 | International Journal of Mental Health Promotion | 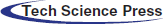 |
DOI: 10.32604/ijmhp.2022.020556
ARTICLE
Psychological and Emotional Responses during Different Stages of the COVID-19 Pandemic Based on a Survey of a Mental Health Hotline
1Department of Psychology, Guangzhou University, Guangzhou, 510006, China
2Department of Psychology, University of Edinburgh, Edinburgh, EH8 9JZ, UK
3Division of Histology and Embryology, Key Laboratory for Regenerative Medicine of the Ministry of Education, Medical College, Jinan University, Guangzhou, 510632, China
*Corresponding Authors: Hong Zeng. Email: zhh0791@163.com; Xuesong Yang. Email: yang_xuesong@126.com
Received: 07 December 2021; Accepted: 28 January 2022
Abstract: Background: The coronavirus (COVID-19) outbreak in 2019 triggered psychological and emotional responses. This research investigates the psychological status and emotional problems of those who sought psychological assistance during the epidemic period by calling a mental health hotline. Methods: This study aims to combine qualitative and quantitative research. Descriptive analysis was used for undertaking qualitative research. We analyzed the data from group 1 (n = 706), in which the people used the mental health hotline from 25 January 2020 to 23 June 2020. A self-designed questionnaire was developed in accordance with the classification and summarized items from group 1’s psychological problems and emotional status. To implement the quantitative research, we conducted a cross-sectional descriptive survey and used the self-compiled scale and HADS to investigate group 2 (n = 553) from May 2020 to June 2020. Results: Descriptive statistics and comparative analysis revealed that: ① Visitors mainly reported behavior, emotional, family relationship problems and sleep disorders. ② Anxiety, comorbidities, sleep disorders and coping problems were the most frequently reported problems. ③ There were significant differences in the number of visitors experiencing various problems or exhibiting harmful behaviors (sorrow, worry, fear, depression, sleep disorders, self-harm or suicide, and coping problems, anxiety, hypochondria, and comorbidity) in the four stages of the epidemic. ④ More than a quarter of participants still suffered from anxiety or depression in the later stages of the epidemic. Conclusion: Different problems manifested at different stages of the epidemic, and psychological interventions and assistance should be tailored to reflect this.
Keywords: COVID-19; comorbidities; different stages; psychological intervention
An outbreak of coronavirus disease 2019 (COVID-19) swiftly spread across the world in early 2020. Although most of the people infected with COVID-19 have mild symptoms or are asymptomatic, some patients have had serious complications and many have died. Specific medication or vaccines have not yet been developed for the early stages of the epidemic [1,2]. The World Health Organization (WHO) received the first report about a small cluster of pneumonia cases with unknown etiology in Wuhan, Hubei Province, China on December 31, 2019. COVID-19 spread to several other countries in southern and Eastern Asia by the middle of January [3]. On January 23 2020, a modern form of quarantine (i.e., shutting down all transportation in and out of Wuhan) was imposed by the Chinese government to control the spread of the COVID-19 virus. The policy was expanded to twelve other cities in Hubei Province [4]. On March 11, 2020, WHO officially declared the outbreak of COVID-19 a pandemic [5]. This work explores the mental health status of inhabitants of China during the COVID-19 pandemic.
COVID-19 is the third global viral epidemic of this century. The previous two were Severe Acute Respiratory Syndrome (SARS), which broke out in 2003 and Middle East Respiratory Syndrome (MERS), which followed in 2012. The SARS epidemic brought great psychological pressure to the public, leading to significantly decreased mental health status [6]. SARS patients were prone to anxiety, fear, loneliness, boredom, anger, etc. [7]. Health care workers involved with the MERS virus were at a high risk of developing Post Traumatic Stress Disorder (PTSD), especially after experiencing home quarantine, with an increased risk of sleep-related and numbness symptoms [8]. Compared with SARS and MERS, COVID-19 is characterized by faster and wider spread, higher incidence of infection and higher mortality [9], which has prompted countries to adopt more rigorous measures to prevent the spread of the epidemic. Thus, there may be a greater impact on public health. It is reasonable that people felt stress during a pandemic. Emotional responses, such as anxiety and fear, could be triggered.
During the COVID-19 pandemic, people have been afraid of being infected, which may cause anxiety. Social loss caused by long periods of isolation that may lead to feelings of loneliness and depression. In addition, excessive attention to unreliable or negative information reported by the media is likely to trigger emotions such as panic and anxiety [10]. The incidence of depression, anxiety, and PTSD is significantly higher than during previous epidemics [11]. More than 70% of Chinese citizens have moderate or higher psychological symptoms [12]. Temperament is an important predictor of both suicide risk and psychopathology [13]. COVID-19 can increase the level of depression, anxiety, stress, and pain in patients with mood disorders [14]. The general population is also at a high risk of psychological problems [15].
The mental health hotline was opened by the Psychological Crisis Intervention Professional Committee of Guangdong Mental Health Association during the COVID-19 epidemic. Psychological and mental health practitioners were recruited to provide public welfare interventions for psychological crises. The goal of the health hotline is to provide emergency psychological assistance to alleviate the discomfort of the epidemic. The hotline was opened in January and continued until mid-August. As the pandemic developed, kinds of problems reported to the hotline were different, suggesting that people’s psychological problems change as the pandemic changes.
Although it is only 17 years since the SARS outbreak in 2003, the country’s inhabitants widely viewed COVID-19 as a novel event. The speed of its spread contributed to the widespread perception that it was strong, and this obviously acted to the detriment of public mental health. It should also be remembered that COVID-19 broke out in the Spring Festival, at a time when thousands of families were reuniting. Its subsequent spread to the whole country and the world had a lasting impact on public mental health.
In spatial terms, it has profoundly impacted different groups in different areas. In parts of the country with serious epidemics, travel restrictions will be adjusted at any time, and it will be necessary to consider epidemic management measures in different areas at any time. These features of COVID-19 are fully consistent with the novelty, destructiveness and criticality of Event System Theory (EST), which provides particular insight into the intensity of the event [16]. It explains the main effect of the event intensity on the individual. When event intensity is greater, it is more novel, destructive and critical, and can cause the individual to focus on the event and change their characteristics and behavior, in addition to stimulating new events. COVID-19’s high novelty, destructive character and critical and obvious characteristics can create uncertainty, a concern about infection and a fear of its implications for life and work, and this can cause individual emotional and cognitive reactions. When an individual is faced with an event or situational feature, some cognitive-emotional units are activated, and this can result in a specific interaction, which triggers the individual’s cognition, emotions and behavior, resulting in the alienation of the event situation. EST establishes that the epidemic situation strongly commands popular attention [17], breaks established routine life trajectories and habits and even alter the individual’s automatic cognitive process [18], resulting in changes in psychological and emotional problems. This study investigated the main psychological problems of visitors in different periods during the epidemic, and conducted a questionnaire survey that addressed the psychological and emotional responses of the general population; in doing so, it gained an improved understanding of the general population’s mental health status during the epidemic, and was able to use EST to discuss psychological and emotional problems encountered at different stages, and this enabled it to provide references for psychological intervention and prevention. The study hypothesized that as the epidemic improves, the public’s psychological and emotional problems decrease. But can all the problems be solved? Some problems may have deeper roots and may not necessarily improve quickly as the pandemic abates.
2.1 Study Design and Participants
This study aims to combine qualitative and quantitative research to explore people’s psychological status and emotional state during the epidemic, and provide effective information that can be used for psychological crisis intervention in the future. In qualitative research, the data from group 1 (n = 706), in which the participants used the mental health hotline from 25 January 2020 to 23 June 2020, were analyzed. A self-designed questionnaire was designed according to the classifiably summarized items from group 1’s psychological problems and emotional status. In quantitative research, a cross-sectional descriptive survey was carried out, and the self-compiled scale and HADS were used to investigate group 2 (n = 553) from May 2020 to June 2020.
As of June 23, the hotline had been in place for more than five months. For this study, the pandemic was divided into four stages: (1) stage 1, from January 25 (mental health hotline started to work) to February 18 (outbreak of infection); (2) stage 2, from February 19 to March 18 (almost no domestic cases); (3) stage 3, from March 19 to April 08 (lifting lockdown in Wuhan, China); (4) and stage 4, from April 09 to June 23 (ending hotline investigation).
2.2.1 A Self-Compiled Questionnaire
The questionnaire’s demographic information included identity status, age, gender, education level, city, marital status, physical status, etc. There were questions on anxiety (Do you feel anxious or worry about yourself or your family during the epidemic?), depression (Is it easy for you to get down, depressed, cry, and feel desperate during the epidemic?), fear (Do you feel fear that you do not know when the epidemic will end?), and so on. Except for the question of family relations (1 = much worse than before; 2 = worse than before; 3 = about the same as before; 4 = better than before; 5 = much better than before), all questions were scored with 5 as the highest (1 = none; 2 = few; 3 = sometimes; 4 = often; 5 = always).
2.2.2 Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS) is mainly used to assess anxiety and depression in hospital patients. It was created by Zigmond and Snaith in 1983 [19], and consists of 14 items, including seven for depression and seven for anxiety. The scores for anxiety and depression were classified as 0~7 asymptomatic, 8~10 suspicious, and 11~21 positive. The scale produced an acceptable Cronbach’s alpha score of 0.843 for the current sample.
2.3.1 Collected the Main Complaint of the Visitors (Group 1)
The information on mental health was collected via a mental health hotline. The hotline used Wechat (using the instant messaging software developed by Tencent) and the telephone to provide psychological assistance. Each visitor from the mental health hotline was required to sign the informed consent form, in which they agreed to recordings of the consultation process for research purposes, and they also agreed to provide the information including age, gender and region, as well as their major psychological problems. Before implementing the survey, researchers were trained and participants were informed that the relevant material would be kept confidential.
2.3.2 Produced the Themes for Mental Problems Experienced by Visitors (Group 1)
Descriptive analysis was used for editing, sorting and coding the main complaint, and then, form the main items of psychological and emotional problems experienced by group 1.
2.3.3 Designed a Self-Compiled Questionnaire
The main items of psychological and emotional problems collected from the mental health hotline, was used to design a self-compiled questionnaire.
2.3.4 Distributed Online Questionnaires to the General Public
The self-compiled questionnaire and HADS were distributed to the general public (group 2) on line via So jump, a service provider engaged in online questionnaire. All the subjects who participated in the questionnaire signed the informed consent form online, and agreed we could use data from the questionnaire they provided.
The data analysis used Microsoft Excel 2016 and IBM SPSS Statistics version 22.0. Microsoft Excel was used for editing, sorting, and coding the visitors’ main complaint from group 1. The Excel file was then imported into SPSS. Descriptive statistics (frequencies, percentages, means, standard deviation) and some first-order analyses (chi-square tests, reliability test, correlation analysis, etc.) were executed with SPSS. We define statistical significance for our purposes as effects at P < 0.05.
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Guangzhou University.
3.1 Psychological and Emotional Responses to the COVID-19 Pandemic from Those Seeking Help from a Mental Health Hotline
Descriptive analysis was used to get the content of Table 1. The themes were produced by analyzing the questionnaire, in which all the participants (i.e., the hotline callers) in group 1 need to answer, and they also provided their own report about the main problems. Before receiving psychological assistance, participants in group 1 were required to complete a simple questionnaire and report their main problems, which were about their psychological problems and emotional status. And then, we completed the coding and classification according to the items of the questionnaires. The participant’s reports were adopted to get the questions presented in Table 1.
In addition to the classification above, visitors with a history of mental illness were also included to explore the relationship between variables.
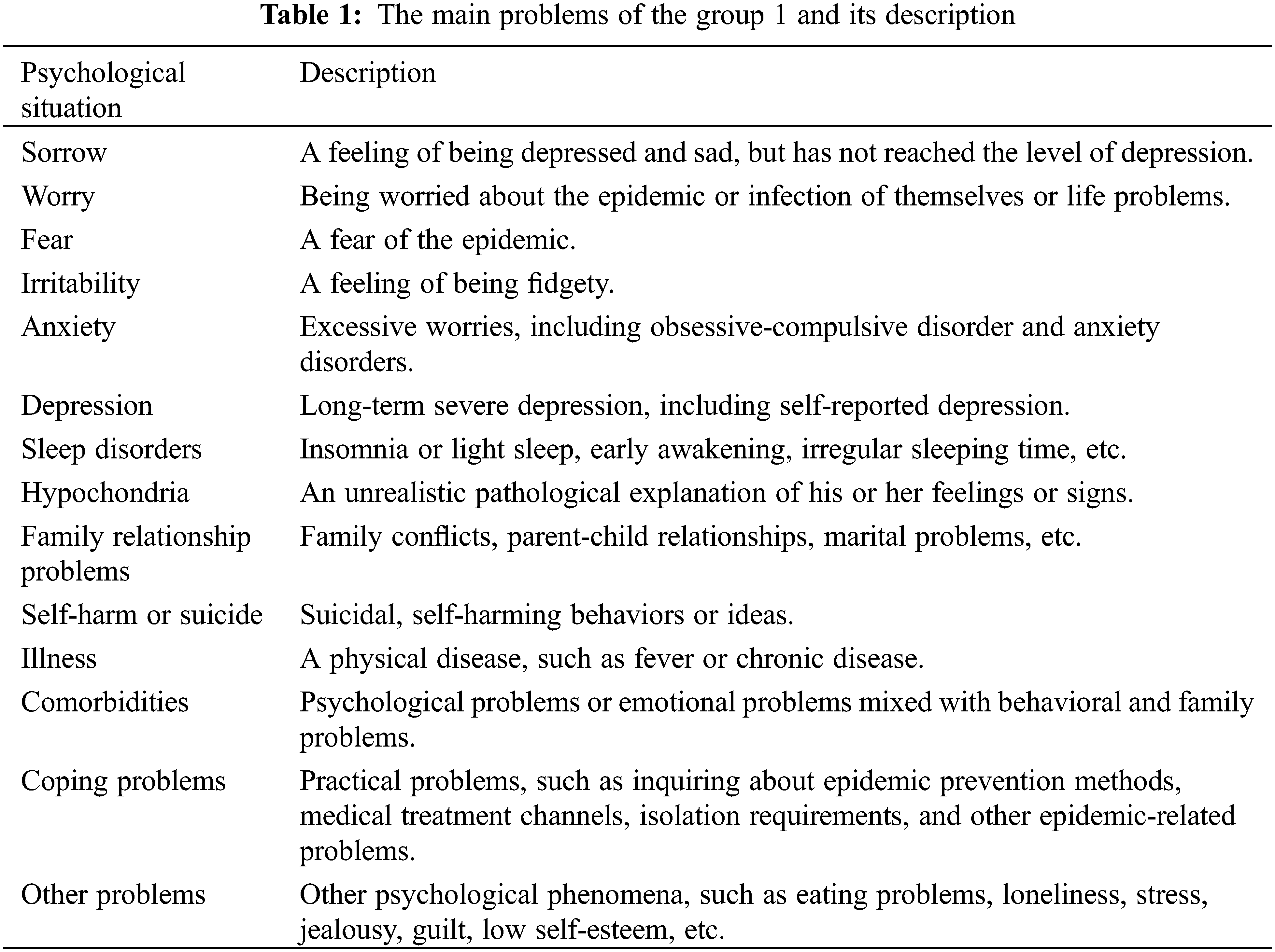
From January 25 to June 23 2020, 706 people (group 1) sought psychological assistance. From May to June 2020, 553 people (group 2) were investigated. In group 2, a total of 632 questionnaires were collected and 79 unqualified questionnaires were excluded, resulting in an effective recovery rate of 87.5%. Incomplete questionnaires were excluded, and so were those that included answers of less than 60 s, incorrect responses to the lie detection question (please answer “yes” to this question) and the ones that featured consistent answers. Their demographic characteristics are shown in Table 2.
3.3 Psychological and Emotional Responses
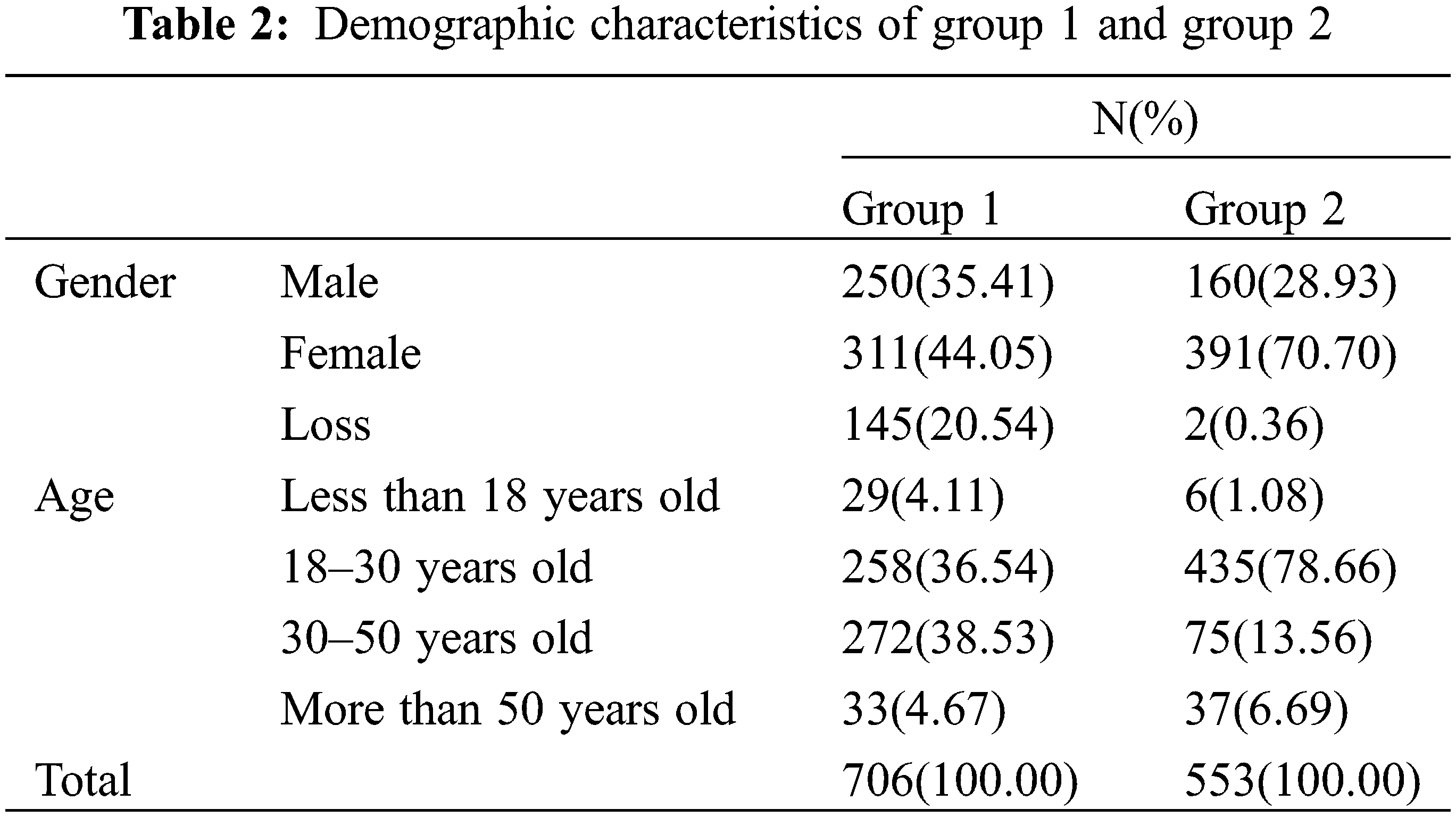
As shown in Table 3, the main problems reported are emotional problems, sleep disorders, and family relationship problems. In group 1, comorbidities (25.50%), sleep disorders (19.69%), anxiety (19.12%), coping problems (17.99%), fear (13.03%), other problems (12.89%) and depression (11.19%) were more frequently reported in group 1.
In group 2, it was found that irritability, anxiety, other problems, and sleep disorders were more serious during the epidemic. 90 people (16.27%) felt irritable, because of self-isolation, 79 people (14.28%) felt anxious and worried about themselves or their families, and 61 people (11.03%) have had other problems such as trouble concentrating, 52 people (9.40%) had comorbidities and 37 people (6.69%) had difficulty falling asleep or had decreased sleep quality (including nightmares, dreaming, talking in sleep, sleepwalking, etc.). The results showed that people still felt anxiety and more irritable when the epidemic slowed down.
3.4 Analysis of Problems in Four Stages of the Epidemic in Group 1
The main problems reported to the hotline were emotional comorbidities, anxiety, and sleep disorders. Different problems were reported during different stages of the pandemic. Comorbidities, anxiety, and sleep disorders were the major problems during the first two stages (January 25 to March 18). The proportion of coping problems increased during the last two stages of the epidemic (March 19 to June 23), and became the main reason for seeking assistance (Fig. 1). Comorbidities were the largest category in all stages of the epidemic. Anxiety and sleep disorders were also top problems in all four stages.
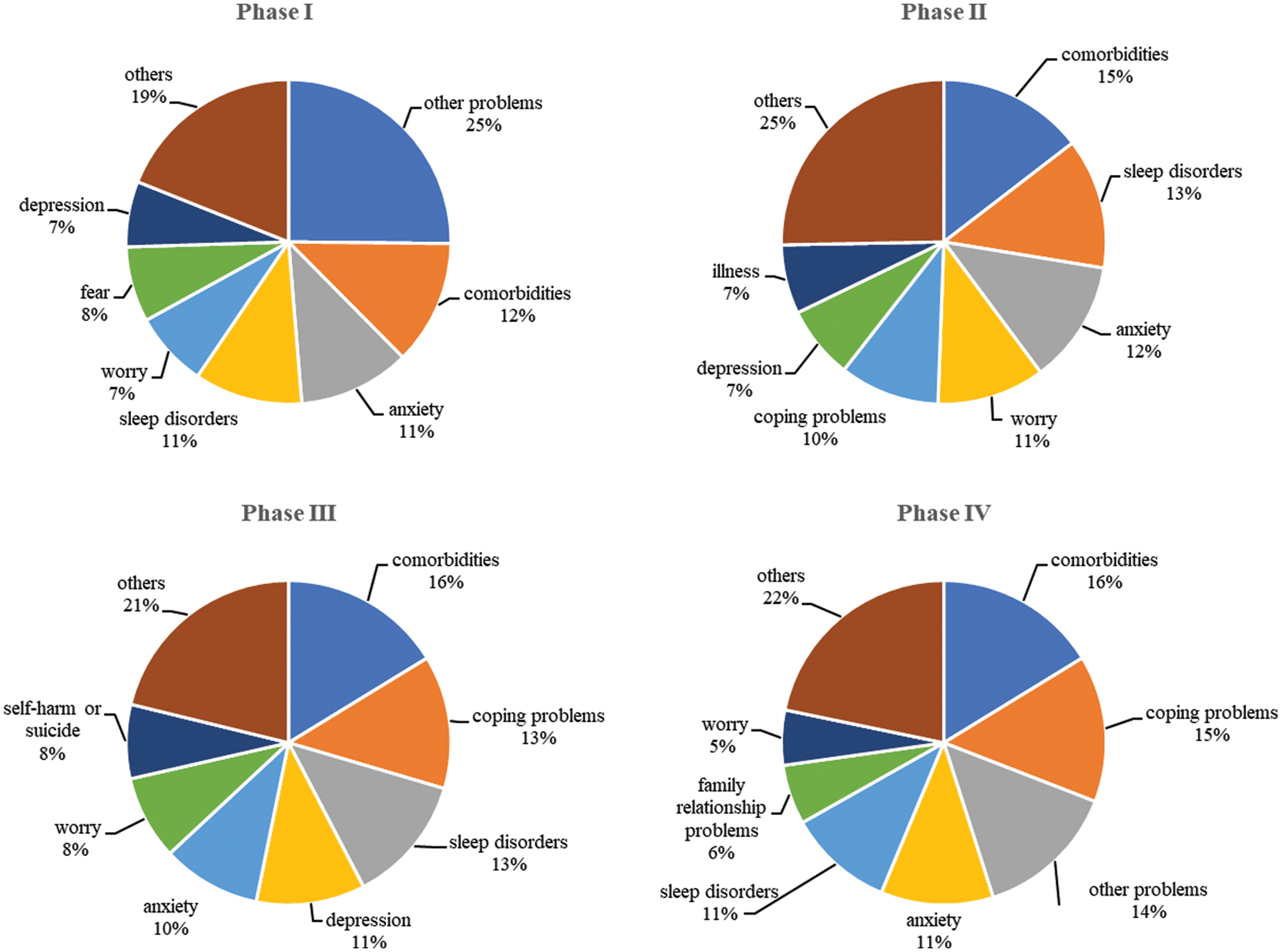
Figure 1: Analysis of problems in four stages of the epidemic
Categories were analyzed using a χ2 test, which found varying psychological statuses in different stages of the epidemic. Table 4 shows no significant difference in irritability and history of mental illness among help-seekers. There were significant differences, however, in the number of people who reported sadness, worry, fear, depression, sleep disorders, self-harm or suicide, coping problems (P = 0.00), anxiety, hypochondria (P = 0.02) and comorbidities (P = 0.03) in the four stages of the epidemic. Visitors reporting family relationship problems (P = 0.07) have marginally-significant differences in the four stages of the epidemic. The Least Significant Difference (LSD) method is used to compare psychological status in four stages. The results are shown in Table 4. As shown in Fig. 2, different emotions show different trends over time.
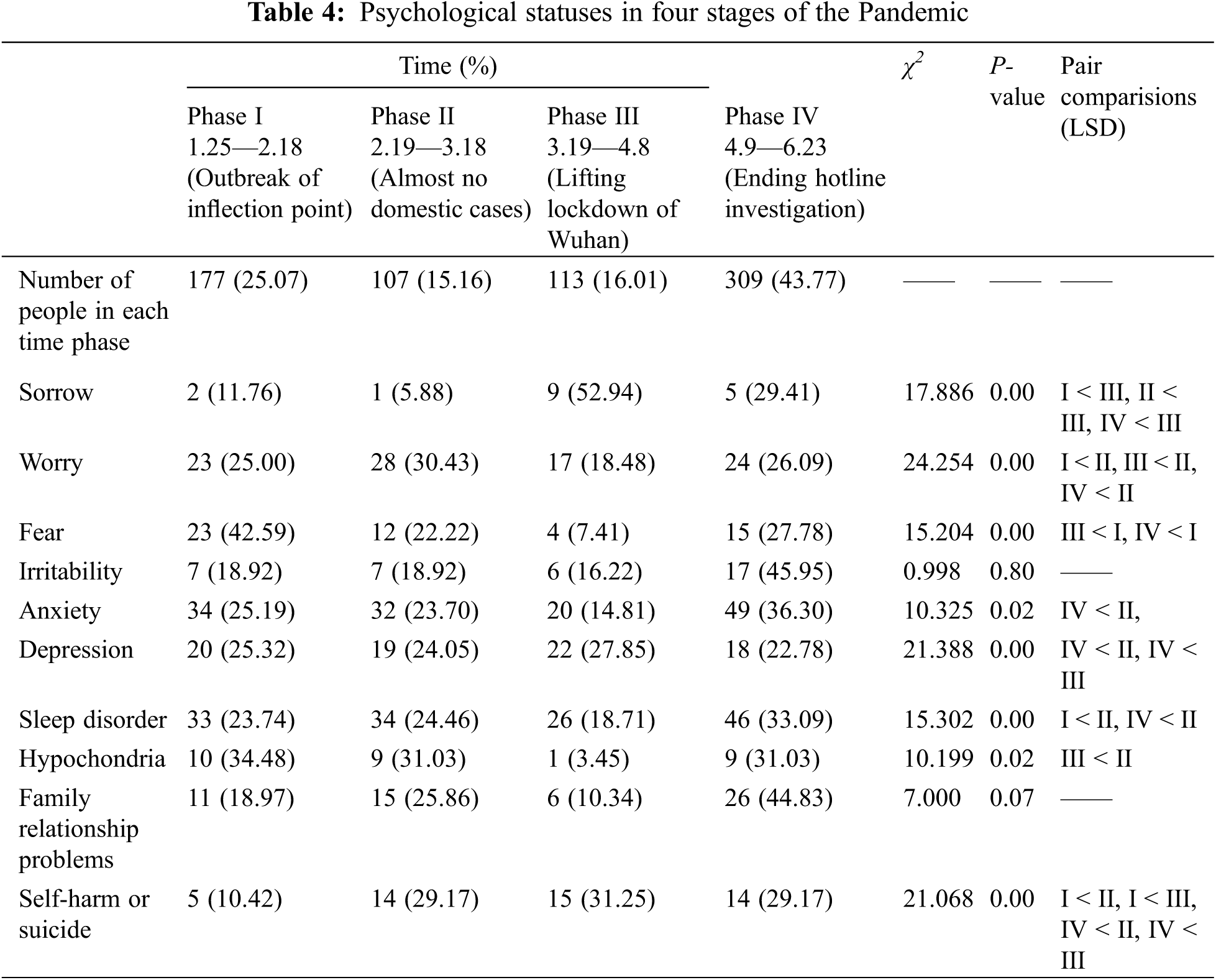
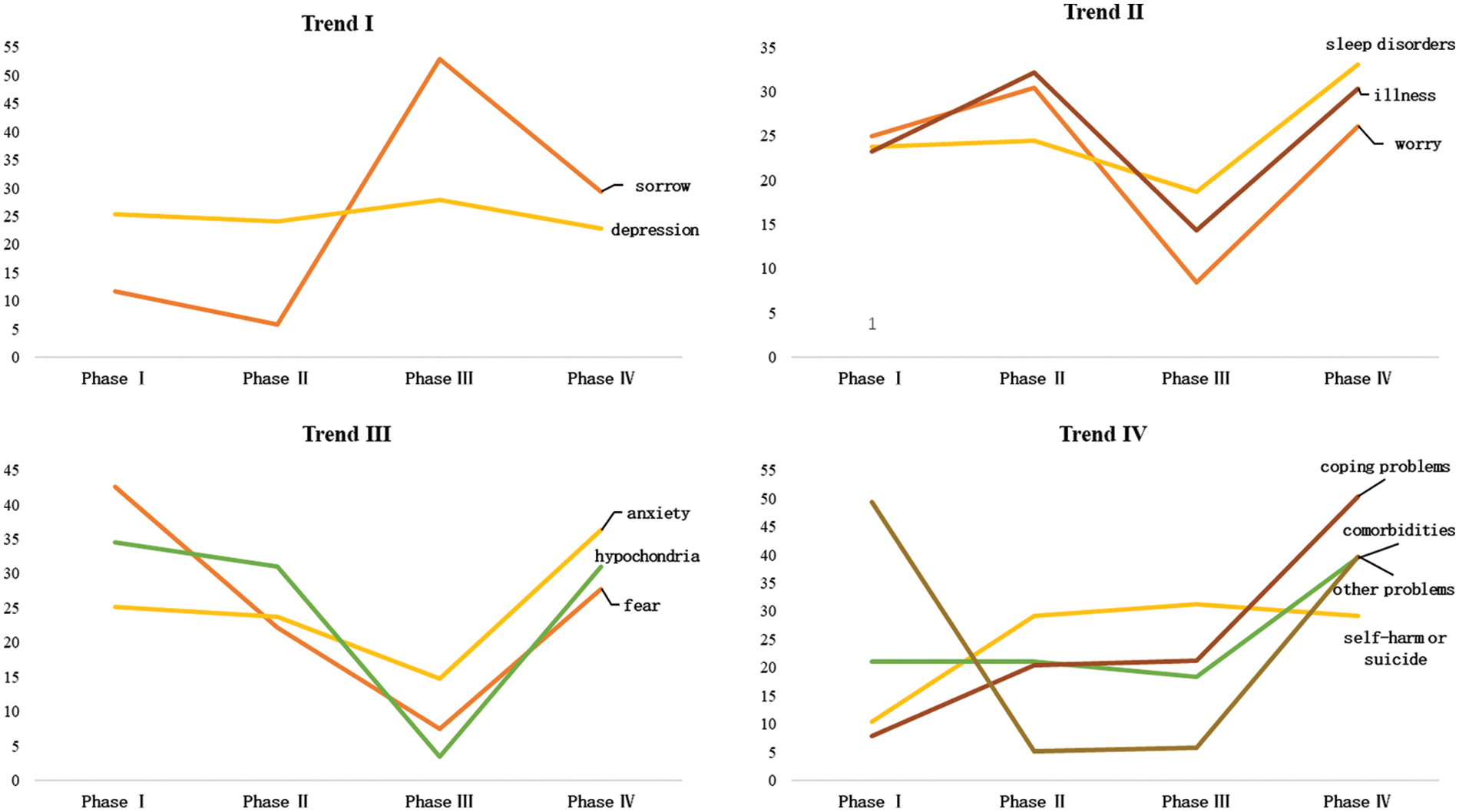
Figure 2: Change trend in visitor problems over the four stages of the epidemic
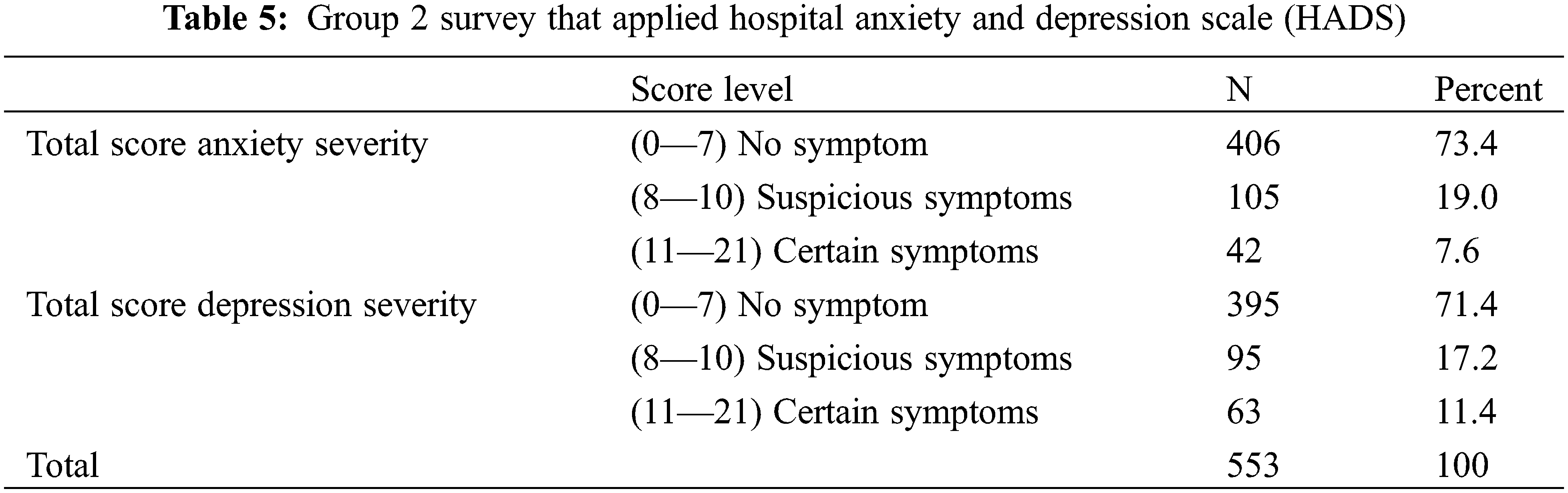
3.5 Comparison of Anxiety and Depression in Group 2
HADS results showed that the score of anxiety subscale was 5.37 ± 3.44, and the score of depression subscale was 5.29 ± 3.77 in group 2. Four hundred six people (73.4%) did not have anxiety symptoms, 105 people (19%) had possible anxiety symptoms, and 42 people (7.6%) show showed affirmative anxiety symptoms. Three hundred ninety-five people (71.4%) did not show depressive symptoms, 95 people (17.2%) had possible depressive symptoms, and 63 people (11.4%) showed affirmative depressive symptoms. The results showed that in the late stages of the epidemic, more than 25% of the general public was still affected by anxiety or depressive symptoms (Table 5).
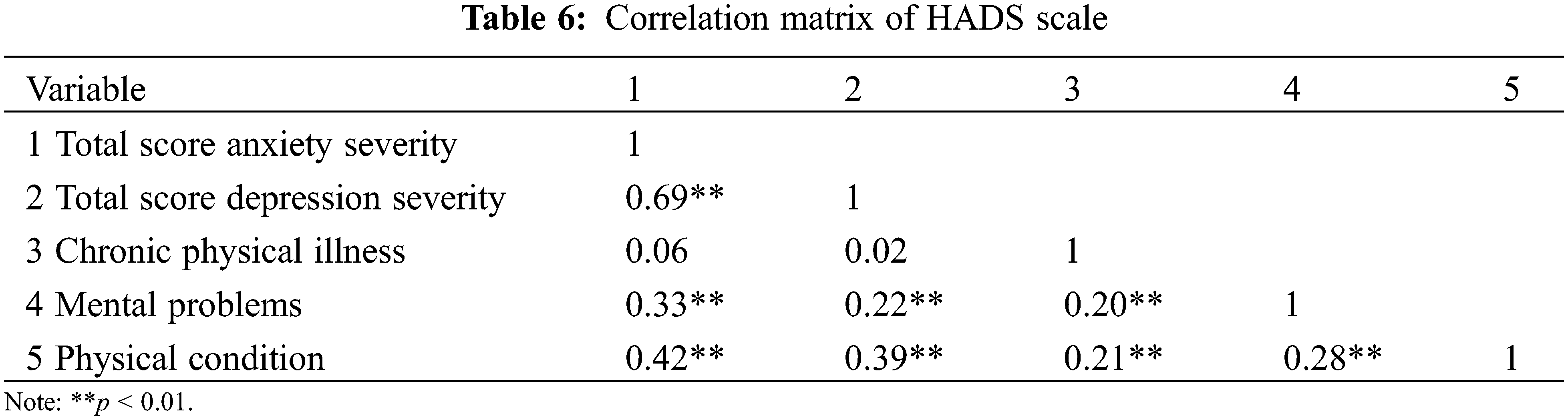
3.6 Correlation Analysis of HADS Scale in Group 2
The correlations between the two subscales of HADS and the history of chronic physical diseases, psychological problems, and physical conditions were analyzed. The results showed no correlation between the total scores of the two subscales and the history of chronic physical disease; however, the scores of the two subscales have a significant positive correlation with psychological problems and the current physical condition. The history of chronic physical disease and physical condition have positive correlation with psychological problems. The details are shown in Table 6.
Due to the uncertainty of the early stage of the epidemic, psychological stress was widespread. A series of emotional, behavioral, and physiological stress responses are generated when people are confronted with a crisis [20]. During this epidemic, negative emotions such as anxiety, anger, and panic led to varying degrees of psychological problems. Some studies demonstrated that as disasters unfold, psychological behavior changes with different phases of the disaster [21]. Visitors seeking psychological assistance through hotline showed this same trend. In each stage of the epidemic, comorbidities ranked first or second in problems reported, indicating that the problems of individuals are complex. Psychological problems often appeared together with emotional problems or behavioral and family problems [22]. Li and coworkers [22] analyzed the word frequency characteristics of posts from active users on Weibo through ecological identification. It was shown that after the outbreak of COVID-19, negative emotions, such as anxiety and anger, overall increased in society, happiness decreased, and sensitivity to social risks increased. At the same time, stress during a crisis disturbs the autonomic nervous and neuroendocrine system, resulting in negatively emotional experience [23]. Individuals experience distinct development stages and have various needs at these different stages. The specific propositions of EST describe how events become impactful and the spatial and temporal processes relating to outcomes. Events are dynamic and evolutionary. That is, as they unfold and interact with circumstances and entities upon their inception, events may become more or less novel, disruptive, and critical. As a result, the overall strength of events can change over time [16].
At the beginning of the epidemic (January 28–February 18), comorbidity, anxiety, sleep disorders, worry, fear, and depression were reported in large numbers of people. This may be because virus-related information was over-reported by the media in the early stage of the epidemic, leading to the outbreak of the “information epidemic” [24]. People were unable to judge the truth of the information, and thus felt panic, which led to anxiety, in turn affected mental health. The high infectiousness of COVID-19 and the rising death toll caused fear. People may have been obsessively worried about whether they had infected COVID-19. During the period of home isolation required by the government, many people spend their most of the time on mobile phones to combat isolation and boredom. Repetitive stimulation, however, can reduce the excitement threshold, which can turn the original happiness into “emptiness” and then cause “affective disorder” [25]. Some studies proved that anxious individuals prefer to look for negative news [26]. This can cause anxiety levels to rise, leading to physical symptoms, such as trouble sleeping, headache, and chest tightness.
In the middle stages of the epidemic (February 19–April 08), comorbidities, sleep disorders, anxiety, worry, and depression were still the main problems. Self-harm or suicide and coping problems increased. Sleep disorders, anxiety, and depression have been found to be the main causes of suicide, and sleep disorders are the most important factor [27]. Despite the continuous advancement in neuroscience and the knowledge the pathophysiology of human behaviors, suicidal behavior still presents a challenge. The World Health Organization (WHO) found that one million people die by suicide every year, a daily rate of one suicide every 40 s [28]. In the middle stage of the epidemic, people had been isolated at home for some time, and loneliness and anxiety caused by long-term home isolation could not be alleviated. Over-cautiousness and even panic attacks appeared because of excessive concern with media information. The negative emotions produced in the early stage could not be relieved, and they sometimes developed into depression and caused somatic symptoms and sleep disorders. The combined effects of loneliness, excessive information exposure, and sleep disorders sometimes led to thoughts or behaviors of self-harm or suicide.
In the late stage of the epidemic (February 09–June 23), family relationships had gradually become one of the main problems. Teenagers complained that their parents were too strict and hard to communicate with, and that the family atmosphere was tense and stifling. Parents had marital problems, financial pressure, and problems communicating with children. During the epidemic, the learning space for students was transferred from school to family. The negative emotions caused by the epidemic fermented in the small space occupied by the family. The study found that the anxiety of college students and their parents was relatively high, with close contact increasing friction and conflicts and making the parent-child relationship more complex [29]. Enterprise employees faced the risk of layoffs and salary cuts. The owners of small to medium enterprises and individual businesses might lose their jobs or go bankrupt because of the epidemic [12]. All these things intensified family conflicts and put stress on family relationships.
An unexpected result was that in the later stage of the epidemic, sorrow and depression decreased, while other problems, including comorbidities, sleep disorders, anxiety, and other problems increased. This may be because most people returned to work, school, and normal social interactions, and economic life was also supported, resulting in reduced sorrow and depression. At the same time, after returning to work, people have new stressors. There is the worry of business closures and layoffs, and the fear of infection is serious.
The problems reported from the hotline may be a microcosm of the issues found in society, and therefore, the general public was also investigated. The results showed various emotional problems required prevention and intervention work, but conditions in general were better than expected. More than 70% of respondents showed no anxiety or depression at all, and about 20% had suspected symptoms, which may indicate that they had experienced anxiety or depression. This is consistent with the number of people seeking assistance through the hotline. Although people might be seeking assistance from other hotlines, 706 is still a very small figure nationwide.
Moreover, anxiety and depression are not completely negative emotions, and may help protect people from infection, although it is necessary to provide appropriate help and support for serious anxiety and depression.
Studies showed that up to 40% of those who seek mental health assistance during or after a disaster had mental problems or disorders before [30]. The epidemic and economic stresses have made many problems more difficult to solve, including difficulties in obtaining face-to-face treatment as well as interference with daily life, social rhythm, and sleep patterns [31]. People are prone to negative emotional reactions in the face of disasters, including depression, anxiety and stress. Studies have shown that people with emotional disorders have more difficulties in adapting to daily life, including lack of entertainment and recreation time, sleeping too little or too much, and drinking more. Patients with mood disorders who experience sleep problems and get less exercise will feel more psychological pain during the epidemic [14]. The individual differential reactivity is related to traumatic events and based on affective temperaments, which are important predictors of negative outcomes. According to the evidence, patients who were more prone to higher hopelessness reported depression and negative clinical outcomes in response to traumatic events more frequently [13].
Through correlation analysis, it was found that people with a history of chronic diseases were more likely to have psychological problems, but were not likely to become easily anxious and depressed. Compared with the general population, people in poor physical condition are more likely to experience anxiety, depression, fear, and worry, to have sleep disorders and suicidal thoughts. The results also showed that people who are currently in poor health are more likely to suspect that they have COVID-19. Because some diseases have symptoms that are similar to COVID-19 [32], or because medical treatment may increase the chance of being exposed to infected people, concerns about long-term health may be exacerbated [33,34]. Therefore, more attention should be paid to the people with physical health problems, and appropriate interventions undertaken.
The main problems presented in the different stages, even in the later stage of the epidemic, including psychological and emotional problems such as comorbidity, sleep disorders, anxiety, and other issues, show a trend that verifies our hypothesis. This report suggests that when giving psychological assistance, we should first consider the psychological impact of the cyclical changes in the epidemic situation and conduct a mental health survey. Second, further screening of psychological problems should be carried out according to the person’s main complaints. Finally, in the context of the normalization of epidemic prevention in China, mental health problems still require that psychological experts maintain sufficient vigilance.
The investigation started at the beginning of the epidemic and continued until the point when there were almost no new cases in China. Problems reported by people seeking psychological assistance, were analyzed statistically, and then a questionnaire was administered to members of the general public. Consistent results were obtained from these two sources. This may lead to a deeper understanding of the psychological status and changes experienced during the epidemic. The targeted focus on those seeking help from the hotline provides an empirical basis for future work. Compared with other studies, this survey covered a longer period and involved more population identities and emotional types. In the context of the normalization of epidemic prevention in China, this study may provide information to help people regain a positive mental health status and resume their normal lives.
Data from the crisis intervention platform is from people who sought help or who had been consulted and received a return visit, so there may be a sample representativeness bias. Further, the questionnaire for the general public was administered in May and June. That was during the late stage of the epidemic, and the situation of China had improved considerably. Subjects were asked to recall the situation since the epidemic, and thus their report may not be accurate. Finally, the distribution of subjects from various identities and regions is uneven, and care should be taken in interpreting and analyzing the results.
In summary, the main problems of visitors seeking psychological assistance during the epidemic include comorbidities, anxiety, and sleep disorders. Different periods showed different main problems. Fear, worry, anxiety, and comorbidity accounted for the largest proportion in the early and middle stages of the epidemic. Self-harm or suicide were the most common in the middle of the epidemic. Family relationship problems were reported by most visitors in the later stage of the epidemic. The investigation of psychological status showed that some people were still affected by the epidemic even in the later stage, resulting in psychological and emotional problems, such as anxiety, hypochondria, fear, worry, comorbidity, and sleep disorders. It is worth noting that although the epidemic has been alleviated at this time, people still have many problems.
Acknowledgement: The authors thank the all participants who responded to the questionnaire.
Funding Statement: This study was supported by Guangdong Philosophy and Social Sciences Funding(GD21CXL03).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Chowell, G., Mizumoto, K. (2020). The COVID-19 pandemic in the USA: What might we expect? Lancet, 395, 1093–1094. DOI 10.1016/S0140-6736(20)30743-1. [Google Scholar] [CrossRef]
2. Saglietto, A. (2020). COVID-19 in Europe: The Italian lesson. Lancet, 395, 1110–1111. DOI 10.1016/S0140-6736(20)30690-5. [Google Scholar] [CrossRef]
3. Li, J. P. O. (2020). Novel Coronavirus disease 2019 (COVID-19The importance of recognising possible early ocular manifestation and using protective eyewear. British Journal of Ophthalmology, 104(3), 297–298. DOI 10.1136/bjophthalmol-2020-315994. [Google Scholar] [CrossRef]
4. Rubin, G. J., Wessely, S. (2020). The psychological effects of quarantining a city. BMJ, 368, m313. DOI 10.1136/bmj.m313. [Google Scholar] [CrossRef]
5. Shultz, J. M., Perlin, A., Saltzman, R. G., Espinel, Z., Galea, S. (2020). Pandemic march: COVID-19’s first wave circumnavigates the globe. Disaster Medicine and Public Health Preparedness, 14(5), 1–13. DOI 10.1017/dmp.2020.103. [Google Scholar] [CrossRef]
6. Ding, S. R., Shi, J., Wang, Y. L., Wang, B. H. (2005). Investigation on mental states of inhabitants during epidemic outbreak stage of SARS. Chinese Journal of Public Health, 21(9), 1119–1120. DOI 10.11847/zgggws2005-21-09-54. [Google Scholar] [CrossRef]
7. Maunder, R., Hunter, J., Vincent, L., Bennett, J., Peladeau, N. et al. (2003). The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. Canadian Medical Association Journal, 168(10), 1245–1251. DOI 10.1001/jama.289.18.2432. [Google Scholar] [CrossRef]
8. Lee, S. M., Kang, W. S., Cho, A. R., Kim, T., Park, J. K. (2018). Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comprehensive Psychiatry, 87(7), 123–127. DOI 10.1016/j.comppsych.2018.10.003. [Google Scholar] [CrossRef]
9. Zhou, M. Y., Xie, X. L., Peng, Y. G., Wu, M. J., Shang, L. H. (2020). From SARS to COVID-19: What we have learned about children infected with COVID-19. International Journal of Infectious Diseases, 96(4), 710–714. DOI 10.1016/j.ijid.2020.04.090. [Google Scholar] [CrossRef]
10. Xiang, Y. T., Yang, Y., Li, Y. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry, 7(3), 228–229. DOI 10.1016/S2215-0366(20)30046-8. [Google Scholar] [CrossRef]
11. Cindy, H. L., Emily, Z., Wong, G. T. F. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. DOI 10.1016/j.psychres.2020.113172. [Google Scholar] [CrossRef]
12. Tian, F. Y., Li, H. X., Tian, S. C., Yang, J., Shao, J. et al. (2020). Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Research, 288, 112992. DOI 10.1016/j.psychres.2020.112992. [Google Scholar] [CrossRef]
13. Pompili, M., R., Z., Akiskal, H., Amore, M., Gonda, X. (2020). Temperaments mediate suicide risk and psychopathology among patients with bipolar disorders. Comprehensive Psychiatry, 53(3), 280–285. DOI 10.1016/j.comppsych.2011.04.004. [Google Scholar] [CrossRef]
14. Van Rheenen, T. E., Denny, M., Erica, N., Andrea, P. et al. (2020). Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Journal of Affective Disorders, 275, 69–77. DOI 10.1016/j.jad.2020.06.037. [Google Scholar] [CrossRef]
15. Huang, Y., Zhao, N. (2020). Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychology, Health & Medicine, 4(14), 1–12. DOI 10.1080/13548506.2020.1754438. [Google Scholar] [CrossRef]
16. Morgeson, F. P., Mitchell, T. R., Liu, D. (2015). Event system theory: An event-oriented approach to the organizational sciences. Academy of Management Review, 40(4), 515–537. DOI 10.5465/amr.2012.0099. [Google Scholar] [CrossRef]
17. Mowday, R. T., Sutton, R. I. (1993). Organizational behavior: Linking individuals and groups to organizational contexts. Annual Review of Psychology, 44(1), 195–229. DOI 10.1146/annurev.ps.44.020193.001211. [Google Scholar] [CrossRef]
18. Frederick, P. (2005). The external leadership of self-managing teams: Intervening in the context of novel and disruptive events. Journal of Applied Psychology, 90(3), 497–508. DOI 10.1037/0021-9010.90.3.497. [Google Scholar] [CrossRef]
19. Zigmond, A. S., Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. DOI 10.1111/j.1600-0447.1983.tb09716.x. [Google Scholar] [CrossRef]
20. Lazarus, R. S., Folkman, S. (1984). Stress, appraisal, and coping. Children’s Health Care, 29(4), 279–293. DOI 10.1207/s15326888chc2904_4. [Google Scholar] [CrossRef]
21. Rudenstine, S., Galea, S. (2014). Behavioral consequences of disasters: A five-stage model of population behavior. Disaster Medicine and Public Health Preparedness, 8(6), 497–504. DOI 10.1017/dmp.2014.114. [Google Scholar] [CrossRef]
22. Li, S. J., Wang, Y. L., Xue, J., Zhao, N., Zhu, T. S. (2020). The impact of COVID-19 epidemic declaration on psychological consequences: A study on active Weibo users. International Journal of Environmental Research and Public Health, 17(6), 2032. DOI 10.3390/ijerph17062032. [Google Scholar] [CrossRef]
23. Xing, X., Zhao, J. F., Zhao, G. X. (2016). Role of social support in buffering effects of stress on neural and endocrine systems. Advances in Psychological Science, 24(4), 517–524. DOI 10.3724/SP.J.1042.2016.00517. [Google Scholar] [CrossRef]
24. Wang, Y., Gao, J. L., Chen, H., Mao, Y. M., Chen, S. H. et al. (2020). The relationship between media exposure and mental health problems during COVID-19 outbreak. Fudan University Journal of Medical Sciences, 47(2), 173–178. DOI 10.3969/j.issn.1672-8467.2020.02.005. [Google Scholar] [CrossRef]
25. Gao, T., Li, J., Han, Z., Gao, J., Mei, S. (2018). The influence of alexithymia on mobile phone addiction: The role of depression, anxiety and stress. Journal of Affective Disorders, 225(1), 761–766. DOI 10.1016/j.jad.2017.08.020. [Google Scholar] [CrossRef]
26. Goodwin, H., Yiend, J., Hirsch, C. R. (2017). Generalized anxiety disorder, worry and attention to threat: A systematic review. Clinical Psychology Review, 54(2), 107–122. DOI 10.1016/j.cpr.2017.03.006. [Google Scholar] [CrossRef]
27. Wang, R. J., Li, J., Mei, J. H., Xiao, M. Z., Li, K. et al. (2020). Poor sleep quality, anxiety and depression are associated with an increased suicide risk in patient. Journal of Third Military Medical University, 14, 1462–1468. DOI 10.16016/j.1000-5404.202003229. [Google Scholar] [CrossRef]
28. de Berardis, D., Fornaro, M., Valchera, A., Cavuto, M. P. G. (2018). Eradicating suicide at its roots: Preclinical bases and clinical evidence of the efficacy of ketamine in the treatment of suicidal behaviors. International Journal of Molecular ences, 19(10), 2888. DOI 10.3390/ijms19102888. [Google Scholar] [CrossRef]
29. Ye, B. Q., Xu, Y., Dong, M. (2021). Investigation and analysis of mental health status of post-2000s freshmen during the COVID-19 pandemic. Journal of Chongqing University of Technology (Social Science), 25(3), 143–151. DOI 10.3969/j.issn.1674-8425(s). 2021.03.016. [Google Scholar] [CrossRef]
30. North, C. S., Pfefferbaum, B. (2013). Mental health response to community disasters. JAMA, 310(5), 507–518. DOI 10.1001/jama.2013.107799. [Google Scholar] [CrossRef]
31. Bowen, R., Balbuena, L., Baetz, M., Schwartz, L. (2013). Maintaining sleep and physical activity alleviate mood instability. Preventive Medicine, 57(5), 461–465. DOI 10.1016/j.ypmed.2013.06.025. [Google Scholar] [CrossRef]
32. Zaman, S., Thomas, L., Schlaich, M. (2020). Cardiovascular disease and COVID-19: Australian and New Zealand consensus statement. Medical Journal of Australia, 213(4), 182–187. DOI 10.5694/mja2.50714. [Google Scholar] [CrossRef]
33. Goldstein, B. I. (2017). Bipolar disorder and the vascular system: Mechanisms and new prevention opportunities. Canadian Journal of Cardiology, 33(17), 1565–1576. DOI 10.1016/j.cjca.2017.10.006. [Google Scholar] [CrossRef]
34. Rodrigo, B. M., Elisa, B., Roger, S. M. (2015). Is there a metabolic-mood syndrome? A review of the relationship between obesity and mood disorders. Neuroscience & Biobehavioral Reviews, 52(5), 89–104. DOI 10.1016/j.neubiorev.2014.12.017. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |