
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/ijmhp.2022.018542
ARTICLE
Specific Types of Screen-Based Sedentary Time and Depressive Symptoms in Adolescents
School of Physical Education and Training, Shanghai University of Sport, Shanghai, 200438, China
*Corresponding Author: Shande Liu. Email: liushande2021@163.com
Received: 18 August 2021; Accepted: 17 November 2021
Abstract: Purpose: Screen-based sedentary behavior (SSB) has been identified as risk factor for mental disorders in most of adolescents. However, there is little literature pertaining to the specific kinds of SSB and its connections with depressive symptoms in most of adolescents. In the present study, we are going to find out the connections between specific types of SSB and depressive symptoms in Chinese adolescents. Methods: A cross-sectional data based on 996 study participants of middle school students in Guangdong Province. SSB was evaluated by distributing the questionnaire of Health Behavior in School-aged Children, while depressive symptoms were evaluated using Chinese version of Children’s Depressive symptoms Inventory (CDI). SSB was categorized into TV/movie time, video games time and other electronic devices-based time (e.g., mobile phone, computer use). Generalized linear models was used to explore the connections between specific kinds of SSB and depressive symptoms. Results: After controlling for variables of sex, ethnicity, grade, residence, siblings, perceived family affluence, father educational level, mother educational background, body mass index (BMI), physical exercise, duration of sleep, other electronic devices-based time was positively correlated with depressive symptoms in Chinese adolescents (B = 0.557%, 95%CI: 0.187–0.926, p = 0.003). This significant connection was also found in girls (B = 0.728%, 95%CI: 0.230–1.225, p = 0.004) instead of boys (p > 0.05). The other types of SSB were not significantly in relation to depressive symptoms in adolescents regardless of sex. Conclusion: This study suggested that it might be effective in reducing or preventing depressive symptoms through limiting electronic devices-based time, like computer use or mobile phone use time. This strategy would be particularly useful in girls. Future studies should negate or replicate the research results by introducing more improved study design, which is beneficial to better understand the connections between SSB and depressive symptoms as well as then design more efficient interventions in adolescents.
Keywords: Screen time; types; middle school students; depression
Depressive symptoms are a common psychiatric disorder, which has gained widespread concerns across the world. Recently, depressive symptoms are considered as a public health priority in adolescents [1,2], because about 20% of adolescents were affected by this psychiatric disorder worldwide [3]. Compared with other psychiatric disorders, depressive symptoms cause higher mortality and morbidity [4]. According to the World Health Organization (WHO), depressive symptoms will have become the second major cause of disease burden in the world by 2030 [5]. Notably, previous data demonstrated that more than 340 million people suffered from depressive symptoms, so this has become a mental health issue worth attention [6]. Specifically, pieces of evidence have revealed that depressive symptoms are associated with several health risks in adolescents, including cognitive impairment, functional impairment, academic performance, suicide, psychosocial [7,8]. Adolescent depressive symptoms can strongly predict the risk of mental health disorders in adulthood [9]. Due to negative consequences caused by depressive symptoms for mental and physical health results in Chinese adolescents, it is a critical to prevent and control depressive symptoms development in adolescents.
Recently, epidemiological surveys have been performed in general populations, and the results show that the prevalence of depressive symptoms is in the range of 10% to 15%. Furthermore, approximately 50% of serious cases of depressive symptoms were found in developed countries, and this proportion in undeveloped countries varied from 76.3% to 85.4%. Notably, the severe depressive symptoms and increasing trend were also found in adolescents [10,11]. Recent epidemiological surveys in Chinese adolescents indicated that the general prevalence of depressive symptoms reached 22.2% [12], and ranged from 6.4% to 54.4% [13,14] across different young subpopulations. Currently, the depressive symptoms are quite prevalent, which has attracted attention from society, and alleviating the burden of depressive symptoms has been proposed in the Healthy China Blueprint 2019–2030 [15]. Based on the current status of depressive symptoms in Chinese adolescents and the growing concern of the Chinese government, it is urgent to identify factors on depressive symptoms in Chinese adolescents.
Previous evidence showed that screen-based sedentary time (SSB) is an important factor of depressive symptoms [16], and positively associated with depressive symptoms [17]. The data from countries featuring low and middle incomes suggested that the prevalence of adolescents who engage in 1–2 h SSB was extremely lower [18]. Besides, one study revealed that SSB may independently and positively affect depressive symptoms [19]. In addition to exploring the connections between SSB and depressive symptoms in Chinese adolescents, recently, more and more studies have sought to explore the connections between specific types of SSB (e.g., time spent on television, internet and video game) and depressive symptoms in Chinese adolescents. Compared with playing computer and video games, television viewing time seems unlikely to be related with depressive symptoms [20]. A study based on a large samples of UK birth cohort found that the use of computer was particularly and significantly correlated with depressive symptoms, while the connections between other types of SSB and depressive symptoms was considered as non-significant [21]. Indeed, studies on the links between specific kinds of SSB and depressive symptoms generated mix results [22,23]. On this regard, it is urgently required to better understand the connections between specific kinds of SSB and depressive symptoms in adolescents.
Across the literature, although some studies have started assessing the connection between specific types of SSB and depressive symptoms. Some other study limitations existed, which should seek to address in the current study or future studies. Specifically, previous evidence showed that regular physical exercise was correlated with depressive symptoms [24,25]. though there is no conclusive claim. However, some of prior research failed to control physical activity when assessing the connections between specific types of SSB and depressive symptoms [21,26]. Furthermore, studies have confirmed that sleep duration is a risk factor of depressive symptoms [27–30], but the variable of sleep in the previous studies. The omission of variables of physical activity and sleep could result in bias when assessing the connections between SSB and depressive symptoms. last but not least, previous studies on the connections between specific types of SSB and depressive symptoms were mainly based on Western countries’ young children and adolescents, there is little evidence on the connections based on Chinese children and adolescents. In fact, Chinese young people are exposed to excessive SSB [31–33], which may increase the risks of depressive symptoms.
Therefore, explore the relationships between different types of SSB and depressive symptoms in adolescents (a sample of Chinese middle school students).
2.1 Study Participants and Design
The purpose of the research is to discover the influence of summertime on the mental and physical health of adolescents. A cross-sectional study is performed to meet the purpose of study, and we have recruited some adolescents (students from grade 7 to 9 at the middle schools). There is one middle school (three grades are set up) at every city of Guangdong Province included in the current study (11 cities are included). Students were recruited from each grade randomly. Generally, 3,456 students have been included in the current study. Because in summer, the respondents will not actively respond to the survey, 1,998 respondents and their parents have filled out the form. The response rate of current survey wasn’t ideal, with the response rate of 57.7%. Among these 1998 respondents, 966 of them gave valid data relevant to the study variables. Before the data was collected, principals of all the schools, the respondents and their parents have been informed of the research purpose, and they were given with relevant instructions. We obtained written consent from every respondent and their parents. To protect the privacy of respondents, the data were obtained and recorded anonymously.
2.2 Measures of Studied Variables
All the respondents were required to provide the following information: gender, BOD (year/month), their grades, ethnicity (minority or Han), residence (rural or urban), weight (Kg) or height (cm), perceived family affluence (based on Family Affluence Scale), educational background of their parents (primary school or below, middle school, occupation school or senior middle school, undergraduate, postgraduate or above), their siblings (give details).
2.2.2 Study Results (Depressive Symptoms)
The results of study were depressive symptoms. The depressive symptoms showed by the respondents had been evaluated using self-reported tool, that is, Children’s Depressive Symptoms Inventory (CDI). The tool is developed by Kovacs [34] and the tool has been further validated among adolescents and children aged between 7 and 17 years at Chinese schools [35]. The tool comprises 27 items and the responses are scored 0 to 2, and the general score is ranged within 0–54. The higher the score, the greater the severity of depression.
2.2.3 Exposure of Study (Screen-Based Sedentary Behaviour, SSB)
SSB has been evaluated based on the health behaviour reported by the children at the questionnaire [36], the questions are: (1) How long did you spend on TV or film during your spare time on the last holidays or weekends? (2) How long did you spend on video games during your spare time on the last holidays or weekends? (3) How long did you spend on activity involving the use of devices based on electronic screen during your spare time on the last holidays or weekends? The answers included 0.5 or 7 h or more. The mean SSB hours every day was worked out using the formula: mean specific type of SB hours every day = (one SSB hours) Under the research background, SSB has been classified into three types, that is, time of playing video game, time of watching TV or movie, and other time of using devices based on electronic screen. For the purpose of statistical analysis, the variables and specific SSB types were considered continuous.
2.2.4 Other Behavioural Controlling Variables
SLP was evaluated using the measures developed based on HBSC questionnaire [36]: (1) When do you generally go to sleep when you need to attend a morning class on the next day? (2) When do you generally go to sleep during holidays or at weekends? (3) When do you generally get up if you need to attend a morning class on the next day? (4) When do you generally get up on Saturday or Sunday? Answers to the questions 1 to 4 are shown below: (1) No later than 21:00; 21:30; 22:00; 22:30; 23:00; 23:30; 24:00; 00:30; 01:00; 01:30; 02:00 or later; (2) No later than 21:00; 21:30; 22:00; 22:30; 23:00; 23:30; 24:00; 00:30; 01:00; 01:30; 02:00; 02:30; 03:00; 03:30; 04:00 or later; (3) No later than 05:00; 05:30; 06:00; 06:30; 07:00; 07:30; 08:00 or later; and (4) no later than 07:00; 07:30; 08:00; 08:30; 09:00; 09:30; 10:00; 10:30; 11:00; 11:30; 12:00; 12:30; 13:00; 13:30; 14:00 or later. Based on the answers, SLP duration at night on weekend or weekdays was worked out. Then, the mean SLP duration every night (hours) was worked out using the following formula: mean duration of SLP = (SLP duration every night on weekdays × 5 + SLP duration every night at weekends × 2)/7. In the statistical analysis, SLP variable was considered continuous.
Based on the questionnaire of Health Behaviour in School-aged Children (HBSC), MVPA was evaluated, and the questionnaire has been frequently adopted in the epidemiological studies in China. One of the questions is: how long did you spend on physical activity that increases heart rates (including PE lesson, sports training, exercise, and regular activities such as excursion, hiking and brisk walking) (for example, sport participations, exercise, physical education). The answers included 0 to 7 days. For the purpose of statistical analysis, the MVPA variables were considered continuous.
The statistical analysis was performed with the use of SPSS (25.0). Descriptive statistics was performed to review the percentage and frequency (%) categorical variables such as gender and residence, and the standard deviation of and mean continuous (BMI). Partial test was performed to check the gender difference across the categorical variables, and the student t test was performed to check the gender difference cross the continuous variables. Partial correlation analysis was performed to obtain the coefficient of correlation between the depressive symptoms and ST of different types, while controlling for grade, ethnicity, gender, affluence, siblings, residence, the educational background of parents, BMI, and physical activity and time of sleep. We have introduced Generalized Linear Models (GLMs) to check the relationship between ST, MVPA and SLP with depressive symptoms. We have adopted Robust Estimator, Maximum Likelihood Estimation (MLE) and GLMs to check the relationship between different ST types and depressive symptoms. Beta estimates adjusted (corresponding 95% confidence intervals (CI) were shown. Statistical significance was found to be p < 0.05 (which is two sided).
Table 1 presents the study sample characteristics. 996 students from junior middle schools (grades 7–9) participated in the study. In total, 48.5% were boys (n = 483), and 51.4% were girls (n = 514). The majority were of Chinese Han ethnicity (97.1%) and from urban area (73.9%). The mean of BMI was 18.93 kg/m2 (SD = 4.02). Overall, participants accumulated time spent in MVPA is 5.05 ± 2.08. The MVPA time of boys was 5.37 days (±2.11), significantly higher than that of girls (4.71 ± 1.89, p < 0.001). In addition, the overall time (hours/day) participants spent on TV/movie is 2.76 ± 1.31, video game time 2.28 ± 1.37, other electronic devices-based time 2.62 ± 0.90, and sleep 8.43 ± 1.27. Moreover, the mean scores of depressive symptoms in girls were greater than that in boys with statistical significance (37.04 ± 5.32 vs. 36.44 ± 5.32). More details can be found in Table 1.
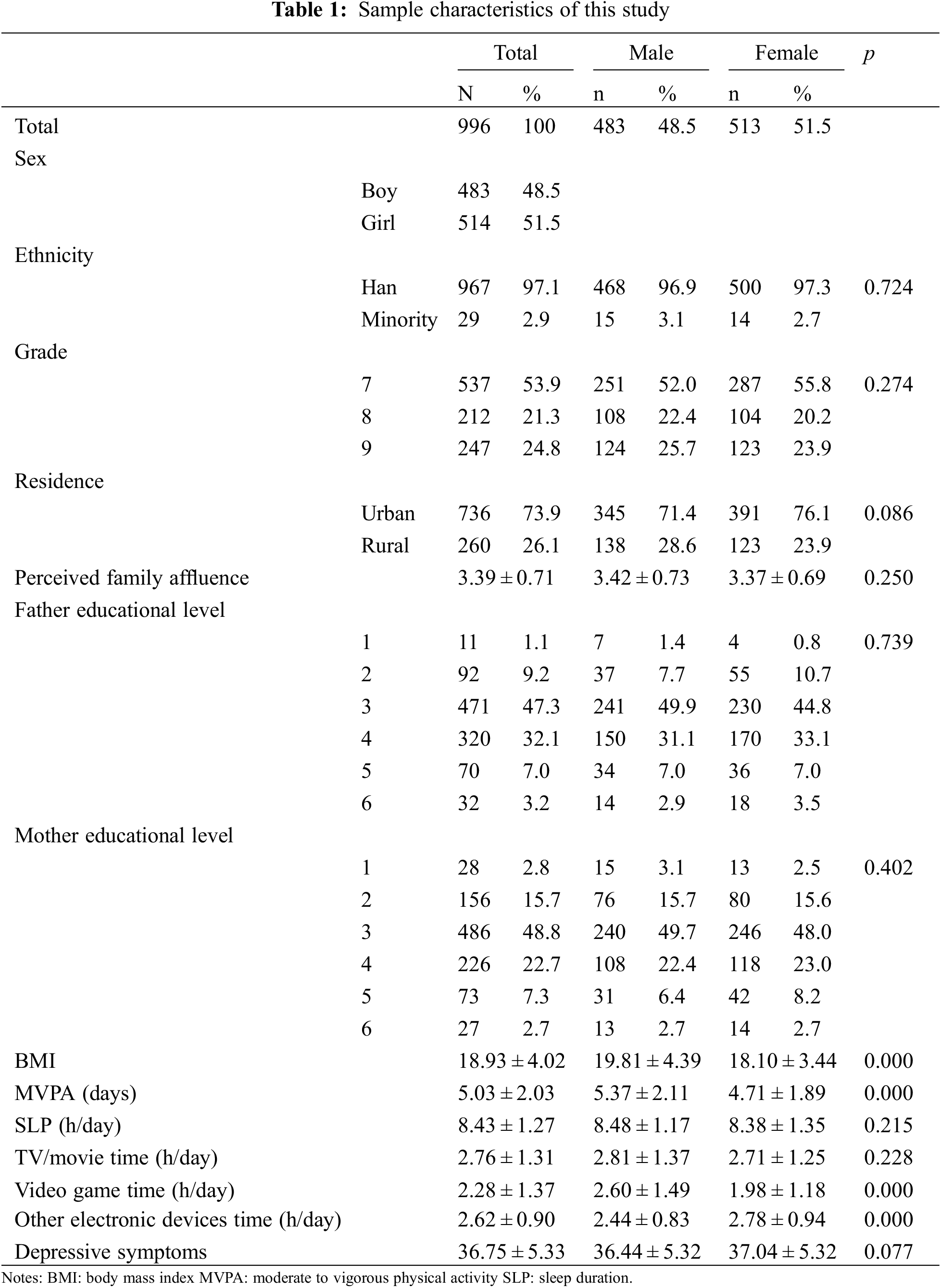
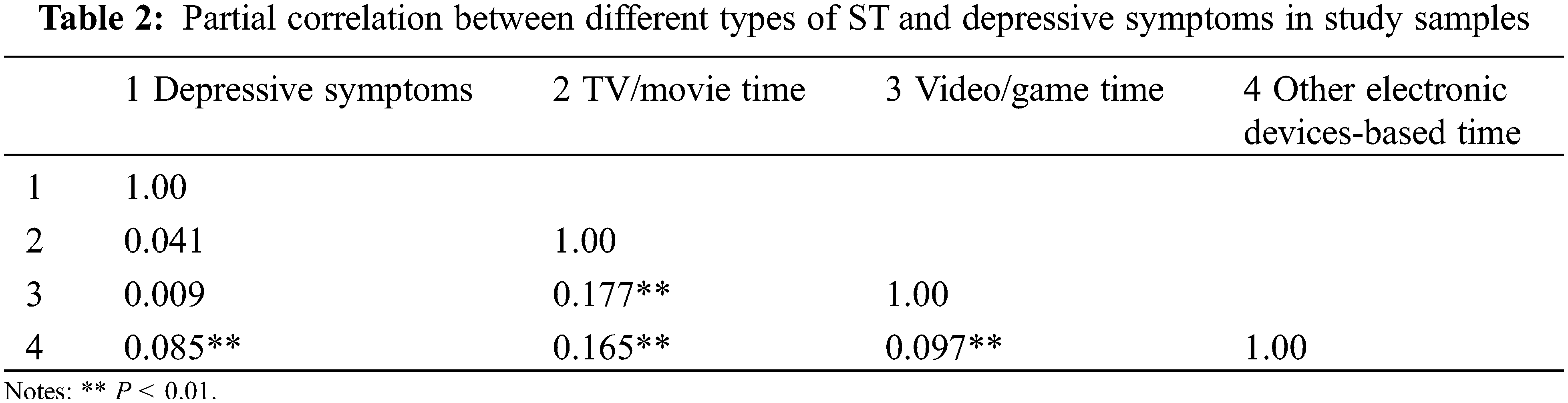
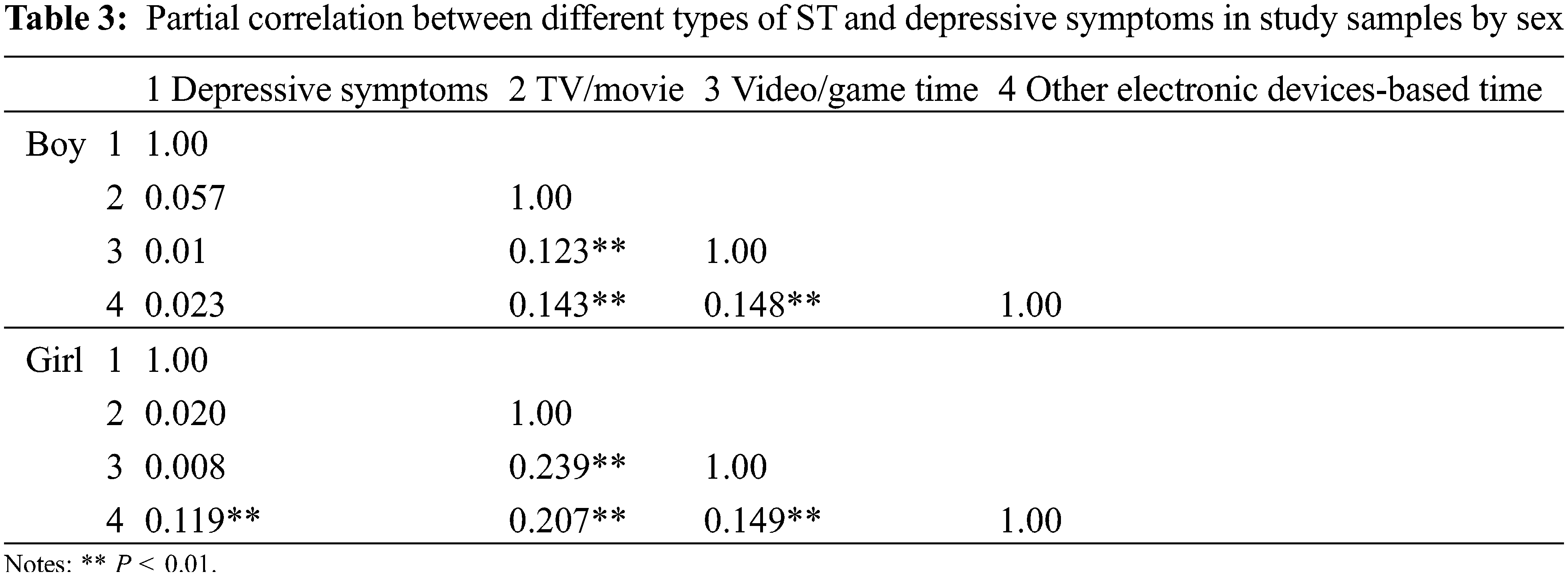
Table 2 shows the bivariate correlation between different types of ST and depressive symptoms. Significant correlation was found between depressive symptoms and other electronic devices-based time (r = 0.085, p < 0.01), TV/movie time and video/game time (r = 0.177, p < 0.01), TV/movie time and other electronic devices-based time (r = 0.165, p < 0.01), and video/game time and other electronic devices-based time (r = 0.097, p < 0.01). The result for further disentangled the difference in variables correlation between two genders are presented in Table 3. Notably, the connection between depressive symptoms and other electronic devices-based time in boys was not significant. However, depressive symptoms were positively related to other electronic devices-based time in girls (r = 0.119, p < 0.01).
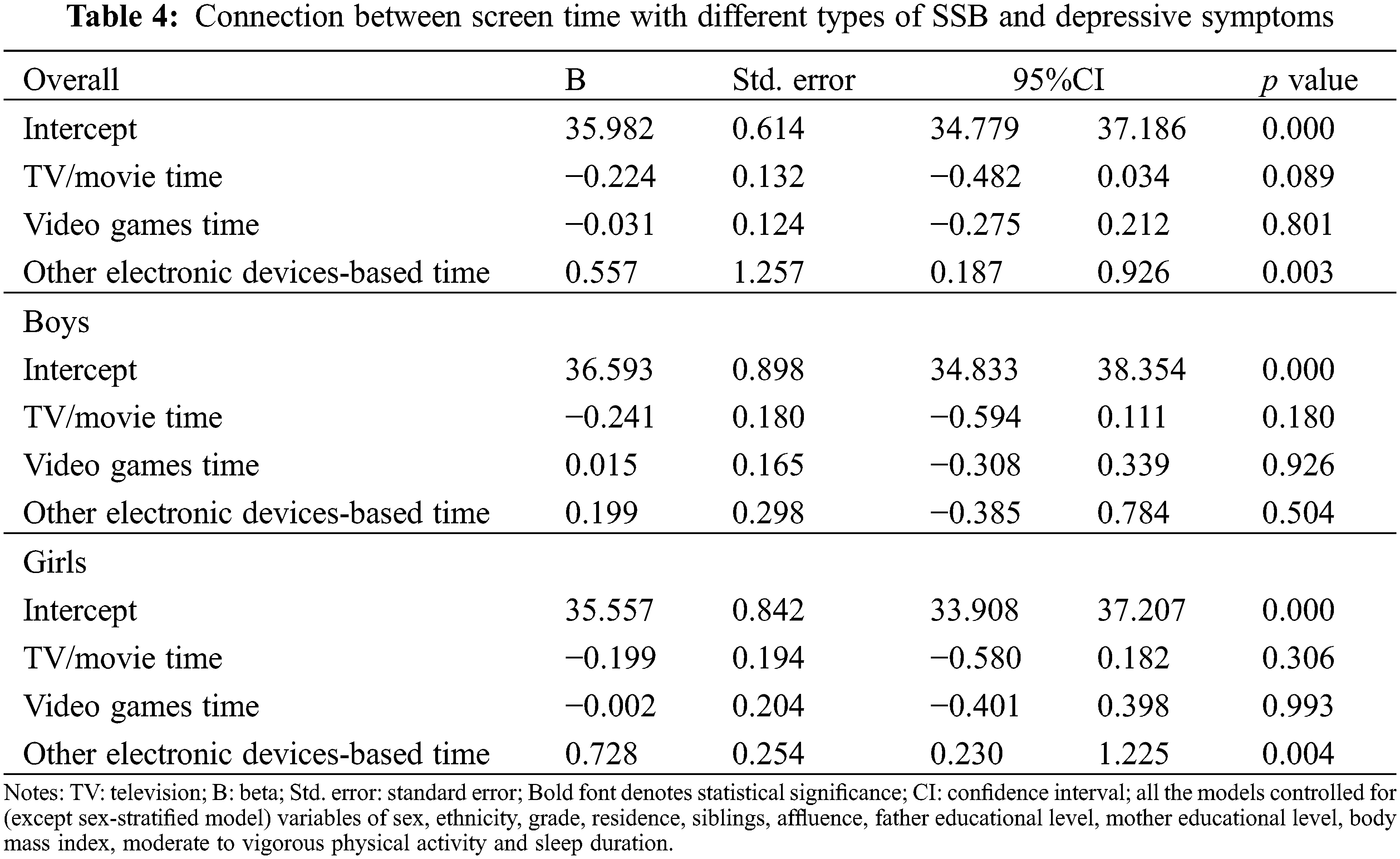
The results of the connection between screen time with different types of SSB and depressive symptoms are presented in Table 4. For the total sample, the results from GLMs indicated that only other electronic devices-based time positively associated with depressive symptoms (B = 0.557%, 95%CI: 0.187–0.926, p = 0.003). However, TV/movie and video games time were not associated with depressive symptoms (both p > 0.05). The similar results were also found in female samples. Specifically, other electronic-based time positively associated with depressive symptoms (B = 0.728%, 95%CI: 0.230–1.225, p = 0.004). In the contrast, no specific type of SSB was associated with depressive symptoms in male samples (p for TV/movie time, p for video games time and p for other electronic devices-based time > 0.05).
The main of our study was to explore the connections between specific types of SSB and depressive symptoms in some typical Chinese adolescents in Guangdong Province. We mainly found that only other electronic devices-based time was positively associated with depressive symptoms in adolescents and this significant connection was observed in girls rather than boys. In addition, the connections of TV/movie time and video games time were not correlated with depressive symptoms in a significant way in adolescents regardless of sex. More discussions and analyses are presented in detail below.
The current study found that other electronic devices-based time was correlated with depressive symptoms in a significant way in adolescents. According to the measurement of other electronic devices-based time in our study can be defined as time spent for computer, mobile phone or tablet use. Some previous research suggested that time for computer [21,26], mobile phone [37,38] and tablet use were risk factors of depressive symptoms. Those prior research findings can support the current study consistently, which further stresses the adverse effects of this kind of SSB on depressive symptoms in adolescents. Standing on a practical perspective, reducing or curbing this kind of SSB may be an effective and preventive approach to reduce depressive symptoms in adolescents. Some plausible explanations can be used to better understand the underlying mechanism linking this specific kind of SSB and depressive symptoms. For example, prolonged time of phone use is positively associated with sleep problems, like insomnia and disturbance, which in turn may increase the risks for depressive symptoms [37,38]. For computer use, it is possible that adolescents who tend to spend more time in computer for various purposes have a higher risk for sleep disturbance, and social isolation as well as other problems in social interactions that are independent factors of depressive symptoms [23,39]. However, the suggested mechanisms are yet conclusive. Future research is strongly recommended to determine the mechanism linking specific types of SSB and depressive symptoms in Chinese adolescents.
The current study suggested that TV/movie and video games time were not correlated with depressive symptoms in a significant way in adolescents. These two research findings are not in line with previous studies that indicated that TV/movie and video games time were independent correlates of depressive symptoms [26,40]. However, some previous studies can support that TV/movie time and video games was not correlated with depressive symptoms [21,22], which is consistent with our research findings. These discrepant findings between the present study and other previously published studies may be owing to methodological differences. Hence, research using standardized and similar study protocols are needed for more comparable evidence, which is beneficial to clearly determine the connections between specific types of SSB and depressive symptoms in adolescents. On this regard, more replicated research should be encouraged.
The non-significant connections between TV/movie time and video games time and depressive symptoms could be explained by the following reasons. However, there were some previous studies that have proposed plausible interpretations for mechanism linking TV/movie and video game time and depressive symptoms. One primary explanation is that adolescents are likely to choose their preferred or interested kinds of TV/movie and video games, which may reduce their negative moods. As a result, depressive symptoms might be reduced significantly. However, there are many studies suggesting extended TV/movie and video games time are risk factors of depressive symptoms as well as proposing potential mechanism. It is needed, thus, to further clarify the underlying mechanism linking TV/movie and video game time and depressive symptoms in adolescents.
Interestingly, the current study has shown that the connections between specific types of SSB and depressive symptoms in adolescents are with a sex difference, particularly in the connections between other electronic devices-based time and depressive symptoms. To our knowledge, littles is known about this sex difference because of a limited number of studies that include sex-stratified analysis [41–43], especially in examining the connections between electronic devices-based time and anxiety symptoms. 23 Based on the previous evidence in the literature, the sex difference in the connections between specific types of SSB and anxiety symptoms is null findings [23]. When explaining this sex difference, the preferences of specific types of SSB may be useful [23]. On this regard, the current study assumes that the sex difference in the connections between other electronic devices-based time and depressive symptoms matters sex-oriented preference on types of SSB. Specifically, girls are more likely to use computer, mobile phone for their social purposes as well as other purposes; in contrast, boys seem to have less interests in using electronic devices [44]. This difference could explain partially why other electronic devices-based time was correlated with depressive symptoms in a significant way in girls. However, its underlying mechanism by sex should be clarified clearly in the future. Practically, to better design and implement interventions aiming at reducing depressive symptoms, sex-specific interventional strategies should be utilized.
Although this study has some strengths, including a relatively large sample, using a standardized ST measure, controlling more potential confounders, some intrinsic limitations with the current study need to be mentioned, which is beneficial to better interpret the research findings of this study. First, our study used cross-sectional design study that cannot draw conclusions with causality. Hence, our study cannot determine the connection between different kinds of SSB and anxiety symptoms based on a perspective of casual reference. The second limitation concerns measurement in this study which was a self-reported questionnaire (although being used widely across the world). This could make our measurement of SSB biased or inaccurate because of recall errors. Third, our study was based on samples recruited from Guangdong Province; so, our research findings may not be generalized into a wider spectrum of populations. As for the future studies, it is strongly recommended that these study limitations are addressed for more reliable and robust evidence, which can be applied for interventions aiming at reducing mental disorders.
In the present study, the connections between different kinds of SSB and depressive symptoms have been explored in adolescents (a sample of Chinese in Guangdong Province). To conclude, this study suggested that except TV/movie and video game screen time, only electronic devices time was a correlate of depressive symptoms in adolescents. This connection was also found in girls instead of boys. Our study could provide practical implication for designing more efficient interventions aiming at reducing depressive symptoms. However, owing to the study design and study characteristics (e.g., sample, measures, survey time), research findings of the current study should be negated or replicated by more research with improvements. On this regard, it is highly required to conduct more studies help researchers better understand specific types of SSB and depressive symptoms in adolescents.
Acknowledgement: The author expressed great appreciate to the students who engaged in this survey.
Funding Statement: The author received no specific funding for this study.
Conflicts of Interest: The author declares that they have no conflicts of interest to report regarding the present study.
1. Merikangas, K. R., Nakamura, E. F., Kessler, R. C. (2019). Epidemiology of mental disorders in children and adolescents. Dialogues of Clinical Neuroscience, 11(1), 7–20. DOI 10.31887/DCNS.2009.11.1/krmerikangas. [Google Scholar] [CrossRef]
2. Vigo, D., Thornicroft, G., Atun, R. (2016). Estimating the true global burden of mental illness. Lancet Psychiatry, 3, 171–178. DOI 10.1016/S2215-0366(15)00505-2. [Google Scholar] [CrossRef]
3. Kieling, C., Baker-Henningham, H., Belfer, M. (2011). Child and adolescent mental health worldwide: Evidence for action. Lancet, 378(9801), 1515–1525. DOI 10.1016/S0140-6736(11)60827-1. [Google Scholar] [CrossRef]
4. Saluja, G., Iachan, R., Scheidt, P. C., Overpeck, M. D., Sun, W. et al. (2004). Prevalence of and risk factors for depressive symptoms among young adolescents. Archives of Pediatrics, 158(8), 760–765. DOI 10.1001/archpedi.158.8.760. [Google Scholar] [CrossRef]
5. Mathers, C. D., Loncar, D. (2006). Projection of global mortality and burden of disease from 2002 to 2030. PLoS Medicine, 3, e442. DOI 10.1371/journal.pmed.0030442. [Google Scholar] [CrossRef]
6. Greden, J. (2003). Physical symptoms of depression: Unmet needs. International Journal of Psychiatry in Clinical Practice, 64(Suppl 7), 5–11. DOI 10.1016/S0887-6185(02)00239-6. [Google Scholar] [CrossRef]
7. Keenan-Miller, D., Hammen, C., Brennan, P. (2007). Health outcomes related to early adolescent depression. Journal of Adolescent Health, 41, 256–262. DOI 10.1016/j.jadohealth.2007.03.015. [Google Scholar] [CrossRef]
8. Lépine, J. -P., Briley, M. (2001). The increasing burden of depression. Neuropsychiatric Disease and Treatment, 7(Suppl 1), 3–7. DOI 10.2147/NDT.S19617. [Google Scholar] [CrossRef]
9. Clayborne, Z. M., Varin, M., Colman, I. (2019). Systematic review and meta-analysis: Adolescent depression and long-term psychosocial outcomes. Journal of the American Academy of Child and Adolescent Psychiatry, 58(1), 72–79. DOI 10.1016/j.jaac.2018.07.896. [Google Scholar] [CrossRef]
10. Barker, M. M., Beresford, B., Bland, M., Fraser, L. K. (2019). Prevalence and incidence of anxiety and depression among children, adolescents, and young adults with life-limiting conditions. JAMA Pediatrics, 173(9), 835. DOI 10.1001/jamapediatrics.2019.1712. [Google Scholar] [CrossRef]
11. Mojtabai, R., Olfson, M., Han, B. (2016). National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics, 138(6), e20161878–e20162016. DOI 10.1542/peds.2016-1878. [Google Scholar] [CrossRef]
12. Li, J. Y., Li, J., Liang, J. H. (2019). Depressive symptoms among children and adolescents in China: A systematic review and meta-analysis. Medical Science Monitor, 25, 7459–7470. DOI 10.12659/MSM.916774. [Google Scholar] [CrossRef]
13. Tan, Y., Chen, Y., Lu, Y., Li, L. (2016). Exploring connections between problematic internet use, depressive symptoms and sleep disturbance among southern Chinese adolescents. International Journal of Environmental Research and Public Health, 13(3), 313. DOI 10.3390/ijerph13030313. [Google Scholar] [CrossRef]
14. Guo, L., Deng, J., He, Y. (2014). Prevalence and correlates of sleep disturbance and depressive symptoms among Chinese adolescents: A cross-sectional survey study. BMJ Open, 4, e005517. DOI 10.1136/bmjopen-2014-005517. [Google Scholar] [CrossRef]
15. The Healthy China Blueprint 2019–2030 (2019). http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm. [Google Scholar]
16. Rezende, L., Lopes, M., Rey, L. J., Matsudo, V., Luiz, O. (2014). Sedentary behavior and health outcomes: An overview of systematic reviews. PLoS One, 9, e105620. DOI 10.1371/journal.pone.0105620. [Google Scholar] [CrossRef]
17. Johnson, C., Murray, D., Elder, J. (2008). Depressive symptoms and physical activity in adolescent girls. Medicine & Science in Sports & Exercise, 40, 818–826. DOI 10.1249/MSS.0b013e3181632d49. [Google Scholar] [CrossRef]
18. Vancampfort, D., Stubbs, B., Firth, J., Van, D. T., Koyanagi, A. (2018). Sedentary behavior and depressive symptoms among 67,077 adolescents aged 12–15 years from 30 low-and middle-income countries. International Journal of Behavioral Nutrition and Physical Activity, 15. DOI 10.1186/s12966-018-0708-y. [Google Scholar] [CrossRef]
19. Breland, J., Fox, A., Horowitz, C. (2012). Screen time, physical activity and depression risk in minority women. Mental Health and Physical Activity, 6(1), 10–15. DOI 10.1016/j.mhpa.2012.08.002. [Google Scholar] [CrossRef]
20. Zink, J., Belcher, B. R., Imm, K., Leventhal, A. M. (2020). The relationship between screen-based sedentary behaviors and symptoms of depression and anxiety in youth: A systematic review of moderating variables. BMC Public Health, 20(1), 1–37. DOI 10.1186/s12889-020-08572-1. [Google Scholar] [CrossRef]
21. Khouja, J. N., Munafò, M. R., Tilling, K. (2019). Is screen time associated with anxiety or depression in young people? results from a UK birth cohort. BMC Public Health, 19(1), 82. DOI 10.1186/s12889-018-6321-9. [Google Scholar] [CrossRef]
22. Wang, X., Li, Y., Fan, H. (2019). The connections between screen time-based sedentary behavior and depression: A systematic review and meta-analysis. BMC Public Health, 19(1), 1524. DOI 10.1186/s12889-019-7904-9. [Google Scholar] [CrossRef]
23. Zink, J., Belcher, B. R., Imm, K., Leventhal, A. M. (2020). The relationship between screen-based sedentary behaviors and symptoms of depression and anxiety in youth: A systematic review of moderating variables. BMC Public Health, 20(1), 472. DOI 10.1186/s12889-020-08572-1. [Google Scholar] [CrossRef]
24. Kremer, P., Elshaug, C., Leslie, E., Toumbourou, J. W., Patton, G. C. et al. (2014). Physical activity, leisure-time screen use and depression among children and young adolescents. Journal of Science and Medicine in Sport, 17(2), 183–187. DOI 10.1016/j.jsams.2013.03.012. [Google Scholar] [CrossRef]
25. Hume, C., Timperio, A., Veitch, J., Salmon, J., Crawford, D. et al. (2011). Physical activity, sedentary behavior, and depressive symptoms among adolescents. Experimental Aging Research, 8, 152–156. DOI 10.1016/j.jsams.2009.10.297. [Google Scholar] [CrossRef]
26. Maras, D., Flament, M. F., Murray, M. (2015). Screen time is associated with depression and anxiety in Canadian youth. Preventive Medicine, 73, 133–138. DOI 10.1016/j.ypmed.2015.01.029. [Google Scholar] [CrossRef]
27. Shochat, T., Cohen-Zion, M., Tzischinsky, O. (2014). Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Medicine Reviews, 18(1), 75–87. DOI 10.1016/j.smrv.2013.03.005. [Google Scholar] [CrossRef]
28. Sampasa-Kanyinga, H., Colman, I., Goldfield, G. S. (2020). Combinations of physical activity, sedentary time, and sleep duration and their connections with depressive symptoms and other mental health problems in children and adolescents: A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 17(1), 72. DOI 10.1186/s12966-020-00976-x. [Google Scholar] [CrossRef]
29. Conklin, A. I., Yao, C. A., Richardson, C. G. (2018). Chronic sleep deprivation and gender-specific risk of depression in adolescents: A prospective population-based study. BMC Public Health, 18(1), 724. DOI 10.1186/s12889-018-5656-6. [Google Scholar] [CrossRef]
30. Lovato, N., Gradisar, M. (2014). A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Medicine Reviews, 18(6), 521–529. DOI 10.1016/j.smrv.2014.03.006. [Google Scholar] [CrossRef]
31. Bao, R., Chen, S. T., Wang, Y. (2020). Sedentary behavior research in the Chinese population: A systematic scoping review. International Journal of Environmental Research and Public Health, 17(10), 3576. DOI 10.3390/ijerph17103576. [Google Scholar] [CrossRef]
32. Chen, S. T., Liu, Y., Tremblay, M. S. (2020). Meeting 24-h movement guidelines: Prevalence, correlates and the relationships with overweight and obesity among Chinese children and adolescents. Journal of Sport and Health Science, 10(3349–359. DOI 10.1016/j.jshs.2020.07.002. [Google Scholar] [CrossRef]
33. Shen, H., Yan, J., Hong, J. T. (2020). Prevalence of physical activity and sedentary behavior among Chinese children and adolescents: Variations, gaps, and recommendations. International Journal of Environmental Research and Public Health, 17(9), 3066. DOI 10.3390/ijerph17093066. [Google Scholar] [CrossRef]
34. Kovacs, M. (2003). Children’s depression inventory. New York: Multi-Health Systems. [Google Scholar]
35. Wu, W., Lu, Y., Tan, F., Yao, S. (2010). Reliability and validity of the Chinese version of children’s depression inventory. Chinese Mental Health Journal, 24(10), 775–779. DOI 10.3969/j.issn.1000-6729.2010.10.014. [Google Scholar] [CrossRef]
36. Liu, Y., Wang, M., Tynjälä, J. (2010). Test-retest reliability of selected items of health behaviour in school-aged children (HBSC) survey questionnaire in Beijing, China. BMC Medical Research Methodology, 10(1), 73. DOI 10.1186/1471-2288-10-73. [Google Scholar] [CrossRef]
37. Liu, J., Liu, C. X., Wu, T., Liu, B. P., Jia, C. X. et al. (2019). Prolonged mobile phone use is associated with depressive symptoms in Chinese adolescents. Journal of Affective Disorders, 259, 128–134. DOI 10.1016/j.jad.2019.08.017. [Google Scholar] [CrossRef]
38. Ng, K. C., Wu, L. H., Lam, H. Y. (2020). The relationships between mobile phone use and depressive symptoms, bodily pain, and daytime sleepiness in Hong Kong secondary school students. Addictive Behaviors, 101, 105975. DOI 10.1016/j.addbeh.2019.04.033. [Google Scholar] [CrossRef]
39. Vidal, C., Lhaksampa, T., Miller, L., Platt, R. (2020). Social media use and depression in adolescents: A scoping review. International Review of Psychiatry, 32(3), 235–253. DOI 10.1080/09540261.2020.1720623. [Google Scholar] [CrossRef]
40. Mathers, M., Canterford, L., Olds, T., Hesketh, K., Ridley, K. et al. (2009). Electronic media use and adolescent health and well-being: Cross-sectional community study. Academic Pediatrics, 9(5), 307–314. DOI 10.1016/j.acap.2009.04.003. [Google Scholar] [CrossRef]
41. Ohannessian, C. M. (2009). Media use and adolescent psychological adjustment: An examination of gender differences. Journal of Child and Family Studies, 18(5), 582–593. DOI 10.1007/s10826-009-9261-2. [Google Scholar] [CrossRef]
42. Ohannessian, C. M. (2018). Video game play and anxiety during late adolescence: The moderating effects of gender and social context. Journal of Affective Disorders, 226, 216–219. DOI 10.1016/j.jad.2017.10.009. [Google Scholar] [CrossRef]
43. Wu, X., Bastian, K., Ohinmaa, A., Veugelers, P. (2016). Influence of physical activity, sedentary behavior, and diet quality in childhood on the incidence of internalizing and externalizing disorders during adolescence: A population-based cohort study. Annals of Epidemiology, 28(2), 86–94. DOI 10.1016/j.annepidem.2017.12.002. [Google Scholar] [CrossRef]
44. Houghton, S., Hunter, S. C., Rosenberg, M. (2015). Virtually impossible: Limiting Australian children and adolescents daily screen based media use. BMC Public Health, 15(1), 5. DOI 10.1186/1471-2458-15-5. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |