 Open Access
Open Access
ARTICLE
Sacrocolpopexy in urology versus gynecology: a contemporary analysis of outcomes and patient profiles
1 Department of Urology, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA 19107, USA
2 Department of Urology, Ochsner Health System, New Orleans, LA 70121, USA
* Corresponding Author: Courtney E. Capella. Email:
Canadian Journal of Urology 2025, 32(1), 63-70. https://doi.org/10.32604/cju.2025.064711
Received 28 November 2024; Accepted 31 December 2024; Issue published 20 March 2025
Abstract
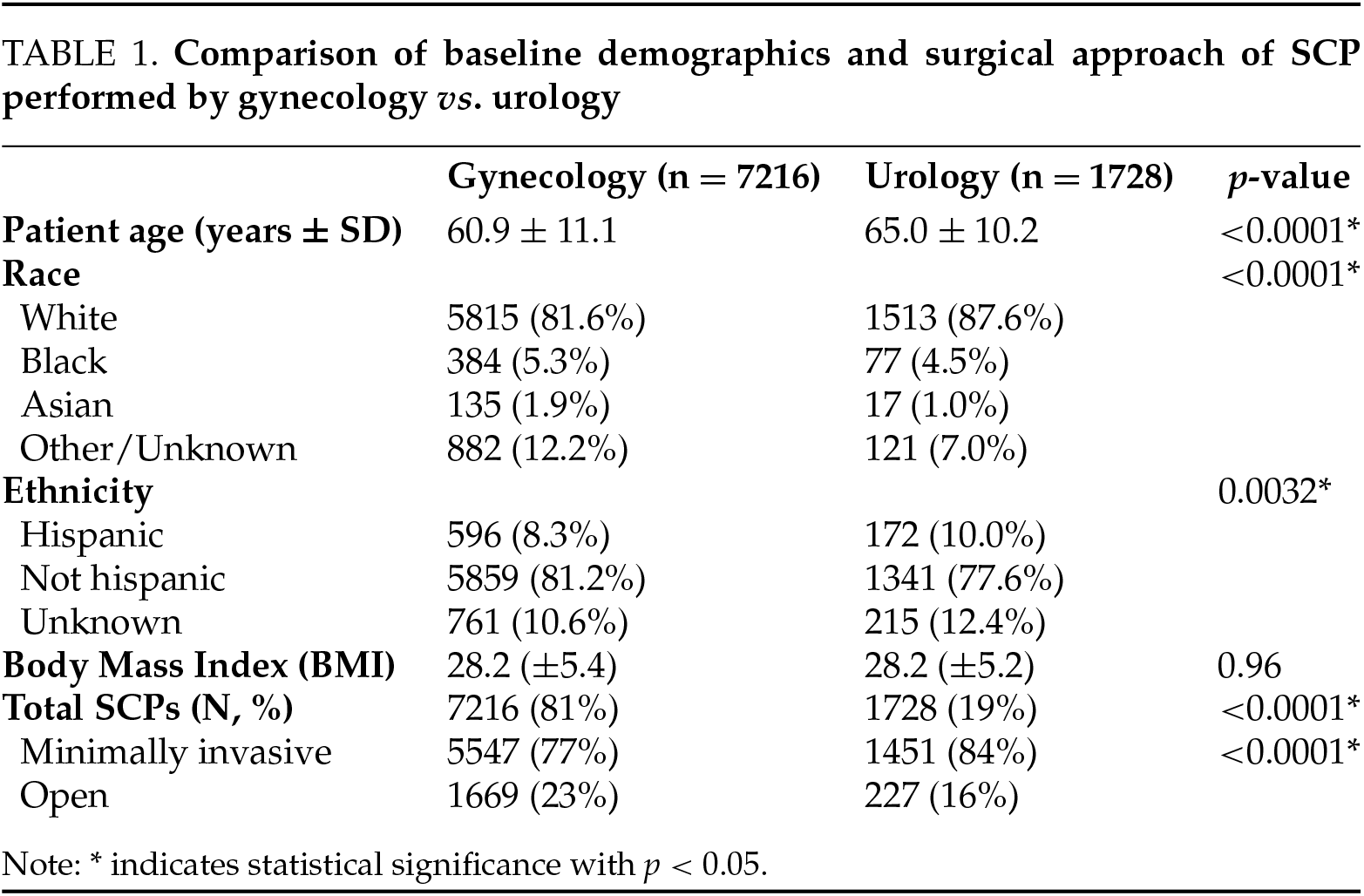
Introduction: With the aging population, more females will suffer from pelvic organ prolapse. Both urologists and gynecologists perform sacrocolpopexy, but there is no comparative study analyzing differences in provision of care, outcomes, or patient population. We aimed to elucidate potential differences in demographics, outcomes, and minimally invasive surgery utilization for SCP performed by urology and gynecology. Methods: In our retrospective analysis, sacrocolpopexies were identified using the American College of Surgeons National Surgical Quality Improvement Project database from 2006–2020. Pearson’s chi-square test was performed to test trends in the utilization of MIS in five-year blocks. Frailty was calculated using the NSQIP modified frailty index and the revised surgical Risk Analysis Index. Univariate analysis was performed using Student’s t-test and Pearson’s chi-square to compare operative parameters, frailty, demographics, and outcomes. Results: We identified 8944 sacrocolpopexies. Gynecology performed 81% of cases while urology performed the remaining 19% (p < 0.001). Between the specialties, there were no significant differences in outcomes, minor or major complications, or 30-day reoperations/hospital readmissions/mortality. However, urologists tended to care for patients who were older (65 vs. 61 years, p < 0.001) and frailer by both frailty indices (p < 0.001). Conclusion: Case distributions have remained stable, with gynecologists four-fold more sacrocolpopexies, in keeping with the larger number of practicing gynecologists vs. urologists. There was no difference in 30-day outcomes between both specialties. However, urologists operated on older, more frail patients.Keywords
Urogynecology and Reconstructive Pelvic Surgery (URPS) is a co-sponsored surgical subspeciality of urology and obstetrics and gynecology (OBGYN) that manages pelvic floor disorders, pelvic pain, urinary incontinence, overactive bladder and pelvic organ prolapse (POP). Specifically, POP occurs when there is
weakness of the pelvic floor leading to descent of the anterior, posterior, and/or apical vaginal wall. Over 1/10 women will need surgical management to treat POP or urinary incontinence.1 Given the aging population and a clinical paradigm shift with an emphasis on quality of life, it is paramount that we properly train physicians to manage this pathology.
Intervention is based on patient factors, such as staging, comorbidities, and symptom burden, as well as surgeon experience. Treatment of prolapse can be performed with a transvaginal approach using a vaginal native tissue repair or an abdominal approach with sacrocolpopexy (SCP). Though the literature is inconclusive, some studies suggest that SCP offers lower recurrence rates vs. transvaginal repair due to increased apical support.2 Therefore, open or minimally invasive surgical (MIS) SCP is considered the gold standard for apical prolapse.3
Laparoscopic approach for SCP was first introduced in the 1990s and favored due to decreased pain, length of stay, and recovery time; however, this technique is arduous due to the extensive suturing requirement. Popularization of robotic surgery further led to a growth in SCP rates.4,5 Additionally, current urology and OBGYN residents, as well as URPS fellows, receive formal robotics training, leading to increased comfort with the technology.6–8
Urologists and gynecologists are both trained in basic surgical treatment of POP. Both specialties can seek additional training through a board-certified URPS fellowship.9,10 Despite these separate pathways of training available to perform SCPs, no literature exists comparing the provision of SCPs performed by the two specialties. Herein, we aim to elucidate trends in patient demographics, surgical outcomes, and utilization of MIS between specialties performing SCP using the American College of Surgeons’ National Surgical Quality Improvement Project (NSQIP) database from 2006–2020.
Patients receiving SCP between 2006–2020 were identified using CPT codes 57425 and 57280 within the NSQIP database. Cases were sorted by primary surgeon specialty (“gynecology” or “urology”) using the “SURGSPEC” variable. Cases performed by other specialties, such as general surgery, were excluded from the analysis. Operative approach was determined using CPT codes, with 57280 referring to open and 57425 referring to MIS.
Baseline demographics were compared between the urology and gynecology cohorts. Factors compared included: age, race, ethnicity, body mass index (BMI), surgical approach, and medical comorbidities, including diabetes mellitus, smoking status, dyspnea, functional status, history of chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), hypertension, renal failure, dialysis dependence, history of disseminated cancer, chronic steroid use, significant preoperative weight loss, or history of bleeding disorder.
Frailty was calculated using the NSQIP modified frailty index (mFI-5), and the revised surgical Risk Analysis Index (RAI-rev). The mFI-5 is a previously validated measure that assigns one point for each of the following: non-independent functional status, hypertension, COPD, CHF, and diabetes.11,12 The RAI-rev is a validated measure that captures frailty through the three following domains: sex, symptom and health indicator components; age and cancer status; and cognition and functional status.13,14 For both scores, higher score indicates more frailty.
Furthermore, operative time, hospital length of stay (LOS), and rates of 30-day minor complications, major complications, readmissions, reoperations, and mortality were compared. Minor complications included urinary tract infections (UTIs), superficial surgical site infections (SSIs), pneumonia, renal insufficiency (rise in creatinine >2 mg/dL without need for dialysis), and bleeding requiring transfusion within 30 days. Major complications were defined as 30-day instances of sepsis, deep vein thrombosis (DVT), stroke, reintubation requirement, renal failure, myocardial infarction (MI), pulmonary embolism (PE), septic shock, wound dehiscence, cardiac arrest, deep would infection, organ space infection, hospital readmission, reoperation, or mortality. This aligned with previously published studies describing complications with the NSQIP database.15
Statistical analysis was performed using Student’s t-tests or Pearson’s chi square for continuous and categorical variables, respectively. All statistical tests were two-tailed, and p < 0.05 was considered significant. All statistical analyses were performed using JMP Pro 17.0 (Cary, NC, USA).
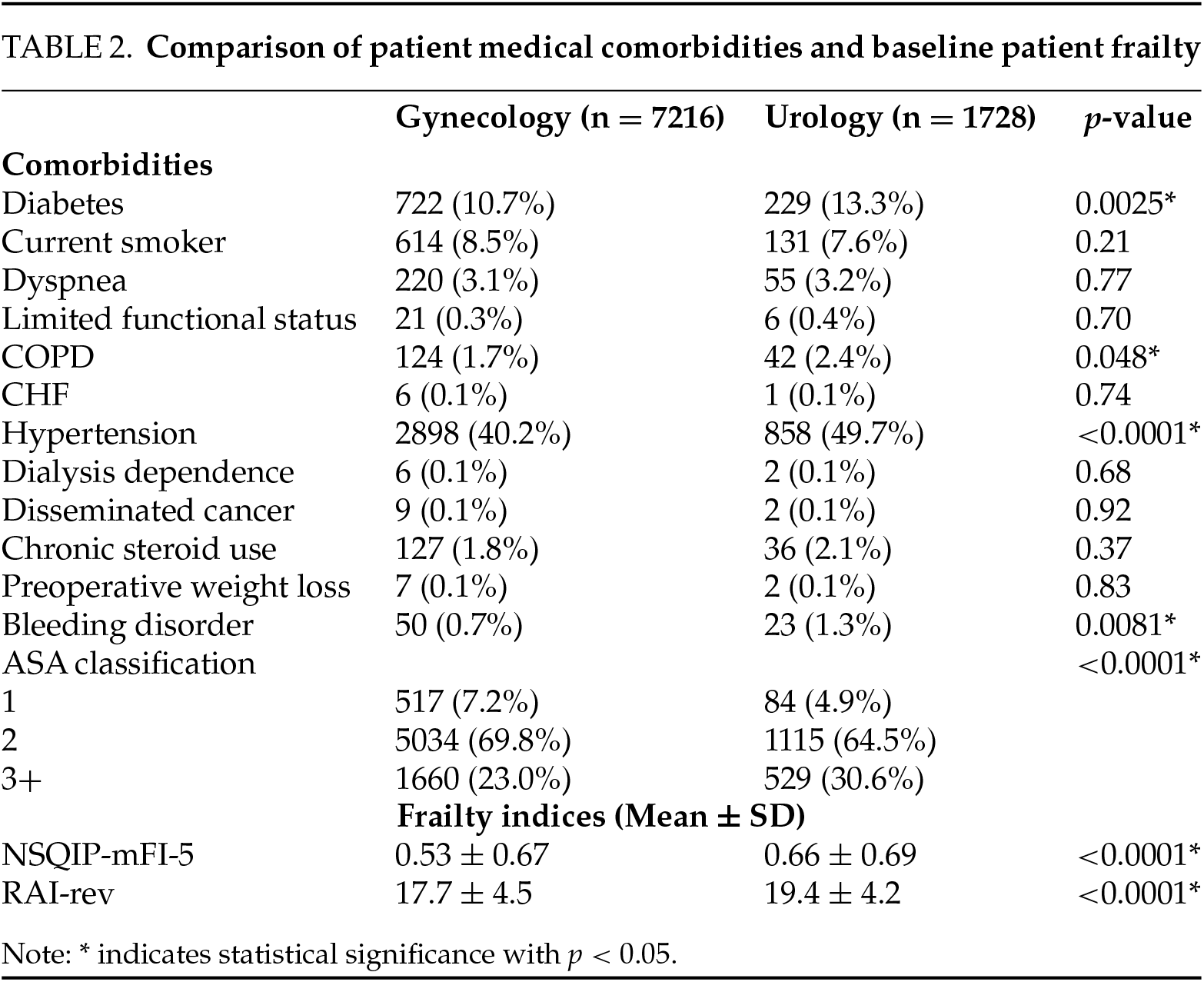
Baseline demographics, comorbidities, and patient frailty
A total of 8945 SCPs were reported to NSQIP. A comparison of baseline demographics is detailed in Table 1. Overall, patients undergoing SCP had low rates of medical comorbidities, as detailed in Table 2. However, urologists operated on older patients (65 years vs. 61 years, p < 0.001). There was no difference in baseline patient BMI, and there were minor differences in patient race and ethnicity (Table 1). Compared to gynecologists, urologists also tended to operate on patients with significantly more comorbidities, particularly diabetes (13.3% vs. 10.7%, p = 0.003), hypertension (50% vs. 40%, p < 0.0001), COPD (2.4% vs. 1.7%, p = 0.048), and bleeding disorders (1.3% vs. 0.7%, p = 0.008). Urologists also operated on patients with higher rates of ASA III or IV classifications, indicating severe systemic disease (p < 0.001) (Table 2). Compared to gynecologists, urologists operated on significantly frailer patients as measured by both mFI-5 (0.7 vs. 0.5, p < 0.001) and RAI-rev (19.4 vs. 17.7, p < 0.001).
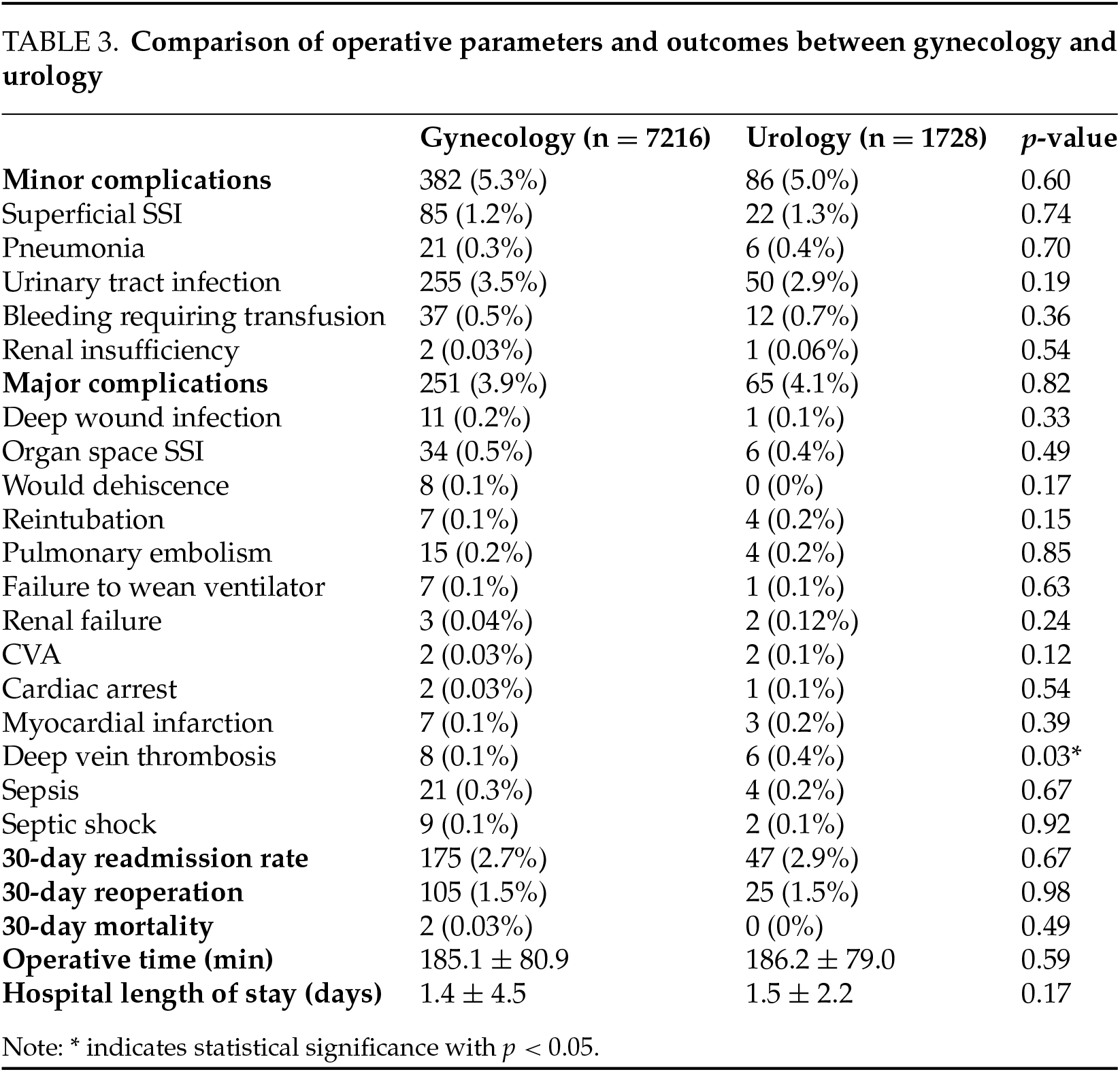
30-day outcomes and complications
A comparison of outcomes and complications between gynecologists and urologists is detailed in Table 3. Overall, the complication rate for SCP is relatively low, with a minor complication rate of 5%, a major complication rate of 4%, and nearly no 30-day mortality (Table 3). Outcomes between urologists and gynecologists were comparable. There was no difference in rates of any 30-day minor complications, major complications, readmissions, reoperations, or mortality. There was a slightly increased rate of DVTs in cases performed by urologists (0.4% vs. 0.1%, p = 0.03). There was no significant difference in operative time or hospital LOS.
Trends in specialty and operative approach performing SCP
Over the 2006–2020 period, gynecology performed 81% of SCPs (p < 0.001). With more institutions contributing data to NSQIP each year, the number of identified cases increased from 1 SCP in 2006 to 974 in 2020, peaking at 1259 in 2019. There was slow evolution in the percentage of SCPs performed by urologists vs. gynecologists, with urologists performing 17% of cases from 2006–2010, 18% of cases from 2011–2015, and 20% from 2016–2020 (p = 0.047). The complete trend over time is demonstrated in Figure 1. We identified an increase in utilization of MIS over time, with 59% of cases from 2006–2010, 70% of cases from 2011–2015, and 84% from 2016–2020 (p < 0.0001) (Figure 2). Over the study period, urologists performed significantly more MIS SCPs vs. gynecologists (84% vs. 77%, p < 0.0001) (Table 1).
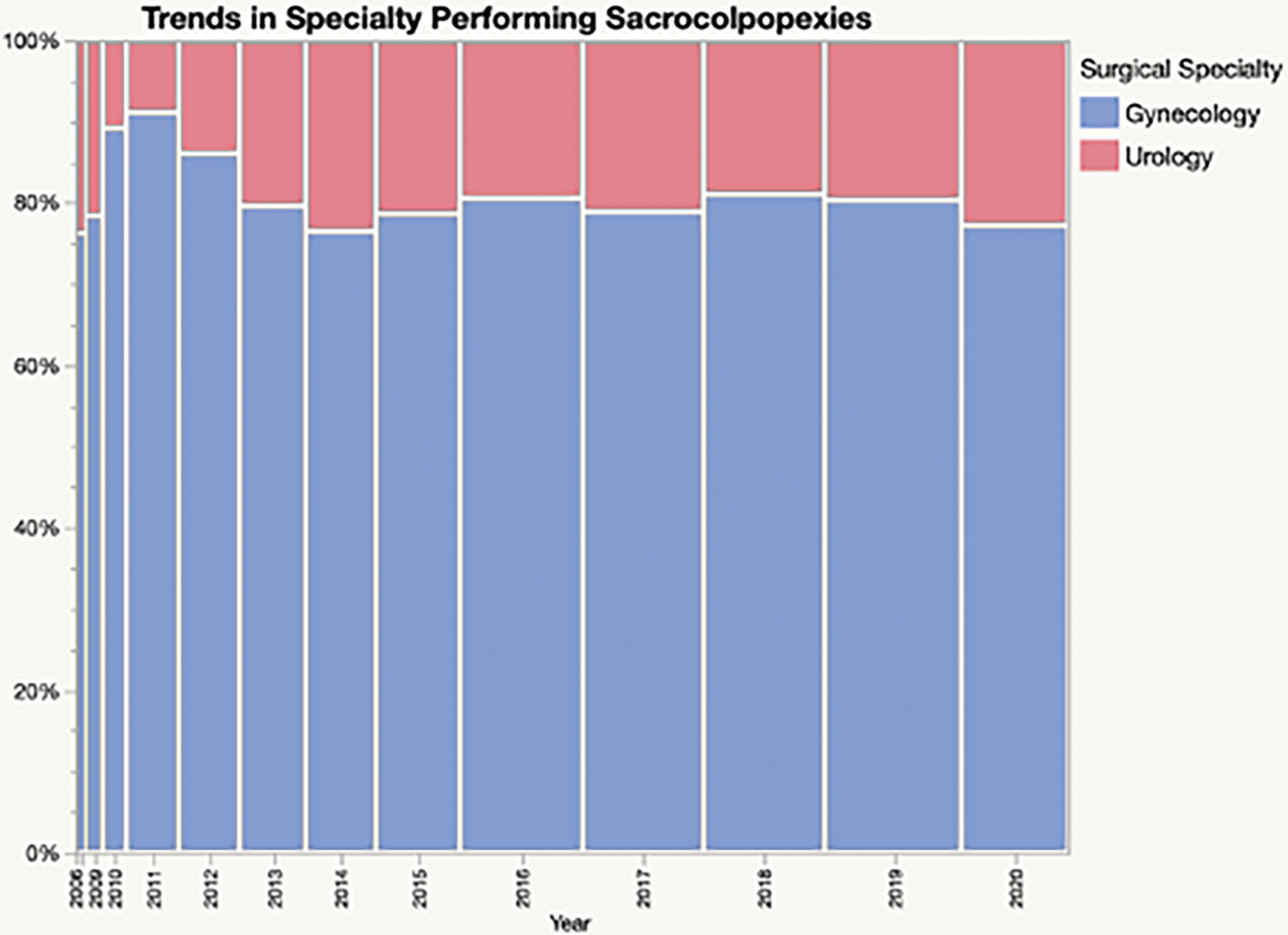
FIGURE 1. Percentage of SCPs performed by urologists and gynecologists over time. Width of bar is proportional to the total number of cases performed in year
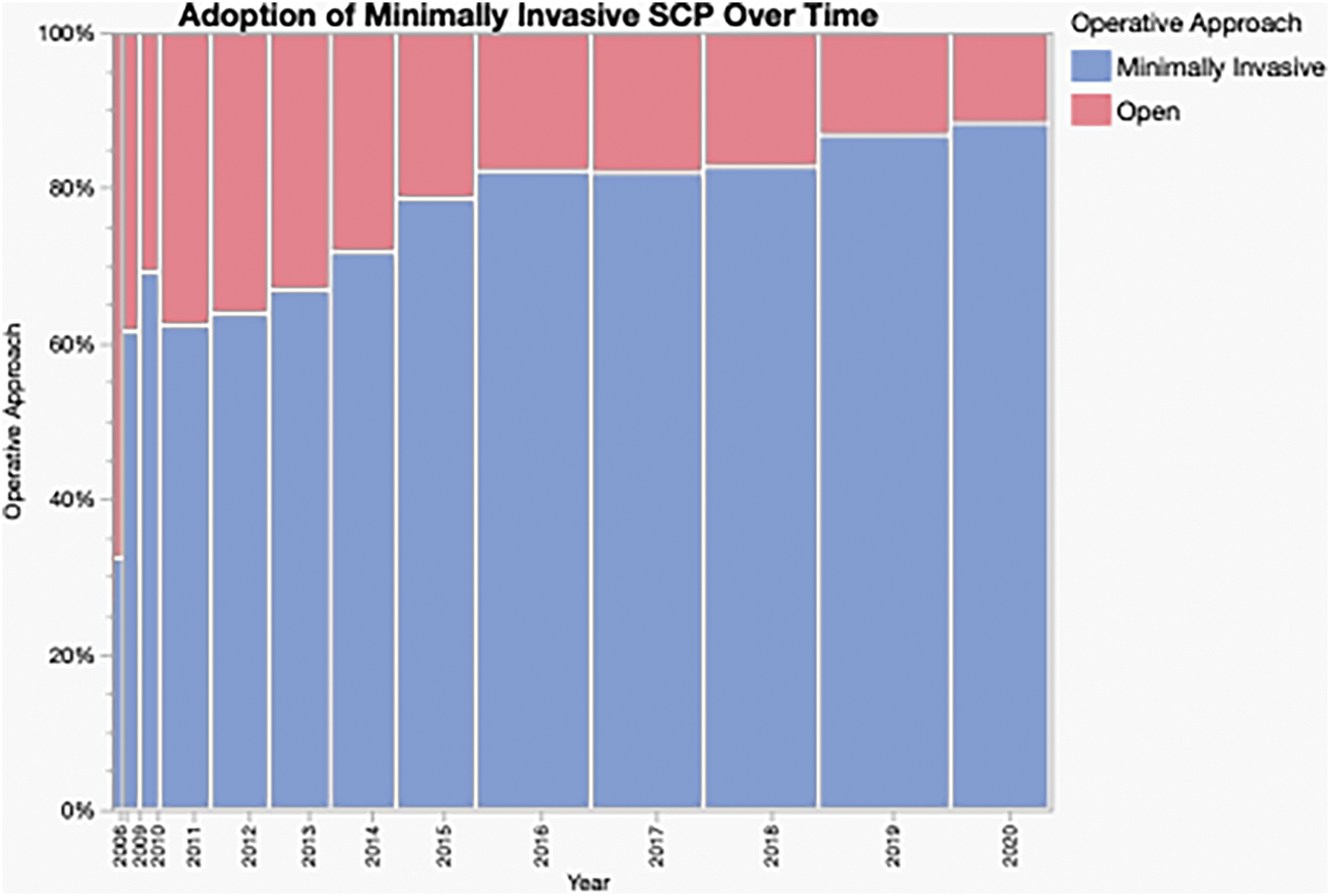
FIGURE 2. Percentage of SCPs performed by open or minimally invasive approach reflecting adaptation over time. Width of bar is proportional to the total number of cases performed in year
Our study shows most SCPs were performed by gynecologists compared to urologists, about 80% vs. 20%, respectively. There was a brief increase in cases performed by gynecologists (91%) in 2011, though this normalized by 2013; this could be explained by sampling error from the rapid increase in institutions participating in NSQIP in 2011. Census data from 2016 showed that 937 (71%) gynecologists and 382 (29%) urologists in the United States are board-certified in URPS.16 This is reflected in our data, as the case distribution of SCPs leans heavily towards gynecology.10
In 2012, the female pelvic and reconstructive surgery fellowship was approved in response to a urology and gynecology partnership advocating a need to advance care for women; this was recently redesignated as URPS.9,17 This fellowship is a unique collaboration. There are 69 approved programs—15 urology and 54 gynecology—with uniform case log requirements.17 The duration of fellowship training reflects the difference in the duration of residency programs, as urology residency is 5–6 years, while OBGYN is 4 years; therefore URPS fellowship programs are 2 years for urologists and 3 years for gynecologists.18
Despite a difference in residency training, our data shows no significant difference in outcomes in any of the analyzed parameters: 30-day minor complications, major complications, readmissions, reoperations, or mortality. The slightly increased rate of DVTs in cases performed by urologists could be explained by an older patient population with more medical comorbidities. There was no significant difference in operative time or hospital LOS. Our data is consistent with previous literature showing SCP as a widely accepted procedure with low complication rate. One meta-analysis of robotic SCP showed low complication rates, with cystotomy (2.6%), wound infection (2.4%), small bowel obstruction (0.7%) enterotomy (0.3%) and post site hernia (0.3%).19
Although our study demonstrates no significant quality difference between specialties, this is within the setting of urologists operating on overall frailer and older patients. Our study shows urologists operated on significantly frailer patients who were four years older, had more cardiovascular and pulmonary comorbidities, and overall reported higher ASA scores. This finding was corroborated by an earlier study comparing urology vs. gynecology for sling procedures.10 The authors explained this difference as a result of likely variation in referral pattern.10 Additionally, this may reflect a difference in residency training between urologists and gynecologists. Within OBGYN residency, providers spend a significant amount of time learning obstetrics, which inherently has a younger population with less medical comorbidities. Conversely, urologic training involves more time in the operating room and includes treatment of pathologies, such as urologic cancers, renal disease, benign prostate hypertrophy, and voiding dysfunction, that average toward older and unhealthy patient populations that present to the urology clinic and operating room. Conversely, gynecologists may be more comfortable with vaginal surgery; these procedures were not included in our study. Importantly, obliterative treatment for prolapse is common among older, frailer patients, though NSQIP data does not allow for surgeon level comparisons to potentially inform this substitution effect.
As expected, there was an increased risk of utilization of MIS over the study period; urologists performed particularly more SCPs via a MIS approach compared to gynecologists (84% vs. 77% p < 0.0001). The increased usage of MIS is likely reflective of increased comfort with surgical robotic technology since its introduction in the early 2000s.
Our database study has inherent limitations of selection bias given its retrospective nature.10 Further, the NSQIP database offers a national spread of data, though not all hospitals are included and this may not be a representative national sample. Additionally, we are limited by the variables collected and accuracy of data abstraction. Further, the data only provides the surgical specialty for the designated primary surgeon, though there are often joint cases where a gynecologist performs hysterectomy while a urologist performs SCP. The data provided does not stratify based on accredited URPS surgeons vs. providers who simply incorporate URPS into their practice. This would be a helpful variable to analyze in future studies of the impact of accreditation and specialty on safety and outcomes. Additionally, NSQIP does not stratify based on POP stage or reintervention cases. Within the parameters of the utilized database, we analyzed short-term complications within 30 days, but our analysis did not include long-term complications, clinical recurrence, or reintervention rates.
Overall, the large, national-level data we present over a 15-year course demonstrates helpful trends in SCP performance by gynecologists and urologists. To our knowledge, this is the first analysis of SCP evaluating patient demographics, surgical outcomes, and the utilization of MIS approaches in the 21st century.
The division of cases with urologists performing roughly 20% of SCPs and gynecologists performing roughly 80% of SCPs has mostly remained stable. From 2006–2020 there was an upward trend in increased utilization of MIS approach for SCP. Our results show no difference in 30-day surgical outcomes for SCPs performed by urologists compared to gynecologists. However, urologists tend to perform more minimally invasive procedures and operate on older, more frail patients, highlighting the differences in practice patterns between the two specialties.
Acknowledgement
Not applicable.
Funding Statement
The authors received no specific funding for this study.
Availability of Data and Materials
Data available on request from the authors. The data that support the findings of this study are available from the corresponding author, AMM, upon reasonable request.
Author Contributions
The authors confirm contribution to the paper as follows: study conception and design: Yash B. Shah, Rishabh K. Simhal, Alana M. Murphy; data collection: Rishabh K. Simhal; analysis and interpretation of results: Maria J. D’Amico; draft manuscript preparation: Yash B. Shah, Courtney E. Capella, Whitney Smith, and Alana Murphy. All authors reviewed the results and approved the final version of the manuscript.
Ethics Approval
Not applicable.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol 2010;116(5):1096–1100. doi:10.1097/AOG.0b013e3181f73729. [Google Scholar] [CrossRef]
2. Zhang W, Cheon WC, Zhang L, Wang X, Wei Y, Lyu C. Comparison of the effectiveness of sacrospinous ligament fixation and sacrocolpopexy: a meta-analysis. Int Urogynecol J 2022;33(1):3–13. doi:10.1007/s00192-021-04823-w. [Google Scholar] [CrossRef]
3. Yang J, He Y, Zhang X et al. Robotic and laparoscopic sacrocolpopexy for pelvic organ prolapse: a systematic review and meta-analysis. Ann Transl Med 2021;9(6):449. doi:10.21037/atm-20-4347. [Google Scholar] [CrossRef]
4. Slopnick EA, Petrikovets A, Sheyn D, Kim SP, Nguyen CT, Hijaz AK. Surgical trends and patient factors associated with the treatment of apical pelvic organ prolapse from a national sample. Int Urogynecol J 2019;30(4):603–609. doi:10.1007/s00192-018-3769-1. [Google Scholar] [CrossRef]
5. Schachar JS, Matthews CA. Robotic-assisted repair of pelvic organ prolapse: a scoping review of the literature. Transl Androl Urol 2020;9(2):959–970. doi:10.21037/tau.2019.10.02. [Google Scholar] [CrossRef]
6. Fatehchehr S, Rostaminia G, Gardner MO, Ramunno E, Doyle NM. Robotic surgery training in gynecologic fellowship programs in the United States. JSLS 2014;18(3):e2014.00402. doi:10.4293/JSLS.2014.00402. [Google Scholar] [CrossRef]
7. Catanzarite T, Tan-Kim J, Nguyen JN, Jakus-Waldman S, Menefee SA. A novel, structured fellow training pathway for robotic-assisted sacrocolpopexy. Perm J 2021;25:20.224. doi:10.7812/TPP/20.224. [Google Scholar] [CrossRef]
8. Turner SR, Mormando J, Park BJ, Huang J. Attitudes of robotic surgery educators and learners: challenges, advantages, tips and tricks of teaching and learning robotic surgery. J Robot Surg 2020;14(3):455–461. doi:10.1007/s11701-019-01013-1. [Google Scholar] [CrossRef]
9. Weissbart SJ, Wein AJ, Smith AL. Female pelvic medicine and reconstructive surgery-what does certification mean? Curr Urol Rep 2018;19(5):30. doi:10.1007/s11934-018-0785-0. [Google Scholar] [CrossRef]
10. James MB, Theofanides MC, Sui W, Onyeji I, Badalato GM, Chung DE. Sling procedures for the treatment of stress urinary incontinence: comparison of national practice patterns between urologists and gynecologists. J Urol 2017;198(6):1386–1391. doi:10.1016/j.juro.2017.06.093. [Google Scholar] [CrossRef]
11. Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-factor modified frailty index using American college of surgeons NSQIP data. J Am Coll Surg 2018;226(2):173–81 e8. doi:10.1016/j.jamcollsurg.2017.11.005. [Google Scholar] [CrossRef]
12. Fagenson AM, Powers BD, Zorbas KA et al. Frailty predicts morbidity and mortality after laparoscopic cholecystectomy for acute cholecystitis: an ACS-NSQIP Cohort analysis. J Gastrointest Surg 2021;25(4):932–940. doi:10.1007/s11605-020-04570-1. [Google Scholar] [CrossRef]
13. Arya S, Varley P, Youk A et al. Recalibration and external validation of the risk analysis index: a surgical frailty assessment tool. Ann Surg 2020;272(6):996–1005. doi:10.1097/SLA.0000000000003276. [Google Scholar] [CrossRef]
14. Dittman JM, Lavingia KS, Larson RA. Elevated Risk Analysis Index (RAI) frailty scores are independently associated with adverse outcomes in lower extremity surgical revascularizations similarly across genders. Ann Vasc Surg 2022;87:47–56. doi:10.1016/j.avsg.2022.04.004. [Google Scholar] [CrossRef]
15. Suskind AM, Walter LC, Jin C et al. Impact of frailty on complications in patients undergoing common urological procedures: a study from the American College of Surgeons National Surgical Quality Improvement database. BJU Int 2016;117(5):836–842. doi:10.1111/bju.13399. [Google Scholar] [CrossRef]
16. Christakis MK, Shore EM, Pulver A, McDermott CD. Female pelvic medicine and reconstructive surgery in Canada: a survey of obstetrician-gynecologists and urologists. Female Pelvic Med Reconstr Surg 2017;23(3):195–203. doi:10.1097/SPV.0000000000000360. [Google Scholar] [CrossRef]
17. Gerjevic KA, Brandes E, Gormley EA, Auty SG, Strohbehn K. Trends among female pelvic medicine and reconstructive surgery fellowships and graduates. Female Pelvic Med Reconstr Surg 2022;28(6):e211–e214. doi:10.1097/SPV.0000000000001186. [Google Scholar] [CrossRef]
18. Steers WD. Establishing the subspecialty of female pelvic medicine and reconstructive surgery in the United States of America. Arab J Urol 2013;11(2):113–116. doi:10.1016/j.aju.2013.01.003. [Google Scholar] [CrossRef]
19. Hudson CO, Northington GM, Lyles RH, Karp DR. Outcomes of robotic sacrocolpopexy: a systematic review and meta-analysis. Female Pelvic Med Reconstr Surg 2014;20(5):252–260. doi:10.1097/SPV.0000000000000070. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools