
Mental Health Promotion
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/IJMHP.2021.016337
ARTICLE
Development of Mental Health Literacy Scale for Depression Affecting the Help-Seeking Process in Health Professional Students
1School of Rehabilitation Sciences, Health Sciences University of Hokkaido, Hokkaido, 061-0293, Japan
2School of Nursing and Social Services, Health Sciences University of Hokkaido, Hokkaido, 061-0293, Japan
3School of Health Sciences, Sapporo Medical University, Hokkaido, 060-8556, Japan
*Corresponding Author: Soshi Kodama. Email: kodamas@hoku-iryo-u.ac.jp
Received: 01 March 2021; Accepted: 26 May 2021
Abstract: Despite depression being a global mental health disorder, many people with depression do not seek psychiatric help. In particular, it has been reported that only 15.7% of medical students seek treatment. A longer duration of untreated illness (DUI) leads to clinically poor results. To shorten the DUI, the mental health literacy (MHL) with regard to depression needs to be improved, although it is unclear which MHL components will improve the help-seeking process. Additionally, the existing MHL scale for depression is poorly validated for structural validity. Therefore, the purpose of this study was to develop an MHL scale for depression with verified reliability and validity (particularly structural validity) and verify its relationship with the help-seeking process. For this purpose, we adapted the mixed research method. First, we conducted a systematic literature review on MHL scales for depression to prepare a draft scale with content validity. Second, we conducted semi-structured interviews on MHL with outpatients with depression. Consequently, 78 questions on MHL for depression were extracted. Third, to develop our scale, we verified the reliability and validity of these questions with 782 health professional students. The sample size was 780 and data collection was performed by collective survey method. It was conducted in 2018 in Japan. To verify the factor structure, exploratory and confirmatory factor analyses were conducted. We also examined the internal consistency, test-retest reliability, and criterion-related validity. The exploratory factor analysis revealed a three-factor structure (recognition of depression symptoms, help-seeking preferences, and depression onset possibility) with 10 items. According to the confirmatory factor analysis results, the goodness of fit indicators had a good fit. The internal consistency, test-retest reliability, and criterion-related validity had good values. Fourth, the relationship between the MHL of depression and other factors affecting the help-seeking process was examined using structural equation modelling. The same sample size (as above) was applied. All three components of the MHL of depression influenced ‘recognition of depression’. In particular, depression onset possibility had the greatest impact on the help-seeking process. Whereas, the MHL of depression had little or no influence on ‘intention of consultation’ and ‘psychiatric consultation’ (second and third steps of help-seeking). The largest influence on psychiatric consultation was the recommendation of consultation from others. The multiple correlation coefficients were the recognition of depression, R2 = 0.33; intention of consultation, R2 = 0.43; and psychiatric consultation, R2 = 0.36; and the model was a good fit. This study identified the specific components of the depression MHL that influence the help-seeking process. Subsequently, it is necessary to provide specific MHL education to health professional students, their families, university staff, and teachers.
Keywords: Depression; health literacy; psychometrics; secondary prevention
Depression is a common mental health disorder worldwide and is a well-known principal risk factor for suicide. For example, over 20,000 suicides are reported annually in Japan [1]. Moreover, suicide in Japan is the leading cause of death among the 15–39-year age group [2]. Thus, in 2013, the Ministry of Health, Labour and Welfare designated mental health disorders as one of the five major diseases in Japan [3]. This emphasised the importance of prevention, early detection, and treatment of mental health disorders.
The duration of untreated illness (DUI) is defined as the interval between the onset of a patient’s first psychiatric episode and the moment they seek appropriate treatment [4]. A previous systematic review and meta-analysis of the relationship between DUI and its effect on clinical outcomes in depression found that a shorter DUI was associated with a positive response to treatment and remission [5]. Furthermore, a longer DUI predicts the persistence of depressive symptoms [5]. Therefore, people with depression need to shorten the DUI to prevent severe depression. Nevertheless, in Japan, only 29.6% of people with mood disorders book a mental health consultation in the same year of onset [6]. Additionally, health professional students, including medical students, experience psychological distress (e.g., depression, anxiety, and burnout) with high frequency. A review of the prevalence of depression among medical students demonstrated that 27.2% (range: 9.3%–55.9%) of students screened positive for depression [7]; however, only 15.7% of these reportedly sought treatment [7].
Promoting help-seeking behaviour to shorten DUI is necessary to improve mental health literacy (MHL). Originally, MHL was defined as the ‘knowledge and beliefs about mental disorders, which aid their recognition, management, or prevention’ [8]. MHL includes six components: a) recognition of mental health disorders, b) knowledge and beliefs about the causes, c) knowledge and beliefs about self-help, d) knowledge and beliefs about professional help, e) attitude that facilitates recognition and seeking help (stigma), and f) knowledge of how to seek mental health information. More recently, the definition of MHL has extended the previous definition to include four components: 1) understanding how to obtain and maintain positive mental health, 2) understanding mental health disorders and their treatments, 3) decreasing the stigma related to mental health disorders, and 4) enhancing help-seeking efficacy (knowing when and where to seek help, and the competencies designed to improve mental health care and self-management capabilities) [9]. This new definition of the MHL considers the current definitions of health literacy (HL). HL has the following components: the competencies needed by people to help obtain and maintain health and identify illness; understanding how and where to access and how to evaluate health information and health care; understanding how to properly apply prescribed treatments; and obtaining and applying skills related to social capital, such as understanding rights related to health and health care and understanding how to advocate for health improvements [10]. Thus, the new MHL definition highlights the competencies required to promote mental health as well as knowledge and beliefs.
As previously mentioned, mental health disorders were seen as major diseases in Japan, and consequently, Japanese prefectural and city governments were required to formulate medical care plans to detect and treat them as early as possible [3]. However, none of these medical plans specifies the MHL components that are useful for promoting help-seeking. Furthermore, help-seeking efficacy is a key component of the MHL [11], and it is necessary to investigate the components of the MHL that promote help-seeking, as this will be beneficial in the future when conducting MHL education for health professional students.
To investigate the relationship between specific MHL components and help-seeking process, a depression MHL scale with a clear factor structure is required. A systematic review of the existing MHL scale’s reliability and validity [12] was conducted that extracted 16 MHL scales, with four of them being specific to depression (Depression Multiple Choice Question, MCQ [13]; Depression Literacy D-Lit [14]; Knowledge about Depression and Mania Inventory, KDMI [15]; and Adolescent Depression Knowledge Questionnaire, ADKQ [16]). Two of these depression MHL scales were developed for people with depression [13,15], and the other two were developed for the healthy population [14,16]. However, none of the scales measure depression MHL among health professional students. Moreover, one of the two studies did not verify the structural validity [14], and the other reported that it had a one-factor structure as a result of verifying structural validity [16]. It is imperative to identify which the specific components of the MHL of depression affect the help-seeking process. Creating a new depression MHL scale with a clear factor structure is essential.
Thus, this study aims to (1) develop an MHL scale for depression and verify its reliability and validity among health professional students, and (2) identify specific MHL of depression affecting the help-seeking process among health professional students using the newly developed MHL scale for depression.
We adopted a mixed research method in which a qualitative study was conducted to extract valid MHL components that facilitated help-seeking process, and then those MHL components were verified by a quantitative study. In particular, this research consisted of four studies. First, two studies were conducted to ensure the content validity of the MHL scale for depression. Study 1 was a systematic literature review for an MHL scale for depression. In Study 2, interviews were conducted with outpatients with depression regarding how MHL affects the help-seeking process. The other purpose of Study 2 was to generate hypotheses about the other factors that influence the help-seeking process other than MHL. We then prepared a draft scale based on the results of Studies 1 and 2, and Study 3 verified the reliability and validity of the MHL scale for depression. In addition, the draft scale included the content of treatment guidelines issued by the Japanese society of mood disorders to ensure content validity (available only in Japanese). Finally, in Study 4, we examined the relationship between specific components of the MHL of depression and help-seeking process using structural equation modelling (SEM).
2.1 Study 1: Systematic Literature Review for a Mental Health Literacy (MHL) Scale for Depression
The inclusion criteria for papers were as follows: 1) published after 1997; 2) MHL regarding depression was investigated, and the specific question items were clear; 3) written in English; 4) targeted the general population; 5) the participants’ ages were between 18 to 65; and 6) the papers were included in the references that met the above inclusion criteria.
We searched the PubMed, PsycINFO, and Cochrane Library databases, using the keywords [literacy] or [knowledge], [depression] or [mental health], and [help seeking]. We first removed duplicate papers from our results. Next, we reviewed titles and abstracts, and papers that met the inclusion criteria were included (first screening). Additionally, we reviewed the papers’ full text, and those with unknown questions about MHL for depression were excluded (second screening). Finally, because similar scales and questions were sometimes used among the papers, only the papers published first were included. Finally, we added papers that did not have details for question items in the text but had them in the references (third screening). This search was carried out in November 2015.
2.2 Study 2: Interviews about MHL for Depression and the Help-Seeking Process
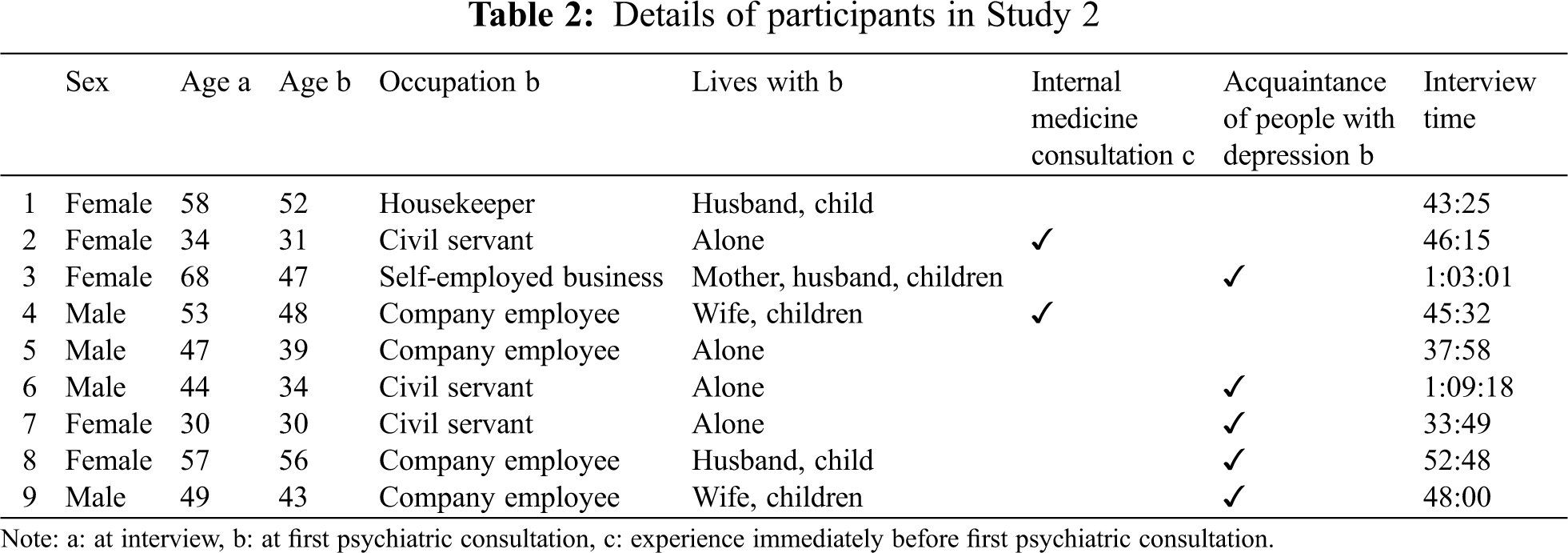
As a result of the theoretical sampling and theoretical saturation, the participants were nine outpatients (4 male, 5 female) with depression who had received a psychiatric consultation due to depressive symptoms, lived in the community, and remembered why they went to the psychiatric consultation. The mean age was 48.8 ± 11.2 years, and the mean age at first consultation was 42.2 ± 8.7 years. All participants were office workers or homemakers. Semi-structured interviews were conducted where first we asked, ‘Would you explain the process of how you consulted a psychiatrist?’ If they did not mention MHL, then we asked the following questions, in accordance with MHL’s six components: 1) ‘How did you recognise your depressive symptoms?’; 2) ‘What knowledge did you have about the causes of depression?’; 3) ‘How do you manage your depression?’; 4) ‘What knowledge do you have about professional help?’; 5) ‘What is your opinion on consulting a psychiatrist?’; and 6) ‘How did you get information about mental health?’ The interviews were recorded verbatim, and the data were analysed using a grounded theory approach [17]. MaxQDA10 software was used for analysis, and Study 2 was conducted from April to July 2017.
2.3 Study 3: Development of an MHL Scale for Depression
The inclusion criteria for the participants were undergraduate health professional students that did not take psychiatric lectures, because it was important to ensure that there was no difference in the degree of MHL of depression. The exclusion criteria were those who had deficiencies in the questionnaire responses.
In the case of statistical analysis by SEM, it is ideal that the sample size is 10 times more than that of the observed variables [18]. The first draft of the MHL scale for depression which is based on the results of Studies 1 and 2 had 78 items. Therefore, the sample size was 780 in Study 3.
We posted a flyer recruiting research participants on the campus of the university and announced the recruitment of research participants in lectures. The data collection was performed by collective survey method, which was collected by having them gather in the lecture room. Considering that the number of participants excluded would be about 25%, sampling was performed so as to satisfy the sample size. The participants were 1,070 undergraduate health professional students, recruited from several departments of one university in Japan (dentistry, pharmacy, nursing, social welfare, physical therapy, occupational therapy, and speech-language-hearing therapy departments). Of the 1,070 respondents, only those who completed all the questions were included. Subsequently, data from 782 participants (238 male and 544 female) were included for the statistical analysis (valid response rate: 73.7%), and the participants mean age was 19.3 ± 1.9 years.
The participants completed a questionnaire, which included the following: 1) first draft of the MHL scale for depression, 2) demographic variables (age, sex), 3) help-seeking process questions, and 4) the Health Locus of Control Scale (HLOC) (available only in Japanese).
The help-seeking process has three steps [19]. To assess the first step, recognition of depression, we asked the question, ‘Do you currently have any depressive symptoms that you are aware of?’ To assess the second step, intention to consultation, we asked the question ‘Do you currently intend to seek help from a psychiatrist due to depressive symptoms?’ Responses to both questions were rated using five-point Likert scales, ranging from ‘Disagree’ (1) to ‘Agree’ (5). To assess the third step, psychiatric consultation, we asked the question; ‘Do you currently receive psychiatric services due to depressive symptoms?’ This was scored using a dichotomous scale: ‘No’ (0) or ‘Yes’ (1).
A study of the relationship between health knowledge and behaviour and HLOC scores indicated that internal control had significantly higher health knowledge than external control [20]. The HLOC scale consists of seven items for internal control (Item I) and seven items for external control (Item E). Both Items I and E have a 1-to 4-point rating scale. The scores range from 14 to 56, and higher total HLOC scores indicate stronger internal control tendencies. Both reliability and validity have been verified, and Study 3 was conducted from April to May 2018.
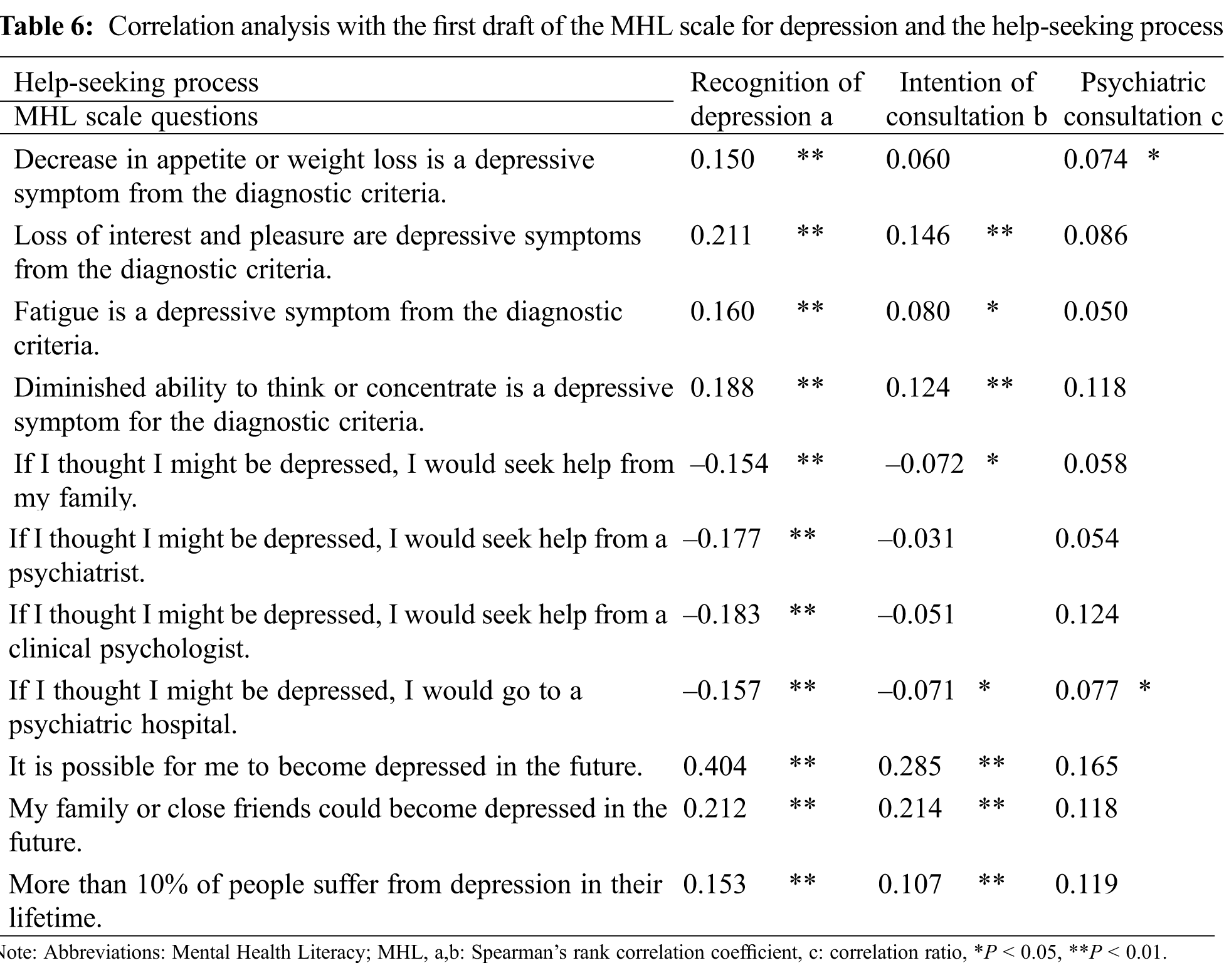
An item analysis was conducted to prepare for the exploratory factor analysis (EFA). We aimed to develop an MHL scale for depression affecting the help-seeking process; hence, we conducted a correlation analysis between scores for the MHL scale and help-seeking process questions. Only the MHL scale items that significantly correlated with help-seeking process scores were included for the EFA.
In the EFA, a principal factor analysis with varimax rotation was used to identify the loading patterns within the MHL scale for depression. The analysis identified the number of factors based on eigenvalues greater than 1. Items with factor loadings ≥0.40 were retained, and two or more questions per factor were used as criteria.
A confirmatory factor analysis (CFA) was performed to evaluate the degree of model fit to the factor structure obtained by the EFA. The Goodness of Fit Index (GFI), Adjusted GFI (AGFI), Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA), and Akaike’s Information Criterion (AIC) were adopted as the goodness of fit indicators. GFI, AGFI, and CFI values closer to 1.00 are desired and values greater than 0.90 are considered a good fit. RMSEA of 0.06 or less is considered good [21].
2.3.4 Criterion-Related Validity
Correlation coefficients were calculated using the HLOC scale as an indicator of criterion-related validity.
Cronbach’s α coefficients were calculated for internal consistency. If the value of Cronbach α is between 0.70 to 0.95, it is judged to be good internal consistency [22]. The test-retest reliability was determined two weeks after the initial measurement by administering the first draft scale again to obtain intraclass correlation coefficients (ICC) [23].
2.3.6 Statistical Analysis Software
The CFA was performed with Amos version 22, and the other statistical analyses were performed with SPSS version 21. The significance level of all statistics was less than 0.05.
2.4 Study 4: Examination of the Components of the MHL of Depression that Affect the Help-Seeking Process
We examined the relationship between the MHL of depression and the help-seeking process using the scale developed in Study 3. The participants were the same as in Study 3.
The participants were asked to complete the following five questionnaires, in addition to the questions from Study 3. Similar to previous research [24–26], the (1) Big Five personality scale (Japanese version), and the (2) Severity of depression symptoms (Center for Epidemiologic Studies-Depression scale; CES-D) were included. Furthermore, based on the results of Study 2, we also set as question items (3) Being pointed out by others as having depression, (4) Being pointed out by others that they need to have a psychiatric consultation, and (5) Receiving information about depression from others. Study 4 was conducted from April to May 2018.
To measure personality traits, the Japanese version of the Big Five personality scale was used. This scale is a dichotomous scale with 70 items, and its reliability and validity have been verified. The five factors are extraversion, neuroticism, agreeableness, conscientiousness, and intellect. Total scores were calculated for each factor. It has been reported that the extroversion trait is associated with a higher intention to seek help than the introverted trait [24]. Furthermore, individuals with depression who receive help score higher for neuroticism than those who suffer from depression but do not recognise the need for care [25].
The CES-D is a 20-item scale developed by the National Institute of Mental Health to screen for depression in the general population [27]. The participants rate each item according to the past week, on a 4-point scale: 0 ‘almost never (less than 1 day)’, 1 ‘sometimes or occasionally (1 or 2 days a week)’, 2 ‘frequently (3 or 4 days a week)’, and 3 ‘most of the time (5 days or more a week)’. The total score ranges from 0 to 60 points. A score of 16 or higher indicates that the individual has depression [27]. The Japanese version of the CES-D scale was used in this study. Previous research has demonstrated that the more severe the depression, the more likely it is that help-seeking intentions and help-seeking behaviours occur [25,26].
The results of Study 2 suggest that social support has the effect of facilitating the help-seeking process. Therefore, we investigated whether the participants’ families or acquaintances identified that they had depression or had advised them to see a doctor. For the statistical analysis, 0 was assigned if participants’ depression had not been identified by others, and 1 if it had been identified. Similarly, 0 was assigned if participants had been advised by others to have a psychiatric consultation, and 1 if they had not received such advice. Moreover, we also investigated whether they had heard about depression from their families and acquaintances. The answers were scored using five-point Likert scales from ‘No’ (1) to ‘Yes’ (5).
The objective variables in Study 4 were the three steps of the help-seeking process explored in Study 3 (recognition of depression, the intention of consultation, and psychiatric consultation). The explanatory variables were age, sex, MHL of depression, personality traits, depression severity, and social support. First, there is a possibility that help-seeking behaviour may differ depending on the individual’s gender [28], and therefore, we examined this. Then, the Spearman’s rank correlation coefficient, correlation ratio, and φ coefficient were used for the correlation analysis between the objective variables and the explanatory variables depending on each scale’s level of measurement. Finally, SEM was performed. The variables with a correlation coefficient of 0.2 or more were included in the path diagram. There are two types of evaluation of SEM: overall evaluation and partial evaluation. First, as a partial evaluation, the standardised partial regression coefficient between the explanatory variables are used as judgment indexes, and non-significant paths are deleted. After that, the goodness-of-fit of the model is judged as an overall evaluation. GFI, AGFI, CFI, RMSEA, and AIC indicators are used as criteria for judgment. If the goodness-of-fit index did not meet the criteria, the validity was further examined using partial evaluation, and non-significant paths were deleted to create a new model. This process was repeated until the goodness-of-fit index of the model became an appropriate value.
SEM was performed with Amos version 22, and the other statistical analyses were performed with SPSS version 21. The significance level of all statistics was less than 0.05.
Studies 2, 3, and 4 (involved human subjects) were approved by the Ethics Committee of Sapporo Medical University (27-2-30). All the participants gave informed consent. In Study 2, the participant’s name was ciphered, and the data were analysed by a dedicated computer. In Studies 3 and 4, the survey was completed anonymously.
3.1 Study 1: Systematic Literature Review for an MHL Scale for Depression
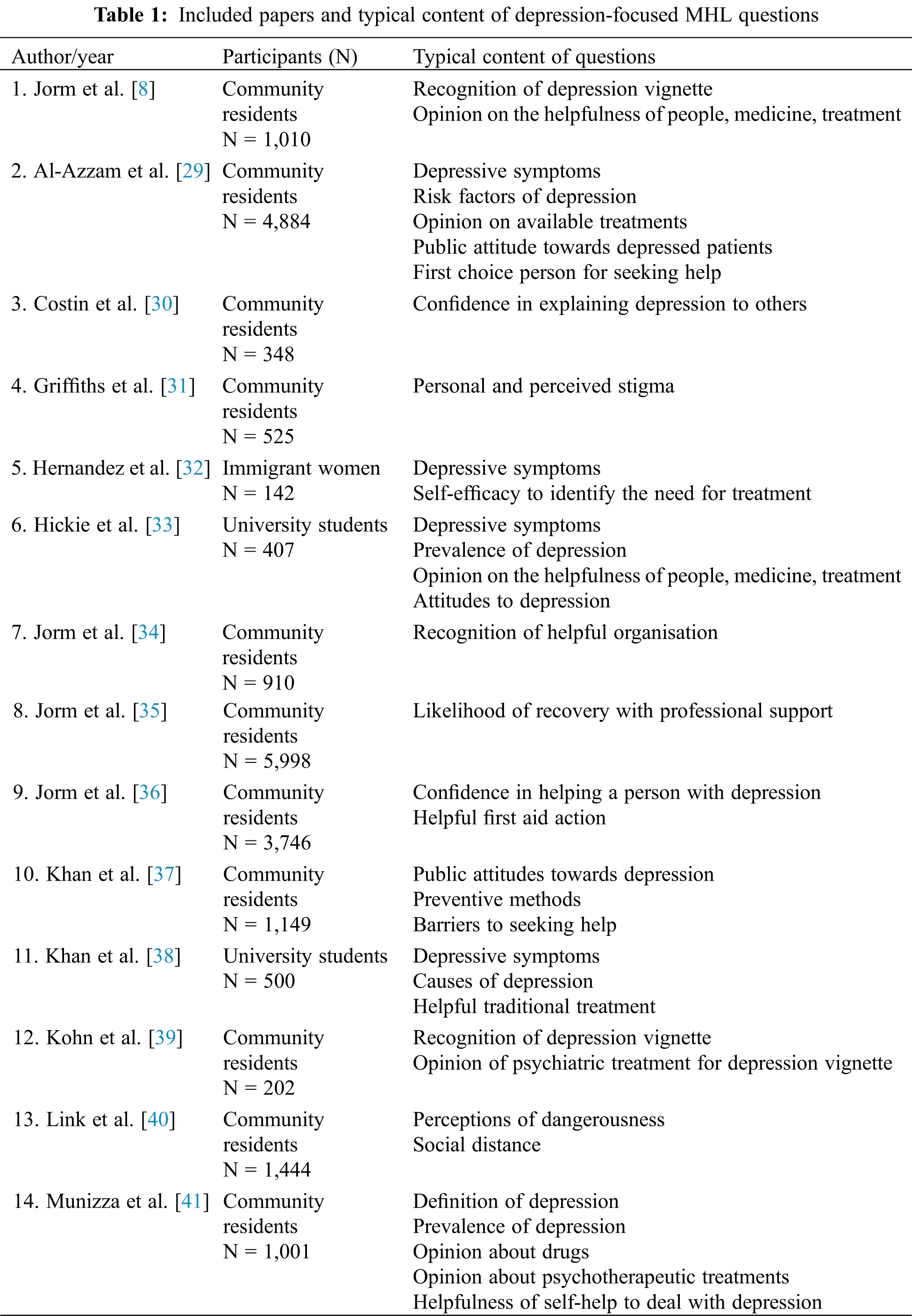
Fig. 1 illustrates the flow chart of the search results. The 14 papers that satisfied the inclusion criteria [8,29–41] and their typical questions are summarised in Tab. 1.
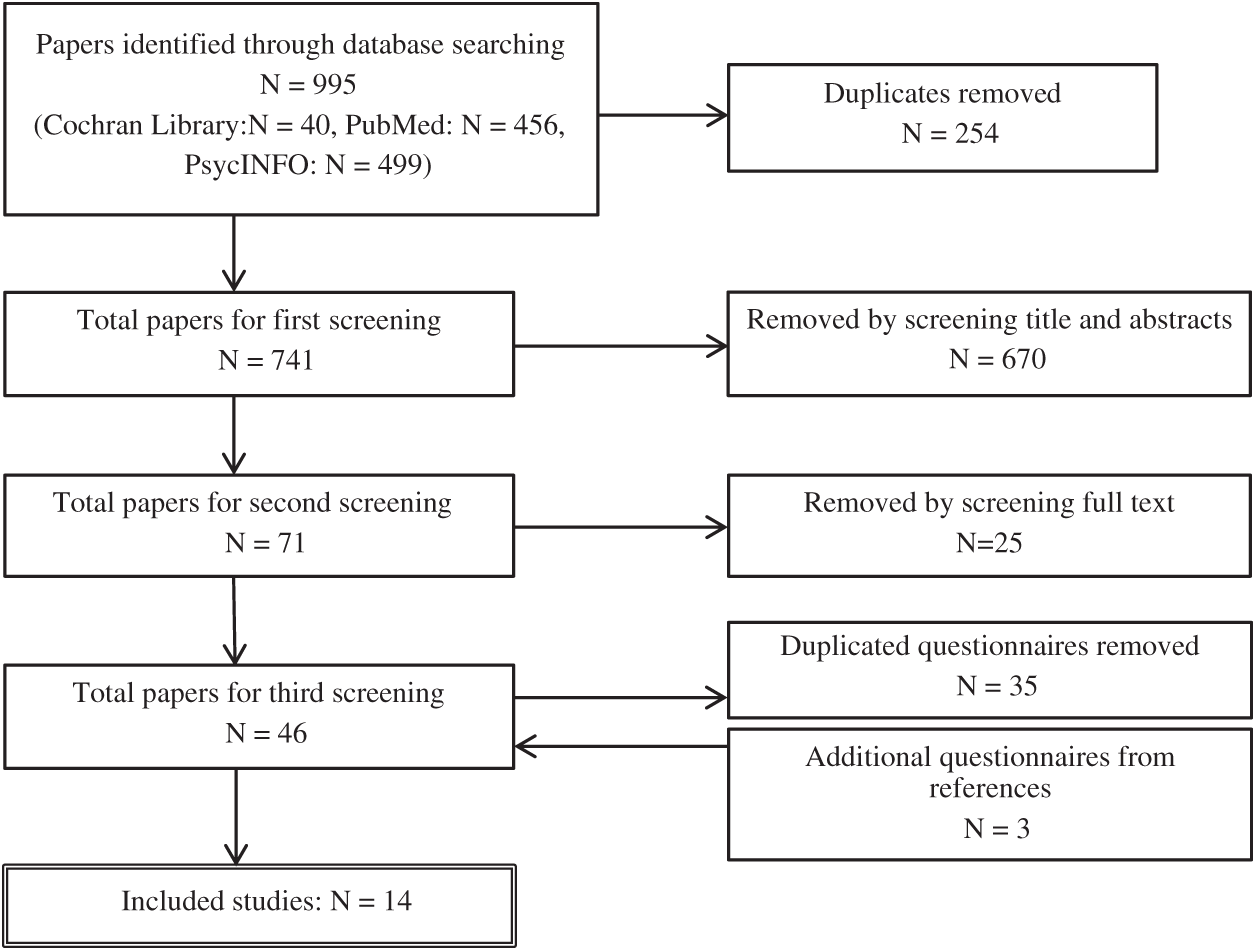
Figure 1: Flow chart of the systematic literature review on mental health literacy (MHL) of depression
3.2 Study 2: Interviews about the MHL for Depression and the Help-Seeking Process
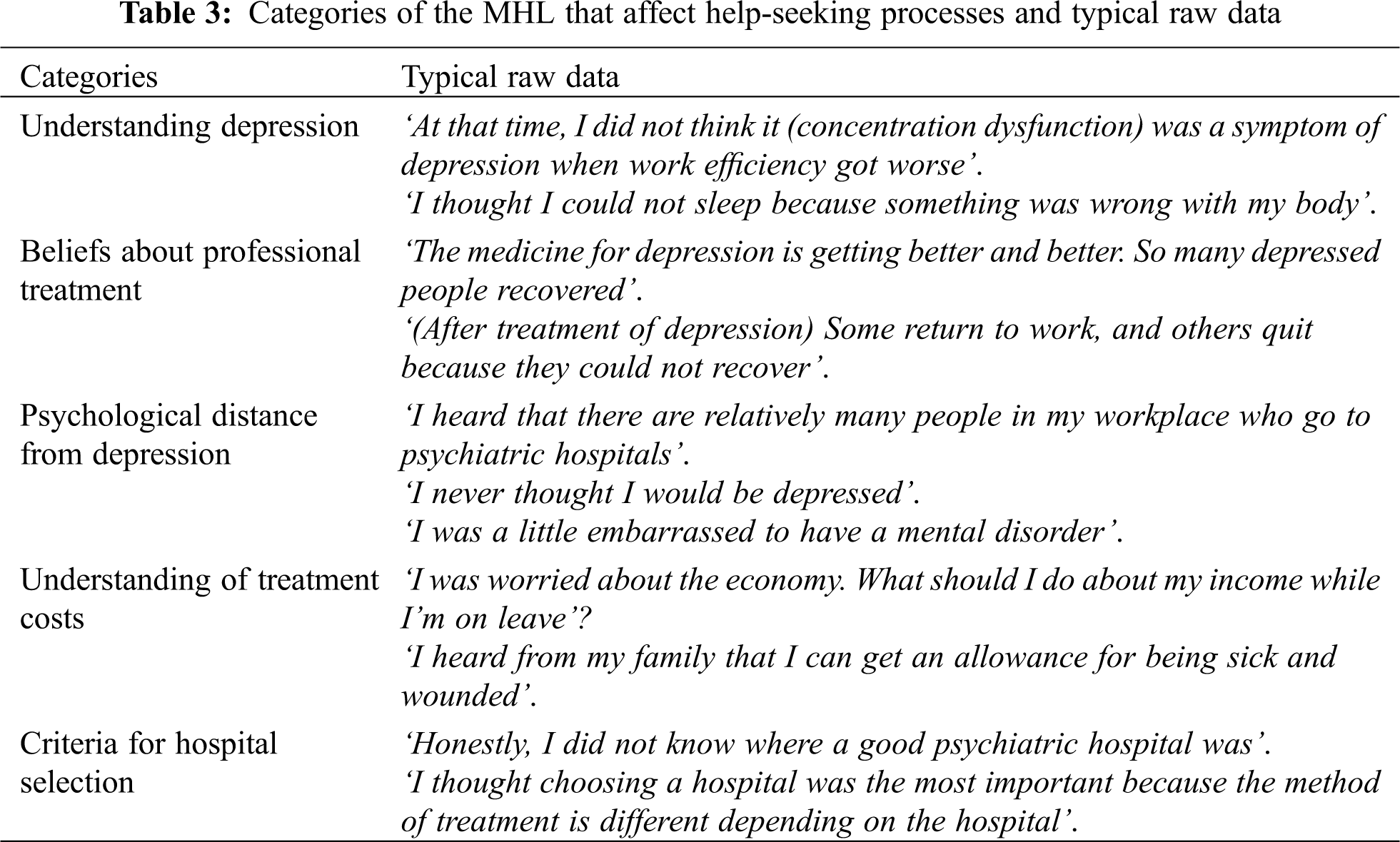
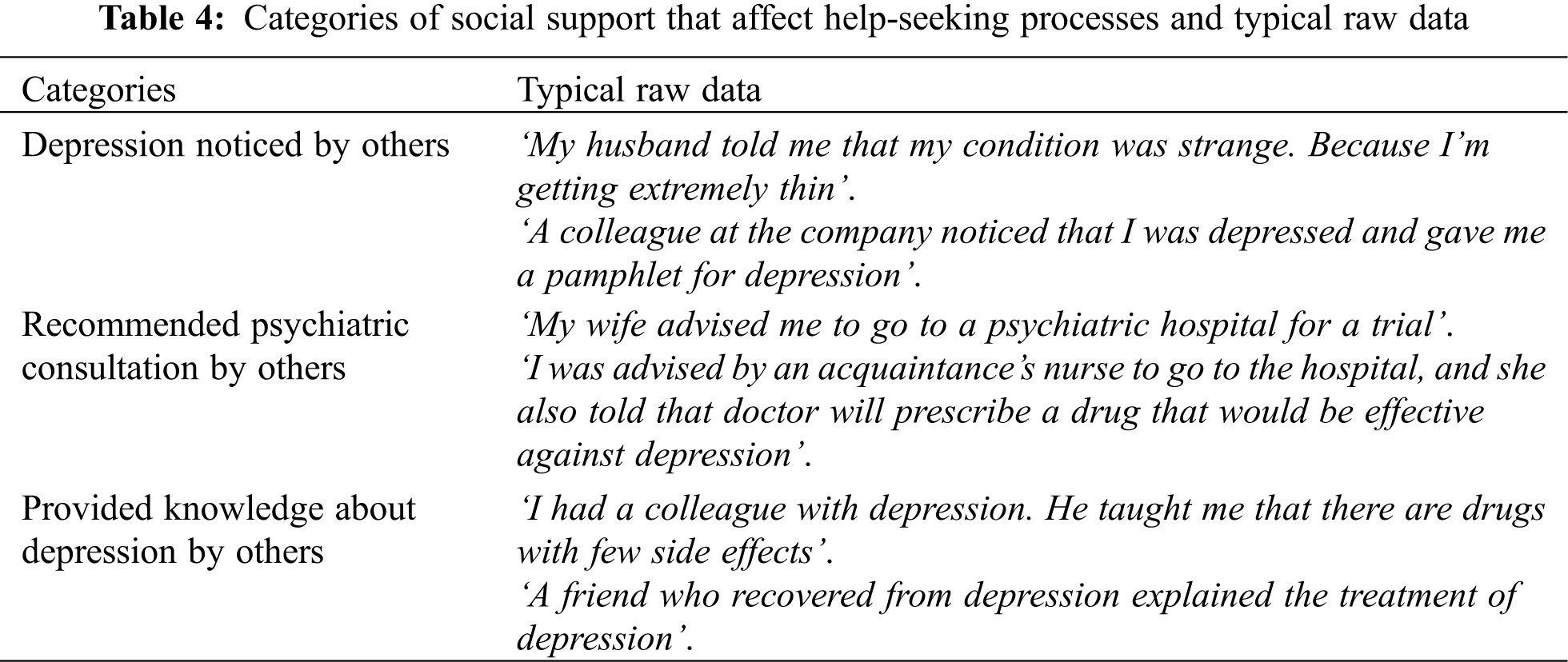
From the first eight participants, new categories emerged. From the data of the ninth participant, no new categories were generated. Thus, we considered that theoretical saturation had been reached. Details of the participants are illustrated in Tab. 2. We extracted five categories of the MHL that affected the help-seeking process: 1) understanding depression, 2) beliefs about professional treatment, 3) psychological distance from depression, 4) understanding treatment costs, and 5) criteria for hospital selection. The typical raw data for each category are presented in Tab. 3. Furthermore, the following three social support categories that promote the help-seeking process were extracted: ‘depression noticed by others’, ‘recommended psychiatric consultation by others’, and ‘provided knowledge about depression from others’. These typical raw data are illustrated in Tab. 4.
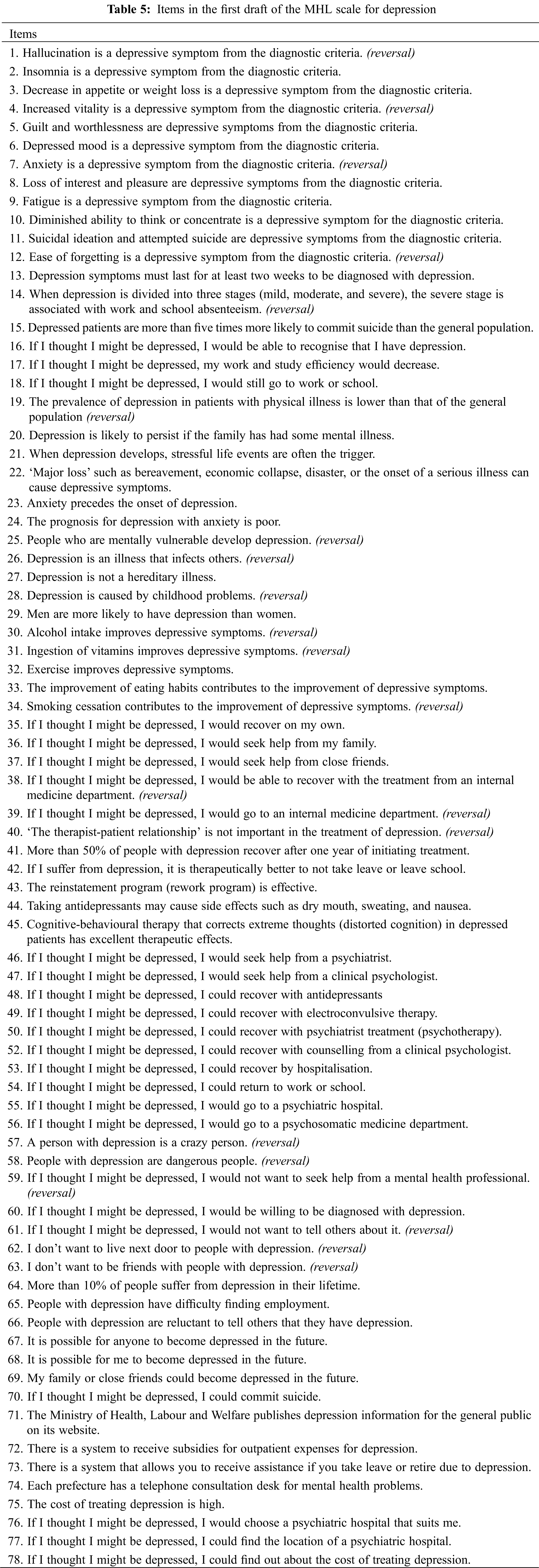
3.3 Study 3: Development of an MHL Scale for Depression
The first draft scale developed from Studies 1 and 2 and consists of 78 questions (Tab. 5). All are rated on five-point Likert scales ranging from ‘don’t think so’ (1) to ‘think so’ (5), including 21 reverse-scored items. Higher scores indicate higher MHL. Spearman’s rank correlation coefficients revealed that 11 items were significantly correlated with the help-seeking process (Tab. 6).
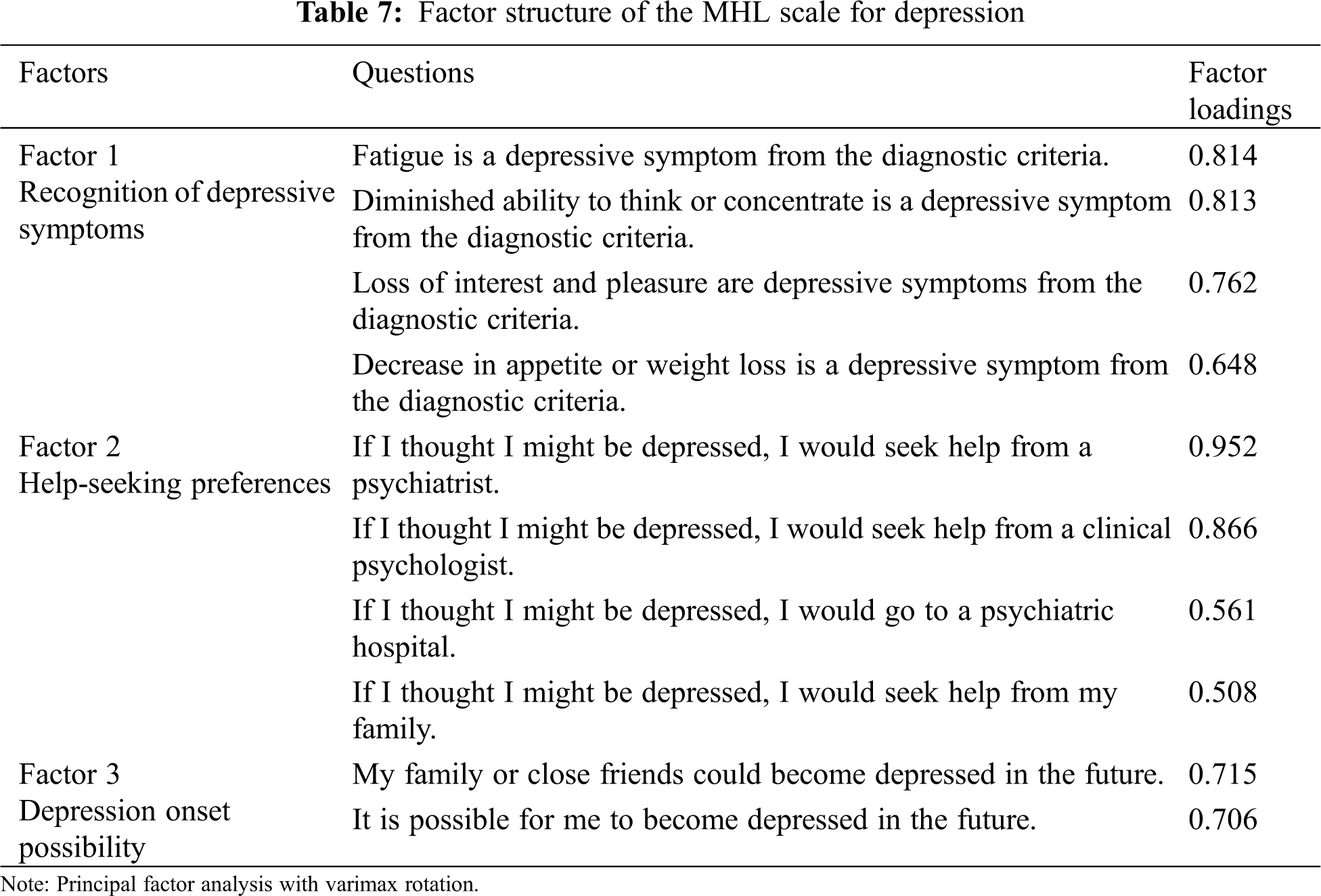
A principal factor analysis with varimax rotation was performed (Tab. 7), and simple structures of the three factors explaining 56.53% of the variance in the MHL for depression were obtained. The Kaiser-Meyer-Olkin’s measure of sampling adequacy was 0.750, and Bartlett’s test of sphericity was 3027.359 (P < 0.001).
Factor 1 was ‘recognition of depression symptoms’, as four items were related to understanding diagnostic criteria for depression, such as ‘fatigue is a depressive symptom from the diagnostic criteria’. Factor 2 was ‘help-seeking preferences’, as four items were related to the possibility of seeking help from others or professional institutions, such as ‘If I thought I might be depressed, I would seek help from a psychiatrist’. Factor 3 was named ‘depression onset possibility’, as two items were related to the possibility of depression onset, such as ‘My family or close friends could become depressed in the future’.
The goodness of fit indices of CFA had good values: GFI = 0.989, AGFI = 0.982, CFI = 0.997, RMSEA = 0.018 (0.000–0.034).
3.3.3 Criterion-Related Validity
HLOC scores indicated a weak positive correlation (r = 0.21) with help-seeking preferences (Factor 2) and a weak negative correlation (r = −0.24) with depression onset possibility (Factor 3).
Regarding internal consistency, Cronbach’s α = 0.85, 0.80, 0.68, and .70 for Factors 1, 2, and 3 and total score, respectively. Test-retest reliability was evaluated for 44 participants, and the ICC of the total score was 0.78.
3.3.5 Features about an MHL Scale for Depression
From the above results, the developed MHL scale for depression consisted of 10 items. The score range is 10 to 50 points because of the 5-point Likert scale which 1 to 5 points. The higher the score, the higher the degree of MHL for depression.
3.4 Study 4: Verifying the Components of the MHL of Depression that Affect the Help-Seeking Process
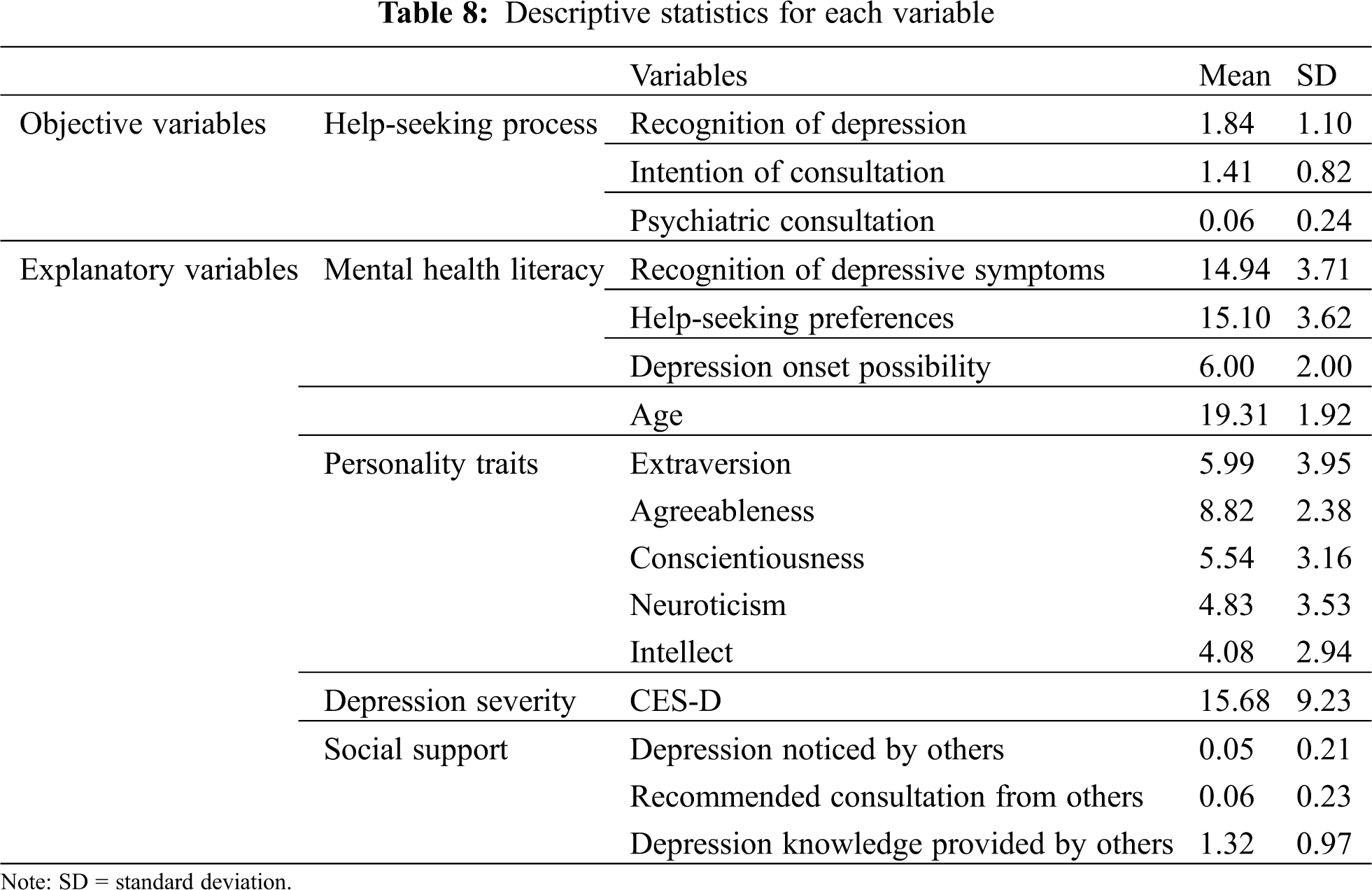
3.4.1 Descriptive Statistics for Each Variable
Tab. 8 illustrates the descriptive statistics for each variable. There were 341 (43.6%) participants who exceeded the cut-off point of suspected depression (CES-D scores ≥16), and 48 participants (14.0% of depressed participants) visited a psychiatric hospital.
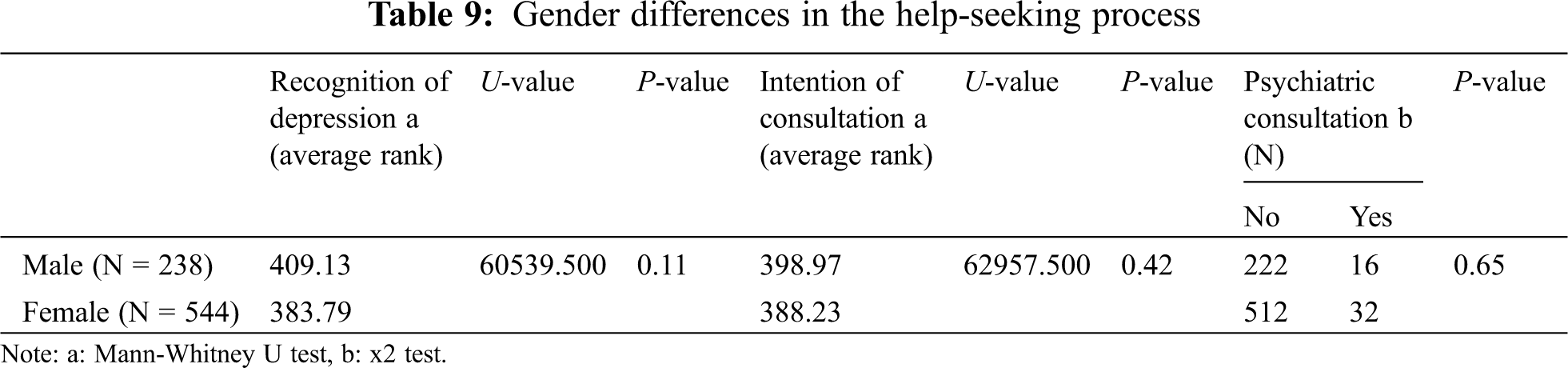
3.4.2 Gender Differences in the Help-Seeking Process
Tab. 9 illustrates the differences in the help-seeking process by gender. There was no significant difference in any help-seeking processes.
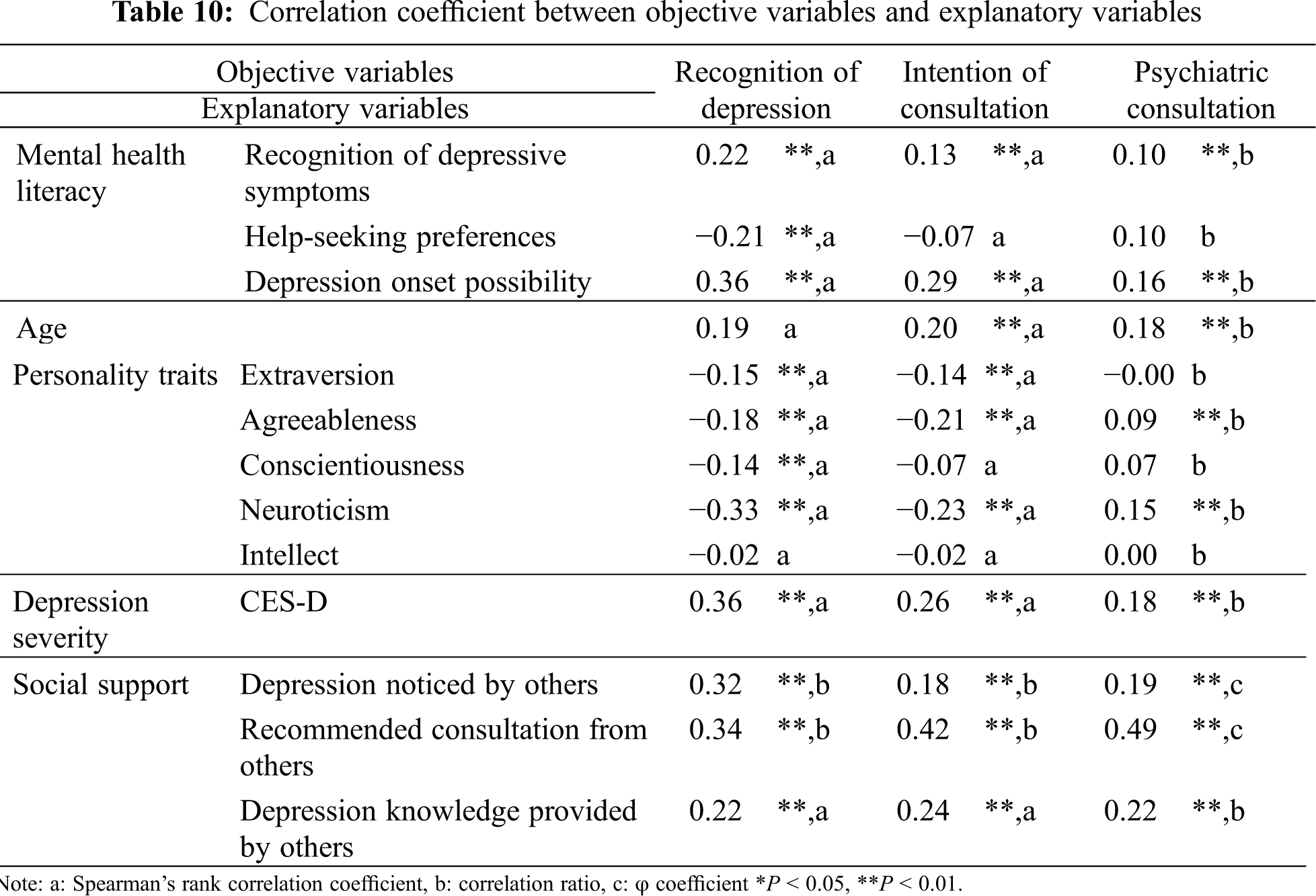
3.4.3 Correlation Coefficient between Objective Variables and Explanatory Variables
Tab. 10 illustrates the correlation coefficient between the objective variables and the explanatory variables. There were ten items with a correlation coefficient of 0.2 or more: recognition of depressive symptoms, help-seeking preferences, depression onset possibility, age, depression severity, personality (agreeableness, neuroticism), depression noticed by others, recommended consultation from others, and depression knowledge provided by others.
3.4.4 Structural Equation Modelling (SEM)
A path diagram consisting of the explanatory variables and objective variables with a correlation coefficient of 0.2 or more was created. We repeatedly deleted paths where the standardised partial regression coefficient or the correlation coefficient between the variables were not significant. Consequently, Fig. 2 was obtained (Model 1). The multiple correlation coefficient of the objective variable was recognition of depression R2 = 0.33, intention of consultation R2 = 0.43, and psychiatric consultation R2 = 0.36. The goodness-of-fit of the model was GFI = 0.990, AGFI = 0.966, CFI = 0.986, RMSEA = 0.043, all of which met the standard values.
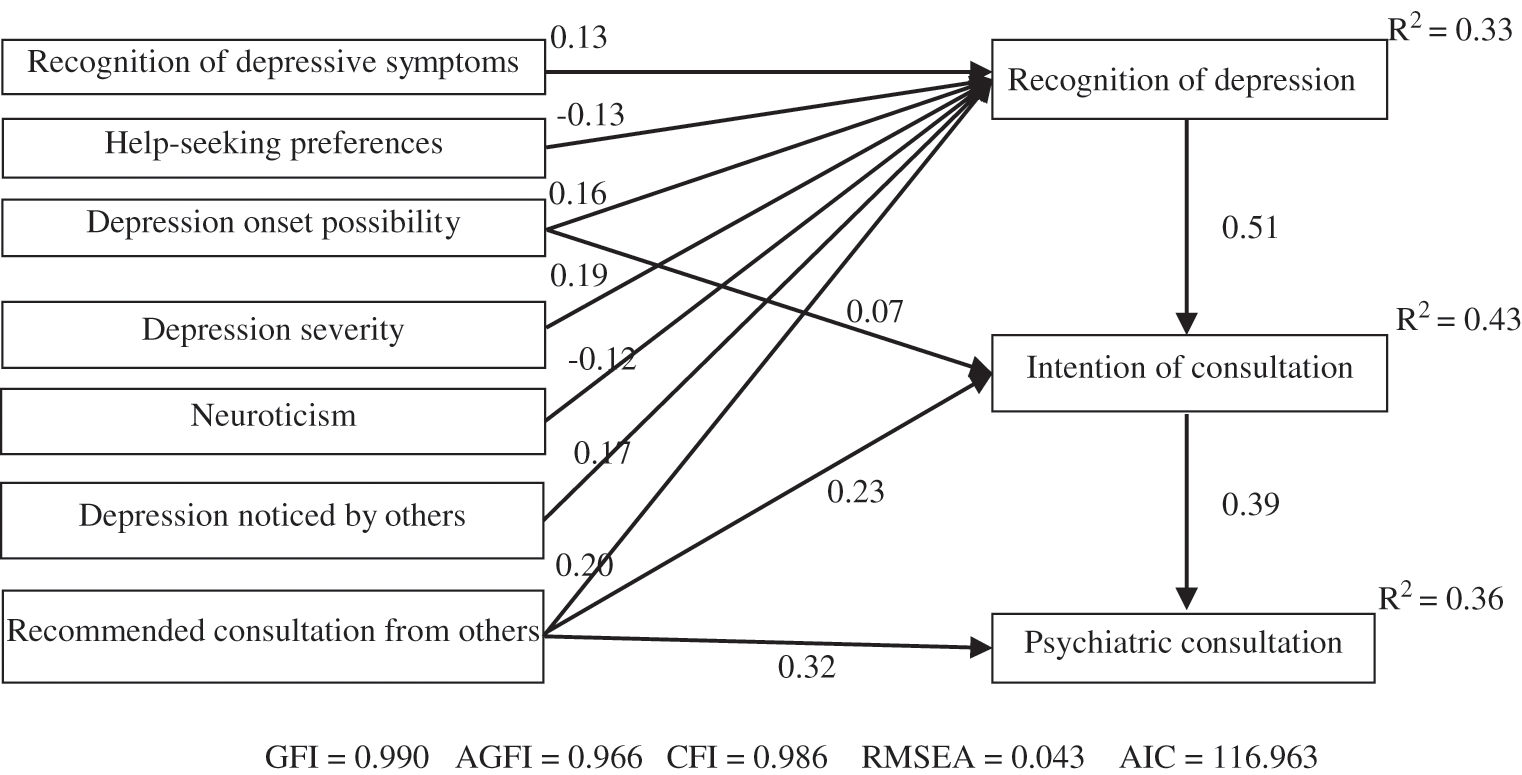
Figure 2: MHL of depression and other factors affecting the help-seeking process (Model 1)
The standardised partial regression coefficient value of the path from help-seeking preferences to recognition of depression was negative (β = −0.13). The reason for this was thought to be through the path of negative effects from the severity of depression. Therefore, we added a path from the severity of depression to help-seeking preferences and performed SEM again (Fig. 3, Model 2). Consequently, good goodness-of-fit indicators were obtained (GFI = 0.988, AGFI = 0.962, CFI = 0.982, RMSEA = 0.046). The multiple correlation coefficients of the objective variable and help-seeking preferences were recognition of depression R2 = 0.33, intention of consultation R2 = 0.43, psychiatric consultation R2 = 0.36, and help-seeking preferences R2 = 0.05. The AIC of Model 1 was 116.963, and the AIC of Model 2 was 122.228.
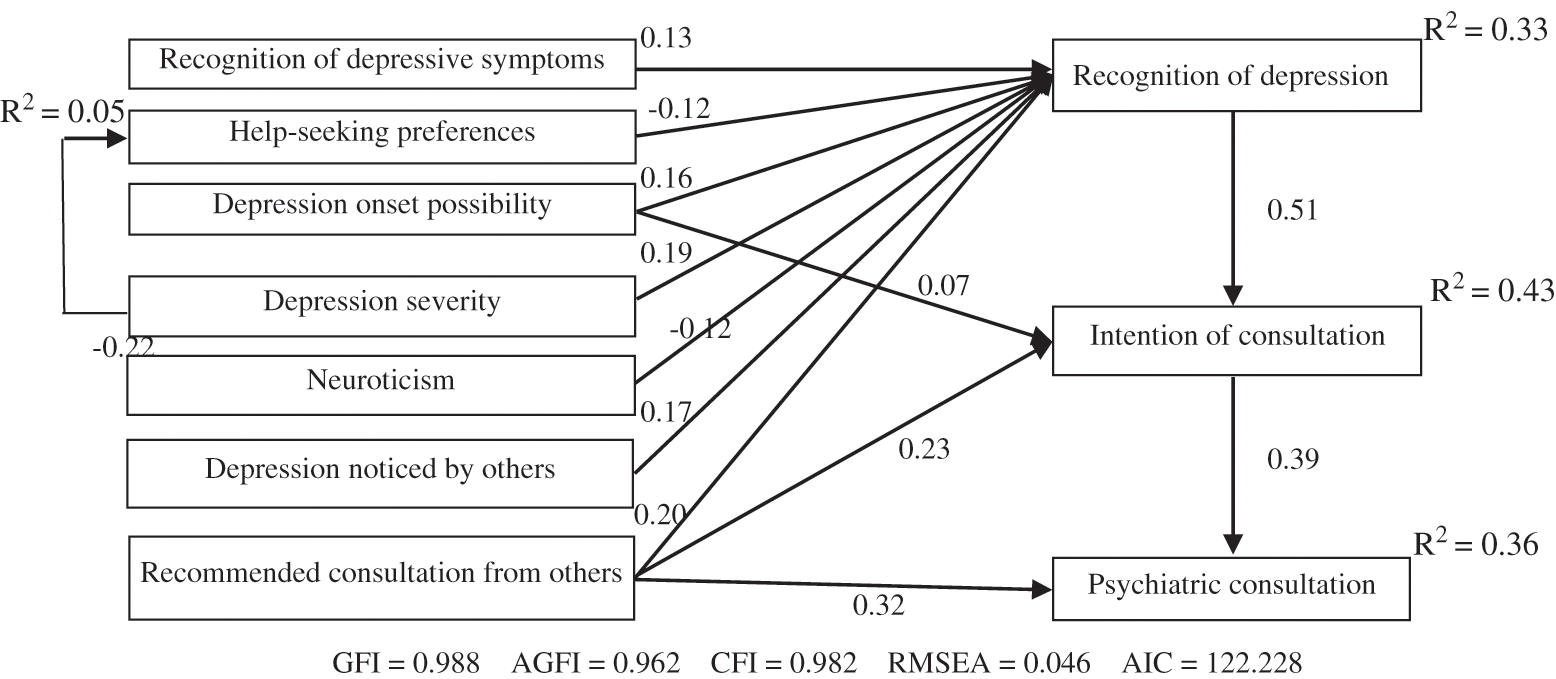
Figure 3: MHL of depression and other factors affecting the help-seeking process (Model 2)
This study aimed to clarify the specific components of the MHL that influences the help-seeking process to obtain evidence to support the shortening of the DUI of depression. In particular, as health professional students are exposed to the burden of depression but rarely seek help, these samples were targeted in this study. There were 341 (43.6%) who exceeded the cut-off point of suspected depression (CES-D scores ≥16). Thirteen previous studies investigated the prevalence rate of depression using CES-D targeted medical students who reported 42.8% (95% CI, 32.7–53.6) exceeded similar cut-off values [7]. Moreover, in this study, only 14% of those with suspected depression went to a psychiatric hospital—a low level consistent with previous studies (15.7%) [7]. Therefore, the sample of this study was considered to represent general health professional students.
In the development of the MHL scale for depression, a two-step factor analysis was performed, and, for the first time, it was possible to create a scale with a strong factor structure. Factor 1 was ‘recognition of depression symptoms’, Factor 2 was ‘help-seeking preferences’, and Factor 3 was ‘depression onset possibility’.
Internal consistency (Cronbach’s α) of Factor 1, Factor 2 and the total score had good values. Whereas Cronbach’s α value of Factor 3 was slightly lower because this factor has only two questions (stigma-related). In the first draft of the MHL scale for depression, there were other questions about stigma, but they were excluded during the factor analysis because they did not correlate significantly with the help-seeking process. As the participants in this study were health professional students, they may have responded positively to having a lower stigma. Namely, it was thought that the rumination bias was influential.
The ICC of test-retest reliability after two weeks was considered good. Of the two existing depression MHL scales developed for healthy populations, one did not verify test-retest reliability [16], and the other did not use the recommended method (correlation analysis) according to the consensus-based standards for the selection of health measurement instruments [14,23].
Spearman’s rank correlation coefficient with the HLOC scale was calculated to examine criterion-related validity. There was a weak positive correlation with Factor 2. This suggested that if people have high internal control scores, they tend to control their health by seeking help from professionals or their families. Additionally, there was a weak negative correlation with Factor 3. Thus, if people believe they can control their health, they are less likely to think they can become depressed. Therefore, we considered the validity of the scale to be assured.
In previous studies, there were several questionnaires that presented a depression vignette developed by Jorm et al. and asked participants to identify the disorder [8]. A study using a vignette of depression reported that those who correctly recognised depression had a stronger intention to seek help than those who could not [42]. However, Study 2’s results suggested that it is important to understand each symptom of diagnostic criteria. For example, participants in Study 2 did not recognise that difficulty in concentrating and sleep disturbances were diagnostic criteria for depression. Therefore, Factor 1 comprising questions on diagnostic criteria seemed to be appropriate. Particularly, diminished ability to think or concentrate and fatigue were considered important symptoms, due to large factor loadings. Additionally, decreased pleasure or interest were considered important symptoms, as they are essential for diagnosing depression.
Study 2 indicated ‘understanding of treatment costs’ and ‘criteria for hospital selection’ influenced the help-seeking process. However, questions that corresponded to those categories were not correlated with the help-seeking process in Study 3. This may be because the participants’ demographic data were not similar between Studies 2 and 3. The participants in Study 2 were working adults, while those in Study 3 were undergraduate students. For young people who have depressive symptoms, it has been reported that important adults in their lives (in many cases, parents) become gatekeepers, and can support the help-seeking process [43]. For undergraduate students, the final decision regarding psychiatric consultation is often made by their parents. Therefore, ‘criteria for hospital selection’ was not correlated with help-seeking. Additionally, for ‘understanding of treatment costs’ a worker may worry about medical expenses for treatment of depression, while undergraduate students are unlikely to pay their own medical expenses in Japan. This suggests that parents who have undergraduate children need to increase their MHL regarding treatment costs and psychiatric care. A previous study on the development of the MHL scale, which primarily targeted the working population, included a component of confidence in obtaining information on mental disorders [44]. In this study, we targeted the undergraduate health professional students, but considering important adults in their lives can support the help-seeking process. It is desirable to develop an MHL scale for depression targetting parents generations who have undergraduate health professional students.
As a noteworthy point of this research, the severity of the depressive symptoms had a negative impact on the recognition of depression through help-seeking preference. Thus, the more severe the depression, the less help-seeking preference. Furthermore, severe symptoms make it difficult for sufferers to recognise their depression. A previous study reported a negative correlation between help-seeking preferences and depression severity [45]. Additionally, previous studies have demonstrated that medical students with severe depression, or other mental health issues, have a higher risk of not seeking help than those with mild mental health conditions [46,47]. The reason for this may be that some of the symptoms of depression (i.e., thought disorders and decreased motivation), interfere with the decision to seek professional help. Another possible reason for this is the stigma related to medical students having depression, which can lead to feelings of embarrassment to seek help. This study’s results emphasise the importance of receiving appropriate treatment at an earlier stage of depression. The significance of this study is the promotion of early detection, a secondary prevention, by clarifying the components of the MHL required to promote the help-seeking process. However, from the results that non- or mildly-depressed people are more likely to receive help, we believe that it is important to prevent depression as much as possible.
Factor 3, which consists of questions about stigma, had the most significant impact on recognising depression, and it also affected the intention to seek consultation. The new definition of the MHL emphasises the importance of the stigma associated with depression [9]. Additionally, a previous study has reported the negative impact of stigma on the help-seeking process [48], and the results of this study are similar. This is considered to be supported by the health belief model [49]. The theory postulates that when individuals recognise they are strongly susceptible to developing illness X, they fear becoming ill with illness X, and subsequently, they are more likely to take appropriate coping actions. Additionally, consistent with this study, it was reported that those who agree that ‘anyone may suffer from depression’ are more likely to seek help from specialists, such as clinical psychologists and psychiatrists, than those who do not [50]. Moreover, in Study 2, the participants who stated ‘I never thought I would have depression’ delayed seeking psychiatric services. Previous studies have also reported that those with optimistic perceptions such as ‘depression does not last long’ and ‘does not cause major problems in daily life’ did not seek help [51]. This suggested that improving awareness of the possibility of depression onset could promote the help-seeking process.
Although this study focused on MHL, two types of social support were the most influential in the help-seeking process. It has been reported that young people have a lower consultation rate than other age groups, which might indicate that young people tend to prefer problem-solving on their own [52]. Also, as mentioned above, it has been reported that parents and other important adults are the main gatekeepers for young people’s requests for help. Furthermore, as increasing the severity of depression may reduce help-seeking preferences, it is important for those around to notice the change in the individual’s condition and provide social support. Therefore, we suggest that it is important to provide the specific MHL components revealed by this study, not only to students but also to family members and university personnel.
This study has some limitations. First, we focused on depression, which is a distressing mental illness. However, it is also necessary to pay attention to anxiety disorders, which have a prevalence similar to depression but a lower rate of seeking help [6,53]. Additionally, depression and anxiety disorders are comorbid [54], and therefore, it is necessary to consider the relationship between MHL for anxiety disorders and the help-seeking process in the future. Additionally, the process of help-seeking may differ in the three groups: depression only, anxiety disorders only, and depression and anxiety disorders. Second, the severity of depression had a negative impact on the recognition of depression through help-seeking preferences. This interpretation must be taken with caution. This is because the severity of depression had a positive impact on the recognition of this illness. In the future, it will be necessary to examine the relationship between the degree of severity, help-seeking preferences, and the degree of recognition of depression in more detail. Third, this study was a cross-sectional study. Longitudinal study techniques may reveal a relationship between varying severity of depression and its recognition. Additionally, taking psychiatric lectures and clinical practice experience in psychiatry may have a positive impact on the MHL of depression and the help-seeking process. A prospective study may reveal the relationship between MHL and educational experience and its impact on the help-seeking process.
Through a systematic literature review and interviews with individuals with depression, this study developed a highly valid MHL scale for depression with a strong three-factor structure. The investigation of the relationship between MHL of depression and the help-seeking process in health professional students revealed that all three factors of the MHL of depression influenced the help-seeking process. MHL education is important, not only for health professional students but also for those involved, as social support has a greater impact than MHL of depression.
Acknowledgement: We would like to thank Dr. Takeharu Ueno for recruiting participants, and Editage (www.editage.com) for English language editing.
Availability of Data and Materials: The data that support the findings of this study are available from the corresponding author upon reasonable request.
Funding Statement: This work was supported by JSPS KAKENHI Grant No. 17K18039.
Conflicts of Interest: The authors have no conflicts of interest directly relevant to the content of this article.
1. Kodaka, M., Matsumoto, T., Takai, M., Yamauchi, T., Kawamoto, S. et al. (2017). Exploring suicide risk factors among Japanese individuals: The largest case-control psychological autopsy study in Japan. Asian Journal of Psychiatry, 27, 123–126. [Google Scholar]
2. Ministry of Health, Labour and Welfare Japan (2021). Vital Statistics of Japan. https://www.e-stat.go.jp/en/stat-search/files?page=1&toukei=00450011&tstat=000001028897. [Google Scholar]
3. Asia Pacific Observatory on Health Systems and Policies (2018). Japan health system review. https://apps.who.int/iris/bitstream/handle/10665/259941/9789290226260-eng.pdf?sequence=1&isAllowed=y. [Google Scholar]
4. Dell’Osso, B., Altamura, A. C. (2010). Duration of untreated psychosis and duration of untreated illness: New vistas. CNS Spectrum, 15(4), 238–246. [Google Scholar]
5. Ghio, L., Gotelli, S., Marcenaro, M., Amore, M., Natta, W. (2014). Duration of untreated illness and outcomes in unipolar depression: A systematic review and meta-analysis. Journal of Affective Disorders, 152–154, 45–51. [Google Scholar]
6. Wang, P. S., Angermeyer, M., Borges, G., Bruffaerts, R., Tat Chiu, W. et al. (2007). Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry, 6(3), 177–185. [Google Scholar]
7. Rotenstein, L. S., Ramos, M. A., Torre, M., Segal, J. B., Peluso, M. J. et al. (2016). Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA, 316(21), 2214–2236. [Google Scholar]
8. Jorm, A. F., Korten, A. E., Jascomb, P. A., Christensen, H., Rodgers, B. et al. (1997). Public beliefs about causes and risk factors for depression and schizophrenia. Social Psychiatry and Psychiatric Epidemiology, 32(3), 143–148. [Google Scholar]
9. Kutcher, S., Wei, Y., Coniglio, C. (2016). Mental health literacy: Past, present, and future. Canadian Journal of Psychiatry, 61(3), 154–158. [Google Scholar]
10. World Health Organization Europe (2013). Health literacy: The solid facts. https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf. [Google Scholar]
11. Wei, Y., McGrath, P. J., Hayden, J., Kutcher, S. (2017). Measurement properties of mental health literacy tools measuring help-seeking: A systematic review. Journal of Mental Health, 26(6), 543–555. [Google Scholar]
12. Wei, Y., McGrath, P. J., Hayden, J., Kutcher, S. (2016). Measurement properties of tools measuring mental health knowledge: a systematic review. BMC Psychiatry, 16(1), 297. [Google Scholar]
13. Gabriel, A., Violato, C. (2009). The development of a knowledge test of depression and its treatment for patients suffering from non-psychotic depression: A psychometric assessment. BMC Psychiatry, 9, 56. [Google Scholar]
14. Gulliver, A., Griffiths, K. M., Christensen, H., Mackinnon, A., Calear, A. L. et al. (2012). Internet-based interventions to promote mental health help-seeking in elite athletes: An exploratory randomized controlled trial. Journal of Medical Internet Research, 14(3), e69. [Google Scholar]
15. Kronmüller, K. T., Saha, R., Kratz, B., Karr, M., Hunt, A. et al. (2008). Reliability and validity of the knowledge about depression and mania inventory. Psychopathology, 41(2), 69–76. [Google Scholar]
16. Hart, S. R., Kastelic, E. A., Wilcox, H. C., Beaudry, M. B., Musei, R. J. et al. (2014). Achieving depression literacy: the adolescent depression knowledge questionnaire (ADKQ). School Mental Health, 6, 213–223. [Google Scholar]
17. Strauss, A., Corbin, J. (1998). Basics of qualitative research, 2nd ed. USA: Sage. [Google Scholar]
18. Kline, R. B. (2011). Principles and practice of structural equation modeling, 3rd ed. USA: Guilford Press. [Google Scholar]
19. Srebnik, D., Cauce, A. M., Baydar, N. (1996). Help-seeking pathways for children and adolescents. Journal of Emotional and Behavioral Disorders, 4(4), 210–220. [Google Scholar]
20. Riggs, R. S., Noland, M. P. (1984). Factors related to the health knowledge and health behavior of disadvantaged black youth. Journal of School Health, 54(11), 432–434. [Google Scholar]
21. Hooper, D., Coughlan, J., Mullen, M. R. (2008). Structural equation modelling: Guidelines for determining model fit. Electronic Journal of Business Research Methods, 6(1), 53–60. [Google Scholar]
22. Tavakol, M., Dennick, R. (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education, 2, 53–55. [Google Scholar]
23. Terwee, C. B., Mokkink, L. B., Knol, D. L., Ostelo, R. W., Bouter, L. M. et al. (2012). Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Quality of Life Research, 21(4), 651–657. [Google Scholar]
24. O’Connor, P. J., Martin, B., Weeks, C. S., Ong, L. (2014). Factors that influence young people’s mental health help-seeking behavior: A study based on the Health Belief Model. Journal of Advanced Nursing, 70(11), 2577–2587. [Google Scholar]
25. van Zoonen, K., Kleiboer, A., Beekman, A. T., Smit, J. H., Boerema, A. M. et al. (2015). Reasons and determinants of help-seeking in people with a subclinical depression. Journal of Affective Disorders, 173, 105–112. [Google Scholar]
26. Bristow, K., Patten, S. (2002). Treatment-seeking rates and associated mediating factors among individuals with depression. Canadian Journal of Psychiatry, 47(7), 660–665. [Google Scholar]
27. Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
28. Ando, S., Nishida, A., Usami, S., Koike, S., Yamasaki, S. et al. (2018). Help-seeking intention for depression in early adolescents: Associated factors and sex differences. Journal of Affecting Disorders, 238, 359–365. [Google Scholar]
29. Al-Azzam, S., Alzoubi, K. H., Ayoub, N. M., Khader, Y. S., Karasneh, R. A. et al. (2013). An audit on public awareness of depression symptoms in Jordan. International Journal of Occupational Medicine and Environmental Health, 26(4), 545–554. [Google Scholar]
30. Costin, D. L., Mackinnon, A. J., Griffiths, K. M., Batterham, P. J., Bennett, A. J. et al. (2009). Health e-Cards as a means of encouraging help seeking for depression among young adults: Randomized controlled trial. Journal of Medical Internet Research, 11(4), 1–14. [Google Scholar]
31. Griffiths, K. M., Christensen, H., Jorm, A. F., Evans, K., Groves, C. (2004). Effect of web-based depression literacy and cognitive-behavioural therapy interventions on stigmatizing attitudes to depression: Randomized controlled trial. British Journal of Psychiatry, 185(4), 342–349. [Google Scholar]
32. Hernandez, M. Y., Organista, K. C. (2013). Entertainment-education? A fotonovela? A new strategy to improve depression literacy and help-seeking behaviors in at-risk immigrant Latinas. American Journal of Community Psychology, 52(3–4), 224–235. [Google Scholar]
33. Hickie, I. B., Davenport, T. A., Luscombe, G. M., Rong, Y., Hickie, M. L. et al. (2007). The assessment of depression awareness and help-seeking behavior: experience with the international depression literacy survey. BMC Psychiatry, 7, 48. [Google Scholar]
34. Jorm, A. F., Christensen, H., Griffiths, K. M. (2005). The impact of beyoundblue: The national depression initiative on the Australian public’s recognition of depression and beliefs about treatments. Australian & New Zealand Journal of Psychiatry, 39(4), 248–254. [Google Scholar]
35. Jorm, A. F., Nakane, Y., Christensen, H., Yoshioka, K., Griffiths, K. M. et al. (2005). Public beliefs about treatment and outcome of mental disorders: A comparison of Australia and Japan. BMC Medicine, 3, 12. DOI 10.1186/1741-7015-3-12. [Google Scholar] [CrossRef]
36. Jorm, A. F., Wright, A., Morgan, A. J. (2007). Beliefs about appropriate first aid for young people with mental disorders: Findings from an Australian national survey of youth and parents. Early Intervention in Psychiatry, 1(1), 61–70. [Google Scholar]
37. Khan, T. M., Sulaiman, S. A., Hassali, M. A., Tahir, H. (2009). Attitude toward depression, its complications, prevention and barriers to seeking help among ethnic groups in Penang. Malaysia Mental Health in Family Medicine, 6(4), 219–227. [Google Scholar]
38. Khan, T. M., Sulaiman, S. A., Hassali, M. A. (2010). Mental health literacy towards depression among non-medical students at a Malaysian university. Mental Health in Family Medicine, 7(1), 27–35. [Google Scholar]
39. Kohn, R., Sharma, D., Camilleri, C. P., Levav, I. (2000). Attitudes towards mental illness in the Commonwealth of Dominica. Pan American Journal of Public Health, 7(3), 148–154. [Google Scholar]
40. Link, B. G., Phelan, J. C., Bresnahan, M., Stueve, A., Pescosolido, B. A. (1999). Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American Journal of Public Health, 89(9), 1328–1333. [Google Scholar]
41. Munizza, C., Argentero, P., Coppo, A., Tibaldi, G., di Giannantonio, M. et al. (2013). Public beliefs and attitudes towards depression in Italy: A national survey. PLoS One, 8(5), e63806. [Google Scholar]
42. Kim, J. E., Saw, A., Zane, N. (2015). The influence of psychological symptoms on mental health literacy of college students. American Journal of Orthopsychiatry, 85(6), 620–630. [Google Scholar]
43. Iskra, W., Deane, F. P., Wahlin, T., Davis, E. L. (2018). Parental perceptions of barriers to mental health services for young people. Early Intervention in Psychiatry, 12(2), 125–134. [Google Scholar]
44. Nejatian, M., Tehrani, H., Momeniyan, V., Jafari, A. (2021). Amodified version of the mental health literacy scale (MHLS) in Iranian people. BMC Psychiatry, 21, 53. [Google Scholar]
45. Garland, A. F., Zigler, E. F. (1994). Psychological correlates of help-seeking attitudes among children and adolescents. American Journal of Orthopsychiatry, 64(4), 586–593. [Google Scholar]
46. Schwenk, T. L., Davis, L., Wimsatt, L. A. (2010). Depression, stigma, and suicidal ideation in medical students. JAMA, 304(11), 1181–1190. [Google Scholar]
47. Seera, G., Arya, S., Sethi, S., Nimmawitt, N., Ratta-Apha, W. (2020). Help-seeking behaviors for mental health problems in medical students: Studies in Thailand and India. Asian Journal of Psychiatry, 54, 102453. DOI 10.1016/j.ajp.2020.102453. [Google Scholar] [CrossRef]
48. Schomerus, G., Stolzenburg, S., Freitag, S., Speerforck, S., Janowitz, D. et al. (2019). Stigma as a barrier to recognizing personal mental illness and seeking help: A prospective study among untreated persons with mental illness. European Archives of Psychiatry and Clinical Neuroscience, 269(4), 469–479. [Google Scholar]
49. Rosenstock, I. M., Strecher, V. J., Becker, M. H. (1988). Social learning theory and the Health Belief Model. Health Education Quarterly, 15(2), 175–183. [Google Scholar]
50. Jiang, Y., Bogner, H. R., Wang, X., Wang, J., Zhu, T. et al. (2018). Primary care patient beliefs and help-seeking preferences regarding depression in China. Psychiatry Research, 269, 1–8. [Google Scholar]
51. Elwy, A. R., Yeh, J., Worcester, J., Eisen, S. V. (2011). An illness perception model of primary care patients’ help seeking for depression. Qualitative Health Research, 21(11), 1495–1507. [Google Scholar]
52. Kessler, R. C., Berglund, P. A., Bruce, M. L., Koch, J. R., Laska, E. M. et al. (2001). The prevalence and correlates of untreated serious mental illness. Health Service Research, 36, 987–1007. [Google Scholar]
53. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators (2017). Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet, 390, 1211–1259. [Google Scholar]
54. Essau, C. A., de la Torre-Luque, A. (2019). Comorbidity profile of mental disorders among adolescents: A latent class analysis. Psychiatry Research, 278, 228–234. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |