 Open Access
Open Access
ARTICLE
Effects of Health Qigong Exercise on Depression and Anxiety in Patients with Parkinson’s Disease
1
School of Physical Education, Yunnan Minzu University, Kunming, 650031, China
2
School of Rehabilitation, Sport and Psychology, AECC University College, Bournemouth, BH52DF, UK
3
Body-Brain-Mind Laboratory, School of Psychology, Shenzhen University, Shenzhen, 518060, China
4
Chinese Traditional Regimen Exercise Intervention Research Center, Beijing Sport University, Beijing, 100084, China
5
Foreign Language School, Yunnan Minzu University, Kunming, 650031, China
6
College of Sports Science, Jishou University, Jishou, 416000, China
7
Hunan Academy of Education Sciences, Changsha, 410082, China
* Corresponding Author: Shenghua Lu. Email: lushenghua6666@126
International Journal of Mental Health Promotion 2022, 24(6), 855-867. https://doi.org/10.32604/ijmhp.2022.021508
Received 18 January 2022; Accepted 25 March 2022; Issue published 28 September 2022
Abstract
Objective: This study explored the effects of Health Qigong exercise on depression and anxiety in patients with Parkinson’s disease (PD). Methods: A total of 42 volunteers who met the inclusion criteria were recruited and randomly allocated into the experimental group and the control group. The experimental group carried out 60-minute sessions of Health Qigong exercise five times a week for 12 weeks while the control group did not perform any regular physical exercise. Data on cognitive impairment, psychomotor retardation, somatic anxiety, weight loss and sleep disorders, the sum score of the 17-item Hamilton Depression Rating Scale (HDRS-17), state anxiety, trait anxiety as well as the sum score of the State-Trait Anxiety Inventory (STAI) were collected for three repeated measurements (baseline, 6, and 12 weeks). Results: Significant differences were observed in depression, state anxiety, trait anxiety, cognitive impairment and psychomotor retardation in the experimental group but no difference in somatic anxiety, weight loss and sleep disorders. Conclusion: Health Qigong exercise can pose positive psychological effects and alleviate the depression and anxiety in patients with Parkinson’s disease. It can be applied as an accessible supplement to the existent drug treatment for PD.Keywords
Depression, also depressive disorder is mental disease which has negative influences on how a person feels, thinks, and behaves, and can cause a variety of physical and emotional troubles, such as feeling sad, obesity, loss of interest, sleeping, slowed movements, purposeless physical activity, and thoughts of suicide [1]. Severe cognitive impairment was found to be 6.7%–25.2% worldwide, and the incidence of depression in the elderly was about 2.8%–22.5%; there was a high probability of coincidence between the two conditions [2]. Anxiety is broadly defined as the anticipation of future threat or danger [3]. The symptoms manifest as difficulty in concentration, low work efficiency, night sweats, choking, and frequent urination, which may be accompanied by tinnitus, blurred vision, and dizziness in severe cases [4]. As depression and anxiety often accompany each other, treatment methods can be applied to both conditions, including drug therapy, medical devices, psychological counseling, nursing, and exercise intervention [5,6].
Parkinson’s disease (PD) is a progressive neurodegenerative movement disorder with core clinical motor features of bradykinesia in combination with rest tremor, rigidity, or both [7]. The symptoms can be categorized according to motor dysfunction and non-motor dysfunction. In non-motor dysfunction, the incidence of depression and anxiety is high. Approximately 17% of patients with PD suffer depression and anxiety [8]. They often resist treatment and socialization, which seriously affects their quality of life. Physical exercise is increasingly used in the field of disease rehabilitation and adjuvant therapy, and its uniqueness has been shown in intervention studies on emotions. Studies on exercise intervention in the field of Parkinson’s depression have mainly adopted systematic training methods, Health Qigong, aerobic exercise, and yoga [9–13].
Health Qigong is the 62nd sport officially recognized by the General Administration of Sport of China. There are nine Health Qigong exercises: Yijingjing Health Qigong, Wuqinxi Health Qigong, Liuzijue Health Qigong, Baduanjin Health Qigong, Twelve-Movement Daoyin Health Qigong, Shierduanjin Health Qigong, Dawu Health Qigong, Mawangdui Daoyinshu Health Qigong and Tai Chi Health Rod Health Qigong. All are characterized as “three integrated into one,” whereby practitioners achieve a state of physical and mental relaxation through a combination of physical movement, breathing, and meditation. Health Qigong is accessible to all ages for health with moderate-intensive movements.
It has been widely used in scientific research on chronic disease prevention and treatment and disease rehabilitation. Fan and her team [14] proved that that the 8-week (60 min per session, five times per week) Health Qigong intervention manifested a significantly positive effect on mood and cognitive ability with increased total scores, attention scores, and delayed memory in the experimental group with the measurements of the Simplified Profile of Mood States (POMS) and Montreal Cognitive Assessment (MoCA). Zhang et al. [15] applied the Beck Anxiety Inventory (BAI) for measurement and found that 10-weeks Health Qigong exercise improved the gait and relieved depression of the patients with PD. The positive effect was enhanced with prolonged intervention duration. Liu and colleagues [16] proved the intervention effect of Baduanjin Health Qigong on the cognitive ability in patients with PD. Xiao and her colleagues [17] also found that Health Qigong improved neuron activity in patients with PD and guided them into a positive mood state while their motor dysfunction was significantly improved. With all these studies, it can be reasonably inferred that Health Qigong may have a positive impact on anxiety and depression in patients with PD.
This study investigated the application of Health Qigong exercise to patients with PD for psychological intervention, analyzing their scores (baseline, 6, and 12 weeks) in the 17-item Hamilton Depression Rating Scale (HDRS-17) and the State-Trait Anxiety Inventory (STAI) to prove that the combined ten Health Qigong movements are suitable and workable for relieving anxiety and depression in patients with PD.
This study was a 12-week intervention trial of Health Qigong exercise with three repeated measurements (baseline, 6, and 12 weeks) to assess its effects on depression and anxiety in patients with PD. The intervention comprised a combination of Health Qigong movements. Written informed consent was obtained from the patients with PD.
A total of 42 patients with PD were recruited from Beijing Aerospace Hospital and Yantai Yuhuangding Hospital of Shandong Province, 27 from Beijing and 15 from Yantai City. A written informed consent was obtained from all participants. They were randomized to different groups in a single-blind design. The inclusion criteria were: (1) meeting the clinical diagnostic criteria for idiopathic PD by the UK Parkinson Disease Association Brain Bank; (2) diagnosed with PD at levels 1–3 (mild to moderate) in Rating Table [18] complicated by depression and anxiety; (3) no changes in medication during the trial, confirmed by their physicians; (4) able to follow the instructor’s directions, fully understand the training content, and carry out Health Qigong exercises; (5) no other concomitant diseases throughout the trial; (6) no regular physical training in the past year. The exclusion criteria were: (1) having cardiovascular and cerebrovascular diseases; (2) having ever received a deep electrode implantation in the brain; and (3) having ever learned and practiced Health Qigong in the past year. Six participants (three from each group) dropped out. Thirty-six participants remained in the study for data analyses (Fig. 1). They all maintained their routine diet, medication, and activities throughout the study. The trial was registered at the Chinese Clinical Trial Register (http://www.chictr.org.cn/index.aspx, ChiCTR2100046918).
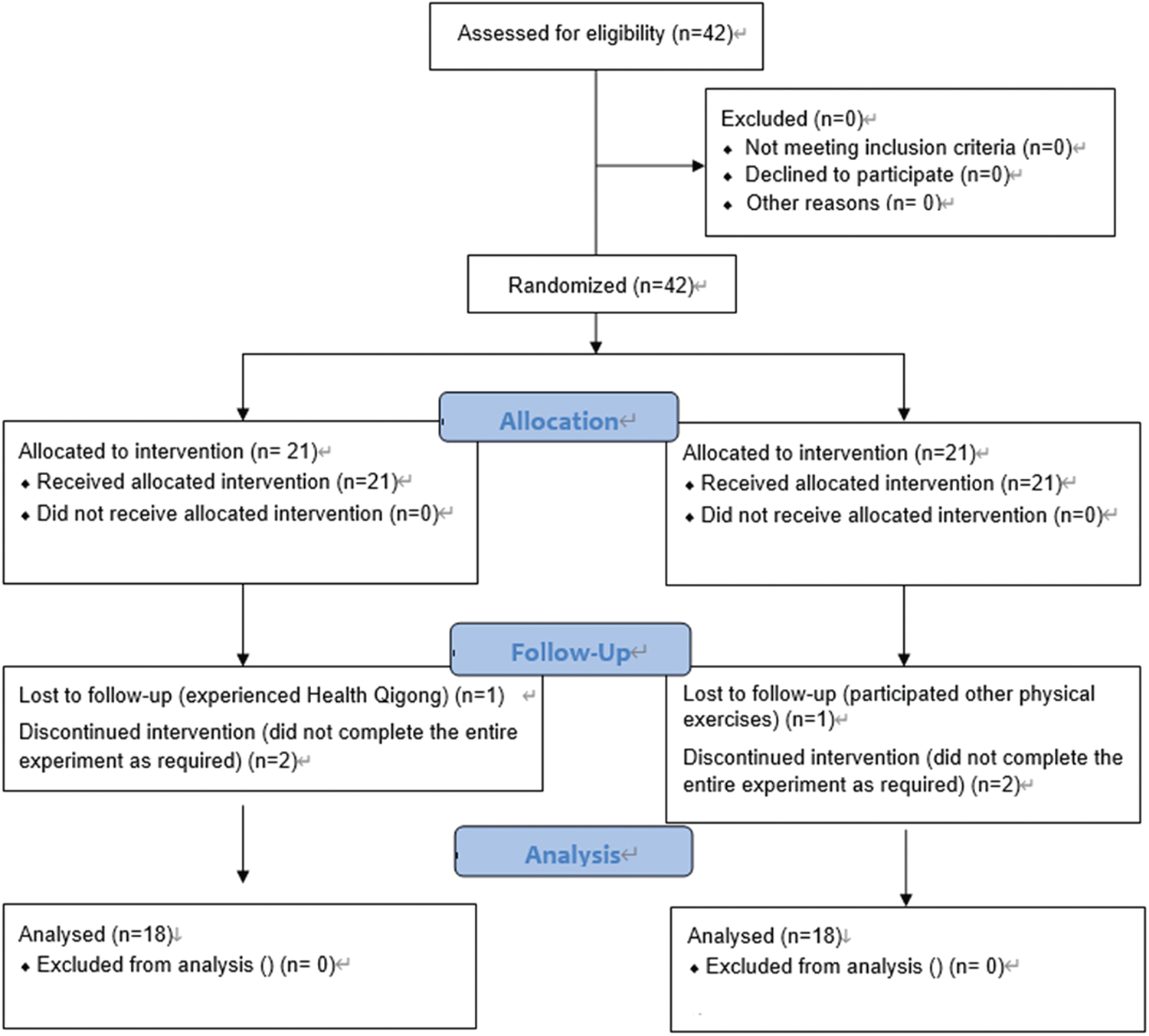
Figure 1: Flow diagram of the progress through the phases of a 2-group parallel randomized trial
2.2 Health Qigong Intervention
Liu and her colleagues [19] have found that the mood of the participants improved while investigating the effects of Health Qigong on lower limb motor function in patients with PD, but it was not discussed at length in their study. So the Health Qigong exercises were borrowed for the present study with their permission. They involved ten movements from the six sets of Health Qigong exercises promoted by the General Administration of Sport of China: Qian Yuan Qi Yun (praying for good fortune at the beginning of heaven’s creation) and Yun Duan Bai He (white crane flying high in the clouds) in Twelve-Movement Daoyin Health Qigong (physical and breathing exercises); Liang Shou Tuo Tian Li San Jiao (holding the hands high with palms up to regulate the internal organs), Wu Lao Qi Shang Wang Hou Qiao (looking backward to prevent sickness and strain), and Cuan Quan Nu Mu Zeng Qi Li (thrusting the fist and glaring the eyes to enhance strength) in Baduanjin Health Qigong (eight silken movements); Long Deng (dragon flying) in Mawangdui Daoyinshu Health Qigong (Dao Yin movements from the drawings of Dao Yin unearthed in Ma Wang Dui Mausoleum); Xu and Xi exercises in Liuzijue Health Qigong (six-character pronunciation); Chu Zhua Liang Chi Shi (showing talons and spreading wings) in Yijinjing Health Qigong (muscle-bone strengthening exercises); and Niao Fei (flying like a bird) in Wuqinxi Health Qigong (five animals playing). During the intervention, participants were required to sign in on site, possible incorrect movements were corrected and participants’ safety were ensured by the instructors, who have received professional guidance and practiced Health Qigong for more than 3 years.
The experimental protocol consisted of pre-, mid-, and post-training measurements. Baseline measurements of anthropometric and demographic indexes were completed within two days. All participants knew the whole procedure. The control group did not receive any regular physical activity and was visited to ensure this was the case throughout the trial. They could receive the Health Qigong intervention after the trial at their own will. The experimental group were instructed Health Qigong exercises once a week for 2 weeks before the trial, 60 min each session. They were required to sign in on site. All instructors had 4 years or more experience in Health Qigong learning, had won prizes at more than one regional Health Qigong competition, and had a National Second-level Referee Certificate of Health Qigong with rich teaching experience. They could correct possible mistakes and ensure safety. The intervention duration was 12 weeks. During the intervention, the participants in the experimental group performed Health Qigong exercises five times a week, 60 min a time. All the participants in both groups took their routine medication according to their doctors’ advice without extra medication for PD.
Measurements were conducted one by one at week 0 (baseline) and at the end of Weeks 6 and 12. Each participant was guided to fill in the forms by a researcher who had been trained by psychology instructors. During the trial, all data of the participants in Beijing and Yantai were recorded twice in crosstab tables and a third time in disorder for final verification. No discrepancies were shown in the three sets of data collection. A Victor Company of Japan (JVC) camera was used for two-dimensional image capture with 50 frames per second. The question-answer process was recorded in the form of photo, and text, and sorted into electronic and paper format (Supplementary 1).
Depression in patients with PD were assessed by the 17-item Hamilton Depression Rating Scale (HDRS-17), which is the most widely used outcome measure in major depressive disorder (MDD) clinical trials. HDRS-17 was originally published in 1960, serving as the standard [20,21]. The sum score on the scale is assessed as follows: 0–7 points for no depression, 8–13 points for mild depression, 14–18 points for moderate depression, and >24 points for severe depression. HDRS-17 involves psychometric properties of depressed mood, feelings of guilty, suicide, agitation, insomnia (sleeping disorder), psychomotor retardation, psychic anxiety, somatic anxiety and so on, which makes it quite suitable for the current study. Each factor has a separate score to further understand the depression status and characteristics of the participants. In this study, cognitive impairment, psychomotor retardation, somatic anxiety, weight loss and sleep disorder were separately measured and analyzed.
Anxiety, as a multidimensional concept [22], has long been separated into the dimensions of state anxiety (the transient anxiety response) and trait anxiety (the stable tendency to become state anxious) [23]. The former describes an unpleasant emotional experience, such as tension, fear, apprehension, and neuroticism, accompanied by a hyperfunction of the autonomic nervous system, generally transient. Trait anxiety is a relatively stable anxiety tendency in personality traits, evaluating an individual’s level of anxiety with individual differences. Traditionally, the State-Trait Anxiety Inventory (STAI) measures state and trait anxiety. It has been extensively used in research, cross-culturally and within different populations, and has sound internal consistency and test–retest reliability [24]. There are 40 questions. The range of possible scores for the STAI varies from a minimum score of 20 to a maximum score of 80 on both the STAI-T and STAI-S subscales. STAI scores are commonly classified as “no or low anxiety” (20–37), “moderate anxiety” (38–44), and “high anxiety” (45–80) [25]. This study applied STAI to explore the effect of Health Qigong on improvement of state and trait anxiety.
SPSS 23.0 (Statistical Product and Service Solutions 23.0) was used to analyze whether there were significant differences in the basic information of the participants (the pretest information) by independent sample T-tests. In the experiment, the data satisfying the Mauchly’s sphericity test, were collected and analyzed by repeated measures analysis of variance (ANOVA) using a group and time mixed-factor design to observe whether the data were significant before the intervention, after 6 and 12 weeks in the control and experimental groups, and whether there was an interaction between the experimental and control groups. We removed the observations that contain missing data.
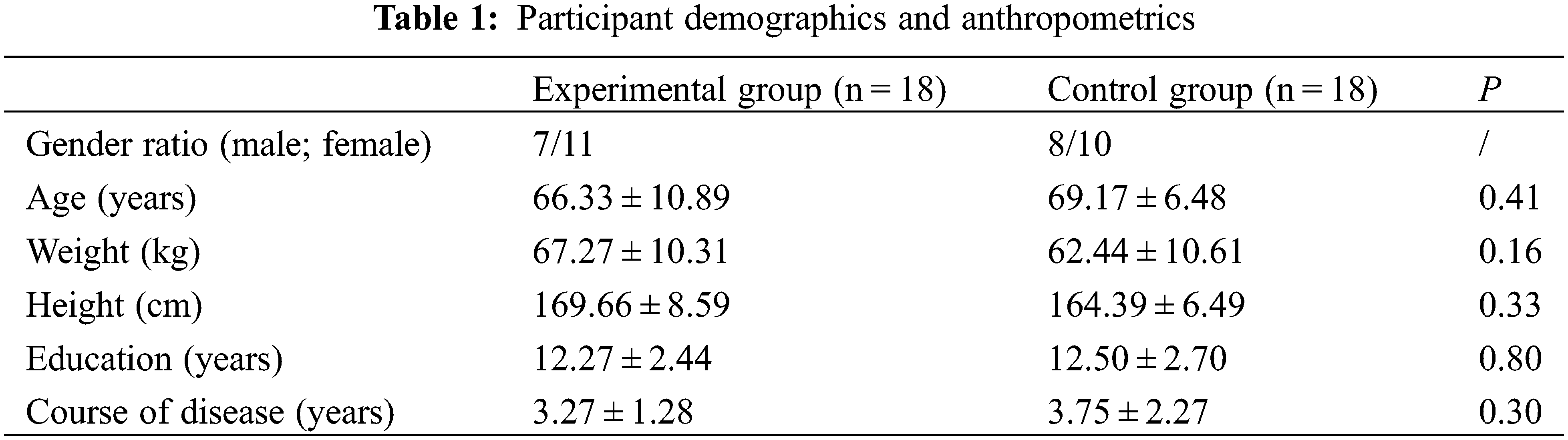
3.1 Demographics and Anthropometrics
They participants were randomly allocated into an experimental group and a control group. In the experimental group, one participant had experienced Health Qigong practice before and two did not complete the entire experiment as required; in the control group, there was incomplete data collection for one participant, one participated in other types of physical exercise, and one did not complete the experiment. There were no demographic differences between the six drop-outs and those who completed the study. The final sample comprised 18 participants in each group. No significant difference was observed in demographics and anthropometrics between the two groups (P > 0.05, Table 1).
3.2 17-Item Hamilton Depression Rating Scale
Repeated measures analysis of variance (ANOVA) was used to analyze the sum score of 17-item Hamilton Depression Rating Scale (HDRS-17), the scores of somatic anxiety, psychomotor retardation, cognitive impairment, weight loss, and sleep disorder. They all met the hypothesis of the Mauchly’s sphericity test and were tested (W = 0.994, P = 0.910; W = 0.940, P = 0.369; W = 0.926, P = 0.283; W = 0.882, P = 0.126; W = 0.872, P = 0.336; W = 0.853, P = 0.445). More details will be presented as follows.
Results showed that there was a significant group by time interaction (P < 0.05), as well as significant group (P < 0.001) and time (P < 0.05) main effects for the sum score of HDRS-17 (Table 2). In the experimental group, a significant difference was noticed at Week 12 (P < 0.001, Table 2). Compared with the control group, the scores of the experimental group significantly decreased at Week 6 and Week 12 (P < 0.01, Table 2).
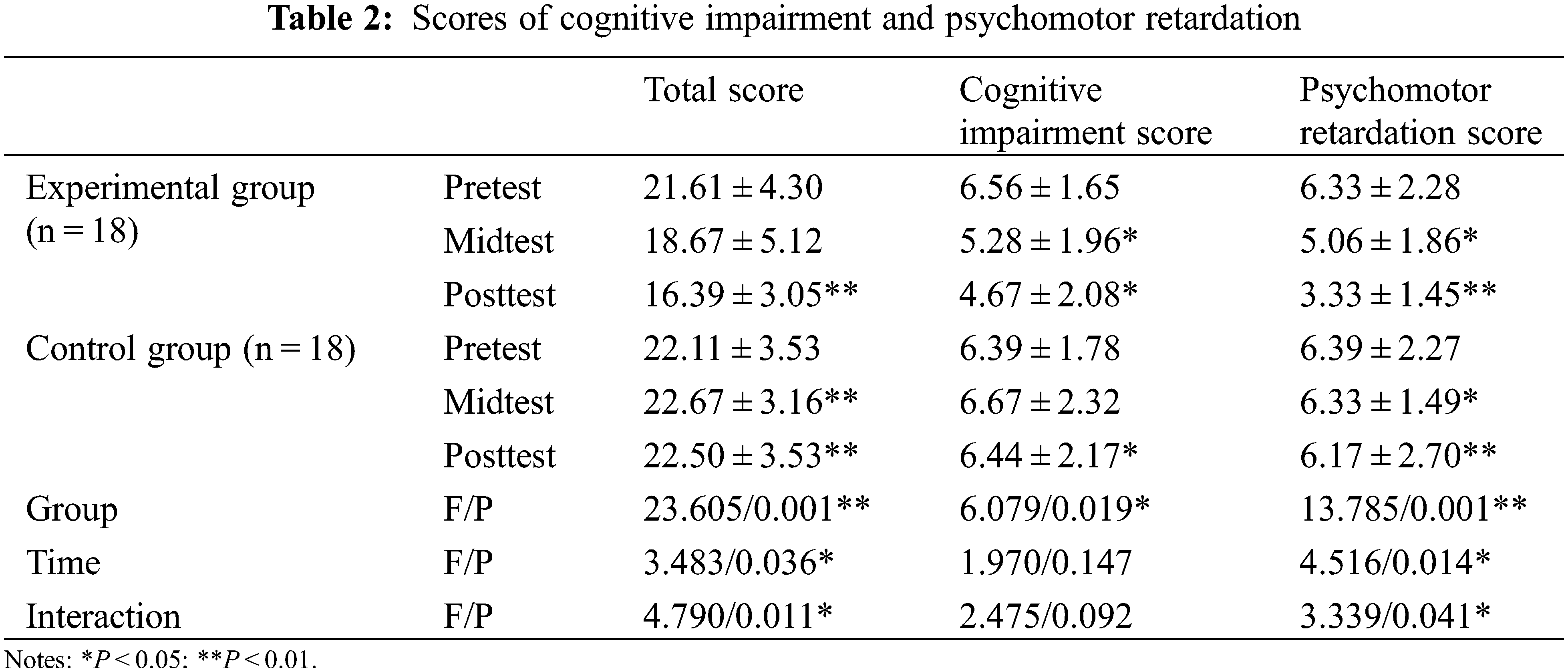
3.2.2 Cognitive Impairment and Psychomotor Retardation
Regarding cognitive impairment, there was a significant group main effect (P < 0.001), no time main effect, and no interaction effect. The score of the experimental group decreased and showed significant differences at Week 6 (P < 0.05, Table 2), which continued to Week 12 (P < 0.05, Table 2). There was a significant difference between the experimental and control groups (P < 0.05, Table 2).
Group (P < 0.01) and time (F = 4.516, P < 0.05) main effects were found in psychomotor retardation. In the experimental group, the score decreased at Week 6 (P < 0.05, Table 2) and significantly at Week 12 (P < 0.01, Table 2). Significant differences were observed between the experimental and control groups at Week 6 (P < 0.05, Table 2) and at Week 12 (P < 0.01, Table 2).
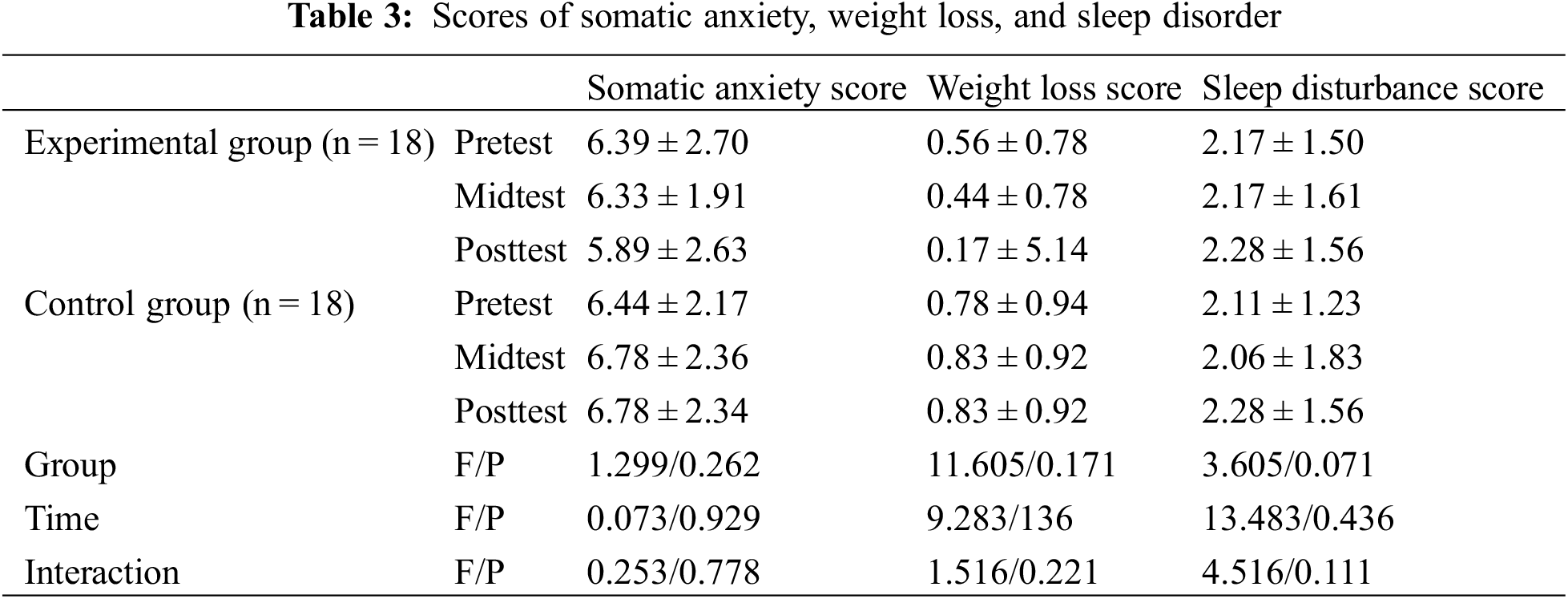
3.2.3 Somatic Anxiety, Weight, Loss and Sleep Disorders
No significant main and interaction effects were found in the scores for somatic anxiety, weight loss, and sleep disorders (Table 3).
3.3 State-Trait Anxiety Inventory (STAI)
The scores of State-Trait Anxiety Inventory (STAI) were analyzed with repeated measures analysis of variance (ANOVA). The Mauchly’s sphericity test was performed to obtain the scores of state anxiety and trait anxiety (W = 0.885, P = 0.075; W = 0.946, P = 0.398), which met its hypotheses. Further data are presented in Table 4.
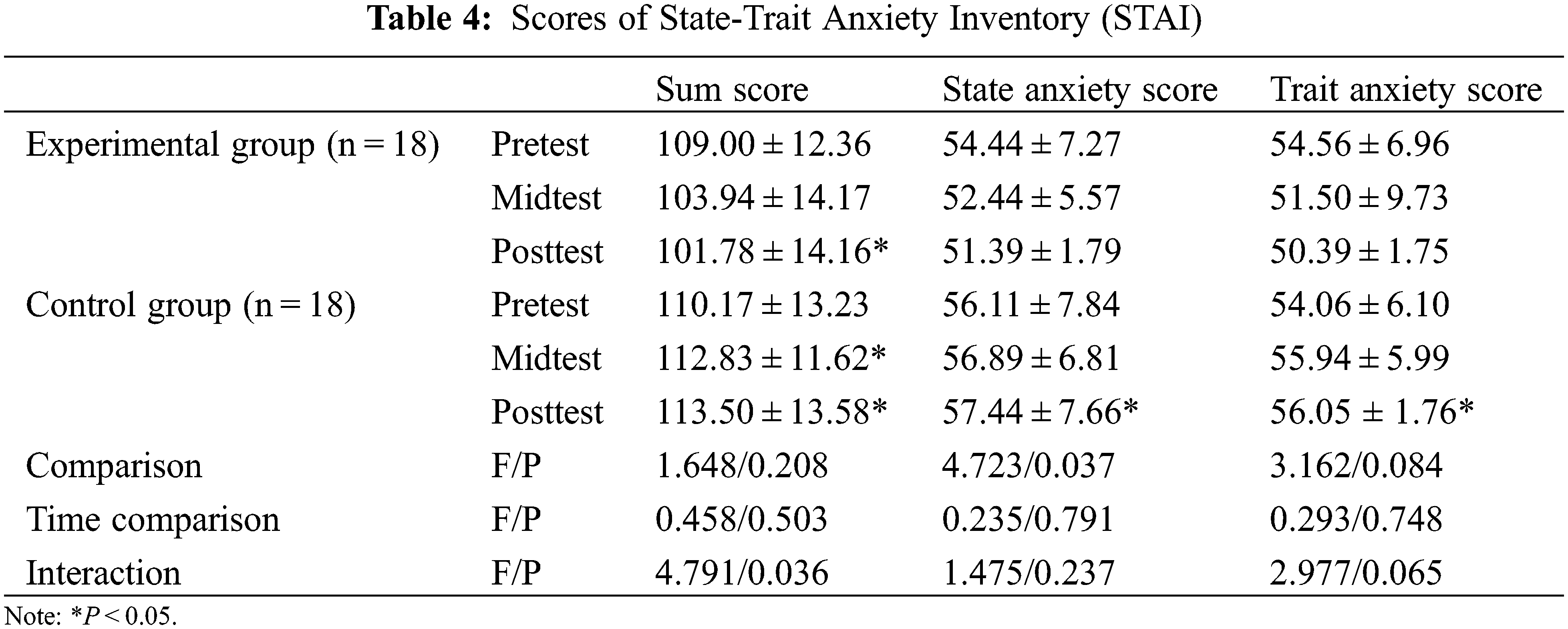
The results showed that there was a significant group by time interaction effect (P < 0.05) with no group or time main effects for the sum score of STAI (Table 2). The scores of state anxiety and trait anxiety in the experimental group decreased and showed a significant difference at Week 12 (P < 0.05). There were significant differences between the experimental and control groups at Week 6 (P < 0.05) and at Week 12 (P < 0.05).
No significant time main and interaction effects were observed. There was a group main effect for state anxiety (P < 0.05). A significant difference was found between the experimental and control groups at Week 12 (P < 0.05).
No significant main and interaction effects were observed for trait anxiety. However, the scores of trait anxiety in the control group increased so that there was a significant difference between the two groups at Week 12 (P < 0.05).
The current study investigated the effects of Health Qigong exercise on depression and anxiety in patients with PD. The results showed significant differences in the somatic anxiety, psychomotor retardation, cognitive impairment, and state and trait anxiety. Health Qigong exercise was effective in decreasing the scores of the 17-item Hamilton Depression Rating Scale (HDRS-17) and the State-Trait Anxiety Inventory (STAI). Further detailed discussion will be presented as follows.
Results indicated that there was no significant difference in the 17-item Hamilton Depression Rating Scale scores between the two groups at enrollment and the scores of both groups were >17. They were allocated into moderate and mild depression groups. The depression of the experimental group significantly was relieved with the increase of intervention time but no significant change in the control group.
Cognitive impairment, as included in the 17-item Hamilton Depression Rating Scale, is composed of three items: self-guilt, suicide, and agitation [26]. In the study, the scores of them decreased significantly at Weeks 6 and 12 in the experimental group. There was a negative time interaction in the cognitive impairment score. The questions on cognitive impairment were related to three items at four levels. The first item is suicide at levels: (1) feels life is not worth living; (2) wishes she/he were dead or any thought of possible death to self; (3) ideas or gestures of suicide; (4) attempts at suicide. The second is feelings of guilt at levels: (1) self-reproach, feels he/she has let people down; (2) ideas of guilt or rumination over past errors or sinful deeds; (3) present illness is a punishment, delusions of guilt; (4) hears accusatory or denunciatory voices and/or experiences threatening visual hallucinations. The third is agitation at levels: (1) fidgetiness; (2) playing with hands, hair, etc.; (3) moving about, cannot sit still; (4) hand wringing, nail biting, hair-pulling, biting of lips.
Thoughts about suicide, guilty feelings and agitation were found in the participants of this present study. Health Qigong exercise (like other types of aerobic exercises) promoted alleviation of negative emotions [27,28]. The patients stretched their arms out in Niao Fei (flying like a bird) in Wuqinxi Health Qigong (five animals playing) while in Qian Yuan Qi Yun (praying for good fortune at the beginning of heaven’s creation) in Twelve-Movement Daoyin Health Qigong (physical and breathing exercises), they stepped aside and cooperated with hand swings. As the patients learned and practiced the Health Qigong exercise, they breathed deeply in Dan Tian and slowly exhaled out, which effectively helped them to deepen their breathing and relax mentally and physically [29]. All these movements made the participants feel comfortable, quiet and eager to communication and demonstration. Consequently, negative emotions such as thought about suicide were alleviated [30–32].
The accompanying music in the practice also relieved the self-reported agitation of the participants [33–35]. In the process, instructors would remind the participants of the names of the movements with lyrical formulas, and so would the accompanying music, which minimized the discomfort caused by blurred memory of the movements. For the participants, Health Qigong exercise is not only a learning process, but also a process of mastering a sport from simplicity to difficulty: from no knowledge to proficiency in sports skills. In this process, the cooperation of movement, breathing, and mind also allows the participants to re-recognize and accept themselves [36,37].
Psychomotor retardation is another item in HDRS-17. Hippocrates and Aretaeus of Cappadocia both described psychomotor retardation as a characteristic of depression [38]. Darwin discussed visible psychomotor symptoms and depressed patients who “no longer wish for action but remain motionless and passive, or may occasionally rock themselves to and fro” [39]. It involved the following questions. Question 1 concerned depressive mood, mainly evaluating the subject’s desire to express themselves; question 7 concerned work and interest, mainly evaluating the subject’s desire to work; question 8 mentioned difficulty in concentration and language, mainly evaluating concentration and retardation; and question 14 concerned the subject’s interest in sexual activity, mainly evaluating sexual desire.
The study suggested that psychomotor retardation was inversely proportional to time. A significant difference was found at Week 6 and Week 12 in the experimental group. At the beginning of the trial, the participants were unsocial and unconfident enough to ask questions. During the trial, the researchers interviewed them and observed that they became increasingly social to communicate with people as time passed and immersed in a comfortable and harmonious atmosphere. While practicing, they spontaneously communicated with one another on Health Qigong culture. Compared with other sports in which the movements were named after body parts along with movement trajectories, Health Qigong movements were named after allusions, Xiangsheng (comic dialogue), and pictographs, which made instruction interesting and storytelling in versed formula. It actively promoted communication between the instructor and participants, making it easier for participants to learn and practice Health Qigong.
Significant improvement in psychomotor retardation was proved as the scores of interest and work decreased after the intervention and so was their dyskinesia. Patients with PD suffer “stiffness” and “tremor,” causing difficulties and loss of interest in daily life. In Long Deng (dragon flying) movement in Mawangdui Daoyinshu Health Qigong and Liang Shou Tuo Tian Li San Jiao (holding the hands high with palms up to regulate the internal organs), the upper and lower limbs cooperated well enough to strengthen the neuromuscular control of the arms and legs. “Stiffness” and “tremor” in the participants were relieved, which boosted the confidence and self-identity in patients. In summary, the results provide evidence that the Health Qigong exercise that the patients with motor dysfunction have learned, practiced and mastered, has effectively improved their self-efficacy, strengthened their self-identity, increased their enthusiasm for work and life, and relieved psychomotor retardation.
4.1.3 Somatic Anxiety, Weight Loss, and Sleep Disorders
There was no significant difference in the scores of somatic anxieties, body weight loss, and sleep disorder in HDRS-17, which might result from insufficient intervention time, as the scores of somatic anxieties at Week 6 and at Week 12 showed a decreasing trend. It indicated that somatic anxiety might gradually be relieved as the intervention prolonged. No significant difference was observed in body weight loss and sleep disorders possibly because the scale in the current study just covered four questions on body weight loss, difficulty in falling asleep, and lots of dreams. These were not sufficient data for detailed analysis of body weight and sleep.
In the current study, the patients in the experimental group learned and performed Health Qigong exercise. Since the sixth week, state and trait anxiety of the experimental group showed a decreasing trend while that of the control group did an increasing trend. In the practice, the patients did not resist Health Qigong exercise as the movements were simple with low intensity. Among the movements, Liang Shou Tuo Tian Li San Jiao (holding the hands high with palms up to regulate the internal organs) in Baduanjin Health Qigong (eight silken movements), Niao Fei (flying like a bird) in Wuqinxi Health Qigong (five animals playing), and Chu Zhua Liang Chi Shi (showing talons and spreading wings) in Yijinjing Health Qigong were performed for body stretching. Xu and Xi exercises in Liuzijue Health Qigong (six-character exercise) and Cuan Quan Nu Mu Zeng Qi Li (thrusting the fist and glaring the eyes to enhance strength) in Baduanjin Health Qigong were performed to regulate the breathing of the participants so that they enjoyed physical and mental relaxation, which alleviated their negative emotions such as depression and anxiety. The scores of the State-Trait Anxiety Inventory (STAI) at the sixth week declined, showing the positive effect of the intervention.
The results demonstrated that long-term Health Qigong exercise relieved trait anxiety of patients with PD. During the Health Qigong exercise, the respiration was regulated to slow, regular, and deep abdominal breathing. With the “introspective self” which guided thinking, the patients effectively reduced mind activities and relaxed themselves. Meditative (mind-body) movements, characterized by musculoskeletal stretching and relaxation, breath control, and a meditative state of mind [40,41], have been shown to be effective for treating depression, anxiety, and sleep problems in people with mental illness [42–44]. Meanwhile, the parasympathetic nervous system was activated to regulate mood by counteracting external stress and stimuli [45]. Compared with the previous studies, the Health Qigong exercises were combined from six sets of Health Qigong, which made them more comprehensive and helpful for relieving anxiety. In the Health Qigong practice, patients were guided to regulate their breathing for eupnea so as to relax themselves and alleviate trait anxiety. In Cuan Quan Nu Mu Zeng Qi Li (thrusting the fist and glaring the eyes to enhance strength) in Baduanjin Health Qigong, the patients performed Wogu (putting the thumb tip on Laogong point and holding the fist), rotated their wrists to stimulate the source points of the channels of Hand San-yin and San-yang, and squatted their legs in a horse stance to stimulate the well points of the channels of Foot San-yin and San-yang to encourage the liver-qi to flow freely and strengthen its capability of retaining blood and promoting blood circulation in the body. Accompanied by this movement, the glaring furiously and relaxing in turn made the patients experience mental strain and relaxation. Liver-qi was guided to flow freely with little stagnation to achieve catharsis and a good mood. The movement regulated San Jiao by pulling Lung Channel and loosening Gallbladder Channel. Additionally, Xi and Xu exercises were practiced to eliminate anxiety and achieve a stable mood by further draining turbid qi in the liver and promoting liver-qi to flow freely in San Jiao.
The environment plays an important role in state anxiety. An unhealthy social and communicative environment is the main factor in the formation of state anxiety in human society. Health Qigong exercise was practiced slowly with low intensity. The patients practiced in a comfortable environment with mnemonics and accompanied music to help them remember the movements. The instructors had rich teaching experience, and the whole process made the participants relaxed and enabled them to enjoy the practice. As the patients were familiar with the environment, state anxiety was further alleviated by immersing themselves in the atmosphere of Health Qigong exercises.
The current study has several strengths. (1) Health Qigong exercise was used for the intervention, and participants did not need to pay high medical costs and endure the side effects of medication in treatment [46]. It provided a new accessible adjutant therapy for anxiety and depression in PD [47]. (2) There was little dependence on the equipment and environment and lower costs for the participants and the study as Health Qigong exercise can performed without fixed places for a long time. After the study, patients with PD were able to independently practice the exercise on their own with good continuity. (3) The project itself involved culture. Practitioners were encouraged to join in the exercise due to its accessibility. (4) Health Qigong regulates breathing so as to effectively alleviate negative emotions. There are also some limitations in this study. First, the experimental time was cut down due to the COVID-19 pandemic, resulting in no significant difference in some indicators, and data relating to the effect of Health Qigong exercise were not easy to be achieved but easy to be lost. Second, two scales were used in this study, but the scales were achieved by the proprioception of the participant, which did not reflect their physiological indicators for in-depth discussion. Third, there were six drop-outs during the trial, which made the sample smaller. And the samples of this experiment were middle-aged and elderly patients with PD in China. They had natural cultural advantages and mastered the movements and the culture easily. If the same instructing method was applied to patients with PD who speak other languages under other cultural backgrounds, the intervention effect may not be as good as that in this study.
This study has provided new evidence of the positive effect of Health Qigong exercise on depression and anxiety in patients with PD, which has not been discussed in previous studies. Health Qigong exercise was supplemented to the existent drug treatment for the patients, and significant alleviated state and trait anxiety, and depression. This traditional Chinese sport is recommended for the treatment of negative mood in patients with PD as an adjutant therapy, which could reduce the treatment cost and improve quality of life. In this study anxiety and depression rating scales were used to quantify the effect of Health Qigong exercise. Subsequent studies could examine biochemical indicators to investigate the possible mechanisms of the intervention for anxiety and depression in patients with PD. The samples could be set with greater diversity so that the effect of Health Qigong exercise on depression and anxiety in patients with PD can be internationally implemented.
Acknowledgement: Thanks to all those who contributed to this study.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorder (5th edition) Washington DC, USA: American Psychiatric Association. [Google Scholar]
2. Sun, N. T., Zhang, W. H. (2021). Research progress on the correlation and intervention with mild cognitive impairment and depression in the elderly. Chinese General Practice Nursing, 19(1), 34–38. DOI 10.12102/j.issn.1009-6493.2020.13.017. [Google Scholar] [CrossRef]
3. Pourakbar, S., Seger, E. W., Neill, B., Jibbe, A., Rajpara, A. (2020). Patient questionnaire to reduce anxiety prior to full-body skin examination. Cutis, 105, 261–262. [Google Scholar]
4. Wang, C. K., Liu, Y. (2000). Correlation between general self-efficacy and trait anxiety, state anxiety and test anxiety. Chinese Journal of Clinical Psychology, 4, 229–230. DOI 10.12102/j.issn.1009-6493.2020.13.017. [Google Scholar] [CrossRef]
5. Landers, M. R., Navalta, J. W., Murtishaw, A. S., Kinney, J. W., Richardson, S. P. (2019). A high-intensity exercise boot camp for persons with Parkinson’s disease: A phase II, pragmatic, randomized clinical trial of feasibility, safety, signal of efficacy, and disease mechanisms. Journal of Neurologic Physical Therapy, 43(1), 17–55. DOI 10.1097/NPT.0000000000000249. [Google Scholar] [CrossRef]
6. Liu, J., Duan, C. L., Yang, H. (2015). Progress in pathogenesis and treatment of Parkinson’s disease. Progress in Physiological Science, 46(3), 163–169. DOI 10.3969/j.issn.1672-6731.2018.01.003. [Google Scholar] [CrossRef]
7. Hughes, A. J., Daniel, S. E., Kilford, L., Lees, A. J. (1992). Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: A clinico-pathological study of 100 cases. Journal of Neurology, Neurosurgery, and Psychiatry, 55(3), 181–184. DOI 10.1136/jnnp.55.3.181. [Google Scholar] [CrossRef]
8. Reijnders, J. S., Ehrt, U., Weber, W. E., Aarsland, D., Leentjens, A. F. (2008). A systematic review of prevalence studies of depression in Parkinson’s disease. Movement Disorders, 23(2), 183–189. DOI 10.1002/mds.21803. [Google Scholar] [CrossRef]
9. Troeung, L., Egan, S. J., Gasson, N. (2013). A meta-analysis of randomized placebo-controlled treatment trials for depression and anxiety in Parkinson’s disease. PLoS One, 8(11), 79510. DOI 10.1371/journal.pone.0079510. [Google Scholar] [CrossRef]
10. Altmann, L. J. P., Stegemller, E. L., Hazamy, A. A. (2016). Aerobic exercise improves mood, cognition, and language function in Parkinson’s disease: Results of a controlled study. Journal of the International Neuropsychological Society, 22(9), 878–889. DOI 10.1017/S135561771600076X. [Google Scholar] [CrossRef]
11. Sagarwala, R., Nasrallah, H. A. (2020). The effects of yoga on depression and motor function in patients with Parkinson’s disease: A review of controlled studies. Annals of Clinical Psychiatry, 32(3), 209–215. [Google Scholar]
12. Liang, H. W., Yang, C. J., Wang, Q. L. (2018). Synergistic effect of physical exercise on depressive disorder. Sichuan Mental Health, 31(3), 246–250. DOI 10.11886/j.issn.1007-3256.2018.03.013. [Google Scholar] [CrossRef]
13. Bao, Q. Y., Wang, Y. J., Xu, Y. J., Sheng, H., Cao, M. J. et al. (2015). Effect of physical exercise on depression induced by estrogen deficiency in mice and its inflammatory mechanism. Journal of the Second Military Medical University, 36(5), 477–482. DOI 10.3724/SP.J.1008.2015.00477. [Google Scholar] [CrossRef]
14. Fan, J., Liu, X. L., Kong, M., Wang, X. Y., Yi, L. Y. et al. (2017). Effect of health qigong on mood state and cognition disorder in patients with moderate Parkinson’s disease. Chinese Journal of Sports Medicine, 36(2), 143–146+149. DOI 10.3969/j.issn.1000-6710.2017.02.008. [Google Scholar] [CrossRef]
15. Zhang, L. W., Cheng, M. X., Liu, H., Kong, Z. W., Li, L. et al. (2019). Effect of health qigong exercise on gait and depression in patients with Parkinson’s disease. 11th National Convention on Sport Science of China, pp. 1674–1676. Beijing, China. DOI 10.26914/c.cnkihy.2019.029470. [Google Scholar] [CrossRef]
16. Liu, X. L., Chen, S., Wang, Y. (2016). Effects of health qigong exercises on relieving symptoms of Parkinson’s disease. Evidence-Based Complementary and Alternative Medicine, 45, 25–33. DOI 10.1155/2016/5935782. [Google Scholar] [CrossRef]
17. Xiao, C. M., Zhuang, Y. C. (2007). Effect of health baduanjin qigong for mild to moderate Parkinson’s disease. Geriatrics & Gerontology International, 16(8), 911–919. DOI 10.1111/ggi.12571. [Google Scholar] [CrossRef]
18. Hoehn, M. M., Yahr, M. D. (2001). Parkinsonism: Onset, progression and mortality. Neurology, 17(5), S11–S26. DOI 10.1212/wnl.17.5.427. [Google Scholar] [CrossRef]
19. Liu, X. L., Chen, S., Wang, Y. (2016). Effect of health qigong exercises on relieving symptoms of Parkinson’s disease. Evidence-Based Complementary and Alternative Medicine, 2016. DOI 10.1155/2016/5935782. [Google Scholar] [CrossRef]
20. Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 85(2), 119–120. DOI 10.1136/jnnp.23.1.56. [Google Scholar] [CrossRef]
21. Hamilton, M. (1967). Development of a rating scale for primary depressive illness. British Journal of Clinical Psychology, 6(4), 278–296. DOI 10.1111/j.2044-8260.1967.tb00530.x. [Google Scholar] [CrossRef]
22. Spielberger, C. D. (1985). Anxiety, cognition and affect: A state-trait perspective. In: Tuma, A. H., Maser, J. D., Anxiety and the anxiety disorders (2nd editionpp. 171–182. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
23. Spielberger, C. D., Sydeman, S. J. (1994). State-trait anxiety inventory and state-trait anger expression inventory. In: Maruish, M. E., The use of psychological testing for treatment planning and outcome assessment (1st editionpp. 292–321. Hillsdale, NJ: Lawrence Erblaum Associates, Inc. [Google Scholar]
24. Barnes, L. B., Harp, D., Jung, W. S. (2002). Reliability generalization of scores on the spielberger state-trait anxiety inventory. Educational and Psychological Measurement, 62, 603–618. DOI 10.1177/0013164402062004005. [Google Scholar] [CrossRef]
25. Skapinakis, P. (2014). Spielberger state-trait anxiety inventory. In: Michalos, A. C. (Ed.Encyclopedia of quality of life and well-being research. Springer: Dordrecht. DOI 10.1007/978-94-007-0753-5_2825. [Google Scholar] [CrossRef]
26. Chen, C. H., Chen, Z. Q., Hu, S. Y., Zhang, H. G., Cao, M. Q. et al. (2003). A survey on the factor scores of hamilton depression scale among cases with various patterns of depression. Journal of TCM University of Hunan, 23(4), 32–34. DOI 000-5633(2003)04-0032-03. [Google Scholar]
27. Rodriguez-Ayllon, M., Acosta-Manzano, P., Coll-Risco, I., Romero-Gallardo, L., Borges-Cosic, M. et al. (2021). Associations of physical activity, sedentary time, and physical fitness with mental health during pregnancy: The GESTAFIT project. Journal of Sport and Health Science, 10, 379–386. DOI 10.1016/j.jshs.2019.04.003. [Google Scholar] [CrossRef]
28. De la Rosa, A., Olaso-Gonzalez, G., Arc-Chagnaud, C., Millan, F., Salvador-Pascual, A. et al. (2020). Physical exercise in the prevention and treatment of Alzheimer's disease. Journal of Sport and Health Science, 9(5), 394–404. DOI 10.1016/j.jshs.2020.01.004. [Google Scholar] [CrossRef]
29. Fang, J., Zhang, L., Wu, F., Ye, J., Cai, S. et al. (2021). The safety of baduanjin exercise: A systematic review. Evidence-Based Complementary and Alternative Medicine, 2021, 8867098. DOI 10.1155/2021/8867098. [Google Scholar] [CrossRef]
30. Chi, X., Liang, K., Chen, S. T., Huang, Q., Huang, L. et al. (2021). Mental health problems among Chinese adolescents during the COVID-19: The importance of nutrition and physical activity. International Journal of Clinical and Health Psychology, 21, 100218. DOI 10.1016/j.ijchp.2020.100218. [Google Scholar] [CrossRef]
31. Chen, S. T., Guo, T., Yu, Q., Stubbs, B., Clark, C. et al. (2021). Active school travel is associated with fewer suicide attempts among adolescents from low-and middle-income countries. International Journal of Clinical and Health Psychology, 21, 100202. DOI 10.1016/j.ijchp.2020.11.001. [Google Scholar] [CrossRef]
32. Powers, S. K., Deminice, R., Ozdemir, M., Yoshihara, T., Bomkamp, M. P. (2020). Exercise-induced oxidative stress: Friend or foe? Journal of Sport and Health Science, 9, 415–425. DOI 10.1016/j.jshs.2020.04.001. [Google Scholar] [CrossRef]
33. Terry, P. C., Karageorghis, C. I., Curran, M. L., Martin, O. V., Parsons-Smith, R. L. (2020). Effects of music in exercise and sport: A meta-analytic review. Psychological Bulletin, 146, 91–117. DOI 10.1037/bul0000216. [Google Scholar] [CrossRef]
34. Jones, L., Ekkekakis, P. (2019). Affect and prefrontal hemodynamics during exercise under immersive audiovisual stimulation: Improving the experience of exercise for overweight adults. Journal of Sport and Health Science, 8, 325–338. DOI 10.1016/j.jshs.2019.03.003. [Google Scholar] [CrossRef]
35. Stork, M. J., Kwan, M. Y., Gibala, M. J., Martin Ginis, K. A. (2015). Music enhances performance and perceived enjoyment of sprint interval exercise. Medicine and Science in Sports and Exercise, 47, 1052–1060. DOI 10.1249/MSS.0000000000000494. [Google Scholar] [CrossRef]
36. Kim, S. H., Schneider, S. M., Kravitz, L., Mermier, C., Burge, M. R. (2013). Mind-body practices for posttraumatic stress disorder. Journal of Investigative Medicine, 61, 827–834. DOI 10.2310/JIM.0b013e3182906862. [Google Scholar] [CrossRef]
37. Li, J., Shen, J., Wu, G., Tan, Y., Sun, Y. (2018). Mindful exercise versus non-mindful exercise for schizophrenia: A systematic review and meta-analysis of randomized controlled trials. Complementary Therapies in Clinical Practice, 32, 17–24. DOI 10.1016/j.ctcp.2018.04.003. [Google Scholar] [CrossRef]
38. Sobin, C., Mayer, L., Endicott, J. (1998). The motor agitation and retardation scale: A scale for the assessment of motor abnormalities in depressed patients. The Journal of Neuropsychiatry and Clinical Neurosciences, 10, 85–92. DOI 10.1176/jnp.10.1.85. [Google Scholar] [CrossRef]
39. Greden, J. F., Carroll, B. J. (1981). Psychomotor function in affective disorders: An overview of new monitoring techniques. American Journal of Psychiatry, 138(11), 1441–1448. DOI 10.1176/ajp.138.11.1441. [Google Scholar] [CrossRef]
40. Zou, L., Yeung, A., Quan, X. (2018). Mindfulness-based baduanjin exercise for depression and anxiety in people with physical or mental illnesses: A systematic review and meta-analysis of randomized controlled trials. International Journal of Environmental Research and Public Health, 15(2), 321. DOI 10.3390/ijerph15020321. [Google Scholar] [CrossRef]
41. Bystritsky, A., Kronemyer, D. (2014). Stress and anxiety: Counterpart elements of the stress/anxiety complex. Psychiatric Clinics of North America, 37(4), 489–518. DOI 10.1016/j.psc.2014.08.002. [Google Scholar] [CrossRef]
42. Zou, L., Wang, H., Li, T., (2017). Effect of health-qigong on spinal mobility and disease activity in people with ankylosing spondylitis. Le Travail Humain, 80, 1585–1597. [Google Scholar]
43. Zou, L., Yeung, A., Quan, X. (2018). A systematic review and meta-analysis of mindfulness-based (Baduanjin) exercise for alleviating musculoskeletal pain and improving sleep quality in people with chronic diseases. International Journal of Environmental Research and Public Health, 15(2), 206. DOI 10.3390/ijerph15020206. [Google Scholar] [CrossRef]
44. Zou, L., Wang, C., Yeung, A. (2018). A review study on the beneficial effects of Baduanjin. Journal of Alternative and Complementary Medicine, 24(4), 324–335. DOI 10.1089/acm.2017.0241. [Google Scholar] [CrossRef]
45. Strohmaier, S., Jones, F. W., Cane, J. E. (2021). Effects of length of mindfulness practice on mindfulness, depression, anxiety, and stress: A randomized controlled experiment. Mindfulness, 12, 198–214. DOI 10.1007/s12671-020-01512-5. [Google Scholar] [CrossRef]
46. Yan, X., Shen, H., Loh, C., Shao, J., Yang, Y. et al. (2013). A longitudinal study about the effect of practicing yan Xin qigong on medical care cost with medical claims data. International Journal of Economic Research, 10(2), 391–403. [Google Scholar]
47. Song, R., Grabowska, W., Park, M., Osypiuk, K., Vergara-Diaz, G. P. (2017). The impact of Tai Chi and qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism & Related Disorders, 41, 3–13. DOI 10.1016/j.parkreldis.2017.05.019. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools