 Open Access
Open Access
REVIEW
Validation of Symptom Dimensions and Sub-Type Responses in Cognitive Behavioral Therapy in Obsessive Compulsive Disorder: A Systemic Review and Meta-Analysis
1 Department of Clinical Psychology, Beijing Anding Hospital, Capital Medical University, Beijing, 100088, China
2 The National Clinical Research Center for Mental Disorders & Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital, Beijing, 100088, China
3 Department of Clinical Psychology, Weifang People’s Hospital, Weifang, 261041, China
* Corresponding Author: Zhanjiang Li. Email:
International Journal of Mental Health Promotion 2022, 24(6), 843-854. https://doi.org/10.32604/ijmhp.2022.021009
Received 22 December 2021; Accepted 10 August 2022; Issue published 28 September 2022
Abstract
Background: Obsessive-compulsive disorder (OCD) is a clinically heterogeneous condition without a conclusive subtype dimension. This study will focus on the meta-analysis of the clinical responses of OCD subtypes to cognitive behavioral therapy (CBT), which might clarify this issue. Methods: We performed a systematic search and a meta-analysis for the studies of OCD subtypes and the response to CBT in PubMed, ScienceDirect, Embase, Web of Science, and Scopus databases. The selective criteria were the OCD without significant medical or psychiatric co-morbidities and pre-and post-treatment changes in scores of OCD dimension. In addition, different subtypes of OCD in symptom dimensions, such as symmetry, contamination, unacceptable thoughts, and hoarding, were compared to find the most significant subtype using the treatment response parameters by CBT. After limited selection, four studies and 479 OCD subjects were enrolled. The meta-analysis was performed by Review Manager 5.4, and only significant results were reported. Results: Among the OCD subtypes, the meta-analysis favors the hoarding subtype with poorer responses to CBT than symmetry, contamination, and unacceptable thoughts. The meta-analysis results were negative mean differences, significant tests for overall effect, and limited heterogeneities in the random effects model. In addition, the results were more significant when the hoarding subtype was compared with non-hoarding subtypes. Conclusion: The hoarding subtype might be the most significant representative subtype of OCD symptom dimension under the impression of unfavorable clinical response to CBT. However, future studies with more treatment parameters will be warranted to confirm this finding.Keywords
Nomenclature
| CBT | Cognitive behavioral therapy |
| Y-BOCS | Yale-Brown Obsessive Compulsive Scale |
| UT | Unacceptable thoughts |
Obsessive-compulsive disorder (OCD) is a clinically heterogeneous condition. With difficult to delineate the classification and validation of OCD subtypes [1–4]. For the subtypes by the symptom dimension, a former meta-analysis of exploratory factor analysis studies showed that four significant factors might be the representative subtypes: symmetry, unacceptable thoughts (UT), cleaning/contamination, and hoarding [2].
Among the treatment options for OCD, medication treatment, such as antidepressants, will be a crucial choice. Apart from the medication treatment, psychotherapy will be another essential part. Cognitive behavioral therapy (CBT) will be the first choice. In the above four subtypes of symptom dimension in OCD, the validations of these factors would still be needed. The different subtypes seemed to be associated with treatment response from the treatment response to CBT in the subjects with OCD. Several studies suggested that sexual/religious/aggressive (UT subtype) would be related to worse treatment response to CBT [5–9]. The poor treatment response of this subtype might be related to delayed treatment and shame of such obsession for such subtype [10] or mental compulsion for reassurance seeking for such subtype [11]. The alterations of amygdala function [12,13] and the front-limbic alterations towards moral sense [14] in such subtype might also play a role in a worse response to CBT. However, one study reported null findings for the subtype response to CBT [15]. In addition, other previous studies reported that the hoarding subtype would be associated with poorer treatment response to CBT [5,16–19]. The lack of adherence and premature termination might be the significant causes [19]. The symmetry subtype was not inferior to other subtypes in the treatment response of CBT [16,18,19]. Therefore, the treatment responses to the CBT of different subtypes might be necessary for the clinical practice and treatment of OCD patients. The systematic review and meta-analysis can validate CBT’s OCD subtypes and related treatment responses. The results can help clinicians determine if the treatment of CBT can be used with better responses according to the OCD subtypes.
The current meta-analysis would address this issue to find the most significant subtype according to the treatment response to CBT. We would enroll the related studies with symptom dimension subtypes and the treatment response under CBT treatment status. The reasons to focus on CBT would be as follows. First, the CBT studies would not suffer from the obstacles of pharmacotherapy when the researchers performed a meta-analysis, such as the different kinds of antidepressants, neurotransmitter modulations, dose equivalents transformations, and various dose ranges. The above issues would make interpretations of meta-analysis results difficult and prone to bias. Second, CBT would be the most appropriate treatment of psychotherapeutic territory for OCD, making the meta-analysis more consistent with the daily life practice of the clinicians. Third, focusing only on CBT might make our meta-analysis results more homogeneous for the enrolled studies, which would be associated with more solid results with less bias.
According to the above literature, the four factors of symptom dimension subtypes [2] would be used as the significant variables to classify OCD. The previous articles used to predict the treatment response by regression analysis. However, the meta-analysis of regression results would not be the primary focus of the current study. The meta-analysis of the improvements in clinical symptoms for a specific subtype of OCD would be a significant issue in the current study. In addition, the studies of treatment responses to CBT would be the primary basis to validate the significance of subtype classification in OCD. We hypothesized that hoarding or UT would be the subtype of OCD associated with worse treatment response to CBT.
This section outlines the methods considered in this work.
2.1 Literature Search and Selection Criteria
This work used the following keywords “obsessive-compulsive disorder” or “obsessive” or “obsession” or “compulsive” or “compulsion” or “symmetry” or “repeating” or “ordering” or “counting” or “forbidden thoughts” or “unacceptable thoughts” or “aggression” or “aggressive” or “sexual” or “religious” or “somatic” or “checking” or “cleaning” or “contamination” or “hoarding” or “treatment” or “outcome” or “response” and “cognitive behavioral therapy” and “behavioral therapy” and “symptom dimension” to search and collect the related articles in the PubMed, ScienceDirect, Embase, Web of Science and Scopus databases. The articles were limited to those published or e-published online before September 2020.
The inclusion criteria of this study were (i) OCD patients without significant comorbidities of physical illness (significant medical diseases, such as cardiovascular diseases, gastrointestinal and renal diseases, metabolic diseases, neurological diseases, and immune diseases). (ii) The studies with CBT treatment outcomes and response profiles (iii) The articles with detailed data on symptom dimension subtypes of OCD and the clinical responses of CBT. The definition of detailed data meant that each subtype of OCD patients had pre-treatment Y-BOCS (Yale-Brown Obsessive Compulsive Scale) scores, post-treatment YBOCS scores, or changes in the YBOCS scores or YBOCS percentages of scores after CBT. (iv) These studies were also published in English in the science citation index database journals. (v) Concurrent medication treatment might be allowed. The exclusion criteria were: (i) Detailed data was partially eligible. With some parts unavailable in the content of the articles (the corresponding authors would be inquired about the data we needed in this meta-analysis), (ii) If the authors did not respond or already could not have access to the dataset, the articles would be excluded as the category without detailed data of CBT response, (iii) The studies without Y-BOCS dimension, (iv) Review articles, (5) Not relatively pure OCD (with significant psychiatric comorbidities, such as major depressive disorder > 50%, psychotic disorders > 50%, substance use disorder > 50%, bipolar disorder > 50%, attention deficit hyperactivity disorder > 50%, autistic disorder > 50%).
2.2 Quality Assessment and Data Extraction
The study was conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [20]. The random sequence generation assessed the risk of bias for each study, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting. We extracted the following data from the eligible articles. First, the pre-treatment (baseline) Y-BOCS scores for each subtype of OCD subjects. Second, the post-treatment Y-BOCS scores for each subtype of OCD subjects. Third, the change in Y-BOCS scores after CBT treatment for each subtype of OCD subjects. Fourth, the percentages of changes in Y-BOCS scores were also transformed into the absolute values of changes in Y-BOCS scores.
2.3 Meta-Analysis and Statistical Analysis
This work considered the Cochrane Collaboration Review Manager Software Package (Rev Man Version 5.4) to perform the meta-analyses. Different subtypes of OCD in symptom dimensions, such as symmetry, contamination, unacceptable thoughts (UT), and hoarding, were compared to each other to find the most significant subtype using the treatment response parameters by CBT. The overall effect size of changes in Y-BOCS scores was calculated as the weighted average of the inverse variance for the study-specific estimates. For continuous variables, the weighted mean difference (WMD) was used to estimate numerical variables. The χ2 distribution test and Higgins I2 index were used to estimate the heterogeneity. The heterogeneity was also tested by Cochran’s Q and Tau square test. The synthesized results were conducted by pooling the data and using a random effects model meta-analysis. If essential, subgroup analysis was performed to explain the heterogeneity and stratify the data according to different periods. In addition, the forest plot was used to estimate if the meta-analysis would favor specific subtypes of OCD subjects in the response status to CBT. Finally, the test for overall effect was calculated to produce the Z value and determine the significance of the p-value.
This section of the work presents the results obtained from the proposed study.
The initial literature search through the dataset found 3129 articles, and additional records from other sources were 15 articles (a total of 3144 articles). Then 1558 duplicates were removed. The residual 1586 articles (the total articles discarding the 1558 duplicate articles) were screened according to the relevance of abstracts and titles. The 1564 articles were discarded after this step. Next, entire text contents were assessed for the eligibility for the remaining 22 articles [5–7,9–11,15–19,21–31]. Among these candidates, 3 were review articles [6,19,23], which were excluded. Fourteen articles were excluded due to no detailed data of CBT response in articles and not being provided by authors after email contact. 5 articles were included in qualitative analyses. However, 1 study was excluded because the dimension was not the dimension of the Y-BOCS scale [15]. At last, four studies [7,16,24,28] were enrolled in the quantitative analysis (meta-analysis). The flow diagram was presented according to the PRISMA guideline (Fig. 1). The detailed characteristics of the four studies were also summarized (Table 1).
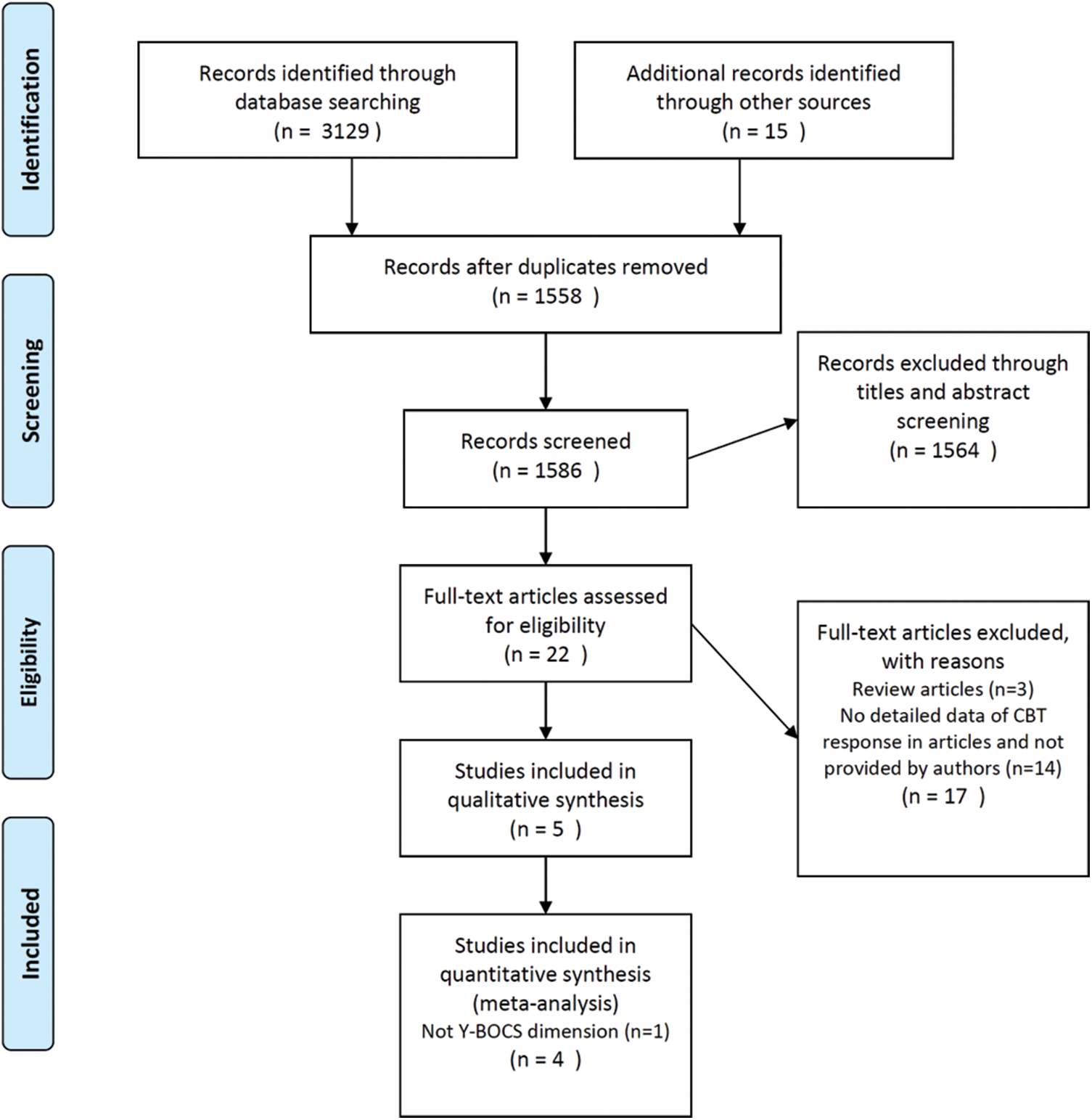
Figure 1: The PRISMA flow diagram of current meta-analysis

Fig. 1 presents the PRISMA flow diagram of the current meta-analysis. The current meta-analysis followed the PRISMA guideline to identify the potentially relevant literature and screen the identified literature using abstract and title selection. Then, the full text of screened literature was assessed to find the eligible studies and include the suitable ones for the final meta-analysis.
3.2 Significant Results: Comparison Between Hoarding Subtype and UT Subtype
In the meta-analysis of changes in Y-BOCS scores after CBT in hoarding and UT subtypes of OCD subjects, the forest plot favored poorer response of hoarding subtype compared to UT subtype (hoarding: 66 subjects; UT: 143 subjects; total: 207 subjects) (Fig. 2). In this meta-analysis, we enrolled three studies [7,16,24] because the three studies had detailed data on hoarding and UT subtype patients. Therefore, one study [28] would be weighted 0% in this meta-analysis. The heterogeneity of this comparison was low (heterogeneity Tau² = 0.32; Chi² = 2.21, df = 2 (p = 0.33); I² = 10%). The result was significant (test for overall effect: Z = 4.24; p < 0.0001).
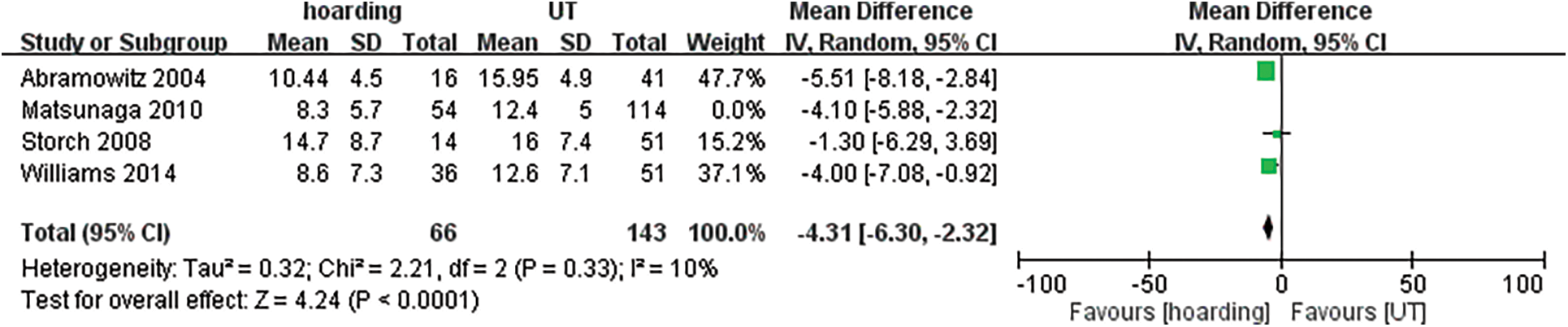
Figure 2: The hoarding vs. UT meta-analysis forest plot
In Fig. 2, the hoarding vs. UT meta-analysis forest plot is presented. The hoarding subtype showed a favorable result with poorer treatment response to CBT than UT. The heterogeneity was low, and the result was statistically significant.
3.3 Significant Results: Comparison Between Hoarding Subtype and Non-Hoarding Subtypes
In this comparison, we enrolled four studies [7,16,24,28]. In addition, these studies recognized the non-hoarding subtype as other subtypes of OCD subjects, such as symmetry, UT, and contamination subtypes. In the meta-analysis of changes in Y-BOCS scores after CBT in hoarding and non-hoarding subtypes of OCD subjects, the forest plot favored a poorer response of the hoarding subtype when compared to the UT subtype (hoarding: 120 subjects; UT: 359 subjects; total: 479 subjects) (Fig. 3). The heterogeneity of this comparison was lowest (Heterogeneity: Tau² = 0.00; Chi² = 1.71, df = 3 (p = 0.64); I² = 0%). The result was most significant (Test for overall effect: Z = 6.46; p < 0.00001).
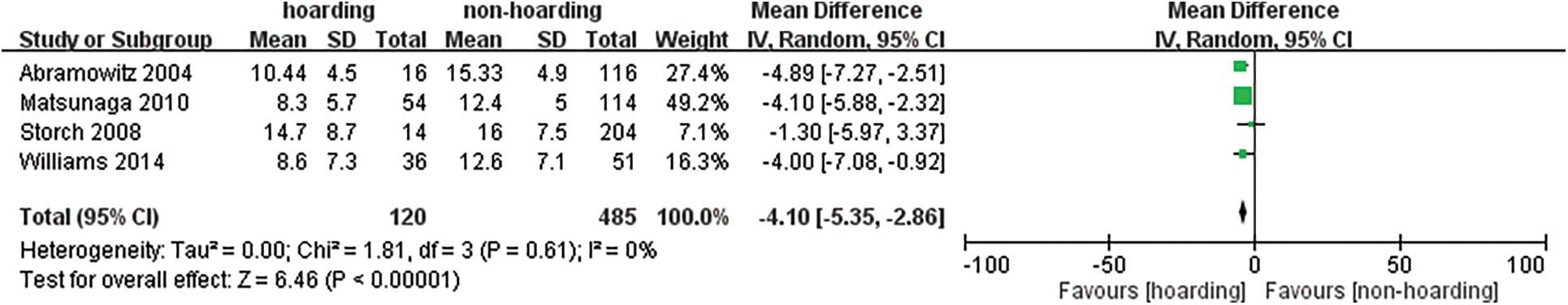
Figure 3: The hoarding vs. non-hoarding meta-analysis forest plot
In Fig. 3, the hoarding vs. non-hoarding meta-analysis forest plot is depicted. When the hoarding subtype was compared to the non-hoarding subtype, the poorer treatment response to CBT was more significant, and the heterogeneity was the lowest.
Because just one child and the adolescent study were enrolled in the current meta-analysis, we performed the subgroup analysis of the adult subgroup. For the adult subgroup analysis, the comparison results of hoarding vs. UT and hoarding vs. non-hoarding were still statistically significant (Figs. 4 and 5). The treatment response of the hoarding subtype was still poorer than UT and non-hoarding subtypes in the adult subgroup.
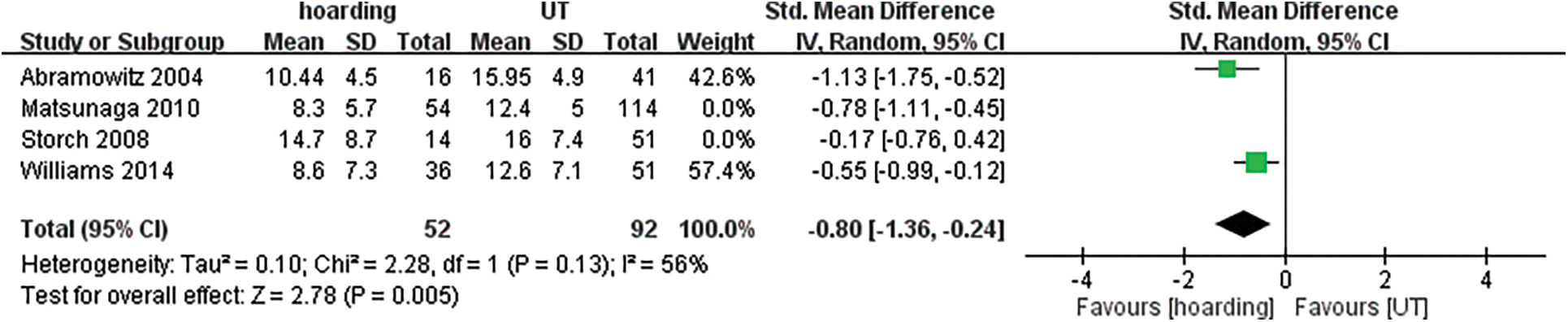
Figure 4: The hoarding vs. UT subgroup analysis (adult) forest plot
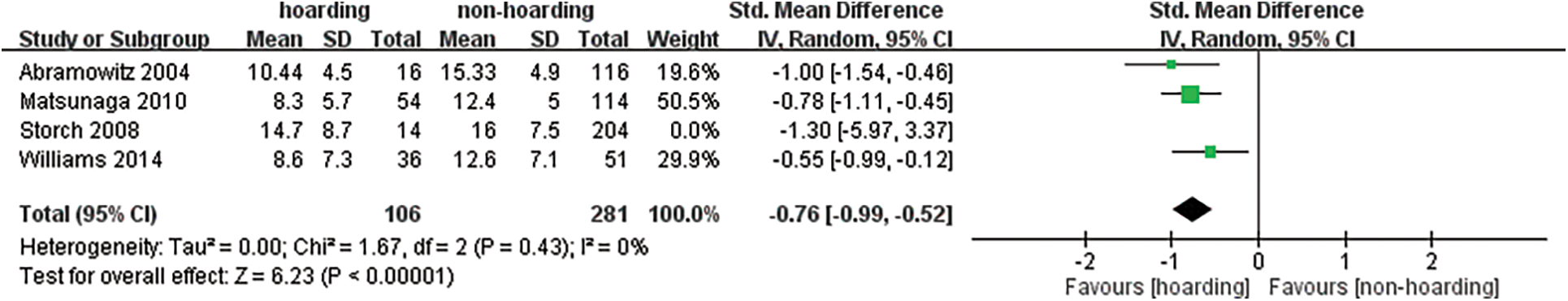
Figure 5: The hoarding vs. non-hoarding subgroup analysis (adult) forest plot
The comparison between hoarding and contamination reached a trend of statistical significance (heterogeneity Tau² = 3.18; Chi² = 1.78, df = 1 (p = 0.18); I² = 44%; test for overall effect: Z = 1.89; p = 0.06). The forest plot favored a poorer response of hoarding subtype to CBT. The comparison between hoarding and symmetry was not significant (test for overall effect: Z = 0.85; p = 0.40). The comparison between contamination and symmetry (test for overall effect: Z = 0.98; p = 0.33) was not significant. The comparison between contamination and UT was not significant (test for overall effect: Z = 0.79; p = 0.43). The comparison between symmetry and UT was also not significant (Test for overall effect: Z = 1.45; p = 0.15).
The significant findings in the current meta-analysis were as follows:
i) The hoarding subtype showed a poorer response to CBT, especially while the hoarding subtype was compared to UT or non-hoarding subtypes.
ii) The other subtypes, symmetry, contamination, and UT, did not represent the significant and specific subtypes based on CBT responses.
iii) The pooled data of hoarding vs. UT and hoarding vs. non-hoarding seemed more homogeneous.
Our study focused on CBT and YBOCS might have the advantages of better homogeneity of results and less bias for interpretations. The homogeneity of enrolled parameters in the current study would make the evaluations of results for the hoarding subtype more consistent and solid. The above will be the innovation points of the current meta-analysis.
Among the four enrolled studies, the characteristics were different from several perspectives. First, three studies [7,16,28] focused on adult OCD patients. Just 1 study focused on children and adolescents [24]. Among the three adult OCD studies, one study focused on patients of age 20–40 years old [28]. Second, just two studies included the complete subtypes of OCD [16,24]. One study classified OCD as hoarding and non-hoarding [28]. Another study included OCD patients with hoarding ad UT subtypes [7]. Third, the number, frequency, and duration of CBT sessions differed in the enrolled studies. The session number was similar in the two studies [16,24]. One study’s CBT duration was one year [28]. One study’s CBT was just four sessions [7]. Third, the study design was different in the enrolled studies. Two studies were the randomized trial design [7,24], and two were the intervention study design [16,28]. At last, for the changes in Y-BOCS scores, three studies reported absolute values [16,24,28], and one study reported the percentage [7].
The hoarding subtype might be associated with low parental warmth and perceived parental rearing style [32]. The distinct subtypes classified by symptom dimension might be related to distinct patterns of the neural substrate and genetic transmission, which would be associated with treatment response [33]. The hoarding subtype was prone to familial associations, suggesting a genetic predisposition [4]. Hoarding was also associated with poor insight, reduced control towards compulsion [34], higher anxiety scores [35], and not-just-right perceptions [36]. The poor insight might be related to the alterations of dopaminergic neurocircuits in the hoarding subtype of OCD [37]. The hoarding subtype was also associated with cognitive sequelae, neuropsychological impairments [38], reduced performance-monitoring activity [39], and impaired immediate verbal recall [40]. These factors might be associated with poorer treatment response to CBT.
The most cited article of meta-analysis in OCD also showed that the hoarding subtype would be associated with poor treatment response to traditional treatment, such as behavioral therapy, pharmacotherapy, and combined therapy. However, this study enrolled different continuous parameters, such as the treatment response and changes in the non-YBOCS rating scales. Including different treatment modalities and evaluation, parameters would predispose the results to the heterogeneity status, which would influence the interpretations of the results [41]. Therefore, our study focused on CBT and YBOCS would have the advantage of more homogeneity and less biased results compared to the study. Our study also supported the results of that meta-analysis. The previous meta-analysis with exploratory factor analysis for exposure and ritual prevention response showed that hoarding and UT subtypes would be related to poor treatment response [7]. Another meta-analysis on the error monitoring ability in OCD also suggested that the hoarding subtype would suffer more significant error-related negativity when performing the probabilistic learning tasks. It might suggest that OCD with hoarding symptoms had different pathophysiological mechanisms of error monitoring [42].
In addition, the changes or shifting of the hoarding subtype to another subtype were rare compared to other subtypes. The temporal stability of adult OCD subtypes in the symptom dimension would be stable and could predict the treatment response [1,43]. Even though some studies did not recognize hoarding as a specific subtype of OCD [44,45], the current study results strongly suggested that hoarding would be associated with poorer treatment response to CBT. Another study by Rufer et al. showed that the hoarding subtype would predict non-response to CBT [5]. In addition, the hoarding subtype would be associated with decreased functioning, treatment resistance [46], longer duration of illness, poor insight, and poorer outcomes [8]. A review also supported that the hoarding subtype would be associated with poor treatment response to CBT and serotonin-related antidepressants [19]. The hoarding subtype might be associated with early-onset OCD and alterations in the neurotransmitter system other than serotonin [47]. The poor treatment response to CBT might also be associated with the behaviors of delaying treatment seeking in the hoarding subtype [48].
Even with one study of children and adolescent OCD in the current meta-analysis that might influence the current study’s interpretations, the symptom dimensions of children and adolescent OCD were predominantly congruent with those of adult OCD [49]. In addition, the four-factor system in the current study can be applied to children and adolescents with OCD [50]. Our meta-analysis results also corresponded to the slower rate of improvement in children and adolescents with OCD [31]. The hoarding in children and adolescents with OCD showed that the hoarding subtype might have impairments in social communication, social interest, motivation, and reciprocity [51], which would be related to the poorer response to CBT [7]. However, one study showed that the hoarding subtype would respond better to CBT [30].
The significant limitations in the current study were as follows. First, the low number of enrolled studies in the meta-analysis might limit the interpretations of our results. Therefore, the results should be interpreted with caution. Second, most enrolled studies also suffered from the bias from the concurrent psychotropic medication treatment, such as antidepressants and benzodiazepines. It led to difficulty delineating the medication’s effects on the response of Y-BOCS scores in this meta-analysis. However, the study design of these enrolled studies used CBT as a combined therapy when the OCD subjects had already received medication treatment for a duration. The response effects might still be related to CBT. Third, the mixture of adults, children, and adolescents with different age ranges in the current meta-analysis would make the interpretation of the results biased. Fourth, the duration of CBT and study design of the enrolled studies were also variable. However, the changes in Y-BOCS scores were listed as the full results in the subtype of OCD subjects, not by the randomly assigned CBT methods or duration. Fifth, even hoarding vs. UT and hoarding vs. non-hoarding reached statistically significant in the subtype validation under the basis of CBT response. However, the hoarding vs. contamination or hoarding vs. symmetry was non-significant in the current meta-analysis, which might be related to a limited sample size of symmetry or contamination in current meta-analysis. A future study focused on more solid validation of hoarding vs. symmetry or contamination might be warranted. Sixth, the frequency and number of sessions of CBT might influence the study results. Therefore, this factor might interfere with the interpretations of this meta-analytic study results, and we should take caution regarding the issue of the quantity and quality of CBT. In addition, the heterogeneity of the application of CBT in the enrolled studies was another important limitation. Seventh, the limited number of enrolled studies and the CBT treatment across different ages (adults and children/adolescents) might also limit the interpretations of current meta-analytic results.
From the results of the current study, the hoarding subtype might be the most significant representative subtype of OCD symptom dimension under the impression of unfavorable clinical response to CBT. The treatment of OCD has particularities, and hoarding is a dimension with challenges in clinical practice. However, future studies with more treatment parameters will be warranted to confirm this finding. In addition, the results should be interpreted with caution due to the limited number of enrolled studies in the current meta-analysis.
Funding Statement: National Natural Science Foundation of China (No. 82171542) Beijing Municipal Administration of Hospitals Incubating Program (code: PX2020075) Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (code: XMLX202129).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Besiroglu, L., Uguz, F., Ozbebit, O., Guler, O., Cilli, A. S. et al. (2007). Longitudinal assessment of symptom and subtype categories in obsessive–compulsive disorder. Depression and Anxiety, 24(7), 461–466. DOI 10.1002/(ISSN)1520-6394. [Google Scholar] [CrossRef]
2. Bloch, M. H., Landeros-Weisenberger, A., Rosario, M. C., Pittenger, C., Leckman, J. F. (2008). Meta-analysis of the symptom structure of obsessive-compulsive disorder. American Journal of Psychiatry, 165(12), 1532–1542. DOI 10.1176/appi.ajp.2008.08020320. [Google Scholar] [CrossRef]
3. Brakoulias, V., Starcevic, V., Berle, D., Milicevic, D., Hannan, A. et al. (2014). The relationships between obsessive–compulsive symptom dimensions and cognitions in obsessive–compulsive disorder. Psychiatric Quarterly, 85(2), 133–142. DOI 10.1007/s11126-013-9278-y. [Google Scholar] [CrossRef]
4. Brakoulias, V., Starcevic, V., Martin, A., Berle, D., Milicevic, D. et al. (2016). The familiality of specific symptoms of obsessive-compulsive disorder. Psychiatry Research, 239, 315–319. DOI 10.1016/j.psychres.2016.03.047. [Google Scholar] [CrossRef]
5. Rufer, M., Fricke, S., Moritz, S., Kloss, M., Hand, I. (2006). Symptom dimensions in obsessive–compulsive disorder: Prediction of cognitive-behavior therapy outcome. Acta Psychiatrica Scandinavica, 113(5), 440–446. DOI 10.1111/j.1600-0447.2005.00682.x. [Google Scholar] [CrossRef]
6. Thorsen, A. L., Kvale, G., Hansen, B., van den Heuvel, O. A. (2018). Symptom dimensions in obsessive-compulsive disorder as predictors of neurobiology and treatment response. Current Treatment Options in Psychiatry, 5(1), 182–194. DOI 10.1007/s40501-018-0142-4. [Google Scholar] [CrossRef]
7. Williams, M. T., Farris, S. G., Turkheimer, E. N., Franklin, M. E., Simpson, H. B. et al. (2014). The impact of symptom dimensions on outcome for exposure and ritual prevention therapy in obsessive-compulsive disorder. Journal of Anxiety Disorders, 28(6), 553–558. DOI 10.1016/j.janxdis.2014.06.001. [Google Scholar] [CrossRef]
8. Matsunaga, H., Hayashida, K., Kiriike, N., Maebayashi, K., Stein, D. J. (2010). The clinical utility of symptom dimensions in obsessive–compulsive disorder. Psychiatry Research, 180(1), 25–29. DOI 10.1016/j.psychres.2009.09.005. [Google Scholar] [CrossRef]
9. Alonso, P. (2001). Long-term follow-up and predictors of clinical outcome in obsessive-compulsive patients treated with serotonin reuptake inhibitors and behavioral therapy. The Journal of Clinical Psychiatry, 62(7), 535–540. DOI 10.4088/JCP.v62n07a06. [Google Scholar] [CrossRef]
10. García-Soriano, G., Rufer, M., Delsignore, A., Weidt, S. (2014). Factors associated with non-treatment or delayed treatment seeking in OCD sufferers: A review of the literature. Psychiatry Research, 220(1–2), 1–10. DOI 10.1016/j.psychres.2014.07.009. [Google Scholar] [CrossRef]
11. Williams, M. T., Farris, S. G., Turkheimer, E., Pinto, A., Ozanick, K. et al. (2011). Myth of the pure obsessional type in obsessive–compulsive disorder. Depression and Anxiety, 28(6), 495–500. DOI 10.1002/da.20820. [Google Scholar] [CrossRef]
12. Via, E., Cardoner, N., Pujol, J., Alonso, P., Lopez-Sola, M. et al. (2014). Amygdala activation and symptom dimensions in obsessive–compulsive disorder. The British Journal of Psychiatry, 204(1), 61–68. DOI 10.1192/bjp.bp.112.123364. [Google Scholar] [CrossRef]
13. Göttlich, M., Krämer, U. M., Kordon, A., Hohagen, F., Zurowski, B. (2015). Resting-state connectivity of the amygdala predicts response to cognitive behavioral therapy in obsessive compulsive disorder. Biological Psychology, 111, 100–109. DOI 10.1016/j.biopsycho.2015.09.004. [Google Scholar] [CrossRef]
14. Harrison, B. J., Pujol, J., Soriano-Mas, C., Hernández-Ribas, R., López-Solà, M. et al. (2012). Neural correlates of moral sensitivity in obsessive-compulsive disorder. Archives of General Psychiatry, 69(7), 741–749. DOI 10.1001/archgenpsychiatry.2011.2165. [Google Scholar] [CrossRef]
15. Chase, T., Wetterneck, C. T., Bartsch, R. A., Leonard, R. C., Riemann, B. C. (2015). Investigating treatment outcomes across OCD symptom dimensions in a clinical sample of OCD patients. Cognitive Behaviour Therapy, 44(5), 365–376. DOI 10.1080/16506073.2015.1015162. [Google Scholar] [CrossRef]
16. Abramowitz, J. S., Franklin, M. E., Schwartz, S. A., Furr, J. M. (2003). Symptom presentation and outcome of cognitive-behavioral therapy for obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology, 71(6), 1049–1057. DOI 10.1037/0022-006X.71.6.1049. [Google Scholar] [CrossRef]
17. Black, D. W., Monahan, P., Gable, J., Blum, N., Clancy, G. et al. (1998). Hoarding and treatment response in 38 nondepressed subjects with obsessive-compulsive disorder. Journal of Clinical Psychiatry, 59(8), 420–425. DOI 10.4088/JCP.v59n0804. [Google Scholar] [CrossRef]
18. Mataix-Cols, D., Marks, I. M., Greist, J. H., Kobak, K. A., Baer, L. (2002). Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: Results from a controlled trial. Psychotherapy and Psychosomatics, 71(5), 255–262. DOI 10.1159/000064812. [Google Scholar] [CrossRef]
19. Starcevic, V., Brakoulias, V. (2008). Symptom subtypes of obsessive–compulsive disorder: Are they relevant for treatment? Australian & New Zealand Journal of Psychiatry, 42(8), 651–661. DOI 10.1080/00048670802203442. [Google Scholar] [CrossRef]
20. Knobloch, K., Yoon, U., Vogt, P. M. (2011). Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. Journal of Cranio-Maxillofacial Surgery, 39(2), 91–92. DOI 10.1016/j.jcms.2010.11.001. [Google Scholar] [CrossRef]
21. Ball, S. G., Baer, L., Otto, M. W. (1996). Symptom subtypes of obsessive-compulsive disorder in behavioral treatment studies: A quantitative review. Behaviour Research and Therapy, 34(1), 47–51. DOI 10.1016/0005-7967(95)00047-2. [Google Scholar] [CrossRef]
22. Grant, J. E., Mancebo, M. C., Pinto, A., Williams, K. A., Eisen, J. L. et al. (2007). Late-onset obsessive compulsive disorder: Clinical characteristics and psychiatric comorbidity. Psychiatry Research, 152(1), 21–27. DOI 10.1016/j.psychres.2006.09.015. [Google Scholar] [CrossRef]
23. Keeley, M. L., Storch, E. A., Merlo, L. J., Geffken, G. R. (2008). Clinical predictors of response to cognitive-behavioral therapy for obsessive–compulsive disorder. Clinical Psychology Review, 28(1), 118–130. DOI 10.1016/j.cpr.2007.04.003. [Google Scholar] [CrossRef]
24. Storch, E. A., Merlo, L. J., Larson, M. J., Bloss, C. S., Geffken, G. R. et al. (2008). Symptom dimensions and cognitive-behavioural therapy outcome for pediatric obsessive-compulsive disorder. Acta Psychiatrica Scandinavica, 117(1), 67–75. [Google Scholar]
25. Matsunaga, H., Nagata, T., Hayashida, K., Ohya, K., Kiriike, N. et al. (2009). A Long-term trial of the effectiveness and safety of atypical antipsychotic agents in augmenting SSRI-refractory obsessive-compulsive disorder. Journal of Clinical Psychiatry, 70(6), 863. DOI 10.4088/JCP.08m04369. [Google Scholar] [CrossRef]
26. Koprivova, J., Kudrnovska, H., Latalova, K., Vyskocilova, J. (2009). Predicting the therapeutic response to cognitive behavioural therapy in patients with pharmacoresistant obsessive-compulsive disorder. Neuroendocrinology Letters, 30(5), 615–623. [Google Scholar]
27. Salomoni, G., Grassi, M., Mosini, P., Riva, P., Cavedini, P. et al. (2009). Artificial neural network model for the prediction of obsessive-compulsive disorder treatment response. Journal of Clinical Psychopharmacology, 29(4), 343–349. DOI 10.1097/JCP.0b013e3181aba68f. [Google Scholar] [CrossRef]
28. Matsunaga, H., Hayashida, K., Kiriike, N., Nagata, T., Stein, D. J. (2010). Clinical features and treatment characteristics of compulsive hoarding in Japanese patients with obsessive-compulsive disorder. CNS Spectrums, 15(4), 258–266. DOI 10.1017/S1092852900000092. [Google Scholar] [CrossRef]
29. Nakatani, E., Krebs, G., Micali, N., Turner, C., Heyman, I. et al. (2011). Children with very early onset obsessive-compulsive disorder: Clinical features and treatment outcome. Journal of Child Psychology and Psychiatry, 52(12), 1261–1268. DOI 10.1111/j.1469-7610.2011.02434.x. [Google Scholar] [CrossRef]
30. Højgaard, D. R., Hybel, K. A., Mortensen, E. L., Ivarsson, T., Nissen, J. B. et al. (2018). Obsessive-compulsive symptom dimensions: Association with comorbidity profiles and cognitive-behavioral therapy outcome in pediatric obsessive-compulsive disorder. Psychiatry Research, 270, 317–323. DOI 10.1016/j.psychres.2018.09.054. [Google Scholar] [CrossRef]
31. McGuire, J. F., Tan, P. Z., Piacentini, J. (2019). Symptom dimension response in children and adolescents with obsessive-compulsive disorder. Journal of Clinical Child & Adolescent Psychology, 48(3), 529–538. DOI 10.1080/15374416.2018.1540009. [Google Scholar] [CrossRef]
32. Alonso, P., Menchón, J. M., Mataix-Cols, D., Pifarré, J., Urretavizcaya, M. et al. (2004). Perceived parental rearing style in obsessive–compulsive disorder: Relation to symptom dimensions. Psychiatry Research, 127(3), 267–278. DOI 10.1016/j.psychres.2001.12.002. [Google Scholar] [CrossRef]
33. Mataix-Cols, D., do Rosario-Campos, M. C., Leckman, J. F. (2005). A multidimensional model of obsessive-compulsive disorder. American Journal of Psychiatry, 162(2), 228–238. DOI 10.1176/appi.ajp.162.2.228. [Google Scholar] [CrossRef]
34. Kashyap, H., Fontenelle, L. F., Miguel, E. C., Ferrão, Y. A., Torres, A. R. et al. (2012). ‘Impulsive compulsivity’ in obsessive-compulsive disorder: A phenotypic marker of patients with poor clinical outcome. Journal of Psychiatric Research, 46(9), 1146–1152. DOI 10.1016/j.jpsychires.2012.04.022. [Google Scholar] [CrossRef]
35. Torres, A. R., Fontenelle, L. F., Ferrão, Y. A., do Rosário, M. C., Torresan, R. C. et al. (2012). Clinical features of obsessive-compulsive disorder with hoarding symptoms: A multicenter study. Journal of Psychiatric Research, 46(6), 724–732. DOI 10.1016/j.jpsychires.2012.03.005. [Google Scholar] [CrossRef]
36. Nissen, J. B., Parner, E. (2018). The importance of insight, avoidance behavior, not-just-right perception and personality traits in pediatric obsessive-compulsive disorder (OCDA naturalistic clinical study. Nordic Journal of Psychiatry, 72(7), 489–496. DOI 10.1080/08039488.2018.1486454. [Google Scholar] [CrossRef]
37. de Avila, R. C. S., do Nascimento, L. G., Porto, R. L. D. M., Fontenelle, L., Brakoulias, V. et al. (2019). Level of insight in patients with obsessive–compulsive disorder: An exploratory comparative study between patients with “good insight” and “poor insight”. Frontiers in Psychiatry, 10, 413. DOI 10.3389/fpsyt.2019.00413. [Google Scholar] [CrossRef]
38. McGuire, J. F., Crawford, E. A., Park, J. M., Storch, E. A., Murphy, T. K. et al. (2014). Neuropsychological performance across symptom dimensions in pediatric obsessive compulsive disorder. Depression and Anxiety, 31(12), 988–996. DOI 10.1002/da.22241. [Google Scholar] [CrossRef]
39. Riesel, A., Kathmann, N., Endrass, T. (2014). Overactive performance monitoring in obsessive–compulsive disorder is independent of symptom expression. European Archives of Psychiatry and Clinical Neuroscience, 264(8), 707–717. DOI 10.1007/s00406-014-0499-3. [Google Scholar] [CrossRef]
40. Kashyap, H., Kumar, J. K., Kandavel, T., Reddy, Y. J. (2017). Relationships between neuropsychological variables and factor-analysed symptom dimensions in obsessive compulsive disorder. Psychiatry Research, 249, 58–64. DOI 10.1016/j.psychres.2016.12.044. [Google Scholar] [CrossRef]
41. Bloch, M. H., Bartley, C. A., Zipperer, L., Jakubovski, E., Landeros-Weisenberger, A. et al. (2014). Meta-analysis: Hoarding symptoms associated with poor treatment outcome in obsessive–compulsive disorder. Molecular Psychiatry, 19(9), 1025–1030. DOI 10.1038/mp.2014.50. [Google Scholar] [CrossRef]
42. Mathews, C. A., Perez, V. B., Delucchi, K. L., Mathalon, D. H. (2012). Error-related negativity in individuals with obsessive–compulsive symptoms: Toward an understanding of hoarding behaviors. Biological Psychology, 89(2), 487–494. DOI 10.1016/j.biopsycho.2011.12.018. [Google Scholar] [CrossRef]
43. Rufer, M., Grothusen, A., Maß, R., Peter, H., Hand, I. (2005). Temporal stability of symptom dimensions in adult patients with obsessive–compulsive disorder. Journal of Affective Disorders, 88(1), 99–102. DOI 10.1016/j.jad.2005.06.003. [Google Scholar] [CrossRef]
44. Wu, K. D., Watson, D. (2005). Hoarding and its relation to obsessive–compulsive disorder. Behaviour Research and Therapy, 43(7), 897–921. DOI 10.1016/j.brat.2004.06.013. [Google Scholar] [CrossRef]
45. Abramowitz, J. S., Wheaton, M. G., Storch, E. A. (2008). The status of hoarding as a symptom of obsessive–compulsive disorder. Behaviour Research and Therapy, 46(9), 1026–1033. DOI 10.1016/j.brat.2008.05.006. [Google Scholar] [CrossRef]
46. Matsunaga, H., Maebayashi, K., Hayashida, K., Okino, K., Matsui, T. et al. (2008). Symptom structure in Japanese patients with obsessive-compulsive disorder. American Journal of Psychiatry, 165(2), 251–253. DOI 10.1176/appi.ajp.2007.07020340. [Google Scholar] [CrossRef]
47. Stein, D. J., Carey, P. D., Lochner, C., Seedat, S., Fineberg, N. et al. (2008). Escitalopram in obsessive-compulsive disorder: Response of symptom dimensions to pharmacotherapy. CNS Spectrums, 13(6), 492–498. DOI 10.1017/S1092852900016722. [Google Scholar] [CrossRef]
48. Demet, M. M., Deveci, A., Taşkın, E. O., Dündar, P. E., Ermertcan, A. T. et al. (2010). Risk factors for delaying treatment seeking in obsessive-compulsive disorder. Comprehensive Psychiatry, 51(5), 480–485. DOI 10.1016/j.comppsych.2010.02.008. [Google Scholar] [CrossRef]
49. Stewart, S. E., Rosario, M. C., Brown, T. A., Carter, A. S., Leckman, J. F. et al. (2007). Principal components analysis of obsessive–compulsive disorder symptoms in children and adolescents. Biological Psychiatry, 61(3), 285–291. DOI 10.1016/j.biopsych.2006.08.040. [Google Scholar] [CrossRef]
50. Stewart, S. E., Rosario, M. C., Baer, L., Carter, A. S., Brown, T. A. et al. (2008). Four-factor structure of obsessive-compulsive disorder symptoms in children, adolescents, and adults. Journal of the American Academy of Child & Adolescent Psychiatry, 47(7), 763–772. DOI 10.1097/CHI.0b013e318172ef1e. [Google Scholar] [CrossRef]
51. Samuels, J., Grados, M. A., Riddle, M. A., Bienvenu, O. J., Goes, F. S. et al. (2014). Hoarding in children and adolescents with obsessive–compulsive disorder. Journal of Obsessive-Compulsive and Related Disorders, 3(4), 325–331. DOI 10.1016/j.jocrd.2014.08.001. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools