
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/ijmhp.2022.018017
ARTICLE
Efficacy of a Community-Based Trauma Recovery Program after a Fire Disaster
1Red Cross College of Nursing, Chung-Ang University, Seoul, Korea
2Department of Nursing, Daewon University College, Jecheon, Korea
*Corresponding Author: Dong-Hee Cho. Email: psydh@cau.ac.kr
Received: 23 June 2021; Accepted: 18 October 2021
Abstract: As industries develop, fire disasters and their associated damage are increasing. Investigating the mental health of victims is imperative because this is an essential issue for community recovery after a disaster. This study was conducted to determine the efficacy of a program implemented by a community mental health center based on the investigation of the victims’ depression and post-traumatic stress disorder (PTSD) levels immediately after the disaster and at one-year follow-up. As a result, victims’ depression and PTSD recovered over time, and more changes were confirmed. In particular, the high-risk group for PTSD showed a high program participation rate, and there was significant recovery over time compared with the group without PTSD. Based on these results, community mental health programs are an effective way to increase community mental health after disasters. In the future, community-based recovery programs after disasters should be expanded, and administrative support for them should be developed.
Keywords: Fire; disaster victims; post-traumatic stress disorder; depression; community mental health services
According to the National Emergency Management Agency [1], a large-scale fire disaster is generally defined as a fire in which property damage is estimated to be ≥5 billion KRW, five or more people have died, or ≥10 people have been injured. As industries develop, both the number and scale of fire disasters are increasing. The concept of a disaster is socially defined, managed, and studied because its impact causes a wide range of damage to communities beyond individuals [2–4]. Disaster management is performed at the national level, and socially, it is constantly emphasized that disaster management should be performed at the public level for disaster prevention, preparedness, response, and recovery [5,6]. In this context, the effects of disasters, especially on mental health and its related factors, are important topics, and interest in trauma and post-disaster psychosocial support is increasing as a public health [7,8].
Previous studies [9,10] have focused on the victims’ post-traumatic stress disorder (PTSD) level, related influential factors, psychological intervention effects, and follow-up support. Influential factors affecting PTSD include demographic characteristics such as gender, age, education level, socioeconomic level, variables other than the trauma experience, such as the type and intensity of the disaster, frequency of exposure, and characteristics of the disaster process, such as mental health symptoms at the time of the disaster. In addition, family relationships, support systems, and secondary stressors surrounding trauma after a disaster have been suggested. Furthermore, post-disaster victims experience PTSD at a high rate and are known to experience depression followed by other issues that require intervention in mental health such as anxiety disorders, alcohol dependence/abuse, and sleep disorders [11,12].
However, the fact that the physical and psychological reactions experienced by disaster victims in the early stages of a disaster are normal reactions to unusual situations and will naturally recover after a certain period of time should not be overlooked [13]. There have been many studies, including longitudinal studies, on the natural recovery course of PTSD, confirming that most people recover on their own within a few months after a traumatic event and that there is a natural resilience after trauma [14]. Although some longitudinal studies have reported that the symptoms and prevalence of mental illness peak within a year of a disaster and then improve over time [9,15] disasters have been associated with only one long-term outcome. Studies have suggested that experiencing a disaster can lead to additional mental health problems even after many years [16,17].
Since a disaster is a traumatic event that cannot be accepted by an individual, the subsequent effects are mainly explained by PTSD; however, other psychiatric problems can also occur. According to a previous study, approximately 78% of victims diagnosed with PTSD will receive one or more additional mental health examinations in their lifetimes [18], and both mood disorders [19] and anxiety disorders [19,20] are common; some view PTSD as followed by mood and anxiety disorders [20]. As such, the effects on mental health after a disaster appear as various and complex transformations over a long period of time [12], suggesting that investigating the characteristics of the disaster and various variables is necessary.
According to previous studies, disaster research in Korea tends to focus more on disaster management administrative systems and the material and economic aspects of disasters. In addition, although the severity of psychological damage for victims of manmade disasters is expected to be more serious, it has the lowest ratio among disaster-related studies, so it is a subject requiring priority attention [21,22].
However, in the case of disaster victims who have not received sufficient attention from society, the fragmentary identification of the situation and support are provided, and the lack of research makes them vulnerable to long-term effects. In addition, since insufficient studies have demonstrated the effectiveness of psychological support and recovery programs provided in communities, further studies are needed [23].
Therefore, the long-term impact on mental health after a fire disaster must be confirmed to provide appropriate community mental health interventions. This study aims to explore 1) the changes in depression and PTSD risk in fire disaster victims over time and 2) the efficacy of community recovery programs for disasters through a retrospective descriptive analysis. This study is expected to provide primary data necessary to support fire disaster victims in the future.
The participants in this study were survivors and bereaved families who experienced a fire at the Jecheon Sports Centre in 2017. Among them, we analyzed data from 116 cases collected with participant consent to a questionnaire from a mental health service organization. These data were non-personally identifiable and coded data including the mental health status of the subjects at the time of the disaster and how their mental health had changed one year later.
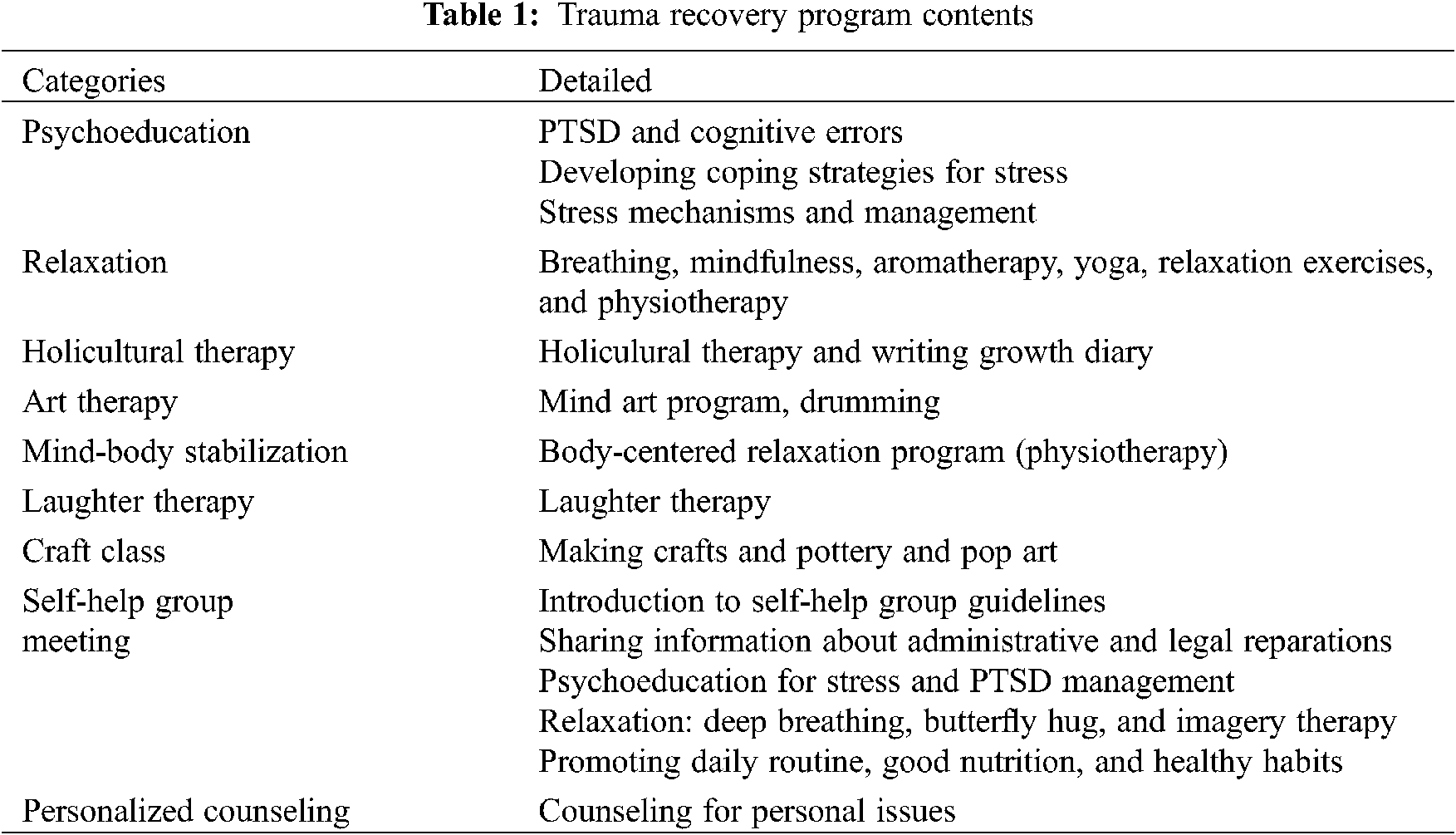
After the fire disaster, mental health services implemented at the public community mental health center in Jecheon included case management, mobile counseling, self-help groups, individual counseling, and various kinds of recovery programs. Table 1 shows the contents of the recovery programs that were implemented.
The level of depression among participants was measured using the Patient Health Questionnaire-9 (PHQ-9). PHQ-9 was developed by Spitzer et al. [24] and consists of nine factors: a sense of discomfort, depression, sleep changes, fatigue, changes in appetite, feelings of guilt or worthlessness, poor concentration, restlessness or suffocation, and suicidal thoughts in the previous two weeks. The total score is 27 on a four-point Likert scale from 0 (not at all) to 3 (almost every day). This study used the Korean version of the PHQ-9, which was translated and standardized by Park et al. [25]; as a result, a score of 0–4 points indicated the normal range (normal), a score of 5–9 points indicated the suspicious group (doubt), and a score >10 points indicated high-risk group. In the study by Park et al. [25], Cronbach’s α was 0.84; in this study, Cronbach’s α was 0.88.
The participants’ post-traumatic stress levels were measured using the PTSD Checklist–Civilian version (PCL-C) questionnaire, which is a self-report questionnaire tool for diagnosing PTSD or for screening high-risk groups, developed by Weathers that is widely used in research and clinical fields. In this study, the Korean version of the PCL-C that was translated and validated by Oh et al. [26] was used; it consists of 17 items each of which are measured on a five-point Likert scale from 1 (not at all) to 5 (very much), the total ranges from 17–85 points. The cut-off score of 44 points recommended by Blanchard et al. [27] was applied. Cronbach’s α was confirmed to be 0.94 in the study by Conybeare et al. [28] and was 0.93 in this study.
The data collection for this study was conducted through self-report questionnaires with the guidance of mental health professionals at the mental health welfare center in Jecheon-si during the course of participating in the case management and recovery programs provided for victims of fire disasters. Mental health professionals who collected data completed training on Psychological First Aid (PFA) and PTSD and received training for one day on the meaning, terminology, and contents of the questionnaire. The first collection period was 2017.12.30–2018.01.05 immediately after the disaster, and the second period was 2019.01.07–2019.12.06, which was more than a year later.
Data analysis was performed using SPSS 26.0, and the general characteristics were analyzed using frequency analysis and descriptive statistics. The t-test was used to compare post-traumatic stress and depression between survivors and bereaved families, and repeated measurement ANOVA and post hoc analysis were used to compare the effects of depression and post-traumatic stress according to participation in recovery programs.
3.1 General Participant Characteristics
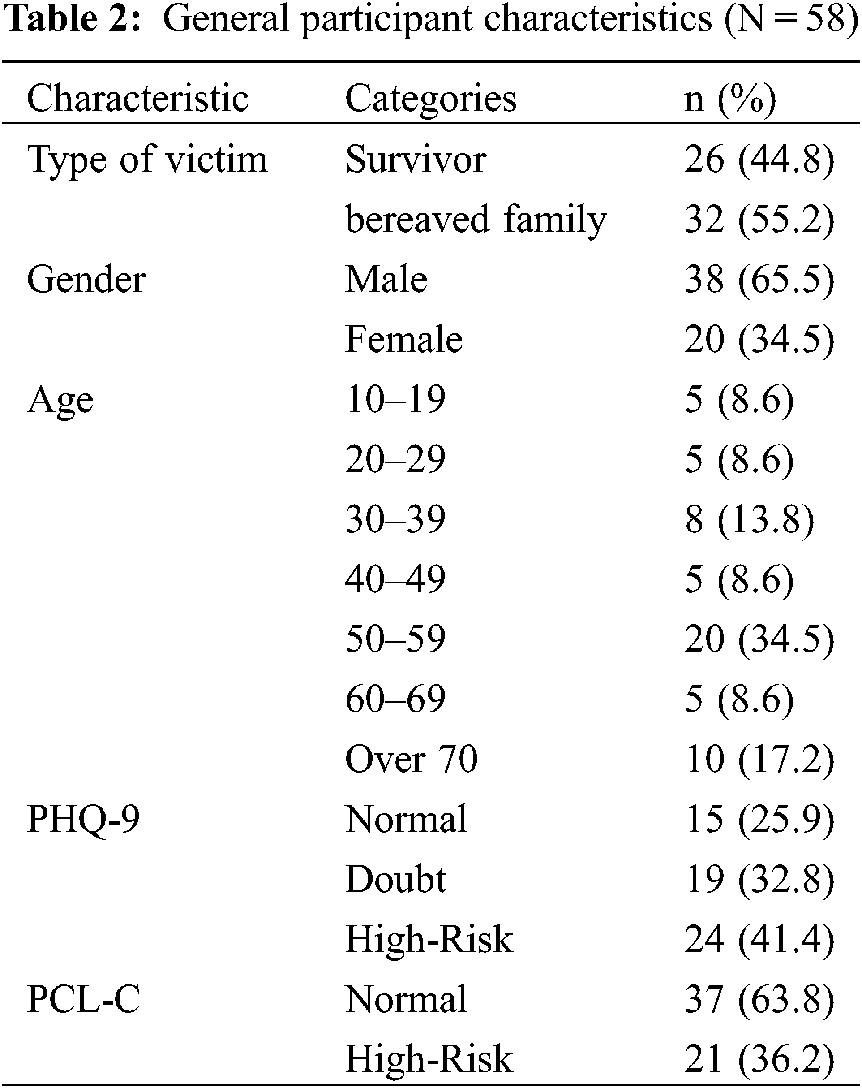
There were 58 participants in this study in total, among whom 38 (65.5%) were male, and 20 (34.5%) were female (Table 2). The most common age group was in their 50s (34.5%). Fig. 1 shows the high-risk group for depression decreased from 24 (41.4%) subjects immediately after the disaster to 15 (25.9%) subjects after one year. In addition, the number of subjects in the high-risk group for post-traumatic stress decreased from 21 (36.2%) to 12 (20.7%).
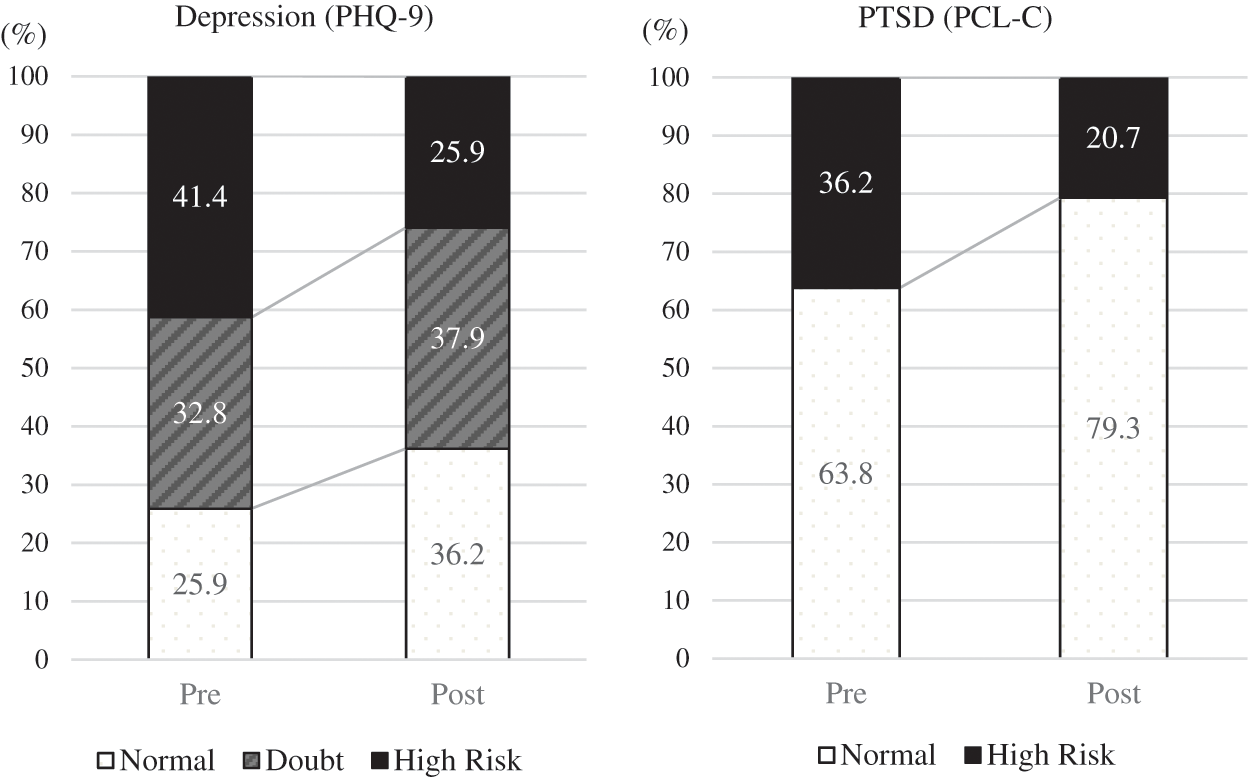
Figure 1: Comparison of participants’ depression and PTSD levels over time
3.2 Mental Health of Victims according to General Characteristics
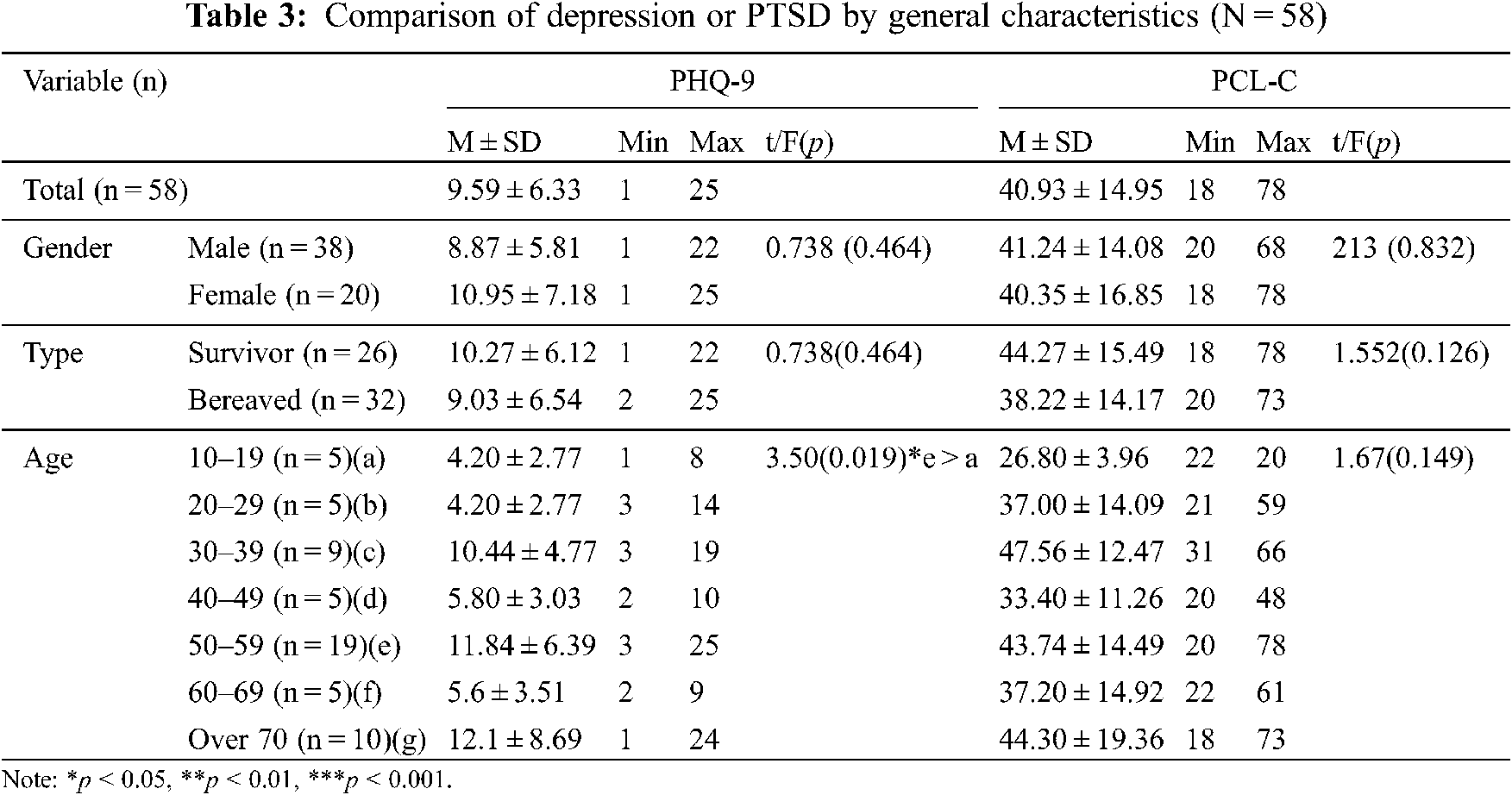
Table 3 shows the comparison of victims’ mental health according to general characteristics. According to the type of victim, survivors’ depression (t = 0.738, p = 0.464) and post-traumatic stress levels (t = 1.552, p = 0.126) were both higher than those of bereaved family members; however, these differences were not statistically significant. In addition, according to gender, depression and post-traumatic stress levels were both higher in men than in women, but the difference was not significant for either depression (t = 0.738, p = 0.464) or post-traumatic stress (t = 0.213, p = 0.832). As a result of ANOVA using Dunnett’s T3 after Welch’s test to analyze the difference by age, depression levels were higher in people in their 50s than in those in their teens (F = 3.50, p = 0.019). However, there was no significant difference in post-traumatic stress (F = 1.665, p = 0.149).
3.3 Comparison of Victims’ Mental Health over Time
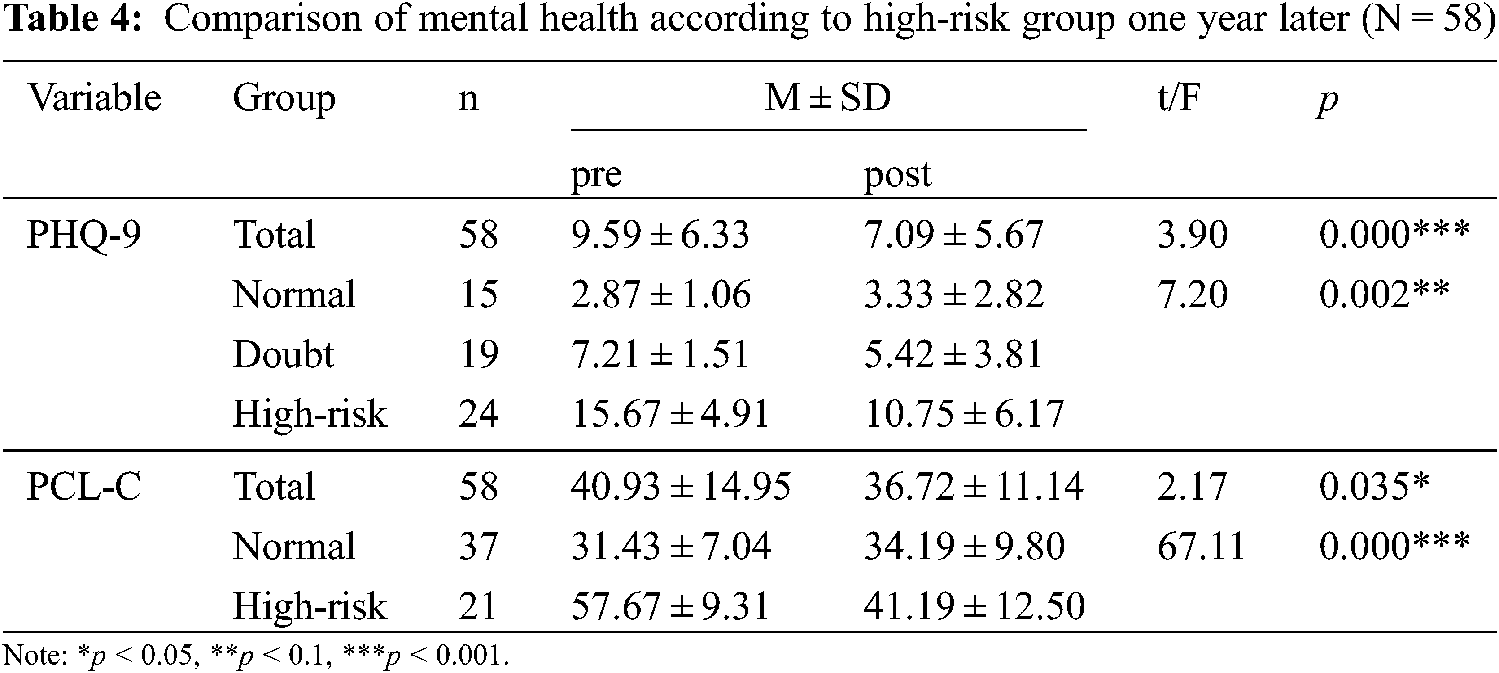
As a result of analyzing the participants’ mental health over time (Table 4), depression (t = 3.90 p = 0.000) and post-traumatic stress (t = 2.17, p = 0.035) were all confirmed to have decreased significantly. These results were confirmed using repeated measures ANOVA over time according to the risk level of the groups; there were significant decreases in depression (F = 7.20, p = 0.002, η2 = 0.207) and post-traumatic stress (F = 67.11, p = 0.000, η2 = 0.545) in the high-risk group. On the other hand, the post-traumatic stress score in the normal group increased further from 31.43 ± 7.04 to 34.19 ± 9.80.
3.4 Comparison of Victims’ Mental Health According to Program Participation
As a result of comparing the effects of program participation centered on PHQ-9 and PCL-C, the average score of PHQ-9 of the attendant group (n = 7) was from 10.86 ± 5.05 (pre) to 8.00 ± 4.5 (post), the non-attendant group (n = 51) had a mean score of 9.41 ± 6.51 (pre) and 6.96 ± 5.84 (post). Also, we confirmed the attendant group’s average score of PCL-C from 52.29 ± 19.36 (pre) to 45.29 ± 11.29 (post), in the case of the non-attendant group (n = 51), was from 39.37 ± 13.76 to 35.55 ± 10.69.
In the case of the program attendant group, it was confirmed that the average score of PCL-C was lowered more, but this was not statistically significant (F = 0.280, p = 0.599). Nevertheless, in the case of the program attendant group, the average score of PHQ-9 and PCL-C was above the cut-off score of each scale, indicating that it was a high-risk group. In other words, it can be confirmed that victims classified as high-risk groups in terms of mental health have higher participation in the program. In particular, the program participant group was significantly higher in PCL-C (t = 2.215, p = 0.031).
This study examined the mental health recovery process based on data collected for disaster psychological support for victims referred to a local mental health welfare center after a fire disaster. Based on these findings, we suggest directions for community disaster mental health services and points that warrant attention.
According to previous studies, trauma exposure and sequelae depend on gender, age, race, gender identity, education level, heredity, high-risk behavior, and the presence of surrounding support systems [29,30]. Furthermore, females have twice the risk of exposure when compared with males [19]. This also applies to bereaved family members who are not direct victims of the accident. According to previous studies, many bereaved family members are classified into high-risk groups for PTSD due to disaster and loss, and in particular, spouses have been found to suffer from more pain than other family members [31,32]. Due to the nature of the casualties associated with the Jecheon fire, many women in their 50s died. Thus, males in their 50s accounted for a greater proportion of survivors or bereaved family members of the disaster than females, and depression and PTSD levels were also significantly higher among males than among females. Although this finding does not support claims made by previous studies that women feel more pain [9], it does demonstrate that specific studies are needed according to the characteristics of the disaster.
Confirming changes over time after disasters showed that those at high risk for depression decreased from 41.4% at the beginning of the disaster to 25.9% and that post-traumatic stress significantly decreased from 36.2% to 12%. This supports the findings of previous studies that most individuals undergo a natural recovery process after a disaster and that disaster experiences do not necessarily have negative effects on mental health alone [9,15]. However, there are limitations to predicting unequivocally that natural recovery occurs over time because both psychological and physical support from the government were provided for three months in the early stages and because the local mental health welfare center was utilized after the initial stages. Various studies have suggested that psychological support in the early stages of disasters is a factor that has a positive effect on victims’ recovery in the future [4,33]. The results of this study can be presented as predictive evidence that psychological support in the early stages of a disaster is helpful for the long-term. In fact, in the case of the Daegu subway fire accident, which was a similar fire disaster, similar psychological problems such as PTSD and depressive disorder have been present from the early stages to after six years had passed; this is because psychological support was not properly implemented after the initial disaster [34].
Furthermore, in the case of PTSD, the high-risk group recovered remarkably, but the normal group worsened. The participants in the high-risk group for PTSD had a higher rate of participation in the recovery program than those in the normal group, and they sought recovery more often. Although the PTSD level was not significantly associated with program participation, members in the high-risk group attended the recovery program on high participation. Therefore, additional research is needed to determine whether the will to participate in a recovery program has a positive effect on recovery. In addition, we emphasize the suggestions of previous studies through this result. Guilaran et al. [35] confirmed that many social support systems must improve the quality of the resources provided rather than simply positively impact the recovery of disaster victims.
Ultimately, quality improvement leads to both post-traumatic growth and disaster recovery. The group program implemented after the Jecheon Fire disaster mainly consisted of various one-time programs that mainly focused on restoring daily activities; however, it did include simple psychological education and relaxation therapy for PTSD. Thus, the program might have had no direct effect on the recovery from depression and PTSD. In addition, since the effect was only analyzed for the presence or absence of attendance due to the nature of the secondary data, effects of case management and visiting counseling cannot be excluded.
According to Osorio et al. [36], the post-disaster intervention model can be classified into four groups: time, disaster type, behavior level, and victim type. The Jechon Mental Health Welfare Center program consists of various activities for promoting daily life. Therefore, depression and PTSD may be unclear indicators for evaluating the effect of the program; therefore, developing clear and detailed indicators to evaluate the results for the purpose of the program for future victims is necessary. Zulch et al. [37] asserted that preparation for mental health after a disaster should be accomplished through a broad review of various literature and should include responses at the individual level, awareness and evaluation of the disaster, and communication methods. In addition, other previous studies have suggested that creating a program based on community participation in the case of social-psychological interventions is essential. At this time, continuity, support, political and economic support are necessary. These findings emphasize the need to approach various perspectives including victims’ needs when planning a future recovery program. Therefore, we suggest that conducting a detailed follow-up evaluation through a survey on the needs of victims and their satisfaction with the implemented program is necessary.
In addition, “peritraumatic stress” is a point that should be sufficiently considered when supporting a person who has experienced a disaster; this is a known risk factor for PTSD and has been studied previously [15,38]. This finding shows that an individual’s emotional response at the time of a disaster has a vital role in depressive symptoms for five years after the disaster. Since these experiences are not well-revealed, it is important to find and support them. A lack of understanding of peritraumatic stress among mental health professionals leading to the provision of general interventions can have long-term negative effects after a disaster. Considering this, post-disaster interventions must consider stress factors in the victim’s ecological and life aspects. For victims of severe mental health problems such as PTSD and depression, treatment and programs that can reduce peritraumatic stress determined according to the characteristics of disaster are needed. For this, we propose that treatment focused on trauma should be provided along with detailed psychoeducation on post-disaster responses.
The study was conducted to provide a basis for future support by comparing and analyzing changes in the mental health of victims centered on a specific disaster called Jecheon Fire Disaster. In the study of disaster victims, it is difficult to control variables that can affect the victims as the research process can lead to ethical issues that can violate and affect the victims’ human rights. Therefore, there is a limit to data collection to analyze all the influence variables. In particular, the program implemented in this study was composed of various themes focusing on the needs and demands of the victims, and there is a limitation because it was difficult to control the variables affecting the victims in the post-disaster situation where humanitarian assistance takes precedence. However, it is meaningful to clarify that victims need community disaster mental health support through this study. Based on this study, it is necessary to develop a disaster mental health program through a more structured and verify its effect in further research.
However, in this study, we can see the disaster victims are striving for their recovery. Thus, there is a need to provide effective and appropriate support in the public community. To recover from disasters in the future, it is necessary for various studies to, specific explanations and consent procedures, and additional variable investigations. In addition, support of the administrative system is essential to track long-term effects, and each consistent indicator must be developed and applied to compare and analyze them. To continue the significance of this study and overcome the limitations, we propose to continuously and diversely study the effects on mental health according to the characteristics of each disaster in the future.
Acknowledgement: We would like to express our appreciation to mental health professionals who planned/implemented recovery programs in the Jecheon Mental Health Welfare Center and disaster victims who participated in this study.
Funding Statement: This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea Government (MEST) (No. 2020R1A2B5B01002082).
Conflicts of Interest: The authors declare that there is no conflict of interest with respect to the research, authorship, and/or publication of this article.
Reference
1. Korea National Emergency Management Agency (2020). National fire agency statistical year book (No. 11-1661000-000001-10). http://www.nfa.go.kr:8005/wv/ezpdf/customLayout.jsp?contentId=L0RBVEEvbmZhL25mYS53YXIvdXBsb2FkLy9ib2FyZC8vYmJzXzAwMDAwMDAwMDAwMDAwMTkvMjAyMDA3MDkvMjAyMDA3MDkwOTQyNDAyNjQ3My5wZGY%3D. [Google Scholar]
2. Fullerton, A., Torgersen, C., Lawler, R., Faux, E., Steel, B. et al. (2015). Rethinking the longitudinal stream temperature paradigm: Region-wide comparison of thermal infrared imagery reveals unexpected complexity of river temperatures. In: Hydrological processes, vol. 29, no. 22, pp. 4719–4737. Indianapolis: John Wiley & Sons, Ltd. [Google Scholar]
3. Goldmann, E., Galea, S. (2014). Mental health consequences of disasters. Annual Review of Public Health, 35, 169–183. DOI 10.1146/annurev-publhealth-032013-182435. [Google Scholar] [CrossRef]
4. Bonnano, G. A., Diminich, E. D. (2013). Annual research review: positive adjustment to adversity–trajectories of minimal-impact resilience and emergent resilience. Journal of Child Psychology and Psychiatry, 54(4), 378–401. DOI 10.1111/jcpp.12021. [Google Scholar] [CrossRef]
5. Abeldaño, R. A., Fernández, R. S. (2016). Community mental health mental in disaster situations. A review of community-based models of approach. Ciência & Saúde Coletiva, 21(2), 431–442. [Google Scholar]
6. Reifels, L., Bassilios, B., Spittal, M., King, K., Fletcher, J. et al. (2014). Patterns and predictors of primary mental health service use following bushfire and flood disasters. European Journal of Psychotraumatology, 5, 26527. [Google Scholar]
7. Frewen, P. A., Schmahl, C., Olff, M. (2017). Interdisciplinary approaches to understand traumatic stress as a public health problem. European Journal of Psychotraumatology, 8(5), 1441582. [Google Scholar]
8. Magruder, K. M., Kassam-Adams, N., Thoresen, S., Olff, M. (2016). Prevention and public health approaches to trauma and traumatic stress: a rationale and a call to action. European Journal of Psychotraumatology, 7, 29715. DOI 10.3402/ejpt.v7.29715. [Google Scholar] [CrossRef]
9. Norris, F. H., Friedman, M. J., Watson, P. J. (2002). 60,000 disaster victims speak: Part II. summary and implications of the disaster mental health research. Psychiatry: Interpersonal and Biological Processes, 65(3), 240–260. [Google Scholar]
10. Brewin, C. R., Andrews, B., Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. [Google Scholar]
11. Hwang, J. W. (1998). Effects of post-traumatic stress interventions for disaster victims: Meta-analysis (Doctoral Dissertation). Inje University, Gimhae, Korea. [Google Scholar]
12. North, C. S. (2010). A tale of two studies of two disasters: Comparing psychosocial responses to disaster among Oklahoma City bombing survivors and hurricane katrina evacuees. Rehabilitation Psychology, 55(3), 241–246. DOI 10.1037/a0020119. [Google Scholar] [CrossRef]
13. Rho, J. C., Lee, D. H., Kim, S. K. (2016). The status of Korea and oversea psychological support system in disaster management. The Journal of Play Therapy, 20(1), 117–133. [Google Scholar]
14. Karstoft, K. I., Armour, C., Elklit, A., Solomon, Z. (2013). Long-term trajectories of posttraumatic stress disorder in veterans: The role of social resources. The Journal of Clinical Psychiatry, 74(12), e1163–e1168. DOI 10.4088/JCP.13.m08482. [Google Scholar] [CrossRef]
15. Neria, Y., Nandi, A., Galea, S. (2008). Post-traumatic stress disorder following disasters: A systematic review. Psychological Medicine, 38(4), 467–480. DOI 10.1017/S0033291707001353. [Google Scholar] [CrossRef]
16. Schwartz, R. M., Liu, B., Sison, C. (2016). Study design and results of a population-based study on perceived stress following hurricane sandy. Disaster Medicine and Public Health Preparedness, 10(3), 325–332. DOI 10.1017/dmp.2015.157. [Google Scholar] [CrossRef]
17. Rhodes, J., Chan, C., Paxson, C. (2010). The impact of hurricane katrina on the mental and physical health of low-income parents in New Orleans. American Journal of Orthopsychiatry, 80(2), 237–247. DOI 10.1111/j.1939-0025.2010.01027.x. [Google Scholar] [CrossRef]
18. Koenen, K. C., Ratanatharathorn, A., Ng, L., McLaughlin, K. A., Bromet, E. J. et al. (2017). Posttraumatic stress disorder in the world mental health surveys. Psychological Medicine, 47(13), 2260–2274. DOI 10.1017/S0033291717000708. [Google Scholar] [CrossRef]
19. Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R. et al. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 593–602. DOI 10.1001/archpsyc.62.6.593. [Google Scholar] [CrossRef]
20. Gradus, J. L., Farkas, D. K., Svensson, E. (2015). Posttraumatic stress disorder and cancer risk: A nationwide cohort study. European Journal of Epidemiology, 30, 563–568. DOI 10.1007/s10654-015-0032-7. [Google Scholar] [CrossRef]
21. Joo, J. Y., Huh, S., Yoon, Y. A., Chae, J. H. (2016). Current trends and future tasks of cohort study for disaster victims. Journal of the Korean Neuropsychiatric Association, 55(3), 168–175. DOI 10.4306/jknpa.2016.55.3.168. [Google Scholar] [CrossRef]
22. Lee, D. H., Kim, S. K., Choi, T. S., Kim, J. H. (2015). A study on research trends on disaster mental health in korea. The Korean Journal of Rehabilitation Psychology, (22), 41–58. [Google Scholar]
23. Park, H. S., Kwon, S. Y. (2020). A study on the life experiences of family of social disaster victim: Focusing on spouse of victim of humidifier disinfectants. Korean Association of Christian Counseling & Psychology, 31(3), 175–221. DOI 10.23909/KJCC.2020.08.31.3.175. [Google Scholar] [CrossRef]
24. Spitzer, R. L., Kroenke, K., Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. patient health questionnaire. JAMA, 282(18), 1737–1744. DOI 10.1001/jama.282.18.1737. [Google Scholar] [CrossRef]
25. Park, S. J., Choi, H. R., Choi, J. H., Kim, K. W., Hong, J. P. (2010). Reliability and validity of the Korean version of the patient health questionnaire-9 (PHQ-9). Anxiety and Mood, 6(2), 119–124. [Google Scholar]
26. Oh, S. I., Won, S. D., Lee, S. H., Yoo, S. Y., Kim, H. C. et al. (2014). Reliability and validity of the Korean version of the PTSD checklist civilian version in north Korean defectors. Journal of Korean Neuropsychiatry Association, 53(6), 410–417. DOI 10.4306/jknpa.2014.53.6.410. [Google Scholar] [CrossRef]
27. Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., Forneris, C. A. (1996). Psychometric properties of the PTSD checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. DOI 10.1016/0005-7967(96)00033-2. [Google Scholar] [CrossRef]
28. Conybeare, D., Behar, E., Solomon, A., Newman, M. G., Borkovec, T. D. (2012). The PTSD checklist-civilian version: Reliability, validity, and factor structure in a nonclinical sample. Journal of Clinical Psychology, 68(6), 699–713. DOI 10.1002/jclp.21845. [Google Scholar] [CrossRef]
29. Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J. et al. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(5), 135–383. DOI 10.1080/20008198.2017.1353383. [Google Scholar] [CrossRef]
30. Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A. et al. (2016). The epidemiology of traumatic event exposure worldwide: Results from the world mental health survey consortium. Psychological Medicine, 46(2), 327–343. DOI 10.1017/S0033291715001981. [Google Scholar] [CrossRef]
31. Park, K. M. (2015). A technical approach to post-traumatic stress disorder of the sewol ferry victims’ parents. The Journal of the Korea Contents Association, 15(9), 134–145. DOI 10.5392/JKCA.2015.15.09.134. [Google Scholar] [CrossRef]
32. Hong, J. K., Kim, C. K., Lee, S. Y., Choi, W. Y. (2005). The study on the posttraumatic stress disorder of the families of the victims in daegu subway disaster. Journal of Emotional & Behavioral Disorders, 21(3), 139–154. [Google Scholar]
33. Bisson, J. I., Berliner, L., Cloitre, M., Forbes, D., Jensen, T. K. et al. (2019). The international society for traumatic stress studies new guidelines for the prevention and treatment of posttraumatic stress disorder: methodology and development process. Journal of Traumatic Stress, 32(4), 475–483 DOI 10.1002/jts.22421. [Google Scholar] [CrossRef]
34. Kwon, H. R., Park, S. H. (2019). Psychological factors as predictors of posttraumatic stress and depressive symptoms among survivors of the Gyeongbuk area earthquake. Korean Journal of Clinical Psychology, 38(2), 128–144. DOI 10.15842/kjcp.2019.38.2.001. [Google Scholar] [CrossRef]
35. Guilaran, J., de Terte, I., Kaniasty, K., Stephens, C. (2018). Psychological outcomes in disaster responders: A systematic review and meta-analysis on the effect of social support. International Journal of Disaster Risk Science, 9(3), 344–358. DOI 10.1007/s13753-018-0184-7. [Google Scholar] [CrossRef]
36. Osorio Yepes, C., Díaz Facio Lince, V. (2012). Models of psychological intervention in disaster situations by natural phenomenon. Revista de Psicoloía Universidad de Antioquia, 4(2), 65–84. [Google Scholar]
37. Zulch, H. R., Reser, J. P., Creed, P. (2012). Psychological preparedness for natural disasters. Proceedings of the First International Conference on Urban Sustainability and ResilienceUCL, London. [Google Scholar]
38. Galea, S., Nandi, A., Vlahov, V. (2005). The epidemiology of post-traumatic stress disorder after disasters. Epidemiologic Reviews, 27, 78–91. DOI 10.1093/epirev/mxi003. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |