 Open Access
Open Access
ARTICLE
Properties of a Scale of Self-Care Behaviors Facing COVID-19: An Exploratory Analysis in a Sample of University Students in Huanuco, Peru
1
Universidad de Huánuco, Facultad de Ciencias de la Salud, Huánuco, Peru
2
EsSalud, Hospital Bicentenario de Jauja, Huancayo, Peru
3
Universidad de Lima, Facultad de Ciencias Empresariales y Economicas, Carrera de Negocios Internacionales, Lima, Peru
4
Universidad Norbert Wiener, Vicerrectorado de Investigación, Lima, Peru
5
Teoma Global, Gerencia Corporativa de Asuntos Científicos y Regulatorios, Lima, Peru
* Corresponding Author: Jaime A. Yáñez. Email:
International Journal of Mental Health Promotion 2022, 24(6), 959-974. https://doi.org/10.32604/ijmhp.2022.021172
Received 30 December 2021; Accepted 29 April 2022; Issue published 28 September 2022
Abstract
The general objective of this article was to construct and describe the psychometric properties of a scale of selfcare behaviors against COVID-19. It was a descriptive, cross-sectional, psychometric validation study of a scale created to measure self-care behaviors in relation to COVID-19 in a total sample of 333 probabilistically selected. Qualitative validity was evaluated by a review of 10 experts and quantitative validity by means of exploratory factor analysis using the principal components method. Internal consistency was measured with Cronbach’s alpha twice and the test-retest was evaluated by calculating the intraclass coefficient. The final scale consisted of 29 items. The Kaiser-Meyer-Olkin test of adequacy yielded a value of 0.926, and the Bartlett’s test of sphericity X² = 4611 with a p-value < 0.001. The variance explained by the three retained factors with a total of 29 items was 50.03%. The Cronbach’s alpha internal consistency evaluation yielded an initial value of 0.923 and, in a second evaluation, showed a value of 0.936. In addition, the intraclass coefficient in the test-retest yielded a value of 0.929. The instrument created and validated possessed the necessary conditions as a useful and reliable tool for measuring self-care behaviors in relation to COVID-19 in a population of university students and it is important that it can be applied in other regions of the world.Keywords
Due to the COVID-19 pandemic, governments implemented measures such as social distancing [1–3] or quarantines [4–7] to avoid contagion by COVID-19. However, the COVID-19 pandemic evidenced the weaknesses of the Peruvian healthcare system and public health policies [8–10]. Specifically, it can be recognized the lack of organizational support for workers in healthcare facilities [11] generating a growth of intention workers to leave their jobs due to mental distress [12–14]. Population, including young people as university students, is massively exposed to fake news [15] and conspiracy theories [16], which generated many doubts between citizens and increase mental distress [17] generating the search for preventive and curative measures with unproven drugs [9,18] and the self-use of medicinal plants [9,19], which affected the intention to get vaccinated against COVID-19 [20]. Another significant impact is in terms of jobs of people such as small firms [21,22], sports events [23], hospitality industry [24,25], education activities in universities [26–28], healthcare services [29], circular economy projects [30], developing of entrepreneurship [31], technology resources [32], which simultaneously generated price variation in products [33].
Many healthcare systems were weakened to cope with the disease, with little response capacity, which has led to changes in self-care behaviors in the face of COVID-19 [34]. These self-care behaviors comprise a set of daily practices by a person, family, or groups of people to take care of their health. As explained by Galdames-Cruz, et al. [35], self-care can vary according to the individual’s experience with a health problem, both personally and with close figures. Lifestyle medicine surges as a multi-disciplinary approach to prevent and/or cure non-communicable diseases such as type 2 diabetes, cancer and cardiovascular disease [36]. Furthermore, it was recommended that the lifestyle medicine multidisciplinary team should focus on the satisfaction of self-care needs of the patient [36]. The World Health Organization (WHO) recommended the adoption of self-care behaviors in the face of COVID-19 by promoting self-care at the physical, mental and social levels [37]. The Peruvian Ministry of Health also established technical criteria and procedures for the care and self-care of the population’s physical and mental health in the context of COVID-19 [38]. Peru implemented extraordinary measures aimed at mitigating the spread of COVID-19 infections; as a result, changes in the way the Peruvian population protect themselves was reported [39,40].
In this context, homes have become places of work, study, recreation, and leisure; it is there were university students went from being in person to virtuality, so they have seen the need to change their health self-care behaviors in the face of COVID-19, adapting to new lifestyles [41,42]. Today’s university students shape the society of the future and make up a considerable part of the country’s economic assets. On the other hand, during the transition to university life, subjects forge certain independence by choosing their eating behaviors in part based on their knowledge and appreciation of foods containing bioactive compounds [43–53], and adopting habits such as smoking, alcohol consumption, psychoactive substances, physical activity, and sex which, in turn, have implications for their physical and psychological health [54–59]. The measurement of self-care behaviors about COVID-19 is essential to implement educational strategies for health intervention at the community level. Therefore, it is essential to identify self-care behaviors in its three main dimensions: self-care of physical, social, and mental health [60], which includes balanced nutrition, hygiene measures, stress management, social relationship, and interpersonal problem-solving skills, physical activity, and exercise, ability to avoid self-medication, consumption of prescription drugs, safe behaviors, recreation and free time management, communication, positive adaptations to life changes and care of morbid processes, among others [37]. Thus, the objective of this study was to develop and validate an instrument to measure validly and reliably the healthy self-care behaviors against COVID-19 in a university context to generate research that helps improve preventive-promotional interventions in the context of COVID-19. Consequently, we constructed and described the psychometric properties of a scale of self-care behaviors against COVID-19 in a sample of university students of Huanuco, Peru.
2.1 Design and Study Population
A descriptive, cross-sectional, psychometric study of validation of a scale to measure self-care behaviors against COVID-19 was conducted in a population of 2000 students of the University of Huanuco in Huanuco, Peru. The study was conducted during July and December 2020. The calculated sample was 333 students, with an expected proportion of 50%, reliability of 95%, and an error of 4.90%. Simple random probability sampling was used, considering a minimum of 5 participants according to the number of items in the instrument (65 items at the beginning of the study). The inclusion criteria were young university students currently enrolled in University of Huanuco. Those who did not wish to participate in the study were excluded.
2.2 Variables and Measurements
The primary variable of the study was oriented to self-care behaviors vis-à-vis COVID-19. We developed the questionnaire, grouping it into 3 dimensions: physical, mental, and social self-care behaviors.
2.3 The Preliminary and Exploratory Phase
At the quantitative level, first, a review of the literature focused on self-care behaviors against COVID-19 was carried out in search of a scale to measure self-care during the COVID-19 pandemic. A recent study performed in Slovakia has validated the correlation between the Patient Health Questionnaire (PHQ-9) for depression and Self-Care Activities Screening Scale (SASS-14) assessing health consciousness, nutrition, physical activity, sleep quality, and interpersonal and intrapersonal coping strategies [61]. The Self-Care Activities Screening Scale (SASS-14) was validated demonstrating good reliability, predictive and convergent validity in coping with COVID-19 lockdown and perceived stress [62]. Because of the social isolation and the increase in telemedicine, various mobile health applications have been used worldwide during the COVID-19 pandemic, which consisted in increasing patient’s awareness, self-care, and self-monitor behaviors [63]. A study performed in Iran identified that 15 data elements for self-care are important to be used during mobile-based applications [63]. Some of these self-care data elements include medication reminders, monitor adherence, training about sign and symptoms of COVID-19, recording of daily fever [63]. A study in Chile implemented an eight-week multifaceted mindfulness-based self-care program on medical students’ distress and well-being during the COVID-19 pandemic [64]. A reduction in burnout prevalence, stress, self-blaming and traumatic stress were observed, accompanied with a higher mindfulness, resilience, and active coping strategies [64]. It is important to note that no scale was found in Peru, and this corresponds the first study of this kind in Peru. The questions of the questionnaire were adapted initially from various regulations of the Ministry of Health of Peru, documents of the World Health Organization (WHO), among other official and academic publications. Thus, the instrument was designed with a multiple-choice Likert-type scale.
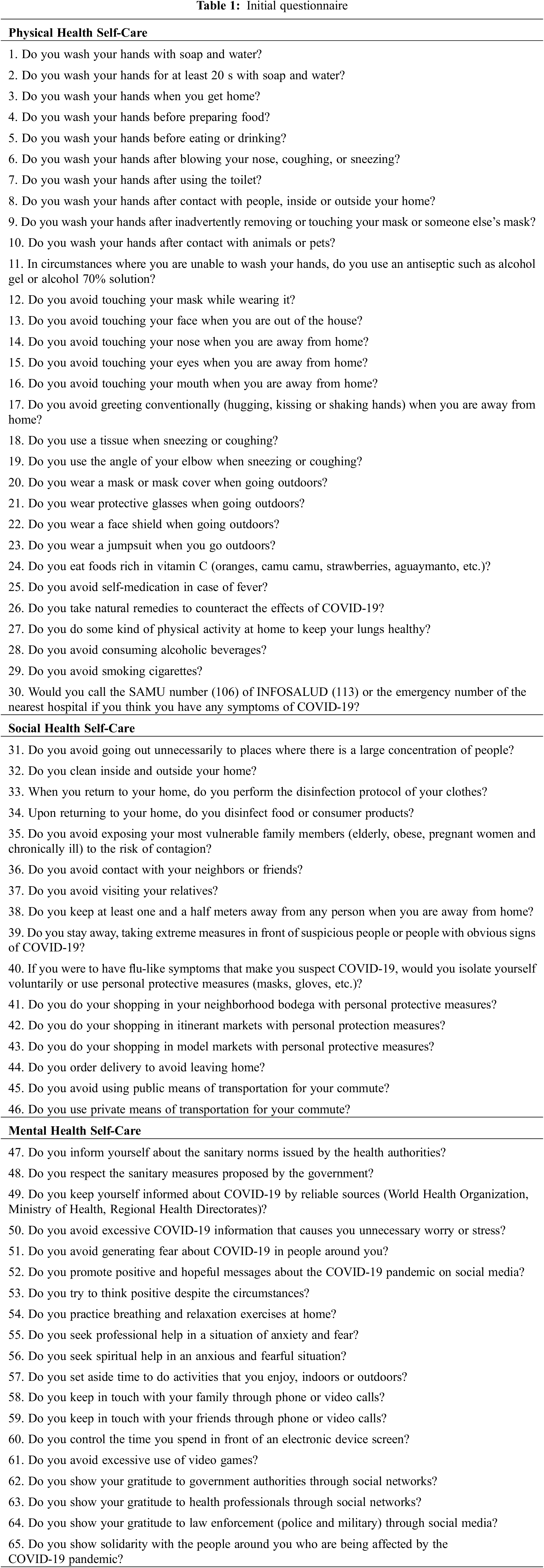
The first version of the questionnaire consisted of 65 items, with 5 options: “never”, “rarely”, “regularly”, “almost always” and “always”; 10 experts and judges then reviewed the questionnaire before undergoing a face validity and quantitative validation analysis. The questionnaire was constructed based on the most relevant questions after reviewing questionnaires or scales in international databases (Pubmed, ScienceDirect, Scielo, and Google Scholar) and other normative documents. Content validity was carried out through the judgment of 10 experts in the form of individual aggregates; this allowed us to have information from each expert. The experts included national and foreign professionals with years of experience in psychometrics and in the clinical and community fields, attending patients with COVID-19 (physicians, nurses, and psychologists).
The information was collected on two occasions through a virtual survey, with a month between the measurements, to avoid response bias [65]. The first application was carried out in November (the last two weeks) and the second in December 2020 (in the last week). In the first measurement of the variable, 333 students participated. In the second measurement, 62.76% (209) of the total were surveyed to have information for the test-retest. Table 1 shows the original questionnaire to be validated.
The necessary adjustments were made for the final version of the scale to measure self-care behaviors about COVID-19. Next, psychometric evaluation and multivariate analysis were carried out to demonstrate the construct validity of the designed instrument to determine the final number of questions to be included.
Construct validity through exploratory factor analysis technique (EFA) of principal components was performed. A correlation matrix was elaborated to observe whether most item-total correlations exceeded the value of 0.3 to verify the preconditions before proceeding with construct validity. In addition, the Kaiser-Meyer-Olkin (KMO) measure of adequacy was determined, and Barlett’s test of sphericity was applied to verify the significant correlations between the items. The correlation matrix was also evaluated, extracting the possible factors, the type of rotation applied was Varimax because the correlations calculated were below 0.20 in many of the items, and the total accumulated variance was evaluated, exceeding 50%.
For the evaluation of internal consistency, Cronbach’s alpha (α) was used at two moments of scale application, which is because it is the most widely used coefficient for measurement scales in the field of healthcare [66] and a higher value of 0.8 was considered a good indicator of internal consistency [67]. In the case of test-retest reliability measurement, the intraclass coefficient was used to check if very similar scores were obtained two times after applying the instrument. All the data collected were transferred to an Excel spreadsheet and then to the SPSS-IBM v.25.0 statistical package.
The present study underwent an evaluation and approval of the research ethics committee of the University of Huanuco. In addition, the recommendations of the Declaration of Helsinki and the principles that guide the ethical practice of online studies were followed. For greater transparency, the primary study protocol was registered in the PRISA repository of the Peruvian National Institute of Health (code: EI0000000875). All included study subjects provided informed consent before answering the online survey, describing the confidentiality and anonymity of the respondent’s data, the objective and procedure of the study, as well as the option to participate in the study, to withdraw at any time, and to communicate with the research team to clarify any doubts.
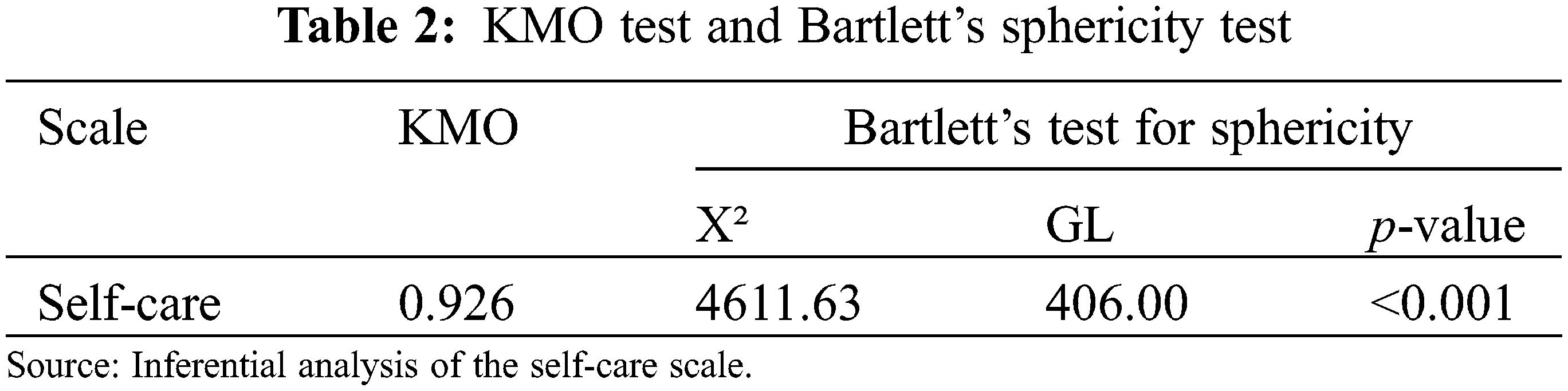
The sample adequacy measure “KMO” proposed by Kaiser, Meyer, and Olkin was evaluated to test whether the items effectively fit the factor analysis model, and the result obtained was 0.926, which indicated that there were grouped items to form factors. Bartlett’s test of sphericity was applied to check whether there was a correlation between the items, and the results obtained indicated that the factor analysis was feasible (Table 2).
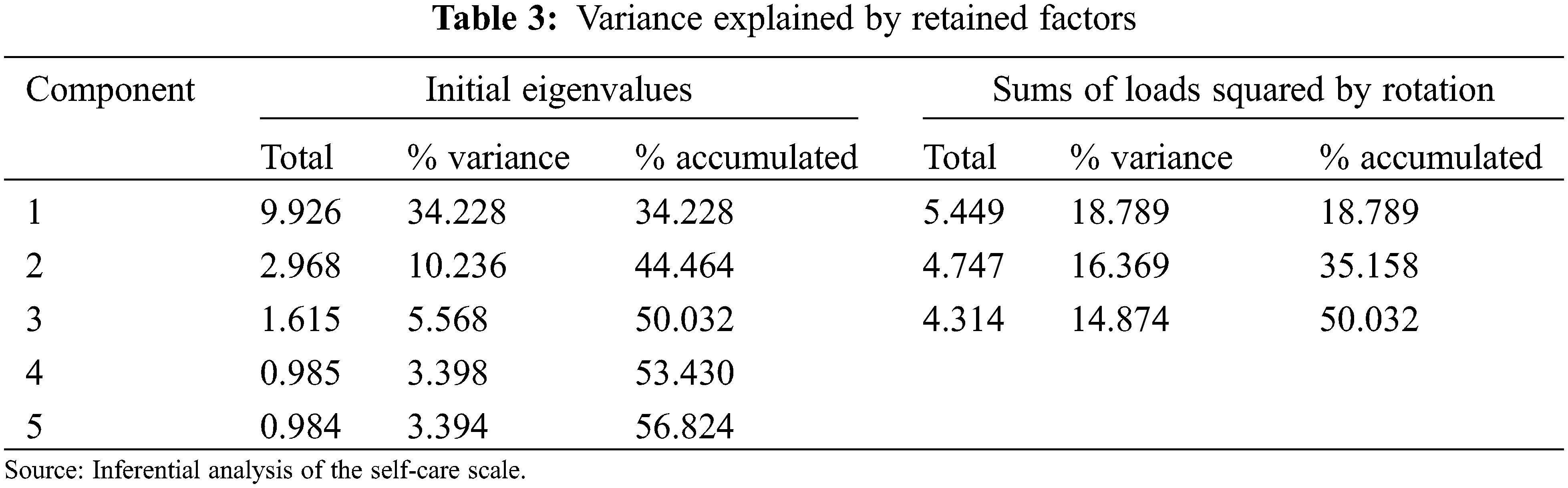
In the case of determining the factors to be retained, 3 factors were considered; these contained eigenvalues above unity with an explained variance of 18.8% for the first factor, 16.4% for the second factor, and 14.9% for the third factor, totaling 50.0% (Table 3).
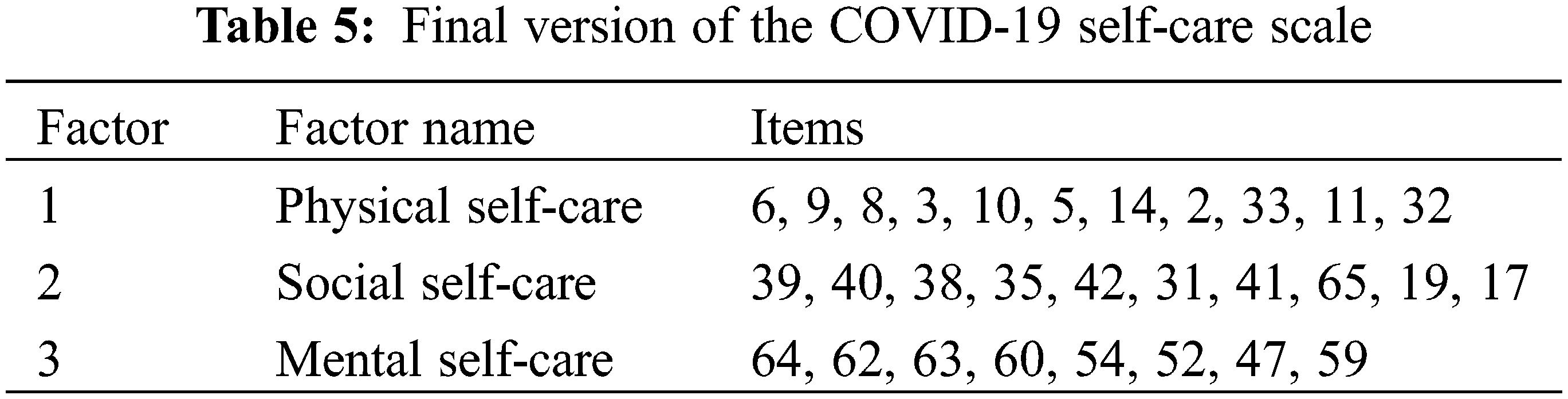
For the assignment of each item to each factor, correlation indexes higher than 0.3 were considered after varimax rotation (Table 4). The retained factors were grouped as physical health self-care with a total of 11 items (6, 9, 8, 3, 10, 5, 14, 2, 33, 11, 32); social health self-care which grouped 10 items (39, 40, 38, 35, 35, 42, 31, 41, 65, 19, 17) and mental health self-care which retained 8 items (64, 62, 63, 60, 60, 54, 52, 47, 59) (Table 5).
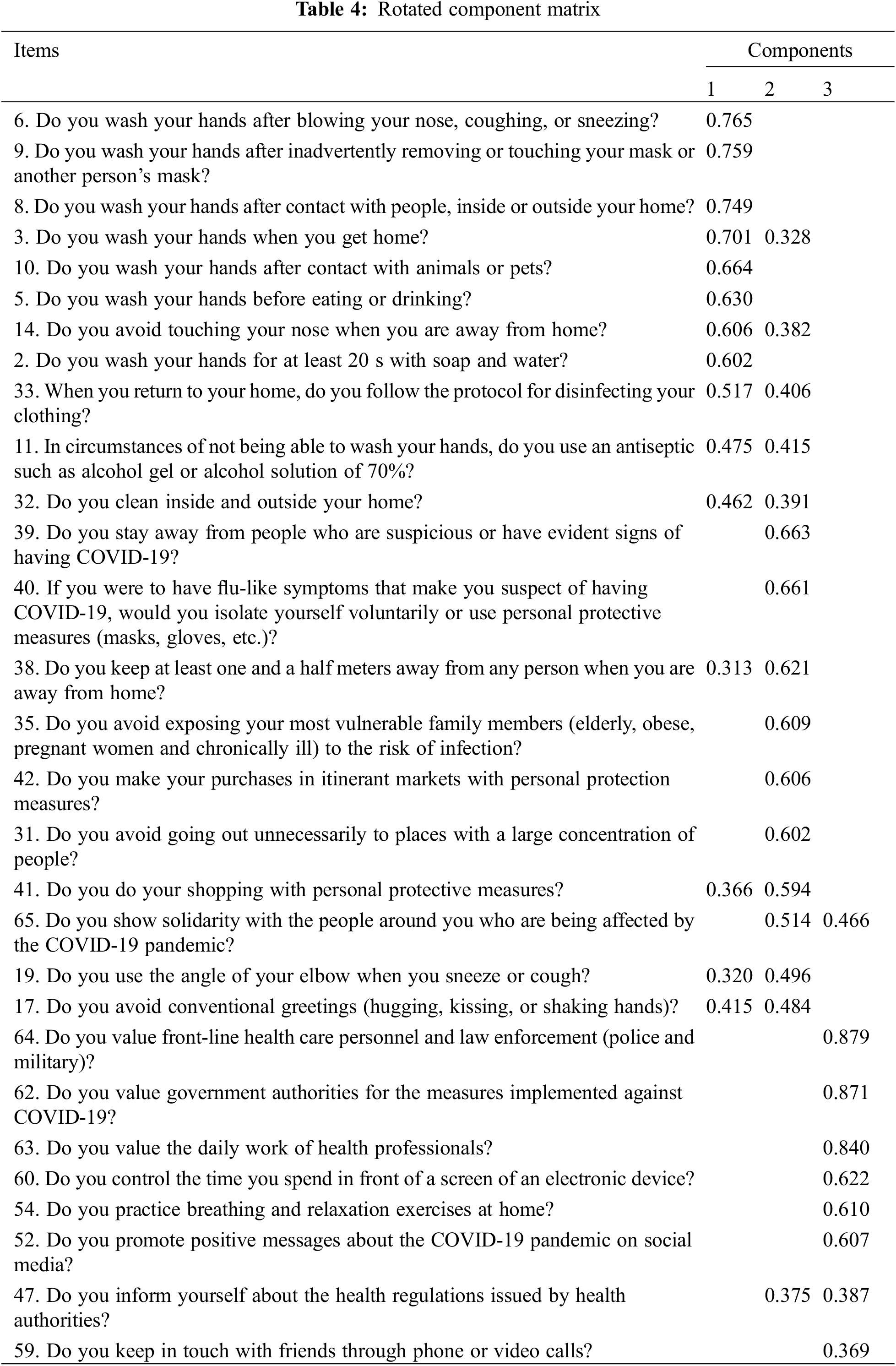
The rest of the items not considered in the three factors and were eliminated because they had no relationship with the fourth or fifth factor during the factor analysis evaluation.
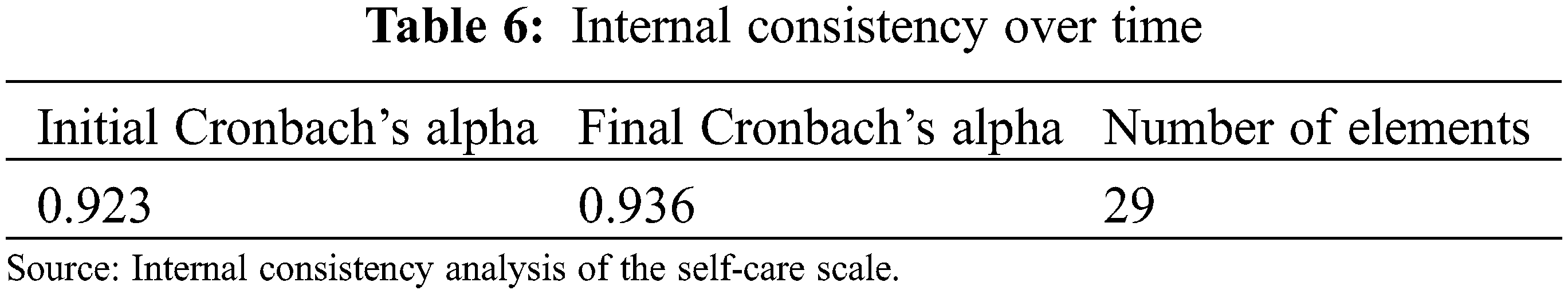
Internal consistency was measured twice, obtaining 0.923 in the first and 0.936 in the second. We consider from these results that the items were reciprocally related (Table 6).
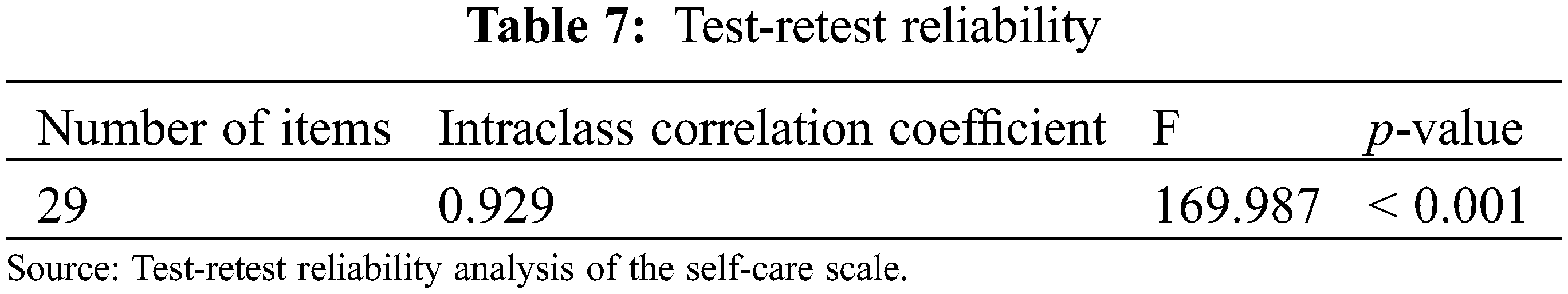
For the test-retest evaluation, the virtual survey was applied for the second time to 209 (62%) students. We found the intraclass correlation coefficient, obtaining a coefficient α = 0.929 (Table 7).
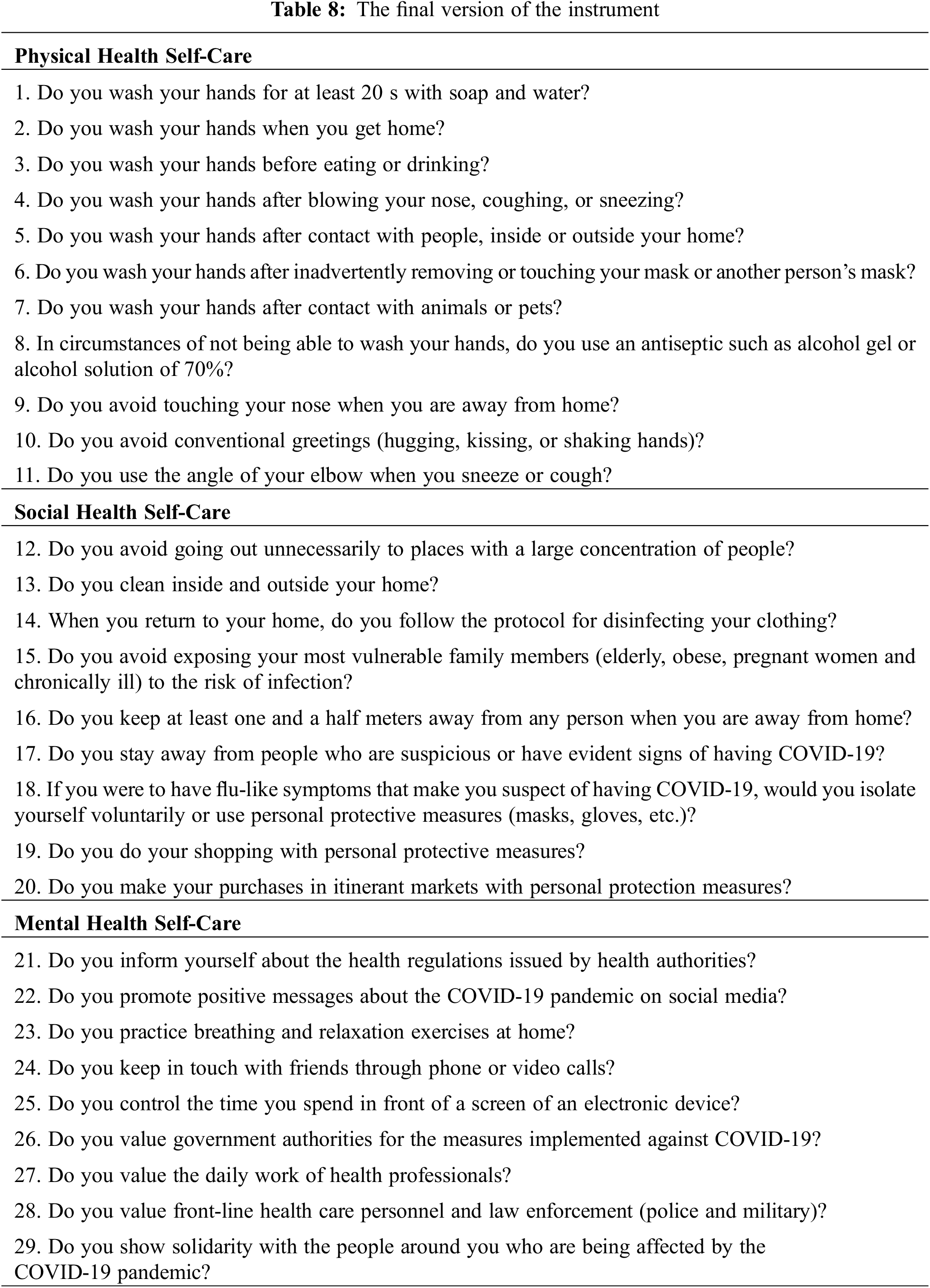
The final version of the instrument is shown in Table 8.
The scale for measuring self-care behaviors against COVID-19 in our study was found to be valid and reliable. In the context of the COVID-19 pandemic, young populations are a high-risk group in Latin American countries since mortality associated with COVID-19 is higher in young and middle-aged people compared to Western European countries [68]. The knowledge of these findings would allow specific interventions or reforms necessary to prevent the spread of COVID-19. In Peru and other Spanish-speaking countries, adequate instruments are needed to measure self-care behaviors related to COVID-19 [69]. Therefore, our scale was found to have adequate internal consistency, presenting three differentiated components (physical, social and mental health self-care). In the determination of factors, 3 were retained, denominated as self-care of physical, social, and mental health, with a total of 29 items and explaining an accumulated variance of 50.03%, which is considered a minimum value according to previous reports [65].
A couple of self-care scales have been validated previously, the Self-Care Activities Screening Scale (SASS-14) was validated in Italy demonstrating good reliability, predictive and convergent validity in coping with COVID-19 lockdown and perceived stress [62]. The second scale was the Self-Care in COVID-19 (SCOVID) Scale, which was validated in Italy demonstrating adequate validity and reliability [70]. Within the same line, in Spain, Martínez, et al. [62] carried out a study with factorial analysis obtaining a KMO = 0.821, where they managed to retain 4 factors, which they named as health awareness, nutrition, physical activity, sleep, and intrapersonal and interpersonal coping skills. In that study, a total of 14 items in the scale-out of a total of 24, raised at the beginning of the analysis, explaining 43.3% of the variance [53]. Another study on the validation of a self-care scale in professionals in the United States, using a confirmatory analysis, resulted in a total of 2 dimensions with 18 items, out of 38 initial items that passed the evaluation [71].
A recent study performed in Slovakia reported that well-practiced self-care activities should be immediately implemented in an individual’s life in order to reduce depressive symptoms [61]. It was reported that sleep quality played an important role, while health consciousness, gender and age also play a critical role that should not be overlooked [61]. This study showed that females and younger individuals need targeted interventions in the terms of depression during the COVID-19 pandemic in Slovakia [61]. A study in Iran evaluated the important indicators for self-care in mobile health applications during the COVID-19 pandemic [63]. It was identified that reminders to take medication and its adherence, the training in COVID-19 signs and symptoms, as well as recording daily fever were the most significant requirements to include in mobile health applications to monitor infectious diseases [63,72]. Medication reminders such as voicemails, app notifications and text messages have been considered critical as self-care behaviors for infectious diseases [73] such as tuberculosis [74] and HIV [75]. A study in Spain performed two analyses: an initial (exploratory) one, with the participation of 226 people, to discover the underlying factor structure and reduce the number of items in the original tool to an influential group of items related to self-care [53]. Subsequently, they conducted a confirmatory factor analysis on a new sample of 261 participants to test the factorial solutions’ fit and goodness of fit [53]. Likewise, in Chile, a study “Validation of the Self-Care Agency Assessment (ASA) scale in Chilean adolescents” was developed in 2020, whose results evidenced the cultural adaptation of some terms of the scale [76]. The exploratory factor analysis suggested the retention of five factors and one factor per sedimentation graph; the structural equations of the possible models resulted in fit index values close to satisfactory [76]. Another study in Chile implemented an eight-week multifaceted mindfulness-based self-care program on medical students’ distress and well-being during the COVID-19 pandemic [64]. A reduction in burnout prevalence, stress, self-blaming and traumatic stress were observed, accompanied with a higher mindfulness, resilience, and active coping strategies [64]. For this, validated scales were utilized observing a decreased emotional exhaustion after the program [64].
Although the present study was not carried out with confirmatory factor analysis, all this compared to our findings highlights the importance of further analyses of a confirmatory nature to have a better tool that allows us to address the issue of self-care in times of the COVID-19 pandemic. Finally, the evaluation of the test-retest has been widely used to determine instrument concordance [77,78]. Out results are similar to the values previously reported by Lee et al. (ICC = 0.97) when validating a self-care scale in a group of professionals from different areas [76].
In sum, our instrument contains the necessary conditions to become a valuable and reliable tool for measuring self-care behaviors against COVID-19 in a group of young university students. The study is not free of limitations; the virtual survey could generate response bias. Although it is not possible to make a complete inference to the entire university population of the country, the characteristics of the students should be considered. There were domains done according to the moment of the second wave of the COVID-19 pandemic in Peru. However, the patterns chosen have been those of greater relevance and consistency to avoid making a long instrument, which causes other types of bias related to the time of making the respective filling. Likewise, the study was only conducted in Huanuco, which is located in the central region of Peru. Thus, it does not adequately represent the general population of Peru and could induce a selection bias, limiting the generalization of the findings to samples from other regions of Peru. Therefore, it is necessary to have a more representative and diverse sample (with different educational levels, employment status, income level, history or presence of chronic diseases, etc.) to compare and generalize the results. Despite the limitations, the above results indicate that the scale of self-care behaviors against COVID-19 is a helpful instrument to understand self-care behaviors better and may also be helpful in large-scale studies in health emergency and third wave situations.
Acknowledgement: We are thankful for our respondents for their time and participation in the survey.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study
References
1. Sun, C., Zhai, Z. (2020). The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustainable Cities and Society, 62, 102390. DOI 10.1016/j.scs.2020.102390. [Google Scholar] [CrossRef]
2. Vokó, Z., Pitter, J. G. (2020). The effect of social distance measures on COVID-19 epidemics in Europe: An interrupted time series analysis. GeroScience, 42(4), 1075–1082. DOI 10.1007/s11357-020-00205-0. [Google Scholar] [CrossRef]
3. Olivera-La Rosa, A., Chuquichambi, E. G., Ingram, G. P. D. (2020). Keep your (social) distance: Pathogen concerns and social perception in the time of COVID-19. Personality and Individual Differences, 166, 110200. DOI 10.1016/j.paid.2020.110200. [Google Scholar] [CrossRef]
4. Hwang, T. J., Rabheru, K., Peisah, C., Reichman, W., Ikeda, M. (2020). Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics, 32(10), 1217–1220. DOI 10.1017/S1041610220000988. [Google Scholar] [CrossRef]
5. Pietrabissa, G., Simpson, S. G. (2020). Psychological consequences of social isolation during COVID-19 outbreak. Frontiers in Psychology, 11, 1–4. DOI 10.3389/fpsyg.2020.02201. [Google Scholar] [CrossRef]
6. Hamza, C. A., Ewing, L., Heath, N. L., Goldstein, A. L. (2021). When social isolation is nothing new: A longitudinal study on psychological distress during COVID-19 among university students with and without preexisting mental health concerns. Canadian Psychology/Psychologie Canadienne, 62(1), 20–30. DOI 10.1037/cap0000255. [Google Scholar] [CrossRef]
7. Filho, L., Wall, W., Rayman-Bacchus, T., Mifsud, L., Pritchard, M. et al. (2021). Impacts of COVID-19 and social isolation on academic staff and students at universities: A cross-sectional study. BMC Public Health, 21(1), 1213. DOI 10.1186/s12889-021-11040-z. [Google Scholar] [CrossRef]
8. Román, R., Moscoso, B., Chung, S., Limpias Terceros, S. A., Álvarez-Risco, B. et al. (2020). Tratamiento de la COVID-19 en perú y Bolivia y los riesgos de la automedicación. Revista Cubana de Farmacia, 53(2), 1–32. [Google Scholar]
9. Yáñez, J. A., Chung, S. A., Román, B. R., Hernández-Yépez, P. J., Garcia-Solorzano, F. O. et al. (2021). Chapter 14–Prescription, Over-the-Counter (OTCherbal, and other treatments and preventive uses for COVID-19. In: Hadi Dehghani, M., Karri, R. R., Roy, S. (Eds.Environmental and health management of novel coronavirus disease (COVID-19), pp. 379–416. London, UK: Academic Press. [Google Scholar]
10. Yáñez, J. A., Alvarez-Risco, A., Delgado-Zegarra, J. (2020). COVID-19 in Peru: From supervised walks for children to the first case of kawasaki-like syndrome. BMJ, 2020, 369. DOI 10.1136/bmj.m2418. [Google Scholar] [CrossRef]
11. Zhang, S. X., Sun, S., Afshar Jahanshahi, A., Alvarez-Risco, A., Ibarra, V. G. (2020). Developing and testing a measure of COVID-19 organizational support of healthcare workers–Results from Peru, Ecuador, and Bolivia. Psychiatry Research, 291, 113174. DOI 10.1016/j.psychres.2020.113174. [Google Scholar] [CrossRef]
12. Zhang, S. X., Chen, J., Afshar Jahanshahi, A., Alvarez-Risco, A., Dai, H. (2021). Succumbing to the COVID-19 pandemic-healthcare workers not satisfied and intend to leave their jobs. International Journal of Mental Health and Addiction, 20(2), 956–965. DOI 10.1007/s11469-021-00502-5. [Google Scholar] [CrossRef]
13. Zhang, S. X., Chen, J., Jahanshahi, A. A., Alvarez-Risco, A., Dai, H. (2021). Correction to: Succumbing to the COVID-19 pandemic—Healthcare workers not satisfied and intend to leave their jobs. International Journal of Mental Health and Addiction, 1. DOI 10.1007/s11469-021-00502-5. [Google Scholar] [CrossRef]
14. Yáñez, J. A., Jahanshahi, A. A., Alvarez-Risco, A., Li, J., Zhang, S. X. (2020). Anxiety, distress, and turnover intention of healthcare workers in Peru by their distance to the epicenter during the COVID-19 crisis. American Journal of Tropical Medicine and Hygiene, 103(4), 1614–1620. DOI 10.4269/ajtmh.20-0800. [Google Scholar] [CrossRef]
15. Alvarez-Risco, A., Mejia, C. R., Delgado-Zegarra, J., Del-Aguila-Arcentales, S., Arce-Esquivel, A. A. et al. (2020). The Peru approach against the COVID-19 infodemic: Insights and strategies. American Journal of Tropical Medicine and Hygiene, 103(2), 583–586. DOI 10.4269/ajtmh.20-0536. [Google Scholar] [CrossRef]
16. Chen, X., Zhang, S. X., Jahanshahi, A. A., Alvarez-Risco, A., Dai, H. et al. (2020). Belief in a COVID-19 conspiracy theory as a predictor of mental health and well-being of health care workers in Ecuador: Cross-sectional survey study. JMIR Public Health and Surveillance, 6(3), e20737. DOI 10.2196/20737. [Google Scholar] [CrossRef]
17. Chung, S. A., Rebollo, A., Quiroga, A., Paes, I., Yáñez, J. A. (2021). Factores de riesgo de ansiedad en estudiantes de Bolivia durante la pandemia de la COVID-19. Revista Cubana de Farmacia, 54(4), 1–18. [Google Scholar]
18. Quispe-Cañari, J. F., Fidel-Rosales, E., Manrique, D., Mascaró-Zan, J., Huamán-Castillón, K. M. et al. (2021). Self-medication practices during the COVID-19 pandemic among the adult population in Peru: A cross-sectional survey. Saudi Pharmaceutical Journal, 29(1), 1–11. DOI 10.1016/j.jsps.2020.12.001. [Google Scholar] [CrossRef]
19. Villena-Tejada, M., Vera-Ferchau, I., Cardona-Rivero, A., Zamalloa-Cornejo, R., Quispe-Florez, M. et al. (2021). Use of medicinal plants for COVID-19 prevention and respiratory symptom treatment during the pandemic in Cusco, Peru: A cross-sectional survey. PLoS One, 16(9), e0257165. DOI 10.1371/journal.pone.0257165. [Google Scholar] [CrossRef]
20. Vizcardo, D., Salvador, L. F., Nole-Vara, A., Dávila, K. P., Alvarez-Risco, A. et al. (2022). Sociodemographic predictors associated with the willingness to get vaccinated against COVID-19 in Peru: A cross-sectional survey. Vaccines, 10(1), 48. DOI 10.3390/vaccines10010048. [Google Scholar] [CrossRef]
21. Shafi, M., Liu, J., Ren, W. (2020). Impact of COVID-19 pandemic on micro, small, and medium-sized enterprises operating in Pakistan. Research in Globalization, 2, 100018. DOI 10.1016/j.resglo.2020.100018. [Google Scholar] [CrossRef]
22. Soriano, V., Corral, O. (2020). Keeping alive enterprises while embracing unprecedented COVID-19 restrictions. Therapeutic Advances in Infectious Disease, 7, 2049936120920175. DOI 10.1177/2049936120920175. [Google Scholar] [CrossRef]
23. Beiderbeck, D., Frevel, N., von der Gracht, H. A., Schmidt, S. L., Schweitzer, V. M. (2021). The impact of COVID-19 on the European football ecosystem–A delphi-based scenario analysis. Technological Forecasting and Social Change, 165, 120577. DOI 10.1016/j.techfore.2021.120577. [Google Scholar] [CrossRef]
24. Alvarez-Risco, A., Estrada-Merino, A., Perez-Luyo, R. (2020). Sustainable development goals in hospitality management. Sustainable Hospitality Management, 24, 159–178. DOI 10.1108/asm. [Google Scholar] [CrossRef]
25. Yan, J., Kim, S., Zhang, S. X., Foo, M. D., Alvarez-Risco, A. (2021). Hospitality workers’ COVID-19 risk perception and depression: A contingent model based on transactional theory of stress model. International Journal of Hospitality Management, 95, 1–11. [Google Scholar]
26. Alvarez-Risco, A., Del-Aguila-Arcentales, S., Yáñez, J. A., Rosen, M. A., Mejia, C. R. (2021). Influence of technostress on academic performance of university medicine students in Peru during the COVID-19 pandemic. Sustainability, 13(16), 8949. DOI 10.3390/su13168949. [Google Scholar] [CrossRef]
27. Alvarez-Risco, A., Estrada-Merino, A., Anderson-Seminario, M. D. L. M., Mlodzianowska, S., García-Ibarra, V. et al. (2021). Multitasking behavior in online classrooms and academic performance: Case of university students in Ecuador during COVID-19 outbreak. Interactive Technology and Smart Education, 18(3), 422–434. DOI 10.1108/ITSE-08-2020-0160. [Google Scholar] [CrossRef]
28. Alvarez-Risco, A., Del-Aguila-Arcentales, S., Rosen, M. A., García-Ibarra, V., Maycotte-Felkel, S. et al. (2021). Expectations and interests of university students in COVID-19 times about sustainable development goals: Evidence from Colombia, Ecuador, Mexico, and Peru. Sustainability, 13(6), 3306. DOI 10.3390/su13063306. [Google Scholar] [CrossRef]
29. Alvarez-Risco, A., Del-Aguila-Arcentales, S., Yanez, J. A. (2021). Telemedicine in Peru as a result of the COVID-19 pandemic: Perspective from a country with limited internet access. The American Journal of Tropical Medicine and Hygiene, 105(1), 6–11. DOI 10.4269/ajtmh.21-0255. [Google Scholar] [CrossRef]
30. Alvarez-Risco, A., Estrada-Merino, A., Rosen, M. A., Vargas-Herrera, A., Del-Aguila-Arcentales, S. (2021). Factors for implementation of circular economy in firms in COVID-19 pandemic times: The case of Peru. Environments, 8(9), 95. DOI 10.3390/environments8090095. [Google Scholar] [CrossRef]
31. Alvarez-Risco, A., Mlodzianowska, S., García-Ibarra, V., Rosen, M. A., Del-Aguila-Arcentales, S. (2021). Factors affecting green entrepreneurship intentions in business university students in COVID-19 pandemic times: Case of Ecuador. Sustainability, 13(11), 6447. DOI 10.3390/su13116447. [Google Scholar] [CrossRef]
32. Apcho-Ccencho, L. V., Cuya-Velásquez, B. B., Alvarado Rodríguez, D., Anderson-Seminario, M. D. L. M., Alvarez-Risco, A. (2021). The impact of international price on the technological industry in the United States and China during times of crisis: Commercial War and COVID-19. Advances in Business and Management Forecasting, 14, 149–160. DOI 10.1108/abmf. [Google Scholar] [CrossRef]
33. Leiva-Martinez, M. A., Anderson-Seminario, M. D. L. M., Alvarez-Risco, A., Estrada-Merino, A., Mlodzianowska, S. (2021). Price variation in lower goods as of previous economic crisis and the contrast of the current price situation in the context of COVID-19 in Peru. Advances in Business and Management Forecasting, 14, 161–166. DOI 10.1108/abmf. [Google Scholar] [CrossRef]
34. Lal, A., Erondu, N. A., Heymann, D. L., Gitahi, G., Yates, R. (2021). Fragmented health systems in COVID-19: Rectifying the misalignment between global health security and universal health coverage. The Lancet, 397(10268), 61–67. DOI 10.1016/S0140-6736(20)32228-5. [Google Scholar] [CrossRef]
35. Galdames-Cruz, S., Jamet-Rivera, P., Bonilla-Espinoza, A., Quintero-Carvajal, F., Rojas-Muñoz, V. (2019). Creencias sobre salud y prácticas de autocuidado en adultos jóvenes: Estudio biográfico de estilos de vida. Hacia la Promoción de la Salud, 24(1), 28–43. DOI 10.17151/hpsal. [Google Scholar] [CrossRef]
36. Cangelosi, G., Grappasonni, I., Pantanetti, P., Scuri, S., Garda, G. et al. (2022). Nurse case manager lifestyle medicine (NCMLM) in the type Two diabetes patient concerning post COVID-19 pandemic management: Integrated-scoping literature review. Annali di Igiene : Medicina Preventiva e di Comunita. [Google Scholar]
37. WHO advice for the public: Coronavirus disease (COVID-19) (2021). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public. [Google Scholar]
38. MINSA (Ministerio de Salud del Peru (2021). MINSA mental health care of the affected population, families and community, in the context of COVID-19 [Cuidado de la salud mental de la población afectada, familias y comunidad, en el contexto del COVID–19]. http://bvs.minsa.gob.pe/local/MINSA/5001.pdf. [Google Scholar]
39. WHO COVID-19 strategy update (2021). https://www.who.int/publications/m/item/covid-19-strategy-update. [Google Scholar]
40. Vera-Ponce, V. J., Torres-Malca, J. R., Tello-Quispe, E. K., Orihuela-Manrique, E. J., Cruz-Vargas, J. A. (2020). Validation of scale of changes in lifestyles during the quarantine period in a population of university students from Lima, Peru. Revista de la Facultad de Medicina Humana, 20(4), 614–623. DOI 10.25176/RFMH. [Google Scholar] [CrossRef]
41. Nakazawa, E., Yamamoto, K., London, A. J., Akabayashi, A. (2021). Solitary death and new lifestyles during and after COVID-19: Wearable devices and public health ethics. BMC Medical Ethics, 22(1), 89. DOI 10.1186/s12910-021-00657-9. [Google Scholar] [CrossRef]
42. Yang, G. Y., Lin, X. L., Fang, A. P., Zhu, H. L. (2021). Eating habits and lifestyles during the initial stage of the COVID-19 lockdown in China: A cross-sectional study. Nutrients, 13(3), 1–12. DOI 10.3390/nu13030970. [Google Scholar] [CrossRef]
43. Bermudez-Aguirre, D., Yáñez, J., Dunne, C., Davies, N., Barbosa-Cánovas, G. (2010). Study of strawberry flavored milk under pulsed electric field processing. Food Research International, 43, 2201–2207. DOI 10.1016/j.foodres.2010.07.021. [Google Scholar] [CrossRef]
44. Yáñez, J. A., Miranda, N. D., Remsberg, C. M., Ohgami, Y., Davies, N. M. (2007). Stereospecific high-performance liquid chromatographic analysis of eriodictyol in urine. Journal of Pharmaceutical and Biomedical Analysis, 43(1), 255–262. DOI 10.1016/j.jpba.2006.06.027. [Google Scholar] [CrossRef]
45. Vega-Villa, K. R., Remsberg, C. M., Ohgami, Y., Yanez, J. A., Takemoto, J. K. et al. (2009). Stereospecific high-performance liquid chromatography of taxifolin, applications in pharmacokinetics, and determination in tu fu ling (Rhizoma smilacis glabrae) and apple (Malus x domestica). Biomed Chromatogr, 23(6), 38–46. DOI 10.1002/bmc.1165. [Google Scholar] [CrossRef]
46. Ramos-Escudero, F., Santos-Buelga, C., Pérez-Alonso, J. J., Yáñez, J. A., Dueñas, M. (2010). HPLC-DAD-ESI/MS identification of anthocyanins in Dioscorea trifida L. yam tubers (purple sachapapa). European Food Research and Technology, 230(5), 745–752. DOI 10.1007/s00217-010-1219-5. [Google Scholar] [CrossRef]
47. Roupe, K. A., Helms, G. L., Halls, S. C., Yanez, J. A., Davies, N. M. (2005). Preparative enzymatic synthesis and HPLC analysis of rhapontigenin: Applications to metabolism, pharmacokinetics and anti-cancer studies. Journal of Pharmaceutical Sciences, 8(3), 374–386. [Google Scholar]
48. Yáñez, J. A., Remsberg, C. M., Takemoto, J. K., Vega-Villa, K. R., Andrews, P. K. (2012). Polyphenols and flavonoids: An overview. In: Flavonoid pharmacokinetics: Methods of analysis, preclinical and clinical pharmacokinetics, safety, and toxicology, pp. 1–69. [Google Scholar]
49. Bonin, A. M., Yáñez, J. A., Fukuda, C., Teng, X. W., Dillon, C. T. et al. (2010). Inhibition of experimental colorectal cancer and reduction in renal and gastrointestinal toxicities by copper-indomethacin in rats. Cancer Chemotherapy and Pharmacology, 66(4), 755–764. DOI 10.1007/s00280-009-1220-5. [Google Scholar] [CrossRef]
50. Yáñez, J. A., Teng, X. W., Roupe, K. A., Davies, N. M. (2005). Stereospecific high-performance liquid chromatographic analysis of hesperetin in biological matrices. Journal of Pharmaceutical and Biomedical Analysis, 37(3), 591–595. DOI 10.1016/j.jpba.2004.10.028. [Google Scholar] [CrossRef]
51. Remsberg, C. M., Yanez, J. A., Roupe, K. A., Davies, N. M. (2007). High-performance liquid chromatographic analysis of pterostilbene in biological fluids using fluorescence detection. Journal of Pharmaceutical and Biomedical Analysis, 43(1), 250–254. DOI 10.1016/j.jpba.2006.06.035. [Google Scholar] [CrossRef]
52. Xiong, M. P., Yáñez, J. A., Kwon, G. S., Davies, N. M., Forrest, M. L. (2009). A cremophor-free formulation for tanespimycin (17-AAG) using PEO-b-PDLLA micelles: Characterization and pharmacokinetics in rats. Journal of Pharmaceutical Sciences, 98(4), 1577–1586. DOI 10.1002/jps.21509. [Google Scholar] [CrossRef]
53. Yanez, J. A., Davies, N. M. (2005). Stereospecific high-performance liquid chromatographic analysis of naringenin in urine. Journal of Pharmaceutical and Biomedical Analysis, 39(1–2), 164–169. DOI 10.1016/j.jpba.2005.02.025. [Google Scholar] [CrossRef]
54. Rodakowska, E., Mazur, M., Baginska, J., Sierpinska, T., La Torre, G. et al. (2020). Smoking prevalence, attitudes and behavior among dental students in Poland and Italy. International Journal of Environmental Research and Public Health, 17(20), 1–12. DOI 10.3390/ijerph17207451. [Google Scholar] [CrossRef]
55. Fernández-García, D., Ordás, B., Fernández-Peña, R., Bárcena-Calvo, C., Ordoñez, C. et al. (2020). Smoking in nursing students: A prevalence multicenter study. Medicine, 99(14), e19414. DOI 10.1097/MD.0000000000019414. [Google Scholar] [CrossRef]
56. Nasser, A. M. A., Geng, Y., Al-Wesabi, S. A. (2020). The prevalence of smoking (Cigarette and waterpipe) among university students in some arab countries: A systematic review. Asian Pacific Journal of Cancer Prevention, 21(3), 583–591. DOI 10.31557/APJCP.2020.21.3.583. [Google Scholar] [CrossRef]
57. Cooke, R., Bailey, O., Jennings, J., Yuen, C., Gardner, B. (2021). Do preparatory behaviours predict alcohol consumption among UK university students? British Journal of Health Psychology, 26(2), 343–359. DOI 10.1111/bjhp.12489. [Google Scholar] [CrossRef]
58. Almulla, A. A., Faris, M. E. A. I. E. (2020). Energy drinks consumption is associated with reduced sleep duration and increased energy-dense fast foods consumption among school students: A cross-sectional study. Asia Pacific Journal of Public Health, 32(5), 266–273. DOI 10.1177/1010539520931351. [Google Scholar] [CrossRef]
59. Ahmed, B., Navid Yousaf, F., Saud, M., Ahmad, A. (2020). Youth at risk: The alarming issue of drug addiction in academic institutions in Pakistan. Children and Youth Services Review, 118, 105385. DOI 10.1016/j.childyouth.2020.105385. [Google Scholar] [CrossRef]
60. Luján-Tangarife, J. A., Cardona-Arias, J. A. (2015). Construcción y validación de escalas de medición en salud: Revi revisión de propiedades psicométricassión de propiedades psicométricas. Archivos de Medicina, 11(3), 1. [Google Scholar]
61. Gavurova, B., Popesko, B., Ivankova, V., Rigelsky, M. (2021). The role of self-care activities (SASS-14) in depression (PHQ-9Evidence from Slovakia during the COVID-19 pandemic. Frontiers in Public Health, 9, 803815. DOI 10.3389/fpubh.2021.803815. [Google Scholar] [CrossRef]
62. Martínez, M., Luis, E. O., Oliveros, E. Y., Fernández-Berrocal, P., Sarrionandia, A. (2021). Validity and reliability of the self-care activities screening scale (SASS-14) during COVID-19 lockdown. Health Qual Life Outcomes, 19(1), 1. DOI 10.1186/s12955-020-01607-6. [Google Scholar] [CrossRef]
63. Mohammad, H., Elham, M., Mehraeen, E., Aghamohammadi, V., Seyedalinaghi, S. et al. (2021). Identifying data elements and key features of a mobile-based self-care application for patients with COVID-19 in Iran. Health Informatics Journal, 27(4), 14604582211065703. DOI 10.1177/14604582211065703. [Google Scholar] [CrossRef]
64. Zúñiga, D., Torres-Sahli, M., Nitsche, P., Echeverría, G., Pedrals, N. (2021). Reduced burnout and higher mindfulness in medical students after a self-care program during the COVID-19 pandemic. Revista medica de Chile, 149(6), 1–12. [Google Scholar]
65. Hair, J. F., Ringle, C. M., Sarstedt, M. (2011). PLS-SEM: Indeed a silver bullet. Journal of Marketing Theory and Practice, 19(2), 139–152. DOI 10.2753/MTP1069-6679190202. [Google Scholar] [CrossRef]
66. Gómez del Pulgar García Madrid, M., Hernández-Iglesias, S., Crespo Cañizares, A., Pérez Martín, A. M., González Jurado, M. A. (2019). Fiabilidad de una escala para la evaluación de competencias enfermeras: Estudio de concordancia. Educación Médica, 20(4), 221–230. [Google Scholar]
67. Taber, K. S. (2018). The use of cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education, 48(6), 1273–1296. DOI 10.1007/s11165-016-9602-2. [Google Scholar] [CrossRef]
68. Fantin R, B. C. G., Barboza-Solís, C. (2021). COVID-19 deaths: Distribution by age and universal medical coverage in 22 countries [Defunciones por COVID-19: Distribución por edad y universalidad de la cobertura médica en 22 países]. Revista Panamericana de Salud Pública, 45, e42. [Google Scholar]
69. Caycho-Rodríguez, T., Ventura-León, J., Barboza-Palomino, M. (2021). Diseño y validación de una escala para medir la preocupación por el contagio de la COVID-19 (PRE-COVID-19). Enfermería Clínica, 31(3), 175–183. [Google Scholar]
70. De Maria, M., Ferro, F., Ausili, D., Alvaro, R., de Marinis, M. G. (2020). Development and psychometric testing of the self-care in COVID-19 (SCOVID) scale, an instrument for measuring self-care in the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 17(21), 1–12. DOI 10.3390/ijerph17217834. [Google Scholar] [CrossRef]
71. Lee, J. J., Miller, S. E., Bride, B. E. (2020). Development and initial validation of the self-care practices scale. Social Work, 65(1), 21–28. DOI 10.1093/sw/swz045. [Google Scholar] [CrossRef]
72. Yamamoto, K., Takahashi, T., Urasaki, M., Nagayasu, Y., Shimamoto, T. et al. (2020). Health observation App for COVID-19 symptom tracking integrated with personal health records: Proof of concept and practical use study. JMIR mHealth and uHealth, 8(7), e19902. DOI 10.2196/19902. [Google Scholar] [CrossRef]
73. Saberi, P., Johnson, M. O. (2011). Technology-based self-care methods of improving antiretroviral adherence: A systematic review. PLoS One, 6(11), e27533. DOI 10.1371/journal.pone.0027533. [Google Scholar] [CrossRef]
74. Narasimhan, P., Bakshi, A., Kittusami, S., Prashant, S., Mathai, D. et al. (2013). A customized m-health system for improving tuberculosis treatment adherence and follow-up in south India. Health and Technology, 4, 1–10. [Google Scholar]
75. Perera, A. I., Thomas, M. G., Moore, J. O., Faasse, K., Petrie, K. J. (2014). Effect of a smartphone application incorporating personalized health-related imagery on adherence to antiretroviral therapy: A randomized clinical trial. AIDS Patient Care and STDs, 28(11), 579–586. DOI 10.1089/apc.2014.0156. [Google Scholar] [CrossRef]
76. Espinoza-Venegas, M., Huaiquián-Silva, J., Sanhueza-Alvarado, O., Luengo-Machuca, L., Valderrama-Alarcón, M. et al. (2020). Validación de escala de valoración de agencia de autocuidado (ASA) en adolescentes chilenos. Escola Anna Nery, 24, 1–7. [Google Scholar]
77. Mandeville-Norden, R., Beech, A. R. (2008). Development of a psychometric typology of child molesters: Implications for treatment. Journal of Interpersonal Violence, 24(2), 307–325. DOI 10.1177/0886260508316479. [Google Scholar] [CrossRef]
78. Cortés-Reyes, É., Rubio-Romero, J. A., Gaitán-Duarte, H. (2010). Métodos estadísticos de evaluación de la concordancia y la reproducibilidad de pruebas diagnósticas. Revista Colombiana de Obstetricia y Ginecología, 61(3), 247–255. DOI 10.18597/rcog.271. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools