 Open Access
Open Access
ARTICLE
Post-operative outcomes in rectourethral fistula repair using gracilis interposition flap
1 Department of Urology, Medical University of South Carolina, Charleston, SC 29425, USA
2 Department of Colorectal Surgery, Medical University of South Carolina, Charleston, SC 29425, USA
3 Department of Plastic Surgery, Medical University of South Carolina, Charleston, SC 29425, USA
* Corresponding Authors: Gabrielle Yankelevich. Email: ,
Canadian Journal of Urology 2025, 32(1), 37-42. https://doi.org/10.32604/cju.2025.064684
Received 23 June 2024; Accepted 10 January 2025; Issue published 20 March 2025
Abstract
Objectives: To assess outcomes of rectourethral fistula repair utilizing a gracilis flap in a largely radiated cohort. Patients and Methods: We performed a retrospective review of all gracilis interposition flap reconstruction surgeries performed for RUF at a university hospital in South Carolina between January 2010 and June 2023. All repairs utilized a multidisciplinary approach with urology, colorectal, and plastic surgery teams. Post-operatively, patients were maximally drained with foley catheter and suprapubic tube (SPT). Initial voiding cystourethrogram (VCUG) was performed at 4 weeks post-repair. If there was a persistent leak, catheter drainage was maintained for 4 additional weeks and VCUG was repeated. Success was defined as absence of leak on VCUG within 3 months after surgery. Results: 22 patients met inclusion criteria. 68% of patients had history of external beam radiation therapy (EBRT), 13.6% had brachytherapy, and 40.9% had cryotherapy. Initial post-operative VCUG was negative in 10 patients (45.5%). Of the 12 patients with a persistent fistula, 5 (42%) had no evidence of fistula on subsequent VCUG after 4 weeks. Overall, 68% of patients were successfully treated with gracilis interposition flap. There was a significant difference of repair success based on EBRT status (p < 0.05). Conclusions: We report a success rate of 68% for gracilis flap repair of RUF. Our cohort had a higher rate of prior radiation therapy compared to other studies. A clinically significant portion of patients with an initial positive VCUG will seal their fistula with prolonged catheter drainage. Gracilis interposition flap is a reasonable surgical treatment for RUF.Keywords
Rectourethral fistula (RUF) is a rare, but devastating `therapies. The incidence of RUF after prostatectomy, radiation, and cryotherapy are 0.9–9%,1 0.5–4%,2 and 0.5–4%3, respectively. Approaches to RUF repair include prolonged urinary catheter drainage or surgical approaches such as a trans-sphincteric approach (York-Mason), urinary and fecal diversion, abdominal approach, or a transperineal approach with a flap.4 The approach for management is dictated by the classification of RUF as simple or complex.4,5 The factors that classify as RUF as complex include size (>2 cm), severe urethral stricture, and/or history of radiation or ablative tissue damage.4,5 Patients who have complex RUFs should be treated with surgical management.4,5
RUF repair utilizing a transperineal approach with gracilis muscle interposition flap has been documented in several retrospective studies as the gracilis muscle is highly vascularized and able to be mobilized via a transperineal approach.6–8 We present our retrospective study including 22 patients, and our study is unique in that it is a largely radiated cohort and we used a standardized imaging pathway.
All repairs were performed utilizing a multidisciplinary approach with urology, colorectal, and plastic surgery team involvement. Plastic surgery harvested and transposed the gracilis flap, while colorectal and urologic surgery teams performed the perineal dissection and primary closure of rectum and urethra, respectively.
Patients were placed into an exaggerated lithotomy position with five folded blankets (Figure 1). The patient was prepped to the umbilicus in the cephalad direction, bilateral legs to the knee laterally, and caudad to below the anus, to allow all surgeons ability to work without re-draping the patient. A suprapubic tube (SPT) was placed via cystoscopic guidance by the urology team, and a urethral catheter was placed. If possible, the fistula tract was cannulated with a wire cystoscopically to aid in identification during perineal dissection. A perineal incision along the mucocutaneous border from the ischial tuberosity in the shape of an inverted U was performed (Figure 2A) and dissection was carried out to the area of the fistula by urology and colorectal surgery teams (Figure 2B). Colorectal surgery typically closed the rectal component using 2 layers of vicryl transversally and urology closed the urethral portion with multiple layers of vicryl sutures, with a leak test to ensure a watertight closure (Figure 2C). Once this was completed, the plastic surgery team isolated a segment of gracilis muscle, typically from the left leg which was secured in the space between the rectal and urethral suture lines (Figure 2D). After, the dead space was closed in multiple layers using vicryl and a penrose 1/4-inch penrose drain was placed within this space and brought out to the skin, typically on the left side of the perineum. The perineal skin was then closed and the plastic surgeons simultaneously reapproximated the leg incision with several layers of synthetic absorbable suture, placed a 15 Fr drain, and wrapped the leg in ace wrap.

FIGURE 1. Artist rendition of patient positioning

FIGURE 2. (A). Artist rendition of initial perineal incision. (B). Artist rendition of perineal dissection with exposure of fistula on rectum and urethra. (C). Artist rendition of perineal dissection with closure of fistula on rectum and urethra (D). Artist rendition of gracilis interposition flap
Post operatively, all patients were managed with foley catheter and suprapubic tube (SPT) drainage with initial voiding cystourethrogram (VCUG) performed at 4 weeks post. If there was a persistent leak, catheter drainage was maintained for 4 additional weeks and VCUG was repeated. Success was defined as absence of leak on VCUG within 3 months post-operatively.
After receiving Institutional Review Board (IRB) approval, we performed a retrospective review of all gracilis interposition flap reconstruction surgeries performed for RUF at a university hospital in South Carolina between January 2010 and June 2023. Inclusion criteria was a diagnosis of rectourethral fistula and history of rectourethral fistula repair with a gracilis flap between 2010 to 2023. Exclusion criteria consisted of prior failed RUF repair. Age, prior prostate cancer treatment type, smoking history, bowel diversion status, postoperative VCUG results, and postoperative complications were indexed. Statistical analysis was performed using excel and SPSS. Chi square test was used to test for the difference in failure rates between the radiated and non-radiated patients.
22 patients met inclusion criteria. All had a pre-operative fistula biopsy and pre-operative bowel diversion. 68% of patients had a history of external beam radiation therapy (EBRT), 13.6% had brachytherapy, and 40.9% had cryotherapy (Tables 1 and 2). There was a mean follow-up of 13.7 months.


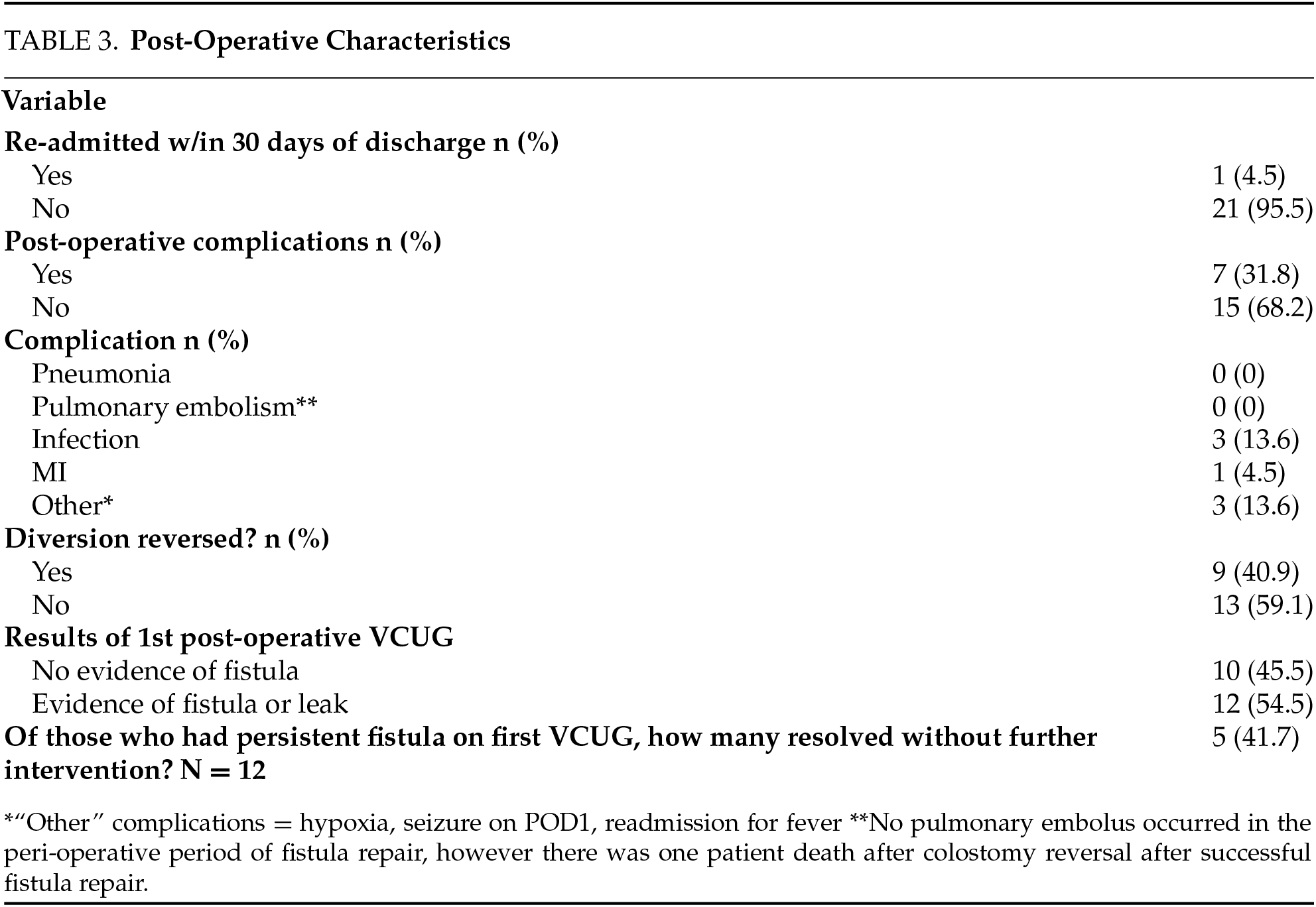
Initial post-operative VCUG was negative for RUF in 10 patients (45.5%). Of the 12 patients with a persistent fistula, 5 (42%) had no evidence of fistula on subsequent VCUG after 4 weeks (Table 3). Overall, 68% of patients were successfully treated with gracilis interposition flap. 3 patients (13.6%) underwent or are planned for simple cystectomy diversion. Of the 7 failures, 3 (42.8%) had a history of salvage cryotherapy and 7 (100%) had history of EBRT. Of the 15 successes, 6 (40%) had history of cryotherapy and 7 (46.6%) had history of EBRT. There was a significant success difference of the repair based on EBRT status (p < 0.05). There was no significant difference in success based on history of cryotherapy (p < 0.05). There were 7 post-operative complications, primarily Clavien-Dindo Class I and II.
Therefore, based on our data, we propose a suggested RUF pathway to assist in clinical decision-making for complex fistulas (Figure 3).

FIGURE 3. Suggested RUF repair pathway
Suggested RUF pathway
In 2010, Vanni et al. compared RUF repair in 35 nonradiated patients to 39 radiated/ablated patients.7 Pre-operatively in the radiated/ablated group, they reported 74% had undergone fecal diversion prior to fistula repair whereas 23% underwent laparoscopic ileostomy concurrent with fistula closure.7 This study suggests that diversion should be performed in all cases of radiation or cryosurgery to prevent rectal wall distension and improve fistula closure rates.7 Of the radiated/ablated patients, 72% underwent repair with a single gracilis flap, 23% underwent repair with 2 gracilis flaps, and 87% required a buccal mucosal graft on the prostatic urethral defect.7 At a mean follow-up of 23 months, 84% of these patients achieve successful closure versus 100% of the non-radiated patients.7 Additionally, Vanni et al. reported that 13% of patients with radiation/ablation history required prolonged catheter drainage (longer than 8 weeks) to allow for closure.7 They found that the gracilis flap could be readily harvested, regardless of patient age or body type, with a reliable vascular supply and ultimately allow for successful repair.7 Their study complements our study in that ~50% of patients had radiation or ablation history and were able to be successfully repaired.
In 2011, Samplaski et al. reported their findings with 13 patients who underwent transperineal repair with gracilis flap for complex RUF with 9 patients that had a history of brachytherapy, radiation therapy, cryoablation or some combination of these.6 Similar to Vanni et al., they selectively utilized a buccal mucosal graft in addition to a gracilis interposition flap.6 All 13 patients underwent preoperative fecal diversion with loop ileostomy, loop colostomy, or end colostomy.6 They performed a VCUG at 6 weeks and all 13 patients had a negative VCUG at this time.6 After fecal diversion reversal, 12 of the 13 patients remained RUF-free after a short median follow-up of 2.5 months.6 They also assessed quality of life measures for urinary and fecal function.6 A significant amount of patients reported urinary urgency (50%), urge incontinence (42%), and stress incontinence (58.4%), with higher bother in patients who had undergone radiation or ablation procedures.6 Fecal outcome showed less bothersome symptoms than urinary outcomes, with only 25% of patients reporting fecal incontinence.6 They reported that though patients can experience urinary and fecal incontinence, the rate of closure with a gracilis flap was high with a reasonable overall quality of life.6
In 2008, Ghoniem et al. published their data on RUF with gracilis flap in 25 patients.8 6 of these patients had a history of prostatectomy and 19 had a history of radiation or cryoablation with or without prostatectomy.8 They reported 100% successful fistula repair with a mean follow-up of 28 months.8 Similar to Samplaski’s study, they assessed urinary and fecal continence with findings of 52% and 76%, respectively.8 These findings supported Samplaski’s findings that the gracilis interposition flap allowed for improved repair rates and that bowel outcomes had a decreased incidence rate postoperatively.8
Our study adds to the existing data in the literature and proposes a pathway for management, with demonstration of successful repair, despite an initial positive VCUG, by prolonged catheter drainage. Future considerations would be to utilize a buccal mucosal graft in addition to gracilis interposition flap as several papers have demonstrated improved outcomes with this approach. Future studies planned at our institution will include use of preoperative and postoperative hyperbaric oxygen (HBO). HBO is used in plastic surgery for skin grafts and flaps, and urology for radiation sequelae, such as radiation cystitis.9 We suspect that it can be utilized as an adjunct tool to promote wound healing prior to and after fistula repair.
We report a success rate of 68% for gracilis flap repair of RUF in the setting of local prostate cancer treatment, with our study having a high rate of prior radiation therapy. We propose a pathway for serial VCUG at 4-week intervals given a clinically significant portion of patients with an initial positive VCUG will seal their fistula with prolonged catheter drainage. Ultimately, by utilizing a multidisciplinary approach, a gracilis interposition flap is a reasonable surgical treatment for RUF.
Acknowledgement
Not applicable.
Funding Statement
The authors received no specific funding for this study.
Author Contributions
All authors contibuted to the conception/design of the study, drafting or revising the article, and final approval of the article. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The patient data used in this study are not publicly available due to ethical considerations regarding patient privacy. De-identified data may be accessed upon reasonable request from the corresponding author with appropriate institutional review board approval and adherence to data protection regulations.
Ethics Approval
The Institutional Review Board determined that this study (Pro00134989) is exempt as it was deemed “Not Human Subjects Research” given its retrospective nature.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study.
References
1. Kitamura H, Tsukamoto T. Rectourinary fistula after radical prostatectomy: review of the literature for incidence, etiology, and management. Prost Can 2011;2011(6):629105. doi:10.1155/2011/629105. [Google Scholar] [CrossRef]
2. Yu KR, Keller-Biehl L, Smith-Harrison L et al. Radiation-induced recto-urinary fistula: a dreaded complication with devastating consequences. Surg Pract Sci 2023;15(3):100216. doi:10.1016/j.sipas.2023.100216. [Google Scholar] [CrossRef]
3. Mouraviev V, Spiess PE, Jones JS. Salvage cryoablation for locally recurrent prostate cancer following primary radiotherapy. Eur Urol 2012;61(6):1204–1211. doi:10.1016/j.eururo.2012.02.051. [Google Scholar] [CrossRef]
4. Chen S, Gao R, Li H, Wang K. Management of acquired rectourethral fistulas in adults. Asian J Urol 2018;5(3):149–154. doi:10.1016/j.ajur.2018.01.003. [Google Scholar] [CrossRef]
5. Ramírez-Martín D, Jara-Rascón J, Renedo-Villar T, Hernández-Fernández C, Lledó-García E. Rectourethral fistula management. Curr Urol Rep 2016;17(3):22. doi:10.1007/s11934-016-0578-2. [Google Scholar] [CrossRef]
6. Samplaski MK, Wood HM, Lane BR, Remzi FH, Lucas A, Angermeier KW. Functional and quality-of-life outcomes in patients undergoing transperineal repair with gracilis muscle interposition for complex rectourethral fistula. Urology 2011;77(3):736–741. doi:10.1016/j.urology.2010.08.009. [Google Scholar] [CrossRef]
7. Vanni AJ, Buckley JC, Zinman LN. Management of surgical and radiation induced rectourethral fistulas with an interposition muscle flap and selective buccal mucosal onlay graft. J Urol 2010;184(6):2400–2404. doi:10.1016/j.juro.2010.08.004. [Google Scholar] [CrossRef]
8. Ghoniem G, Elmissiry M, Weiss E, Langford C, Abdelwahab H, Wexner S. Transperineal repair of complex rectourethral fistula using gracilis muscle flap interposition—can urinary and bowel functions be preserved? J Urol 2008;179(5):1882–1886. doi:10.1016/j.juro.2008.01.021. [Google Scholar] [CrossRef]
9. Bhutani S, Vishwanath G. Hyperbaric oxygen and wound healing. Indian J Plast Surg 2012;45(2):316–324. doi:10.4103/0970-0358.101309. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools