
 | International Journal of Mental Health Promotion |  |
DOI: 10.32604/IJMHP.2021.013093
ARTICLE
Emotional and Behavioral Problems of Left-Behind Children in Impoverished Rural China: A Comparative Cross-Sectional Study of First Grade Junior High School
1Beijing Anding Hospital, Capital Medical University, The National Clinical Research Center for Mental Disorders, Beijing Key Laboratory of Mental Disorders, Beijing Institute for Brain Disorders, Beijing, 100088, China
2United Nations Children’s Fund (UNICEF China Office), Beijing, 100600, China
3School of Medicine, Griffith University, Queensland, 4222, Australia
*Corresponding Authors: Jing Sun. Email: j.sun@griffith.edu.au; Yi Zheng. Email: yizheng@ccmu.edu.cn
Received: 23 July 2020; Accepted: 17 August 2020
Abstract: Objective: To investigate the prevalence of emotional and behavioral problems and related factors of left-behind children in impoverished rural China (mainly in the first grade of junior high school). Methods: A cross-sectional survey of rural households in 27 poverty-stricken counties in 12 provinces across China was conducted using the Strengths and Difficulties Questionnaire (SDQ). Results: The prevalence of emotional and behavioral problems in left-behind children was 11.7%, and that of non-left-behind children was 8.9%. There was statistical difference between the two groups (P < 0.01). There are no differences between the two groups in terms of the various factors of SDQ. The incidence of insomnia in the left-behind group was 58.3%, which was higher than that in the non-left-behind group 50.9% (P < 0.01); loneliness (62.1% vs. 51.8%, P < 0.01); running away from home (23.1% vs. 18.8%, P < 0.01), and self-injury behavior (16.8% vs. 12.2%, P < 0.01). Left-behind children are more likely to have negative psychological feelings including insomnia, loneliness, self-injury, and run away from home. They also experienced more bullying including maliciously teased by peers, intentionally excluded or isolated, physically threatened or intimidated. All of these factors are associated with their abnormal emotional and behavioural development. Conclusion: The incidence of emotional and behavioral problems of left-behind children in rural areas in poverty-stricken areas is significantly higher than that of non-left-behind children; Logistic regression analysis showed that bullying behavior and abnormal psychological characteristics are significantly associated with left-behind adolescents abnormal emotional and behavioral development.
Keywords: Rural areas; left-behind children; emotional and behavioral problems; incidence; related factors
Left-behind children (LBC) refer to children below 16 years old living in rural areas whose parents go out to work, or where one of the parents does not have the guardianship and cannot live together with their children for more than 12 months. According to the definition of rural LBC issued by the Chinese government in 2016 [1], there are a total of 9.02 million rural left-behind children. Most of these children are cared for by grandparents or other relatives and living in remote, impoverished, and rural areas. A number of previous studies have found that compared with non-left-behind children (NLBC), the long-term lack of parental care has a long lasting adverse effect on their mental health outcome in LBC children [1], such as low self esteem [2], strong sense of loneliness [3], and high social anxiety level [4].
The emotional and behavioral problems in adolescents have frequently been identified as critical risk factors of mental health outcome in their later life [5]. In the SDQ questionnaires answered by the adolescents themselves, 28.4% of adolescents have emotional and behavior problems [5]. These problems have a negative impact on family life, friendship, learning, and entertainment activities, and place a heavy economic and social burden on families and communities [6]. A Chinese study showed the factors that increase the risk of emotional and behavioral problems include poor family relationships, negative life events, learning stress, and living in poor rural areas. Another survey from Indonesia demonstrated that poor socioeconomic conditions and family environment increase the risk of emotional behavioral problems [5].
Social-ecological resilience framework emphasizes that the healthy emotional and behavioral development are the outcomes of the interaction among proximal and distal support systems including caregivers, families, peers, community and broad environment. At proximal level, the care and sense of safety that caregivers have provided to children has provided children a proximal level, secure and positive feeling about themselves, others and environment [7,8]. Lack of primary caregivers’ care often leads to insure attachment patterns, emotional distress, and behavioral problems and the LBC were more lonely than non-LBC [9,10]. They were also more likely to be unhappy and reluctant to share their emotions with other people compared to non-LBC. Studies have found that the absence of migrant parents had caused the adolescents to be more likely to have psychological problems, and the LBC are prone to have psychopathology and less prosocial behavior [9,10].
An socio-ecological resilience framework emphasizes the importance of context including social factors, environmental and child’s psychological factors, suggest that the emotional and behavioural development in children interacts with the social and surrounding environmental factors [10]. As not all LBC children have emotional and behavioural problems, LBC children who have normal emotional and behavioural development may have strong support from family members, peers, community and their positive psychological traits.
Most of the selected children in these previous studies were concentrated in only one city or in several cities in one province, such as Chongqing, Hunan, Sichuan and other places [11]. In addition, the standards and the results of previous research on depression, anxiety, or personality traits of the LBC were inconsistent [12,13]. To fill in the research gaps, the proposed study aimed to conduct a national study using an international standardized measure to explore the emotional and behavioral problems and related risks factors for the LBC using resilience framework.
This study aimed to investigate the areas with the majority of LBC in China to understand the prevalence of emotional and behavioral problems amongst LBC and to explore variables that could predict the occurrence of emotional and behavioral problems for LBC. We analyzed various influencing factors affecting emotional and behavioral problems, such as parenting factors, family factors, peers and school community. We hypothesized that the prevalence of emotional and behavioral problems of LBC are higher than those of Non-LBC because of the unstable parenting, poor family, peer and school environment, and negative psychological characteristics.
The study used a cross-sectional research design and was conducted from November 2016 to January 2017. The purposive sampling methodology was used to recruit counties which were at poverty-stricken level. Poverty-stricken county is defined as a county with more 2 percent of its population living below the poverty line, defined with a per capita annual income of 2,300 Chinese Yuan (http://www.xinhuanet.com/english/2018-10/17/c_137538566.htm). There were 27 poverty-stricken counties in rural areas in 12 provinces across China met the inclusion criteria and were included. In each county, LBC and NLBC children aged 12–15 years were recruited. In this study, LBC were defined as [7]: children 12–15 years old who were registered in rural areas with both parents away for work or one parent away for work while the other does not have the ability to look after the children for more than half a year. NLBC refer to children who were 12–15 years old with local rural household registration.
Sample size calculation formula N = (D_deff × Z^2 P(1 − P))/d^2 was used to calculate the sample size. In this formula, the confidence level for each parameter was 95% with a Z value of = 1.96. Probability P demonstrated the low incidence of psychological problems with an incidence rate for LBC over 15.0%, and the design effect Ddeff was 3 with a relative error of 15%, thus d = 15%*15.0%. Given these calculations, the corresponding sample size needed of the survey group was estimated to be about 2,900. There were no less than 200 people in each province. The ratio of the experimental group to the control group was 2:1. As the sample we had for this study was 5026, the size of the sample is adequate for the data analysis for this study.
Quota sampling method was used to recruit participants to ensure representation of the population using post-weighting adjustment. The survey sample was distributed among each project county. The quotas were adjusted separately for the grade one of junior high school students for each county based on the following information: the total number of children and their age, the total number of left-behind children (LBC), and the corresponding ratio of male to female in each country for each province. The survey was conducted in a few selected townships so children lived far from the center of the county can participate in the nearby towns. Surveys were collected from NLBC children at the same locations where the LBC were surveyed.
This study was part of the epidemiological survey on mental health status among children and adolescents in China. The study was approved by the Ethics Committee of Beijing Anding Hospital affiliated with Capital Medical University with ethical approval number of 2013 (06). The survey was also approved by the local health administration bureaus and approved by the participating schools. The participants had a choice to participate in the survey and signed an informed consent form. During the research process, trained local health workers identified students who met the inclusion criteria at the schools and briefed teachers in the selected classes. After the class teachers described questionnaires to the class and schools, students were asked to complete the questionnaires.
2.4.1 Outcome Measures: Strength and Difficulties Questionnaire
Strength and difficulty questionnaire is reliable and valid instrument in assessing emotional and behavioural problems in Chinese children and adolescents [14]. It was selected to assess adolescents’ emotional and behavioral problems for this study. SDQ has total 25 items with three responses: “not true”, “somewhat true” and “certainly true”, with 0, 1, and 2 points attributed to each response, respectively. Reverse scoring for items 7, 11, 14, 21 and 25 was conducted. SDQ consists of five subscales: (1) Emotional symptoms; (2) Conduct problem; (3) Hyperactivity-inattention; (4) Peer problems; and (5) Prosocial behavior. The total difficulty score obtained by adding the items related to the subscale 1 to 4 comprises the total difficulties score. The higher the obtained total difficulties score, the more severe the psychological behavioral problems of the child. The higher the score from the subscale 5 of prosocial behavioral questions, the better the interpersonal ability of the child. Using Chinese standard score, we defined a SDQ total difficulties score of over 17 as abnormal psychological behavior, and a SDQ prosocial behavior score below five points as abnormal.
2.4.2 Risk Factors of Emotional and Behavioral Problems
Information in risk factors including school and community environment and adolescents psychological feelings was collected and these questions are below.
Parenting questions: Information related to parent-child communication was collected. This included how often and for how long did the parents communicate with their child through various means, including videos, phone calls, and letters. Whether parents/guardian scolded child was asked.
School environment: Information related to school environment including feeling safe in the school, physical fighting with someone (one or more) in the past 12 months; poor school experience including been maliciously teased; been asked for property; being intentionally excluded or isolated; be threatened, intimidated; be hit, kicked, pushed, squeezed, or locked in; being teased for a child’s physical defect or appearance, was collected. The responses are from no to often. The total poor school experience score was derived by adding these six items together. The higher the score, the poorer the school experience that adolescent had.
Psychological characteristics of adolescents: Questions related to adolescent’s psychological feelings were collected. These questions are related to: (1) Unhappy because of stress or academic problems; (2) Been having insomnia due to fear of something; (3) Ever felt lonely in the past 6 months; (4) Have considered leaving home in the past 6 months; (5) Have intentionally hurt yourself (such as burn with a cigarette butt, cut with a blade, hit a wall with your head). In addition, if an adolescent answered the question relating to difficulty questions, their psychological feeling of botherness to themselves and others due to difficulties are asked whether they felt their difficulties bothered: Family life, relationship with friends, study in class, extracurricular leisure activities, a burden for others around you (family, friends, teachers). The total score for feelings of botherness was obtained by adding these five questions together.
Demographic characteristics: Demographic information was collected. This included nationality, whether attend school, who is adolescent’s primary guardian (the person who looks after your life), education of main guardian, length being primary guardian age, parent’s custody ability, father’s education, mother education, number of sibling the adolescent is living with more than six month, whether family had Family car, washing machine, computer (Internet access), motorcycle and refrigerator.
Chi square test was used to compare the differences in characteristics of adolescents with abnormal emotional and behavior and normal adolescents in whether parents went out to work, who is the guardians, guardians age and education, length of parents going out to work, adolescents age, gender, ethnicity, and family economic status.
If there are any differences between abnormal and normal adolescents in any of these demographic variables, these variables were included in the subsequent multivariate analysis.
Multilevel and multivariate regression analysis was used to assess the association among parenting, school environment and adolescent psychological characteristics with the emotional and behavioral problems. MLwin statistical package version 2.4 was used to analyse the associations between risk factors and the emotional and behavioural problems. Two level of data was used to evaluate the impact of province level and individual level impact on the total variance explained for the association between risk factors and emotional and behavioral problems. Statistical analysis significant level was adjusted to be P value less than 0.01 due to multiple risk factors in the analysis.
Among 4952 adolescents, 3316 (67.0%) were left-behind adolescents and 1636 (33.0%) were non-left-behind adolescents. There were no significant differences between left-behind and non-left-behind adolescents in gender, education, mother and father’s education and nationalities. However, more left-behind adolescents (20.3%) had abnormal difficulties score compared with non- left-behind adolescents (16.8%) (See Tab. 1). As majority of the participants in this study were left-behind adolescents, the subsequent results focused on left-behind adolescents’ results in details.
Table 1: Risk factors related to psychological behavior abnormalities in the left-behind children group (n = 3316) (n, %)
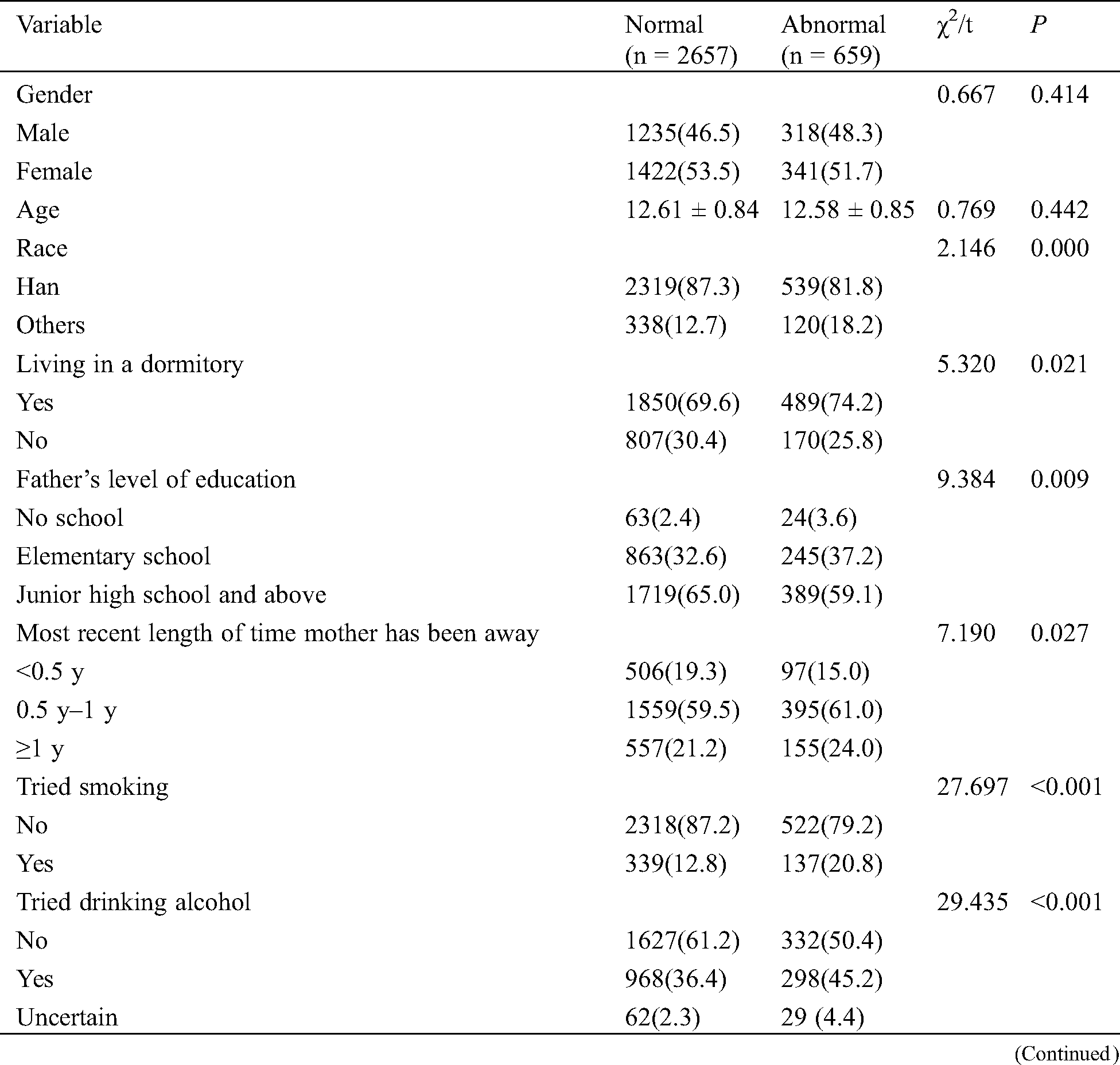
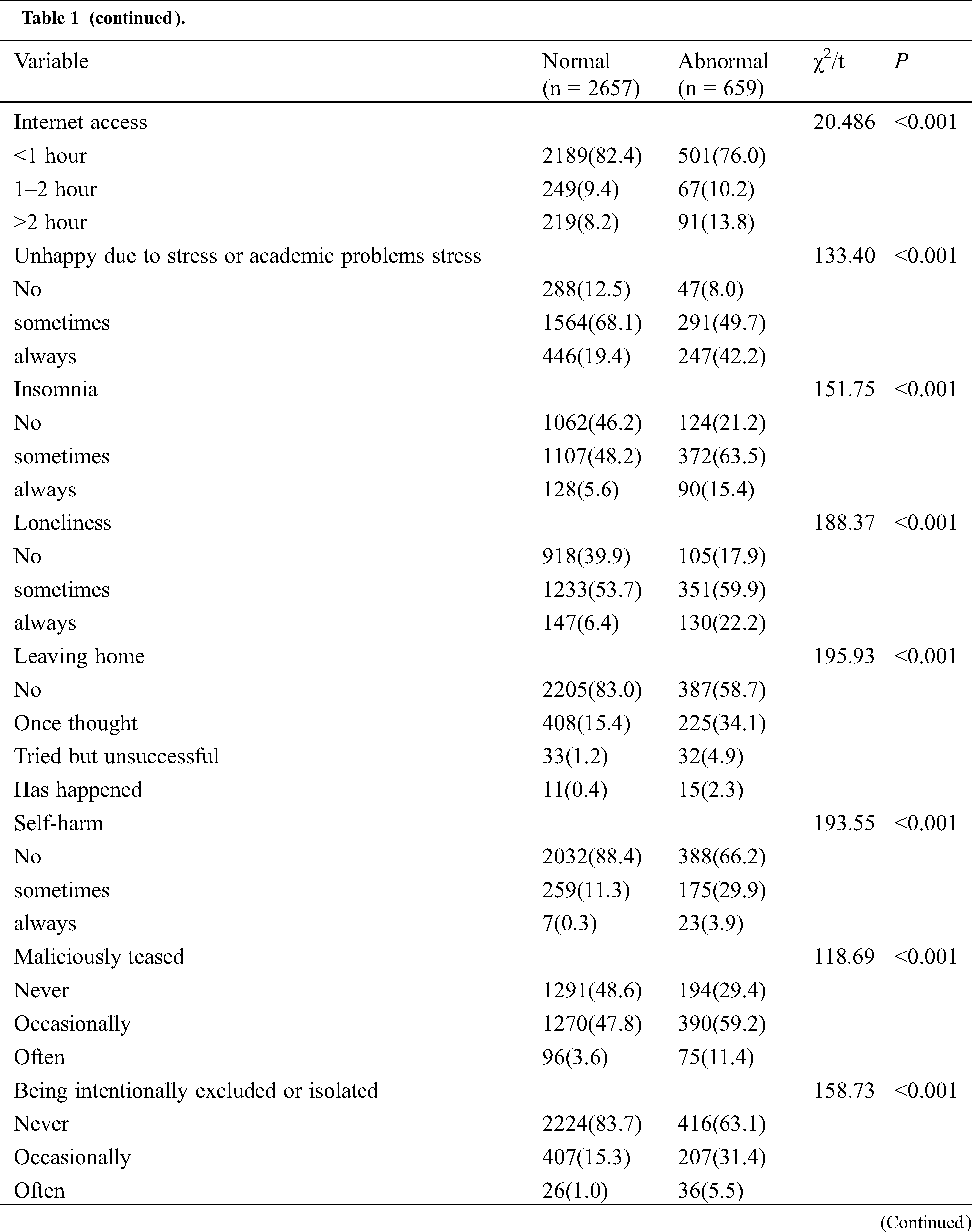
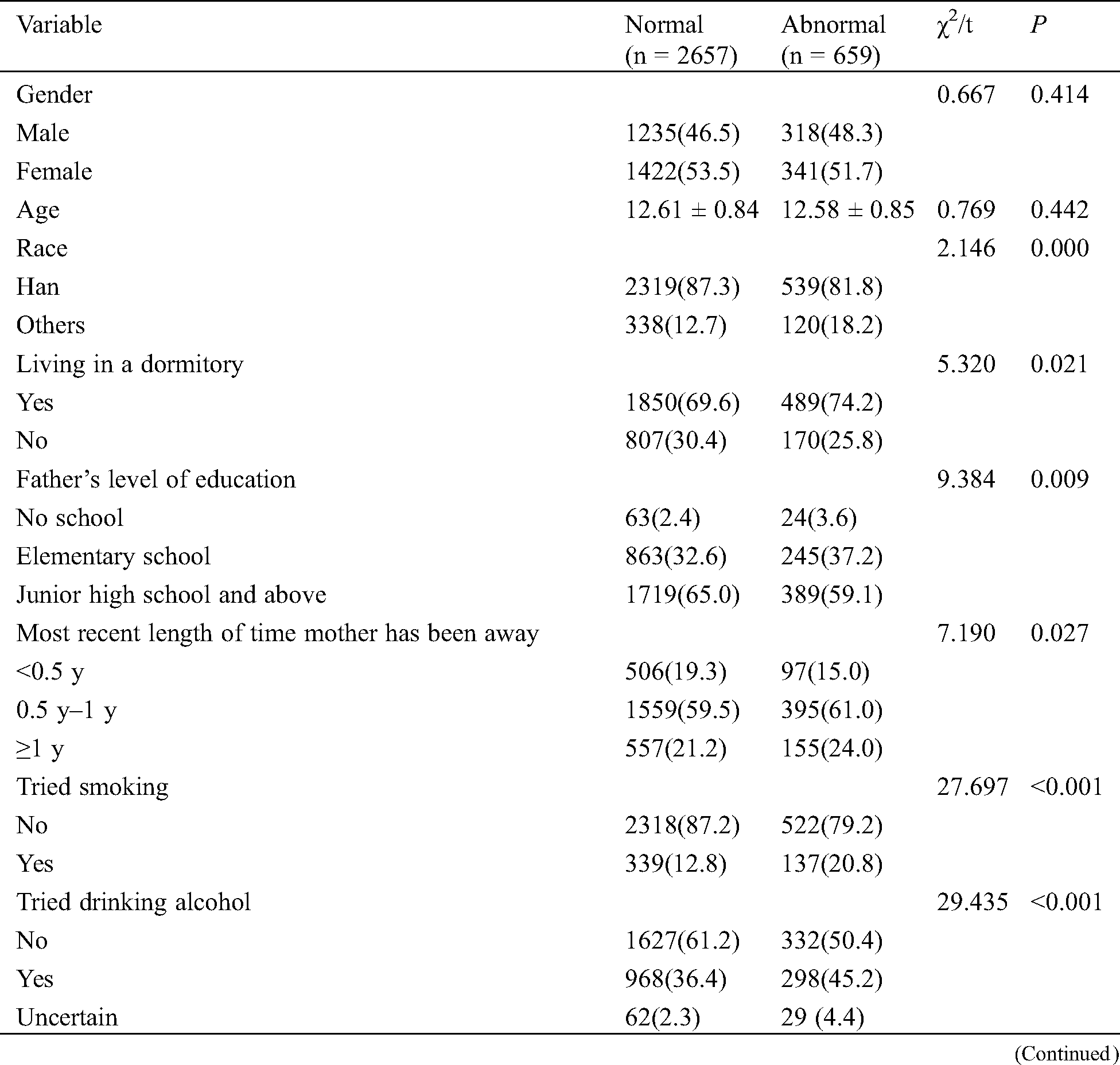
As shown in Tab. 1 in the comparison between normal and abnormal group of left-behind adolescents, more adolescents had minority nationality background with abnormal emotional and behavoural problems compared with adolescent with normal emotional and behavioural development. More adolescent with emotional and behavioural problems lived in a dormitory, had father’s education less than junior high school, and had more than half year having not seen their mothers. At behavior level, more left-behind adolescent with the abnormal emotional and behavioural problems had smoking, drinking and internet access more than 1 hours per day compared to left-behind adolescents with normal emotional and behavioural scores. In their psychological characteristics, more left-behind adolescents with emotional and behavioural problems felt unhappy and loneliness, had insomnia and and feelings of wanting to leave home, and had self harm behavior compared to left-behind adolescents with normal emotional and behavioural status. In the school environment factors, more left-behind adolescents with emotional and behavioural problems had experience of trouble with friend, maliciously teased, being intentionally excluded, being threatened and joking, or being teased for physical appearance than left-behind adolescents with normal emotion and behavior.
As there were significant differences between left-behind adolescents with normal and abnormal emotion and behavior groups in student behavior, psychological characteristics and school ethos and psychological environment, these factors were included in the subsequent logistic regression model (see Tab. 2).
Table 2: Left-behind group and control group, SDQ total score and each factor score, chi-square test results

As it is shown in Tab. 2, left-behind adolescents are statistically different from non-left-behind adolescents in Total difficulty scores, hyperactivity-inattention, and peer problems.
The multiple logistic regression model shows school environment related questions including “Maliciously teased even at occasionally level”, “being intentionally excluded or isolated”, “joking with a child” are significantly associated with abnormal emotional and behavioural problems (Tab. 3). The results of this study found left-behind adolescents who had emotional and behavior problems had higher proportion of self harm behavior (33.8%), unhappiness (91.9), insomnia (78.9), and lonliness (82.1%), and leaving home (2.3%) compared with left-behind adolescents who did not have emotional and behavioural problems in self harm (11.6%), unhappiness (87.5%), insomnia (53.8%), loneliness (60.6%), and leaving home (0.4%). Psychological characteristics including “Insomnia due to fear of something”, “Felt lonely in the past 6 months”, “Considered leaving home in the past 6 months”, “Having intentionally hurt yourself” are all significantly associated with abnormal emotional and behavioral problems. There are no significant association between parenting factors and abnormal emotional and behavioural problems in left-behind adolescents.
Table 3: Risk factors associated with psychological behavioral abnormalities in the left-behind group

Findings in our study indicate school environment and adolescent’s psychological characteristics are associated with their emotional and behavioual development. In particular, negative school environment and psychological characteristics are associated with their abnormal emotional and behavior. Our results support the socio-ecological resilience framework that the emotional and behavioural development in adolescents interact with school environment and adolescents’ psychological characteristics in left-behind adolescents [10].
Left-behind adolescents who have abnormal emotional and behavioural development had less school and peers, community support and developed poorer psychological feelings than non-left-behind adolescent who had normal emotional and behavioural development. Bullying behviours including maliciously teased by peers, intentioinally excluded or isolated, physically threatened or intimidated are associated with young people’s emotional and behavioural problem in our study. Our result supports the finding form the previous study that the chronic maliciously teasing is harmful to young adolescents’ mental health and wellbeing [15]. Being teased about physical appearance, family background, social skills and academic grades is significantly associated with increased loneliness, depressive symptoms, anxiety and decreased participation in social activities in 10 to 14 year old children [16,17]. The findings in our study indicate being intentionally excluded or isolated in left-behind adolescents is 2.75 times more likely than not being intentionally excluded or isolated adolescents to have emotional and behavioural problem in left-behind adolescents. Our results support previous studies that there is a significant relationship between bullying and mental ill health in adolescents [18,19]. But our study extends the existing literature and found even occasionally been maliciously teased, excluded or isolated, physically threatened or intimidated are significantly associated with abnormal emotional and behavior in left-behind adolescents. This supports the previous study that social exclusion that was upsetting irrespective of frequency was associated with psychological distress in older adolescents [20], and left-behind adolescents are more likely to be upsetting due to their lack of support when parents and family members were absent.
The findings in psychological characteristics report that there are more adolescents who had abnormal emotional and behavioural problems had feelings of unhappiness (91.9%), insomnia (78.9%), loneliness (82.1%) and self harm (33.8%) comparing with left-behind adolescents with normal emotional and behaviours in unhappiness (87.5%), insomnia (53.8%), feelings of loneliness (60.1%), and self harm (11.6%) respectively. Left-behind adolescents who had insomnia had 1.42 times (P < 0.01) more likely to have abnormal emotional and behavioral problems (P < 0.01). Left-behind adolescents who felt lonely had 2.56 times (P < 0.001) more likely to have abnormal emotional and behavioural problems. Left-behind adolescents who had self harm had 1.55 (P < 0.001) times to 5.06 times (P < 0.001) more likely to have abnormal emotional and behavioural problems. Our results support previous studies that adolescents who have experienced loneliness had sense of abandonment, which may discourage them to discover their sense of belonging, and this is related to mental health problems [21]. Our results extend the literature that even when they sometimes experienced loneliness can be detrimental to adolescents emotional and behavioural status. It is possible left-behind adolescent had prolonged separation with their parents that they had developed the sense of abandonment, which may discourage them to discover their sense of belonging and sense of safety. Our survey results found that compared with the non-left-behind adolescent group, left-behind adolescents had more symptoms of inattention and hyperactivity (10.9% vs. 9.1%, P < 0.05), and due to lack of timely intervention, they also showed more peer relation problems (14.2% vs. 11.2%, P < 0.05). Our results also found left-behind adolescents who sometimes had insomnia, self harm, and always had self-harm are related to abnormal emotional and behavioral development. This is consistent with previous studies that self-injury is related to common mental disorders [22,23], substance abuse [22,23], and these problems were persisted into the adulthood in mid-thirties [22]. The possible reasons may be that insecure parent–child attachment is negatively related to the affect regulation ability of left-behind children [24]. Our study is the first time to show insomnia even is at infrequent level can also lead to abnormal emotional and behavioural development in left-behind adolescents. The possible reasons could be because the pressure and stress that they had from the academic grade and lack of emotional and academic support for their academic study. In addition, our research also found that due to improper parental supervision, left-behind adolescents are more likely to develop physical illnesses and cannot go to school normally. This increases the risk of emotional and behavioral problems by 1.28–2.26 times. The possible mechanism may be left-behind adolescents did not get good nutrition and physical health that they subsequently had poor mental health which is consistent with previous studies [21,25].
5 Limitations and Implications for Services
There are a number of limitations for the study. First, the study design used cross-sectional study design that it is not possible to examine the cause and effect relationship relating to the school environment, adolescent psychological characteristics relating to the emotional and behavioural outcomes. Second, the results are self-reported that the results may be subjective. Third, there are potentially other confounding factors such as community and school support factors may confound the study results and they were not assessed and examined in this study. Future study using longitudinal and representative sample is needed to examine the causal relationship between emotional and behavioural development and left-behind adolescents psychological characteristics, bullying and family support. It is necessary to include adolescents outside schools and adolescents who dropped the schooling and recruit more representative sample.
Acknowledgement: Acknowledgements and Reference heading should be left justified, bold, with the first letter capitalized but have no numbers. Text below continues as normal.
Contributor’s Statements: Yuming Zhou collected data, conducted statistical analysis, drafted the manuscript, and edited and submitted the manuscript. Email: 18612610297@163.com. Chunxia Zhao organized the program, collected data, reviewed and revised the manuscript, and approved the final manuscript as submitted. Email: czhao@unicef.org. Fan He collected data, reviewed and revised the manuscript, and approved the final manuscript as submitted. Email: hf981207@163.com. Jing Sun designed the study, conducted statistical analysis; drafted, critically reviewed, edited, and revised the manuscript; and approved the final manuscript as submitted. Email: j.sun@griffith.edu.au. Xiaobo Tian, reviewed and revised the manuscript, and approved the final manuscript as submitted. Email: xtian@unicef.org. Yi Zheng conceptualized and designed the study, collected data, and approved the final manuscript as submitted. Email: yizheng@ccmu.edu.cn.
Funding Statement: National “Twelfth Five-Year” Science and Technology Support Program (No. 2012BAI01B02); Research on prevention and control of major chronic non-communicable diseases in the Ministry of Science and Technology (No. 2016YFC1306100).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Fan, F., Su, L., Gill, M., Birmaher, B. (2009). Emotional and behavioral problems of Chinese left-behind children: A preliminary study. Social Psychiatry and Psychiatric Epidemiology, 45(6), 655–664. DOI 10.1007/s00127-009-0107-4. [Google Scholar] [CrossRef]
2. Luo, J., Wang, L. G., Gao, W. B. (2012). The influence of the absence of fathers and the timing of separation on anxiety and self-esteem of adolescents: A cross-sectional survey. Child: Care, Health and Development, 38(5), 723–731. DOI 10.1111/j.1365-2214.2011.01304.x. [Google Scholar] [CrossRef]
3. Chai, X., Du, H., Li, X., Su, S., Lin, D. (2019). What really matters for loneliness among left-behind children in rural China: a meta-analytic review. Frontiers in Psychology, 10, 774. DOI 10.3389/fpsyg.2019.00774. [Google Scholar] [CrossRef]
4. Xu, J., Ni, S., Ran, M., Zhang, C. (2017). The relationship between parenting styles and adolescents’ social anxiety in migrant families: A study in Guangdong, China. Frontiers in Psychology, 8, 626. DOI 10.3389/fpsyg.2017.00626. [Google Scholar] [CrossRef]
5. Umami, R., Turnip, S. (2019). Emotional and behavioral problems among left-behind children in Indonesia. Indian Journal of Psychological Medicine, 41(3), 240–245. DOI 10.4103/IJPSYM.IJPSYM_370_18. [Google Scholar] [CrossRef]
6. Zhang, X., Li, M., Guo, L., Zhu, Y. (2019). Mental health and its influencing factors among left-behind children in South China: a cross-sectional study. BMC Public Health, 19(1), 1725. DOI 10.1186/s12889-019-8066-5. [Google Scholar] [CrossRef]
7. Cannon, D., Sriram, K. B., Liew, A., Sun, J. (2018). Resilience factors important in health-related quality of life of subjects with COPD. Respiratory Care, 63(10), 1281–1292. DOI 10.4187/respcare.05935. [Google Scholar] [CrossRef]
8. Sun, J., Stewart, D. (2007). Development of population-based resilience measures in the primary school setting. Health Education, 107(6), 575–599. DOI 10.1108/09654280710827957. [Google Scholar] [CrossRef]
9. Fan, F., Su, L., Gill, M. K., Birmaher, B. (2010). Emotional and behavioral problems of Chinese left-behind children: A preliminary study. Social Psychiatry and Psychiatric Epidemiology, 45(6), 655–664. DOI 10.1007/s00127-009-0107-4. [Google Scholar] [CrossRef]
10. Wen, M., Lin, D. (2012). Child development in rural china: children left behind by their migrant parents and children of nonmigrant families. Child Development, 83(1), 120–136. DOI 10.1111/j.1467-8624.2011.01698.x. [Google Scholar] [CrossRef]
11. Huang, Y., Zhong, X., Li, Q., Xu, D., Zhang, X. et al. (2015). Health-related quality of life of the rural-China left-behind children or adolescents and influential factors: a cross-sectional study. Health and Quality of Life Outcomes, 13(1), 29. DOI 10.1186/s12955-015-0220-x. [Google Scholar] [CrossRef]
12. Cheng, J., Sun, Y. H. (2015). Depression and anxiety among left-behind children in China: A systematic review. Child: Care, Health and Development, 41(4), 515–523. DOI 10.1111/cch.12221. [Google Scholar] [CrossRef]
13. Wang, F., Lu, J., Lin, L., Zhou, X. (2019). Mental health and risk behaviors of children in rural China with different patterns of parental migration: a cross-sectional study. Child and Adolescent Psychiatry and Mental Health, 13(1), 39. DOI 10.1186/s13034-019-0298-8. [Google Scholar] [CrossRef]
14. Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology & Psychiatry, 38(5), 581–586. DOI 10.1111/j.1469-7610.1997.tb01545.x. [Google Scholar] [CrossRef]
15. Hayden-Wade, A., Stein, R. I., Ghaderi, A., Saelens, B. E., Zabinski, M. F. et al. (2005). Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obesity Research, 13(8), 1381–1392. DOI 10.1038/oby.2005.167. [Google Scholar] [CrossRef]
16. Jones, D. C., Newman, J. B., Bautista, S. (2005). A three-factor model of teasing: The influence of friendship, gender, and topic on expected emotional reactions to teasing during early adolescence. Social Development, 14(3), 421–439. DOI 10.1111/j.1467-9507.2005.00309.x. [Google Scholar] [CrossRef]
17. Storch, E. A., Roth, D. A., Coles, M. E., Heimberg, R. G., Bravata, E. A. et al. (2004). The measurement and impact of childhood teasing in a sample of young adults. Journal of Anxiety Disorders, 18(5), 681–694. DOI 10.1016/j.janxdis.2003.09.003. [Google Scholar] [CrossRef]
18. Cook, C. R., Williams, K. R., Guerra, N. G., Kim, T. E., Sadek, S. (2010). Predictors of bullying and victimization in childhood and adolescence: A meta-analytic investigation. School Psychology Quarterly, 25(2), 65–83. DOI 10.1037/a0020149. [Google Scholar] [CrossRef]
19. Kaltiala-Heino, R., Rimpelä, M., Rantanen, P., Rimpelä, A. (2000). Bullying at school—an indicator of adolescents at risk for mental disorders. Journal of Adolescence, 23(6), 661–674. DOI 10.1006/jado.2000.0351. [Google Scholar] [CrossRef]
20. Thomas, H. J., Chan, G. C. K., Scott, J. G., Connor, J. P., Kelly, A. B. et al. (2016). Association of different forms of bullying victimisation with adolescents’ psychological distress and reduced emotional wellbeing. Australian & New Zealand Journal of Psychiatry, 50(4), 371–379. DOI 10.1177/0004867415600076. [Google Scholar] [CrossRef]
21. Fellmeth, G., Rose-Clarke, K., Zhao, C., Busert, L. K., Zheng, Y. et al. (2018). Health impacts of parental migration on left-behind children and adolescents: a systematic review and meta-analysis. Lancet, 392(10164), 2567–2582. DOI 10.1016/S0140-6736(18)32558-3. [Google Scholar] [CrossRef]
22. Borschmann, R., Becker, D., Coffey, C., Spry, E., Moreno-Betancur, M. et al. (2017). 20-year outcomes in adolescents who self-harm: A population-based cohort study. Lancet Child & Adolescent Health, 1(3), 195–202. DOI 10.1016/S2352-4642(17)30007-X. [Google Scholar] [CrossRef]
23. Moran, P., Coffey, C., Romaniuk, H., Degenhardt, L., Borschmann, R. et al. (2015). Substance use in adulthood following adolescent self-harm: A population-based cohort study. Acta Psychiatrica Scandinavica, 131(1), 61–68. DOI 10.1111/acps.12306. [Google Scholar] [CrossRef]
24. Wang, Y., Zhang, M., Chen, H. (2019). Self-injury among left-behind adolescents in rural China: The role of parental migration and parent-child attachment. Frontiers in Psychology, 9(2672), 1–8. DOI 10.3389/fpsyg.2018.02672. [Google Scholar] [CrossRef]
25. Zhou, H., Qu, X., Yang, Y., Kc, A., Liu, X. et al. (2020). Relationship between moderate to late preterm, diet types and developmental delay in less-developed rural China. Nutritional Neuroscience, 1–10 DOI 10.1080/1028415X.2020.1712534. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |