
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/ijmhp.2021.017660
ARTICLE
Meeting 24-h Movement Guidelines is Related to Better Academic Achievement: Findings from the YRBS 2019 Cycle
1College of Sports Science, Haikou University of Economics, Haikou, China
2College of Sports Science, Jishou University, Jishou, China
3Exercise Psychophysiology Laboratory, Institute of KEEP Collaborative Innovation, School of Psychology, Shenzhen University, Shenzhen, China
4Department of Health Promotion and Community Health Sciences, School of Public Health, Texas A&M University, College Station, USA
5College of Education and Health Professions, Limestone University, South Carolina, USA
6School of Physical Education and Sport Training, Shanghai University of Sport, Shanghai, China
7The Library of Shandong University of Sport, Shandong, China
8Priority Research Centre in Physical Activity and Nutrition, School of Education, University of Newcastle, Callaghan, Australia
9Beckman Institute, University of Illinois, Urbana, Illinois, USA
10Canter for Cognitive & Brain Health, Northeastern University, Boston, USA
*Corresponding Author: Jin Yan. Email: jin.yan@uon.edu.au
#Equally contributed to this manuscript
Received: 26 May 2021; Accepted: 15 August 2021
Abstract: This research is designed to investigate the relationship between the 24-h movement guidelines (24-HMG) and self-reported academic achievement (AA) using nationally representative data derived from the 2019 U.S. National Youth Risk Behaviour Survey. A multiple-stage cluster sampling procedure has been adopted to ensure a representative sample (N = 9127 adolescents; mean age = 15.7 years old; male% = 49.8%). Logistic regression has been adopted to obtain the odds ratio (OR) regarding the associations between adherence to 24-HMG and AA while controlling for ethnicity, body mass index, sex and age. The prevalence of meeting the 24-h movement guidelines in isolation and combination varied greatly (physical activity = 23.3%, screen time = 32.5%, sleep = 22.3%, and 24-HMG = 2.8%), while the percentage of highest-class AA was 42.5%. Compared with the situation when none of 24-HMG is met, the achievement of any of the combined guidelines (except for meeting the physical activity guidelines) was significantly associated with higher odds of achieving first-class AA. Meeting the sleep guideline had 1.42 times increased likelihood to achieve highest-class AA as compared with not meeting the sleep guideline. Meeting screen time guidelines and physical activity guidelines, respectively, were 1.32 and 1.13 times more likely to report first-class AA; but meeting the guidelines of physical activity was not significantly related to AA. Meeting the 24-HMG had the highest odds of achieving first-class AA (OR = 2.01, 95%CI: 1.47–2.73). In both sexes, adolescents who met 24-HMG self-reported better AA (boys OR = 2.05, 95%CI: 1.34–3.15; girls OR = 2.26, 95%CI: 1.36–3.76). Significant relationships were observed in adolescents from 9–10th grade, but not higher grades. Our research findings suggest that optimal movement behaviours can be seen as an important element to better academic achievement among U.S. adolescents. Future studies can adopt our discoveries to promote adolescents’ academic achievement through implementing optimal 24-h movement behaviour patterns.
Keywords: Sedentary behaviour; physical activity; sleep; academic performance; high school students; U.S.
The Health benefits of sufficient physical activity (PA), limited screen time (ST), or recommended duration of sleep for children and adolescents have been extensively investigated in previous studies [1–5]. Recently, as the three key components within a 24-h movement behaviour period [6], PA, ST, and sleep have been proposed to combine collectively in relevant research because of their interactions and co-dependence [7–10]. Time-use epidemiology provides a solid framework for researchers to integrate PA, sedentary behaviour and sleep in one day, as this combination can inform more reliable health messages and behaviour changes [8]. To this end, through a vigorous review process, the Canadian 24-h movement guidelines (24-HMG) for Children and Youth was developed and published in 2016 [6], which provides researchers with a novel research paradigm in the field of behaviour epidemiology. The 24-HMG suggests that adolescents and children should meet moderate-to-vigorous PA (≥60 min/day), ST (≤2 h/day), and duration of sleep (9–11 h/day for children aged from 11 to 13 and 8–10 h/day for 14 to 17-year-olds) [11]. Accumulating evidence has shown that individuals who adhered to the 24-HMG received physical and psychological benefits, like preventing obesity and improving cardio-metabolic, social and emotional health indicators [7,12]. Thus, there is a growing body of interest in public health research using the 24-HMG [13], supporting the integrated effects of combining PA, ST and sleep.
Previous studies have suggested that sufficient PA (at least 60 min per day or meeting the PA guidelines) [14,15], limited ST (≦2 h/day) [16,17] and sleep (meeting the age-appropriate duration) [18,19] were separately linked to academic achievement (AA) among adolescents and children. Furthermore, increasing PA level was positively and significantly related to optimal AA through improving cognitive functions in adolescents and children [14,15]. However, excessive ST was related to poorer AA in adolescents and children. One Chinese study showed that more time spent on ST, including watching television, social media time and videos, was negatively related to AA of adolescents [16]. Another study also indicated that ST was negatively related to academic performance among adolescents, but a similar result was not found in computer usage time [17]. With respect to other movement behaviour components, sufficient sleep can promote brain development and neuroplasticity, which may generate a positive outcome-optimizing verbal skills, intelligence quotient among adolescents and children [20]. As a result, adolescents and children with sufficient sleep would have better AA. Of note, a recent large-scale study indicated that a shorter duration of sleep was negatively related to AA among adolescents regardless of sex [18]. Moreover, research revealed that ethnicity may also play a potential effect on academic performance [21,22].
Numerous children and adolescent researchers have studied the relationship between meeting the 24-HMG with emotion (anxiety and depression), physical fitness, cognitive functions, obesity, as well as academic performance [23–25]. The findings are promising. For example, Canadian adolescents who adhered to 24-HMG were linked to better AA [11]. In another study including Australian primary school students, results indicated superior effects of adhering to a minimum of two guidelines over one alone in terms of literacy and numeracy levels [26]. The aforementioned studies have supported the integrated roles of 24-HMG in optimal AA in adolescents and children. However, it is acknowledged that previous evidence is still limited, which may reduce the generalizability of research findings. Thus, it is necessary to replicate and extend this research in other populations with different cultures to further corroborate associations between 24-HMG and AA in adolescents and children. Additionally, previous studies were not based on nationally representative samples. Using nationally representative samples is beneficial for improving the generalizability of research findings, which can inform policymakers in the design of effective initiatives. For this reason, the research purposes included: 1) to explore the relationship between meeting 24-HMG and AA high school students in the United States; 2) to determine whether the association could be influenced by sex and grade.
2.1 Research Design and Relevant Participants
Data used in the present research was retrieved from the 2019 cycle of the Youth Risk Behaviour Surveillance (YRBS). YRBS is a biennial and cross-sectional survey that is based on schools, and it is designed to study the behaviours related to health among students of high schools in the US by collecting representative samples nationwide. Most questions of YRBS has proven highly test-retest reliability, kappa = 61% to 100% [27]. To be specific, YRBS involves a cluster sample that is performed in three stages, and the students are recruited from private and public schools in grades 9 to 12 (age ranges: 12–18 years). The survey was conducted in person.
Of note, the present study included YRBS dating back to 2019 as this cycle (n = 13,677) represented the first administration in which PA, ST and duration of sleep were measured concurrently. Of the eligible participants, a total of 9127 participants aged 14–17 years provided data without missing values for all variables of interest in the 2019 cycle and were therefore included in the present study. We excluded participants aged 12–13 years, as the sample size only accounted for a tiny proportion of the overall sample (<2%). Overall response rates were above 60% during the administration of each cycle of the YRBS. Survey results were weighted to represent the national-level results. The data adopted in the present secondary analysis has been de-identified, and they are available to the public; for this reason, there is no need to obtain protocol approval from any institutional review board. As for the details on YRBS, please refer to https://www.cdc.gov/healthyyouth/data/yrbs.
Demographics. The participants provided their demographic data including sex (female or male), grade (9, 10, 11, 12), and ethnicity/race (Black/African American, White, Latino/Hispanic, or other), body weight and height for determination of body mass index (BMI) using a self-reported questionnaire.
Movement behaviours. Movement behaviours were operationalized according to the Canadian 24-h Movement Guidelines for Youth and Children [28]. Our analysis focused on the three threshold-based movement behaviour guidelines: recreational ST, moderate-to-vigorous PA (MVPA), and sleep. Items used to assess each of the movement behaviours have shown acceptable reliability and validity in previous epidemiological studies [27].
Physical activity. Participants responded to one item that asked: “For the past 7 days, how many days were you physically active for a total of at least 60 min every day”. Response options included “0–7 days”. Responses were dichotomized to represent whether participants met the guideline of engaging in ≥1 h of MVPA every day or not refer to the Canadian 24-h Movement Guidelines for Youth and Children [28]. The Canadian 24-h Movement Guidelines has been increasingly recognized as a new paradigm to investigate associations of physical activity, sedentary behaviour, and sleep with both physical and mental (brain-academic performance) health outcomes across different age groups. Thus, it can be applied in the current study including adolescents.
Screen time. Participants responded to two items that asked: “on average, at daytime, how many hours do you spend on the computer or video games, watch TV, or use the computer for things other than the schoolwork? (Including activities like Xbox, PlayStation, Game Boy, Nintendo, computer games and the Internet)”. Responses were dichotomized to represent whether participants met the guideline of engaging in ≤ 2h of ST per day or not according to Canadian 24-h Movement Guidelines for Youth and Children [28].
Sleep. Participants responded to one item that asked: “on average, at night time, how many hours do you spend on sleep?”. Responses have been dichotomized to represent whether participants met the guideline of 8–10 h of sleep per night for adolescents who are aged between 14 and 17, or not, refer to the Canadian 24-h Movement Guidelines for Youth and Children [28].
Academic achievement. The students have been told to provide the average scores they get in school. The response selections include mostly F’s, D’s, C’s, B’s, mostly A’s. The response of mostly A’s was treated as first-class AA, while others were treated-non-first-class AA. This item was used frequently in previous literature and surveys [19,29,30], despite no convincing evidence of its reliability and validity.
Statistical analysis.All analyses have been conducted with the aid of Stata 16.1 (Stata Corporation, College Station, TX, USA). Commands of the complex survey based on design have been adopted to regulate the complex design of the survey sample of the YRBS. Weights of the population have been included to regulate the unequal possibility of selection. The complete case was done to treat missing data (remove all the cases with missing data). Descriptive statistics were performed to describe the characteristics of the study sample. Binary analyses of logistic regression were performed to check the relationship between meeting combinations of the 24-HMG for MVPA (at least 60 min), screen time (no more than 2 h), and duration of sleep (8–10 h for ages 14–17 years) and AA (first-class vs. non-first-class grades). All the students were classified and included in one of 8 types of guidelines adherence below: MVPA and screen time, sleep and MVPA, sleep and screen time, only MVPA, only screen time, only sleep and none, or all three guidelines. Covariates included ethnicity, body mass index, sex and age. Statistical significance has been defined as P < 0.05.
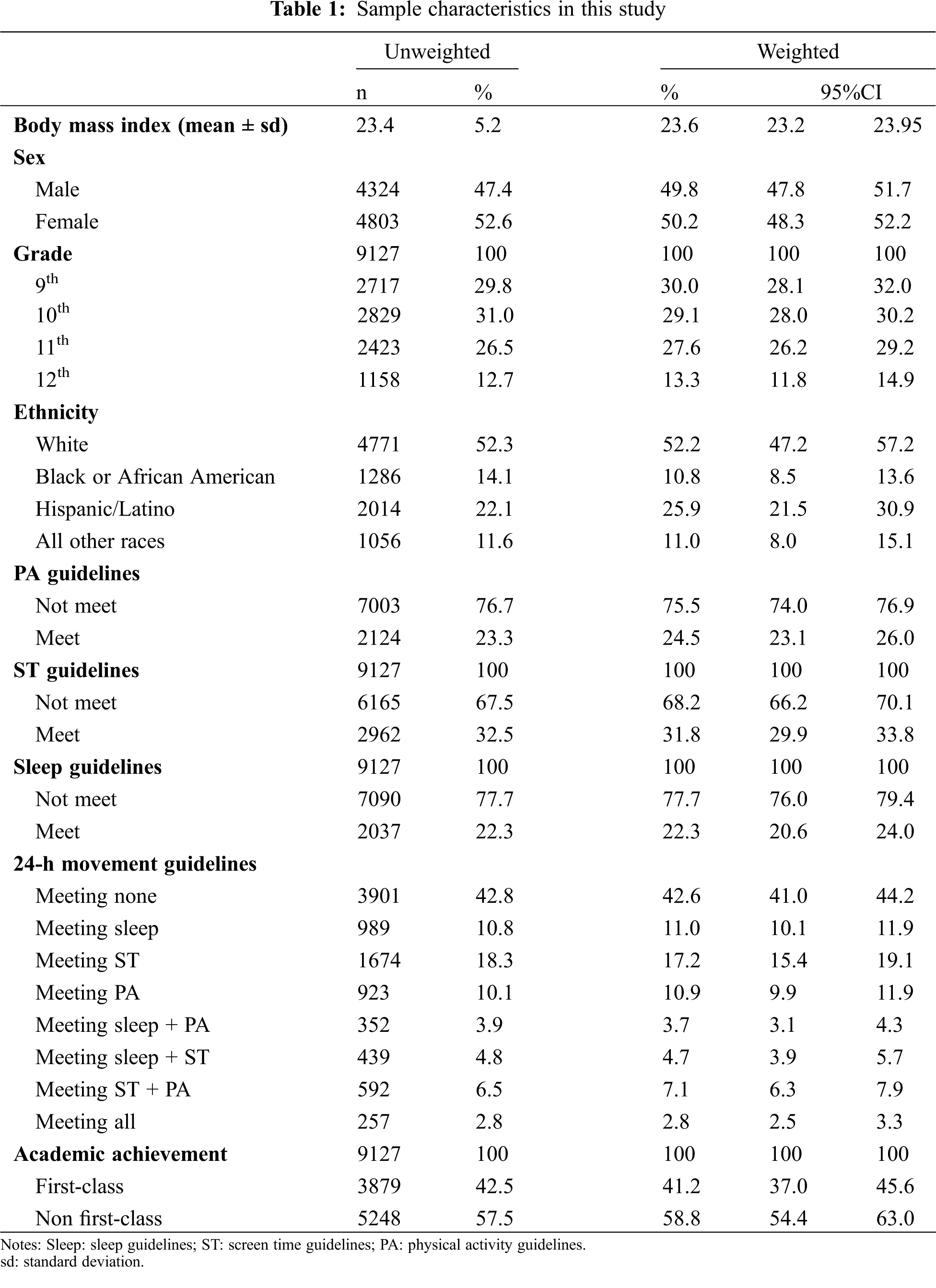
This study consisted of 9127 adolescents (males = 47.4%) with average BMI: 23.4 ± 5.2 kg/m2. 31% of the participants were 10th graders at the highest level, while the lowest percentage was 12.7% (12th graders). White adolescents accounted for 52.3% of the study sample, being the highest proportion as compared to other ethnic groups. The prevalence of adherence to each guideline (PA, ST, and sleep), was 23.3%, 32.5% and 22.3%, respectively. The prevalence of meeting all of the guidelines of movement behaviour within 24 h was 2.8%. The percentage of first-class AA was 42.5%. Information and weighted values are detailed in Table 1.
In Table 2, the results obtained through the logistic regression for the relationship between 24-h movement guidelines and first-class AA are shown. Compared with meeting none of the recommendations, meeting any of the combined guidelines (except for meeting the PA guidelines) was significantly related to higher odds for first-class AA. Meeting the sleep guideline had a 1.42 times greater likelihood to report first class AA compared with meeting none. Meeting the ST guideline and PA guideline, respectively, were 1.32 and 1.13 times greater to report first-class AA; but meeting the PA guidelines was not significantly related to AA. Meeting all of the 24-h movement guidelines showed the greatest odds for reporting first-class AA (OR = 2.01, 95%CI: 1.47–2.73).
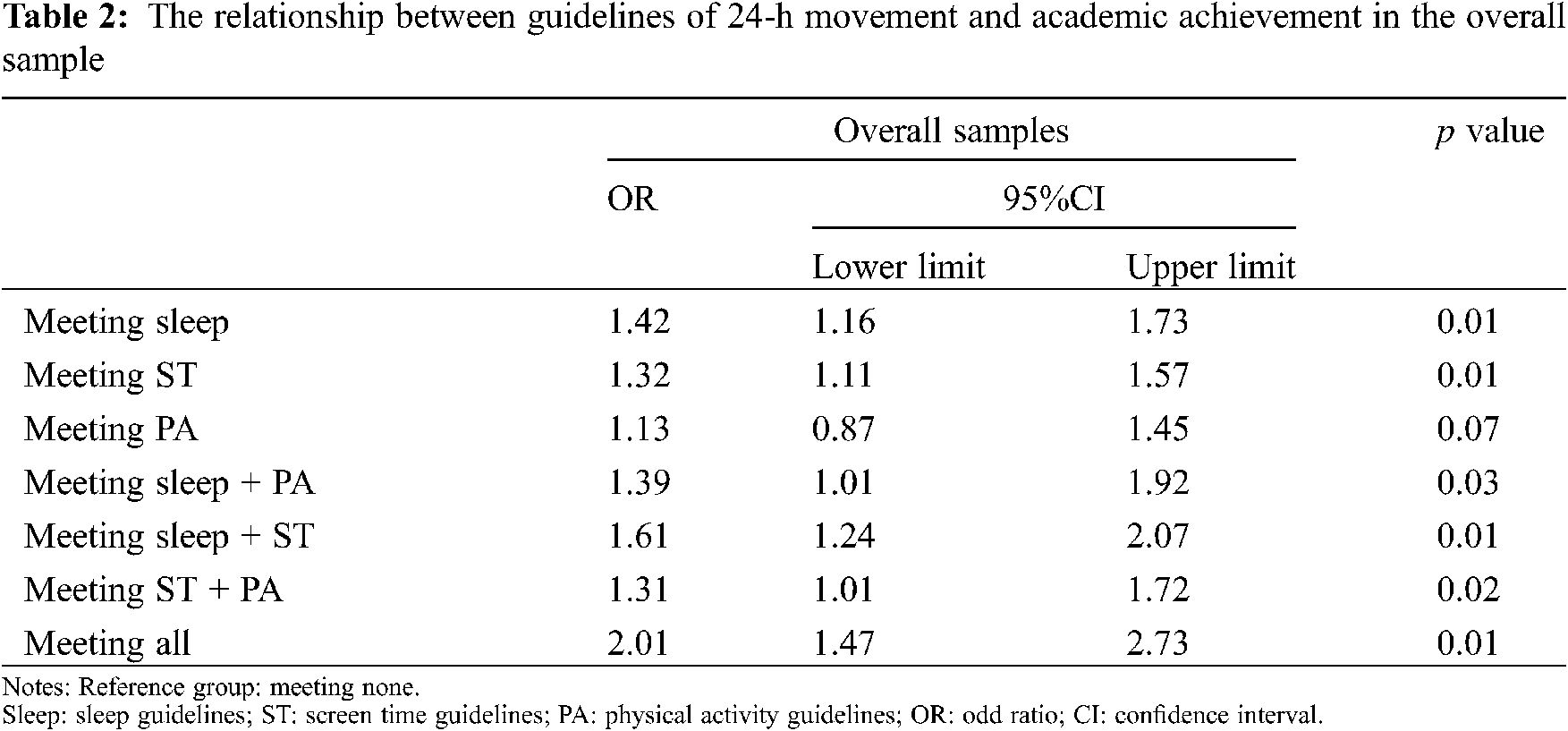
Models controlled for sex, grade, ethnicity/race and body mass index.
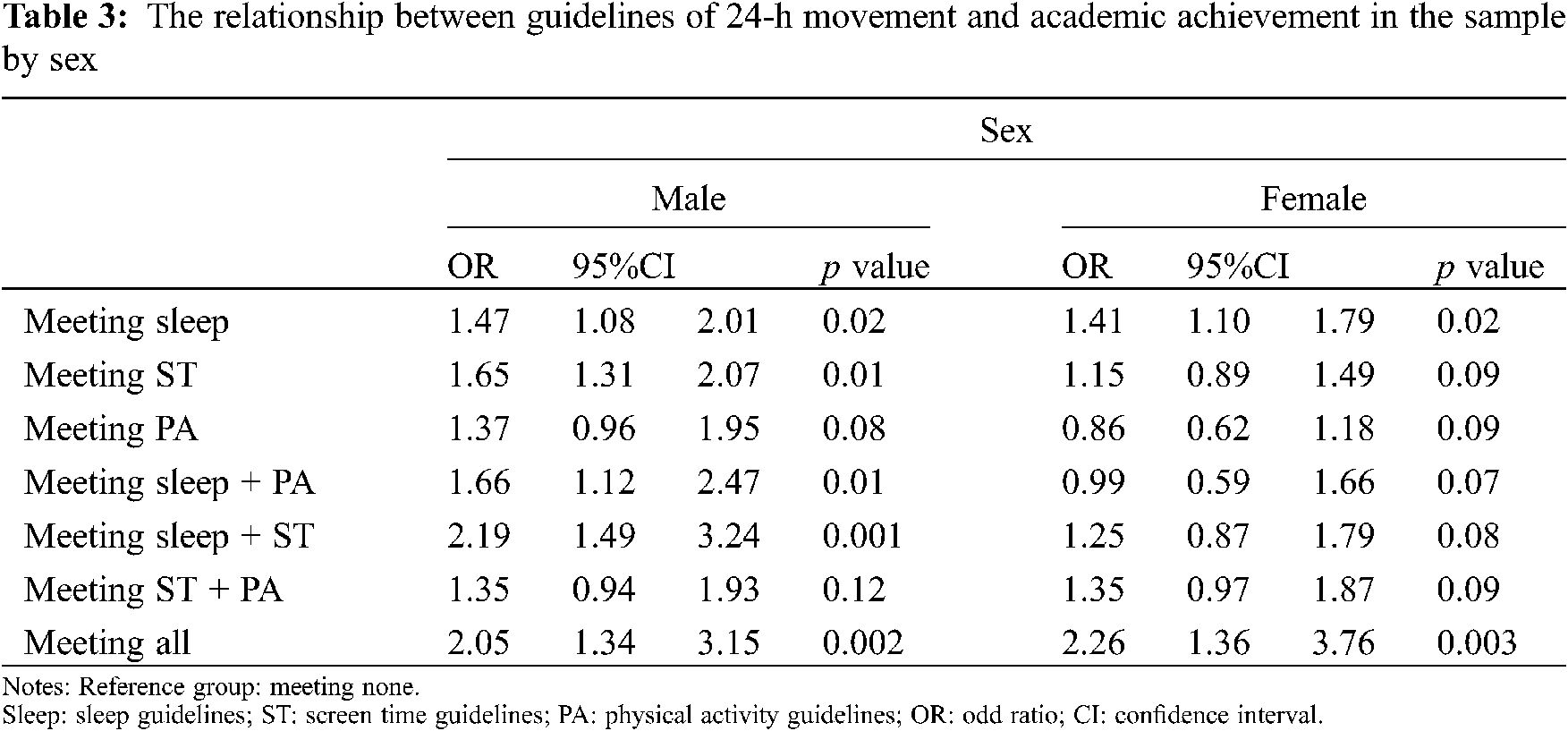
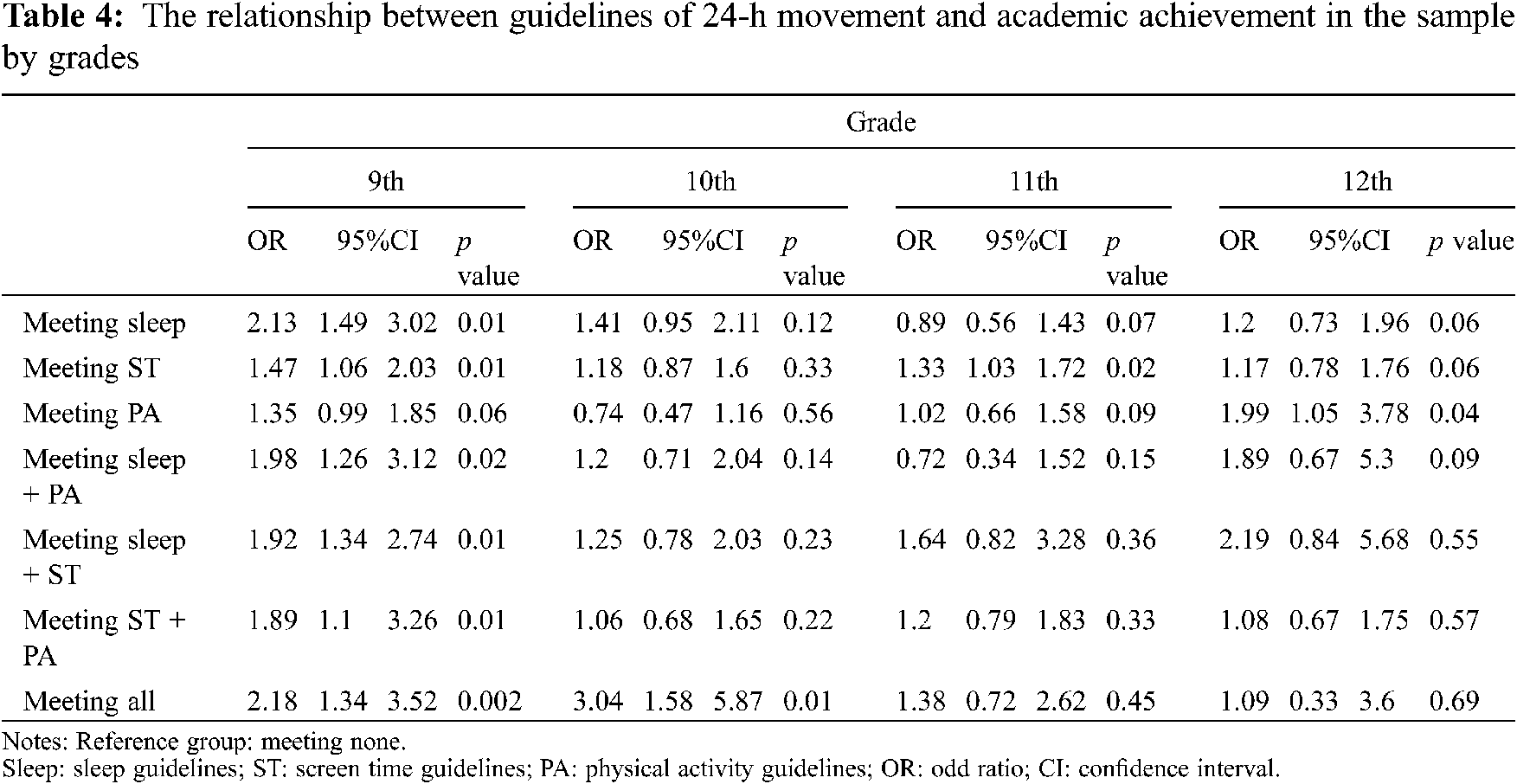
Data on the relationship between 24HMG and first-class AA in both sexes are presented in Table 3. Meeting all of the 24-h movement guidelines showed the greatest odds for reporting first-class AA (male OR = 2.05, 95%CI: 1.34–3.15; female OR = 2.26, 95%CI: 1.36–3.76). The relationship between 24-h movement guidelines and first-class AA across all ethnic groups are presented in Table 4. Interestingly, meeting the 24HMG is only significantly related to first-class AA in 9th and 10th-grade students.
Models controlled for grade, ethnicity/race and body mass index.
Models controlled for sex, ethnicity/race and body mass index.
The present study identified the relationship between the 24-h movement guidelines and AA using a representative sample of high school students based on the YRBS 2019 cycle. The current study found that in U.S. adolescents aged 14–17, roughly 3% of included participants met all of the 24HMG, indicating concerning levels of healthy movement behaviours. Another major research finding is that adolescents who adhered to the 24-h movement guidelines had a higher likelihood of achieving first-class AA. The significant relationship between 24-h movement guidelines and better AA (first-class) varied across sexes and grades.
Less than 3% of the U.S. youth met the 24-h movement guidelines in the present study that indicates a lower adherence to the guidelines compared to previous research [12,31,32]. This level indicates a concerning trend for U.S. youth’s movement behaviour, which may threaten clinical and public health outcomes, as several research has indicated the health benefits of adherence to the 24-h movement guidelines. Specifically, using Chinese nationally representative samples, Chen et al. [33] found that 5% of Chinese adolescents and children met the 24-h movement guidelines, which is slightly higher than the generated number in the present study. Our data on the adherence to 24-h movement guidelines is also lower than some national levels [34,35] but higher than those in South Korea [36]. The inconsistent levels of adherence to the 24-h movement guidelines may be due to survey data collected at different times and with different measurement tools. However, it should be noted that unhealthy movement behaviour in the U.S. youth is highly prevalent, which should be addressed by effective public health approaches [37]. Owing to limited evidence regarding how to efficiently optimize healthy movement behaviour, more relevant research on promoting movement behaviour separately and concurrently should be encouraged.
Consistent with past studies [11], our study showed that meeting 24-h movement guidelines was related to better self-reported AA in adolescents. A possible explanation for the significant relationship is cognition, as a recent study indicated that optimal 24-h movement behaviour was related to better cognition in children [24], which in turn probably contributes to better AA. However, our study cannot fully explain the underlying mechanism linking 24-h movement guidelines to better AA in adolescents, which requires further investigation by adding cognitive measures during EEG, fNIRS, and/or fMRI. Regarding the health benefits of adherence to the 24-h movement guidelines [33,38,39], it is recommended to improve levels of each behaviour to meet the 24-h movement guidelines for health promotion. Numerous studies have reported Health promotion benefits of interventions to improve children and youth of PA, particularly in educational settings [40,41]. Such interventions may enhance adherence to PA guidelines. For example, a multicomponent school-based intervention for one academic year has shown significant improvements in health behaviours including 24-h movement guidelines [42]. This study suggests potential opportunities to address PA disparities in children and adolescents through sustainable health promotion efforts, which should be considered alongside other multipronged interventions.
Interestingly, our study also revealed that meeting the PA guidelines alone was not related to better AA. This research finding is inconsistent with prior research [43–45]. However, we further found that meeting combinations of either ST or sleep guidelines and PA guidelines was related to better AA. This interesting finding is inconsistent with Lien et al. [11] in which appropriate duration of sleep or limited ST was not an important factor separately for promoting better AA while stressing the positive roles of meeting the PA guidelines. The discrepant research finding between the current study and Lien et al. [11] may be due to different cut-offs of AA in the analysis. In our study, AA was divided into first-class and non-first class, which was different from Lien et al [11]. Another explanation for this inconsistency may be sample characteristics, such as varied age groups or different perceptions of questionnaire questions. Hence, these two differences may explain the controversial research finding. In our study, the roles of limited ST and sufficient duration of sleep for promoting better AA should be confirmed, and its associated underlying mechanism should be further explored.
When looking at the sex difference in the relationship between 24-h movement guidelines and better AA, more interesting research findings were observed. In boys, those adolescents who met sleep guidelines separately or concurrently in any combination of PA or ST guidelines displayed higher odds for better AA, whereas a similar finding was not observed in girls. The underlying mechanism explaining this cannot be proposed in the present study, but this study stresses the potential roles of the appropriate duration of sleep in promoting better AA in male adolescents. For female adolescents, meeting the PA, ST and sleep guidelines concurrently might be the most significant to secure better AA. These assumptions are merely based on our results, which should be confirmed or negated in the future by research with more rigorous research designs.
Grade differences were also observed in the relationship between 24-h movement guidelines and better AA in the current study. This is consistent with previous studies’ findings [11], suggesting in adolescents of higher grades, the association between 24-h movement guidelines and better AA may not exist. In the current study, we found that meeting the 24-h movement guidelines was related to better AA in adolescents of 9th and 10th grades only, rather than 11–12th grades. Despite the absence of convincing interpretation for this research finding, some possible explanations can be applied in the context of this study. In later grades, the difficulty of academic activities would also increase, which in turn may require the students in later grades to spend more time on academic activities. Such increased workload of high school courses is likely to occupy a larger proportion of time limiting opportunities for sufficient PA and adequate duration of sleep. This might be an influencing factor resulting in a non-significant relationship between 24-h movement behaviours and better AA in adolescents of higher grades.
Some limitations should be acknowledged. One of the limitations of this study was that our findings were from a cross-sectional design, which cannot be applied to infer a causal relationship. Future research is needed to conduct experiments to verify our research findings. Furthermore, despite that the results from logistic regression analysis, it is still unknown whether higher academic performance is the cause or consequence of meeting the 24-h movement guidelines. The influence might be bidirectional. Another limitation was the self-report measures used to assess the independents and dependents of our study, including measurement of BMI, which involved the social desirability and recall bias of participants [46]. The last limitation was using single-item measurements and the crude data it provided. For instance, sleep health cannot be determined with individual-item measures which only requires quantity rather than quality. Similarly, a 7-day PA recall question may not reflect the typical PA behaviours, depending on the time when the survey was performed.
Overall, meeting the 24-h movement guidelines appears to be a positive correlate of better AA in adolescents. Future studies should include longitudinal designs including interventions and collecting objective measures for movement behaviours to determine the current causality of the relationships.
Acknowledgement: The authors hope to give thanks to the availability of data provided by the YRBS survey.
Author Contribution:
Study Design: LYZ, AFK, SYL
Data Analysis: YPZ, MMH
Manuscript Draft: SYL, LYZ; RB; JY
Manuscript Revision: XL, JXY, QY, JY, LYZ, SD
Founding Statement: This project was financially supported by the National Social Science Foundation (217BTY032) and Key Project from the Social Science Foundation of Hunan Province (16ZDB015).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the current study.
1. Carson, V. (2016). Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Applied Physiology, Nutrition, and Metabolism, 41(6 (Suppl. 3)), S240–S265. DOI 10.1139/apnm-2015-0630. [Google Scholar] [CrossRef]
2. Chaput, J. P. (2016). Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism, 41(6 (Suppl. 3)), S266–S282. DOI 10.1139/apnm-2015-0627. [Google Scholar] [CrossRef]
3. Poitras, V. J. (2016). Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism, 41(6 (Suppl. 3)), S197–S239. DOI 10.1139/apnm-2015-0663. [Google Scholar] [CrossRef]
4. Shen, H. (2020). Prevalence of physical activity and sedentary behavior among Chinese children and adolescents: Variations, gaps and recommendations. International Journal of Environmental Research and Public Health, 17(9), 3066. DOI 10.3390/ijerph17093066. [Google Scholar] [CrossRef]
5. Chen, S. T., Yan, J. (2020). Prevalence and selected sociodemographic of movement behaviors in school children from low-and middle-income families in Nanjing, China: A cross-sectional questionnaire survey. Children, 7(2), 13. DOI 10.3390/children7020013. [Google Scholar] [CrossRef]
6. Tremblay, M. S. (2016). Canadian 24-h movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism, 41(6 (Suppl. 3)), S311–S327. DOI 10.1139/apnm-2016-0151. [Google Scholar] [CrossRef]
7. Carson, V. (2017). Health associations with meeting new 24-h movement guidelines for Canadian children and youth. Preventive Medicine, 95(5), 7–13. DOI 10.1016/j.ypmed.2016.12.005. [Google Scholar] [CrossRef]
8. Pedišić, Ž., Dumuid, D., Olds, T. S. (2017). Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: Definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology, 49(2), 252–269. [Google Scholar]
9. Buman, M. P. (2014). Reallocating time to sleep, sedentary behaviors, or active behaviors: Associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. American Journal of Epidemiology, 179(3), 323–334. DOI 10.1093/aje/kwt292. [Google Scholar] [CrossRef]
10. Donnelly, J. E. (2016). Physical activity, fitness, cognitive function, and academic achievement in children. Medicine & Science in Sports & Exercise, 48(6), 1197–1222. DOI 10.1249/MSS.0000000000000901. [Google Scholar] [CrossRef]
11. Lien, A. (2020). Adherence to 24-h movement guidelines and academic performance in adolescents. Public Health, 183, 8–14. DOI 10.1016/j.puhe.2020.03.011. [Google Scholar] [CrossRef]
12. Janssen, I. (2017). Is adherence to the Canadian 24-h movement behaviour guidelines for children and youth associated with improved indicators of physical, mental, and social health? Applied Physiology, Nutrition, and Metabolism, 42(7), 725–731. DOI 10.1139/apnm-2016-0681. [Google Scholar] [CrossRef]
13. Wu, X. Y. (2017). The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS One, 12(11), e0187668. DOI 10.1371/journal.pone.0187668. [Google Scholar] [CrossRef]
14. Singh, A. S. (2019). Effects of physical activity interventions on cognitive and academic performance in children and adolescents: A novel combination of a systematic review and recommendations from an expert panel. British Journal of Sports Medicine, 53(10), 640–647. DOI 10.1136/bjsports-2017-098136. [Google Scholar] [CrossRef]
15. Rasberry, C. N. (2011). The association between school-based physical activity, including physical education, and academic performance: A systematic review of the literature. Preventive Medicine, 52, S10–S20. DOI 10.1016/j.ypmed.2011.01.027. [Google Scholar] [CrossRef]
16. Yan, H. (2017). Associations among screen time and unhealthy behaviors, academic performance, and well-being in Chinese adolescents. International Journal of Environmental Research and Public Health, 14(6), 596. DOI 10.3390/ijerph14060596. [Google Scholar] [CrossRef]
17. Peiró-Velert, C. (2014). Screen media usage, sleep time and academic performance in adolescents: Clustering a self-organizing maps analysis. PLoS One, 9(6), e99478. DOI 10.1371/journal.pone.0099478. [Google Scholar] [CrossRef]
18. Hysing, M. (2016). Sleep and academic performance in later adolescence: Results from a large population-based study. Journal of Sleep Research, 25(3), 318–324. DOI 10.1111/jsr.12373. [Google Scholar] [CrossRef]
19. Burns, R. D. (2018). Relationships among physical activity, sleep duration, diet, and academic achievement in a sample of adolescents. Preventive Medicine Reports, 12(5), 71–74. DOI 10.1016/j.pmedr.2018.08.014. [Google Scholar] [CrossRef]
20. Short, M. A. (2018). Cognition and objectively measured sleep duration in children: A systematic review and meta-analysis. Sleep Health, 4(3), 292–300. DOI 10.1016/j.sleh.2018.02.004. [Google Scholar] [CrossRef]
21. Blair, S. L., Blai, M. C. L., Madamba, A. B. (1999). Racial/ethnic differences in high school students’ academic performance: Understanding the interweave of social class and ethnicity in the family context. Journal of Comparative Family Studies, 30(3), 539–555. DOI 10.3138/jcfs.30.3.539. [Google Scholar] [CrossRef]
22. Salamonson, Y., Andrew, S. (2006). Academic performance in nursing students: Influence of part-time employment, age and ethnicity. Journal of Advanced Nursing, 55(3), 342–349. DOI 10.1111/j.1365-2648.2006.03863_1.x. [Google Scholar] [CrossRef]
23. Saunders, T. J. (2016). Combinations of physical activity, sedentary behaviour and sleep: Relationships with health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism, 41(6), 283–293. DOI 10.1139/apnm-2015-0626. [Google Scholar] [CrossRef]
24. Walsh, J. J. (2018). Associations between 24 h movement behaviours and global cognition in US children: A cross-sectional observational study. The Lancet Child & Adolescent Health, 2(11), 783–791. DOI 10.1016/S2352-4642(18)30278-5. [Google Scholar] [CrossRef]
25. Ghildiyal, R. (2015). Role of sports in the development of an individual and role of psychology in sports. Mens Sana Monographs, 13(1), 165. DOI 10.4103/0973-1229.153335. [Google Scholar] [CrossRef]
26. Watson, A. (2021). Associations between meeting 24-h movement guidelines and academic achievement in Australian primary school-aged children. Journal of Sport and Health Science, 140(Suppl. 3), S240. DOI 10.1016/j.jshs.2020.12.004. [Google Scholar] [CrossRef]
27. Brener, N. D. (1995). Reliability of the youth risk behavior survey questionnaire. American Journal of Epidemiology, 141(6), 575–580. DOI 10.1093/oxfordjournals.aje.a117473. [Google Scholar] [CrossRef]
28. Tremblay, M. S. (2016). Canadian 24-h movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Applied Physiology, Nutrition, and Metabolism, 41(6 (Suppl. 3)), S311–S327. DOI 10.1139/apnm-2016-0151. [Google Scholar] [CrossRef]
29. Burns, R. D. (2020). Sports participation correlates with academic achievement: Results from a large adolescent sample within the 2017 U.S. national youth risk behavior survey. Perceptual and Motor Skills, 127(2), 448–467. DOI 10.1177/0031512519900055. [Google Scholar] [CrossRef]
30. Rasberry, C. N. (2017). Health-related behaviors and academic achievement among high school students-United States, 2015. Morbidity and Mortality Weekly Report, 66(35), 921–927. DOI 10.15585/mmwr.mm6635a1. [Google Scholar] [CrossRef]
31. Patte, K. A. (2020). Are one-year changes in adherence to the 24-h movement guidelines associated with depressive symptoms among youth? BMC Public Health, 20(1), 1–12. DOI 10.1186/s12889-020-08887-z. [Google Scholar] [CrossRef]
32. Santos, R. (2017). Compliance with the Australian 24-h movement guidelines for the early years: Associations with weight status. BMC Public Health, 17(5), 199–205. DOI 10.1186/s12889-017-4857-8. [Google Scholar] [CrossRef]
33. Chen, S. T. (2020). Meeting 24-h movement guidelines: Prevalence, correlates and the relationships with overweight and obesity among Chinese children and adolescents. Journal of Sport and Health Science, 10(3), 349–359. DOI 10.1016/j.jshs.2020.07.002. [Google Scholar] [CrossRef]
34. Gallant, F. (2020). One size does not fit all: Identifying clusters of physical activity, screen time, and sleep behaviour co-development from childhood to adolescence. International Journal of Behavioral Nutrition and Physical Activity, 17(1), 58. DOI 10.1186/s12966-020-00964-1. [Google Scholar] [CrossRef]
35. Roman-Viñas, B. (2016). Proportion of children meeting recommendations for 24-h movement guidelines and associations with adiposity in a 12-country study. International Journal of Behavioral Nutrition and Physical Activity, 13(1), 123. DOI 10.1186/s12966-016-0449-8. [Google Scholar] [CrossRef]
36. Lee, E. Y. (2020). Six-year trends and intersectional correlates of meeting 24-h movement guidelines among South Korean adolescents: Korea youth risk behavior surveys 2013-2018. Journal of Sport and Health Science, 54(Suppl. 3), 308. DOI 10.1016/j.jshs.2020.11.001. [Google Scholar] [CrossRef]
37. Wilfley, D. E., Hayes, J. F., Balantekin, K. N., van Buren, D. J., pstein, L. H. (2018). Behavioral interventions for obesity in children and adults: Evidence base, novel approaches, and translation into practice. American Psychologist, 73(8), 981–993. DOI 10.1037/amp0000293. [Google Scholar] [CrossRef]
38. Hinkley, T. (2020). Prospective associations with physiological, psychosocial and educational outcomes of meeting Australian 24-h movement guidelines for the early years. International Journal of Behavioral Nutrition and Physical Activity, 17(1), 36. DOI 10.1186/s12966-020-00935-6. [Google Scholar] [CrossRef]
39. Dumuid, D. (2021). Balancing time use for children’s fitness and adiposity: Evidence to inform 24-h guidelines for sleep, sedentary time and physical activity. PLoS One, 16(1), e0245501. DOI 10.1371/journal.pone.0245501. [Google Scholar] [CrossRef]
40. van de Kop, J. H. (2019). School-based physical activity interventions in prevocational adolescents: A systematic review and meta-analyses. Journal of Adolescent Health, 65(2), 185–194. DOI 10.1016/j.jadohealth.2019.02.022. [Google Scholar] [CrossRef]
41. Owen, M. B. (2017). The effectiveness of school-based physical activity interventions for adolescent girls: A systematic review and meta-analysis. Preventive Medicine, 105(1), 237–249. DOI 10.1016/j.ypmed.2017.09.018. [Google Scholar] [CrossRef]
42. Sevil, J. (2019). Can high schools be an effective setting to promote healthy lifestyles? Effects of a multiple behavior change intervention in adolescents. Journal of Adolescent Health, 64(4), 478–486. DOI 10.1016/j.jadohealth.2018.09.027. [Google Scholar] [CrossRef]
43. Fox, C. K. (2010). Physical activity and sports team participation: Associations with academic outcomes in middle school and high school students. Journal of School Health, 80(1), 31–37. DOI 10.1111/j.1746-1561.2009.00454.x. [Google Scholar] [CrossRef]
44. Burns, R. D., Bai, Y., Brusseau, T. A. (2020). Physical activity and sports participation associates with cognitive functioning and academic progression: An analysis using the combined 2017–2018. National Survey of Children’s Health. Journal of Physical Activity and Health, 17(12), 1197–1204. DOI 10.1123/jpah.2020-0148. [Google Scholar] [CrossRef]
45. Singh, A. S. (2019). Effects of physical activity interventions on cognitive and academic performance in children and adolescents: A novel combination of a systematic review and recommendations from an expert panel. British Journal of Sports Medicine, 53(10), 640–647. DOI 10.1136/bjsports-2017-098136. [Google Scholar] [CrossRef]
46. Nuttall, F. Q. (2015). Body mass index: Obesity, BMI, and health: A critical review. Nutrition Today, 50(3), 117–128. DOI 10.1097/NT.0000000000000092. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |