
 | International Journal of Mental Health Promotion | 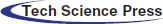 |
DOI: 10.32604/ijmhp.2022.019829
REVIEW
Virtual Reality Neurorehabilitation
1Department of Game Design, Faculty of Arts, Uppsala University, Uppsala, SE 75105, Sweden
2College of Computer Science and Technology, Qingdao University, Qingdao, 266071, China
*Corresponding Author: Zhihan Lv. Email: lvzhihan@gmail.com
Received: 18 October 2021; Accepted: 24 December 2021
Abstract: The present work investigates the application of virtual reality (VR) technology to neurorehabilitation. By consulting a wealth of data, the advantages of VR in neurorehabilitation are introduced, followed by the application status of VR in the rehabilitation of stroke patients, Parkinson’s patients, mental and psychological diseases. Besides, many research experiments on the application of VR technology in rehabilitation medicine at the present stage are investigated. The results indicate that compared with traditional balance training, the VR-based neurological rehabilitation training method can more effectively ease the tilt degree and strengthen the trunk control ability and balance function of patients with post-stroke tilt syndrome. When the effect of traditional rehabilitation training on the gait and balance of Parkinson’s patients is not good enough, VR-based rehabilitation training can at least be used as an alternative therapy. Moreover, VR games have made great breakthroughs in promoting limb rehabilitation and brain injury rehabilitation, which is of incredible benefit to those with motor and activity disorders. It is also beneficial to the treatment and recovery of mental disorders of patients with nerve injury. Although VR still has limitations such as high cost and technical breakthrough bottleneck, it has great advantages in relieving pain, enhancing interest, and recovering patients’ mental health in neurological rehabilitation training.
Keywords: Virtual reality; neurorehabilitation; stroke patients; Parkinson’s patients; virtual reality games
With the joint promotion of national policies, capital, and technology, rehabilitation medicine has become a substantial part of modern medicine worldwide. With the continuous influence of foreign experience in the development of rehabilitation medicine, the continuous improvement and opening of domestic policies of China, new models and new technologies of rehabilitation medicine emerge in an endless stream [1]. The disease spectrum changes from the aging of China’s population, the rehabilitation demand of seniors for high-risk diseases, and the demand due to chronic disease disabilities continuously expand the application range of the rehabilitation medical industry. Based on traditional medical concepts, the precision rehabilitation medical system integrates modern information technologies and intelligent network platforms, such as the medical Internet of Things, telemedicine, and big data intelligent decision engine. These devices perceive and monitor human life characteristics through embedded wearable devices, collect and return information related to rehabilitation, and offer medical intervention information and treatment plan [2–4]. In the process of diagnosis and treatment, the big data intelligent decision engine performs data analysis and mining, mathematical simulation, and image analysis to obtain or transmit information, diagnose and evaluate disease risk, make intelligent judgments and decisions, and display and provide intervention measures.
Digital precision rehabilitation medical system is an expert system established through high-tech means. It is the extension and amplification of human wisdom in the medical field through machines and artificial intelligence (AI). Wang et al. [5] investigated the information demands for Coronavirus Disease 2019 (COVID-19) in Chinese Online Health Communities (OHCs). Specifically, they conducted topic mining and data analysis based on the questions and answers about COVID-19 in six Chinese OHCs. Virtual Reality (VR) is a technology that produces virtual effects for the human senses. It has been extensively used in the field of rehabilitation therapy [6], such as cognitive rehabilitation including attention deficit, spatial perception disorder, and memory disorder, rehabilitation of mental diseases such as anxiety, depression, and phobia, and rehabilitation of motor disorders such as poor balance and coordination ability. These applications have achieved excellent rehabilitation effects [7] and draw much attention from related scholars, especially in the field of neurological rehabilitation. Imbimbo et al. [8] noticed that the cognitive reserve (CR) might influence the rehabilitation outcome, helping to address the patient toward technological or conventional rehabilitation. Therefore, they investigated how CR affected motor rehabilitation outcomes in Parkinson’s patients who underwent VR rehabilitation, aimed at improving walking and balance. Clark et al. [9] evaluated the effectiveness of robots and VR technologies for neurorehabilitation of stroke survivors. Before considering the combination of these techniques and the complexity of the evaluation of rehabilitation outcomes, the authors examined each rehabilitation technique in turn. They found that there was high-quality evidence supporting that upper-limb robotic rehabilitation technology could improve the movement, strength, and activities of daily life; moreover, VR training (VRT) allowed the creation of the most applicable practical environment and incorporation into computer-generated multi-sensory images. Lee et al. [10] investigated the upper limb function and quality of life of community residents with chronic hemiplegia in a virtual training program based on Rapael smart gloves [11]. They selected 36 outpatients who were diagnosed with their first stroke to receive a therapeutic rehabilitation program at the local rehabilitation unit, and randomly assigned participants to a non-immersive VRT (intervention) group and a recreational activity (control) group. Their experimental results indicated that after completing the non-immersive VRT, the intervention group showed a significantly higher Wolf Motor Function Test (WMFT) score. Choi et al. [12] explored the effect of wearable multi-inertial sensing VR rehabilitation systems in improving the upper limb function of children with brain injury. They experimented to evaluate 80 children with brain injuries, including patients with cerebral palsy between the ages of 3 and 16, and implemented 30 minutes of VR intervention and 30 minutes of conventional occupational therapy on the intervention group. Their experimental result showed that the VR group had more significant improvements in upper limb dexterity, the performance of daily living, and forearm supination (p < 0.05).
In summary, the application of VR in rehabilitation therapy has been proven to have brilliant effects. Although conventional occupational therapy is effective for upper limb training, VR has advantages in enhancing flexibility, activities of daily living, and active forearm supination, and has significant effects on children with more severe dyskinesias. VR can be used as an auxiliary means of medical rehabilitation in the future.
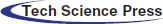
VR uses an interactive simulation created by computer hardware and software to generate an artificial environment through a computer, giving people an immersive feeling [13]. VR can also provide participants with the opportunity to participate in an environment that has a similar look and feel to real-world objects and events. Participants interact with the projected images, manipulate virtual objects, perform activities in the task program, and receive various forms of feedback through the environment, the most common being visual and auditory feedback, and real-time feedback and instant effects. This provides diverting experience for people in movement study [14]. The application fields of VR are becoming even more extensive. For example, simulated tourism through VR technology can help people set more reasonable tourism routes in reality, liberate cultural relics from geographical restrictions, and display global scenic spots and historical sites stereoscopically. In addition, an interactive three-dimensional (3D) shopping environment can be generated through VR, which breaks through the limitations of time and space [15]. VR can also change the traditional game mode using keyboard, mouse, and fingers, allowing players to play games with their heads, hands, feet, and even the entire body [16]. At present, VR technology has been successfully integrated into many fields such as medicine, psychology, and rehabilitation, and it has been proved to have an active role in the treatment of balance disorders caused by various neurological diseases. Fig. 1 shows the application of VR technology in various fields.
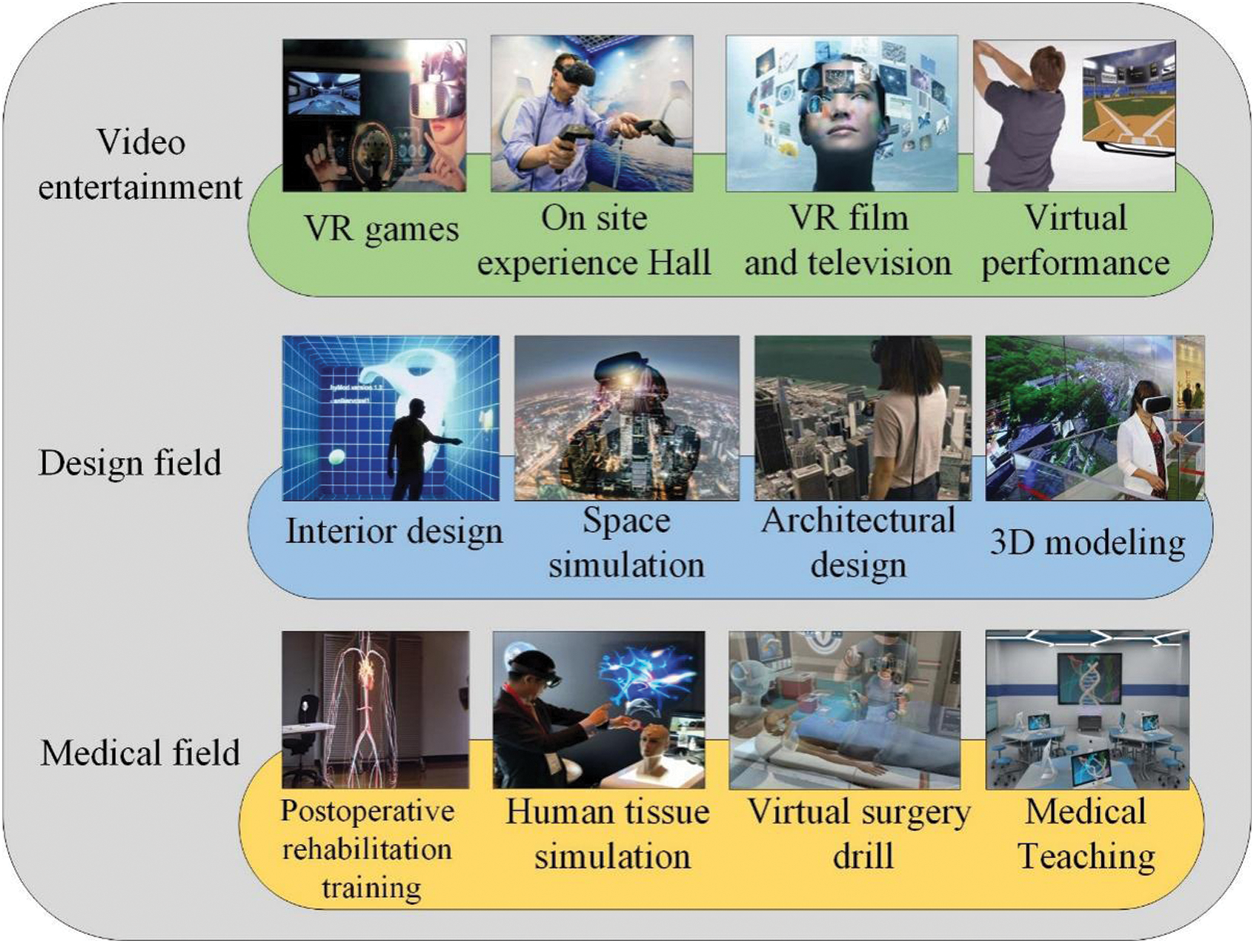
Figure 1: VR technology application field
2.1 Advantages of VR in Rehabilitation
VR rehabilitation has the following advantages in terms of training intensity and rehabilitation motivation. It can stimulate patients’ participation by improving game elements to increase entertainment. Besides, it can increase the repetitiveness of the task by assigning the rules of the game to a task to encourage patients to participate. Flexible and individualized rehabilitation schemes can also be formulated by VR rehabilitation according to the patient’s motor dysfunction to realize gradual rehabilitation. Moreover, VR can provide real-time feedback during exercise and increase participation and pleasure in rehabilitation tasks of patients [17–19]. The VR rehabilitation system can be used as an auxiliary treatment for routine rehabilitation without the direct supervision of the therapist, as well as a remote or home rehabilitation tool, such as VR game consoles and rehabilitation robots. Furthermore, utilizing motion sensors combined with a scene simulation system for rehabilitation training in VR scenes can realize the evaluation and tracking of patients’ motion functions.
A general VR device is equipped with at least a screen, a set of sensors, and a set of computing components. Fig. 2 shows the composition of VR equipment. The screen can display the analog image projected onto the user’s retina. Sensors can sense the user’s rotation angle. The computing component collects sensor data and determines what is displayed on the screen [20]. During physical rehabilitation, the patient’s body shape change and position movement must be captured by the motion tracking sensor and simultaneously transmitted to the virtual object in VR [21]. Sensors that track patient motion must have accessories with motion visualization functions, including mice, joystick, depth-sensing cameras [22], electromagnetic sensors [23], inertial sensors, bending sensors, and data gloves. Sensor technology to identify movement is also crucial in VR rehabilitation.

Figure 2: Composition of VR equipment
There are wearable VR devices and non-wearable VR devices for recognizing upper limb rehabilitation exercises [24]. Non-wearable devices include vision sensors and robot-based controllers or three-degree-of-freedom controllers (used alone or in combination). Wearable devices cover devices that use data gloves and devices that use the exoskeleton. Sensing cameras in non-wearable devices have been upgraded from web cameras that track markers or color patches to depth-sensing cameras that track body or hand signals. In this way, the user’s movement can be perceived without obstacles in a limited space.
3 Application Status of VR in Neurorehabilitation
3.1 Application of VR in Stroke Rehabilitation
Stroke is one of the main causes of adult disability. Due to various dysfunctions secondary to stroke, many stroke patients are unable to take care of themselves completely in life. In addition to having a serious impact on the quality of life of patients, it also brings a heavy burden to their families and society [25–27]. Stroke has caused many disabilities and a tremendous socio-economic burden worldwide. Although the incidence of age-standardized stroke has declined in most regions, the incidence of stroke due to an aging population has increased. There are about 2 million new stroke patients in China each year, and 70% to 80% of them cannot live independently because of disability. Peng et al. [28] constructed a model based on hybrid feature selection and XGBoost for hypertension detection and prediction. After successfully using Lasso regression to identify factors related to hypertension, they used the XGBoost model to predict hypertension. Stroke is prone to cause various life dysfunctions in patients after surgery. For example, many patients suffer from tilt syndrome with balance disorders during the acute phase of stroke recovery. Moreover, the severity of balance disorder is also related to the severity of the disability of stroke patients.
In the process of rehabilitation training, functional training and specific task training are the key elements of treatment, designed to help stroke patients restore motor control and achieve normal functional movement patterns [29]. Rehabilitation training for stroke patients focuses on the affected limbs or bilateral symmetrical movement through exercise reeducation to effectively improve the movement control and strength of the patient’s body and limbs [30]. Based on the theory of motor learning, task-oriented intensive training, i.e., more doses and exercises and repetitive training, can promote neuroplasticity, thereby promoting sports recovery. Meanwhile, the rehabilitation of stroke patients is usually carried out in standardized treatment rooms and clinical environments. These sites are more monolithic than outdoor environments and lack complex individual and community settings to meet the multitasking needs of stroke patients. VRT aims to improve neuroplasticity by providing a safe and enriching environment and increasing the number of repetitions, exercise intensity, and motivation to comply with interventions when performing specific functional tasks. Fig. 3 reveals the intervention process of VR rehabilitation of stroke patients commonly used in rehabilitation training centers in China.
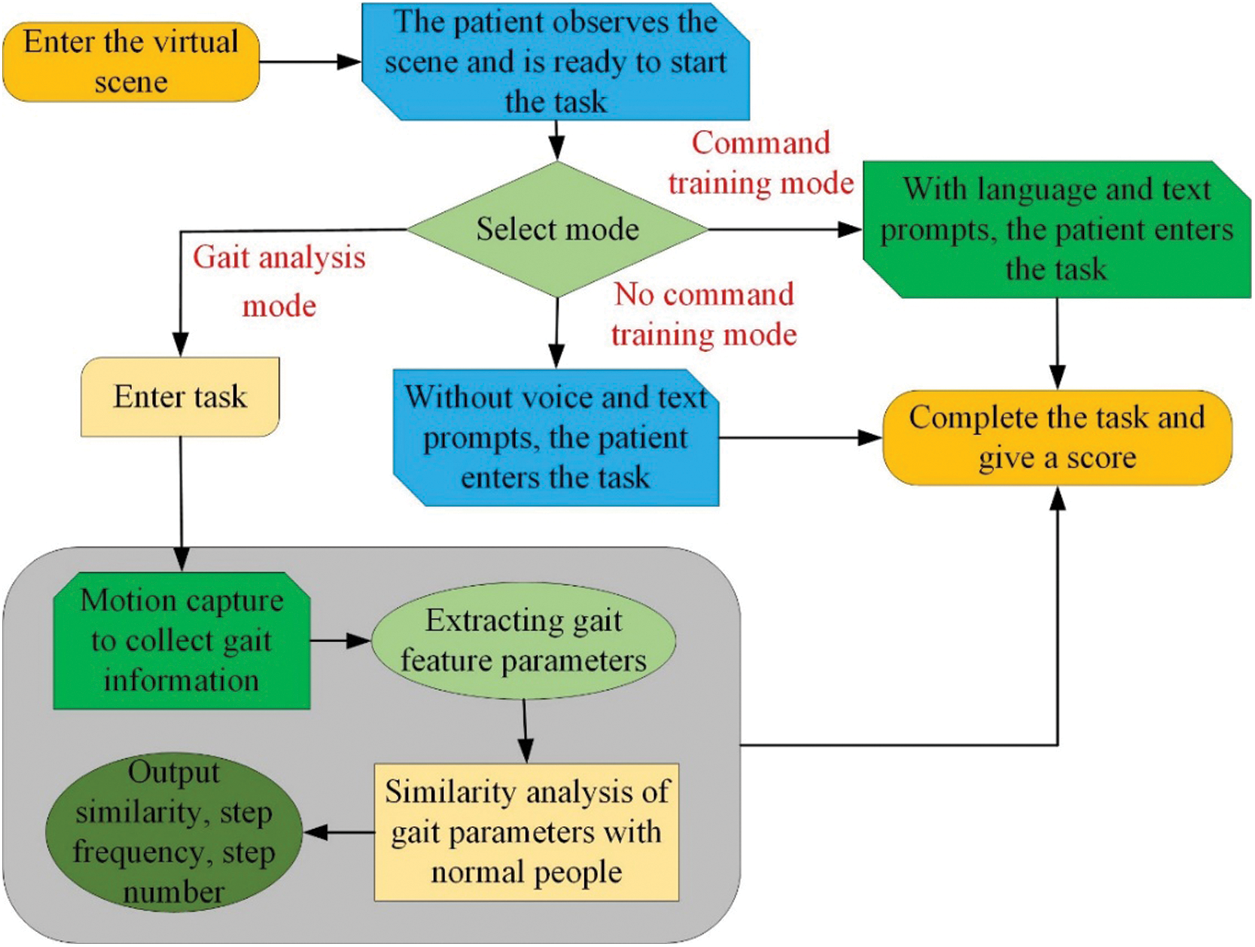
Figure 3: The intervention process of VR in rehabilitation treatment of stroke patients
3.1.1 Effect of VR on the Balance Function of Patients with Post-Stroke Tilt Syndrome
Tilt syndrome–Pusher Syndrome (PS) [31] is a serious postural control disorder that occurs during the recovery from brain injury. It is characterized by the patient leaning to the affected side under various postures (e.g., sitting and standing) and obstructing the correction of weight transfer to the midline of the body or across the midline to the non-paralyzed side. In addition to poor sitting balance and standing balance, they also have a reduced ability to turn, transfer, and walk. Studies have shown that 5% to 63% of stroke patients will exhibit tilt syndrome, and PS seriously affects the patient’s balance ability.
Robot-assisted gait training provides huge therapeutic advantages for functional activities of posture control [32]. Park et al. [33] studied the impact of robot-assisted gait training using VR and auditory stimulation on the balance and gait ability of stroke patients. The authors randomly divided all subjects into three groups. Among them, 12 subjects consisted of a VR robot-assisted gait training (VRGT) group [34], 12 subjects were in the Auditory Robot Gait Training (ARGT) group, and 16 subjects were in the control group. The subjects received VR and auditory stimulation, meanwhile received robot-assisted gait training for 45 min each time, 3 times a week for a total of 6 weeks, and received general physical therapy for 30 min, five times a week for 6 weeks. Experimental results showed that the Berg balance scale [35], timed up and go test [36], and 10-meter walk test [37] scores significantly improved post-intervention (p < 0.05). Berg Balance Scale. This proved that the balance and gait ability after VRGT were improved compared with general physical therapy, and it was found to effectively enhance the functional activity of stroke patients.
De Luca et al. [38] utilized the interactive semi-immersive program (I-SIP) [39] and BTs-Nirvana’s VRT [40] to affect the cognitive function recovery of stroke patients. The authors randomly divided 12 subjects into two groups, namely the experimental group and the control group. The experimental group received BTs-Nirvana VRT, while the control group received standard cognitive therapy. Besides, both groups received the same routine physical therapy plan. Each course lasted 45 min and was repeated 3 times a week for 8 weeks. The experimental group showed greater improvement in trunk control test (p = 0.03), Montreal cognitive assessment (p = 0.01), selective attention assessment score (p = 0.01), language memory (p = 0.03), etc. They concluded that VRT and I-SIP were useful supplementary treatments, which could promote the functional recovery of stroke patients in attention, visual space defects, and motor function [41,42].
Qian et al. [43] studied the impact of VR-based exercise on the physical, psychological, and rehabilitation outcomes of different groups of people. Through 9 databases including Academic Search Premier and PubMed, they retrieved 246 articles with keywords such as VR, Sport Intervention, Physiology, Psychology, and Rehabilitation. They found that four articles studied the impact on psychological outcomes, and three showed positive effects. For example, VR exercise could relieve fatigue, tension, and depression, promote calm, and improve the quality of life. Besides, nine articles investigated the effects of VR-based exercise on physical and/or psychological outcomes of rehabilitation, and six articles observed significant positive changes. In detail, patients suffering from chronic stroke, hemodialysis, spinal cord injury, early cerebral palsy, and cognitive decline usually used VR-based exercise to get improvement.
Therefore, rehabilitation training based on VR technology can effectively ameliorate the tilt degree, trunk control ability, and balance function of patients with post-stroke tilt syndrome than traditional balance training, and significantly improve the depression status of patients. Furthermore, compared with traditional sports, VR sports may have a positive impact on the individual’s physical, psychological, and rehabilitation results.
3.1.2 Effect of VR on the Functional Recovery of Upper Limbs after Stroke
In the early 20th century, the theory of rehabilitation medicine based on neurophysiology was extensively developed. Correspondingly, a series of related treatment methods have emerged, such as Proprioceptive Neuromuscular Facilitation [44], Brunnstrom therapy [45], Bobath therapy [46], multiple sensory stimulation therapy, and Motor Relearning Program [47]. With the progress of neuroplasticity research, treatment methods have also undergone rapid changes based on the theoretical basis of neurological function reorganization, such as compulsory exercise therapy, Constraint-induced Movement [48], and Mirror therapy [49]. These treatment methods have been widely used in the clinical rehabilitation of upper limb function of stroke patients. There are also many research advances in VR technology in the recovery of upper limb function of stroke patients.
Kim [50] studied the impact of VR rehabilitation programs on upper limb function and daily living activities of stroke patients. The subjects were randomly divided into an experimental group with a VR rehabilitation plan and a control group receiving traditional occupational therapy. The intervention was applied five times a week for 30 min each time for six weeks. The scholars conducted the Jebsen-Taylor hand function test [51] to measure the subjects’ manual function test, check the upper limb function before and after the treatment intervention, and calculate the Barthel index to observe their daily activities. The results showed that after the intervention, the upper limb function and activities of daily living of the two groups of participants were significantly improved (p < 0.05). Besides, the improvement of these parameters of participants in the VR rehabilitation program was incredibly greater than that of the control group.
Kim et al. [52] focused on the effect of the new rehabilitation system Rapael smart gloves [53] on the upper limb recovery of patients with subacute stroke. They recruited 41 subacute stroke patients with hemiplegia to receive 40 treatments over four weeks, five times a week for one hour a day. The experimental group took each lesson includes 30 min of training using smart gloves and 30 min of training using conventional Occupational Therapy (OT) [54]. The control group received regular OT for 60 minutes every day. The authors performed the functional evaluation and functional near-infrared spectroscopy measurement before the intervention, immediately after the intervention, and 1 month after the intervention, and repeatedly measured variance for statistical analysis. Results indicated that the experimental group obtained higher scores than the control group (p < 0.05) in all sub-tests of the Failure Mode Analysis [55] of upper limb parameters and the Jebsen-Taylor hand function test [56].
Song et al. [57] evaluated the effect of a virtual training program using Rapael smart gloves on the upper limb function of stroke survivors with chronic hemiplegia. They selected ten chronic hemiplegic stroke survivors who were diagnosed with their first strokes for treatment and rehabilitation at the rehabilitation center. All participants used the VR program with Rapael smart gloves for 30 min 3 days a week for 8 weeks. They also received the regular OT for 40 min 3 days a week for 8 weeks as additional therapy. After completing the eight-week intervention, all participants had improved WMFT [58], Jebsen-Taylor hand function test, grip strength, and cross-country scores compared to their respective baseline before the intervention.
Therefore, VR technology combined with task-oriented training can improve the upper limb function and daily living skills of stroke patients, bringing about a better treatment effect task-oriented training.
3.2 Application of VR Technology to Recovery from Parkinson’s Disease (PD)
PD can impair the movement and coordination of people. More than 10 million people worldwide are affected by it. Approximately 60,000 Americans are diagnosed with PD each year, and by 2020, there were nearly 1 million Parkinson’s patients. Parkinson’s patients may face challenges in vision, cognition, and mobility with the development of the disease and the side effects of certain drugs. Visual impairment can make it difficult to distinguish objects, perceive depth, and safely manipulate space. Changes in cognitive abilities may make previously automated tasks (such as walking) more troublesome [59,60]. Although drug treatment can delay the progression of PD, many patients eventually develop limb motor dysfunction, especially limb balance disorder. These limb dyskinesias can lead to patients with reduced fine movement ability, limited motor ability, and reduced self-care ability, seriously affecting the patient’s quality of life. The rehabilitation treatment methods for PD include physical therapy, OT, and walking training. The gait test process of rehabilitation therapy for Parkinson’s patients frequently adopted by the National Rehabilitation Medical Center is shown in Fig. 4. Some new treatments are emerging, such as motor imagery therapy, behavioral observation therapy, VR, rehabilitation robots, and game training.
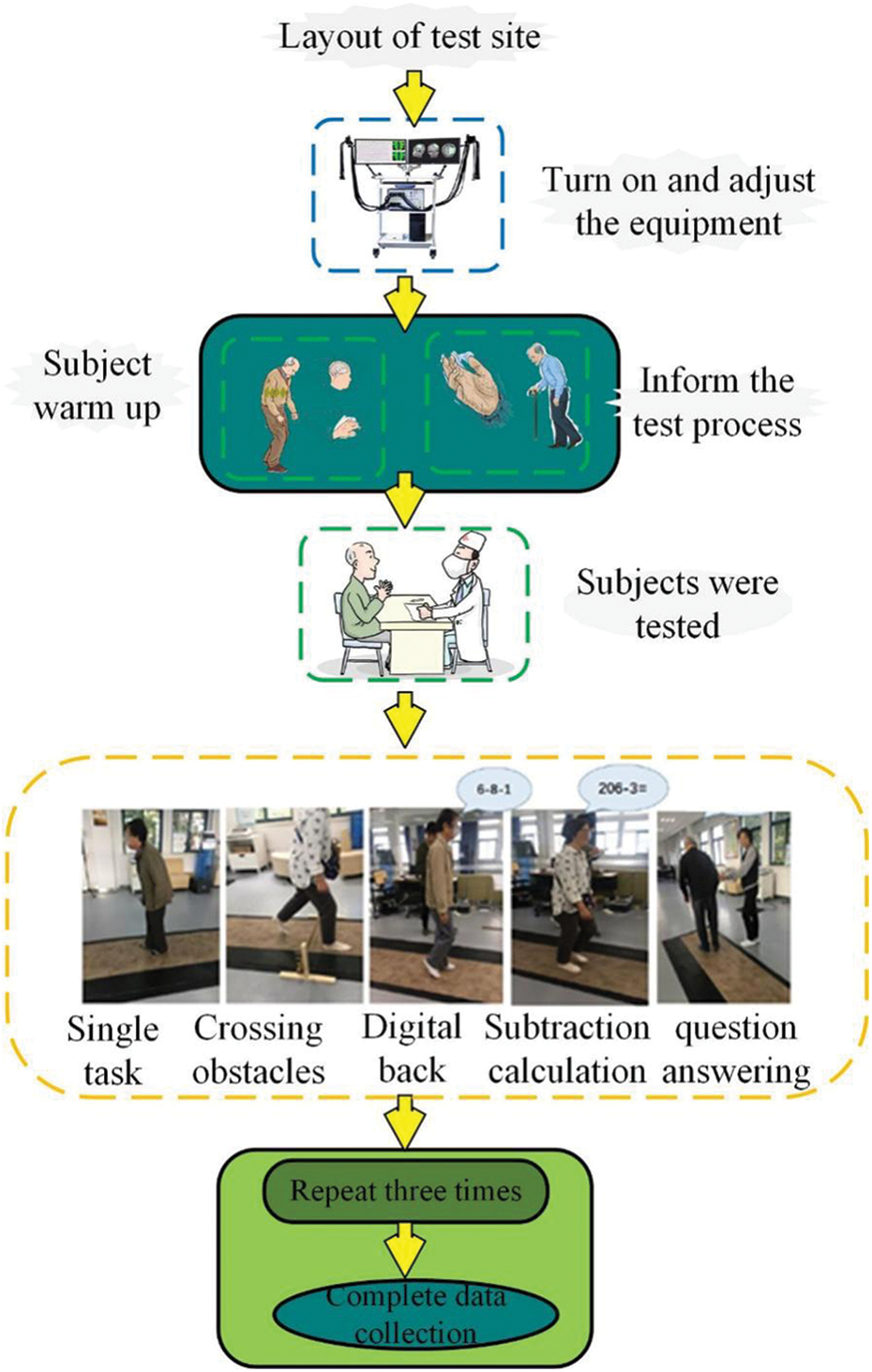
Figure 4: Gait test process of the rehabilitation treatment for Parkinson’s patients
In recent years, VR, as a therapeutic tool, has become a new topic in neurorehabilitation research. Lei et al. [61] pointed out that from the perspective of kinesiology learning, VR provided the possibility of high-intensity, task-oriented, multi-sensory feedback training, which could promote the visual, auditory, and tactile input of patients and increase the patient’s interest in the rehabilitation process. Besides, the immersive or non-immersive virtual environment could effectively improve the patient’s treatment compliance. At this stage, VR technology has become a promising tool for the research and rehabilitation of Parkinson’s patients with gait and balance disorders, because it allows users to participate in a rich and highly personalized complex environment [62]. Canning et al. [63] reviewed the basic principles and evidence for the use of VR in the evaluation and rehabilitation of patients with PD, made recommendations for future research, and discussed the use of VR in clinical practice. In the assessment of Parkinson’s patients, VR has been used to manipulate the environment to enhance research into the behavioral and neural basis of gait and balance, and to improve the understanding of the motor cognitive neural circuits involved.
Maggio et al. [64] evaluated the effect of using the BTS-Nirvana (BTS-N) system [65] for VRT on the cognitive and behavioral recovery of Parkinson’s patients. BTS-N is a semi-immersive treatment system for sports and cognitive rehabilitation of patients with neurological diseases by creating virtual scenes that patients can interact with. The authors recruited 20 Parkinson’s patients undergoing neurorehabilitation therapy and randomly divided them into 2 groups, i.e., the experimental group used BTS-N for semi-immersive VRT, and the control group received traditional cognitive training. They evaluated each participant before and immediately after the end of each training that was performed three times a week, lasting 60 min for 8 weeks, with a total of 24 times in each group. They ultimately found that compared with the control group, the experimental group had greater improvement in cognitive function in terms of executive and visuospatial ability. The results of the study indicated that rehabilitation through new VR instruments might be a valuable tool for improving the cognitive and behavioral outcomes of Parkinson’s patients.
VR is a common intervention for the rehabilitation of patients with neurological disorders. Chen et al. [66] determined the short-term effect of VR on balance and compared it with the effect of active intervention in Parkinson’s patients. The authors conducted fourteen randomized controlled trials, including 574 individuals eligible for qualitative analysis, of which 12 studies involving 481 individuals were identified as eligible for meta-analysis. Analysis results showed that compared with active intervention, VR improved the Berg balance scale score (mean difference = 1.23; 95% CI = 0.15 to 2.31; I2 = 56%). After sensitivity analysis, the results of dynamic gait index and functional gait assessment were also significant (mean difference = 0.69; 95% CI = 0.12 to 1.26; I2 = 0%). Both provide moderate statistical evidence. However, the Timed Up & Go Test (TUGT) and the Activities-Specific Balance Confidence Scale did not differ significantly. They concluded that existing moderate evidence of the effectiveness of VR with the Berg Balance Scale, Dynamic Gait Index, and Functional Gait Assessment for individuals with PD was promising. Moreover, although these differences did not reach the clinically important threshold of change, VR was comparable to active interventions and could be regarded as adjuvant therapy for the balanced rehabilitation of patients with PD.
Lina et al. [67] evaluated the influence of VR on balance, motor function, gait, and ability of daily living activities of Parkinson’s patients. The authors independently screened related articles for inclusion, extracted data, and evaluated quality, included 12 randomized clinical trials involving 360 patients with PD. They found that VR could improve balance, measured by the Berg balance scale (fixed model weighted average difference = 2.28, 95% CI = 1.39 to 3.16, p < 0.00001); strengthens motor function, evaluated by TUGT (fixed Model weighted average difference = –1.66, 95% CI = –2.74 to 0.58, p = 0.003); passed the 10-meter walking test time (fixed model weighted average difference = 0.13, 95% CI = 0.02 to 0.24, p = 0.02) evaluation Gait ability of patients with PD. Moreover, VR could improve the ability of individuals to perform activities of daily living, assessed by modified Barthel index [68] (fixed model weighted average difference = 2.93, 95% CI = 0.8 to 5.06, p = 0.007). These research results indicated that VR rehabilitation could help improve the balance, motor function, gait, and activities of daily living in patients with PD.
To sum up, VR rehabilitation training can achieve the same effect as traditional rehabilitation training, and has better performance in the gait and balance of Parkinson’s patients. On the whole, when traditional rehabilitation training is not good enough for the gait and balance of patients with PD, VRT can at least be used as an alternative therapy. Of course, this therapy requires a more rigorous large-sample and multi-center randomized controlled trial design to provide a stronger evidence-based basis for verifying its potential advantages.
3.3 Role of VR Games in Neurological Rehabilitation
In the ever-changing technological era, the trend of VR is undoubted. It can improve the sound, stage, and game effects to the extreme, and bring the audience a new audio-visual experience. It has been noticed that VR, which has emerged in concerts by major domestic and foreign artists, adds a sense of technology to the gorgeous stage. VR is also a human-computer interaction (HCI) technology currently used to assist disease treatment. It is a computer simulation system that can create a virtual world. The 3D digital model composed of computer graphics is compiled into the computer to create a realistic virtual environment and make users feel immersed. This is the VR immersion [69] or presence [70]. Based on the sense of presence, users can experience different identities and explore different forms of self. In traditional video games, users are mainly involved in vision and thinking. In VR technology, the users immerse themselves in the virtual environment in the form of an entire biological entity, where they can fully mobilize their visual imagination, and fully stimulate and express consciousness and emotions.
The reason why video games can assist in the treatment of diseases may be the use of psychological theories in games. Patients can vent their emotions to control their behaviors by playing games. The HCI can interfere with patients’ cognitive and behavioral skills, ease emotional and physical symptoms, and adjust immune effects accordingly, furnishing certain therapeutic effects [71,72]. Nowadays, the adjuvant therapy of video games has shown a vigorous trend worldwide, and it can play an auxiliary role in the treatment and rehabilitation of mental illness. Serious games have also made great breakthroughs in promoting physical rehabilitation and brain injury rehabilitation, which are very valuable to people with movement disorders and mobility impairments. For example, some somatosensory games can be used in VR scenes to arrange training tasks such as grasping and stepping to help Parkinson’s patients with symptoms such as limb dyskinesia and abnormal gait recover their posture and gait. In addition, VR allows epilepsy patients to control the flight path of the aircraft through brain waves when playing a flying game. This method helps to stimulate the patient to generate the trace current of normal human brain waves, and there are currently clinical application cases. Fig. 5 illustrates a summary of the methods that VR games are often used to help with upper limb rehabilitation training in Chinese rehabilitation training centers.
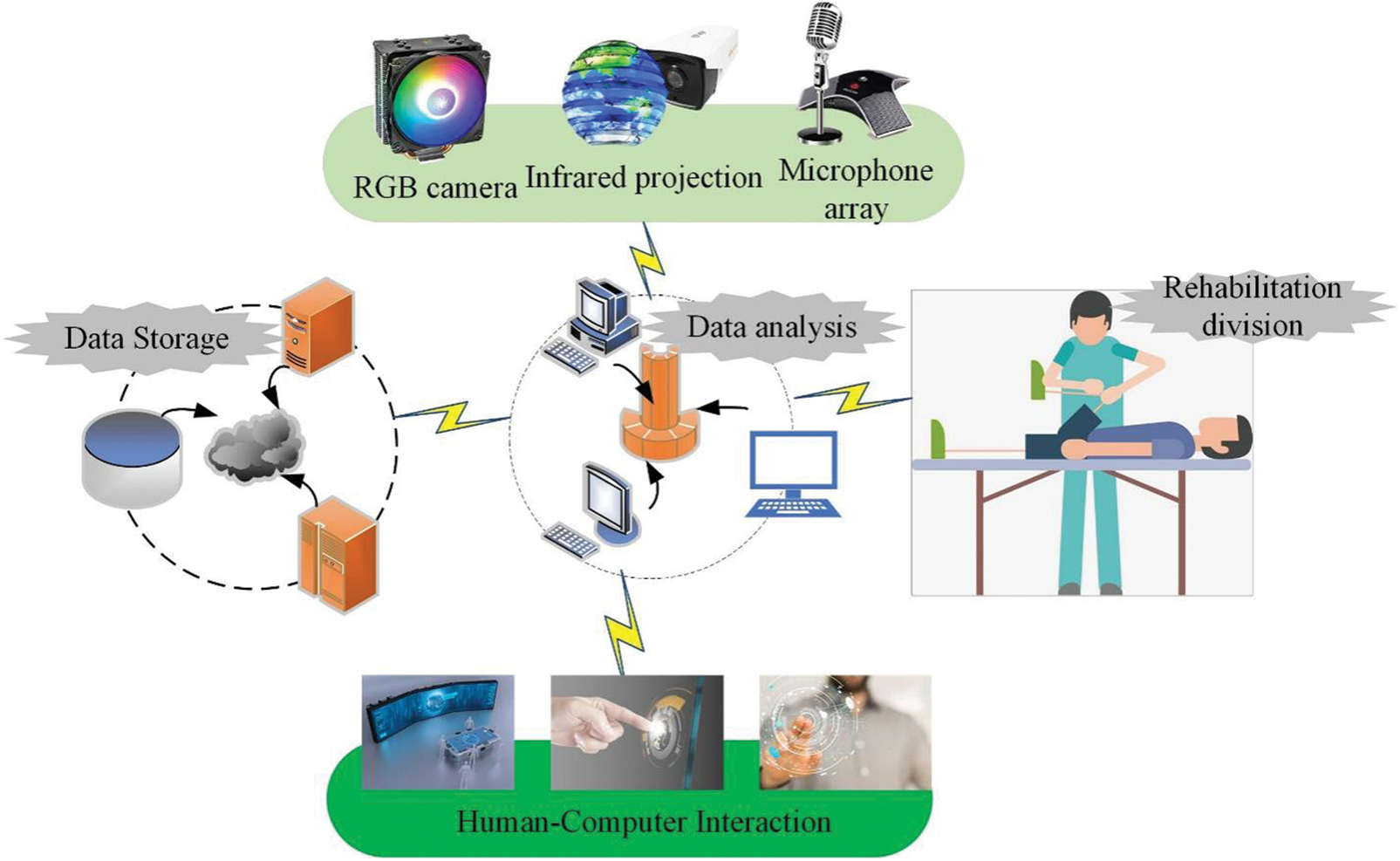
Figure 5: VR games-assisted upper limb rehabilitation training
Karamians et al. [73] compared the therapeutic effects of VR games with those of traditional physical therapy, and utilized a random-effects meta-analysis model to qualify the proportion of people recovering after rehabilitation training in VR games. They also studied studies on whether the effect of VR on neurological rehabilitation therapy was different because of the pathological characteristics or therapeutic factors of participants. They found that VR game intervention improved the rehabilitation effect up to 28.5%; when computer training involved game components rather than just visual feedback, the overall therapeutic benefit was much greater (10.8%); meanwhile, VR game intervention showed a significant therapeutic advantage over active control therapy (10.4%).
Qidwai et al. [74] explored the feasibility of Electroencephalogram (EEG) and (Electromyography) EMG combined with a VR game system in the direction of relief and rehabilitation of facial paralysis. They selected a 23-year-old female patient with facial paralysis as a single case for a 10-day exercise program (days 2–11) using immersive VR equipment, randomly launching virtual animations in an unpredictable test mode. In this experiment, they collected the EEG and EMG patterns corresponding to the upper quadrant of the face at baseline, post-intervention, and follow-up. The survey results showed that muscle activation gradually improved in response to impulsive and unpredictable activities in the virtual environment provided by immersive VR equipment. The case report found a positive correlation between VR, EMG activation in the upper quadrant of the face, and EEG pattern changes after intervention.
Loss of arm function and hand mobility can reduce the independence of activities of daily living in patients with multiple sclerosis (MS) [75]. Jonsdottir et al. [76] verified the feasibility and effectiveness of a serious game method to supervise the upper limb rehabilitation of the larger affected arm of MS patients and the cross effect on the untreated arm. They investigated eighteen people with moderate to severe MS symptoms (mean age 56.1 (range 28–73) years; average disease duration 17.6 (4–35) years). Each participant underwent 12 serious and supervised games (45 minutes, 12 times) aimed at improving the most severely affected upper limbs. The authors chose Nine Hole Peg Test [77] and Box and Blocks Test [78] for validation and used the Visual Analogue Scale [79] of EuroQual-5DL [80] to evaluate the perceived health before and after the intervention. Besides, they adopted non-parametric tests and set p to 0.05. Analysis proved that after serious game training, participants’ bilateral mobility and arm function improved (10%–18%); however, only the treatment group had a statistically significant improvement (p < 0.05). Moreover, perceived mental health improved after training (p < 0.05), but perceive physical health did not. They found that clinical interventions using the VR method of serious games had a positive impact on the arm recovery of patients with moderate to severe MS, mainly improving the treated arm, but positively affecting the untreated arm. Moreover, these people were motivated during the intervention and expressed willingness to continue this training at home as part of the continuity of care.
It is worth emphasizing that video game therapy cannot completely replace traditional medical therapy. However, video games are superior to traditional therapies in assisting the treatment of diseases. Through interesting HCI, it can increase the interest of patients and enhance the motivation of patients to treat diseases, which is conducive to disease treatment. Many patients have benefited from video game-assisted therapy. In the future, the application of video games to medical treatment will gradually become popular and expand, but its drawbacks will become increasingly obvious. It is not recommended to rely solely on one treatment for any disease problem. Reasonable adjustment of the body and mind and maintaining an optimistic attitude are the prerequisites for obtaining obvious therapeutic efficacy.
3.4 Application of VR Technology to Rehabilitation Treatment of Mental Illness
VR is a new way of HCI created by computers and the latest detection technology. In brief, VR creates a virtual world, but users think everything is real. So far, VR has not only attracted people’s attention to the field of computer graphics, but also involved a wide range of fields, including video conferencing, network technology, and distributed computing technology. In the field of collaborative design, there is a technology called VE, which allows engineers to interact with the prototypes they design in real-time.
In addition to watching movies and playing games, VR can also have a more profound impact on humans. The Virtual Human Interaction Lab of Stanford University was established about 15 years ago. Unlike other laboratories, it does not develop new technologies, but focuses on the changes in human thinking and behavior that VR technology can bring. For example, experts use VR technology to create a virtual distress scene for patients with post-traumatic stress disorder (PTSD) to guide them out of the dark mind. Persistent intrusive memories and repeated traumatic scenario dreams will bring psychological pain to patients with PTSD, especially those with childhood trauma, which will affect their lives. In the future, PTSD could be alleviated by VR technology. The subject can return to the “virtual pain site” more realistically, and even the doctor can enter the “virtual pain site” to guide and treat them through communication with the subject.
Although the development of VR in the game field is still constrained by factors such as the high cost of VR equipment, limited audiences, and lack of core VR games, domestic and foreign scholars and therapists have conducted many attempts to use VR technology to assist disease treatment. For example, VR technology has achieved rich results in the treatment of phobias, attention deficit disorder, schizophrenia, anorexia, male sexual dysfunction, and pain relief. For some diseases, it is difficult to achieve the desired results using traditional diagnostic methods or treatment methods, while video games show advantages. For instance, one of the clinical manifestations of autism is a social communication disorder, and it is often difficult for patients to understand human facial expressions in real life. In 2005, a British study found that in a cooperative VR environment, more than 90% of the subjects could accurately recognize human expressions in the virtual environment. Fig. 6 illustrates the specific VR treatment methods for mental and psychological diseases after investigation.
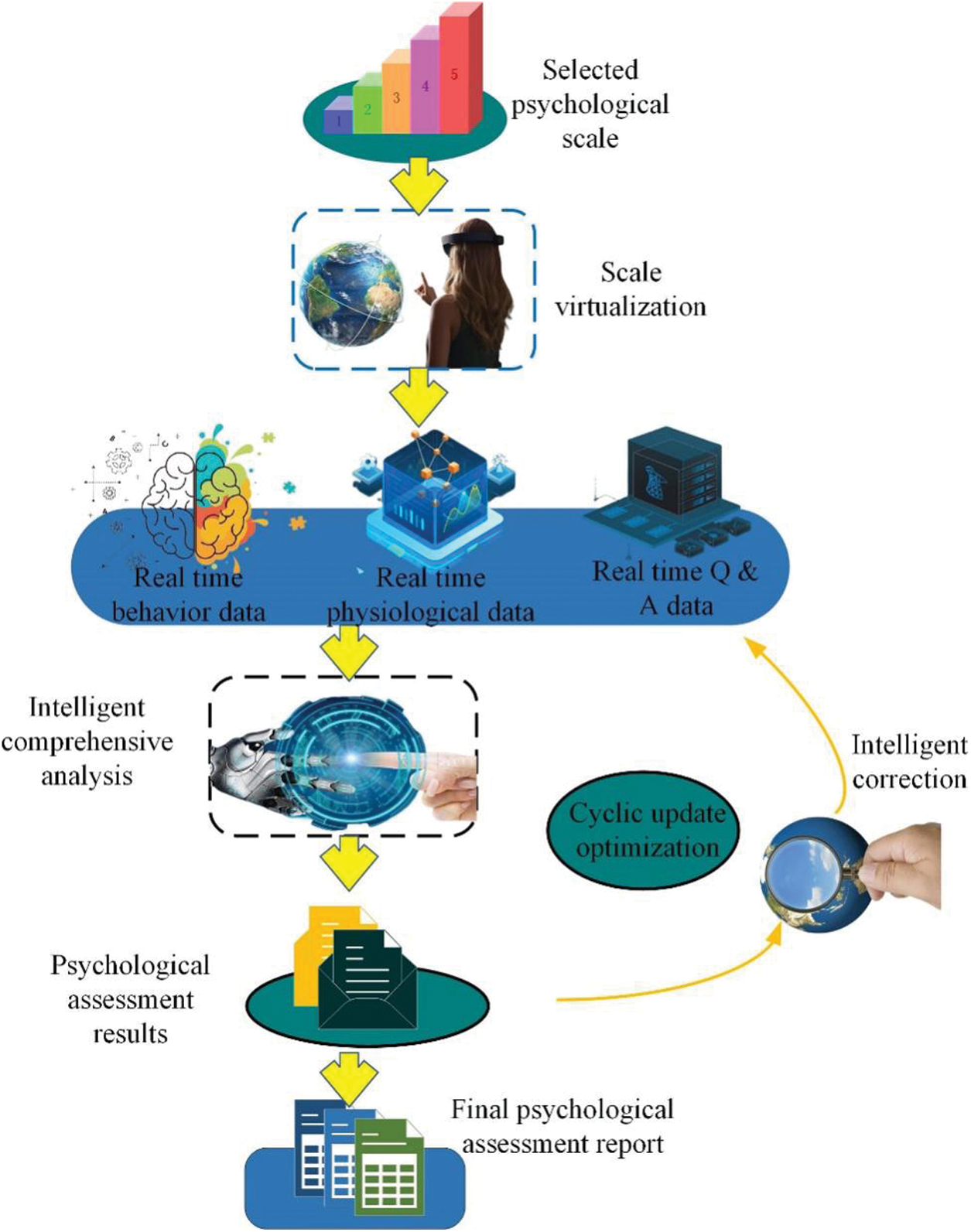
Figure 6: VR applying to the treatment of mental and psychological diseases
Another example is the diagnosis of schizophrenia. Research has found that cognitive inconsistencies can cause schizophrenic patients to misinterpret things and make wrong judgments. For example, the patient thinks that the tree is blue, the barking of the dog is made by the cow, etc. These behaviors are usually difficult to detect. Israeli researchers began to use virtual games to help patients diagnose diseases as early as possible. With the special glasses designed by the researchers, people can feel different 3D visual effects from their environment. Things in the real environment have 3D sounds, shapes, and directions, which makes cognitive inconsistencies easy to distinguish. The results show that 85% of patients with schizophrenia can be correctly predicted. In the past two decades, there has been a rapid increase in testing the effectiveness and acceptability of VR in the evaluation and treatment of mental health problems. Rus-Calafell et al. [81] investigated the application of VR to psychiatric assessment and treatment. They searched the Web of Science, PsychInfo, EMBASE, Scopus, ProQuest, and PubMed databases, and identified 638 articles that might meet the inclusion criteria, of which 50 articles were included in the review. They concluded that VR provided a valuable method to assess the presence of symptoms in an ecologically effective environment, and facilitated the learning of new emotional and behavioral responses. In summary, VR is a promising method that can be used for the assessment of neurocognitive deficits and the study of related clinical symptoms. Fig. 7 shows a mental health adjustment method using VR combined with brain waves.
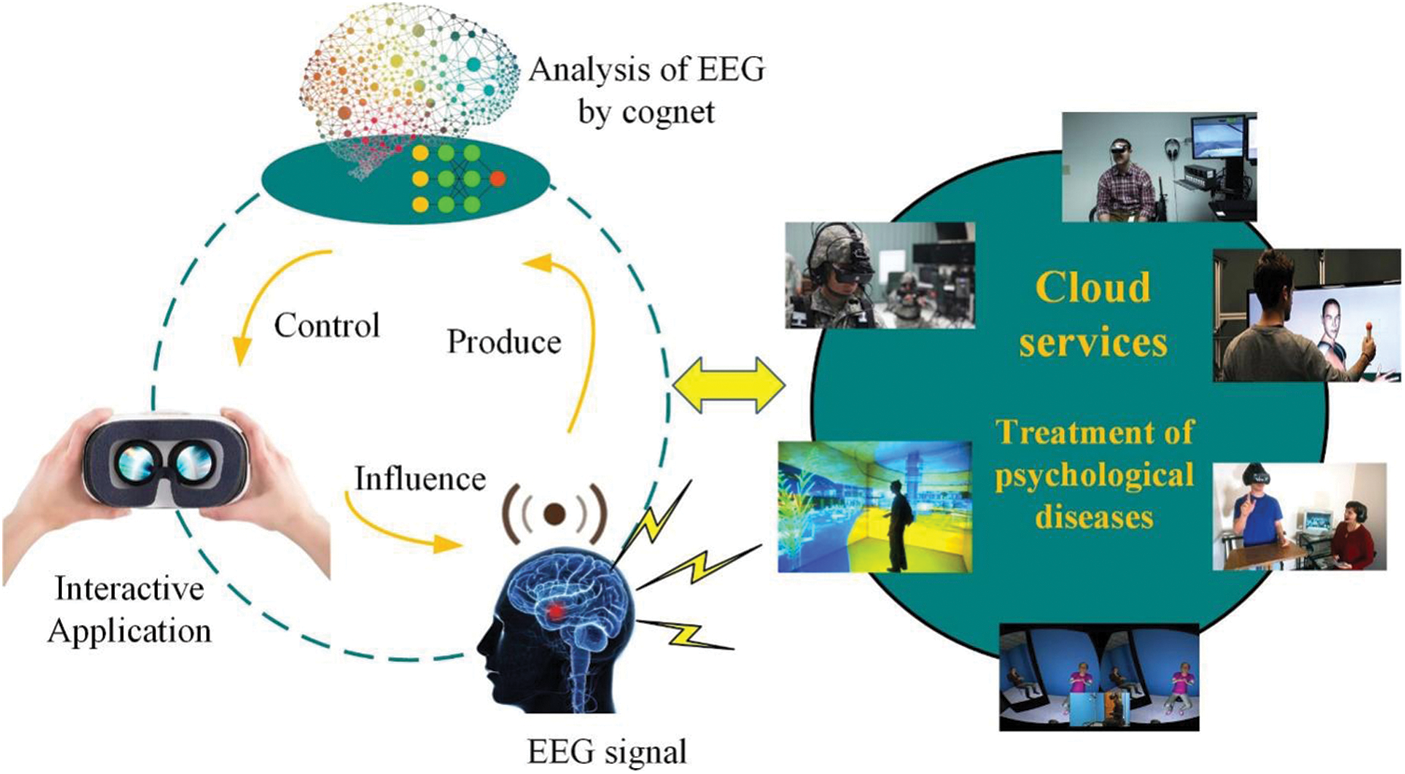
Figure 7: VR mental health adjustment method combined with brain waves
Memory bias (such as overconfidence in false memories) is related to the pathogenesis of delusions. VR can offer an opportunity to observe this prejudice and improve the cognitive insight of mental patients through corrective feedback. Dietrichkeit et al. [82] designed a VR environment for 39 mental patients and 20 healthy controls to elicit false memories and subsequently had to recollect items and faces. They used a stochastic-controlled design where half of the sample received performance feedback on the recollection task to correct overconfidence, and utilized the Baker Cognitive Insight Scale to measure changes in cognitive insights. They concluded that patients with psychosis showed impaired social cognition and there was evidence for impaired metacognition, as patients reported higher cognitive insight despite comparable or worse performance as well as overconfidence relative to controls.
McDonnell et al. [83] collected the data of 64 high-risk individuals with clinical psychosis in a cross-sectional study, including bullying victimization history, interpersonal sensitivity, and state paranoia after exposure to social VR environment. They used an underground trip in London as the scene of the VR experiment. Through result analysis, they found that interpersonal sensitivity fully explained the significant relationship between severe bullying victims in childhood and paranoid concepts in clinical high-risk groups [84]. They also reported that according to the Akaike Information Criterion standard, the best model selected was the complete mediation model: severe bullying→interpersonal sensitivity→status paranoia. Through the results, they found that the severity of bullying was more important than the frequency of bullying when explaining state paranoia. Therefore, they suggested that interpersonal sensitivity was a target for intervention due to its significant role played in the association between being bullied in childhood and paranoid ideation in the clinical high-risk group.
The imagination of memory [85] is to be stored in an interconnected network. To extract part of the memory, the individual must activate a guiding index, which is called “beginning” in psychology. For example, when something wakes up unconsciously, the connection is activated. For example, a person watching a horror movie at home begins to think that he will evoke terrible or fearful memories; even if he hears leaves falling from the window, he feels very bad, just like someone is about to climb in. For another example, when a mother saw other children’s mouths filled with cream bubbles, she cannot help laughing because this scene activates her memories of her children. Therefore, it is essential to grasp the scale when VR technology is used in the treatment of mental illness. Although there are still some practical obstacles, the therapeutic advantages of VR games in rehabilitation medicine are still prominent.
4 Challenges of VR Technology in Neurorehabilitation
4.1 Advantages and Limitations of VR Rehabilitation in Recovery from Stroke and PD
Taking stroke patients as an example, with the assistance of VR rehabilitation robots, patients can carry out active or passive rehabilitation training according to different conditions of patients without the whole process assistance of medical staff. This treatment method can recuperate patients from diseases more efficiently and improve their quality of life. At present, the upper and lower limb rehabilitation robots used in clinics are bulky and expensive, and most of them belong to non-wearable rehabilitation robots. In recent years, the emerging exoskeleton wearable rehabilitation robot is small, lightweight, convenient, and practical, putting forward new requirements for the research and development of rehabilitation robots. The HCI mode of rehabilitation robots in daily clinical contact is monotonous, and they mostly furnish two-dimensional scenes with simple structure and single color, which are far from the sufficient environment for patients’ rehabilitation training. Therefore, higher requirements are put forward for VR technology, which needs to create a highly immersive and interactive scene through 3D vision and hearing effects, form a loop of feedback information and control commands, and strengthen the awareness of patients’ independent participation. The challenges faced by the application of VR technology in neurorehabilitation include several aspects, such as high treatment cost and limited application prospects.
Compared with traditional rehabilitation treatment methods, such as physical therapy, occupational therapy, and speech therapy, the existing rehabilitation robots are costly. If the cost cannot be reduced, the prohibitive cost will inevitably impede the popularization of rehabilitation robots among the public. VR equipment can improve the rehabilitation effect and reduce the medical cost and treatment cost, which can generalize the rehabilitation robot. VR technology can also spice up the training by adopting games and offering patients real-time feedback through the screen and game results, to boost the self-confidence and training compliance of patients. In addition, compared with traditional rehabilitation approaches, VR is easier to operate. Patients can connect online and conduct remote rehabilitation training by terminals in clinics or at home to save labor and reduce technical requirements. This is a rehabilitation method suitable for promoting community and family rehabilitation. However, VR technology has some limitations. First, VR equipment is not popular at this stage. Second, the planning and adjustment results of VR games will affect the training intensity, and sometimes tough games make patients prone to resistance and reduce the degree of cooperation of patients. In addition, VR equipment requires patients to have many left-behind functions, indicating that they can understand and cooperate with treatment with the help of pedal props of the system. Therefore, VR technology cannot be applied to patients with more serious symptoms. Moreover, some patients feel dizzy when wearing VR devices.
Although it has yet to establish itself as a mainstream treatment model, VR technology has changed from an interesting concept to a hot topic in the field of digital medicine. With the in-depth study of this immersive technology by researchers, it is becoming even more clear that this new entertainment technology in life can solve some perennial problems in the medical industry. Freezing of Gait (FoG) [86] is a crucial motor disorder in patients with PD. The pathophysiological mechanism of FoG symptoms is unknown yet, and there are no definite and effective therapeutic drugs and means in clinical practice. FoG disease causes difficulty in walking for patients, increases the risk of falls, and seriously affects the quality of daily life of patients. Hence, there is an urgent need to develop effective rehabilitation treatment techniques. The follow-up work studies the following aspects.
Firstly, the influence of speed and spatial frequency of dynamic vision index on walking motion is only studied in two stages of parameter change. Future research will expand the variation range of displacement velocity and spatial frequency, and find new influence effects. The study of the single-factor effect shall consider the comprehensive effect of two factors, and the study of the double-factor effect may also be one of the directions of future research. Secondly, due to the limitations of EEG detection technology in the laboratory, most of the research on the impact of visual cues on walking adopts the motor imagination test method. Although some studies have confirmed that the EEG signals in the process of movement are similar to the actual moving process, this method has been widely used in many studies on the impact of external conditions on walking. However, it is hoped that the portable and highly sensitive EEG detection technology can be used in the future to obtain the EGG signals during the real walking movement stimulated by visual cues. As a result, analysis of visual signal frequency characteristics, i.e., the time of electroencephalogram signals, will achieve a more informative content for the content design. Finally, the brain is a complex control center, which receives visual signals as well as auditory, vibration, and proprioceptive signals. It is unclear whether the combination of several sensory indicators can more effectively ameliorate the symptoms of FoG. Multi-sensors suggest effective fusion to reduce the symptoms of FoG.
4.2 Advantages and Limitations of VR Games in the Rehabilitation of Mental Illness
VR games have been tentatively applied in the diagnosis and treatment of various diseases. The existing application effect research involves both commercial games and games developed by researchers. Most studies have proved the effectiveness of VR game-assisted disease treatment to varying degrees through empirical research. However, due to the diversity of different research and evaluation tools, the length of intervention, and the flexibility of intervention activities, it is difficult to compare the actual effect of different games. The optimization effect of VR games-assisted disease treatment on traditional therapy is manifested in the following aspects.
VR games can enhance treatment efficiency and effect. The common treatment method for phobia is “flooding therapy”, also known as “implosive therapy” or “impact therapy”. Rothbaum et al. [87], scholars of Emory University School of medicine in Atlanta, pointed out that phobia was mainly due to the memory of some fears, that was, by activating the patient’s fear and then eliminating it in his worried state. In the traditional “flooding therapy”, doctors guide patients into situations that frighten them through imagination through oral narration. However, this method is restricted by both doctors and patients, and there is great uncertainty. Using the “telepresence” of VR technology, patients can directly enter a safe and controllable computer simulation situation.
VR games can enhance the interest and motivation of rehabilitation training. The treatment process of many diseases is lengthy and dull, while VR games can stimulate users’ interest by using multi-sensory stimulation. The reward and punishment rules set in the game and personalized, diversified, and progressive game content can strengthen and keep users’ interest and motivation. Moreover, in traditional therapy, there is a host-client relationship between active physicians and passive patients. In contrast, VR games are user-oriented, which can dramatically enhance users’ active motivation. For example, in a previous study, doctors conducted a six-week monitoring experiment on 26 elderly people; the results showed that the total time of training was more than three times longer than that under the supervision of rehabilitation medical staff. This reveals that interactive games can enable the elderly to exercise spontaneously and do rehabilitation training.
Hoffman et al. [88] found that VR could effectively help patients immerse themselves in the virtual world and achieve the effect of pain relief. They arranged that two patients received dental treatment in three situations in one study: (1) distracted attention with VR; (2) watching movies; (3) without anything. They found that Patient 1 had the highest pain when watching movies and when nothing was used, and the pain was mild in VR; Patient 2 reported mild to moderate pain when watching movies, and almost no pain during VR. From the limited sample of this study, they proved the effect of VR in reducing pain by diverting patients’ attention.
In addition, using VR in the diagnosis of internal diseases can improve the diagnosis rate and reduce the pain of patients. In March 1999, the Mayo Clinic in Minnesota reported that using VR games to diagnose colon cancer allowed doctors to “walk” in the colon as if they were looking for tumors or polyps. The new technology can also enlarge the image of the colon locally, examine small pieces, “cut” them, and expose the intestinal wall so that doctors can better examine them. A study for 70 patients showed that the use of VR technology would make the diagnosis more accurate. The whole scanning process was less than 2 minutes, and the patient did not need to remain calm. Using the most commonly used blood test method, patients have to endure certain pain, and the diagnosis rate is less than 50%. Therefore, by using VR technology to simulate disease reality, doctors’ diagnosis is more direct and intuitive, and doctors’ diagnosis process will not bring substantive pain to patients in reality.
Moreover, VR games can protect patients’ privacy. Patients with obsessive-compulsive disorder (OCD) are more likely to accept the typical treatment method of cognitive-behavioral therapy, including thought stopping, exposure method, and response prevention, which requires massive intervention from doctors. Thought stopping is a method to block forced thinking by diverting attention or external control. For example, when forced thinking occurs repeatedly in the patient, it is feasible to transfer attention by adjusting the alarm sound. The exposure method and response prevention refer to encouraging patients to face and gradually accept situations that lead to forced thinking under the guidance of clinicians. For instance, if a patient is afraid of getting dirty, he will uncontrollably wash his hands repeatedly to ensure that he is not sick. He must insist on not washing his hands during multiple treatments such as exposure to sweat, soles of shoes, handles of public toilet doors, etc., and realize that he will not get sick. Anxiety associated with OCD symptoms will be relieved after multiple treatments until it disappears.
After years of randomized controlled clinical trials and open research, the British Institute of Psychiatry has developed a behavioral therapy project called OCFighter [89], a self-help project for the treatment of OCD. Interactive voice response in this treatment program has been widely tested and praised. This form enables patients to participate in treatment autonomously and provides them with continuous support and supervision. Many users trust OCFighter very much because it reduces the stigma of patients. Research has validated that OCFighter is effective.
So far, there are multitudes of applications related to VR game-assisted disease treatment, which is essentially the assistance and optimization of traditional therapy, rather than negation. Many studies have proved that, to a certain extent, the intervention of VR games has a better effect than traditional therapy. However, in the future, it still needs a wider scope, longer cycle, more scientific, fine, and in-depth application effect research to draw more convincing conclusions. Meanwhile, due to its state and its development stage, it is hard for VR game-assisted disease treatment to avoid some problems and limitations. Nevertheless, with the progress of science and technology and the deepening of research, these problems will be solved gradually. The problems related to the VR game or its use are not uncontrollable. Based on studying the mechanism of VR games on various systems of the human body, targeted monitoring and adjustment are needed. This is not only a research gap at present, but also a direction worth effort in the future.
4.3 Advantages and Limitations of VR Technology in the Rehabilitation of Mental Illness
At present, there is no particularly good way to diagnose and treat mental illness other than psychological counseling and medication. However, according to the latest research report, VR technology can effectively improve the treatment efficiency of mental illness. Meanwhile, people can use VR for emotional counseling in their own homes without worrying about privacy issues. For example, depression is undoubtedly the psychological problem that bothers people the most. The main manifestations of depression are persistent low mood, slow thinking, decreased volition, cognitive impairment, and physical discomfort, and even more serious suicide attempts and behaviors. VR can build a virtual world to evaluate situational memory or to dissolve habitual and selective attention patterns, allowing depression patients to discover that their past thoughts are wrong. Research conducted by the University of London shows that when depressed patients are placed in a VR environment, patients can give themselves more sympathy and treat themselves more tolerantly. VR therapy can make depression patients realize that excessive self-blame is undesirable, and they need to let it go and soothe themselves.
Schizophrenia is a common disease in mental illness. Patients with schizophrenia often have no insight and clear consciousness and normal intelligence. The clinical symptoms of schizophrenia are comprehensive, often involving various obstacles in perception, thinking, emotion, and behavior, and incoordination of mental activities. The treatment of schizophrenia should be carried out as soon as possible, but early schizophrenia is difficult to judge. Researchers from the University of Exeter in the United Kingdom have developed a VR-based mirror game that can give a more accurate early diagnosis report of schizophrenia than a psychological clinic through imitation and interaction. In fact, VR is more excellent in psychological treatment than physical treatment. As a new type of treatment technology, VR technology breaks through the limitations of previous psychotherapy technology, with a very real sense of presence and immersion. This kind of immersion can help the patient to activate the individual sense of fear and also effectively help the patient adjust to the dissonance hypothesis. In addition, the environment of VR treatment is controllable. Through VR equipment, people can perform psychotherapy in a safe environment. At present, VR psychotherapy is still in its early stage. The popularization of VR psychotherapy is still enslaved to factors such as lack of standardization of treatment technology and software, single application, expensive equipment, and high research and development costs.
In general, VR medicine is still in its infancy in terms of breakthroughs in treatment models and practical clinical applications. Through a proliferation of experiments, innovators in this field will further verify the effectiveness of VR medicine. Shortly, the integration of VR and AI, big data, sensors, biofeedback, augmented reality, and other technologies will make VR medical treatment more intelligent. These application cases of VR technology in the field of medical rehabilitation not only show the convenience brought to people by the rapid development of VR technology, but also prove the necessity of the continuous development of VR technology in the future. VR technology allows us to provide some new treatment methods for some of the existing diseases that are difficult to treat. It is believed that in the future, it will help more patients to alleviate the pain of the disease.
Moreover, there are still many hurdles to clear in the large-scale clinical application of VR. Firstly, VR headsets and other hardware need to be designed. At present, these hardware devices are relatively large, not light enough, and not convenient to use. It is difficult for patients to adapt to them because of their sensitivity. Secondly, when using VR therapy, patients will also consider whether insurance companies cover it. In the United States, insurance companies pay for the treatment services of patients, so whether the insurance company includes VR therapy in the reimbursement plan will directly affect the popularization of VR in medical care. Thirdly, VR needs to be integrated with the hospital management system, especially the electronic medical record system. As a digital treatment method, VR technology must be connected to a hospital’s network system to implement more effective tracking of use and prescribing. Finally, VR is a new thing after all, and many doctors are not familiar with the technology and do not understand its application potential. Therefore, VR education and training for doctors and patients still have a long way to go. Although VR faces many obstacles, it is definitely that this novel technology will obtain an increasingly tolerant and open attitude from the health care industry.
For a long time, influenced by the view that nerve cells cannot regenerate after death, the academic community has always believed that patients are difficult to recover after severe nerve damage. However, the practice of clinical rehabilitation medicine proves that the function after neurological disease and injury can be recovered. After brain injury, the brain function can be reconstituted to some extent. Many brain injury patients have recovered their impaired nerve function after rehabilitation. In particular, modern medical treatment combined with advanced computer technology brings new hope to neurological rehabilitation medicine. With the continuous enhancement of research, VR is no longer satisfied with the treatment of certain diseases, but is forming a platform. On this platform, various treatment plans can be better deployed to suit the conditions of different patients and meet the individual needs of patients.
Multitudes of studies mentioned here have shown that VR technology combined with task-oriented training in postoperative rehabilitation can effectively improve the upper limb function of stroke patients, and the treatment effect is better than task-oriented training. Moreover, it can effectively improve the quality of life of stroke patients and Parkinson’s patients. VR games have the advantages of relieving pain, increasing the fun of rehabilitation treatment, and enhancing treatment efficiency in the process of neurorehabilitation. Even simulating the patient’s memory through a virtual environment can help treat mental and psychological illnesses. Of course, VR technology also has its shortcomings, such as expensive equipment and low penetration. VR technology involves many uncertain factors and requires a wealth of experiments and research for theoretical support. Experts agree that therapeutic VR will be most effective if researchers and suppliers can find ways to support the technology in a wider range of medical operations. Although many cases have proven the role of VR, it is just a tool. In the medical and health field, tools must have the environment and conditions to use them, and be combined with other treatment techniques or tools. In the medical and health field, tools must have qualified use environment and conditions and be combined with other treatment techniques or tools.
Acknowledgement: Thank all those who have helped me in my research.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Scrutinio, D., Giardini, A., Chiovato, L., Spanevello, A., Vitacca, M. et al. (2019). The new frontiers of rehabilitation medicine in people with chronic disabling illnesses. European Journal of Internal Medicine, 61(4), 1–8. DOI 10.1016/j.ejim.2018.10.019. [Google Scholar] [CrossRef]
2. Boldrini, P., Bernetti, A., Fiore, P., Bargellesi, S., Bonaiuti, D. et al. (2020). Impact of COVID-19 outbreak on rehabilitation services and physical and rehabilitation medicine physicians’ activities in Italy: An official document of the Italian PRM Society (SIMFER). European Journal of Physical and Rehabilitation Medicine, 56(3), 315–318. DOI 10.23736/S1973-9087.20.06256-5. [Google Scholar] [CrossRef]
3. Carda, S., Invernizzi, M., Bavikatte, G., Bensmaïl, D., Bianchi, F. et al. (2020). COVID-19 pandemic. What should physical and rehabilitation medicine specialists do? A clinician’s perspective. European Journal of Physical and Rehabilitation Medicine, 56(4), 1245. DOI 10.23736/S1973-9087.20.06317-0. [Google Scholar] [CrossRef]
4. Giacino, J. T., Whyte, J., Nakase-Richardson, R., Katz, D. I., Arciniegas, D. B. et al. (2020). Minimum competency recommendations for programs that provide rehabilitation services for persons with disorders of consciousness: A position statement of the American Congress of Rehabilitation Medicine and the National Institute on Disability, Independent Living and Rehabilitation Research Traumatic Brain Injury Model Systems. Archives of Physical Medicine and Rehabilitation, 101(6), 1072–1089. DOI 10.1016/j.apmr.2020.01.013. [Google Scholar] [CrossRef]
5. Wang, J., Wang, L., Xu, J., Peng, Y. (2021). Information needs mining of COVID-19 in Chinese online health communities. Big Data Research, 24, 100193. DOI 10.1016/j.bdr.2021.100193. [Google Scholar] [CrossRef]
6. Lee, S. H., Jung, H. Y., Yun, S. J., Oh, B. M., Seo, H. G. (2020). Upper extremity rehabilitation using fully immersive virtual reality games with a head mount display: A feasibility study. PM&R, 12(3), 257–262. DOI 10.1002/pmrj.12206. [Google Scholar] [CrossRef]
7. de Keersmaecker, E., Beckwée, D., Denissen, S., Nagels, G., Swinnen, E. (2021). Virtual reality for multiple sclerosis rehabilitation. Cochrane Database of Systematic Reviews, 2020(12), CD013834. DOI 10.1002/14651858.CD013834. [Google Scholar] [CrossRef]
8. Imbimbo, I., Coraci, D., Santilli, C., Loreti, C., Piccinini, G. et al. (2021). Parkinson’s disease and virtual reality rehabilitation: Cognitive reserve influences the walking and balance outcome. Neurological Sciences, 1–7. DOI 10.1007/s10072-021-05123-3. [Google Scholar] [CrossRef]
9. Clark, W. E., Sivan, M., O’Connor, R. J. (2019). Evaluating the use of robotic and virtual reality rehabilitation technologies to improve function in stroke survivors: A narrative review. Journal of Rehabilitation and Assistive Technologies Engineering, 6, 2055668319863557. DOI 10.1177/2055668319863557. [Google Scholar] [CrossRef]
10. Lee, H. S., Lim, J. H., Jeon, B. H., Song, C. S. (2020). Non-immersive virtual reality rehabilitation applied to a task-oriented approach for stroke patients: A randomized controlled trial. Restorative Neurology and Neuroscience, 38(2), 165–172. DOI 10.3233/RNN-190975. [Google Scholar] [CrossRef]
11. Caeiro-Rodríguez, M., Otero-González, I., Mikic-Fonte, F. A., Llamas-Nistal, M. (2021). A systematic review of commercial smart gloves: Current status and applications. Sensors, 21(8), 2667. DOI 10.3390/s21082667. [Google Scholar] [CrossRef]
12. Choi, J. Y., Yi, S. H., Ao, L., Tang, X., Xu, X. et al. (2021). Virtual reality rehabilitation in children with brain injury: A randomized controlled trial. Developmental Medicine & Child Neurology, 63(4), 480–487. DOI 10.1111/dmcn.14762. [Google Scholar] [CrossRef]
13. Radianti, J., Majchrzak, T. A., Fromm, J., Wohlgenannt, I. (2020). A systematic review of immersive virtual reality applications for higher education: Design elements, lessons learned, and research agenda. Computers & Education, 147(4), 103778. DOI 10.1016/j.compedu.2019.103778. [Google Scholar] [CrossRef]
14. Hohmann, V., Paluch, R., Krueger, M., Meis, M., Grimm, G. (2020). The virtual reality lab: Realization and application of virtual sound environments. Ear and Hearing, 41(Suppl 1), 31S–38S. DOI 10.1097/AUD.0000000000000945. [Google Scholar] [CrossRef]
15. Zhan, T., Yin, K., Xiong, J., He, Z., Wu, S. T. (2020). Augmented reality and virtual reality displays: Perspectives and challenges. iscience, 23, 101397. DOI 10.1016/j.isci.2020.101397. [Google Scholar] [CrossRef]
16. Keil, J., Edler, D., O’Meara, D., Korte, A., Dickmann, F. (2021). Effects of virtual reality locomotion techniques on distance estimations. ISPRS International Journal of Geo-Information, 10(3), 150. DOI 10.3390/ijgi10030150. [Google Scholar] [CrossRef]
17. Cassani, R., Novak, G. S., Falk, T. H., Oliveira, A. A. (2020). Virtual reality and non-invasive brain stimulation for rehabilitation applications: A systematic review. Journal of Neuroengineering and Rehabilitation, 17(1), 1–16. DOI 10.1186/s12984-020-00780-5. [Google Scholar] [CrossRef]
18. Xu, Y., Tong, M., Ming, W. K., Lin, Y., Mai, W. et al. (2021). A depth camera-based, task-specific virtual reality rehabilitation game for patients with stroke: Pilot usability study. JMIR Serious Games, 9(1), e20916. DOI 10.2196/20916. [Google Scholar] [CrossRef]
19. Weber, H., Barr, C., Gough, C., van den Berg, M.(2020). How commercially available virtual reality-based interventions are delivered and reported in gait, posture, and balance rehabilitation: A systematic review. Physical Therapy, 100(10), 1805–1815. DOI 10.1093/ptj/pzaa123. [Google Scholar] [CrossRef]
20. Hong, H. (2021). A measurement method of the focal distance of the virtual image in an augmented reality or virtual reality device. Journal of the Society for Information Display, 29(4), 230–236. DOI 10.1002/jsid.981. [Google Scholar] [CrossRef]
21. Yu, D., Zhou, Q., Newn, J., Dingler, T., Velloso, E. et al. (2020). Fully-occluded target selection in virtual reality. IEEE Transactions on Visualization and Computer Graphics, 26(12), 3402–3413. DOI 10.1109/TVCG.2020.3023606. [Google Scholar] [CrossRef]
22. Hübner, P., Clintworth, K., Liu, Q., Weinmann, M., Wursthorn, S. (2020). Evaluation of HoloLens tracking and depth sensing for indoor mapping applications. Sensors, 20(4), 1021. DOI 10.3390/s20041021. [Google Scholar] [CrossRef]
23. Farhat, M., Yang, M., Ye, Z., Chen, P. Y. (2020). PT-symmetric absorber-laser enables electromagnetic sensors with unprecedented sensitivity. ACS Photonics, 7(8), 2080–2088. DOI 10.1021/acsphotonics.0c00514. [Google Scholar] [CrossRef]
24. Zhao, Y., Liang, C., Gu, Z., Zheng, Y., Wu, Q. (2020). A new design scheme for intelligent upper limb rehabilitation training robot. International Journal of Environmental Research and Public Health, 17(8), 2948. DOI 10.3390/ijerph17082948. [Google Scholar] [CrossRef]
25. Morelli, N., Rota, E., Terracciano, C., Immovilli, P., Spallazzi, M. et al. (2020). The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. European Neurology, 1(2), 213–215. DOI 10.1159/000507666. [Google Scholar] [CrossRef]
26. Stinear, C. M., Lang, C. E., Zeiler, S., Byblow, W. D. (2020). Advances and challenges in stroke rehabilitation. Lancet Neurology, 19(4), 348–360. DOI 10.1016/S1474-4422(19)30415-6. [Google Scholar] [CrossRef]
27. Fara, M. G., Stein, L. K., Skliut, M., Morgello, S., Fifi, J. T. et al. (2020). Macrothrombosis and stroke in patients with mild COVID-19 infection. Journal of Thrombosis and Haemostasis, 18(8), 2031–2033. DOI 10.1111/jth.14938. [Google Scholar] [CrossRef]
28. Peng, Y., Xu, J., Ma, L., Wang, J. (2021). Prediction of hypertension risks with feature selection and XGBoost. Journal of Mechanics in Medicine and Biology, 21, 2140028. DOI 10.1142/S0219519421400285. [Google Scholar] [CrossRef]
29. Jia, T., Liu, K., Qian, C., Li, C., Ji, L. (2020). Denoising algorithm for event-related desynchronization-based motor intention recognition in robot-assisted stroke rehabilitation training with brain-machine interaction. Journal of Neuroscience Methods, 346, 108909. DOI 10.1016/j.jneumeth.2020.108909. [Google Scholar] [CrossRef]
30. Mao, H., Li, Y., Tang, L., Chen, Y., Ni, J. et al. (2020). Effects of mirror neuron system-based training on rehabilitation of stroke patients. Brain and Behavior, 10(8), e01729. DOI 10.1002/brb3.1729. [Google Scholar] [CrossRef]
31. Luque-Moreno, C., Jiménez-Blanco, A., Cano-Bravo, F., Paniagua-Monrobel, M., Zambrano-García, E. et al. (2021). Effectiveness of visual feedback and postural balance treatment of post-stroke pusher syndrome. A systematic review. Revista Científica de la Sociedad de Enfermería Neurológica (English Edition), 53, 16–24. DOI 10.1016/j.sedeng.2019.12.001. [Google Scholar] [CrossRef]
32. Manfredini, F., Straudi, S., Lamberti, N., Patergnani, S., Tisato, V. et al. (2020). Rehabilitation improves mitochondrial energetics in progressive multiple sclerosis: The significant role of robot-assisted gait training and of the personalized intensity. Diagnostics, 10(10), 834. DOI 10.3390/diagnostics10100834. [Google Scholar] [CrossRef]
33. Park, J., Chung, Y. (2018). The effects of robot-assisted gait training using virtual reality and auditory stimulation on balance and gait abilities in persons with stroke. Neuro Rehabilitation, 43(2), 227–235. DOI 10.3233/NRE-172415. [Google Scholar] [CrossRef]
34. Shideler, B. L., Martelli, D., Prado, A., Agrawal, S. K. (2021). Overground gait training using virtual reality aimed at gait symmetry. Human Movement Science, 76, 102770. DOI 10.1016/j.humov.2021.102770. [Google Scholar] [CrossRef]
35. Liao, W. L., Chang, C. W., Sung, P. Y., Hsu, W. N., Lai, M. W. et al. (2021). The Berg balance scale at admission can predict community ambulation at discharge in patients with stroke. Medicina, 57(6), 556. DOI 10.3390/medicina57060556. [Google Scholar] [CrossRef]
36. Christopher, A., Kraft, E., Olenick, H., Kiesling, R., Doty, A. (2021). The reliability and validity of the timed up and go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review: Psychometric properties of the timed up and go. Disability and Rehabilitation, 43(13), 1799–1813. DOI 10.1080/09638288.2019.1682066. [Google Scholar] [CrossRef]
37. Alıpsatıcı, Ç., Alaca, N., Canbora, M. K. (2020). Comparison of the effects of treadmill trainings on walking and balance functions by increasing the speed and incline in chronic patients with stroke. Turkish Journal of Neurology/Turk Noroloji Dergisi, 26(4), 316–321. DOI 10.4274/tnd.2020.48921. [Google Scholar] [CrossRef]
38. de Luca, R., Russo, M., Naro, A., Tomasello, P., Leonardi, S. et al. (2018). Effects of virtual reality-based training with BTs-Nirvana on functional recovery in stroke patients: Preliminary considerations. International Journal of Neuroscience, 128(9), 791–796. DOI 10.1080/00207454.2017.1403915. [Google Scholar] [CrossRef]
39. Maggio, M. G., de Luca, R., Manuli, A., Buda, A., Foti Cuzzola, M. et al. (2020). Do patients with multiple sclerosis benefit from semi-immersive virtual reality? A randomized clinical trial on cognitive and motor outcomes. Applied Neuropsychology: Adult, 1–7. DOI 10.1080/23279095.2019.1708364. [Google Scholar] [CrossRef]
40. Howard, M. C., Gutworth, M. B. (2020). A meta-analysis of virtual reality training programs for social skill development. Computers & Education, 144(4), 103707. DOI 10.1016/j.compedu.2019.103707. [Google Scholar] [CrossRef]
41. Grassini, S., Laumann, K., Rasmussen Skogstad, M. (2020). The use of virtual reality alone does not promote training performance (but sense of presence does). Frontiers in Psychology, 11, 1743. DOI 10.3389/fpsyg.2020.01743. [Google Scholar] [CrossRef]
42. Ning, A. P., Mok, W. Q., Chieng, Y. J. S., Zhang, H. M., Ramos, P. et al. (2020). Effectiveness of virtual reality training in improving knowledge among nursing students: A systematic review, meta-analysis and meta-regression. Nurse Education Today, 98, 104655. DOI 10.1016/j.nedt.2020.104655.. [Google Scholar] [CrossRef]
43. Qian, J., McDonough, D. J., Gao, Z. (2020). The effectiveness of virtual reality exercise on individual’s physiological, psychological and rehabilitative outcomes: A systematic review. International Journal of Environmental Research and Public Health, 17(11), 4133. DOI 10.3390/ijerph17114133. [Google Scholar] [CrossRef]
44. Sayaca, C., Serel-Arslan, S., Sayaca, N., Demir, N., Somay, G. et al. (2020). Is the proprioceptive neuromuscular facilitation technique superior to Shaker exercises in swallowing rehabilitation? European Archives of Oto-Rhino-Laryngology, 277(2), 497–504. DOI 10.1007/s00405-019-05772-3. [Google Scholar] [CrossRef]
45. Naghdi, S., Ansari, N. N., Mansouri, K., Hasson, S. (2010). A neurophysiological and clinical study of Brunnstrom recovery stages in the upper limb following stroke. Brain Injury, 24(11), 1372–1378. DOI 10.3109/02699052.2010.506860. [Google Scholar] [CrossRef]
46. Díaz-Arribas, M. J., Martín-Casas, P., Cano-de-la-Cuerda, R., Plaza-Manzano, G. (2020). Effectiveness of the Bobath concept in the treatment of stroke: A systematic review. Disability and Rehabilitation, 42(12), 1636–1649. DOI 10.1080/09638288.2019.1590865. [Google Scholar] [CrossRef]
47. Ullah, I., Arsh, A., Zahir, A., Jan, S. (2020). Motor relearning program along with electrical stimulation for improving upper limb function in stroke patients: A quasi experimental study. Pakistan Journal of Medical Sciences, 36(7), 1613. DOI 10.12669/pjms.36.7.2351. [Google Scholar] [CrossRef]
48. Simon-Martinez, C., Mailleux, L., Hoskens, J., Ortibus, E., Jaspers, E. et al. (2020). Randomized controlled trial combining constraint-induced movement therapy and action-observation training in unilateral cerebral palsy: Clinical effects and influencing factors of treatment response. Therapeutic Advances in Neurological Disorders, 13, 1756286419898065. DOI 10.1177/1756286419898065. [Google Scholar] [CrossRef]
49. Luo, Z., Zhou, Y., He, H., Lin, S., Zhu, R. et al. (2020). Synergistic effect of combined mirror therapy on upper extremity in patients with stroke: A systematic review and meta-analysis. Frontiers in Neurology, 11, 155. DOI 10.3389/fneur.2020.00155. [Google Scholar] [CrossRef]
50. Kim, K. (2019). Effect of virtual reality rehabilitation program with RAPAEL smart glove on stroke patient’s upper extremity functions and activities of daily living. Journal of the Korean Society of Integrative Medicine, 7(2), 69–76. DOI 10.15268/ksim.2019.7.2.069. [Google Scholar] [CrossRef]
51. Tofani, M., Castelli, E., Sabbadini, M., Berardi, A., Murgia, M. et al. (2020). Examining reliability and validity of the Jebsen-Taylor hand function test among children with cerebral palsy. Perceptual and Motor Skills, 127(4), 684–697. DOI 10.1177/0031512520920087. [Google Scholar] [CrossRef]
52. Kim, H., Lee, A., Shin, Y. I., Chang, W. H., Koo, K. H. et al. (2018). Effects of digital smart glove system on motor recovery of upper extremity in subacute stroke patients. Annals of Physical and Rehabilitation Medicine, 61, e28. DOI 10.1016/j.rehab.2018.05.061. [Google Scholar] [CrossRef]
53. Park, Y. S., An, C. S., Lim, C. G. (2021). Effects of a rehabilitation program using a wearable device on the upper limb function, performance of activities of daily living, and rehabilitation participation in patients with acute stroke. International Journal of Environmental Research and Public Health, 18(11), 5524. DOI 10.3390/ijerph18115524. [Google Scholar] [CrossRef]
54. Jung, S. M. (2020). Effects of somatosensory stimulation therapy in improving upper limb function of patients with hemiplegic stroke. Journal of Korean Society for Neurotherapy, 24(1), 11–15. [Google Scholar]
55. Gul, M., Yucesan, M., Celik, E. (2020). A manufacturing failure mode and effect analysis based on fuzzy and probabilistic risk analysis. Applied Soft Computing, 96, 106689. DOI 10.1016/j.asoc.2020.106689. [Google Scholar] [CrossRef]
56. Sears, E. D., Chung, K. C. (2010). Validity and responsiveness of the Jebsen-Taylor hand function test. Journal of Hand Surgery, 35(1), 30–37. DOI 10.1016/j.jhsa.2009.09.008. [Google Scholar] [CrossRef]
57. Song, C. S., Lim, J. H., Jeon, B. H., Lee, H. S. (2019). The effects of virtual upper extremity training using the RAPAEL smart glove on physical and cognitive function in stroke survivors—A single group study. PNF and Movement, 17(2), 199–206. DOI 10.21598/JKPNFA.2019.17.2.199. [Google Scholar] [CrossRef]
58. Martinez, C., Bacon, H., Rowe, V., Russak, D., Fitzgerald, E. et al. (2020). A reaching performance scale for 2 wolf motor function test items. Archives of Physical Medicine and Rehabilitation, 101(11), 2015–2026. DOI 10.1016/j.apmr.2020.05.003. [Google Scholar] [CrossRef]
59. Parmar, M., Grealish, S., Henchcliffe, C. (2020). The future of stem cell therapies for Parkinson disease. Nature Reviews Neuroscience, 21(2), 103–115. DOI 10.1038/s41583-019-0257-7. [Google Scholar] [CrossRef]
60. Tan, E. K., Chao, Y. X., West, A., Chan, L. L., Poewe, W. et al. (2020). Parkinson disease and the immune system—Associations, mechanisms and therapeutics. Nature Reviews Neurology, 16(6), 303–318. DOI 10.1038/s41582-020-0344-4. [Google Scholar] [CrossRef]
61. Lei, C., Sunzi, K., Dai, F., Liu, X., Wang, Y. et al. (2019). Effects of virtual reality rehabilitation training on gait and balance in patients with Parkinson’s disease: A systematic review. PLoS One, 14(11), e0224819. DOI 10.1371/journal.pone.0224819. [Google Scholar] [CrossRef]
62. Simon, D. K., Tanner, C. M., Brundin, P. (2020). Parkinson disease epidemiology, pathology, genetics, and pathophysiology. Clinics in Geriatric Medicine, 36(1), 1–12. DOI 10.1016/j.cger.2019.08.002. [Google Scholar] [CrossRef]
63. Canning, C. G., Allen, N. E., Nackaerts, E., Paul, S. S., Nieuwboer, A. et al. (2020). Virtual reality in research and rehabilitation of gait and balance in Parkinson disease. Nature Reviews Neurology, 16(8), 409–425. DOI 10.1038/s41582-020-0370-2. [Google Scholar] [CrossRef]
64. Maggio, M. G., de Cola, M. C., Latella, D., Maresca, G., Finocchiaro, C. et al. (2018). What about the role of virtual reality in Parkinson disease’s cognitive rehabilitation? Preliminary findings from a randomized clinical trial. Journal of Geriatric Psychiatry and Neurology, 31(6), 312–318. DOI 10.1177/0891988718807973. [Google Scholar] [CrossRef]
65. de Luca, R., Russo, M., Naro, A., Tomasello, P., Leonardi, S. et al. (2018). Effects of virtual reality-based training with BTs-Nirvana on functional recovery in stroke patients: Preliminary considerations. International Journal of Neuroscience, 128(9), 791–796. DOI 10.1080/00207454.2017.1403915. [Google Scholar] [CrossRef]
66. Chen, Y., Gao, Q., He, C. Q., Bian, R. (2020). Effect of virtual reality on balance in individuals with Parkinson disease: A systematic review and meta-analysis of randomized controlled trials. Physical Therapy, 100(6), 933–945. DOI 10.1093/ptj/pzaa042. [Google Scholar] [CrossRef]
67. Lina, C., Guoen, C., Huidan, W., Yingqing, W., Ying, C. et al. (2020). The effect of virtual reality on the ability to perform activities of daily living, balance during gait, and motor function in Parkinson disease patients: A systematic review and meta-analysis. American Journal of Physical Medicine & Rehabilitation, 99(10), 917–924. DOI 10.1097/PHM.0000000000001447. [Google Scholar] [CrossRef]
68. Yang, C. M., Wang, Y. C., Lee, C. H., Chen, M. H., Hsieh, C. L. (2020). A comparison of test-retest reliability and random measurement error of the Barthel Index and modified Barthel Index in patients with chronic stroke. Disability and Rehabilitation, 100, 1–5. DOI 10.1080/09638288.2020.1814429. [Google Scholar] [CrossRef]
69. Servotte, J. C., Goosse, M., Campbell, S. H., Dardenne, N., Pilote, B. et al. (2020). Virtual reality experience: Immersion, sense of presence, and cybersickness. Clinical Simulation in Nursing, 38, 35–43. DOI 10.1016/j.ecns.2019.09.006. [Google Scholar] [CrossRef]
70. Weech, S., Kenny, S., Lenizky, M., Barnett-Cowan, M. (2020). Narrative and gaming experience interact to affect presence and cybersickness in virtual reality. International Journal of Human-Computer Studies, 138(10), 102398. DOI 10.1016/j.ijhcs.2020.102398. [Google Scholar] [CrossRef]
71. Matsangidou, M., Otkhmezuri, B., Ang, C. S., Avraamides, M., Riva, G. et al. (2020). “Now I can see me” designing a multi-user virtual reality remote psychotherapy for body weight and shape concerns. Human-Computer Interaction, 1–27. DOI 10.1080/07370024.2020.1788945. [Google Scholar] [CrossRef]
72. Hadri, S. A., Bouramoul, A. (2020). Recent virtual reality advances in psychotherapy: A highly selective review. International Journal of Informatics and Applied Mathematics, 3(2), 23–34. [Google Scholar]
73. Karamians, R., Proffitt, R., Kline, D., Gauthier, L. V. (2020). Effectiveness of virtual reality-and gaming-based interventions for upper extremity rehabilitation poststroke: A meta-analysis. Archives of Physical Medicine and Rehabilitation, 101(5), 885–896. DOI 10.1016/j.apmr.2019.10.195. [Google Scholar] [CrossRef]
74. Qidwai, U., Ajimsha, M. S., Shakir, M. (2019). The role of EEG and EMG combined virtual reality gaming system in facial palsy rehabilitation—A case report. Journal of Bodywork and Movement Therapies, 23(2), 425–431. DOI 10.1016/j.jbmt.2019.02.012. [Google Scholar] [CrossRef]
75. Sormani, M. P. (2020). An Italian programme for COVID-19 infection in multiple sclerosis. Lancet Neurology, 19(6), 481–482. DOI 10.1016/S1474-4422(20)30147-2. [Google Scholar] [CrossRef]
76. Jonsdottir, J., Perini, G., Ascolese, A., Bowman, T., Montesano, A. et al. (2019). Response to commentary of shirani and okuda regarding unilateral arm rehabilitation for persons with multiple sclerosis using serious games in a virtual reality approach: Bilateral treatment effect? Multiple Sclerosis and Related Disorders, 35(4), 76–82. DOI 10.1016/j.msard.2019.07.010. [Google Scholar] [CrossRef]
77. Solaro, C., di Giovanni, R., Grange, E., Mueller, M., Messmer Uccelli, M. et al. (2020). Box and block test, hand grip strength and nine-hole peg test: Correlations between three upper limb objective measures in multiple sclerosis. European Journal of Neurology, 27(12), 2523–2530. DOI 10.1111/ene.14427. [Google Scholar] [CrossRef]
78. Morgan, A. S., Hang, K., Bircher, W. G., Alladkani, F. M., Gandhi, A. et al. (2019). Benchmarking cluttered robot pick-and-place manipulation with the box and blocks test. IEEE Robotics and Automation Letters, 5(2), 454–461. DOI 10.1109/LRA.2019.2961053. [Google Scholar] [CrossRef]
79. Jonsdottir, J., Perini, G., Ascolese, A., Bowman, T., Montesano, A. et al. (2019). Unilateral arm rehabilitation for persons with multiple sclerosis using serious games in a virtual reality approach: Bilateral treatment effect? Multiple Sclerosis and Related Disorders, 35(4), 76–82. DOI 10.1016/j.msard.2019.07.010. [Google Scholar] [CrossRef]
80. Huang, Z., Kohler, I. V., Kämpfen, F. (2020). A single-item visual analogue scale (VAS) measure for assessing depression among college students. Community Mental Health Journal, 56(2), 355–367. DOI 10.1007/s10597-019-00469-7. [Google Scholar] [CrossRef]
81. Rus-Calafell, M., Garety, P., Sason, E., Craig, T. J., Valmaggia, L. R. (2018). Virtual reality in the assessment and treatment of psychosis: A systematic review of its utility, acceptability and effectiveness. Psychological Medicine, 48(3), 362–391. DOI 10.1017/S0033291717001945. [Google Scholar] [CrossRef]
82. Dietrichkeit, M., Grzella, K., Nagel, M., Moritz, S. (2020). Using virtual reality to explore differences in memory biases and cognitive insight in people with psychosis and healthy controls. Psychiatry Research, 285(1), 112787. DOI 10.1016/j.psychres.2020.112787. [Google Scholar] [CrossRef]
83. McDonnell, J., Stahl, D., Day, F., McGuire, P., Valmaggia, L. R. (2018). Interpersonal sensitivity in those at clinical high risk for psychosis mediates the association between childhood bullying victimisation and paranoid ideation: A virtual reality study. Schizophrenia Research, 192(3), 89–95. DOI 10.1016/j.schres.2017.04.029. [Google Scholar] [CrossRef]
84. You, Z., Zhang, Y., Zhang, L., Xu, Y., Chen, X. (2019). How does self-esteem affect mobile phone addiction? The mediating role of social anxiety and interpersonal sensitivity. Psychiatry Research, 271(3–4), 526–531. DOI 10.1016/j.psychres.2018.12.040. [Google Scholar] [CrossRef]
85. Schacter, D. L., Addis, D. R. (2020). Memory and imagination: Perspectives on constructive episodic simulation. In: Abraham, A. (Ed.The cambridge handbook of imagination, pp. 111–131. Cambridge, England: Cambridge University Press. [Google Scholar]
86. Weiss, D., Schoellmann, A., Fox, M. D., Bohnen, N. I., Factor, S. A. et al. (2020). Freezing of gait: Understanding the complexity of an enigmatic phenomenon. Brain, 143(1), 14–30. DOI 10.1093/brain/awz314. [Google Scholar] [CrossRef]
87. Rothbaum, B., Stein, A. T., Levihn-Coon, A., Pogue, J. R., Carl, E. et al. (2019). Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. Journal of Anxiety Disorders, 61(5), 27–36. DOI 10.1016/j.janxdis.2018.08.003. [Google Scholar] [CrossRef]
88. Hoffman, K. M., Trawalter, S., Axt, J. R., Oliver, M. N. (2016). Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proceedings of the National Academy of Sciences of the United States of America, 113(16), 4296–4301. DOI 10.1073/pnas.1516047113. [Google Scholar] [CrossRef]
89. Wheaton, M. G., Patel, S. R., Andersson, E., Rück, C., Simpson, H. B. (2021). Predicting treatment outcomes from internet-based cognitive behavior therapy for obsessive-compulsive disorder. Behavior Therapy, 52(1), 77–85. DOI 10.1016/j.beth.2020.02.003. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |