
Mental Health Promotion
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/IJMHP.2021.015699
ARTICLE
Stressors and Coping Strategies of Medical Staff in the COVID-19 Pandemic in Wuhan
1College of Health Science and Nursing, Wuhan Polytechnic University, Wuhan, 430026, China
2Wuhan Red Cross Hospital, Wuhan, 430021, China
3Optics Valley Hospital, District of Wuhan Third Hospital, Wuhan, 430070, China
4Hubei Provincial Hospital of Traditional Chinese Medicine, Wuhan, 430068, China
5Wuhan Hospital of Integrated Traditional Chinese and Western Medicine, Wuhan, 430001, China
6The Central Hospital of Wuhan, Wuhan, 430004, China
7Nursing Department of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, China
*Corresponding Authors: Yanlin Shi. Email: shiyanli222@126.com; Qiaoyuan Yan. Email: yanqiaoyuan@163.com
Received: 07 January 2021; Accepted: 11 April 2021
Abstract: Exploring whether medical staff perceive stress on the assigned medical tasks, what are the specific sources of stress, what are the tangible sources of support they expected to be helpful, and individual coping with stress to provide more accurate, personal support for psychological crisis. This study uses a cross-sectional descriptive survey adopting convenience sampling among the medical staff who worked for over seven days in the infected areas of one Grade 2A and three Grade 3A hospitals during the COVID-19 pandemic. The assessment includes attitude when receiving tasks, major stressors, factors relieving stress, and personal management of stress. A total of 104 (76.8%) valid questionnaires are received. A majority (94.3%) of the medical staff held a positive attitude taking duty for granted but feeling nervous and afraid (81.1%). Contacting the infected (90.6%) and compensation (92.5%) are the main concerns. The major pressure sources are regarding safety for oneself (98.1%), colleagues (92.5%), and family (94.3%), as well as lack of effective treatment (92.5%), inadequate protective equipment (94.3%) and incomplete disinfection (94.3%). The main positive pressure adjustments include strict infection controlling measures (98.4%), maintaining a positive attitude (95.2%), actively attain more information 95.2%, and engage in recreational activities (93.6%), but more than 40% takes negative adjustments to vent their emotions and relieve anxiety, suggesting the importance of early psychological intervention. During the COVID-19 pandemic, the main stressors among medical staff are safety, uncertainty and shortage of resources. Positive coping includes taking effective protective measures and achieving thorough understanding of the virus.
Keywords: COVID-19; pandemics; psychological stress; medical staff
On February 11, 2019 at the global forum for research and innovation in Geneva, the general director of the World Health Organization (WHO), Dr. Tandesay, announced the official designation of diseases caused by the novel coronavirus (2019-nCoV) as the 2019 Coronavirus disease (COVID-19) [1]. Until 6 January 2021, data released by WHO showed globally over 83 million reported cases and over 1.8 million deaths [2]. Thus, the situation remains severe.
COVID-19 has higher homogeneity in clinical research compared with the SARS that broke out in Guangzhou, China in 2003. Both viruses combine S-Protein of CoV with human airway mucosa angiotensin to convert Enzyme II (ACE2), which then enters the epithelial cells [3]. However, with its 10–20 times higher adhesion, SARS-CoV-2 is more contagious than SARS-CoV [3,4]. Since January 2020, when the battle with the new coronavirus infected with pneumonia began, China has sent more than 32,000 medical staff to support Wuhan, wherein 11,000 critical medical staff accounted for nearly 10% of the entire country’s resources [5,6]. Throughout China, 3,387 medical staff from 476 medical institutes cared for infected COVID-19 patients (2055 confirmed cases, 1,070 clinically diagnosed cases, and 157 suspected cases) [7]. Over 90% of the medical staff (3,062) were from Hubei province [7], and 26 died at work due to COVID-19 infection or overloaded work [8].
When facing severe public crisis, the first-line medical workers are not only at high risk from the epidemic but also from psychological stress problems [9]. Firstly, ethical questions raises when it comes to the duties and concern for their own safety [10]. Questions can be asked such as “Do health care professionals have obligations to provide care to infected patients especially in lack of personal protective equipment” [11]. Secondly, being overworked, several medical staff began to show extreme fatigue, uncontrollable anxiety, nervousness, irritability, memory decline, and other illnesses, accompanied by dizziness, headache, insomnia, breathing difficulties, nausea, muscle tension, shaking, and other somatic symptoms [12,13]. To better understand these negative emotional and mental outcomes, additional information regarding stressors is required. During previous outbreak of SARS, several factors contributing to stress have been identified, including perception of risk, impact on work life, working in high-risk units and performing infection-related tasks [14–16]. Also, numerous coping strategies have been developed to reduce psychological stress. Hastings et al. revealed four reliable coping dimensions, such as active avoidance coping and positive coping [17].
Despite that there is evidence of COVID-19 related stress and coping strategies have been developed, the whole picture of whether they perceive stress on the assigned medical tasks, what are the specific sources of stress, tangible sources of support they expected to be helpful, and individual coping methods with stress, is missing for medical staff especially in a high-risk infected setting. On this basis, this study aims to explore the perceived stress, stressors, factors reducing stress and coping strategies of medical staff during the COVID-19 outbreak to provide support and suggestions for addressing the consequential psychological crisis not only in the current situation but also in the future.
Ethical statements
The ethics committee of Tongji Medical College of Huazhong University of Science and Technology approved the conduct of this study.
The subjects of this study were all medical staff who worked for over seven days in the infected areas of one Grade 2A and three Grade 3A hospitals during the COVID-19 outbreak. All the target population had constant exposure to COVID-19 patients.
The conditions of the hospitals are as follows:
Three Grade 3A hospitals: 1) Houhu district of Wuhan Central Hospital has 510 open beds, 525 available beds, and 40 emergency rooms. During the outbreak, the hospital admitted and confirmed 564 COVID-19 patients, including 142 hospital staff. A total of 14 patients, including three medical staff, developed respiratory failure that required intubation and mechanical ventilation. Eight patients died from COVID-19, two of whom were medical staff; 2) Hubei Hospital of Traditional Chinese Medicine has 430 open beds and 321 available beds, including 16 beds in emergency rooms and 10 beds in critical care units. The hospital admitted and confirmed 321 patients, including 32 hospital staff. Among the patients, 15, including three hospital medical staff, developed respiratory failure that required intubation and mechanical ventilation. A total of 26 patients died from COVID-19, two of whom were medical staff; 3) Optics Valley Area of Wuhan Third Hospital has 300 open beds and 600 available beds, including 10 beds in critical care units. The hospital admitted and confirmed 695 patients, including 24 medical staff.
Grade 2A hospital: Wuhan Red Cross Hospital has 342 open beds and 576 available beds, including 18 beds in critical care units. The hospital admitted and confirmed 611 patients, including 53 medical staff. Eight patients developed respiratory failure that required intubation and mechanical ventilation, and two patients were equipped with extracorporeal membrane oxygenation (ECMO). One doctor from the hospital died from COVID-19.
The research tool is an electronic questionnaire derived and modified from the COVID-19 medical staff stressors questionnaire used by Lee et al. [18], which has also been used by Hummel et al. [19], Cai et al. [20] for hospital staff during the SARS epidemic in 2003. In the present study, the questionnaire survey is forwarded to respondents through the QR code of WeChat (SO JUMP ID: 62545539). The starting and ending times are from 9:00 on February 21, 2020 to 24:00 on February 24, 2020. Convenience sampling is adopted for anonymous, voluntary, and self-filled questionnaire survey.
The questionnaire consists of four parts and 62 items. First, the assessment contents included immediate response to a task with 12 items to mainly investigate the attitude of medical staff when they received medical tasks for COVID-19, which indirectly reflects perceived psychological stress. Second, stressors during the medical procedure were assessed on the 20 conditions that may trigger stress in medical staff. Third, 16 items that help relieve stress were used to understand the external factors affecting the personal stress relief of medical staff. Fourth, coping strategies adopted were determined through 14 items to examine the internal solutions by which medical staff cope with stress. Questions were answered with either “yes” or “no”, and those answered with “yes” are scored with the four-level standard (0 = completely not; 1 = slight; 2 = medium; 3 = awfully) to illustrate the level.
The data were organized, coded, and input using SPSS 20.0 software for statistical processing. The data were described as mean (standard deviation) for continuous variables or frequency for categorical variables. The internal consistency of the questionnaire was evaluated by correlational analysis. A Cronbach’s α > 0.70 is considered acceptable.
This study collected 104 valid questionnaires from qualified medical staff (76.8%). Incomplete or questionnaires that were not filled according to the requirements were excluded. The overall Cronbach’s α of the questionnaire reached 0.93, and the Cronbach’s α of all dimensions ranges 0.76–0.92. Cumulative variance contribution rate reached 58.19%, indicating good reliability.
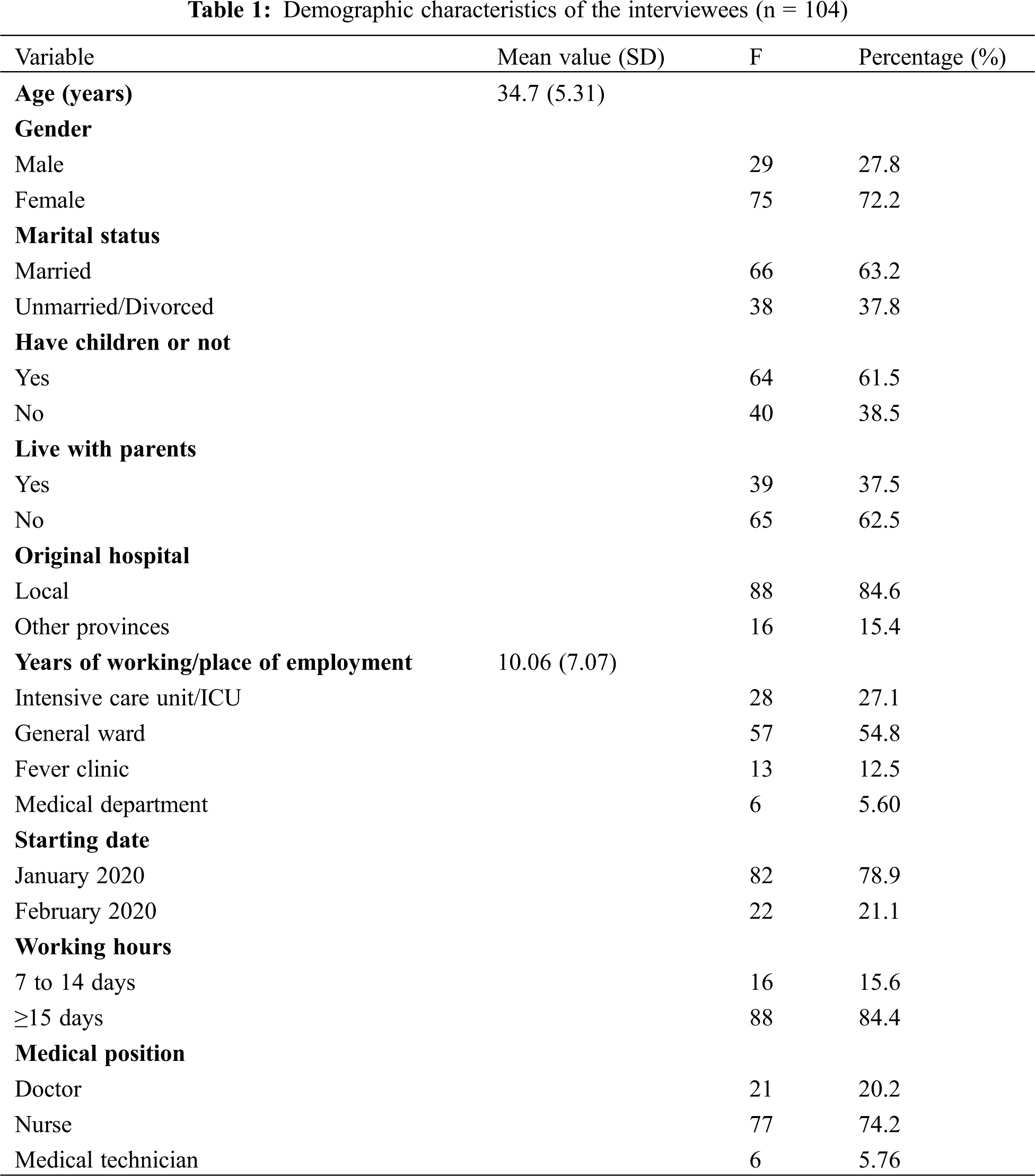
Tab. 1 shows the demographic profile of the included medical staff. The majority of respondents were local medical staff (84.6%), with nurses accounting for the majority (74.2%). The age of the interviewees ranged from 23–41 years old and the average was 34.7 years old (SD = 5.31). Professional working experiences ranged from 1–21 years (average = 10.06, SD = 7.07). More than half (58.4%) worked in the general infection ward, followed by those in ICU (27.1%); all joined in the rescue work since the most severe period of the COVID-19 (January–February 2020). Most of the respondents were married (63.2%) and had children (61.5%), while several lived with parents (37.5%).
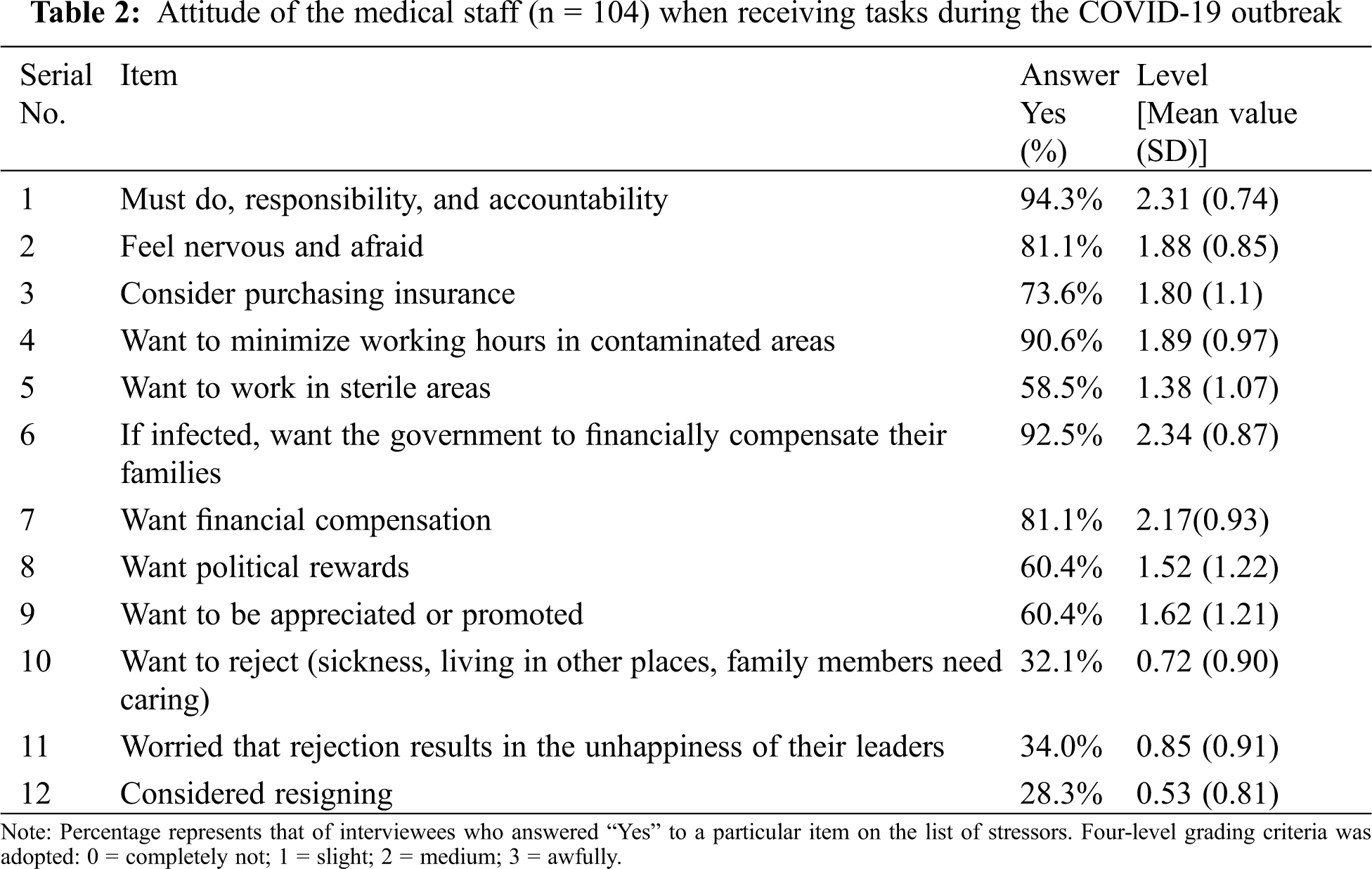
Over 94% of the medical staff held a positive attitude feeling that their medical tasks must be done due to “responsibility and accountability” (Tab. 2). Nevertheless, most of them felt nervous and afraid (81.1%). Many (73.6%) began to consider purchasing insurance given their own safety. In addition, they preferred to minimize their contact hours with the patients (90.6%) and stay in safe sterile areas of the hospital (58.5%). Once they get infected, they wanted to have their family members received financial compensate from the government (92.5%). On top of safety considerations, 81.1% thought of personal financial compensation, and more than half of the respondents expressed their demands for political rewards (60.4%) or promotion of their post (60.4%) in this questionnaire. However, some reported negative feeling of the medical tasks assigned, with 32.1% declared rejection due to sickness, living in distant regions and caring for family members. Also, they were worried about the adverse outcomes of rejection, which could annoy their leaders (34.0%). Moreover, several medical staff presented extreme negative attitude considering of resigning (28.3%).
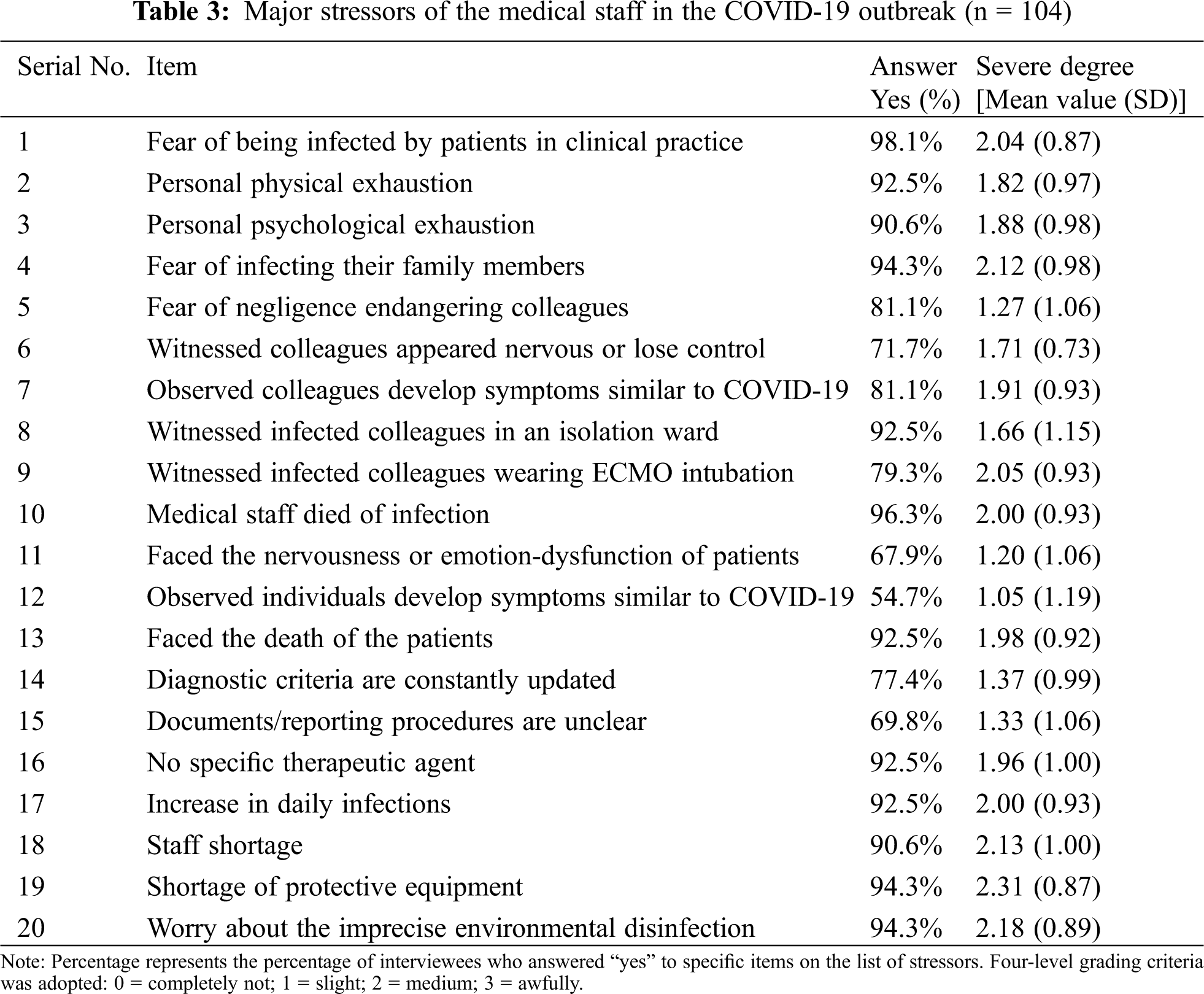
Tab. 3 shows that the major pressure felt by most of the interviewees are regarding safety for themselves (98.1%), colleagues (92.5%), and their family members (94.3%). In addition, 92.5% and 90.6%, respectively, perceived physical exhaustion and psychological exhaustion. Moreover, witnessing death (96.3%) or rescuing for other medical staff (79.3%) also caused significant psychological burden. On the other hand, we presented results of stress from external environment which refers to lack of clear information and resources in the management of COVID-19. To be specific, frequent update of the diagnostic criteria (77.4%), undefined documenting process (69.8%), lack of effective treatment (92.5%), and uncertainty resulting from the rising death tolls (92.5%) further posed great pressure. Regarding resources, 90.6% declared staff shortage, 94.3% complained of inadequate protective equipment, 94.3% claimed incomplete disinfection of environment, all causing greater than medium severity of stress.
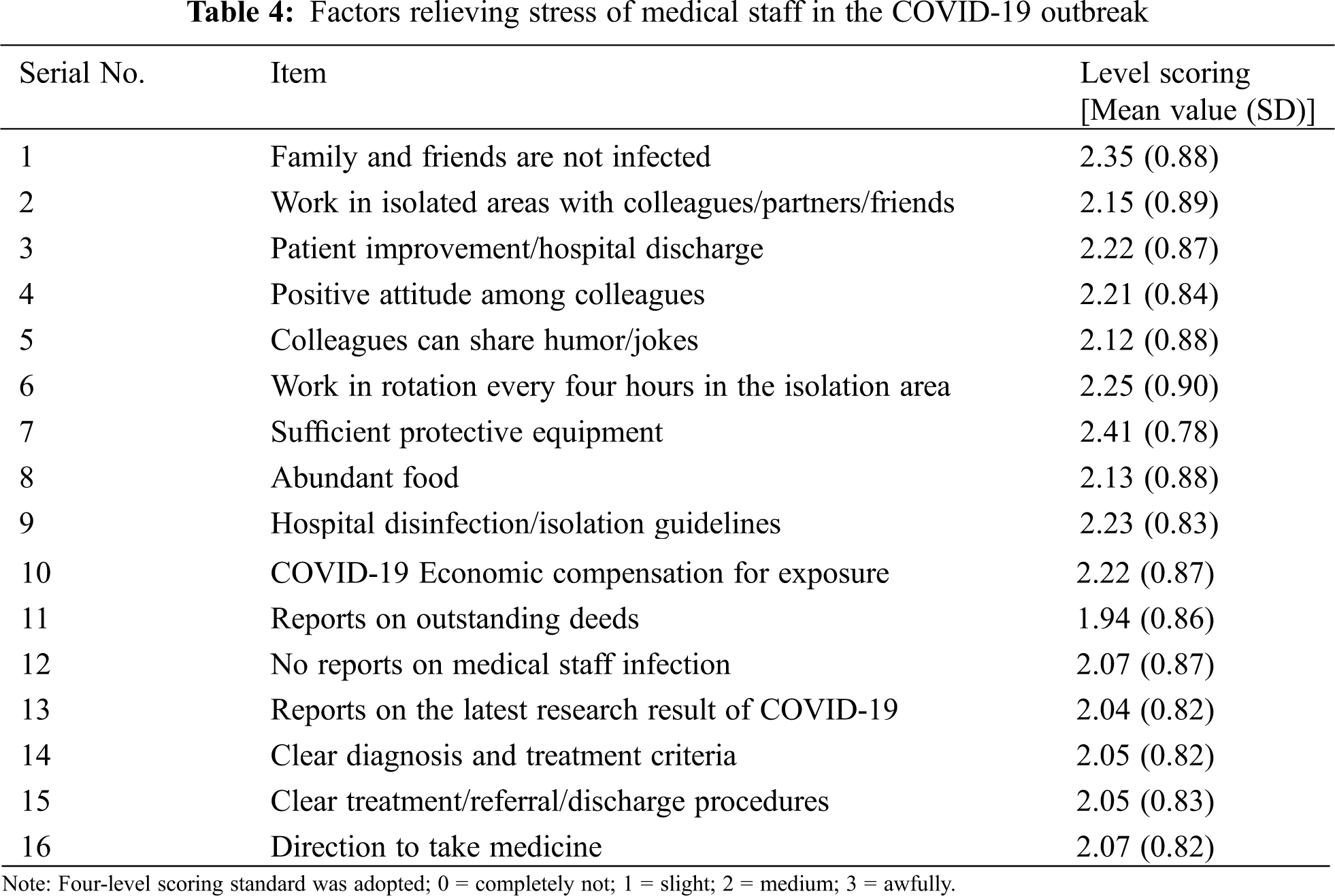
In response to the attitude and stressors abovementioned, effective interventions and supply of resources from hospitals and the society have been provided to front-line caregivers during COVID-19 outbreak. Not surprisingly, when safety issues of family members, friends and individuals have been delt with, psychological burden is reduced (Tab. 4). Positive attitude is reported to relieve stress as well. In terms of the external environment, improvement of working conditions, such as working in rotation, sufficient personal protective equipment, abundant food, and hospital disinfection, can decrease anxiety and pressure of safety-related issues. Economic compensation and honor somehow shift one’s emotion and attitude. Additionally, the up-to-date information and instructions help release stress.
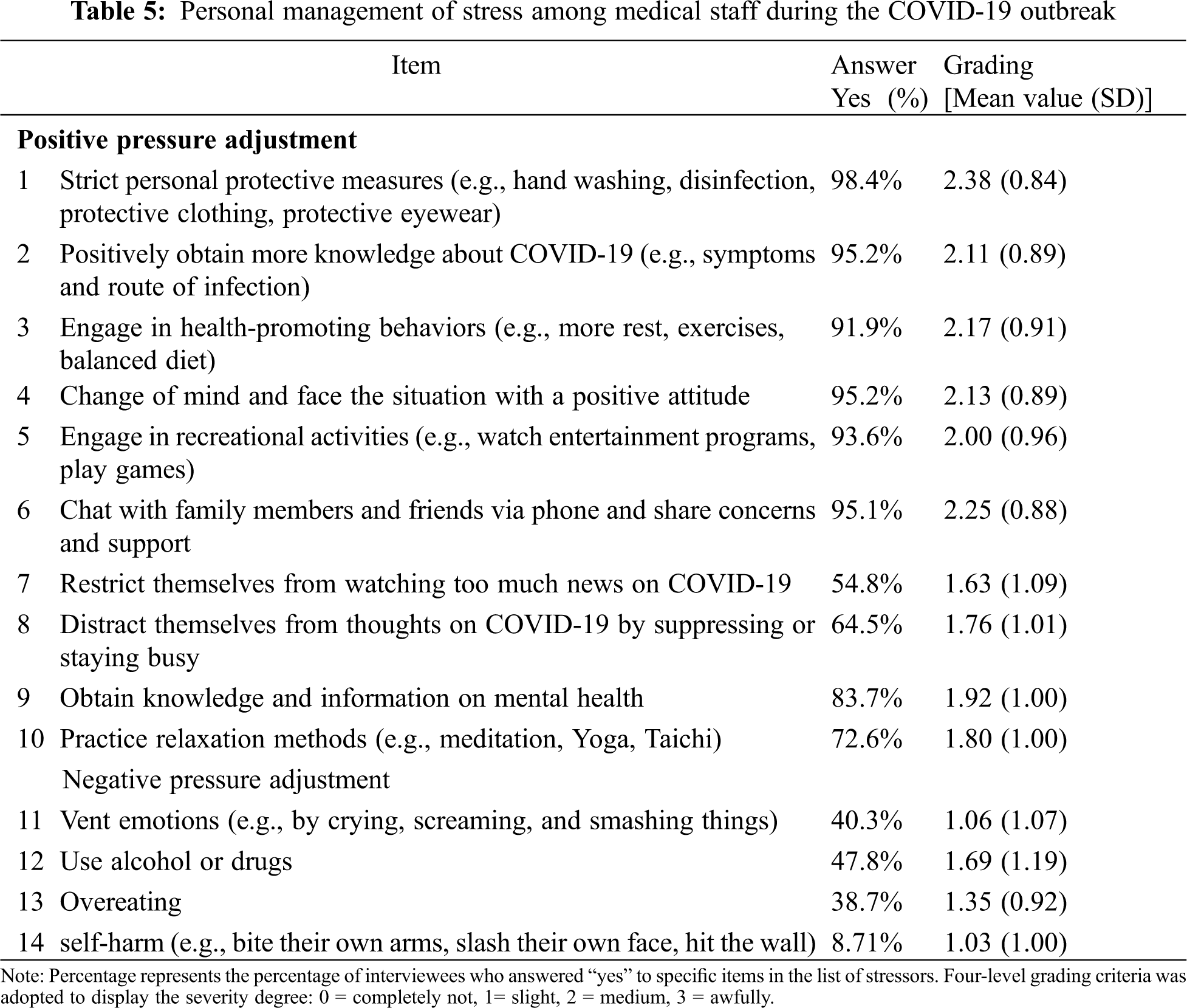
Tab. 5 reveals variable coping strategies that respondents seek and implement to relieve stress. The coping was categorized into two opposite directions, namely, positive and negative perspective. The main positive pressure adjustment includes strict infection controlling measures (98.4%), for instance, handwashing, protective gear. On top of that, maintaining a positive attitude whatever the situation is (95.2%) is quite beneficial. To be specific, 95.2% of the respondents actively attain more information, 91.9% engaged health-promoting activities, 93.6% involved themselves in recreation. In addition, communicating with family members and friends is frequently observed to reduce stress. However, 40% of the medical staff relieved their pressure by “crying, screaming, and smashing things”. Alcohol or drug (e.g., sleeping pills) is an alternative choice (47.8%) and healthcare providers did so mainly to help with sleeping disorders. Interestingly, 38.7% chose to gourmandize instead to release negative feelings. Those who confessed self-harm occupied a minority (8.71%) but such actions occurred occasionally.
Previous studies have demonstrated that healthcare workers reported more severe psychological symptoms and even mental illness [9]. Even though all medical staffs are exposed to the risk of infection more or less, the degree of such risk is not evenly distributed and varies in different working environments [21]. The respondents in our study represent relatively good generalization, from ICUs to general wards, including doctors, nurses, laboratory technicians, and imaging inspectors, most of whom have families and children and come from local areas. Similar to other studies, females, nurses, younger healthcare workers are more likely to experience emotional burnout [9].
The results revealed that upon receiving mission, the vast majority of medical staff had a feeling of anxiety, nervousness, and uneasiness which have been characterized in other outbreaks as well [22] despite that the difference was intensity of exposure [23]. They also consider various ways to avoid risks and expect extra compensation under the pressure of getting infected. The proposal of special considerations of job promotion and political rewards may be due to age characteristics as well as excessive and competitive pressure of their jobs. In that the average working life of the medical staff is 10.06 years, with a minimum of only one year in this survey. Insurance and compensation were identified as predictors of psychological morbidity [15]. Financial concerns, for example, worrying about loss of current job or lack of resources, were found one of the most stressful factors in the first national US survey [24]. Nevertheless, when facing the dilemma of avoidance or acceptance, most of the medical staff feel less stressed because they recognize work ethic and professional responsibility as priority.
The largest perceived stressor from the respondents in our survey is safety, whether their own or of colleagues, family members, or the public. The medical staff had to endure significant psychological pressure especially in witnessing the end-of-life treatment for colleagues or patients suffering from the disease [25]. In addition, the uncertainty of COVID-19 makes them feel considerably helpless in their roles and responsibilities. Our results were consistent with previous listening sessions which identified 8 sources of anxiety, such as personal protective equipment, exposed to virus at work and infecting their family [26]. Surprisingly, in a survey investigating mental health among medical professional in European countries, highest rated stressors included uncertainty, frequent modification of infection control procedures, while respondents were least concerned about themselves or colleagues [19]. The contradiction was possibly due to different culture and value or varied severity of the pandemic. Other highly endorsed sources of stress included insufficient infection prevention and control, and shortage of protective equipment and medical staff brought by the lockdown of the entire city to constrain the spread of the pandemic. In line with prior research among nurses, inadequate personal protective equipment and ventilators, and shortage related to hospital staff both contributed to high-level stress [27–30].
Factors that could alleviate pressure were in accordance with the collected major stressors. First of all, once the safety of family members and friends were ensured, for instance, working in isolated areas with colleagues/partners/friends, the psychological burden would be released significantly. The safety of family members was observed the biggest impact on reducing stress and positive attitude among colleagues was also an essential factor that reduces distress of medical staff during the outbreak [27]. Secondly, plentiful resources like sufficient protective equipment [31] and abundant food [27] entail the alleviation of the distress. Thirdly, updated reliable information about the COVID-19 (i.e., having received the clear instructions [32], accurate dissemination of health-related knowledge to the public [33]) is able to solve the uncertainty-caused stress [30]. Numerous clinical treatment regimens are accumulated in the process, namely, guided antiviral medication, symptomatic and supportive treatment for multi-organ loss, effective program of TCM treatments, and plasma treatment methods [34], boosting the confidence of medical staff to treat COVID-19.
The most commonly used coping strategy based on this survey were taking protective measures, changing one’s thoughts and facing the situation with a positive attitude, actively acquiring more knowledge about COVID-19, video chatting with family and friends by phone to share concerns and support, and engaging in recreational activities. Similar results were found in another cross-sectional study [35]. A review suggested encouraging physicians to participate in relaxation techniques like yoga, meditation and also to seek psychological therapists for help to vent their frustrations [36]. Other coping strategies have also been evaluated, for instance, problem-focused coping and emotion-focused coping [37]. Burns et al. believed that dealing with problems and seeking solutions are the most effective ways to relieve pressure, which can not only ensure the strength of work but also improve the quality of work [38]. However, other coping methods could produce heterogeneous results among the subscales, and the items concerning specific coping behaviors in our study generate more practical answers in a pandemic. On the other hand, negative stress adjustment, sometimes can be reckoned as emotion-focused coping style, also plays an important role in times of crisis. More than 40% of medical staff who underwent negative adjustment during the outbreak used drugs and alcohol to help them sleep, vented their emotions by crying, screaming, smashing things, and overeating. Self-harm was even used to ease their nervousness and anxiety. Lewis also believed that the greater the pressure, the greater the response, and the more often that the negative adjustment method is used [39]. On the contrary, it was reported that emotion-focused strategies sometimes backfire, associated with higher anxiety [40]. When investigating the relationship with depression and anxiety, negative coping was found positive associated whereas positive coping was involved in negative association [41].
This study facilitates in the understanding that personal safety assurance and optimistic environment are the keys to the continued work of medical staff. Interventions related to safety and master of knowledge are considered as effective stress-relief measures Special compensation and recognition are major incentives. Moreover, psychological intervention and counseling are indispensable auxiliary coping strategies.
It is acknowledged that there are several limitations in our study. The sample size is relatively small and survey was conducted in Wuhan, the results of which may not be characterized as nationally or globally. However, the results do provide insight into the perceived stress level and coping methods for medical staff. Furthermore, the sampling method administered in this survey is convenience sampling, which could generate selection bias. To illustrate, those who really carry serious stress might not respond to the questionnaire which was collected online, resulting in underestimation of the severity of stress among medical staff. Additionally, given the study design, the relationship between stressors, coping strategies and psychological stress cannot be determined in the present.
In 2020, the COVID-19 outbreak in Wuhan, China caused emotional distress among the first-line medical staff. The major stressors include the safety of individuals, colleagues, and their family members, the availability of protective equipment and personnel, clear medical guidelines, and special compensation and recognition. To overcome or alleviate stress, healthcare providers can take effective protective measures, acquire thorough up-to-date knowledge of the virus, engage themselves in relaxation activities and have more communication with friends or family members. Studies evaluating long-term effect of these aforementioned stressors and coping strategies in the psychological burden induced by COVID-19 are warranted in the future.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. WHO Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020 (2020). https://www.who.int/director-general/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020. [Google Scholar]
2. Weekly epidemiological update (2020). https://www.who.int/publications/m/item/weekly-epidemiological-update---5-january-2021. [Google Scholar]
3. Sohrabi, C., Alsafi, Z., O’Neill, N., Khan, M., Kerwan, A. et al. (2020). World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). International Journal of Surgery, 76, 71–76. DOI 10.1016/j.ijsu.2020.02.034. [Google Scholar] [CrossRef]
4. Yang, Y., Peng, F., Wang, R., Yange, M., Guan, K. et al. (2020). The deadly coronaviruses: The 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. Journal of Autoimmun, 109, 102434. DOI 10.1016/j.jaut.2020.102434. [Google Scholar] [CrossRef]
5. Lin, Q., Zhao, S., Gao, D., Lou, Y., Yang, S. et al. (2020). A conceptual model for the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China with individual reaction and governmental action. International Journal of Infectious Diseases, 93, 211–216. DOI 10.1016/j.ijid.2020.02.058. [Google Scholar] [CrossRef]
6. Li, Z., Ge, J., Yang, M., Feng, J., Qiao, M. et al. (2020). Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behavior and Immunity, 88, 916–919. DOI 10.1016/j.bbi.2020.03.007. [Google Scholar] [CrossRef]
7. A press conference of the state council on the joint prevention and control mechanism of pneumonia caused by novel coronavirus (2020). http://www.nhc.gov.cn/xcs/fkdt/202002/5329d7ab7af24690a1d5b66982333af3.shtml. [Google Scholar]
8. China-WHO COVID-19 joint inspection report (2020). http://www.nhc.gov.cn/xcs/yqfkdt/202002/87fd92510d094e4b9bad597608f5cc2c.shtml. [Google Scholar]
9. Vizheh, M., Qorbani, M., Arzaghi, S. M., Muhidin, S., Javanmard, Z. (2020). The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. Journal of Diabetes & Metabolic Disorders, 19(2), 1967–1978. DOI 10.1007/s40200-020-00643-9. [Google Scholar] [CrossRef]
10. McDougall, R. J., Gillam, L., Ko, D., Holmes, I., Delany, C. (2020). Balancing health worker well-being and duty to care: An ethical approach to staff safety in COVID-19 and beyond. Journal of Medical Ethics, 47(5318–323. DOI 10.1136/medethics-2020-106557. [Google Scholar] [CrossRef]
11. Schuklenk, U. (2020). What healthcare professionals owe us: Why their duty to treat during a pandemic is contingent on personal protective equipment (PPE). Journal of Medical Ethics, 46(7), 432. DOI 10.1136/medethics-2020-106278. [Google Scholar] [CrossRef]
12. Cao, J., Wei, J., Zhu, H., Duan, Y., Geng, W. et al. (2020). A study of basic needs and psychological Wellbeing of medical workers in the fever clinic of a Tertiary General Hospital in Beijing during the COVID-19 outbreak. Psychotherapy and Psychosomatics, 89(4), 252–254. DOI 10.1159/000507453. [Google Scholar] [CrossRef]
13. Liang, Y., Chen, M., Zheng, X., Liu, J. (2020). Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. Journal of Psychosom Research, 133, 110102. DOI 10.1016/j.jpsychores.2020.110102. [Google Scholar] [CrossRef]
14. Styra, R., Hawryluck, L., Robinson, S., Kasapinovic, S., Fones, C. et al. (2008). Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. Journal of Psychosom Research, 64(2), 177–183. DOI 10.1016/j.jpsychores.2007.07.015. [Google Scholar] [CrossRef]
15. Tam, C. W., Pang, E. P., Lam, L. C., Chiu, H. F. (2004). Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychological Medicine, 34(7), 1197–1204. DOI 10.1017/s0033291704002247. [Google Scholar] [CrossRef]
16. Lee, S. M., Kang, W. S., Cho, A. R., Kim, T., Park, J. K. (2018). Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comprehensive Psychiatry, 87, 123–127. DOI 10.1016/j.comppsych.2018.10.003. [Google Scholar] [CrossRef]
17. Hastings, R. P., Kovshoff, H., Brown, T., Ward, N. J., Espinosa, F. D. et al. (2005). Coping strategies in mothers and fathers of preschool and school-age children with autism. Autism, 9(4), 377–391. DOI 10.1177/1362361305056078. [Google Scholar] [CrossRef]
18. Lee, S. H., Juang, Y. Y., Su, Y. J., Lee, H. L., Lin, Y. H. et al. (2005). Facing SARS: Psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. General Hospital Psychiatry, 27(5), 352–358. DOI 10.1016/j.genhosppsych.2005.04.007. [Google Scholar] [CrossRef]
19. Hummel, S., Oetjen, N., Du, J., Posenato, E., Losada, R. et al. (2021). Mental health among medical professionals during the COVID-19 pandemic in Eight European Countries: Cross-sectional survey study. Journal of Medical Internet Research, 23(1), e24983. DOI 10.2196/24983. [Google Scholar] [CrossRef]
20. Cai, Z., Zheng, S., Huang, Y., Zhang, X., Qiu, Z. et al. (2020). Emotional and cognitive responses and behavioral coping of Chinese medical workers and general population during the Pandemic of COVID-19. International Journal of Environmental Research and Public Health, 17(17), 6198. DOI 10.3390/ijerph17176198. [Google Scholar] [CrossRef]
21. Simonds, A. K., Sokol, D. K. (2009). Lives on the line? Ethics and practicalities of duty of care in pandemics and disasters. European Respiratory Journal, 34(2), 303. DOI 10.1183/09031936.00041609. [Google Scholar] [CrossRef]
22. Lin, C. Y., Peng, Y. C., Wu, Y. H., Chang, J., Chan, C. H. et al. (2007). The psychological effect of severe acute respiratory syndrome on emergency department staff. Emergency Medicine Journal, 24(1), 12–17. DOI 10.1136/emj.2006.035089. [Google Scholar] [CrossRef]
23. Khalid, I., Khalid, T. J., Qabajah, M. R., Barnard, A. G., Qushmaq, I. A. (2016). Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clinical Medicine Research, 14(1), 7–14. DOI 10.3121/cmr.2016.1303. [Google Scholar] [CrossRef]
24. Park, C. L., Russell, B. S., Fendrich, M., Finkelstein-Fox, L., Hutchison, M. et al. (2020). Americans’ COVID-19 Stress, Coping, and Adherence to CDC Guidelines. Journal of General Internal Medicine, 35(8), 2296–2303. DOI 10.1007/s11606-020-05898-9. [Google Scholar] [CrossRef]
25. Lorente, L., Vera, M., Peiró, T. (2021). Nurses’ stressors and psychological distress during the COVID-19 pandemic: The mediating role of coping and resilience. Journal of Advanced Nursing, 77(3), 1335–1344. DOI 10.1111/jan.14695. [Google Scholar] [CrossRef]
26. Shanafelt, T., Ripp, J., Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA, 323(21), 2133–2134. DOI 10.1001/jama.2020.5893. [Google Scholar] [CrossRef]
27. Cai, H., Tu, B., Ma, J., Chen, L., Fu, L. et al. (2020). Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the Outbreak of Coronavirus Disease 2019 (COVID‐19) in Hubei. China Medical Science Monitor, 26, e924171. DOI 10.12659/msm.924171. [Google Scholar] [CrossRef]
28. Babore, A., Lombardi, L., Viceconti, M. L., Pignataro, S., Marino, V. et al. (2020). Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Research, 293, 113366. DOI 10.1016/j.psychres.2020.113366. [Google Scholar] [CrossRef]
29. Labrague, L. J., De Los Santos, J. A. A. (2020). COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. Journal of Nursing Management, 28(7), 1653–1661. DOI 10.1111/jonm.13121. [Google Scholar] [CrossRef]
30. Ali, H., Cole, A., Ahmed, A., Hamasha, S., Panos, G. (2020). Major stressors and coping strategies of frontline nursing staff during the outbreak of Coronavirus Disease 2020 (COVID-19) in Alabama. Journal of Multidisciplinary Healthcare, 13, 2057–2068. DOI 10.2147/jmdh.s285933. [Google Scholar] [CrossRef]
31. Shalhub, S., Mouawad, N. J., Malgor, R. D., Johnson, A. P., Wohlauer, M. V. et al. (2021). Global vascular surgeons’ experience, stressors, and coping during the coronavirus disease 2019 pandemic. Journal of Vascular Surgery, 73(3), 762–771. DOI 10.1016/j.jvs.2020.08.030. [Google Scholar] [CrossRef]
32. Vagni, M., Maiorano, T., Giostra, V., Pajardi, D. (2020). Coping with COVID-19: Emergency stress, secondary trauma and self-efficacy in healthcare and emergency workers in Italy. Frontiers in Psychology, 11, 2294. DOI 10.3389/fpsyg.2020.566912. [Google Scholar] [CrossRef]
33. Ho, C. S., Chee, C. Y., Ho, R. C. (2020). Mental health strategies to combat the psychological impact of COVID-19 beyond Paranoia and Panic. Annals of the Academy of Medicine Singapore, 49(3), 155–160. [Google Scholar]
34. Diagnosis and treatment plan for pneumonitis infected by new coronavirus (trial version 6) (2020). http://www.nhc.gov.cn/yzygj/s7652m/202002/54e1ad5c2aac45c19eb541799bf637e9.shtml. [Google Scholar]
35. Du, J., Mayer, G., Hummel, S., Oetjen, N., Gronewold, N. et al. (2020). Mental health burden in different professions during the final stage of the COVID-19 lockdown in China: Cross-sectional survey study. Journal of Medical Internet Research, 22(12), e24240. DOI 10.2196/24240. [Google Scholar] [CrossRef]
36. Patel, R. S., Bachu, R., Adikey, A., Malik, M., Shah, M. (2018). Factors related to physician burnout and its consequences: A review. Behavioral Sciences, 8(11), 98. [Google Scholar]
37. Jie, Y. (1998). Reliablility and validity of the Chinese version of coping style scale. Chinses Journal of Clinical Psychology, 2, 114–115. [Google Scholar]
38. Burns, C., Harm, N. J. (1993). Emergency nurses’ perceptions of critical incidents and stress debriefing. Journal of Emergency Nursing, 19(5), 431–436. [Google Scholar]
39. Lewis, D. J., Robinson, J. A. (1992). ICU nurses’ coping measures: Response to work-related stressors. Critical Care Nurse, 12(2), 18–23. [Google Scholar]
40. Snyder, C. M., Fauth, E., Wanzek, J., Piercy, K. W., Norton, M. C. et al. (2015). Dementia caregivers’ coping strategies and their relationship to health and well-being: The Cache County Study. Aging & Mental Health, 19(5), 390–399. DOI 10.1080/13607863.2014.939610. [Google Scholar] [CrossRef]
41. Mark, G., Smith, A. P. (2012). Occupational stress, job characteristics, coping, and the mental health of nurses. British Journal of Health Psychology, 17(3), 505–521. DOI 10.1111/j.2044-8287.2011.02051.x. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |