
Mental Health Promotion
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/IJMHP.2021.013098
ARTICLE
Effectiveness of Half-Cut Wood Training of Close and Kinetic Chain Method on Mental Health and Physical Health of Patients with Knee Instability in China
1School of Medicine and Dentistry, Griffith University, Queensland, 4222, Australia
2Tonwo Technology Health Clinics, Guangzhou, 510435, China
3Menzies Health Institute Queensland, Griffith University, Queensland, 4222, Australia
4School of International and Public Affairs, Shanghai Jiaotong University, Shanghai, 200230, China
*Corresponding Author: Jing Sun. Email: j.sun@griffith.edu.au
Received: 11 September 2020; Accepted: 15 March 2021
Abstract: Knee instability as a symptom of ligament injury usually only receives attention when it causes pain or impacts patients’ mobility in China. In this study both the physical and psychosocial impact of an innovative approach to treatment, Half-cut Wood Training, was examined. Twenty individuals with knee instability who received Half-cut Wood Training (Intervention group) and twenty two individuals with knee instability who did not receive Half-cut Wood Training (as Control group) participated in the study. The electric WIFI based HBF-306 was used to collect the anthropometry and biomedical data. Symptom severity was assessed by a doctor and through response to a specific question. Half-cut Wood Training was used as the intervention for the knee instability patients, and the effects among pre-intervention, post-intervention and control group on self-esteem, self-efficacy, quality of life and reductions in knee instability were assessed and compared to patients in the control group. The Half-cut Wood Training has significantly improved the physical health, self-esteem, self-efficacy, legs and feet functioning of patients in the intervention group compared with control group. Moreover, the Symptom were decreased (F = 15.47, P < 0.001), and the doctor reported knee function was improved (F = 36.20, P < 0.001). The subgroups including number of sessions of attending the Half-cut Wood Training had effects on the reduction of symptoms and duration of training time more than one month has effect on the improvement of physical health. Half-cut Wood Training provides beneficial means of improving knee function, self-esteem, self-efficacy, and physical health of the quality of life of patients with the knee instability.
Keywords: Knee instability; half-cut wood training; self-esteem; self-efficacy; quality of life
Knee instability is a major symptom in patients with anterior cruciate ligament injury or knee osteoarthritis [1], and is a significant contributing factor to knee joint degeneration (pain and bone hyperplasia). The prevalence of knee instability is approximately 9–17% [2,3]. Instability is experienced as a sensation of buckling, shifting or giving way of the knee during dynamic activities such as walking [4]. If it is untreated, it leads to pain, restrictions in daily activities, altered walking patterns and an increased number of falls [5].
Through the action of walking on different types of surfaces, people gained knees stability and feet flexibility. Our knees are more suited for movement on a sagittal plane (anterior-posterior) rather than a coronal plane (left-right direction). When people turn around, ankle and articulation hip joint play important roles such that improving the mobility of ankles is an ideal means of preventing instable movement of knees. However, walking on flat and hard surfaces such as cement, makes humans’ ankles become immobile. This resulted in the stress associated with mobility being transferred to knees, damaging this joint and surrounding tissue.
Through the action of walking, knee instability can lead to larger frontal and sagittal plane knee movements, which results in alterations in knee joint loading [6,7]. Patients with increased laxity and self-reported instability have been shown to increase co-contraction of their knee musculature and reduced knee flexion and internal rotation angles when they are walking in order to reduce discomfortness [1].
Previous studies have shown that if a series of overlapping segments were connected via pin joints, these interlocking joints would create a system that would allow the movement of one joint to affect the movement of another joint within the kinetic chain [8,9]. This leads to knees and ankles operating in unity. In order to stabilize knees, ankle mobility should therefore be improved.
Knee function improvement is subject to continuous movement and exercise in daily life. To meet this demand, Half-cut Wood Training method is designed as a new rehabilitation approach using the Close Kinetic Chain principle in combination with Open Kinetic Chain strategies to patients with knee instability. The inspiration for it is drawn from Plum-blossom Boxing, an activity in the tradition of Kung Fu that commenced at the end of the Ming Dynasty. People who practice Plum-blossom Boxing need to walk on quincuncial piles to improve the stability and flexibility of their limbs.
Previous studies have shown knee instability can be treated through surgery [10]. Most of these surgery based studies have focused on the improvement of physical functioning and reduction of pain [11,12]. No studies have comprehensively tested the assumption that continuous movement and daily exercise can produce positive effect on improvement of both physical and mental health outcomes. There is an increasing evidence that quality of life, and positive mental health factors such as self-efficacy, self-esteem and mental health domain of quality of life have effects on their functional ability in people with knee instability. For example, people with knee instability after injury have shown significantly lower scores in mental health domain of quality of life as it was measured by SF 12 [13]. There is evidence suggesting that exercise and physical activity promote mental health and prevent mental health disorders such as depression and anxiety [14,15]. It would seem reasonable that if exercise had a positive effect on mental health, self-efficacy and self-esteem, then changes in these psychological factors in response to exercise could be associated with improved physical function and knee instability.
Self-efficacy, and the mental health domain of quality of life are essential factors in the well-being and rehabilitation of patients with knee instability [16], yet most research has focused on physical health. Health-related quality of life (HRQoL), a concept intended to reflect the physical and mental limitations of illness, has rarely been addressed after meniscectomy. This study aimed to evaluate the effectiveness of repeated training method using Half-cut Wood Training on the improvement of knee stability of patients. The mental health factors (self-esteem, self-efficacy, mental health domain of quality of life) associated with knee instability were investigated as secondary outcome of treatment using Half-cut Wood Training.
A prospective intervention study design was used, with data collected from October 2018 to March 2019 from patients who attended the Half-Cut Wood Training Clinic in Guangzhou, China. The Clinic was chosen because it specialized for the treatment of the condition and therefore sufficient patients could be obtained for the study. There were 42 patients participated in this study and they were randomized into two groups. Knee instability for the present study is defined as patients with mild or moderate level of a sensation of buckling, shifting or giving way of the knee during dynamic activities such as walking. When walking, the dynamics seem to cause the knee joint to shake side to side, and the lower limb muscle strength is unbalanced. If this person walks in this form for a long time, to a certain extent, the periosteum on the surface of the knee joint will be unevenly worn, the gap will increase, and finally it will gradually develop into the knee instability. Participants with anterior cruciate ligament injury, severe pain or anhydrous swelling fluid were excluded from the study, Twenty patients with mild and moderate knee instability during walking were randomized into the treatment group (male = 5, female = 15) aged from 15 to 38 years (M = 24.85). The control group consisted of 22 people with mild or moderate level of knee instability (male = 8, female = 14) aged from 22 years to 42 years (M = 29.33). As the intervention program was conducted in the clinics, there was no one dropped out of the program in the intervention group, and there were five patients in the control group did not complete post-intervention measures.
2.1 Half-Cut Wood Training Program
Previous studies have shown that if a series of overlapping segments were connected via pin joints, these interlocking joints would create a system that would allow the movement of one joint to affect the movement of another joint within the kinetic chain [8,9]. This leads to knees and ankles operating in unity. In order to stabilize knees, ankle mobility should therefore be improved. Our study therefore developed Half-wood Training method to reflect these principles. In this method, endways quincuncial piles were cut into half and placed transversely, in order to decrease the risk and the degree of difficulty, allowing for comfortable and convenient practice for patients with knee instability. Undertaking a supervised series of exercises on the Half-cut woods improves ankle flexion, and simultaneously strengthens the ankle and back of the calf muscles, quadriceps strength, knee and ankle range of motion, lower extremity muscle flexibility.
Half-cut Wood Training was designed for this study in Guangzhou Half-cut Wood Training Clinic. Half-cut Wood Training materials consist of logs that are cut into halves and placed transversely across the floor (length = 40 cm–50 cm, width = 15 cm–25 cm, height = 10 cm–20 cm). The logs are pictured in Fig. 1. As can be seen patients undertake the treatment barefooted.

Figure 1: Barefoot half wood training
The intervention group received the Half-cut Wood Training and the control group continued with usual activity. The intervention duration was from one month to three months, equating to between 20 and 40 sessions depending on patients’ symptom severity. The intervention was implemented in Half-cut Wood Trianing Clinic by one senior clinician and three clinical assistants who have completed over 500 hours supervision for the training. A randomized controlled trial intervention study was used to examine the effectiveness of the intervention program and protocol was registered in ANZCTR site with registration number: ACTRN12618001739202. Ethics approval was obtained through Griffith University Human Ethics Committee.
There are four phases of the intervention consisting of four phases with 40 lessons in total and the intervention will take both supervised individual level training plus self-directed exercise and qualified physicians will deliver the intervention program. Each lesson takes 45 min. This process is described as below:
Specifically, (1). Phase 1: 10 lessons in Education and posture training. This include basic understanding of the function of joints, characteristics of normal and abnormal postures and movements and joint related exercise. (2). 10 lessons in Phase 2. This phase will focus on multiple joints’ training and respiratory training. The purpose of the exercise is to facilitate coordination of action and respiration by exercise starting from one joint exercise to multiple joint based exercise. (3). 10 lessons in Phase 3. This phase will focus on abnormal knee joint and spine training. This phase exercise is to correct abnormal posture and shape of the spine. (4). 10 lessons in phase 4. This phase will focus on application in daily life. This will include rolling and balance training to enhance physical flexibility.
Undertaking a supervised series of exercises on the Half-cut woods improves ankle flexion, and simultaneously strengthens the ankle and back of the calf muscles, quadriceps strength, knee and ankle range of motion, lower extremity muscle flexibility. Half-cut Wood Training was designed for this study and was run in a clinics in China. Half-cut Wood Training materials consist of logs that are cut into halves and placed transversely across the floor (length = 40 cm–50 cm, width = 15 cm–25 cm, height = 10 cm–20 cm).
An intervention guideline is designed for this study. The intervention consisted of 3 hours exercise session per day (which is equivalent 2 lessons per day) for maximum 3 months period of time depending on individual’s improvement level. The intervention is individual level based.
Functional measures: Knee functioning was assessed by physician using performance based tests including questions and image processing analysis. The question includes: How well does knee work now? from 0 (Cannot do any movement) to 10 (Can do any movement) [17]. The image processing of video fluoroscopic (VFC) was analysed during movement. The analysis focused on the main biomechanics parameters such as the leg stability during a walking task, and leg flexion and extension during half wood walking tasks and the diagnosis was made by clinician.
Symptom Severity: was assessed firstly by doctor using motor and movement assessment method, then patients themselves provided self-report about their severity of knee instability from 1 (Not at all) to 5 (Extremely severe). The clinician reported effect of Half-cut Wood Training was assessed by the medical doctor about the improvement of patient knee instability from 0 to 100%.
Telehealth assessment on anthropometry and biomedical factor: The HBF-306 is a body-fat analyzer device that uses bioelectrical impedance analysis (BIA) to assesses anthropometric and biomedical indexes of participants including BMI, waist circumference, fat percentage, protein percentage, bone mass, and muscle mass [18]. Formulas were used to calculate these indexes, for example, Body fat percentage (%) = {body fat mass (kg)/body weight (kg)} × 100, Body fat mass (kg) = Body weight (kg) – Fat-free mass (kg). The HBF-306 connected with an APP via WIFI connection, and measurement results were sent instantly to the APP when body composition factors were measured.
Self-efficacy: An adapted version of the Self-efficacy questionnaire [19], consisting of 10 items using a five-point Likert Scale from 1 = Strongly disagree to 5 = Totally agree was used to measure self-efficacy. The overall reliability of the scale is acceptable (Cronbach’s alpha = 0.83).
Quality of life scale: The SF-12 scale [20], consisting of 12 items, was used to assess quality of life on eight dimensions including physical functioning (PF), role-physical (RP), body pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE), and mental health, (MH). The summary score for physical health includes four dimensions of PF, RP, BP, and GH. The summary score for mental health includes four dimensions of VT, SF, RE, and MH. The raw scores were converted to the standard score. The range of the score is 0–100. The higher the score means the healthier and better perception of health. The scale has a reliability level of Cronbach’s Alpha of 0.78.
A total of 42 subjects with knee instability were recruited for the study, consisting of 20 patients joined the Half-cut Wood Training as in the intervention group and 22 did not participate in Half-cut Wood Training therapy as the control group. Independent-samples t-tests and Pearson’s χ2-tests were conducted to examine differences and associations in relation to the demographic characteristics of each sample (see Tab. 1). It was apparent the two groups were well matched on all baseline demographic characteristics except age and education.
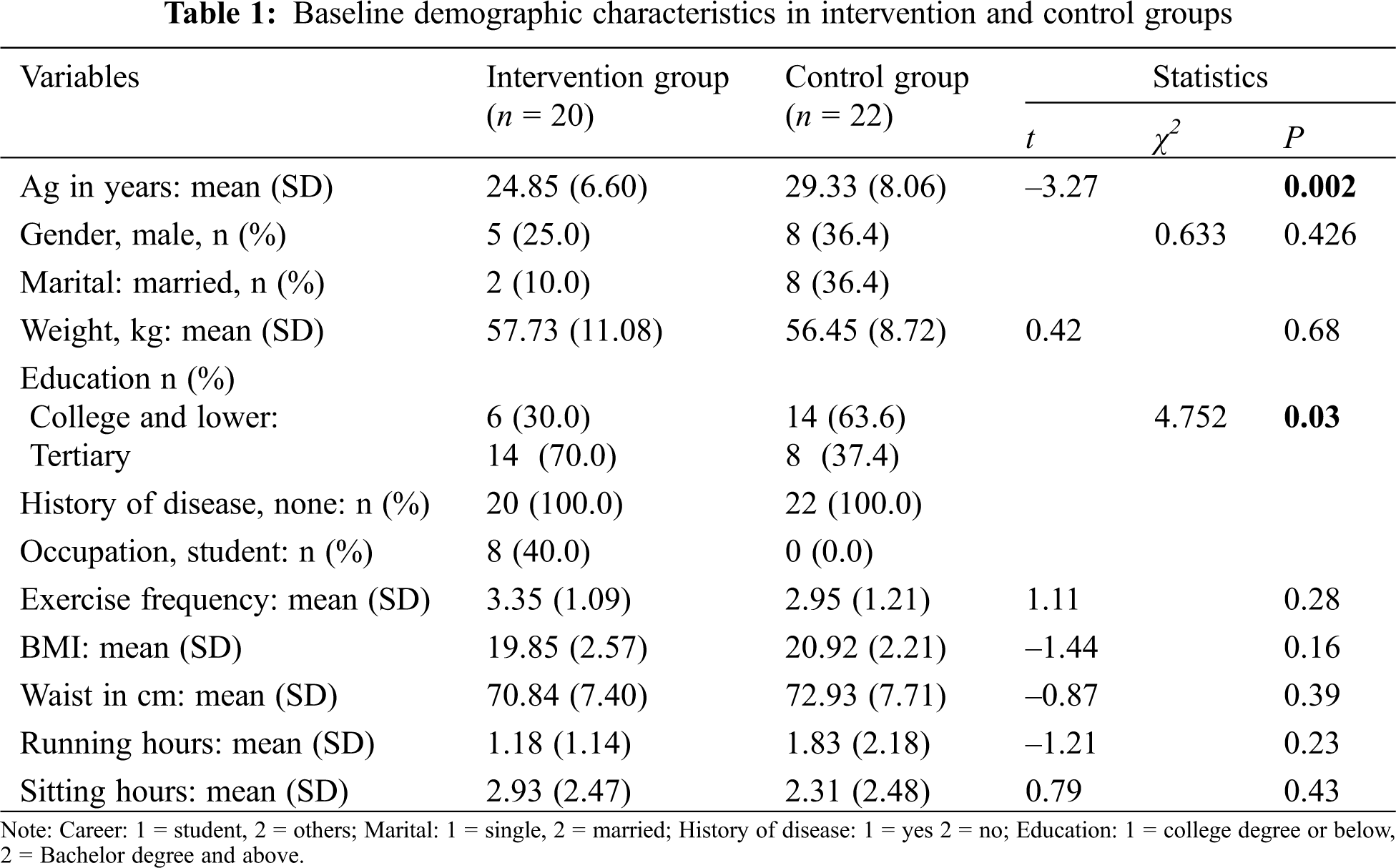
The means and standard deviations of all outcome measure scores at pre-intervention and post-intervention are provided in Tab. 2. Repeated-measures analysis of variance (ANOVA) was employed to compare the two groups over time on these variables. The main effect of time was significant, but there was no main effect of group on mental health, suggesting that there was a significant improvement in mental health score over the period of Half-cut Wood Training therapy F (1, 39) = 8.86, P = 0.005. There was also a significant time × group interaction in relation to physical health, indicating that there was significant intervention effect on physical health outcome. Analyses of the self-esteem score revealed a time × group interaction effect suggesting there was significant intervention effect on self-esteem. Analyses of the self-efficacy score revealed a significant time × group interaction effect suggesting the self-efficacy of intervention group was significantly improved than the control group after the intervention was completed, F (1, 40) = 5.02, P = 0.03. The time × group interaction in the function of legs and feet was marginally significant, indicating that the functional capacity of legs and feet of the intervention group was improved in comparison to the control group over the intervention period, F (1, 39) = 13.60, P = 0.08. There were no intervention effects in other variables.
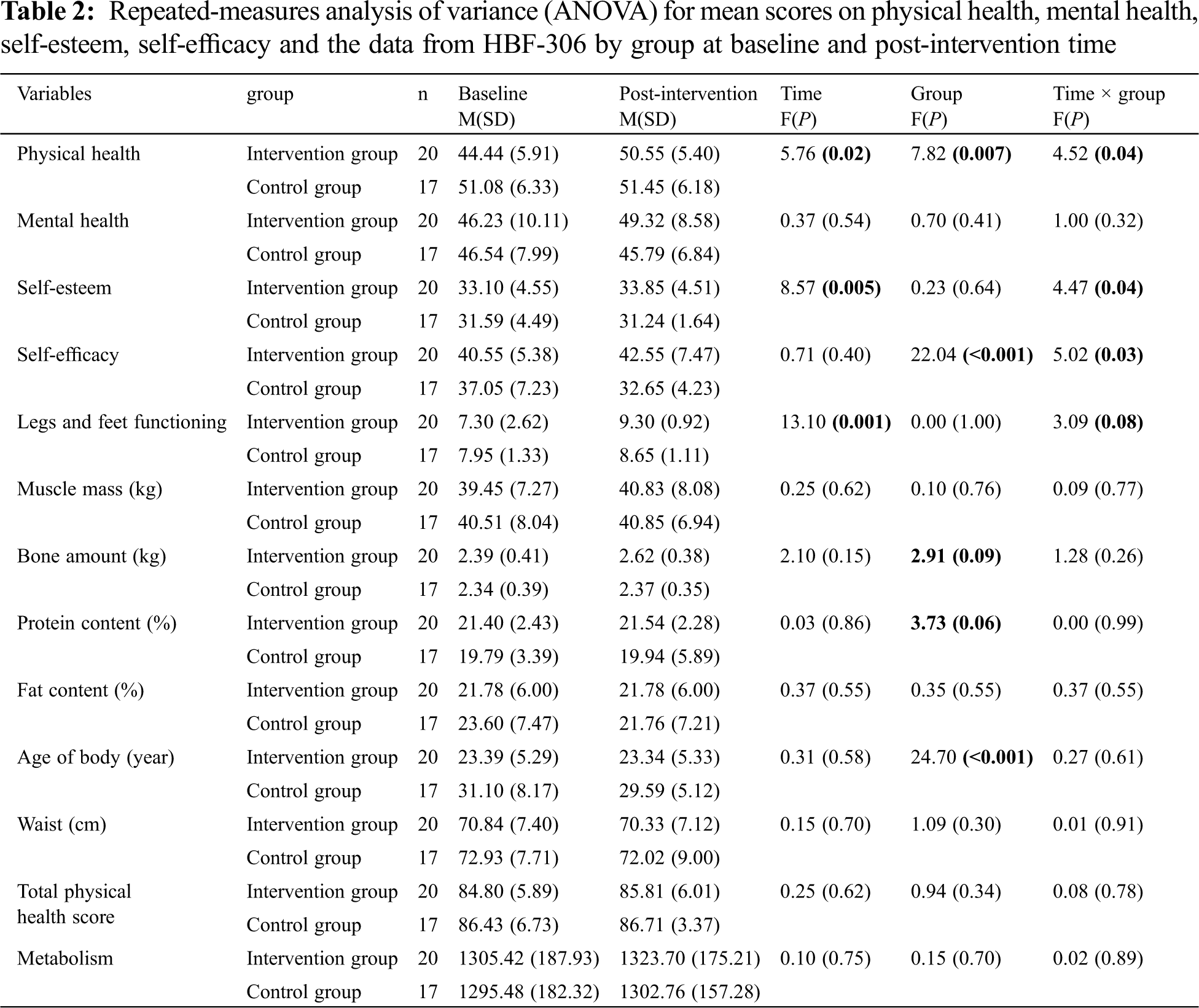
In Tab. 3, analyses of the muscle content revealed a main effect of time, indicating that there was a significant increase in muscle content across time F (1, 39) = 6.84, P = 0.013. The main effect of group means that the muscle content of the intervention group was significantly higher than the control group, F (1, 39) = 5.31, P = 0.027. The significant time × group interaction showed that the muscle content of the intervention group was significantly higher than the control group throughout the trial. Analyses of the bone content revealed a main effect of time, indicating that there was a significant increase in bone content across time F (1, 39) = 22.17, P < 0.001. The main effect of group means that the bone content of the intervention group was significantly higher than the control group, F (1, 39) = 4.29, P = 0.045. The main effect of time was found in the score of body’s quality suggesting that there was a significant increase in the body’s quality of intervention group, F (1, 39) = 7.09, P = 0.011. There was a significant time × group interaction in the body’s quality score, but there was no main effect of group, indicating that there was no significant difference between the intervention and control groups.
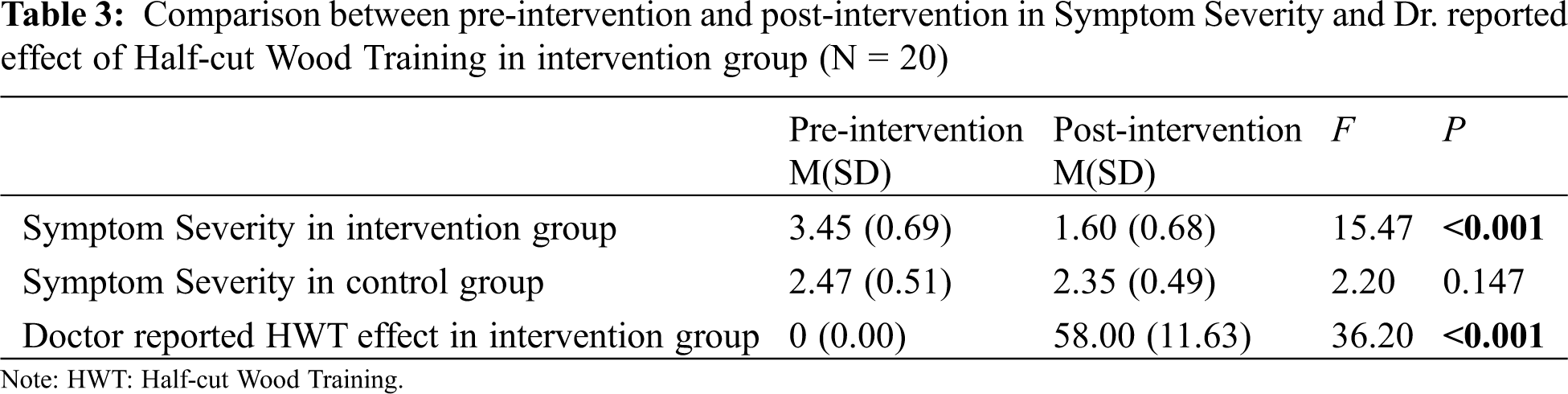
Tab. 3 shows that symptom severity at post-intervention (M = 1.60, SD = 0.68) was significantly lower than at pre-intervention (M = 3.45, SD = 0.69), F = 15.47, P < 0.001 in the intervention group. The doctor reported effect of Half-cut Wood Training at the post-intervention (M = 58.00, SD = 11.63) was significantly higher than pre-intervention (M = 0.00, SD = 0.00), F = 36.20, P < 0.001 in the intervention group. There was no significant difference in the control group relating to the symptoms improvement.
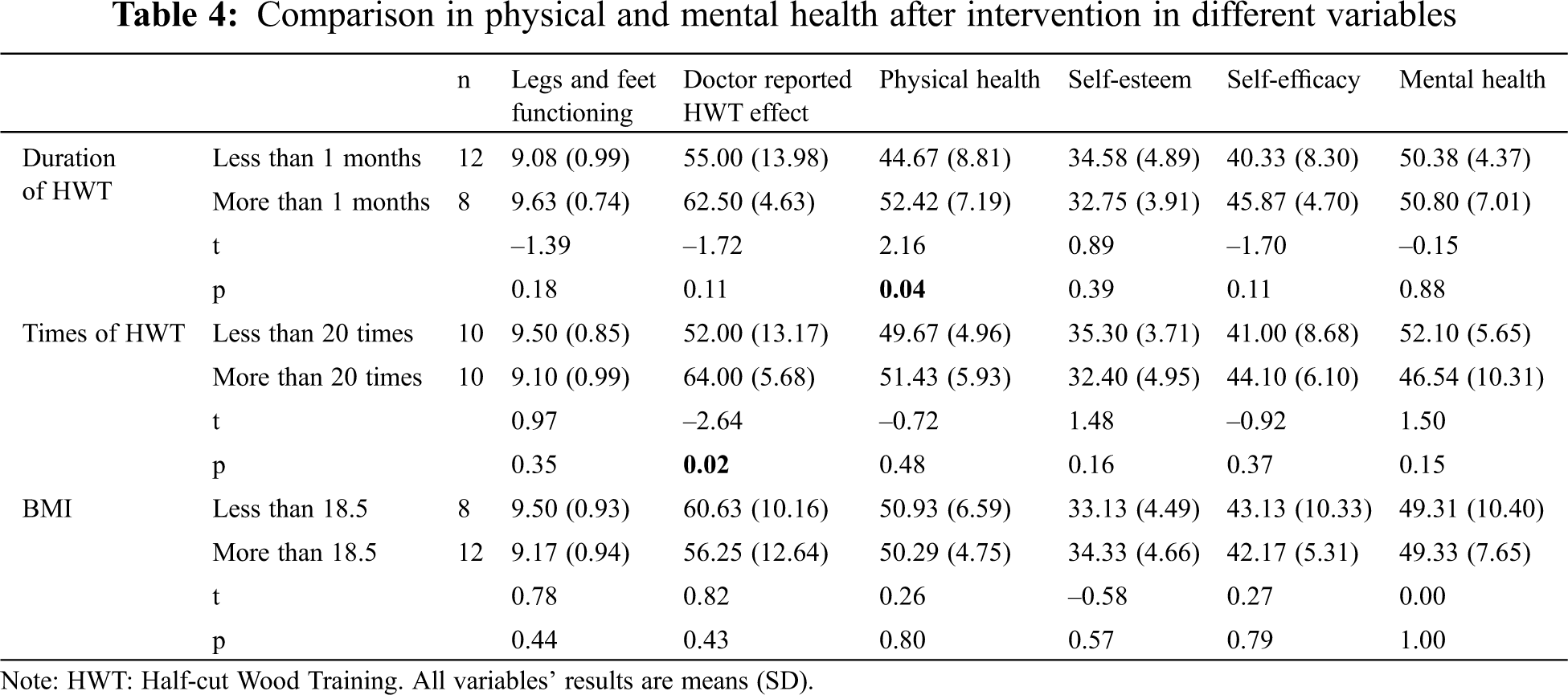
Tab. 4 shows there was a doctor reported significant effect of Half-cut Wood Training on the symptoms improvement (t = –2.64, P = 0.02) of patients who attended equal to or greater than 20 sessions compared to patients who attended less than 20 sessions. There was a significant improvement in physical health in patients who attended more than one month training than patients who attended less than one month training (t = 2.16, P = 0.04).
There was no significant difference between the duration of Half-cut Wood Training from less than 1 month and more than 1 month (including 1 month) in the functioning of legs and feet, doctor reported effect of Half-cut Wood Training, physical health, self-esteem, self-efficacy and mental health. In relation to the functioning of legs and feet, doctor reported effect of Half-cut Wood Training, physical health, self-esteem, self-efficacy and mental health, there were no significant differences between the BMI less than 18.5 and BMI more than 18.5. Regarding the number of treatment sessions, the functioning of legs and feet, physical health, self-esteem, self-efficacy and mental health were not significantly different between less than 20 and equal to or greater than 20 sessions.
Previous studies have shown that knee instability is a major cause of anterior cruciate ligament injury or knee osteoarthritis [1]. These problems were treated through surgery [10,21], and the results reported were primarily restricted to physical health domains and ignored the mental health of patients. In contrast to this type of traditional treatment, the present study utilized a Half-cut Wood Training natural therapy approach and found it effectively reduces symptoms of knee instability, without the need for surgery. In addition, it not only improves the stability of knees, but also self-esteem, self-efficacy, physical health, and leg and feet functioning.
The reduced symptoms of knee instability, improved physical health of quality of life, and foot and leg functioning suggests Half-cut Wood Training method is an effective intervention to improve physical health. Other studies have found knee instability was associated with activity limitation, the knee stability improvement through Half-cut Wood Training rehabilitation has enhanced daily activities level [22]. The effectiveness of Half-cut Wood Training therapy in stimulating and strengthening ankle, foot and hip mobility, as well as quadricep muscles, may be explained by the principle of Closed Kinetic Chain and Open Kinetic Chain approaches [23]. Steindler and colleagues proposed the kinetic chain as “a combination of several successively arranged joints constituting a complex motor unit.” and “The lower extremity of bone components, such as the foot, lower leg, thigh, and pelvis, can be viewed as a rigid link, with the subtalar, ankle, knee, and hip joints acting as the connecting joints” [24]. When a patient has an abnormal gait, ankle, knee, hip, and quadricep muscles could not undergo eccentric contraction resulting in knee flexion instability or “knee buckling,” and therefore the rate and amount of knee flexion could not be controlled. These results are in agreement with other studies in anterior cruciate ligament (ACL) injury or reconstruction that combined exercise methods produced a better outcomes on knee laxity, knee pain, and function; greater quadriceps torque return and a quicker return to sport than Close Kinetic Chain exercise [25], thereby enhanced daily activity level.
The effects of Half-cut Wood Training exercise may be further explained by frequency of training sessions more than 20 times, increasing and improving level of bone and muscle density through the exercise. Patients with knee instability had weakness of muscle and bone density. The mechanism of the effect of Half-cut Wood Training rehabilitation method can be Half-cut Wood Training has significantly increased the muscle and bone strength while fat and protein remained from pre-intervention to post intervention time. Previous studies support the close relationship between muscle and bone density and strength both in children and in adults (R2 = 0.6–0.95) [26], and that exercise strengthens muscle strength [27]. Cross-sectional, retrospective, and prospective observational studies involving elite and amateur athletes have also confirmed the role of exercise in increasing of bone mass and developing optimal bone architecture and bone strength [22].
The significant effect of Half-cut Wood Training rehabilitation on improvement of self-esteem and self-efficacy of the patients in our study is consistent with other studies that exercise that combination of closed kinetic chain exercises and open kinetic chain exercises are beneficial to self-esteem and self-efficacy [28]. This is also is consistent with a cohort study that physical activity status was negatively associated with a risk of subsequent affective disorders [29]. It is possible that physical activity is related to reduced oxidative and inflammatory pathways [30] and increased immunity and metabolism levels [31], which have been associated with self-esteem and self-efficacy. The improvement in self-efficacy in the intervention group is consistent with previous studies that physical activity can promote coping with stress and self-efficacy [31]. The improvement in self-esteem and self-efficacy in response to exercise may be in turn also associated with the improved physical health, and leg and feet functioning.
Many previous studies were conducted in patients with anterior cruciate ligament injury or reconstruction and had limited number of participants. Our study is the first of its type to examine patients with knee instability before they had anterior cruciate ligament injury and. Our findings contribute to the literature in showing that combined Closed Kinetic Chain and Open Kinetic Chain exercises are beneficial in improving joint function in ankles, knees and hips, thereby improved the knee functioning and stability but also self-esteem and self-efficacy which are closely linked to mental health status.
This study has a number of limitations. First, the study sample was small so error may have arisen due to the small sample size. However, we endeavored to match intervention and control group participants on severity of knee instability symptoms to minimize confounding effect of the severity of symptoms. The study had imbalanced match in age and education due to the matching variable was based on knee instability symptoms, thus our findings need to be treated with caution. Future studies using randomized controlled trials with large representative samples are needed to confirm the study results and mitigate the effects of age and education background. The study was limited to people in China. Future study will be designed to evaluate its effectiveness in other countries.
The present study has significant clinical significance and implication in prevention of anterior cruciate ligament injury and ligament tear when patients were at early knee instability stage. This may lead to significant reduction of the prevalence of anterior cruciate ligament injury and ligament tear and improve knee functioning in people with early stage of knee instability.
In conclusion, our findings suggest that Half-cut Wood Training is beneficial to reduce the symptoms of knee instability and improve knee functioning. It also improved self-esteem and self-efficacy of people who had symptoms of knee instability. Even though the sample size is small for this study, interventions using Half-cut Wood Training method to improve both knee instability and mental health in people with knee instability may represent an opportunity to provide life-long health outcome and healthy life style.
Acknowledgement: We thank Fang Li’s support during the data collection process.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Alkjaer, T., Simonsen, E. B., Jørgensen, U., Dyhre-Poulsen, P. (2003). Evaluation of the walking pattern in two types of patients with anterior cruciate ligament deficiency: Copers and non-copers. European Journal of Applied Physiology, 89(3), 301–308. [Google Scholar]
2. di Vico, G., di Donato, S. L., Balato, G., Correra, G., D’Addona, A. (2017). Correlation between time from injury to surgery and the prevalence of ramp and hidden lesions during anterior cruciate ligament reconstruction. A new diagnostic algorithm. Muscles, Ligaments and Tendons Journal, 7(3), 491–497. [Google Scholar]
3. Bollen, S. R. (2010). Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament. Journal of Bone and Joint Surgery, 92(2), 222–223. [Google Scholar]
4. Felson, D. T., Niu, J., McClennan, C., Sack, B., Aliabadi, P. et al. (2007). Knee buckling: Prevalence, risk factors, and associated limitations in function. Annals of Internal Medicine, 147(8), 534–540. [Google Scholar]
5. Knoop, J., Leeden, M., Esch, M., Thorstensson, C. A., Gerritsen, M. et al. (2012). Association of lower muscle strength with self-reported knee instability in osteoarthritis of the knee: Results from the Amsterdam osteoarthritis cohort. Arthritis Care & Research, 64(1), 38–45. [Google Scholar]
6. Farrokhi, S., O’Connell, M., Gil, A. B., Sparto, P. J., Fitzgerald, G. K. (2015). Altered gait characteristics in individuals with knee osteoarthritis and self-reported knee instability. Journal of Orthopaedic & Sports Physical Therapy, 45(5), 351–359. [Google Scholar]
7. Gustafson, J. A., Robinson, M. E., Fitzgerald, G. K., Tashman, S., Farrokhi, S. (2015). Knee motion variability in patients with knee osteoarthritis: The effect of self-reported instability. Clinical Biomechanics, 30(5), 475–480. [Google Scholar]
8. Gray Cook, G. (2010). Movement: Functional movement systems: screening, assessment, and corrective strategies. Corrective strategies, pp. 73–106. USA: On Target Publications. [Google Scholar]
9. Steindler, A. (1940). Orthopedic operations, indications, technique and end results. American Journal of the Medical Sciences, 199(6), 860. [Google Scholar]
10. Badhe, N. P., Forster, I. W. (2002). High tibial osteotomy in knee instability: The rationale of treatment and early results. Knee Surgery, Sports Traumatology, Arthroscopy, 10(1), 38–43. [Google Scholar]
11. Luttjeboer, J. S., Bénard, M. R., Defoort, K. C., van Hellemondt, G. G.,Wymenga, A. B. (2016). Revision total knee arthroplasty for instability—Outcome for different types of instability and implants. Journal of Arthroplasty, 31(12), 2672–2676. [Google Scholar]
12. Wilson, C. J., Theodoulou, A., Damarell, R. A., Krishnan, J. (2017). Knee instability as the primary cause of failure following Total Knee Arthroplasty (TKAA systematic review on the patient, surgical and implant characteristics of revised TKA patients. Knee, 24(6), 1271–1281. [Google Scholar]
13. McGuine, T. A., Winterstein, A., Carr, K., Hetzel, S., Scott, J. (2012). Changes in self-reported knee function and health-related quality of life after knee injury in female athletes. Clinical Journal of Sport Medicine, 22(4), 334–340. [Google Scholar]
14. Appelqvist-Schmidlechner, K., Vaara, J., Makinen, J., Vasankari, T., Kyrolainen, H. (2017). Relationships between leisure time physical activity, physical fitness and mental health among young adult males. 25th European Congress of Psychiatry/European Psychiatry. Paris: Elsevier France-Editions Scientifiques Medicales Elsevier. [Google Scholar]
15. Sun, J., Buys, N. (2016). Effects of community singing program on mental health outcomes of Australian aboriginal and Torres Strait islander people: A meditative approach. American Journal of Health Promotion, 30(4), 259–263. [Google Scholar]
16. Crossman, J. (2001). Coping with sports injuries: Psychological strategies for rehabilitation. Oxford, New York: Oxford University Press. [Google Scholar]
17. Nasreddine, A. Y., Connell, P. L., Kalish, L. A., Nelson, S., Iversen, M. D. et al. (2017). The pediatric international knee documentation committee (Pedi-IKDC) subjective knee evaluation form: Normative data. American Journal of Sports Medicine, 45(3), 527–534. [Google Scholar]
18. Guangdong Lexin Medical Electronics Co. L. (2016). Body fat measuring instrument. https://usermanual.wiki/Transtek-Medical-Electronics/LS208-B07/pdf. [Google Scholar]
19. Thomeé, P., Währborg, P., Börjesson, M., Thomeé, R., Eriksson, B. I. et al. (2006). A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scandinavian Journal of Medicine & Science in Sports, 16(3), 181–187. DOI 10.1111/j.1600-0838.2005.00472.x. [Google Scholar] [CrossRef]
20. Ware, J. E., Kosinski, M., Keller, S. D. (1996). A 12-item short form health survey. Medical Care, 3(34), 220–233. [Google Scholar]
21. Cudejko, T., van der Esch, M.,van der Leeden, M.,van den Noort, J. C.,Roorda, L. D. et al. (2017). The immediate effect of a soft knee brace on pain, activity limitations, self-reported knee instability, and self-reported knee confidence in patients with knee osteoarthritis. Arthritis Research & Therapy, 19, 260. [Google Scholar]
22. Nilsson, M., Ohlsson, C., Mellström, D., Lorentzon, M. (2009). Previous sport activity during childhood and adolescence is associated with increased cortical bone size in young adult men. Journal of Bone and Mineral Research, 24(1), 125–133. [Google Scholar]
23. Lehman, J. F. (1992). Ankle foot orthoses for paresis and paralysis. Physical Medicine and Rehabilitation Clinics of North America, 3, 139–159. [Google Scholar]
24. Lefever, S. (2005). Closed kinetic chain training. In: Hall, C. M., Brody, L. T. (eds.Therapeutic exercise: Moving towards function, pp. 283. Philadelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
25. Glass, R., Waddell, J., Hoogenboom, B. (2010). The effects of open versus closed kinetic chain exercises on patients with ACL deficient or reconstructed knees: A systematic review. North American Journal of Sports Physical Therapy, 5(2), 74–84. [Google Scholar]
26. Ferrucci, L., Russo, C. R., Lauretani, F., Bandinelli, S., Guralnik, J. M. (2002). A role for sarcopenia in late-life osteoporosis. Aging Clinical and Experimental Research, 14(1), 1–4. [Google Scholar]
27. Burd, N. A., Tang, J. E., Moore, D. R., Phillips, S. M. (2009). Exercise training and protein metabolism: Influences of contraction, protein intake, and sex-based differences. Journal of Applied Physiology, 106(5), 1692–1701. [Google Scholar]
28. Elavsky, S., McAuley, E. (2007). Physical activity and mental health outcomes during menopause: A randomized controlled trial. Annals of Behavioral Medicine, 33(2), 132–142. [Google Scholar]
29. Suetani, S., Mamun, A., Williams, G. M., Najman, J. M., McGrath, J. J. et al. (2017). Longitudinal association between physical activity engagement during adolescence and mental health outcomes in young adults: A 21-year birth cohort study. Journal of Psychiatry Research, 94, 116–123. [Google Scholar]
30. Moylan, S., Eyre, H. A., Maes, M., Baune, B. T., Jacka, F. N. et al. (2013). Exercising the worry away: How inflammation, oxidative and nitrogen stress mediates the beneficial effect of physical activity on anxiety disorder symptoms and behaviours. Neuroscience Biobehavior Review, 37(4), 573–584. [Google Scholar]
31. Sun, J., Buys, N., Jayasinghe, R. (2014). Effects of community-based meditative Tai Chi programme on improving quality of life, physical and mental health in chronic heart-failure participants. Aging Mental Health, 18(3), 289–295. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |