 Open Access
Open Access
ARTICLE
Detrimental Effects of COVID-19 Measures on Mental Health and Social-Economic Disparities
1
School of Tourism, Hainan University, Haikou, 570228, China
2
Department of Education Sciences, Islamic Azad University of Gorgan, Gorgan, 471667636, Iran
* Corresponding Author: Narges Sanchuli. Email:
International Journal of Mental Health Promotion 2023, 25(1), 63-79. https://doi.org/10.32604/ijmhp.2022.022319
Received 04 March 2022; Accepted 01 August 2022; Issue published 29 November 2022
Abstract
The COVID-19 pandemic has struck nations worldwide, pushing worldwide health and socioeconomic systems to extreme limits. Various factors, such as drastic alterations in public environments, prolonged quarantine, revenue loss, and anxiety of disease contraction, have caused mental turmoil. Although there was a need to cope with an excess of psychological strain among the public, post-COVID patients, and those with a previously diagnosed psychiatric condition, mental health programs faced a substantial decline in services, mirroring the dramatic rise in psychological issues. Interestingly, certain coping strategies play protective or deleterious effects on mental health outcomes. Moreover, social media exposure has played a double-edged role in the mental health of the public during the pandemic, leaving grounds for further debates. Protean cultural themes have taken center stage in the discussion on social resilience and compliance to COVID-19 measures, driving their impact through certain work ethics, social capital, and public attitudes in different societies. On the other hand, exceedingly rising poverty rates cemented the deleterious economic impact of the pandemic. Attention has been called to the racial implications of the pandemic, driving millions of individuals with low socioeconomic position (SEP) and belonging to minority groups out of the paid workforce. Interestingly, we turn attention to an array of elements implicated in this dramatic effect, such as public transport, living arrangements, and health insurance coverage among these vulnerable groups. We attempt to address the mechanisms COVID-19 channeled its mental health and socioeconomic impacts by explaining the risk factors and pave the way for stronger crisis management in the future by evaluating the socioeconomic and psychological effects in stark detail.Keywords
COVID-19 cases have exponentially risen worldwide, and early in March 2020, WHO declared the progressively growing infection, a worldwide pandemic of emergent concern. At the beginning of April 2020, the pandemic caused 3.9 bn individuals (over half of the world’s population) to undergo concrete lockdown policies to stem the pandemic’s rapid outgrowth. As of August 2021, 197,368,310 people globally have been afflicted by SARS-CoV-2, pushing a drastic death toll up to 4,208,555 deaths worldwide [1]. The groundbreaking impact of these numbers is put into context by considering different outbreaks, including the 2003 severe acute respiratory syndrome (SARS) outbreak, which afflicted 8,000 people and caused 800 deaths. Indeed, significant morbidities and mortalities and profound financial fallouts of COVID-19 make it imperative to assess its sequelae on inextricably interconnected mental health and socioeconomic factors [2].
Most nations have enacted lockdown restrictions to curb the infection spike, including an extended curfew, strict social distancing measures, stay indoor orders, the compulsory shutdown of social events and recreational activities, closures of many business sectors and schools, and widespread travel bans [3]. Despite the mitigating effect of lockdown policies to stem the viral spread, researchers presume the ripple effect of COVID-19 struck could implicate in adverse economic, social, and psychiatric outcomes.
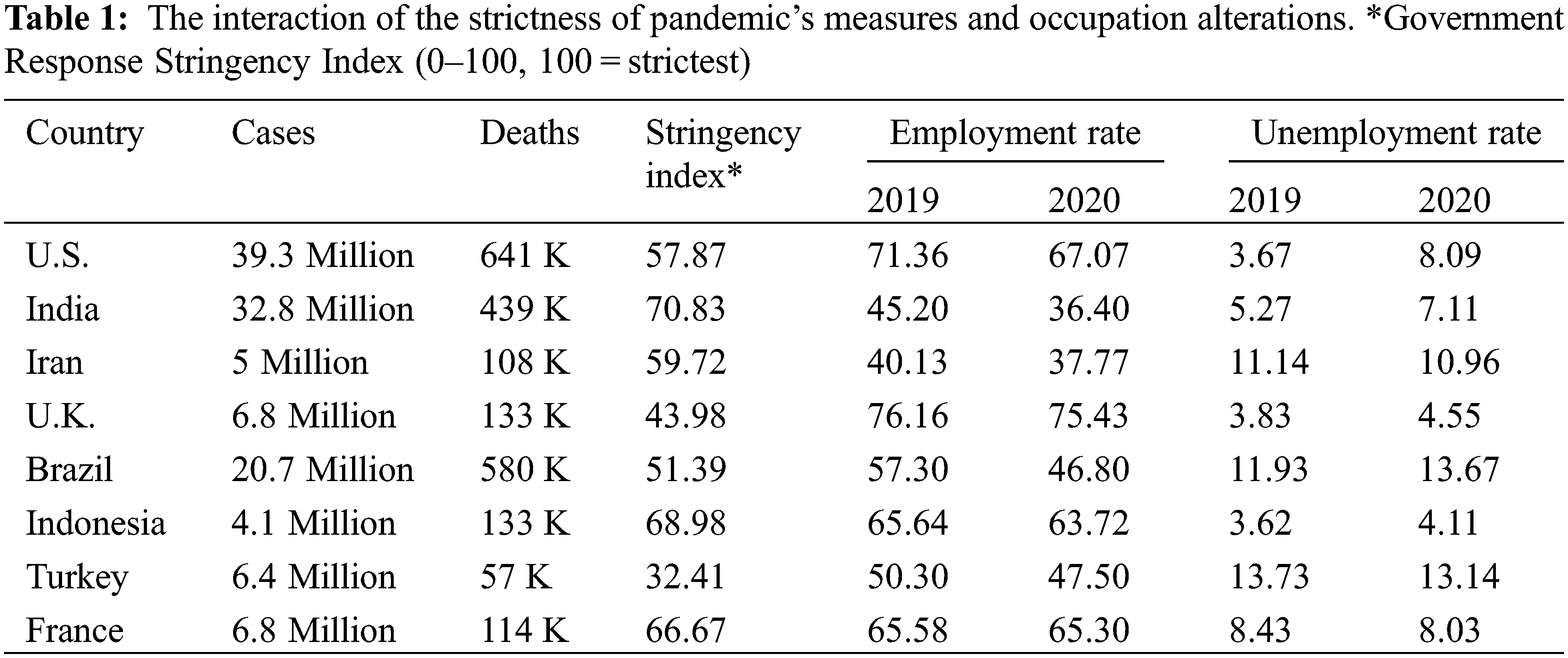
Compelling data intended the unprecedented fallout in liquidity as well as stocks dropping [4]. The International Labor Organization (ILO) investigations on the early days of the pandemic predicted a nosedive decline in jobs between an approximate array of 5.3 million and 24.7 million, increasing the worldwide unemployment rate from 4.89% and 5.65%, respectively (Table 1). These COVID-19-related job losses could take a toll of between 2140 to 9585 suicide commitments every year [5]. World Bank estimates that worldwide extreme poverty increases for the first time since the 1990s, and over 150 million individuals will fall below the absolute poverty line by 2021. Countries with lower income indexes, particularly countries facing fragility, conflict, and violence (FCV) challenges, are COVID-19 hardest hits due to the higher vulnerability of their health and social and financial structures. Of note, the COVID-19 outbreak has ramified business sectors differently; while healthcare and drug development services have faced an exponential rise in demand to contend with the infection, most other sectors are mandated to shut down or are slowed down due to supply chain disruptions. Also, a substantial portion of corporations had shifted to remote working. Taken together, the health system turmoil could collude in severe social harm and a financial downturn, contributing to an enormous economic recession [6].
Besides the COVID-19 crisis’s financial perturbations, the excessive health concerns to contain the infection, including protracted lockdown orders, social distancing, and the precariousness of the future, would imperatively affect the population’s psychological health resources and resilience. To add weight to this, in contrast to data on 2017–19, research on young adult U.S. and U.K. citizens in April 2020 witnessed a significant boost in mental turmoil [7]. There is ample evidence that two-tenths of individuals afflicted with coronavirus concomitantly show neuropsychological manifestations; also, the high-risk groups develop anxiousness, insomnia, posttraumatic stress syndrome (PTSS), and depressive symptoms. WHO surveys demonstrated that despite the robust increase in the call for psychiatric consultant services, in over 90% of nations, the community psychologic health programs are ceased or postponed. Thus, researchers speculate that insufficient evidence-based psychological aid resources may lead to an impending pandemic of mental health disorders [8]. Consistently, besides the excessive demands of prompting actions for the socioeconomic sequelae of the pandemic, further research to create appropriate scientific methods to address mental health implications and tailor resources hold a promise of better outcomes in perturbed people.
Viewing the pandemic’s impacts through the lens of public health authorities enables researchers to get novel insights into psychosocial and financial effects. In the hunt for the extent to which the pandemic influenced these perspectives, we cast about most of the relevant ongoing streams of scientific literature, organizing a full-scale dataset exploration, such as google scholar, MEDLINE, PsycARTICLES, Web of Science, and PubMed. The search query classifications encompass “COVID-19”, psychological effect, such as “mental*”, “psych*”, “psychology programs”, “anxi*”, “depress*”, and socioeconomics such as “social distancing”, “cop*”, “curfew policies”, “economic crisis”, combined together in various ways up to May 2022. Firstly, 117 records were identified through database searching, accompanied by 21 records explored through other resources. Secondly, upon omission of duplicates, 126 documents were further evaluated and screened, which led to the exclusion of 94 records. Thirdly, the eligibility of the remaining 32 records was further assessed by evaluating the full-text articles, which led to the exclusion of 2 full-text articles. Finally, we included 30 studies in our data extraction process. We restricted our search to English published and preprint peer-reviewed original papers with relevant content to our selected scope.
3 Mental Health Implications of the SARS-CoV-2 Outbreak
There is a plethora of relevant evidence regarding the COVID-19 implication in public mental well-being. Researchers asserted a broad array of contributing factors; firstly, the non-pharmacological interventions (NPIs) posed to stem the growing infection, including tightened social distancing measures; and protracted closures of educational, recreational, and financial facilities, are perceived to influence people’s psychological health worldwide. Secondly, financial upheavals such as unemployment and furloughs, resulting in loss of income and depletion of family’s savings, contribute to further mental distress. Thirdly, fear of infection and transmitting the virus to one’s social network, shock, and bereavement aggravate psychological pressures. These conditions orchestrate psychological manifestations in the pandemic era, such as drug abuse, sleep disorder, depression, and anxiousness. Noteworthy, there is a growing strand of literature ascribing the neuropsychiatric manifestations witnessed in COVID-19 patients (for instance, encephalitis, confusion, altered consciousness, and stroke) to the substantial brain tropism of the SARS-CoV-2 [9].
The psychological well-being of the public is the cornerstone for optimal public health and its viability. In this realm, the COVID-19 pandemic severely affects society’s resilience, and by providing a fertile ground for emotional disturbances to flourish, it hinders efficient public recuperation. Particularly, uncontrolled psychologic symptoms in frontline healthcare professionals could dampen their efficiency and enthusiasm at work, thus, insufficient response to the pandemic [10].
Despite immense research and clinical efforts spanning months to declare the variety of the pandemic’s psychiatric complications, the potential risk determinants, and different human sociodemographic statuses and their role in aggravating or attenuating the disease is yet to be understood. In the following sections, we have attempted to shed more lights on these factors and their modifying role in the pandemic.
3.1 Mental Health Services Have Been Widely Disrupted upon COVID-19 Hit
Considerable evidence has recognized the excessively accelerated call for psychological health programs worldwide. WHO declared that 65% of countries have faced a paucity of prevention and promotion community-based mental health programs in the high-risk groups, particularly in pediatrics, there is over 70% insufficiency in mental, neurological, and substance use (MNS) services. In addition, approximately three-quarters of young adults experience psychological peer support disruptions, and perinatal mental health services have been perturbed for at least 60% of women. Drastically, further assessments revealed that over 70% of student and workplace psychological health support programs are ceased or postponed, leaving people susceptible to mental sequelae of the pandemic [11].
Researchers have attributed the occurrence of these worldwide perturbations to the lack of enough health professionals with experience in giving psychological support (33%), inadequate amounts of face masks and disinfectants (30%), and the utilization of psychological support constructions such as field hospitals and isolation centers (in one-fifths of nations). In this realm, to reinforce the psychological support during the pandemic era, policymakers in 116 countries reinstated extended mental health programs in their COVID-19 response plans; howsoever, in less than 20% of these nations, the plans were accompanied by enough enacted financial support. This contributes to the hotly debated mental crisis in the post-pandemic era [12].
Notably, the prevalence of psychological issues was remarkably high even prior to the pandemic. Data from 2018 assessments asserted that 970 million individuals (13% of the worldwide burden of diseases) globally are afflicted with psychiatric illness or drug use complications. Howsoever, the expense of mental healthcare services hinders their deployment, as the 2013 U.S. data records that the medical treatment and prescriptions for psychologic problems and drug abuse cost 188.7 bn USD. WHO data underscores the profound shortages in global mental health resources, thus cementing the notion that COVID-19 repercussions could herald a deep mental health crisis without imminent unparalleled scale support, particularly in LIC and MICs [10].
3.2 Mental Health Detrimental Effect of COVID-19 in Association with a Previous Psychiatric Condition
As of the burst of SARS-CoV-2 cases, concerns about its impending mental sequelae have spiked, particularly among lifetime psychiatric patients. Of note, the evidence before the pandemic intends that in the U.S., one out of five of the population are afflicted with one or more chronic psychiatric conditions. Data analysis has explained that about 60% of the U.S. population faces COVID-19’s mental repercussions. Multiple independent avenues of research have attempted to shed light on these consequences; however, most evaluations are limited to cross-sectional assessments, making it elusive that mood changes ensue after the pandemic [13]. For instance, in a Chinese survey, in contrast to healthy people, participants with a lifetime burden of clinical psychologic conditions exerted sleep disorders, depressed emotional reactions, anxiousness, risky behaviors including alcohol and tobacco overconsumption, and increased rate of sedentary behaviors. In line with that, an Australian study witnessed individuals with self-perceived psychologic issues assert higher mental distress levels, fear of affliction, and less confidence and resilience to lockdown orders and undermined social support networks [14].
The severity of the psychological consequences of the crisis varies across public subgroups. The less extended social support networks and limited economic resources across individuals with psychological disorders contribute to further mental strains during the pandemic. Moreover, the WHO demonstrated that with quarantine in place, perturbation of the MNS support services and diminished access to mental healthcare programs progressively exacerbate the present psychiatric conditions and increase relapses [15]. On the other hand, intriguingly, help-seeking behavior and applying for external assistance from mental healthcare services during the crisis have been associated with substantial levels of fear of infection, depression, and anxiety disorders, compared with people with other coping strategies [16].
To get the ball rolling, a prestigious study on major Netherlands clinical psychiatric cohorts has extensively assessed COVID-19’s effect on previously mentally ill cases. Researchers witnessed a dose-response association between the burden of previous psychologic issues and the reported mental turmoil and opting for harmful coping strategies during the pandemic crisis. In fact, during the national quarantine, depressive symptoms, anxiousness, worrying, and loneliness are estimated to be significantly higher in individuals with a previous history of a psychiatric condition, which is in concordance with the pre-pandemic data [17]. It is noteworthy that despite increased rates of symptoms as of the lockdowns in healthy and minimal to moderately afflicted individuals, evaluations on the most severely afflicted people with chronic psychologic disorders in this study declare minimized symptoms or relief of clinical manifestations to some extent in this group. Researchers have intended multiple reasons for this, including the higher compatibility of severely mentally ill individuals to stay-at-home orders and isolations. Indeed, their routine lifestyle has become new normal living behavior to the rest of the population [18]. While others face progressively growing difficulties coping with stay-at-home orders, people with highly severe and chronic psychologic disorders have already developed a fixed daily plan at home to increase their safety. Although clinical severity of symptoms was evaluated on average scores across multiple waves over many years, various psychiatric disorders’ breadth and interactions were underestimated. Taken together, however, there is no evidence that the higher burden of the preexisting mental conditions imperatively leaves individuals more susceptible to the psychological effect of COVID-19 and exacerbations [14].
The devastating implication of the crisis on the people afflicted with psychological problems is undeniable, prompting mental healthcare professionals to reassess and organize resources to hinder their further frustrations.
3.3 Mental Health Sequelae in the Post-COVID-19 Conditions of the Patients
Leaving aside the straining course of the disease, COVID-19 affliction establishes a detrimental mood that is hostile to the patient’s mental health. Similarly, meta-analytic studies on severe acute respiratory syndrome’s (SARS) psychologic outcomes unveiled that approximately one-third of SARS inpatients experienced major depression, anxiousness, cognitive deficits, hallucination, and sleep disorders in the course of the disease or during the rehabilitation period [19]. Mounting evidence from the Ebola outbreak also leverages the fact that psychotic manifestations are common among afflicted individuals. Consistently, a recent cohort study on SARS-CoV-2 survivors proposed the profound rise in the mental illness diagnosis as post-COVID conditions in the aftermath of the acute and post-acute impacts of the coronavirus, concomitant with the self-isolation orders [20]. Scientists perceive coronavirus survivors’ deconditioning, stigma, and social exclusion as the most common causes of mood disturbances. Other clues for the rife neuropsychiatric manifestations to occur in the course of the infection are the multi-organ inflammatory syndrome (MIS) and the post-intensive care syndrome (PICS), which lead to lingering consequences [21].
On the whole, however, differential diagnosis, including masked previously undiagnosed psychiatric illness or coronavirus reinfection, should not be downplayed. Interestingly, with a delicate patient-focused theme, post-COVID conditions have yielded promising amelioration by implementing primary healthcare approaches to improve the quality of life and socio-psychologic well-being in afflicted individuals.
3.4 Risk Factors Implicated in Worse COVID-19 Outcomes
Researchers have appraised a broad spectrum of risk determinants worldwide through comprehensive surveys compounding the post-pandemic psychosocial consequences. Investigations in the U.K. have postulated that young age, female gender, and accounted in the high-risk group for the infection are among major contributors to mental illness. In the same line, studies in the eastern declared that well-educated young adults, single and divorced individuals, along with high exposure to COVID-19 patients and low perceived survival levels, entail psychologic turmoil [22]. By contrast, being men, having children (that is, crowded households >6 people), maintaining income, trust in healthcare providers, and less exposure to COVID-19 media could avert the adverse psychologic outcomes. Strikingly, living in extended families plays a protective role against the pandemic, representing the significance of family support across Asian society in response to stress [23]. In this perspective, it is noteworthy that the imposed physical distancing, which is pivotal to tackling the infection and particularly dampens the risk of contagiousness in nurses and doctors to their families, has negatively impacted the effectiveness of social support networks in alleviating the mental pressures [24].
Evaluations on the clinical course of the coronavirus infection have established that among the vast array of symptoms, coughing, headache and pharyngitis have a monumental impact on the pandemic’s psychological repercussions. On the other hand, compared to controls, adherence to personal protective equipment (PPE) and hand hygiene improve the perceived susceptibility to coronavirus transmission and thus reinforce positive mood [25].
3.5 The Impact of Engagement in Reward-Seeking and Threat-Avoidance Behaviors during the COVID-19 Outbreak
Across a broad range of coping strategies for the high load of stressors, research perceives that anxiousness disorders are entwined with threat-avoidance themes. Moreover, individuals with depressive symptoms tend to exert diminished compliance with the reward-seeking coping approach. Evaluations on coping themes in pregnant women have concluded that quarantine has strengthened social support networks for pregnant women as the family members are at home and dedicate time and consideration to them, which has contributed to less threat-avoidance behaviors and thus moderately decelerated anxiety among pregnant women. On the contrary, with the lockdown policies in place, hampering pregnant women’s access to essential obstetric care services accompanied by less involvement in social events has led to a significant decline in applying reward-seeking coping strategies and thus a substantial rise in major depression incurred [26,27].
3.6 Mental Health Deterioration in Association with the Social Media Exposure
Despite the great promise of the technology and social media platforms to accelerate communities’ awareness, safety, and support networks, pressing scientific assessments have cemented the contention that the upsurge in the exploitation of social media platforms is the primary culprit undermining public health resources by disseminating misinformation [22]. To get the ball rolling, the perceived boosted infodemic, which is rife with information on large scales, has gotten play in some respects, including a dramatic fold rise in stigma, inefficient health measures monitoring, amplified conflicts and violations, and reigniting intense debates on the effectiveness of COVID-19 measures. These downsides hamper health policies’ yield due to a lack of trust and accurate data and ramify the communities’ cohesion, thus establishing a hostile environment for the coronavirus to thrive [28].
It is widely accepted that the fear of SARS-CoV-2 contraction for individuals and their community network puts them under extreme mental upheaval. Besides this, multiple studies have presented puzzling evidence towards the positive association of the ruminating media coverage and the internet community’s far-reaching spread of pandemic metrics with unprecedentedly aggravated psychologic distress [28]. Following that, researchers utilizing multinominal logistic regression approaches on the data obtained from the healthcare system of china evaluated the effect of social media exposure on psychological well-being. Intriguingly, they demonstrated that upon imposition of quarantine in Wuhan, over half of the citizens with self-perceived excess exposure to media suffered from severe depressive symptoms, and one out of five experienced a combination of depressive and anxiety symptoms, which is two-fold higher than those with limited internet surfing during the same period [29].
Strikingly, the burgeoning rise in the SARS-CoV-2 cases harbingers flares of uncertainty and harmful cyber activities, which underscores extended calls for more profound progress in managing social media exposure to sustain public resilience. In this realm, United Nations (U.N.), early in May 2020, implemented action plans to tackle the infodemic and disturbing groundswell of anti-COVID-19 plans. In addition, WHO enacted Resolution WHA73.1 as a plan of action toward the pandemic, focusing on the crucial role of accurate information delivery and avoidance of disinformation spread and hampering menacing internet content against health policies in the way to stem the COVID-19 [30].
On the other page, an observational study examined over 10,000 pandemic-related Weibo posts at the Wuhan in the early days of the pandemic. They unveiled the anxiety and misplaced optimism concerning individuals and the community upon the burst of the COVID-19 outbreak [31]. The complexity of the links between the triangle of public health authorities, media, and general people is established through appraisal of the people’s social behaviors, concerns, and idea exchange while facing the rapidly changing load of news about the pandemic. Figuring out these connections that ramify social behaviors helps improve health policies and compliance. This is in line with the agenda-setting hypothesis, which underscores the progressively prominent role of news media in eliciting knowledge, choreographing the perception of reality, and highlighting specific topics on the public agenda [32].
4 Social Impact of the Pandemic
4.1 Critical Role of Social and Cultural Factors in the Efficacy of the Implemented Social Measures
Adherence to the life-changing social measures, particularly at the beginning of the pandemic before vaccine design, is a major determinant of COVID-19 outcomes. Researchers have exploited the stay-at-home orders as a chance to evaluate compliance with these policies through the lens of cultural perspectives, assuming a solid association with shared cultural beliefs. Work ethics and social capital consistently enhance adherence to the implemented NPIs [33].
Work ethics is considered of prominent value in terms of individuals’ adherence to the implemented governmental measures. Work ethics encompass an array of moral values and attitudes in the workplace atmosphere employees apply and perform accordantly. Adherence to the life-changing social measures, particularly at the beginning of the pandemic prior to vaccine design, is a major determinant of COVID-19 outcomes and strongly relies on shared cultural beliefs about work [34]. Alfano investigated the speculative aggravating or ameliorating role of work ethics on the COVID-19 outcomes in many European countries [35]. They witnessed the higher burden of the disease in nations with a constellation of perceptions centered on the value of work, such as the deification of workaholics, disparaging unemployed people who rely on financial cushions, and perceiving productivity increases by hard work.
In contrast, records from cultures maintaining a more balanced work-leisure lifestyle unfolded a substantial decline in the COVID-19 toll. However, controversy remains about nations considering work as a social responsibility to fulfill civic duty, which disclosed fewer afflicted individuals. The rationale lies in the presumed varying compliance of people to shelter-in-place orders driven by certain attitudes towards work value. This necessitates further considerations towards contemporary work values in society prior to implementing NPIs such as lockdown measures [36]. For instance, the abrupt shutdown of workplaces in cultures with high values for work, insufficient resources for smart working along with inadequate governmental support programs might lay a foundation for firstly the rise in mental disorders during quarantine. Secondly, in lingering periods, these may lead to rebound amplification of uncontrolled workforce with inadequate workplace safety measures ensuing mounting new cases compared to policies to keep firms afloat while establishing safe workplace atmospheres [35].
Social capital is defined as connections people tend to grow through interactions in society during life. Capital is the armamentarium to boost productivity; thus, social capital implies harnessing social assets to accrue production efficacy [37,38]. Bonding and bridging subgroups of social capital are implicated in the different levels of compliance with lockdown measures observed in communities. Bonding is a strong connection among people with shared interests, such as family members. Bridging are social links with lesser strength than bonding, commonly developed by intermediate parties bridging among colleagues in institutions [39]. To shed light on this, one hypothesis to address this focuses primarily on the people with bonding social capital that yield profound belonging to the group and distrust of outsiders. Hence, they reduce the risk of contracting the disease in their group by averting connection with untrusted individuals with unknown COVID profiles. Besides, they exhibit greater attention towards those at risk of COVID-19 contraction, such as the elderly [40].
Overall, social capital, by orchestrating the social networks, has come to play an impotent function in behavioral adaption to pandemic-associated changes. This is confirmed by the lower load of patients in countries with more outstanding social capital, particularly the bonding subgroup.
4.1.3 Public Attitudes and Behavior
Exploration of the contributing factors to NPIs’ non-adherence among the general public would improve outcomes. Researchers conducted a population-based cross-section study during the first wave of the pandemic in the U.S. to appraise the common perceptions regarding the efficacy and convenience of NPIs. The prevailing attitude toward NPIs was their high potency to decrease the risk of COVID-19 contraction (p = 0.014). Among 1,005 participants, although over one-third asserted their difficulty with NPIs, less than one percent mistrusted the total efficacy of NPIs in fending off the disease. Approximately one-third revealed their doubt about the effectiveness of the facemasks, and 20% declared concerns about the potency of the face shields in curbing the infection [41]. Interestingly, adherence to more intensely announced, rife and uncomplicated NPIs, including hand hygiene, was reportedly higher compared to more strenuous burdensome interventions, including the use of surface disinfectants and facemasks. Consistently, public health stakeholders should compile a range of resources to inform the people about the salient impact of interventions on diminishing the COVID-19 death toll. Establishing validated avenues for publishing pandemic-related knowledge to the public lies at the heart of providing a trustful atmosphere for deploying NPIs in the pandemic. Also, lowering the cost of sanitizers and attempts to make NPIs’ protocols simple and uncomplicated for the public hold a promise of better compliance [42].
4.2 Socioeconomic Disparities among Races Predispose Individuals to COVID-19
Epidemic curves have demonstrated significant racial segregation in COVID cases. In the same fashion, a Well-established stream of the literature on the link between race and SEP affirms their pivotal role in providing a fertile ground for COVID-19 susceptibility. Consistently, researchers disclosed that in the U.S., the mortality rate for Black Americans exceeded that of Whites by 40%, 178 deceased per 100 k population, and 124 per 100 k, respectively [43,44].
Although preliminary data disclosed a higher burden of disease in minorities and Blacks, whether the higher susceptibility to COVID-19 drives its impact by intrinsic and biological factors or acts through the environmental determinants is often hard to entangle. Notably, the commonly found clinical manifestations in COVID-19 cases, including hypertension and diabetes mellitus, are more pronounced among Black males, which raises ongoing debate on the implication of the innate racial risk determinants [45]. In controversy, despite the higher burden of COVID-19 affliction among African-Americans, mortality rates failed to show greater inpatient deaths between them compared to Whites, provided adjusting for covariates, which rules out higher fatality due to physiologic susceptibility, and implying the robust association between risk of exposure and the greater contraction rates [2,46]. To shed light on this, researchers indicated that a large proportion of Black Americans suffer from chronic physical and psychiatric conditions, substandard housing, and financial instabilities. Thus, lending additional support to the hypothesis that despite their up to 13% contribution to the U.S. population, due to their low SEP, African Americans are inordinately hit by the pandemic. Mortality rates across racial-ethnic minorities are related to the burden of chronic conditions, the proportion of older adults, and financial strains. Although, the implication of chronic morbidities and the share of older adults is more prominent upon the exposure to the economic downturn. Thus, implying that low socioeconomic status orchestrates the greater susceptibility among Blacks and ethnic minorities [47].
Researchers evaluated four distinct categories to address the mechanism of the environmental force’s involvement in the COVID-19 death toll. First, racial-based workforce alterations across the microeconomics, and second, the public transits’ utility rate during the outbreak concordantly modulates the risk of affliction to COVID-19 infection. Third, housing conditions contribute to the further spread of the infection, and fourth, the level of out-of-pocket expenditures for healthcare, which controls the disease progression or remission in afflicted individuals [48]. Herein, we will further discuss each category to assess their speculative role in orchestrating the environmental stressors and thus the COVID-19 outcomes.
4.3 Labor Force Sway in the Marketplace Due to the Pandemic’s Ripple Effect
Conflicting evidence has been compiled to address the workforce occupational changes in the pandemic era concerning race-ethnic issues. Researchers exploiting the CPS databank have recognized the slighter ramification of the SARS-CoV-2 upsurge-associated unemployment rise among Blacks. The latter is perceived to occur due to their remarkably increased propensity towards holding essential and frontline occupations, including healthcare, retail trade, and public transit. In contrast, data thus far estimated from the U.K. establishes that the ethnic minorities have faced unprecedented unemployment rates since the beginning of the outbreak [49].
On the other hand, Occupational Information Network (O*NET) in the U.S. has spotted jobs for their potency to adjust to smart working themes and underscored the least feasibility of the construction industry, healthcare services, mass transit jobs, accommodation, and food sector to adapt to remote working. Notably, the workers in these low-wage jobs, which require close proximity to others and thus, immensely increase the risk of contracting the infection in the workplace, are predominantly from Blacks and minorities [50].
We will further discuss how the pandemic choreographs its ramifications through economic channels in the financial section.
Commuting with public transit services is inevitable across frontline workers, particularly low-paid workers, which in turn, due to impeded complying with social distancing measures; inextricably contribute to further increase in the risk of SARS-CoV-2 exposure. Scientists perceive that the length of the way to work and limited physical space unprecedentedly accelerate the latter [51].
Commuting flows revealed different perturbation levels according to sociodemographic and labor market determinants, including local occupational framework and employment rates. For instance, downtowns hit harder than suburbs regarding mobility changes and social contacts. Also, compelling data evidenced that young adults and women were at higher risk of non-adherence to the transportation restrictions and expressing depressive symptoms, unhealthy diet, and low sleep quality [52]. This is further concreted by data from Gauvin et al., unveiling more significant mobility restrictions in areas with a higher load of the elderly population. On the same line, observational studies from many European countries cemented that disobeying the lockdown measures was more prominent among younger adults of lower SEP working in critical industries. Thus, considering the significant role of socioeconomic disparities in adherence to implemented measures, policymakers should be aware of specific characteristics of their target population to promote social responsibility and fend off the pandemic [53].
Another key player in increasing the rate of contraction is the housing condition. Researchers assert that for individuals who face the pronounced risk of COVID-19 contraction at the workplace, living in overcrowded multi-generational housing increases the risk of SARS-CoV-2 contagion to older parents. In particular, workplace-related COVID-19 spread is spurred while distance working is not applicable for individuals with low SEP due, in part, to limited space and isolation of the afflicted ones in the household. Researchers assume that African Americans and ethnic minority groups exert a higher propensity to disease transmission due to unsafe households. On the other hand, tangible resources of mental support and sharing of the household expenses are of critical advantages of the crowded dwellings [54].
Compelling evidence has cemented that the health insurance coverage across afflicted individuals holds a great promise of enhanced COVID-19 outcomes. Notably, over 9.2% of the U.S. population are uninsured. In this perspective, SEP choreographs accessibility to sufficient treatment in the course of the disease and hence, indirectly modulates case-mortality rates [55].
In sum, the data we thus far evaluated documents that the high rate of public-facing jobs held by minorities in the pandemic-hit marketplace, along with the amplified risk of transmission on the way to work and at crowded homes, compounds the risk of contraction across racial minorities. In the same fashion, high costs of medical therapy through lower access to health insurance adversely affect people with low SEP, which addresses the higher pandemic disadvantages across minorities [56].
Throughout the history of nations, particularly the U.S., they have had never experienced such a profound gross domestic product (GDP) hit similar to the early waves of the pandemic in April 2020. An overwhelming bulk of data has been discussed about the lingering effects of the pandemic on local revenues, money supply, workplace atmosphere, and unemployment level [57]. The U.S. Bureau of Labor Statistics (BLS) has unveiled the socioeconomic hit of the pandemic, indicating that government fiscal response could substantially resuscitate the global labor income, which had fallen by 8.2%, contributing to 4.5% of the global gross domestic product and worthy of 3.7 trillion USD. On the same line, compared to 2019, working hours declined by 8.9% in 2020, which is 4-fold greater in comparison with the worldwide economic crash in 2008, accounting for 227 million full-time jobs (Table 2). Together, these shreds of evidence paint a worrying picture of the pandemic’s economic impact and necessitate further evaluations of the challenges labor force and occupations will be entangled within the post-pandemic era [58].
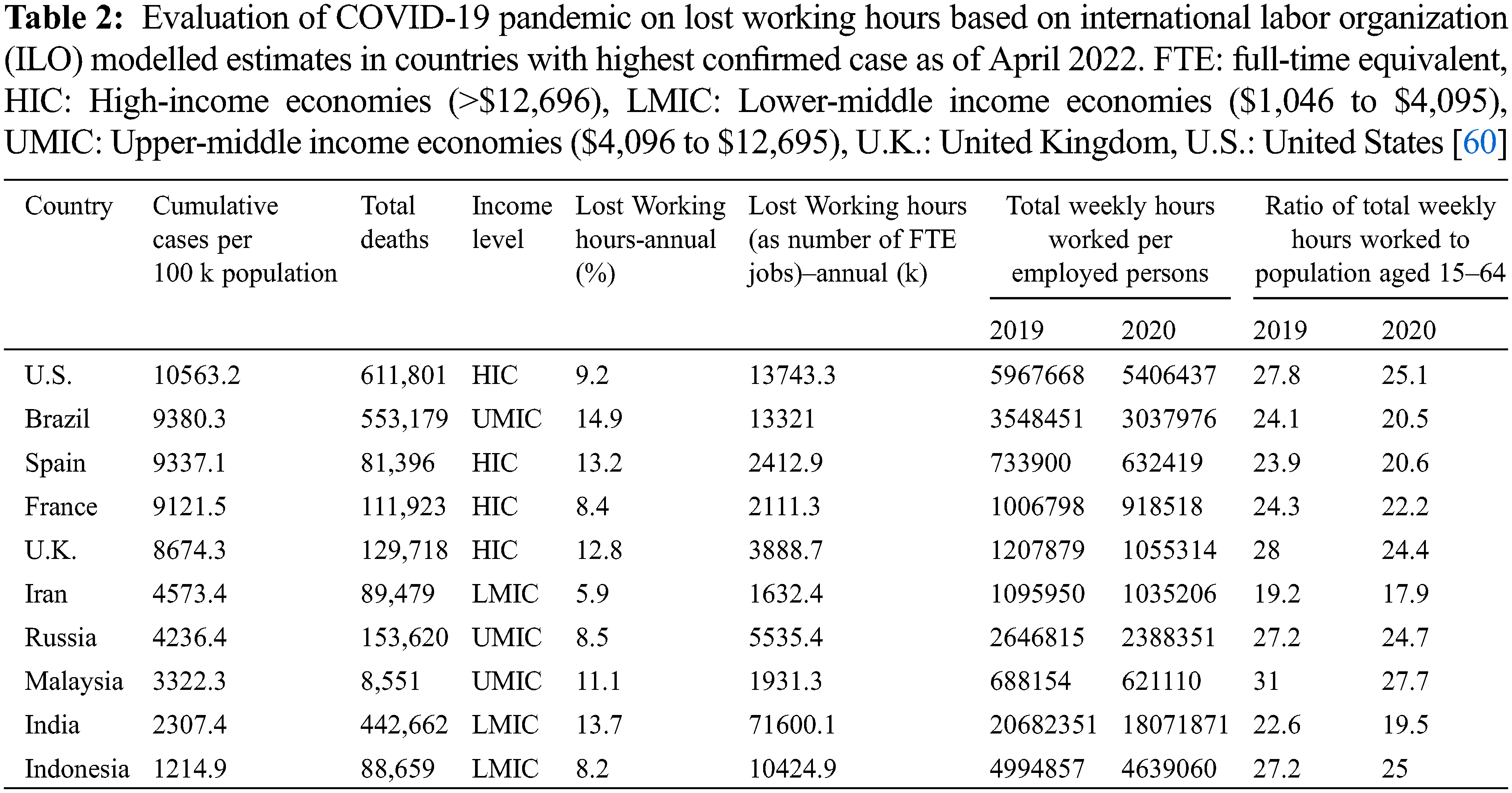
On the same line, multiple financial analytic associations, including OECD, have unveiled the remarked country-wide disparities in the labor economies and social policy responses in terms of alleviating the pandemic’s blow [59].
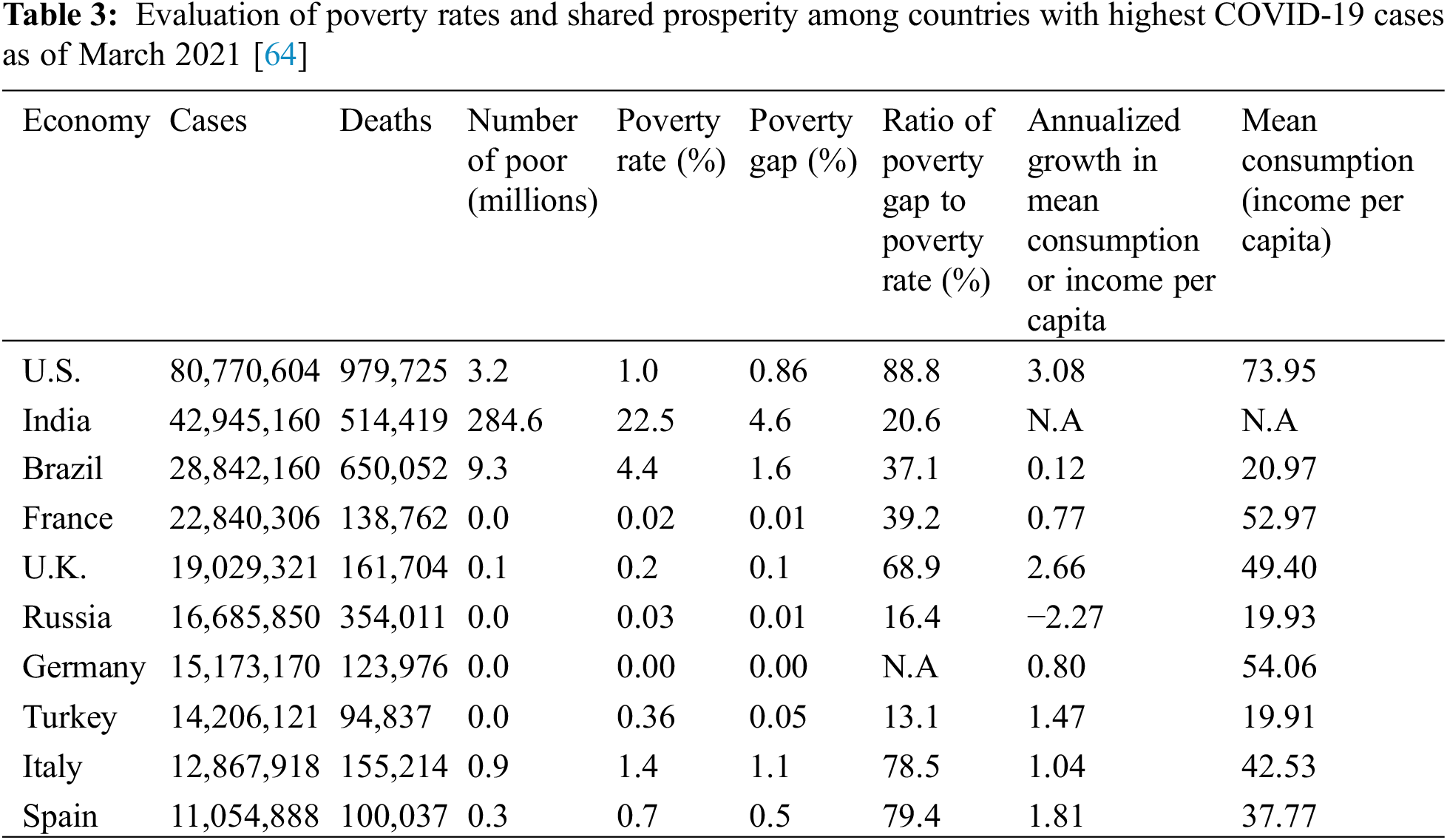
5.1 COVID-19 Impact on Poverty Rates Increase
World data lab has compiled a range of resources intending that emerging markets and developing economies experience an exponential rise in extreme poverty rates, defined as daily income less than 1.9 USD, which has been decelerating since 1998. In fact, the total number of people living in extreme poverty raised from 668 million in 2019 to 750 million in 2020, which will decline to 711 million by the end of 2021, and stabilize to 690 million in 2022. In addition, although United Nations (U.N.) had targeted the 2020 scape rate from extreme poverty to be 2.3 people/second, the rate was estimated to be −154.9 people/minute during 2020 [61]. Notably, scientists assume that 80% of individuals pushed into extreme poverty levels will be in MIC. World Bank data uncovered that in 2020, extreme poverty entangled around 9.5% of the global population [62]. Data before the pandemic had estimated the poverty rate to decelerate to 7.9% in 2020. On the same page, dampened growth in average income during 2019–2021 leads to a nosedive decline in shared prosperity, an index defined as the growth in revenue and consumption of the poorest 40% of the population (Table 3). In sum, revenue disparities and lower resilience across underprivileged families are inextricable without a proper policy response to the pandemic’s economic burden [63].
5.2 COVID-19 Impact on Occupations and Labor Force
According to BLS, the U.S. met its most extraordinary rise in the unemployment rate in April 2020 since the Great Depression in the 1930s, ranging between 14.5% to 19.5%. Consistently, the employment rate among the prime-age workforce has taken a nosedive, dropping to its lowest since 1949, by 51%. Annual employment indicators in 2020 disclose that the employment-to-population ratio declined by 3.2%, 4.8%, and 5.4% among Whites, Hispanics, and Blacks, respectively [65].
Inevitable categorization of occupations as essential such as healthcare and transport services, and non-essential, including the food sector, by the governmental quarantine measures has entailed certain pros and cons. In fact, given the higher exposure to COVID-19, the essential workers exert higher vulnerability and affliction rates; however, unemployment rates significantly rise among the non-essential sectors [66]. Interestingly, remote working has been widely harnessed by many companies to both reduce infection exposure and hamper unemployment. Although, it is notable that a vast proportion of the U.S. workforce, particularly, in low-wage jobs, including healthcare services, accommodation and food sector, public transition, and administrative positions, which are predominantly fared by low SEP workers, are not available remotely. Thus, leading to an increased risk of disease transmission among these low SEP workers [47,67].
The tradeoff between the unemployment rate and COVID-19 contraction is debatable. For example, although a substantial portion of the workforce in the food and accommodation sector is underpaid, which is a risk factor for greater coronavirus exposure, the rate of COVID-19 contraction is not statistically significant. This is attributed to the extensive closures because of the lockdowns, putting thousands of workers on furlough and layoff [68].
Future policymakers should consider three primary avenues to put their endeavors towards. Firstly, emergent and semi-urgent plans toward the acute ramifications of the outbreak on psychosocial and financial aspects. Secondly, long-term actions to choreograph countries’ health and economic resources to enhance the quality of life and provide support plans to keep firms afloat. Thirdly, resilience training programs focus on improving adaptability, sustainability, and inclusivity in the pandemic’s perturbed environment globally [69]. To further explore, economists believe that post-crisis financial response plans should consist of three main subjects. Firstly, a broad array of short-time works (STW) should be set up to achieve flexibility in the workplace and help employees sustain their jobs even with fewer earnings. Secondly, establish revenue protection arrangements for the self-employed and entrepreneurs. Thirdly, prioritizing particular challenges the marketplace is currently dealing with [70].
Given that 20% of the population suffers from mental health issues and 50% of the general public is at risk, public health authorities should prompt actions to avoid a mental turmoil outbreak. Notably, mental health support services through teletherapy have shown great promise [71]. Psychotherapeutic approaches such as motivational interviewing (MI), cognitive behavioral therapy (CBT), and crisis intervention accompanied with avoidance of pandemic-related infodemic and establishing a productive living environment are deemed to help achieve better psychologic results [71]. Management of the psychological outcomes in the labor force relies on several factors, including implementing plans to stem the disease spread in the workplace (i.e., PPE supply) and administering resilience training programs [72]. Moreover, supporting a healthy work/life balance for employees, transparent and science-based data about COVID-19 and its mental sequela, along with training them for future epidemics will contribute to more resilience. Constant evaluation of the workforce’s psychologic status, along with considering their specific demands while planning, are also essential mental health interventions in the workplace [73].
The pandemic’s toll, such as drastic alterations in public and workplace environments, extended quarantine, and revenue loss, have caused financial and mental turmoil. This paints a worrying picture regarding the public’s psychological health, particularly vulnerable individuals. The first contribution of this manuscript is to establish that a vast multitude of psychological conditions has been on the rise since the COVID-19 hit. This notion is corroborated by the steep decline in mental health services and the accelerating prevalence of psychological issues among vulnerable groups, including the COVID-19 survivors with and without mental conditions before the pandemic. As our remarked result of interest, we assessed the mental risk determinants, such as excessive exposure to social media and its interactions with the COVID-19 disease severity.
Moreover, stronger work-centered work ethics, bonding, and bridging social capital are among the main cultural principles contributing to the various public reactions around the world toward the pandemic’s measures. COVID-19 has also surfaced the racism and persistent health disparities that have severely harmed communities of color. We cemented that the high rate of frontline jobs held by minorities and the increased risk of infection transmission by commuting on public transport services and in crowded households, accompanied by high costs of medical therapy due to lower access to health insurance, adversely affected people with low SEP, which addresses the higher pandemic disadvantages across minorities. There are also highlights of economic effects, the unprecedented rise in the unemployment rate in April 2020 since the Great Depression in the 1930s and the fact that the number of people living in extreme poverty raised from 668 million in 2019 to 750 million in 2020 robustly affirms the economic effects of the pandemic.
Ethics Approval: Not applicable.
Consent to Participate: Authors agreed to publish this manuscript in this journal.
Availability of Data and Material: The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Code Availability: Not applicable.
Authorship: N.S and H.W designed the study, collected the relevant literature, drafted the data, and revised the manuscript. All authors reviewed the results and approved the final version of the manuscript.
Funding Statement: This study was financially supported by the Social Science Program of Hainan Province (HNSK(Y.B.)19-10) and the Program of the Ministry of Culture and Tourism (TYETP201552).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Velavan, T. P., Meyer, C. G. (2020). The COVID-19 epidemic. Tropical Medicine & International Health, 25(3), 278–280. DOI 10.1111/tmi.13383. [Google Scholar] [CrossRef]
2. Paul, A., Englert, P., Varga, M. (2021). Socio-economic disparities and COVID-19 in the USA. Journal of Physics: Complexity, 2(3), 035017. DOI 10.1088/2632-072X/ac0fc7. [Google Scholar] [CrossRef]
3. Birhane, M., Bressler, S., Chang, G., Clark, T., Dorough, L. et al. (2021). COVID-19 vaccine breakthrough infections reported to CDC—United States, January 1–April 30, 2021. Morbidity and Mortality Weekly Report, 70(21), 792–793. DOI 10.15585/mmwr.mm7021e3. [Google Scholar] [CrossRef]
4. Almeida, H. (2021). Liquidity management during the COVID-19 pandemic. Asia-Pacific Journal of Financial Studies, 50(1), 7–24. DOI 10.1111/ajfs.12322. [Google Scholar] [CrossRef]
5. Demmou, L., Franco, G., Calligaris, S., Dlugosch, D. (2021). Liquidity shortfalls during the COVID-19 outbreak: Assessment and policy responses. [Google Scholar]
6. Didier, T., Huneeus, F., Larrain, M., Schmukler, S. L. (2021). Financing firms in hibernation during the COVID-19 pandemic. Journal of Financial Stability, 53, 100837. [Google Scholar]
7. McGinty, E. E., Presskreischer, R., Han, H., Barry, C. L. (2020). Psychological distress and loneliness reported by US adults in 2018 and April 2020. Jama, 24(1), 93–94. DOI 10.1001/jama.2020.9740. [Google Scholar] [CrossRef]
8. Pierce, M., McManus, S., Jessop, C., John, A., Hotopf, M. et al. (2020). Says who? the significance of sampling in mental health surveys during COVID-19. The Lancet Psychiatry, 7(7), 567–568. DOI 10.1016/S2215-0366(20)30237-6. [Google Scholar] [CrossRef]
9. Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S. et al. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. DOI 10.1016/S2215-0366(20)30168-1. [Google Scholar] [CrossRef]
10. Pfefferbaum, B., North, C. S. (2020). Mental health and the COVID-19 pandemic. New England Journal of Medicine, 383(6), 510–512. DOI 10.1056/NEJMp2008017. [Google Scholar] [CrossRef]
11. McDowell, C. P., Herring, M. P., Lansing, J., Brower, C. S., Meyer, J. D. (2021). Associations between employment changes and mental health: US data from during the COVID-19 pandemic. Frontiers in Psychology, 12, 255. DOI 10.3389/fpsyg.2021.631510. [Google Scholar] [CrossRef]
12. Moreno, C., Wykes, T., Galderisi, S., Nordentoft, M., Crossley, N. et al. (2020). How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry, 7(9), 813–824. DOI 10.1016/S2215-0366(20)30307-2. [Google Scholar] [CrossRef]
13. Cullen, W., Gulati, G., Kelly, B. D. (2020). Mental health in the COVID-19 pandemic. QJM: An International Journal of Medicine, 113(5), 311–312. DOI 10.1093/qjmed/hcaa110. [Google Scholar] [CrossRef]
14. Pan, K. Y., Kok, A. A., Eikelenboom, M., Horsfall, M., Jörg, F. et al. (2021). The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. The Lancet Psychiatry, 8(2), 121–129. DOI 10.1016/S2215-0366(20)30491-0. [Google Scholar] [CrossRef]
15. Ma, D., Zhu, Q. (2022). Innovation in emerging economies: Research on the digital economy driving high-quality green development. Journal of Business Research, 145, 801–813. DOI 10.1016/j.jbusres.2022.03.041. [Google Scholar] [CrossRef]
16. Ogrodniczuk, J. S., Rice, S. M., Kealy, D., Seidler, Z. E., Delara, M. et al. (2021). Psychosocial impact of the COVID-19 pandemic: A cross-sectional study of online help-seeking Canadian men. Postgraduate Medicine, 133(7), 750–759. DOI 10.1080/00325481.2021.1873027. [Google Scholar] [CrossRef]
17. Usher, K., Durkin, J., Bhullar, N. (2020). The COVID-19 pandemic and mental health impacts. International Journal of Mental Health Nursing, 29(3), 315–318. DOI 10.1111/inm.12726. [Google Scholar] [CrossRef]
18. van Tilburg, T. G., Steinmetz, S., Stolte, E., van der Roest, H., de Vries, D. H. (2021). Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. The Journals of Gerontology: Series B, 76(7), e249–e255. DOI 10.1093/geronb/gbaa111. [Google Scholar] [CrossRef]
19. Jabbour, D., Masri, J. E., Nawfal, R., Malaeb, D., Salameh, P. (2022). Social media medical misinformation: Impact on mental health and vaccination decision among university students. Irish Journal of Medical Science (1971-), 1–11. DOI 10.1007/s11845-022-02936-9. [Google Scholar] [CrossRef]
20. Ohannessian, C. M. (2021). Introduction to the special issue: The impact of the COVID-19 pandemic on the lives of emerging adults. Emerging Adulthood, 9(5), 431–432. [Google Scholar]
21. Zhao, Y., Wang, Z. (2022). Subset simulation with adaptable intermediate failure probability for robust reliability analysis: An unsupervised learning-based approach. Structural and Multidisciplinary Optimization, 65(6), 1–22. [Google Scholar]
22. Han, R. H., Schmidt, M. N., Waits, W. M., Bell, A. K., Miller, T. L. (2020). Planning for mental health needs during COVID-19. Current Psychiatry Reports, 22(12), 1–10. DOI 10.1007/s11920-020-01189-6. [Google Scholar] [CrossRef]
23. Bhar, S., Bhattacharya, D., Bose, S. (2020). Analysing mental health of India during COVID using twitter. [Google Scholar]
24. Ma, H., Qiao, H., Qu, H., Wang, H., Huang, Y. et al. (2020). Role stress, social support and occupational burnout among physicians in China: A path analysis approach. International Health, 12(3), 157–163. DOI 10.1093/inthealth/ihz054. [Google Scholar] [CrossRef]
25. Leung, C. C., Lam, T. H., Cheng, K. K. (2020). Mass masking in the COVID-19 epidemic: People need guidance. Lancet, 395, 945–947. DOI 10.1016/S0140-6736(20)30520-1. [Google Scholar] [CrossRef]
26. Dong, H., Hu, R., Lu, C., Huang, D., Cui, D. et al. (2021). Investigation on the mental health status of pregnant women in China during the pandemic of COVID-19. Archives of Gynecology and Obstetrics, 303(2), 463–469. DOI 10.1007/s00404-020-05805-x. [Google Scholar] [CrossRef]
27. Hudd, T., Moscovitch, D. A. (2022). Reconnecting in the face of exclusion: Individuals with high social anxiety May feel the push of social pain, but not the pull of social rewards. Cognitive Therapy and Research, 46(2), 420–35. [Google Scholar]
28. Gao, J., Zheng, P., Jia, Y., Chen, H., Mao, Y. et al. (2020). Mental health problems and social media exposure during COVID-19 outbreak. PLoS One, 15(4), e0231924. DOI 10.1371/journal.pone.0231924. [Google Scholar] [CrossRef]
29. Mokona, H., Yohannes, K., Ayano, G. (2020). Youth unemployment and mental health: Prevalence and associated factors of depression among unemployed young adults in gedeo zone, southern Ethiopia. International Journal of Mental Health Systems, 14(1), 1–11. DOI 10.1186/s13033-020-00395-2. [Google Scholar] [CrossRef]
30. Almeida, M., Shrestha, A. D., Stojanac, D., Miller, L. J. (2020). The impact of the COVID-19 pandemic on women’s mental health. Archives of Women’s Mental Health, 23(6), 741–748. DOI 10.1007/s00737-020-01092-2. [Google Scholar] [CrossRef]
31. Lv, Z., Chen, D., Lv, H. (2022). Smart city construction and management by digital twins and BIM big data in COVID-19 scenario. ACM Transactions on Multimidia Computing Communications and Applications. DOI 10.1145/3529395. [Google Scholar] [CrossRef]
32. Xu, Q., Shen, Z., Shah, N., Cuomo, R., Cai, M. et al. (2020). Characterizing weibo social media posts from Wuhan, China during the early stages of the COVID-19 pandemic: Qualitative content analysis. JMIR Public Health and Surveillance, 6(4), e24125. DOI 10.2196/24125. [Google Scholar] [CrossRef]
33. Bonetto, E., Dezecache, G., Nugier, A., Inigo, M., Mathias, J. D. et al. (2021). Basic human values during the COVID-19 outbreak, perceived threat and their relationships with compliance with movement restrictions and social distancing. PLoS One, 16(6), e0253430. DOI 10.1371/journal.pone.0253430. [Google Scholar] [CrossRef]
34. Farkas, K. J., Romaniuk, J. R. (2020). Social work, ethics and vulnerable groups in the time of coronavirus and COVID-19. Society Register, 4(2), 67–82. DOI 10.14746/sr.2020.4.2.05. [Google Scholar] [CrossRef]
35. Ohrnberger, J., Segal, A. B., Forchini, G., Miraldo, M., Skarp, J. et al. (2021). The impact of a COVID-19 lockdown on work productivity under good and poor compliance. European Journal of Public Health, 31(5), 1009–1015. [Google Scholar]
36. Liu, S., He, X., Chan, F. T., Wang, Z. (2022). An extended multi-criteria group decision-making method with psychological factors and bidirectional influence relation for emergency medical supplier selection. Expert Systems with Applications, 202, 117414. DOI 10.1016/j.eswa.2022.117414. [Google Scholar] [CrossRef]
37. Alfano, V. (2022). Does social capital enforce social distancing? The role of bridging and bonding social capital in the evolution of the pandemic. Economia Politica, 1–21. DOI 10.1007/s40888-021-00255-3. [Google Scholar] [CrossRef]
38. Alfano, V., Ercolano, S. (2021). Social capital, quality of institutions and lockdown. Evidence from Italian provinces. Structural Change and Economic Dynamics, 59, 31–41. DOI 10.1016/j.strueco.2021.08.001. [Google Scholar] [CrossRef]
39. Chen, J. J., Jiang, T. N., Liu, M. F. (2021). Family socioeconomic status and learning engagement in Chinese adolescents: The multiple mediating roles of resilience and future orientation. Frontiers in Psychology, 12, 714346. DOI 10.3389/fpsyg.2021.714346. [Google Scholar] [CrossRef]
40. Alfano, V., Ercolano, S. (2022). Stay at home! Governance quality and effectiveness of lockdown. Social Indicators Research, 159(1), 101–123. DOI 10.1007/s11205-021-02742-3. [Google Scholar] [CrossRef]
41. Kantor, B. N., Kantor, J. (2020). Non-pharmaceutical interventions for pandemic COVID-19: A cross-sectional investigation of US general public beliefs, attitudes, and actions. Frontiers in Medicine, 7, 384. DOI 10.3389/fmed.2020.00384. [Google Scholar] [CrossRef]
42. Chen, Y., Sivakumar, V. (2021). Investigation of finance industry on risk awareness model and digital economic growth. Annals of Operations Research, 1–22. DOI 10.1007/s10479-021-04287-7. [Google Scholar] [CrossRef]
43. Wiemers, E. E., Abrahams, S., AlFakhri, M., Hotz, V. J., Schoeni, R. F. et al. (2020). Disparities in vulnerability to severe complications from COVID-19 in the United States. National Bureau of Economic Research. DOI 10.3386/w27294. [Google Scholar] [CrossRef]
44. Fabic, M. S., Choi, Y., Bishai, D. (2020). Deaths among COVID cases in the United States: Racial and ethnic disparities persist. medRxiv. DOI 10.1101/2020.11.15.20232066. [Google Scholar] [CrossRef]
45. Bowleg, L. (2020). We’re not all in this together: On COVID-19, intersectionality, and structural inequality. American Public Health Association, 917. DOI 10.2105/AJPH.2020.305766. [Google Scholar] [CrossRef]
46. Krieger, N. (2020). ENOUGH: COVID-19, structural racism, police brutality, plutocracy, climate change—and time for health justice, democratic governance, and an equitable, sustainable future. American Public Health Association, 110, 1620–1623. DOI 10.2105/AJPH.2020.305886. [Google Scholar] [CrossRef]
47. Garnier, R., Benetka, J. R., Kraemer, J., Bansal, S. (2021). Socioeconomic disparities in social distancing during the COVID-19 pandemic in the United States: Observational study. Journal of Medical Internet Research, 23(1), e24591. DOI 10.2196/24591. [Google Scholar] [CrossRef]
48. Khanijahani, A., Iezadi, S., Gholipour, K., Azami-Aghdash, S., Naghibi, D. (2021). A systematic review of racial/ethnic and socioeconomic disparities in COVID-19. International Journal for Equity in Health, 20(1), 1–30. DOI 10.1186/s12939-021-01582-4. [Google Scholar] [CrossRef]
49. Brooks, M. M., Mueller, J. T., Thiede, B. C. (2021). Rural-urban differences in the labor-force impacts of COVID-19 in the United States. Socius, 7, 23780231211022094. DOI 10.1177/23780231211022094. [Google Scholar] [CrossRef]
50. Bueno, M., Perez, F., Valerio, R., Areola, E. M. Q. (2022). A usability study on google site and wordwall .net: Online instructional tools for learning basic integration amid pandemic. Journal of Global Business and Social Entrepreneurship (GBSE), 7(23), 61–71. [Google Scholar]
51. Polzin, S., Choi, T. (2021). COVID-19’s effects on the future of transportation. United States Department of Transportation, Office of the Assistant Secretary for Research and Technology. DOI 10.21949/1520705. [Google Scholar] [CrossRef]
52. Yao, L., Li, X., Zheng, R., Zhang, Y. (2022). The impact of Air pollution perception on urban settlement intentions of young talent in China. International Journal of Environmental Research and Public Health, 19(3), 1080. DOI 10.3390/ijerph19031080. [Google Scholar] [CrossRef]
53. Gauvin, L., Bajardi, P., Pepe, E., Lake, B., Privitera, F. et al. (2021). Socio-economic determinants of mobility responses during the first wave of COVID-19 in Italy: From provinces to neighbourhoods. Journal of the Royal Society Interface, 18(181), 20210092. DOI 10.1098/rsif.2021.0092. [Google Scholar] [CrossRef]
54. Verdery, A. M., Smith-Greenaway, E., Margolis, R., Daw, J. (2020). Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proceedings of the National Academy of Sciences, 117(30), 17695–17701. DOI 10.1073/pnas.2007476117. [Google Scholar] [CrossRef]
55. Jordà, Ò., Singh, S. R., Taylor, A. M. (2020). Longer -run economic consequences of pandemics. Covid Economics: Vetted and Real-Time Papers, 1, 1–15. [Google Scholar]
56. Ramgobin, D., McClafferty, B., Kramer, C., Golamari, R., McGillen, B. et al. (2021). Papering over the cracks: COVID-19’s amplification of the failures of employer-based health insurance coverage. Journal of Community Hospital Internal Medicine Perspectives, 11(1), 107–110. DOI 10.1080/20009666.2020.1851869. [Google Scholar] [CrossRef]
57. Bagchi B, Chatterjee S, Ghosh R, Dandapat D. (2020). Impact of COVID-19 on global economy. In: Coronavirus outbreak and the great lockdown 2020, 15–26. Springer, Singapore. [Google Scholar]
58. Wang, C., Wang, D., Abbas, J., Duan, K., Mubeen, R. (2021). Global financial crisis, smart lockdown strategies, and the COVID-19 spillover impacts: A global perspective implications from Southeast Asia. Frontiers in Psychiatry, 12. DOI 10.3389/fpsyt.2021.643783. [Google Scholar] [CrossRef]
59. Obayelu, A. E., Edewor, S. E., Ogbe, A. O. (2020). Trade effects, policy responses and opportunities of COVID-19 outbreak in Africa. Journal of Chinese Economic and Foreign Trade Studies, 14(1), 44–59. [Google Scholar]
60. Lee, S., Schmidt-Klau, D., Verick, S. (2020). The labour market impacts of the COVID-19: A global perspective. The Indian Journal of Labour Economics, 63(1), 11–15. DOI 10.1007/s41027-020-00249-y. [Google Scholar] [CrossRef]
61. Valensisi, G. (2020). COVID-19 and global poverty: Are LDCs being left behind? The European Journal of Development Research, 32(5), 1535–1557. [Google Scholar]
62. Huang, P. H. (2020). Pandemic emotions: The good, the bad, and the unconscious-implications for public health, financial economics, law, and leadership. Northwestern Journal of Law & Social Policy, 16, 81. [Google Scholar]
63. Tandon, A., Ivatts, S., Cowley, P., Roubal, T., Dodd, R. et al. (2020). Economic contraction from COVID-19 in the Pacific: Implications for health financing. Health Systems & Reform, 6(1), e1847991. [Google Scholar]
64. Managi, S. (2018). Accounting for the inclusive wealth of nations: Key findings of the IWR 2018. In: Inclusive wealth report 2018, pp. 3–52. Routledge. [Google Scholar]
65. Coibion, O., Gorodnichenko, Y., Weber, M. (2020). Labor markets during the COVID-19 crisis: A preliminary view. National Bureau of Economic Research. DOI 10.3386/w27017. [Google Scholar] [CrossRef]
66. Falvey, J. R., Krafft, C., Kornetti, D. (2020). The essential role of home-and community-based physical therapists during the COVID-19 pandemic. Physical Therapy, 100(7), 1058–1061. DOI 10.1093/ptj/pzaa069. [Google Scholar] [CrossRef]
67. Zheng, G., Zhang, X., Wang, Y., Ma, M. (2021). The strengthening mechanism of the relationship between social work and public health under COVID-19 in China. International Journal of Environmental Research and Public Health, 18(19), 9956. [Google Scholar]
68. Côté, D., Durant, S., MacEachen, E., Majowicz, S., Meyer, S. et al. (2021). A rapid scoping review of COVID-19 and vulnerable workers: Intersecting occupational and public health issues. American Journal of Industrial Medicine, 64(7), 551–566. DOI 10.1002/ajim.23256. [Google Scholar] [CrossRef]
69. Issa, U. H., Balabel, A., Abdelhakeem, M., Osman, M. (2021). Developing a risk model for assessment and control of the spread of COVID-19. Risks, 9(2), 38. DOI 10.3390/risks9020038. [Google Scholar] [CrossRef]
70. Hijzen, A., Martin, S. (2013). The role of short-time work schemes during the global financial crisis and early recovery: A cross-country analysis. IZA Journal of Labor Policy, 2(1), 1–31. [Google Scholar]
71. Cheng, P., Xia, G., Pang, P., Wu, B., Jiang, W. et al. (2020). COVID-19 epidemic peer support and crisis intervention via social media. Community Mental Health Journal, 56(5), 786–792. DOI 10.1007/s10597-020-00624-5. [Google Scholar] [CrossRef]
72. Ma, D., Zhang, C., Hui, Y., Xu, B. (2022). Economic uncertainty spillover and social networks. Journal of Business Research, 145, 454–467. DOI 10.1016/j.jbusres.2022.03.015. [Google Scholar] [CrossRef]
73. Dewa, C. S., McDaid, D.(2011). Investing in the mental health of the labor force: Epidemiological and economic impact of mental health disabilities in the workplace. In: Work accommodation and retention in mental health 2011, pp. 33–51. New York, NY: Springer. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools