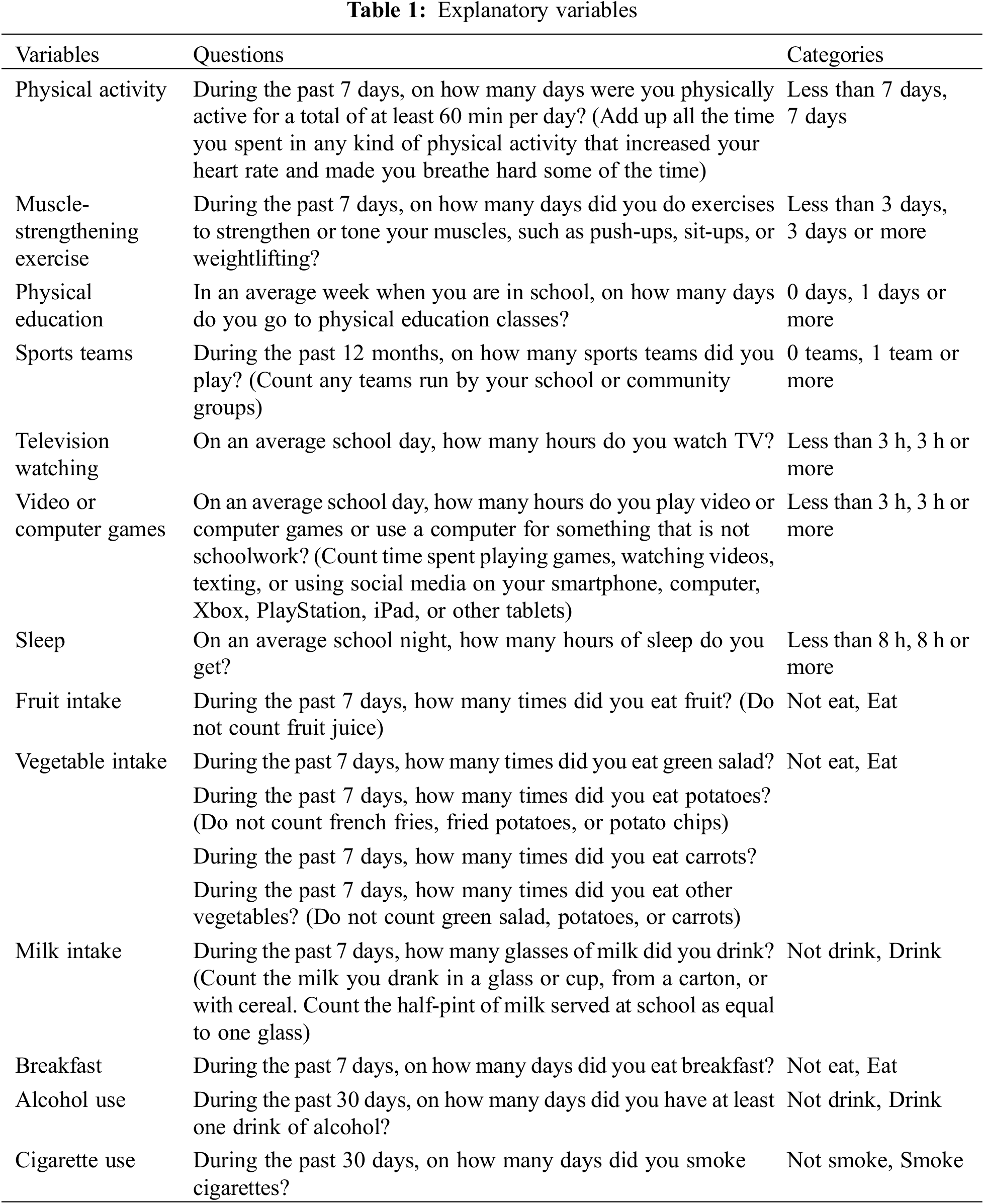
A total of 13 explanatory variables were used, including physical activity, muscle-strengthening exercise, physical education, sports teams, television viewing, video or computer games, sleep, fruit intake, vegetable intake, milk intake, breakfast, alcohol use, and cigarette use. All the explanatory variables were selected considering their significant association with depressive symptoms in the previous literature, as well as their availability in the datasets. Items measuring these variables are listed in Table 1.
Sex (female or male), age (12–18 years old, including 12 years old or younger, 18 years old or older), grade (9th–12th), race (white, black or African American, Hispanic/Latino, or all other races). Study participants’ status of overweight or obesity was determined by body mass index that was estimated based on self-reported height and weight. These variables were treated as control variables in the further statistical analysis.
All statistical analyses were performed using SPSS 26.0. Missing data were not imputed. All the statistical analyses took complex sampling design into consideration for nationally representative estimates according to the YRBS design. The weighted percentage of each variable was also reported with a 95% confidence interval. Binary logistic regression was utilized to assess the associations of lifestyle behavior with depressive symptoms while controlling for sex, age, grade, race, overweight, and obesity. Adjusted odds ratios with 95% CI were reported to assess the associations of lifestyle behavior with depressive symptoms. The above statistical analysis was run through the Complex Sample Module in the SPSS. Statistical significance was set up as p < 0.0025 (0.05/20) as 20 independent variables were included in the final regression model.
Table 1 displays the sample characteristics of this study. For the YRBS 2019 survey, 13677 participants completed the investigation. Of them, girls were more than boys (50.3% vs. 48.6%). A few of the participants were grouped as 11 or 12 years old, while most of them ranged from 15–17 years old. The proportion of participants in grades 9, 10, 11, and 12 was 26.6, 27.2, 24.3, and 20.8, respectively. Participants with the race of white account for the whole participants predominantly. Concerning obesity and overweight, the prevalence of them was 14.1% and 13.1%, respectively. The weighted results can be also found in Table 2.
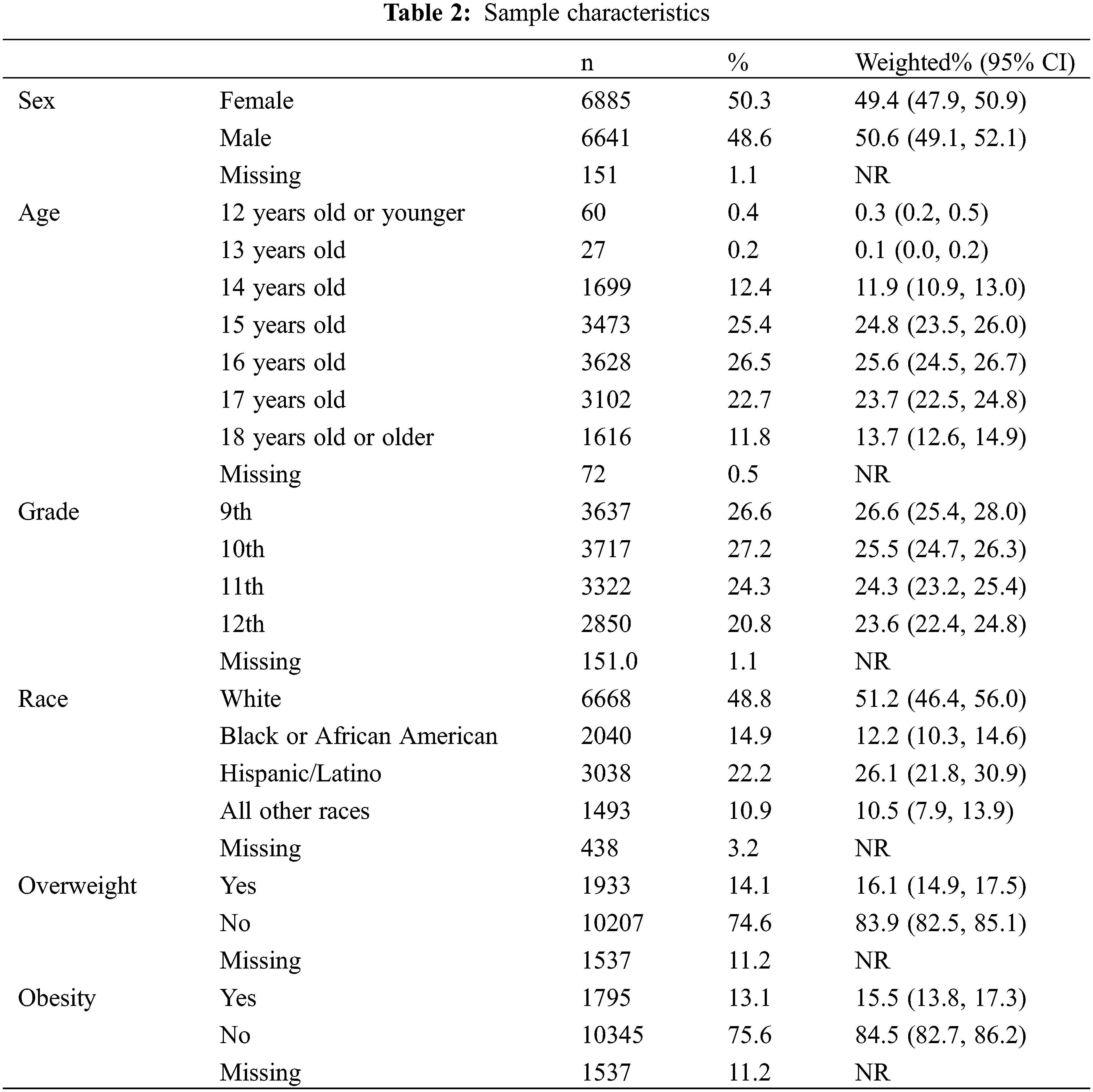
Table 3 presents the prevalence (unweighted and weighted) of each lifestyle behavior included in the study and depressive symptoms. The prevalence of four healthy physical activity-related variables was all less than half, ranging from 21.6% (sufficient physical activity) to 40.5% (sports team participation). Similarly, participants who slept for more than 8 years nightly also account for a minor proportion (21.4%). On the contrary, the prevalence of healthy screen use-related variables was high (television watching hours: 74.6%, played video or computer games or used a computer: 53.0%). Besides, the prevalence of unhealthy diet behaviors was low, ranging from 5.3% (currently smoking) to 26.8% (currently alcohol use). The prevalence of depressive symptoms was 36.0% in the study sample.
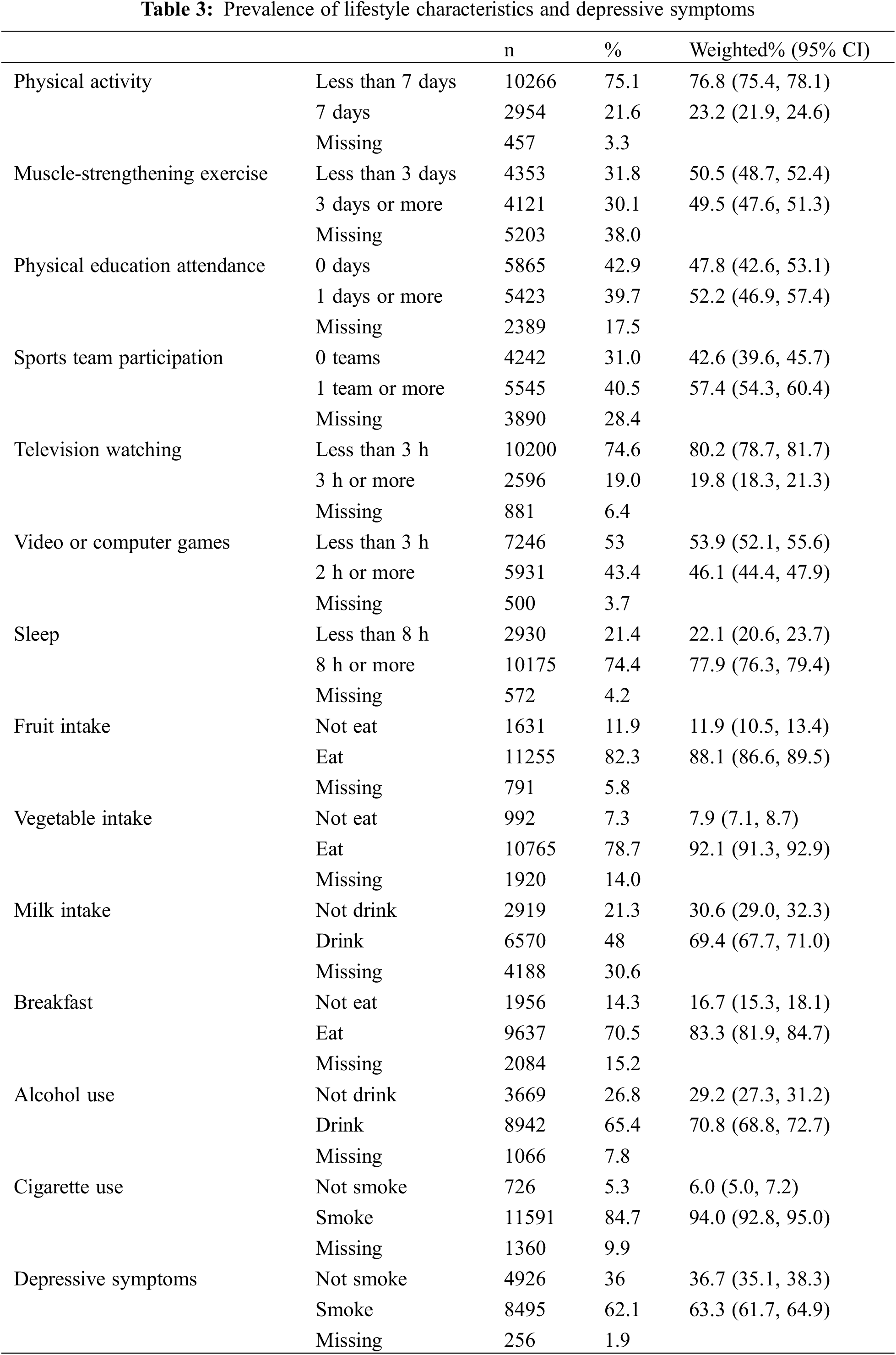
Table 4 shows the associations between each lifestyle behavior and depressive symptoms. Participating in no sports team was associated with a higher odds (1.53 [1.32–1.77]) of depressive symptoms than participating in at least one. Spending more than 2 h per day on video or computer or using a computer was associated with a higher OR (1.64 [1.40–1.92)] of depressive symptoms than spending less. Sleeping less than 8 h nightly was associated with a higher OR (1.79 [1.45–2.20]) of depressive symptoms than sleeping more. Besides, not eating breakfast (OR = 1.56 [1.37–1.78]), currently smoking (OR = 1.74 [1.49–2.02]). Both alcohol use (OR = 1.83 [1.42–2.37]) and cigarette use (OR = 1.83 [1.42, 2.37]) were associated with higher odds of depressive symptoms.
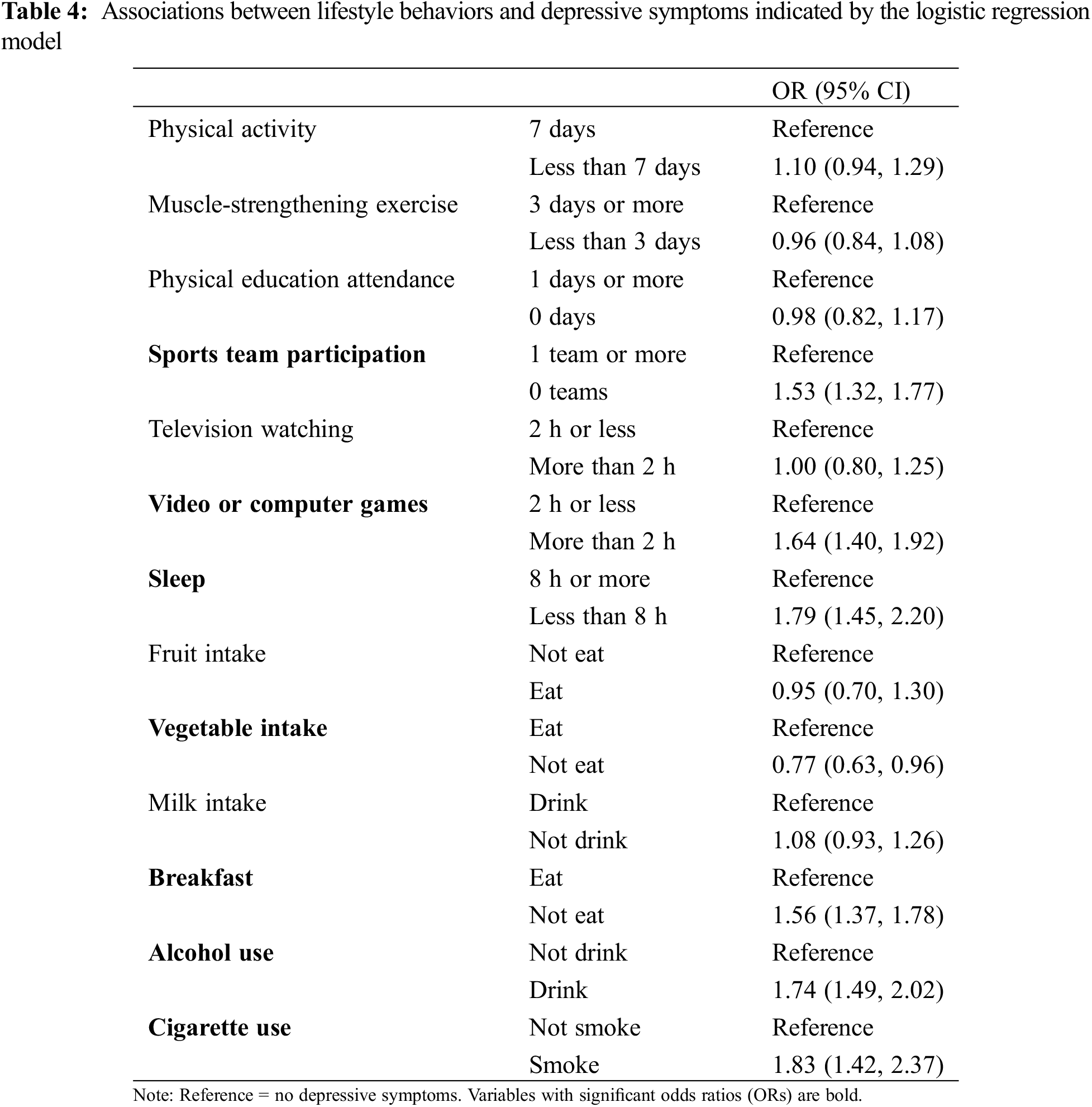
The present study aimed to examine the association between lifestyle behaviors (e.g., eating, movement, and substance use) and depressive symptoms in adolescents using the data collected in 2019 from the national US YRBS survey. We mainly found that no sports team participation, spending more than 2 h per day on video or computer games, shorter sleep duration (less than 8 h per day), not eating breakfast, alcohol use, and cigarette use were associated with self-reported confirmed depressive symptoms in the US adolescents. Yet, physical activity, muscle-strengthening exercise, physical education attendance, television watching, fruit intake, and milk intake were not associated with depressive symptoms. The current study has some implications on lifestyle behavior changes for the prevention and intervention of depressive symptoms in adolescents. Although some meaningful associations were found, no causal inference can be drawn due to the cross-sectional study design. A discussion of our research findings and public health implications is analyzed further.
In the present study, we found that adolescents who participated in team sports were less likely to self-report depressive symptoms, which is consistent with the previous studies [34–36]. This longitudinal study showed that team sport participation during adolescence was longitudinally associated with lower depressive symptoms in early adulthood [34]. The potential explanation may be that team sports participation can provide social connections, feelings of belongingness, and perceptions of enjoyment, which can be viewed as a treatment for lowering depressive symptoms [35,37]. In addition, the positive experiences like peer support and skill development gained by team sport participation can enhance perceived social acceptance and reduce body dissatisfaction [36], which, in turn, may be beneficial to preventing depressive symptoms [38]. Another 10-year prospective study revealed that current and past team sport participation were both negatively linked to depressive symptoms [35]. Therefore, sports team participation could be an important way to prevent depressive symptoms in adolescents.
Our study showed that video or computer games time was positively associated with increased odds of depressive symptoms in adolescents. This is consistent with some previous studies that support the positive association between screen time and depressive symptoms [39,40]. However, the existing evidence also indicated that video gaming [41] or computer use [42] were not associated with increased depressive symptoms among adolescents, which is discordant with our research findings. The possible explanation may be that adolescents play video or computer games with friends, which is not socially isolated, and then can be beneficial to adolescents’ mental well-being, reducing the odds of depressive symptoms [43,44]. Hence, this implies that when examining the associations between video or computer games time and depressive symptoms, the associated contexts should be investigated, like with whom to play, and play what kinds of games, this would be beneficial to understand the mechanism linking video or computer games and depressive symptoms. Merely based on our research findings, reducing time for video or computer games may be a good way to limit the development of depression in adolescents. Interestingly, in our study, television viewing time was not associated with depressive symptoms, which is consistent with Maras et al. [39]. However, this finding is contradictory to the assumption that more screen time is positively associated with depression. To gain insights into the association between screen time and depression, distinguishing kinds of screen time is needed and meaningful.
Compared with adolescents with more than 8 h of nightly sleep duration, those who had insufficient sleep duration (no more than 8 h) were more likely to report having depressive symptoms in our study, which is consistent with several prior studies [45–47]. The literature has shown that insufficient sleep duration was associated with difficulties in emotion control [48], risk behaviors [49], and suicidal behavior [50], which have also been identified as factors of depressive symptoms [51]. Although the bidirectional relationship between sleep duration and depressive symptoms cannot be explored in this study, the previous study has indicated that depressive symptoms caused by insufficient sleep duration will lead to sleep quality in children and adolescents [45]. Considering the relatively high prevalence of depressive symptoms (weighted percentage = 36.7%), the regulation of sleep duration may be an important means to prevent depressive symptoms in adolescents.
Apart from the above-discussed lifestyle behaviors factors, our study also found that eating behaviors, including vegetable intake, and eating breakfast, were also associated with depressive symptoms in adolescents. Though previous studies have demonstrated that eating vegetables can digest antioxidants and anti-inflammatory ingredients which have been shown to have a protective impact on depression development [52,53], findings in the present study (not eating vegetables was associated with lower risks for depression symptoms) contradicted the previous research findings. This unexpected research finding cannot be supported by current knowledge, and we call for more studies to confirm or negate our results. In addition, we found that not eating breakfast was associated with increased depressive symptoms in adolescents. Although limited studies targeted this topic, a significant association between eating breakfast and depression has been observed in adolescents [54,55].
Alcohol use [56] and cigarette use [57] were positively associated with depressive symptoms in our study, which is consistent with a population-based sample study [54]. Besides, one review study showed that a large number of longitudinal research evidence have identified the positive relationships between smoking and depressive symptoms in adolescents [57]. The previous studies revealed that neurochemical pathways damaged by exposure to nicotine (such as monoamine neurotransmission) may explain this cross-sectional association between smoking and depressive symptoms [58,59]. Several potential explanations may contribute to the association between alcohol use and depressive symptoms. For example, youth with heavy alcohol use has negative impacts on the emotional functioning area in the brain, which may cause depressive symptoms [60]. In addition, evidence has revealed that alcohol use was also related to environmental stressors (e.g., poor academic performance, social relationships), biological changes, and emotional disorders, which are all associated with inducing bad mood problems [11]. Based on our research findings, limiting substance use can play an important role in reducing depressive symptoms in adolescents.
Some counterintuitive research findings are worth discussing. For example, sufficient physical activity was not associated with depressive symptoms in our study, which is inconsistent with the established evidence [21,61]. Possible explanations may be owing to the inclusion of muscle-strengthening exercise and sports team participation, offsetting the roles of physical activity on depressive symptoms. As for the measure of physical activity, it might be more difficult to respond to days of physical activity reliably and accurately compared with measures of muscle-strengthening exercise and sports team participation, because the latter two measures were easier to recall. This reason can explain why physical activity was not associated with depressive symptoms. Concerning physical education, as a form of physical activity, it is unexpected to be not associated with depressive symptoms based on previous studies. However, a recent systematic review and meta-analysis indicated that physical education was not associated with any indicators of mental health or illness [62], which is consistent with our study. Muscle-strengthening exercise, as a recently studied form of physical activity, has been indicated negatively associated with depression symptoms in adults [63,64] and adolescents [65]. Yet, we did not such a significant association, perhaps owing to methodological differences or different sample characteristics. Collectively, in our study, these counterintuitive research findings should be re-examined in future studies.
The current study includes some strengths, of which one is using a nationally representative sample that can increase the generalizability of research findings and the other one is the inclusion of many lifestyle behaviors factors that can determine the specific association between different kinds of lifestyle behaviors factors and depressive symptoms. However, some study limitations of the current study should be acknowledged in light of a better understanding of the research findings. First, the secondary analysis study is limited by the cross-sectional nature of YRBS, leading to the failure to determine casual associations. Therefore, behaviors studied in the current study may actually be the manifestation of depression symptoms, such as insufficient sleep, which can be raised by sleep disturbance caused by depressive symptoms. Not participating in the sports team, though set as an explanatory variable, may also be the outcome of depressive symptoms, because depressive individuals always lose interest in activities and feel fatigued. Second, the self-reported measures that this study used may have negative impacts on the assessment. Third, specific associations between various lifestyle behaviors and depressive symptoms were not examined, and strong associations between lifestyles, such as screen time and smoking and alcohol consumption, were potentially linked. Fourth, the outcome (depressive symptoms) of this study was assessed by a single-item question asking about a two-week period of persistent depressive feelings, along with a decline in functioning in the past year. This is considered to be a criterion but is not sufficient for a definite diagnosis of depression. By using simplified diagnostic criteria, the prevalence of depressive symptoms may have been overestimated. However, this item is still meaningful for understanding youth mental health status in such a large sample size from a nationwide general adolescent population survey. Future research is highly recommended to explore the association between lifestyle behaviors and depressive symptoms using more improved study designs, which can, in turn, negate or confirm our study findings.
This cross-sectional study suggests that different lifestyle behaviors have varied associations with depressive symptoms in children and adolescents. Specifically, engaging in sports team participation, reducing time for video or computer games time, sleeping enough, regularly eating breakfast, avoiding alcohol, and smoking might be some important protective lifestyle behaviors against depression symptoms. Behavioral change strategies or mental health interventions can consider our research findings to design or implement efficient plans to reduce depressive symptoms and then inhibit developing depression in adolescents. Future studies are encouraged to improve study design, which can negate or confirm our research findings reliably.
Acknowledgement: The authors thank the data from the YRBS website for public use.
Authorship: JG: writing-original draft. WK: writing-original draft and project administration. JG and WK: writing-review and editing. Both authors contributed to and have approved the final manuscript.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Erskine, H. E., Baxter, A. J., Patton, G., Moffitt, T. E., Patel, V. et al. (2017). The global coverage of prevalence data for mental disorders in children and adolescents. Epidemiology and Psychiatric Sciences, 26(4), 395–402. DOI 10.1017/S2045796015001158. [Google Scholar] [CrossRef]
2. Merikangas, K. R., Nakamura, E. F., Kessler, R. C. (2009). Epidemiology of mental disorders in children and adolescents. Dialogues in Clinical Neuroscience, 11(1), 7–20. DOI 10.31887/DCNS.2009.11.1/krmerikangas. [Google Scholar] [CrossRef]
3. Liu, Q., He, H., Yang, J., Feng, X., Zhao, F. et al. (2020). Changes in the global burden of depression from 1990 to 2017: Findings from the global burden of disease study. Journal of Psychiatric Research, 126, 134–140. DOI 10.1016/j.jpsychires.2019.08.002. [Google Scholar] [CrossRef]
4. Mojtabai, R., Olfson, M., Han, B. (2016). National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics, 138(6), e20161878. DOI 10.1542/peds.2016-1878. [Google Scholar] [CrossRef]
5. Birmaher, B., Ryan, N. D., Williamson, D. E., Brent, D. A., Kaufman, J. (1996). Childhood and adolescent depression: A review of the past 10 years. Part II. Journal of the American Academy of Child & Adolescent Psychiatry, 35(12), 1575–1583. DOI 10.1097/00004583-199612000-00008. [Google Scholar] [CrossRef]
6. Balazs, J., Miklósi, M., Keresztény, Á., Apter, A., Bobes, J. et al. (2012). Prevalence of adolescent depression in Europe. European Psychiatry, 27. DOI 10.1016/S0924-9338(12)74426-7. [Google Scholar] [CrossRef]
7. Allen, J. P., Chango, J., Szwedo, D., Schad, M. (2014). Long-term sequelae of subclinical depressive symptoms in early adolescence. Development and Psychopathology, 26(1), 171–180. DOI 10.1017/S095457941300093X. [Google Scholar] [CrossRef]
8. Wagner, S., Müller, C., Helmreich, I., Huss, M., Tadić, A. (2015). A Meta-analysis of cognitive functions in children and adolescents with major depressive disorder. European Child & Adolescent Psychiatry, 24(1), 5–19. DOI 10.1007/s00787-014-0559-2. [Google Scholar] [CrossRef]
9. Butterworth, P., Leach, L. S. (2017). Early onset of distress disorders and high-school dropout: Prospective evidence from a national cohort of Australian adolescents. American Journal of Epidemiology, 187(6), 1192–1198. DOI 10.1093/aje/kwx353. [Google Scholar] [CrossRef]
10. Chaiton, M. O., Cohen, J. E., O’loughlin, J., Rehm, J. (2009). A systematic review of longitudinal studies on the association between depression and smoking in adolescents. Bmc Public Health, 9, 1–11. DOI 10.1186/1471-2458-9-356. [Google Scholar] [CrossRef]
11. Pedrelli, P., Shapero, B., Archibald, A., Dale, C. (2016). Alcohol use and depression during adolescence and young adulthood: A summary and interpretation of mixed findings. Current Addiction Reports, 3, 91–97. DOI 10.1007/s40429-016-0084-0. [Google Scholar] [CrossRef]
12. Goldstein, B. I., Carnethon, M. R., Matthews, K. A., Mcintyre, R. S., Miller, G. E. et al. (2015). Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: A scientific statement from the American heart association. Circulation, 132(10), 965–986. DOI 10.1161/CIR.0000000000000229. [Google Scholar] [CrossRef]
13. Firth, J., Solmi, M., Wootton, R. E., Vancampfort, D., Schuch, F. B. et al. (2020). A meta-review of “lifestyle psychiatry”: The role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry, 19(3), 360–380. DOI 10.1002/wps.20773. [Google Scholar] [CrossRef]
14. Zink, J., Belcher, B. R., Imm, K., Leventhal, A. M. (2020). The relationship between screen-based sedentary behaviors and symptoms of depression and anxiety in youth: A systematic review of moderating variables. Bmc Public Health, 20(1), 472–509. DOI 10.1186/s12889-020-08572-1. [Google Scholar] [CrossRef]
15. Wang, X., Li, Y., Fan, H. (2019). The associations between screen time-based sedentary behavior and depression: A systematic review and meta-analysis. BMC Public Health, 19(1), 1524–1533. DOI 10.1186/s12889-019-7904-9. [Google Scholar] [CrossRef]
16. Sampasa-Kanyinga, H., Colman, I., Goldfield, G. S., Janssen, I., Wang, J. et al. (2020). Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 17(1), 72–88. DOI 10.1186/s12966-020-00976-x. [Google Scholar] [CrossRef]
17. Maggie, Z., Fatch, K., He, G. P., Wang, H. H. (2012). Depression among Chinese children and adolescents: A review of the literature. International Journal of Child, Youth and Family Studies, 3, 442–457. DOI 10.18357/ijcyfs34.1201211543. [Google Scholar] [CrossRef]
18. Brown, H. E., Pearson, N., Braithwaite, R. E., Brown, W. J., Biddle, S. J. (2013). Physical activity interventions and depression in children and adolescents: A systematic review and meta-analysis. Sports Medicine, 43(3), 195–206. DOI 10.1007/s40279-012-0015-8. [Google Scholar] [CrossRef]
19. Lopresti, A. L., Hood, S. D., Drummond, P. D. (2013). A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. Journal of Affective Disorders, 148(1), 12–27. DOI 10.1016/j.jad.2013.01.014. [Google Scholar] [CrossRef]
20. Vancampfort, D., Stubbs, B., Firth, J., van Damme, T., Koyanagi, A. (2018). Sedentary behavior and depressive symptoms among 67,077 adolescents aged 12–15 years from 30 low- and middle-income countries. International Journal of Behavioral Nutrition and Physical Activity, 15(1), 73–82. [Google Scholar]
21. Biddle, S. J. H., Ciaccioni, S., Thomas, G., Vergeer, I. (2019). Physical activity and mental health in children and adolescents: An updated review of reviews and an analysis of causality. Psychology of Sport and Exercise, 42, 146–155. DOI 10.1016/j.psychsport.2018.08.011. [Google Scholar] [CrossRef]
22. Saghafian, F., Malmir, H., Saneei, P., Milajerdi, A., Larijani, B. et al. (2016). Fruit and vegetable consumption and risk of depression: Accumulative evidence from an updated systematic review and meta-analysis of epidemiological studies. British Journal of Nutrition, 119(10), 1087–1101. DOI 10.1017/S0007114518000697. [Google Scholar] [CrossRef]
23. Huang, P., O’keeffe, M., Elia, C., Karamanos, A., Goff, L. M. et al. (2019). Fruit and vegetable consumption and mental health across adolescence: Evidence from a diverse urban British cohort study. International Journal of Behavioral Nutrition and Physical Activity, 16(1), 19–32. DOI 10.1186/s12966-019-0780-y. [Google Scholar] [CrossRef]
24. Liu, M. W., Chen, Q. T., Towne, S. D., Zhang, J., Yu, H. J. et al. (2020). Fruit and vegetable intake in relation to depressive and anxiety symptoms among adolescents in 25 low- and middle-income countries. Journal of Affective Disorders, 261, 172–180. DOI 10.1016/j.jad.2019.10.007. [Google Scholar] [CrossRef]
25. Richards, G., Smith, A. P. (2016). Breakfast and energy drink consumption in secondary school children: Breakfast omission, in isolation or in combination with frequent energy drink use, is associated with stress, anxiety, and depression cross-sectionally, but not at 6-month follow-up. Frontiers in Psychology, 7, 106–116. DOI 10.3389/fpsyg.2016.00106. [Google Scholar] [CrossRef]
26. Ferrer-Cascales, R., Sánchez-Sansegundo, M., Ruiz-Robledillo, N., Albaladejo-Blázquez, N., Laguna-Pérez, A. et al. (2018). Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in Spanish adolescents. International Journal of Environmental Research and Public Health, 15(8), 1781–1791. DOI 10.3390/ijerph15081781. [Google Scholar] [CrossRef]
27. Johannessen, E. L., Andersson, H. W., Bjørngaard, J. H., Pape, K. (2017). Anxiety and depression symptoms and alcohol use among adolescents-a cross sectional study of Norwegian secondary school students. BMC Public Health, 17(1), 494–503. DOI 10.1186/s12889-017-4389-2. [Google Scholar] [CrossRef]
28. Fluharty, M., Taylor, A. E., Grabski, M., Munafò, M. R. (2019). The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine & Tobacco Research, 19(1), 3–13. DOI 10.1093/ntr/ntw140. [Google Scholar] [CrossRef]
29. Ranjit, A., Buchwald, J., Latvala, A., Heikkilä, K., Tuulio-Henriksson, A. et al. (2019). Predictive association of smoking with depressive symptoms: A longitudinal study of adolescent twins. Prevention Science, 20(7), 1021–1030. DOI 10.1007/s11121-019-01020-6. [Google Scholar] [CrossRef]
30. Zvolensky, M. J., Stewart, S. H., Vujanovic, A. A., Gavric, D., Steeves, D. (2009). Anxiety sensitivity and anxiety and depressive symptoms in the prediction of early smoking lapse and relapse during smoking cessation treatment. Nicotine & Tobacco Research, 11(3), 323–331. DOI 10.1093/ntr/ntn037. [Google Scholar] [CrossRef]
31. Chadi, N., Li, G., Cerda, N., Weitzman, E. R. (2019). Depressive symptoms and suicidality in adolescents using e-cigarettes and marijuana: A secondary data analysis from the youth risk behavior survey. Journal of Addiction Medicine, 13(5), 362–336. DOI 10.1097/ADM.0000000000000506. [Google Scholar] [CrossRef]
32. Pontes, N., Ayres, C. G., Pontes, M. (2020). Trends in depressive symptoms and suicidality: Youth risk behavior survey 2009–2017. Nursing Research, 69(3), 176–185. DOI 10.1097/NNR.0000000000000424. [Google Scholar] [CrossRef]
33. Brener, N. D., Kann, L., Shanklin, S., Kinchen, S., Eaton, D. K. et al. (2016). Methodology of the youth risk behavior surveillance system–2013. Morbidity and Mortality Weekly Report: Recommendations and Reports, 62(1), 1–20. [Google Scholar]
34. Sabiston, C. M., Jewett, R., Ashdown-Franks, G., Belanger, M., Brunet, J. et al. (2016). Number of years of team and individual sport participation during adolescence and depressive symptoms in early adulthood. Journal of Sport and Exercise Psychology, 38(1), 105–110. DOI 10.1123/jsep.2015-0175. [Google Scholar] [CrossRef]
35. Brunet, J., Sabiston, C. M., Chaiton, M., Barnett, T. A., O’loughlin, E. et al. (2013). The association between past and current physical activity and depressive symptoms in young adults: A 10-year prospective study. Annals of Epidemiology, 23(1), 25–30. DOI 10.1016/j.annepidem.2012.10.006. [Google Scholar] [CrossRef]
36. Boone, E. M., Leadbeater, B. J. (2006). Game on: Diminishing risks for depressive symptoms in early adolescence through positive involvement in team sports. Journal of Research on Adolescence, 16(1), 79–90. DOI 10.1111/j.1532-7795.2006.00122.x. [Google Scholar] [CrossRef]
37. Eime, R. M., Young, J. A., Harvey, J. T., Charity, M. J., Payne, W. R. (2013). A systematic review of the psychological and social benefits of participation in sport for children and adolescents: Informing development of a conceptual model of health through sport. International Journal of Behavioral Nutrition and Physical Activity, 10, 98–119. DOI 10.1186/1479-5868-10-98. [Google Scholar] [CrossRef]
38. Wiles, N. J., Haase, A. M., Lawlor, D. A., Ness, A., Lewis, G. (2012). Physical activity and depression in adolescents: Cross-sectional findings from the ALSPAC cohort. Social Psychiatry and Psychiatric Epidemiology, 47(7), 1023–1033. DOI 10.1007/s00127-011-0422-4. [Google Scholar] [CrossRef]
39. Maras, D., Flament, M. F., Murray, M., Buchholz, A., Henderson, K. A. et al. (2015). Screen time is associated with depression and anxiety in Canadian youth. Preventive Medicine, 73, 133–138. DOI 10.1016/j.ypmed.2015.01.029. [Google Scholar] [CrossRef]
40. Zink, J., Belcher, B. R., Kechter, A., Stone, M. D., Leventhal, A. M. (2019). Reciprocal associations between screen time and emotional disorder symptoms during adolescence. Preventive Medicine Reports, 13, 281–288. DOI 10.1016/j.pmedr.2019.01.014. [Google Scholar] [CrossRef]
41. Boers, E., Afzali, M. H., Newton, N., Conrod, P. (2019). Association of screen time and depression in adolescence. JAMA Pediatrics, 173(9), 853–859. DOI 10.1001/jamapediatrics.2019.1759. [Google Scholar] [CrossRef]
42. Grøntved, A., Singhammer, J., Froberg, K., Møller, N. C., Pan, A. et al. (2015). A prospective study of screen time in adolescence and depression symptoms in young adulthood. Preventive Medicine, 81, 108–113. DOI 10.1016/j.ypmed.2015.08.009. [Google Scholar] [CrossRef]
43. Granic, I., Lobel, A., Engels, R. C. (2014). The benefits of playing video games. American Psychologist, 69(1), 66–78. DOI 10.1037/a0034857. [Google Scholar] [CrossRef]
44. Slater, M. D. (2007). Reinforcing spirals: The mutual influence of media selectivity and media effects and their impact on individual behavior and social identity. Communication Theory, 17(3), 281–303. DOI 10.1111/j.1468-2885.2007.00296.x. [Google Scholar] [CrossRef]
45. Pasch, K. (2010). Adolescent sleep, risk behaviors, and depressive symptoms: Are they linked? American Journal of Health Behavior, 34(2), 237–248. DOI 10.5993/AJHB.34.2.11. [Google Scholar] [CrossRef]
46. Wang, W., Du, X., Guo, Y., Li, W., Zhang, S. et al. (2021). Associations among screen time, sleep duration and depressive symptoms among Chinese adolescents. Journal of Affective Disorders, 284, 69–74. DOI 10.1016/j.jad.2021.01.082. [Google Scholar] [CrossRef]
47. Short, M. A., Booth, S. A., Omar, O., Ostlundh, L., Arora, T. (2020). The relationship between sleep duration and mood in adolescents: A systematic review and meta-analysis. Sleep Medicine Reviews, 52, 101311. DOI 10.1016/j.smrv.2020.101311. [Google Scholar] [CrossRef]
48. Dahl, R. E., Lewin, D. S. (2002). Pathways to adolescent health sleep regulation and behavior. Journal of Adolescent Health, 31(6), 175–184. DOI 10.1016/S1054-139X(02)00506-2. [Google Scholar] [CrossRef]
49. Owens, J., Wang, G., Lewin, D., Skora, E., Baylor, A. (2016). Association between short sleep duration and risk behavior factors in middle school students. Sleep, 40(1), 1–10. [Google Scholar]
50. Liu, X. (2004). Sleep and adolescent suicidal behavior. Sleep, 27, 1351–1358. DOI 10.1093/sleep/27.7.1351. [Google Scholar] [CrossRef]
51. Yap, M. B. H., Allen, N. B., Sheeber, L. (2007). Using an emotion regulation framework to understand the role of temperament and family processes in risk for adolescent depressive disorders. Clinical Child and Family Psychology Review, 10(2), 180–196. DOI 10.1007/s10567-006-0014-0. [Google Scholar] [CrossRef]
52. Winpenny, E. M., Van Harmelen, A. L., White, M., van Sluijs, E. M., Goodyer, I. M. (2018). Diet quality and depressive symptoms in adolescence: No cross-sectional or prospective associations following adjustment for covariates. Public Health Nutrition, 21(13), 2376–2384. DOI 10.1017/S1368980018001179. [Google Scholar] [CrossRef]
53. Liu, M. W., Chen, Q. T., Towne Jr, S. D., Zhang, J., Yu, H. J. et al. (2020). Fruit and vegetable intake in relation to depressive and anxiety symptoms among adolescents in 25 low-and middle-income countries. Journal of Affective Disorders, 261, 172–180. DOI 10.1016/j.jad.2019.10.007. [Google Scholar] [CrossRef]
54. Fulkerson, J. A., Sherwood, N. E., Perry, C. L., Neumark-Sztainer, D., Story, M. (2004). Depressive symptoms and adolescent eating and health behaviors: A multifaceted view in a population-based sample. Preventive Medicine, 38(6), 865–875. DOI 10.1016/j.ypmed.2003.12.028. [Google Scholar] [CrossRef]
55. Tajik, E., Latiffah, A. L., Awang, H., Siti Nur’asyura, A., Chin, Y. S. et al. (2016). Unhealthy diet practice and symptoms of stress and depression among adolescents in Pasir Gudang, Malaysia. Obesity Research & Clinical Practice, 10(2), 114–123. DOI 10.1016/j.orcp.2015.06.001. [Google Scholar] [CrossRef]
56. Skogen, J. C., Knudsen, A. K., Hysing, M., Wold, B., Sivertsen, B. (2016). Trajectories of alcohol use and association with symptoms of depression from early to late adolescence: The Norwegian longitudinal health behaviour study. Drug and Alcohol Review, 35(3), 307–316. DOI 10.1111/dar.12350. [Google Scholar] [CrossRef]
57. Chaiton, M. O., Cohen, J. E., O’loughlin, J., Rehm, J. (2009). A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public Health, 9, 356–367. DOI 10.1186/1471-2458-9-356. [Google Scholar] [CrossRef]
58. Pomerleau, O. F., Turk, D. C., Fertig, J. B. (1984). The effects of cigarette smoking on pain and anxiety. Addictive Behaviors, 9, 265–271. DOI 10.1016/0306-4603(84)90018-2. [Google Scholar] [CrossRef]
59. Harris, K. M., Gordon-Larsen, P., Chantala, K., Udry, J. R. (2006). Longitudinal trends in race/Ethnic disparities in leading health indicators from adolescence to young adulthood. Archives of Pediatrics & Adolescent Medicine, 160(1), 74–81. DOI 10.1001/archpedi.160.1.74. [Google Scholar] [CrossRef]
60. Squeglia, L. M., Tapert, S. F., Sullivan, E. V., Jacobus, J., Meloy, M. et al. (2015). Brain development in heavy-drinking adolescents. American Journal of Psychiatry, 172(6), 531–542. DOI 10.1176/appi.ajp.2015.14101249. [Google Scholar] [CrossRef]
61. Lubans, D., Richards, J., Hillman, C., Faulkner, G., Beauchamp, M. et al. (2016). Physical activity for cognitive and mental health in youth: A systematic review of mechanisms. Pediatrics, 138(3), e20161642. DOI 10.1542/peds.2016-1642. [Google Scholar] [CrossRef]
62. White, R. L., Babic, M. J., Parker, P. D., Lubans, D. R., Astell-Burt, T. et al. (2017). Domain-specific physical activity and mental health: A meta-analysis. American Journal of Preventive Medicine, 52(5), 653–666. DOI 10.1016/j.amepre.2016.12.008. [Google Scholar] [CrossRef]
63. Bennie, J. A., Teychenne, M., Tittlbach, S. (2020). Muscle-strengthening exercise and depressive symptom severity among a nationally representative sample of 23,635 German adults. Journal of Affective Disorders, 266, 282–287. DOI 10.1016/j.jad.2020.01.172. [Google Scholar] [CrossRef]
64. Bennie, J. A., de Cocker, K., Biddle, S. J. H., Teychenne, M. J. (2020). Joint and dose-dependent associations between aerobic and muscle-strengthening activity with depression: A cross-sectional study of 1.48 million adults between 2011 and 2017. Depress Anxiety, 37(2), 166–178. DOI 10.1002/da.22986. [Google Scholar] [CrossRef]
65. Yu, W., Sun, J., Wu, Y., Chen, S. T. (2021). Muscle-strengthening exercise links with lower odds for depression in adolescents. International Journal of Mental Health Promotion, 23(2), 277–288. DOI 10.32604/IJMHP.2021.016153. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools